Abstract
The objective of this systematic review was to examine the influence of treatments for postmenopausal osteoporosis (parathyroid hormone [PTH], bisphosphonates, strontium ranelate, and denosumab) on bone quality and discuss the clinical implications. Most bone-quality data for PTH is from teriparatide. Teriparatide results in a rapid increase in bone-formation markers, followed by increases in bone-resorption markers, opening an “anabolic window,” a period of time when PTH is maximally anabolic. Teriparatide reverses the structural damage seen in osteoporosis and restores the structure of trabecular bone. It has a positive effect on cortical bone, and any early increases in cortical porosity appear to be offset by increases in cortical thickness and diameter. Bisphosphonates are antiresorptive agents which reduce bone turnover, improve trabecular microarchitecture, and mineralization. Concerns have been raised that the prolonged antiresorptive action of bisphosphonates may lead to failure to repair microdamage, resulting in microcracks and atypical fragility. Strontium ranelate is thought to have a mixed mode of action, increasing bone formation and decreasing bone resorption. Strontium ranelate improves cortical thickness, trabecular number, and connectivity, with no change in cortical porosity. Denosumab exerts rapid, marked, and sustained effects on bone resorption, resulting in falls in the markers of bone turnover. Evidence from bone-quality studies suggests that treatment-naive women, aged 60–65 years, with very low BMD T scores may benefit from PTH as primary therapy to improve bone substrate and build bone. Post-PTH treatment with bisphosphonates will maintain improvements in bone quality and reduce the risk of fracture.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Rationale for Exploring Measures of Bone Quality
Typically, agents for the treatment of osteoporosis have been assessed in 3-year trials with vertebral fracture as the primary end point and bone mineral density (BMD) as a secondary end point. However, as a measure of the amount of bone, BMD does not always reliably predict fracture risk [1].
Data from the large National Osteoporosis Risk Assessment (NORA) study revealed that only 6.4% of postmenopausal women with an osteoporotic fracture (including hip fracture) had T scores of <−2.5 (the World Health Organization definition of osteoporosis) in the year preceding the fracture [2]. Although fracture rates were highest in this group of women, they experienced only 18% of osteoporotic fractures overall. More than one-half (52%) of the women with fractures were osteopenic (T score −2.5 to −1) (see Fig. 1).
The majority of osteoporotic fractures are in women with osteopenia [2]
Studies of agents used in the treatment of osteoporosis reveal that although low BMD is correlated with increased fracture risk, increasing BMD (using drug treatment) seems to account for only a small percentage of the reduction in fracture risk observed [3]. Data suggest that only 16–28% of the reduction in vertebral fracture risk seen with the bisphosphonates (alendronate and risedronate) and 30–41% of the reduction in risk seen with parathyroid hormone (PTH) can be attributed to increases in lumbar spine BMD. Therefore, the majority of the fracture risk reduction is caused by improvements in non-BMD determinants of bone strength [3].
Typically, fracture-prevention studies for agents for the treatment of osteoporosis are undertaken over 3 years,; and although longer-term postmarketing studies have been carried out, numbers of patient dropouts are considerable and long-term safety data are unreliable. Recently, potential long-term adverse effects of bisphosphonates have come to light, including microcracks [4], atypical fractures [5–7], and osteonecrosis of the jaw [8–10].
Given that BMD is only part of the antifracture picture and the potential long-term concerns with treatment, other measures of bone fragility such as bone quality have become increasingly important. However, bone quality is difficult, impractical, and expensive to measure in clinical practice. Therefore, BMD remains the standard measure of bone strength, despite the limitations. Bone quality has remained an academic afterthought, although it has the potential to explain, in large part, the underlying impact of treatments for osteoporosis.
Bone Quality
Bone quality together with bone density are the two key elements of bone strength. Although there is no clear consensus on the exact components of bone quality, it is influenced by bone turnover, mineralization, microarchitecture, geometry, and the accumulation of damage (Fig. 2).
Bone remodeling, the constant turnover of bone, helps to maintain tissue integrity by selectively removing damaged bone and replacing it with new bone. Bone remodeling is reduced with increasing age, and a reduction in the volume of bone resorbed coupled with an even greater reduction in the volume of bone formed leads to a net loss of bone in older people [11]. At the same time, the number of remodeling units within endosteal bone increases with age and there is a reduction in the formation of periosteal bone. The overall consequences of these age-related changes are cortical thinning, increased cortical porosity, thinning of the trabeculae, and loss of trabecular connectivity, all of which reduce bone quality and consequently bone strength [11].
Agents for the management of postmenopausal osteoporosis vary in their mode of action. PTH has an anabolic mode of action, directly increasing bone formation [12]. In contrast, the bisphosphonates and denosumab prevent the loss of bone by reducing bone resorption [13, 14]. The mechanism of action of strontium ranelate is uncertain, though a mixed mode of action has been suggested [15]; however, this has not been confirmed in studies using bone-biopsy specimens from postmenopausal women [16].
Objective
The objective of this systematic review is to examine the influence of agents used in the management of postmenopausal osteoporosis (PTH, bisphosphonates, strontium ranelate, and denosumab) on bone quality and discuss the clinical implications of these effects. The selective estrogen receptor modulator (SERM) raloxifene was not included since it is not commonly used in clinical practice as an antiosteoporosis treatment, due in part to the lack of effect on nonvertebral fracture risk.
Methods
Clinical trials assessing bone quality (bone microarchitecture and markers of bone turnover) in postmenopausal women with osteoporosis receiving pharmacological treatment for osteoporosis (PTH, bisphosphonates, strontium ranelate, and denosumab) were included. Review articles which considered bone quality were also included. No language restrictions were imposed.
-
Types of article: clinical trials and review articles
-
Types of population: women with postmenopausal osteoporosis
-
Types of intervention: pharmacological treatment for osteoporosis with bisphosphonates (alendronate, risedronate, ibandronate, zoledronate), strontium ranelate, PTH(1–84 and 1–34), and denosumab
-
Types of outcome measure: bone quality, bone microarchitecture, bone histomorphometry, markers of bone turnover (markers of bone formation including osteocalcin and alkaline phosphatase as well as markers of bone resorption including collagen type 1 telopeptides [Ctx and Ntx])
Information Sources
Studies were identified by searching electronic databases (Medline and Embase) and scanning reference lists of articles.
The search was applied to Medline (1996–2009). We hand-searched Osteoporosis International, Bone, Journal of Bone and Mineral Research, and Calcified Tissue International for the previous 3 years.
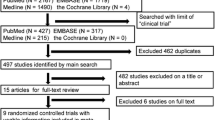
Search
We used the following search terms: alendronate, risedronate, ibandronate, zoledronate, strontium ranelate, teriparatide, preotact, hPTH, 1–84, 1–34, denosumab, bone quality, bone strength, bone microarchitecture, bone histomorphometry, osteocalcin, alkaline phosphatase, Ctx, Ntx, bone turnover, osteoporosis. Searches were limited to adult humans. See Fig. 3 and appendix for further details.
Parathyroid Hormone
Two PTH analogues are available as treatment for postmenopausal osteoporosis. Teriparatide (Forsteo), recombinant human PTH containing the amino acid sequence 1–34 of the complete molecule, and Preotact, recombinant human PTH identical to the full-length native 1–84-amino acid sequence. In the United Kingdom, the licensed doses are 20 μg/day for teriparatide and 100 μg/day for PTH(1–84). The majority of data on bone quality come from studies using teriparatide.
Teriparatide has been shown to reduce the risk of fracture in postmenopausal women with osteoporosis. The Fracture Prevention Trial [17] enrolled postmenopausal women with osteoporosis (defined as at least one moderate or two mild atraumatic vertebral fractures on X-ray of the thoracic and lumbar spine) to daily subcutaneous injections of either placebo (n = 544), teriparatide 20 μg (n = 541), or teriparatide 40 μg (n = 552) for 18 ± 5, 18 ± 6, and 17 ± 6 months, respectively. With teriparatide 20 μg, BMD increased by 9% at the lumbar spine and by 3% at the hip but remained unchanged at the radius. The prespecified end point was new fragility fracture. Patients in the teriparatide arms had a reduction in new vertebral fractures (14% in the placebo arm vs. 5 and 4% in the 20- and 40-μg teriparatide arms, respectively; P ≤ 0.001) and in nonvertebral fractures (6 vs. 3% in both teriparatide arms). The reduction in hip fracture was not significant; however, the Fracture Prevention Trial was not designed to show a reduction in hip fracture, and to date no trials have been conducted with teriparatide (or PTH[1–84]) with a hip fracture end point. Given the concerns over this lack of hip-fracture data, evidence of an improvement in cortical bone quality with PTH therapy has become increasingly important.
The reduction in fracture in the Fracture Prevention Trial was similar in both the 20- and 40-μg teriparatide arms. However, only the 20-μg dose is licensed in the United Kingdom, although for completeness bone-quality data are presented for both doses.
Mode of Action
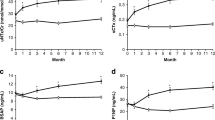
PTH is an anabolic agent, resulting in increased deposition of bone [12]. Teriparatide leads to a rapid increase in bone-formation markers, followed by increases in bone-resorption markers. A biopsy substudy of the Fracture Prevention Trial used paired iliac crest biopsies from placebo (n = 21) and teriparatide-treated (n = 36) patients. Biochemical markers of bone turnover revealed an early (within 28 days) increase in the markers of bone formation (bone alkaline phosphatase and procollagen 1 C-terminal propeptide [P1CP]). P1CP reached maximal levels within 1 month and bone alkaline phosphatase, at 12 months. The increase in bone-resorption markers (Ntx and deoxypyridinoline) was significantly different from placebo at 3 months; deoxypyridinoline reached maximal levels at 6 months and Ntx, at 12 months [18]. Changes in markers of bone formation at 1 month, which are highly predictive of outcome, correlated with improvements in bone structure after 22 months of treatment with teriparatide; but changes in markers of bone resorption did not. This sequence of events has led to the concept of the “anabolic window,” a period of time when the actions of PTH are maximally anabolic [19] (Fig. 4).
The anabolic window [19]
Bone formation with PTH appears to result from an increase in the rate of both remodeling and modeling. Unlike remodeling, modeling-based bone formation does not generally occur in normal adult bone. During modeling, bone is formed without prior resorption and leads to overfilling of bone-resorption pits and bone formation beyond the limits of the resorption pit [12] (Fig. 5).
Bone formation resulting from normal bone remodeling (top), bone modeling (middle), and combination remodeling/modeling (bottom) [12]
Evidence from markers of bone turnover (see above) and bone biopsies suggests that modeling occurs early in treatment, followed by remodeling later in treatment [12].
A 2-year study randomized 29 postmenopausal women with severe osteoporosis to intermittent teriparatide (50 μg/day for 28 days every 3 months) with or without calcitonin [20]. Bone biopsies after 28 days of treatment revealed significantly larger increases in bone formation with teriparatide than with untreated controls (n = 15), suggesting rapid deposition of bone onto quiescent bone surfaces. The number of osteoblasts per centimeter of bone surface was higher at 28 days than at 2 years, further suggesting modeling rather than remodeling early in treatment.
Histomorphometric analysis of 52 iliac crest biopsies from patients enrolled in the Fracture Prevention Trial revealed evidence of remodeling, mixed remodeling/modeling, and modeling in patients receiving teriparatide. Remodeling appeared as scalloped reversal lines interrupting the surrounding collagen fibers, mixed remodeling/modeling appeared as a mixture of very short scalloped cement lines and long smooth cement lines, and modeling hemiosteons appeared as smooth cement lines with parallel collagen fibers without interruption of adjacent bone tissue. Patients receiving placebo did not have mixed remodeling/modeling or modeling hemiosteons, which is consistent with a lack of physiological modeling in adults [21]. Patients receiving 40 μg teriparatide had significantly higher levels of modeling alone compared with those receiving the licenced dose of 20 μg. At the 20-μg dose of teriparatide, mixed remodeling/modeling and remodeling alone predominated and there was very little modeling alone.
PTH results in an increase in the trabecular remodeling rate as demonstrated by a threefold increase in activation frequency of trabecular remodeling over a 2-year treatment period [20]. Iliac crest bone biopsies from 27 postmenopausal women treated with teriparatide (50 μg) for 1 month were compared with 13 untreated controls [22]. Bone-formation rate on the trabecular and endocortical surfaces was 4.5- and fivefold higher, respectively, in the teriparatide arm. There was also a fourfold increase in bone-formation rate on the periosteal surface. On the trabecular and endocortical surfaces, the increased bone-formation rate was primarily due to remodeling, with some modeling on previously quiescent surfaces. Bone formation was associated with an increase in osteoblast apoptosis, which may reflect enhanced turnover of the osteoblast population [22].
An increase in bone resorption is seen after the initial increase in bone formation (see Fig. 4). Receptor activator for nuclear factor-κB ligand (RANKL), a key mediator of osteoclast differentiation, function, and survival, may mediate the increased bone resorption. A small study of 23 postmenopausal women with established osteoporosis treated with teriparatide (20 μg) for 12 months revealed a gradual but significant increase in RANKL. There was no change in osteoprotegerin (OPG), which competes for and neutralizes RANKL. The authors suggest that this may reflect an increase in active osteoblasts and in bone turnover [23].
Effect on Trabecular Bone
PTH reverses the structural damage seen in osteoporosis and restores the structure of trabecular bone, increasing both the volume and connectivity of the trabeculae.
A study using biopsy specimens from the Fracture Prevention Trial analyzed iliac crest bone in patients receiving placebo (n = 19) or teriparatide 20 or 40 μg (n = 32) after a mean treatment time of 19 months [24]. Teriparatide significantly increased trabecular bone volume compared with placebo (median change 14 vs. −24%, P = 0.001) as shown on two-dimensional (2-D) histomorphometry. There was a significant increase in connectivity (19 vs. −14%, P = 0.034) and improvements in the trabecular structure model index (an indicator of the number of rods and plates; 22 vs. 3%, P = 0.012) as shown on 3-D microcomputed tomography (μCT) with teriparatide compared to placebo.
A further study also using iliac crest–biopsy specimens from 36 women enrolled in the Fracture Prevention Trial found a significant and positive correlation between increases in BMD at the lumbar spine and femoral neck at 12 and 18 months and improvements in trabecular microarchitecture (including 2-D mean wall thickness, 3-D bone volume, 3-D trabecular thickness, 3-D trabecular separation, 3-D structural model index) at 22 months [3].
The effect of teriparatide on vertebral microarchitecture has been assessed using high-resolution CT scanning in 65 postmenopausal women. After 6 months of teriparatide, there were highly significant improvements in both trabecular microarchitecture and BMD [25]. After 12 months’ treatment with teriparatide, there were increases of 30% in apparent trabecular volume and 19% in apparent trabecular number.
The effect of PTH(1–84) on trabecular bone has also been assessed using iliac crest biopsies from postmenopausal women enrolled in a large placebo-controlled trial of PTH(1–84) [26]. Biopsies were available from eight women receiving placebo, eight receiving PTH(1–84) for 18 months, and seven receiving PTH(1–84) for 24 months. At 18 months, trabecular bone volume was 45–48% higher in the patients receiving PTH(1–84) compared with placebo. Trabecular number, thickness, connectivity density, and trabecular bone-formation rate were all higher in the PTH(1–84) patients than in the placebo patients.
Effect on Cortical Bone
PTH has a positive effect on cortical bone at both the microscopic and macroscropic levels. It stimulates periosteal and endosteal bone growth, resulting in increases in cortical thickness and cross-sectional area. Such changes appear to strengthen cortical bone despite the small changes in BMD at cortical sites such as the femoral neck and the radius and potential early increases in cortical porosity. Indeed, iliac crest biopsies do not show a significant increase in cortical porosity after treatment with teriparatide for up to 24 months [20, 24], and any potential adverse events on cortical bone appear to be offset by the increase in cortical thickness and diameter due to new periosteal bone apposition [27].
Teriparatide improves the structure of cortical bone in terms of cortical thickness [20, 24]. Postmenopausal women randomized to teriparatide (50 μg/day for 28 days every 3 months) with or without calcitonin for 2 years had an increase in cortical thickness of 23% versus untreated controls (P < 0.05) without significant changes in cortical porosity [20]. Analysis of iliac crest biopsies from patients in the Fracture Prevention Trial using 3-D μCT demonstrated a similar increase in cortical thickness of 22% compared with an increase of 3% in placebo-treated bone (P = 0.0012) without increases in cortical porosity [24]. Images obtained using 3-D μCT suggest that the increased cortical thickness seen with teriparatide results from increased bone formation at both the periosteal and endosteal surfaces [24]. Analysis of samples from the Fracture Prevention Trial (metacarpals, ulna, and radius) using digital X-ray radiogrammetry showed an increase in cortical thickness at all areas. Teriparatide increased the outer diameter and decreased the inner diameter of cortical bone compared with placebo [28].
A study which used 3-D quantitative CT (QCT) of the femoral neck in postmenopausal women with severe osteoporosis treated with teriparatide for 2 years revealed an increase in cortical cross-sectional area of 4.3% but no increase in total cross-sectional area, suggesting endosteal, but not periosteal, growth [29].
A small iliac crest–biopsy study in postmenopausal women receiving PTH(1–84) for 18 (n = 8) or 24 (n = 7) months or placebo (n = 8) found no change in cortical thickness or endocortical or periosteal bone-formation rate with PTH(1–84), although there was a trend toward increased cortical porosity when measured by μCT but not when measured by histomorphometric means [26]. The change in cortical porosity was similar at 18 and at 24 months, suggesting an early change which stabilizes later in treatment.
Effect on Bone Matrix
Teriparatide appears to stimulate the deposition of younger bone which is new, not fully mineralized bone, with divalent collagen cross-links. Material properties, such as matrix mineralization, hydroxyapatite characteristics, and collagen cross-linking, also have an impact on bone quality. Fourier transform infrared imaging (FTIRI) of bone sections can be used to investigate mineral properties [30]. Bone biopsies taken from patients entered in the Fracture Prevention Trial (n = 14 at 12 months [range 11–14 months] and n = 24 at study end point [range 19–24 months]) revealed that patients receiving teriparatide had significantly lower matrix mineralization, mineral crystallinity, and collagen cross-link ratio compared with those receiving placebo. The difference was significant at periosteal, endosteal, and trabecular bone sites (P < 0.025 versus placebo). Younger bone is more flexible and less likely to buckle on impact compared with older, more heavily mineralized bone, which has clear implications for the risk of fracture.
Effect on Bone Geometry
Teriparatide treatment leads to an increase in bending strength and a decrease in buckling ratio, which results in increased bone stability [29, 31, 32].
The impact of teriparatide on the structural geometry of bone has been assessed using repeated dual-energy X-ray absorptiometric (DXA) scans at the hip of 558 women from the Fracture Prevention Trial. The scans revealed significant increases in BMD and cross-sectional geometry at the femoral neck and intertrochanteric region but not at the femoral shaft [31]. The study showed dose-dependent increases in cross-sectional area and bending strength (defined as an increase in section modulus) and a decrease in local cortical instability (buckling ratio), which were significantly greater than in patients receiving placebo. The differences were statistically significant after 1 year of treatment and greater at the end of the study (1.8 years).
Zanchetta et al. [32] assessed bone geometry by peripheral QCT in the nondominant distal radius in 101 women from the Fracture Prevention Trial. Total bone mineral content, total and cortical bone areas, periosteal circumference, and axial and polar cross-sectional moment of inertia (architectural indicators of the bone’s resistance to bending and torsional loading, respectively) were significantly higher with teriparatide versus placebo.
Bisphosphonates
Bisphosphonates are antiresorptive agents which act via the inhibition of osteoclasts, leading to reduced bone turnover, increased bone mass, and improved mineralization [13]. Recently, it has been suggested that bisphosphonates (specifically alendronate) may also promote osteoblast proliferation and maturation [33].
The evidence base for bisphosphonates in the prevention of fracture in postmenopausal women is well established. Treatment with alendronate 10 mg/day results in statistically significant reductions in vertebral, nonvertebral, hip, and wrist fractures in patients with prior osteoporotic fracture or low BMD. For those patients without osteoporotic fracture or low BMD, treatment with alendronate results in a significant reduction in vertebral fracture but no significant reduction in fracture at other sites [34]. A similar picture is seen with risedronate 5 mg/day, although the reduction in wrist fractures in patients with prior fracture or low BMD was not statistically significant and there was no significant benefit in patients with normal BMD [35]. Treatment with a once-yearly infusion of zoledronate (5 mg) significantly reduces the risk of vertebral, nonvertebral, hip, and wrist fracture in postmenopausal women with osteoporosis [36]. In contrast, the evidence for ibandronate in postmenopausal women with osteoporosis supports a significant reduction in vertebral fracture only [37].
Recently, concern has been raised regarding the optimal treatment period for bisphosphonates [38]. There is evidence of benefit of treatment for up to 5 years with the bisphosphonates. Indeed, alendronate has been studied out to 10 years and risedronate out to 7 years; however, studies which continue for longer than 5 years have high levels of patient dropout and lack appropriate controls, and data should be viewed with caution. Furthermore, both alendronate and zoledronate bind strongly to the bone matrix and become internalized within bone; therefore, suppression of bone resorption continues even after treatment ends. There have been recent concerns that long-term suppression of bone remodeling and increased mineralization may result in detrimental changes to bone quality and accumulation of damage [38].
Bone Quality
Bisphosphonates improve trabecular microarchitecture; however, they have a relatively small effect on cortical bone. Trabecular microarchitecture is improved (greater bone volume, greater trabecular thickness, decreased trabecular spacing) after 2–3 years of alendronate treatment compared with placebo [39]. Preservation of the trabecular architecture is seen within 1 year of treatment with risedronate [40] and is continued for up to 5 years [41, 42].
Neutral effects on cortical thickness have been reported with alendronate [43] and risedronate [40, 42]. However, data are conflicting on the impact of bisphosphonates on cortical porosity. Data from iliac crest biopsies after 3 years’ treatment with alendronate reveal a significant decrease in cortical porosity [43], as does a study using DXA [28], although data from patients receiving risedronate [40, 42] and zoledronate [44] do not show a change in cortical porosity with treatment.
Persistent long-term inhibition of bone turnover leads to a fall in the number of bone-resorption pits, and secondary mineralization may be extended. Data from postmenopausal women receiving alendronate for 3 years showed decreases in activation frequency of 87% at year 2 and 92% at year 3, which allowed for increased secondary mineralization [45]. Overall mineralization was increased compared with placebo—the mean degree of mineralization was 7.5% higher than placebo at year 2 and 10.7% higher at year 3. A further study of iliac crest biopsies reported that alendronate treatment for up to 3 years was associated with an increase in mineralization [43]. Studies using μCT of the trabecular bone in transiliac biopsies taken from women treated with risedronate for 3 years [46] and 5 years [47] revealed increased mineralization, comparable to that of young premenopausal women.
However, histomorphometric data from postmenopausal women receiving alendronate [48] for up to 10 years or risedronate [49, 50] for up to 5 years found markedly decreased trabecular bone turnover and normal mineralization. Transiliac bone biopsies of a subgroup of patients from the Fracture Intervention Trial Long-Term Extension (FLEX) trial found that patients receiving alendronate (5 or 10 mg/day) for 10 years had similar bone matrix mineralization to those receiving alendronate for 5 years followed by 5 years of placebo. Data from these FLEX participants were compared to those from a previously published healthy population, and no difference in bone mineralization density distribution between treated and untreated patients was found [51]. A similar picture is seen with ibandronate [52] for treatment up to 34 months.
Annual dosing for 3 years with intravenous zoledronate 5 mg resulted in reduction of bone turnover and preservation of bone structure and mass without any signs of adynamic bone. Osteoid formation and mineralization of newly formed bone did not differ between the zoledronate and placebo groups [44]. Women switched to zoledronate 5 mg intravenously after at least 1 year of treatment with alendronate had comparable bone histomorphometry on iliac crest bone biopsy to women remaining on alendronate [53].
FTIRI assessment of the mineral properties of bisphosphonates in a small iliac crest–biopsy study revealed that postmenopausal women treated with alendronate for 3 years had a significantly higher mineral content (mineral/matrix ratio) within cortical bone than untreated control women [54]. There was a trend toward increased mineral content within trabecular bone, although this was not significant. The study also revealed a decrease in tissue heterogeneity with alendronate treatment, which the authors considered may impair tissue mechanical properties.
A similar study using FTIRI in postmenopausal women receiving risedronate for 5 years [41] revealed that at 3 and 5 years the risedronate group retained baseline values in bone mineral indices (mineral maturity/crystallinity and collagen cross-link ratio). In contrast, at 3 years women in the placebo arm had increased bone mineral indices relative to baseline values, indicating continued maturation of bone. After 5 years of risedronate, the bone mineral indices in areas of bone formation were comparable to those reported in premenopausal women.
FTIRI data suggest that there are differences between bisphosphonates in terms of the impact on bone mineral indices: Alendronate appears to increase bone matrix mineralization, whereas risedronate appears to maintain it. Although both studies were on small numbers of patients—17 and 18 women, respectively—the data provide some insight into the differing properties of bisphosphonates within the bone. Data from patients receiving teriparatide reveal a significantly lower matrix mineralization, mineral crystallinity, and collagen cross-link ratio compared with those receiving placebo [30], a similar picture to that seen in the risedronate study [41].
Bone-Quality Concerns with Bisphosphonates
Bone remodeling helps to maintain tissue integrity by selectively removing damaged bone and replacing it with new bone. Concerns have been raised that the prolonged antiresorptive action of bisphosphonates may result in bone becoming adynamic or “frozen.” The severely reduced bone remodeling associated with adynamic bone may be unable to repair microdamage, resulting in microcracks and atypical fragility.
It may be that a proportion of patients on long-term bisphosphonate treatment develop marked suppression of bone turnover. In a study of 87 women with osteoporosis treated with either alendronate or risedronate, the bone-resorption marker urinary Ntx was highly suppressed in 13% of the women [55].
A study which assessed microcrack frequency using transiliac bone biopsies in 50 postmenopausal women who had received bisphosphonate therapy (37 on oral alendronate, 10 on oral risedronate, and three on intravenous pamidronate) for at least 3 years found no significant difference between treated women and cadaver controls (0.13 vs. 0.05 microcracks/mm2, P = 0.59) [56]. Just over half of the samples had no observable microcracks (54 vs. 58%). However, a further study revealed that, after adjustment for age, prevalent fractures, femoral neck BMD, activation frequency, and investigational center, microdamage density was significantly increased in transiliac crest biopsies of women who had been treated with alendronate for an average of 5 years [4]. Low femoral neck BMD was the only independent predictor of microdamage in women receiving alendronate, suggesting that microdamage may be more likely in patients with low BMD treated with alendronate. However, it has been suggested that assessment of microcracks in humans is limited by the use of invasive techniques since the only site to obtain bone samples in humans is the iliac crest, which seems to have lower rates of microcracks than other weight-bearing sites such as the femur and the vertebrae [57].
It has been suggested that microdamage accumulation with long-term bisphosphonate use might result in atypical stress fractures. A recent secondary analysis of three large long-term bisphosphonate trials [58] revealed 12 atypical fractures in 10 women out of 14,195 women receiving bisphosphonates (alendronate or zoledronate) for up to 10 years, resulting in a rate of 2.3 per 10,000 patient-years. These data emphasize the importance of considering the risks versus the benefits of long-term bisphosphonate therapy and the option of “drug holidays,” particularly for those patients with markedly reduced bone turnover [59].
A retrospective review of women of Chinese ethnicity in Singapore experiencing a low-energy subtrochanteric femur fracture while on alendronate therapy found 17 patients with fracture over a 20-month period [5]. The mean duration of alendronate treatment was 4.8 years. X-ray assessment of the patients revealed cortical thickening in the lateral side of the subtrochanteric region, a transverse fracture and a medial cortical spike. Most patients (76%) experienced pain prior to their fracture, and 53% had bilateral findings of stress fracture. Another case report detailed nine patients who experienced spontaneous nonvertebral fracture while on long-term alendronate treatment; furthermore, six of the nine patients experienced delayed fracture healing [6]. Histomorphometric analysis of trabecular, intracortical, and endocortical bone revealed severely suppressed bone turnover. Bone-formation rate was reduced, matrix formation was severely impaired, and bone resorption was reduced in most patients. A further case report revealed severely suppressed bone turnover in three patients on long-term bisphosphonate therapy with spontaneous nonvertebral fracture, prodromal pain, and delayed healing [7]. A proportion of patients in the case reports were also taking glucocorticoids, hormone-replacement therapy, or raloxifene or had concomitant disease (glucocorticoid-induced osteoporosis, hypoparathyroidism), all of which could have exaggerated the antiresorptive effects of alendronate.
Comparison of the Effects of PTH and Bisphosphonates on Bone Quality
Data on patients from the Forteo Alendronate Comparator Trial (FACT) receiving teriparatide 20 μg/day or alendronate 10 mg/day allow comparison of the effects of the two agents on bone quality. Transiliac crest bone biopsies were obtained after tetracycline double labeling from patients enrolled in FACT at 6 and 18 months [60]. Markers of bone formation (P1NP) and markers of bone resorption (Ntx) were decreased in the alendronate arm and increased in the teriparatide arm. As expected, histomorphometric indices of bone formation were significantly and markedly greater in the teriparatide-treated patients than in the alendronate-treated patients at both 6 and 18 months. Indices of bone resorption were significantly greater in the teriparatide-treated patients at 6 months. In the teriparatide-treated patients, formation and activation frequency were significantly higher at 6 months than at 18 months. There was no difference in cortical porosity at 6 months; however, cortical porosity was significantly higher with teriparatide than with alendronate at 18 months.
A further study used spinal QCT scans to assess measures of vertebral strength in a subset of patients enrolled in FACT [61]. Both teriparatide and alendronate resulted in an increase in vertebral strength—at least 75% of patients in both groups had increased vertebral strength compared with baseline after 6 months of treatment. Average volumetric density and trabecular bone strength were increased in both groups; however, the increases in the teriparatide-treated patients were five- to 12-fold higher than those in the alendronate-treated patients. The strength:density ratio was fivefold higher in the teriparatide-treated patients, due to preferential increases in trabecular strength (Table 1).
Strontium Ranelate
Mode of Action
The mechanism of action of strontium ranelate is uncertain, although a mixed mode of action has been suggested, with increased bone formation and decreased bone resorption [15]. It is thought that strontium ranelate increases preosteoblast replication, osteoblast differentiation, collagen type I synthesis, and bone matrix mineralization, probably through a calcium-sensing receptor (CaR)-dependent mechanism. Paralleling this potentially anabolic effect, it is thought that there is inhibition of osteoclast differentiation and activity mediated by an increase in OPG and a decrease in RANKL [62].
Data from bone-turnover markers are conflicting in that some studies show an increase in markers of bone formation [16] while others show a decrease [63, 64]. However, a bone-biopsy study in postmenopausal women failed to show any evidence of bone formation, despite showing an increase in markers of bone formation [16].
Bone-biopsy specimens from postmenopausal women with osteoporosis treated with strontium ranelate show a reduction in bone resorption but no evidence of increased bone formation [16]. Further work on postmenopausal women receiving strontium ranelate after teriparatide treatment does not demonstrate an anabolic action with strontium ranelate. Postmenopausal women previously treated with teriparatide were randomized to strontium ranelate plus calcium and vitamin D or calcium and vitamin D alone [63]. Bone-turnover markers were increased after treatment with teriparatide and decreased to a similar extent after treatment with strontium ranelate or calcium and vitamin D, suggesting that in this context strontium ranelate acts predominantly as an antiresorptive agent, with no evidence of anabolic action. A small study in postmenopausal women receiving strontium ranelate after 18 months’ treatment with teriparatide revealed a similar picture in terms of bone-turnover markers [64]. Lumbar spine BMD increased significantly after teriparatide treatment and further improved with sequential strontium ranelate treatment.
It should be noted that the true BMD increase with strontium ranelate is difficult to interpret since strontium ranelate has an atomic number greater than that of calcium, which weakens X-ray penetration and results in an overestimation of measured BMD.
There is evidence to support the efficacy of strontium ranelate for the reduction of fracture risk in postmenopausal women with osteoporosis [65]. A meta-analysis of four trials of strontium ranelate revealed a 37% reduction in vertebral fractures (RR = 0.63, 95% CI 0.56–0.71) and a 14% reduction in nonvertebral fractures (RR = 0.86, 95% CI 0.75–0.98) in postmenopausal women with osteoporosis receiving strontium ranelate 2 g/day for 3 years [65]. A significant reduction in hip fracture has been demonstrated in patients at high risk of hip fracture (women aged 74 or over, femoral neck BMD ≤−3) [66].
Bone Quality
Data from a 3-year placebo-controlled trial in women with existing vertebral fracture revealed that strontium ranelate results in a significant 8.1% increase in a marker of bone formation (bone-specific alkaline phosphatase) from month 3 to the end of year 3 (P < 0.001). In contrast, the marker of bone resorption (C-telopeptide cross-links) was significantly decreased by 12.2% compared with placebo (P < 0.001) [16].
Histomorphometric analysis of transiliac bone biopsies showed that strontium ranelate results in the formation of normal lamellar bone and maintains normal mineralization of bone [16, 67].
2-D histomorphometry of transiliac bone biopsies using μCT from postmenopausal women receiving strontium ranelate for up to 5 years revealed a significantly higher mineral apposition rate in trabecular bone compared with women receiving placebo treatment [67]. There was also a trend toward higher mineral apposition rate in cortical bone with strontium ranelate [67].
A further study revealed that bone mineral quality, including mineralization and collagen cross-links, was preserved in postmenopausal women receiving strontium ranelate for 3 years [68]. Strontium is exclusively deposited in bone formed during treatment with strontium ranelate [68], with a plateau reached after 3 years [69].
Improvements were also seen in microarchitecture on 3-D μCT (improved cortical thickness, higher trabecular number, lower trabecular separation) with no change in cortical porosity compared to placebo controls [67].
There was evidence of more osteoblast activity in patients receiving strontium ranelate compared with placebo, suggesting an increase in bone formation, but no evidence of a reduction in bone resorption [67].
Denosumab
Mode of Action
The monoclonal antibody denosumab binds to RANKL, a key mediator of osteoclast differentiation, function, and survival, preventing the binding of RANKL to RANK (Fig. 6) [70].
Denosumab exerts rapid, marked, and sustained effects on bone resorption by preventing RANKL-induced increases in osteoclasts. The antiresorptive effect of a 60-mg subcutaneous injection of denosumab is significantly greater than that seen with oral alendronate [14]. Although denosumab is removed from bone much more rapidly than the bisphosphonates, concerns have been raised over the clinical impact of potent long-term osteoclast inhibition [70].
A large placebo-controlled trial of 7,868 women (the FREEDOM trial) has demonstrated the antifracture efficacy of denosumab. In the FREEDOM trial, 3 years’ treatment with denosumab (60 mg as a subcutaneous injection every 6 months) resulted in reductions in vertebral fracture (2.3 vs. 7.2%, P < 0.001), hip fracture (0.7 vs. 1.2%, P = 0.04), and nonvertebral fracture (6.5 vs. 8.0%, P = 0.01) in postmenopausal women with osteoporosis [71].
Bone Quality
Bone-turnover markers fall with denosumab treatment [71]. Serum Ctx, a marker of bone resorption, was decreased by 86% compared with placebo 1 month after the initial injection of denosumab and by 72% at the end of the 3-year trial. Serum P1NP, a marker of bone formation, was decreased by 18 and 76% compared with the placebo group at the same time points.
There are little bone-quality data for denosumab. A study on 1,189 postmenopausal women with low BMD (T score ≤2) randomized participants to denosumab (60 mg as a subcutaneous injection every 6 months) plus oral placebo or to oral alendronate (70 mg once weekly) plus subcutaneous placebo [14]. Significantly greater increases in BMD were seen with denosumab compared with alendronate at all measured sites including the total hip and femoral neck. Denosumab treatment led to significantly greater reductions in bone-turnover markers compared with alendronate. Evaluation of the bone-formation marker P1NP showed a time delay in reduction relative to CTX with both treatments, demonstrating that bone remodeling remained coupled with both denosumab and alendronate therapy.
A post hoc study of patients randomized to placebo, alendronate, or denosumab analyzed hip DXA scans with hip structural analysis software to evaluate BMD and cross-sectional geometric parameters at the narrowest segment of the femoral neck, the intertrochanter, and the proximal shaft [72]. At 12 and 24 months denosumab and alendronate both improved bone cross-sectional area, section modulus, and buckling ratio compared with placebo. The effects of denosumab were greater than those of alendronate at the intertrochanteric and shaft sites.
The use of denosumab after at least 6 months of alendronate treatment resulted in a greater increase in BMD compared with patients remaining on alendronate (1.9 vs. 1.05% increase at 12 months, P < 0.0001). Serum Ctx was significantly decreased in patients switched to denosumab compared with patients remaining on alendronate, in whom serum Ctx remained near baseline, demonstrating the potent antiresorptive effects of denosumab [73].
Using Bone-Quality Data to Inform Clinical Practice
A number of studies have set out to determine the optimal place in therapy for PTH with respect to bisphosphonate use (whether it should be used before, after, or in combination with bisphosphonates) and potential treatment options at the end of PTH therapy. There is a lack of fracture data to support this part of the decision-making process, and future studies of sequential therapy with fracture as an outcome are unlikely. In the absence of fracture-outcome data, the evidence is from surrogate end points such as BMD and bone quality, primarily bone-turnover marker data.
BMD is simple to measure; however, BMD is a relatively poor predictor of fracture [2, 3]. Assessing bone quality can provide further supporting evidence, although many of the tools used to measure bone quality are not available for everyday use. However, bone turnover, one aspect of bone quality, can be readily measured using biomarkers. The routine use of biomarkers is costly and often unnecessary but may be of clinical value in patients receiving PTH or long-term bisphosphonate treatment. In the absence of readily available bone-quality testing, reviewing the available evidence from clinical studies of bone quality and considering the underlying mechanisms of change within bone structure can help to inform treatment decisions.
The BMD and bone-quality data outlined below suggest that PTH should probably be used prior to bisphosphonates.
Post hoc analysis of data from the Fracture Prevention Trial revealed that the relative risk reduction in fracture with teriparatide treatment was independent of pretreatment bone turnover [74], demonstrating benefit across all disease severities.
Data are conflicting on the potential “blunting” of response to teriparatide in patients pretreated with bisphosphonates. A number of studies have shown that previous long-term treatment with bisphosphonates does not appear to have a significant impact on the effects of teriparatide on BMD and markers of bone formation in postmenopausal women with established osteoporosis [75]. Women treated with teriparatide for 12 months following at least 24 months of alendronate or risedronate treatment show an early increase in bone-turnover markers with teriparatide and increases in BMD [76]. A review of patients from one U.K. unit treated with teriparatide for at least 12 months compared those patients who had received bisphosphonates prior to teriparatide (n = 38) with bisphosphonate-naive patients (n = 14) [77]. P1NP increased significantly with teriparatide in both groups; however, bisphosphonate-naive patients had higher baseline P1NP levels, which remained higher at 6 and 12 months of teriparatide treatment. There was no significant difference in BMD at the spine or the hip between the two groups at 12 and 18 months.
However, a study of postmenopausal women receiving teriparatide for 24 months after treatment with bisphosphonates (split into responders to bisphosphonates, n = 134, and nonresponders to bisphosphonates, n = 85) and bisphosphonate-naive women (n = 84) revealed a modest blunting of response to teriparatide [78]. The gain in lumbar spine BMD over 24 months was greatest in the bisphosphonate-naive women (13 vs. 10.2% for bisphosphonate responders and 9.8% for nonresponders, P < 0.005). A similar trend was seen in hip BMD (3.8 vs. 2.3% for both bisphosphonate groups). The study was not powered or designed to assess the effect of pretreatment with bisphosphonates on fracture risk.
Patients pretreated with risedronate show a greater response to treatment with teriparatide than those pretreated with alendronate as measured by bone-turnover markers, particularly P1NP, at month 3 and a greater response in terms of BMD. Iliac crest biopsies have demonstrated an early (<1 month) response to teriparatide in patients previously treated with bisphosphonates [79]. There was an increase in bone-remodeling units as early as 1 week after the first dose of teriparatide.
A prospective study assessed the effect of teriparatide (20 μg) on microcracks in postmenopausal women with osteoporosis previously treated with alendronate for a mean of 5.3 years (n = 38) and previously untreated women (n = 28) [80]. After 2 years of treatment with teriparatide, assessment of the iliac crest showed a reduction in crack density, crack surface density, and crack length in patients previously treated with alendronate; however, only crack length was decreased in previously untreated patients. It appears that teriparatide reduces microdamage accumulation in the iliac crest of patients previously treated with alendronate and reduces crack length regardless of prior treatment.
Teriparatide is given for a maximum of 2 years. After discontinuation of teriparatide, there is a fall in BMD, which appears to be greater in women than in men [81]. It seems sensible to attempt to retain the new bone formed during the treatment period, and a number of strategies have been suggested.
Retreatment with teriparatide is costly and may be associated with a blunting of the response to retreatment. A study in men and women with osteoporosis found increases of 12.5 and 16.9% in posterior–anterior and lateral spine BMD with the first 12-month course of teriparatide, which were reduced to 5.2 and 6.2%, respectively, after 12 months of teriparatide retreatment following a 12-month teriparatide-free period [82]. A similar picture was seen in terms of bone-turnover markers.
Treating postmenopausal women with alendronate after PTH treatment results in an increase in vertebral BMD greater than that seen with alendronate alone [83]. Postmenopausal women received PTH(1–84) or placebo for 12 months, followed by alendronate for an additional 12 months. After 12 months of PTH(1–84), BMD changed by 7.1 ± 5.6% at the spine, 0.3 ± 6.2% at the femoral neck, and −2.3 ± 3.3% for the total body. Sequential treatment with alendronate resulted in increases of 13.4 ± 6.4, 4.4 ± 7.2, and 2.6 ± 3.1%, respectively. All markers of bone turnover increased during PTH(1–84) treatment and decreased to below baseline during alendronate treatment.
The PaTH (PTH and alendronate) study compared the use of PTH(1–84), alendronate, or PTH(1–84) plus alendronate (combination therapy) in postmenopausal women with osteoporosis over a 12-month period. Spinal BMD and volumetric density of trabecular bone at the spine increased substantially in all groups, but the increase in volumetric density in the PTH(1–84) group was about twice that found in either of the other groups. Bone formation increased markedly in the PTH(1–84) group but not in the combination group, while bone resorption decreased in the combination and alendronate groups [84]. Changes in the volumetric density of trabecular bone, the cortical volume at the hip, and levels of markers of bone turnover suggest that the concurrent use of alendronate may reduce the anabolic effects of PTH [84]. Patients in PaTH were switched to alendronate or placebo in year 2 of treatment, resulting in four treatment arms (PTH-placebo, PTH-alendronate, combination-alendronate, and alendronate-alendronate). Patients randomized to PTH-alendronate showed the greatest increase in BMD at the spine, hip, and distal radius, while those randomized to placebo in year 2 (PTH-placebo) showed the greatest decrease in BMD and lost considerable BMD [85]. Finite element analysis of QCT scans from women in PaTH allowed assessment of changes in femoral strength [86]. Significant improvements in femoral strength were seen in the PTH (2.08%) and alendronate (3.6%) groups in year 1 of treatment; at year 2 the improvements were significant in the PTH-alendronate (7.74%), combination-alendronate (4.18%), and alendronate-alendronate (4.83%) groups but not in the PTH-placebo group (1.17%). The increases in strength were primarily due to improvements in trabecular density (Fig. 7).
Mean change from baseline in femoral strength at years 1 and 2 compared with baseline. For year 1 the two PTH groups have been pooled into one bar (white bar). * Change from baseline was statistically significant, P < 0.05 [86]
Conclusions
PTH is given over a 2-year period, and a number of studies have demonstrated an increase in bone strength and BMD during the treatment period, together with a reduction in fracture risk. However, the effects of treatment appear to reverse once treatment is halted [85, 86], and a treatment strategy should consider the appropriate treatment post-PTH.
The lack of hip fracture–outcome data and issues around cortical porosity with PTH may raise concerns around the first few months of PTH use in older women. However the bone-quality data available do not suggest any impairment in bone strength in this context. The effects of PTH on bone quality may make this an attractive treatment option for younger patients. Younger women are at greater risk of “trabecular” fractures—e.g., vertebral fractures—and there is good evidence for the antifracture efficacy of PTH at this site.
Younger treatment-naive women, aged 60–65 years, with very low BMD T scores at high absolute fracture risk may benefit from PTH as primary therapy to improve the bone substrate and build bone. High risk in this context has been defined as women aged under 65 years with a T score of −3.5 or less, even in the absence of fracture [27]. This recommendation was based on the premise that although there are no head-to-head trials comparing the antifracture efficacy of PTH and bisphosphonates, PTH produces a rapid improvement in bone quality, specifically microarchitecture, which is not seen with bisphosphonates. It has been suggested that patients with additional risk factors, such as low body mass index, use of glucocorticoids, and malabsorption, may benefit still further with PTH treatment [27]. Treatment-naive patients are likely to achieve the maximal benefit from PTH since any potential blunting with prior bisphosphonate use is avoided.
PTH is given for a maximum of 2 years; treatment with an antiresorptive after cessation of treatment with PTH will further improve BMD and reduce the risk of fracture [27]. There is evidence to support sequential treatment with alendronate after PTH [83] from a study in postmenopausal women which demonstrated that the typical improvement in BMD with alendronate was added to the prior improvement resulting from treatment with PTH. By treating with bisphosphonates after PTH, the benefit of PTH on BMD continues into later years. Bisphosphonates reduce bone loss and have a strong evidence base to support fracture reduction at all sites, including the hip.
References
Delmas PD, Seeman E (2004) Changes in bone mineral density explain little of the reduction in vertebral or nonvertebral fracture risk with antiresorptive therapy. Bone 34:599–604
Siris ES, Chen YT, Abbott TA, Barrett-Connor E, Miller PD, Wehren LE et al (2004) Bone mineral density thresholds for pharmacological intervention to prevent fractures. Arch Intern Med 164:1108–1112
Chen P, Miller PD, Recker R, Resch H, Rana A, Pavo I et al (2007) Increases in BMD correlate with improvements in bone microarchitecture with teriparatide treatment in postmenopausal women with osteoporosis. J Bone Miner Res 22:1173–1180
Stepan JJ, Burr DB, Pavo I, Sipos A, Michalska D, Li J et al (2007) Low bone mineral density is associated with bone microdamage accumulation in postmenopausal women with osteoporosis. Bone 41:378–385
Kwek EB, Goh SK, Koh JS, Png MA, Howe TS (2008) An emerging pattern of subtrochanteric stress fractures: a long-term complication of alendronate therapy? Injury 39:224–231
Odvina CV, Zerwekh JE, Rao DS, Maalouf N, Gottschalk FA, Pak CY (2005) Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab 90:1294–1301
Visekruna M, Wilson D, McKiernan FE (2008) Severely suppressed bone turnover and atypical skeletal fragility. J Clin Endocrinol Metab 93:2948–2952
Khan AA, Sándor GK, Dore E, Morrison AD, Alsahli M, Amin F, Canadian Taskforce on Osteonecrosis of the Jaw et al (2009) Bisphosphonate associated osteonecrosis of the jaw. J Rheumatol 36:478–490
Khan A (2010) Osteonecrosis of the jaw and bisphosphonates. BMJ 340:c246
Khosla S, Burr D, Cauley J, Dempster DW, Ebeling PR, Felsenberg D, American Society for Bone and Mineral Research et al (2007) Bisphosphonate-associated osteonecrosis of the jaw: report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 22:1479–1491
Szulc P, Seeman E (2009) Thinking inside and outside the envelopes of bone: dedicated to PDD. Osteoporos Int 20:1281–1288
Compston JE (2007) Skeletal actions of intermittent parathyroid hormone: effects on bone remodeling and structure. Bone 40:1447–1452
Reszka AA, Rodan GA (2003) Bisphosphonate mechanism of action. Curr Rheumatol Rep 5:65–74
Brown JP, Prince RL, Deal C, Recker RR, Kiel DP, de Gregorio LH et al (2009) Comparison of the effect of denosumab and alendronate on BMD and biochemical markers of bone turnover in postmenopausal women with low bone mass: a randomized, blinded, phase 3 trial. J Bone Miner Res 24:153–161
Marie PJ (2006) Strontium ranelate: a dual mode of action rebalancing bone turnover in favour of bone formation. Curr Opin Rheumatol 18(Suppl 1):S11–S15
Meunier PJ, Roux C, Seeman E, Ortolani S, Badurski JE, Spector TD et al (2004) The effects of strontium ranelate on the risk of vertebral fracture in women with postmenopausal osteoporosis. N Engl J Med 350:459–468
Neer RM, Arnaud CD, Zanchetta JR, Prince R, Gaich GA, Reginster JY et al (2001) Effect of parathyroid hormone (1–34) on fractures and bone mineral density in postmenopausal women with osteoporosis. N Engl J Med 344:1434–1441
Dobnig H, Sipos A, Jiang Y, Fahrleitner-Pammer A, Ste-Marie LG, Gallagher JC et al (2005) Early changes in biochemical markers of bone formation correlate with improvements in bone structure during teriparatide therapy. J Clin Endocrinol Metab 90:3970–3977
Bilezikian JP (2008) Combination anabolic and antiresorptive therapy for osteoporosis: opening the anabolic window. Curr Osteoporos Rep 6:24–30
Hodsman AB, Kisiel M, Adachi JD, Fraher LJ, Watson PH (2000) Histomorphometric evidence for increased bone turnover without change in cortical thickness or porosity after 2 years of cyclical hPTH(1–34) therapy in women with severe osteoporosis. Bone 27:311–318
Ma YL, Zeng Q, Donley DW, Ste-Marie LG, Gallagher JC, Dalsky GP et al (2006) Teriparatide increases bone formation in modeling and remodeling osteons and enhances IGF-II immunoreactivity in postmenopausal women with osteoporosis. J Bone Miner Res 21:855–864
Lindsay R, Zhou H, Cosman F, Nieves J, Dempster DW, Hodsman AB (2007) Effects of a one-month treatment with PTH(1–34) on bone formation on cancellous, endocortical, and periosteal surfaces of the human ilium. J Bone Miner Res 22:495–502
Anastasilakis AD, Goulis DG, Polyzos SA, Gerou S, Pavlidou V, Koukoulis G et al (2008) Acute changes in serum osteoprotegerin and receptor activator for nuclear factor-kappaB ligand levels in women with established osteoporosis treated with teriparatide. Eur J Endocrinol 158:411–415
Jiang Y, Zhao JJ, Mitlak BH, Wang O, Genant HK, Eriksen EF (2003) Recombinant human parathyroid hormone (1–34) [teriparatide] improves both cortical and cancellous bone structure. J Bone Miner Res 18:1932–1941
Graeff C, Timm W, Nickelsen TN, Farrerons J, Marín F, Barker C, EUROFORS High Resolution Computed Tomography Substudy Group et al (2007) Monitoring teriparatide-associated changes in vertebral microstructure by high-resolution CT in vivo: results from the EUROFORS study. J Bone Miner Res 22:1426–1433
Recker RR, Bare SP, Smith SY, Varela A, Miller MA, Morris SA (2009) Cancellous and cortical bone architecture and turnover at the iliac crest of postmenopausal osteoporotic women treated with parathyroid hormone 1–84. Bone 44:113–119
Hodsman AB, Bauer DC, Dempster DW, Dian L, Hanley DA, Harris ST et al (2005) Parathyroid hormone and teriparatide for the treatment of osteoporosis: a review of the evidence and suggested guidelines for its use. Endocr Rev 26:688–703
Hyldstrup L, Jorgensen JT, Gaich G (2002) Assessment of effects of ly333334 [recombinant human parathyroid hormone (1–34)] on cortical bone using digital X-ray radiogrammetry. Bone 28:S97
Borggrefe J, Graeff C, Nickelsen TN, Marin F, Glüer CC (2009) Quantitative computed tomography assessment of the effects of 24 months of teriparatide treatment on 3-D femoral neck bone distribution, geometry and bone strength: results from the EUROFORS study. J Bone Miner Res 25:472–481
Paschalis EP, Glass EV, Donley DW, Eriksen EF (2005) Bone mineral and collagen quality in iliac crest biopsies of patients given teriparatide: new results from the fracture prevention trial. J Clin Endocrinol Metab 90:4644–4649
Uusi-Rasi K, Semanick LM, Zanchetta JR, Bogado CE, Eriksen EF, Sato M et al (2005) Effects of teriparatide [rhPTH (1–34)] treatment on structural geometry of the proximal femur in elderly osteoporotic women. Bone 36:948–958
Zanchetta JR, Bogado CE, Ferretti JL, Wang O, Wilson MG, Sato M et al (2003) Effects of teriparatide [recombinant human parathyroid hormone (1–34)] on cortical bone in postmenopausal women with osteoporosis. J Bone Miner Res 18:539–543
Xiong Y, Yang HJ, Feng J, Shi ZL, Wu LD (2009) Effects of alendronate on the proliferation and osteogenic differentiation of MG-63 cells. J Int Med Res 37:407–416
Wells GA, Cranney A, Peterson J, Boucher M, Shea B, Welch V et al (2008) Alendronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev 1:CD001155. doi:10.1002/14651858.CD001155.pub2
Wells GA, Cranney A, Peterson J, Boucher M, Shea B, Welch V et al (2008) Risedronate for the primary and secondary prevention of osteoporotic fractures in postmenopausal women. Cochrane Database Syst Rev 1: CD004523. doi:10.1002/14651858.CD004523.pub3
Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, for HORIZON Pivotal Fracture Trial et al (2007) Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med 356:1809–1822
Chesnut CH III, Skag A, Christiansen C, Recker R, Stakkestad JA, Hoiseth A, for the Oral Ibandronate Osteoporosis Vertebral Fracture Trial in North America, Europe (BONE) et al (2004) Effects of oral ibandronate administered daily or intermittently on fracture risk in postmenopausal osteoporosis. J Bone Miner Res 19:1241–1249
Seeman E (2009) To stop or not to stop, that is the question. Osteoporos Int 20:187–195
Recker R, Masarachia P, Santora A, Howard T, Chavassieux P, Arlot M et al (2005) Trabecular bone microarchitecture after alendronate treatment of osteoporotic women. Curr Med Res Opin 21:185–194
Dufresne TE, Chmielewski PA, Manhart MD, Johnson TD, Borah B (2003) Risedronate preserves bone architecture in early postmenopausal women in 1 year as measured by three-dimensional microcomputed tomography. Calcif Tissue Int 73:423–432
Durchschlag E, Paschalis EP, Zoehrer R, Roschger P, Fratzl P, Recker R et al (2006) Bone material properties in trabecular bone from human iliac crest biopsies after 3- and 5-year treatment with risedronate. J Bone Miner Res 21:1581–1590
Borah B, Dufresne TE, Chmielewski PA, Johnson TD, Chines A, Manhart MD (2004) Risedronate preserves bone architecture in postmenopausal women with osteoporosis as measured by three-dimensional microcomputed tomography. Bone 34:736–746
Roschger P, Rinnerthaler S, Yates J, Rodan GA, Fratzl P, Klaushofer K (2001) Alendronate increases degree and uniformity of mineralization in cancellous bone and decreases the porosity in cortical bone of osteoporotic women. Bone 29:185–191
Recker RR, Delmas PD, Halse J, Reid IR, Boonen S, García-Hernandez PA et al (2008) Effects of intravenous zoledronic acid once yearly on bone remodeling and bone structure. J Bone Miner Res 23:6–16
Boivin GY, Chavassieux PM, Santora AC, Yates J, Meunier PJ (2000) Alendronate increases bone strength by increasing the mean degree of mineralization of bone tissue in osteoporotic women. Bone 27:687–694
Borah B, Ritman EL, Dufresne TE, Jorgensen SM, Liu S, Sacha J et al (2005) The effect of risedronate on bone mineralization as measured by micro-computed tomography with synchrotron radiation: correlation to histomorphometric indices of turnover. Bone 37:1–9
Borah B, Dufresne TE, Ritman EL, Jorgensen SM, Liu S, Chmielewski PA et al (2006) Long-term risedronate treatment normalizes mineralization and continues to preserve trabecular architecture: sequential triple biopsy studies with micro-computed tomography. Bone 39:345–352
Chavassieux PM, Arlot ME, Reda C, Wei L, Yates AJ, Meunier PJ (1997) Histomorphometric assessment of the long-term effects of alendronate on bone quality and remodeling in patients with osteoporosis. J Clin Invest 100:1475–1480
Eriksen EF, Melsen F, Sod E, Barton I, Chines A (2002) Effects of long-term risedronate on bone quality and bone turnover in women with postmenopausal osteoporosis. Bone 3:620–625
Zoehrer R, Roschger P, Paschalis EP, Hofstaetter JG, Durchschlag E, Fratzl P et al (2006) Effects of 3- and 5-year treatment with risedronate on bone mineralization density distribution in triple biopsies of the iliac crest in postmenopausal women. J Bone Miner Res 21:1106–1112
Roschger P, Lombardi A, Misof BM, Maier G, Fratzl-Zelman N, Fratzl P et al (2010) Mineralization density distribution of postmenopausal osteoporotic bone is restored to normal after long-term alendronate treatment: qBEI and sSAXS data from the Fracture Intervention Trial Long-Term Extension (FLEX). J Bone Miner Res 25:48–55
Recker RR, Weinstein RS, Chesnut CH III, Schimmer RC, Mahoney P, Hughes C et al (2004) Histomorphometric evaluation of daily and intermittent oral ibandronate in women with postmenopausal osteoporosis: results from the BONE study. Osteoporos Int 15:231–237
McClung M, Recker R, Miller P, Fiske D, Minkoff J, Kriegman A et al (2007) Intravenous zoledronic acid 5 mg in the treatment of postmenopausal women with low bone density previously treated with alendronate. Bone 41:122–128
Boskey AL, Spevak L, Weinstein RS (2009) Spectroscopic markers of bone quality in alendronate-treated postmenopausal women. Osteoporos Int 20:793–800
Iba K, Takada J, Hatakeyama N, Ozasa Y, Wada T, Yamashita T (2008) Changes in urinary NTX levels in patients with primary osteoporosis undergoing long-term bisphosphonate treatment. J Orthop Sci 13:438–441
Chapurlat RD, Arlot M, Burt-Pichat B, Chavassieux P, Roux JP, Portero-Muzy N et al (2007) Microcrack frequency and bone remodeling in postmenopausal osteoporotic women on long-term bisphosphonates: a bone biopsy study. J Bone Miner Res 22:1502–1509
Chapurlat RD, Delmas PD (2009) Bone microdamage: a clinical perspective. Osteoporos Int 20:1299–1308
Black DM, Kelly MP, Genant HK, Palermo L, Eastell R, Bucci-Rechtweg C, the Fracture Intervention Trial and HORIZON Pivotal Fracture Trial Steering Committees et al (2010) Bisphosphonates and fractures of the subtrochanteric or diaphyseal femur. N Engl J Med 362:1761–1771
Shane E (2010) Evolving data about subtrochanteric fractures and bisphosphonates. N Engl J Med 362:1825–1827
Arlot M, Meunier PJ, Boivin G, Haddock L, Tamayo J, Correa-Rotter R et al (2005) Differential effects of teriparatide and alendronate on bone remodeling in postmenopausal women assessed by histomorphometric parameters. J Bone Miner Res 20:1244–1253
Keaveny TM, Donley DW, Hoffmann PF, Mitlak BH, Glass EV, San Martin JA (2007) Effects of teriparatide and alendronate on vertebral strength as assessed by finite element modeling of QCT scans in women with osteoporosis. J Bone Miner Res 22:149–157
Fonseca JE (2008) Rebalancing bone turnover in favour of formation with strontium ranelate: implications for bone strength. Rheumatology (Oxford) 47(Suppl 4):iv17–iv19
Anastasilakis AD, Goulis DG, Polyzos SA, Gerou S, Ballaouri I, Efstathiadou Z et al (2009) No difference between strontium ranelate (SR) and calcium/vitamin D on bone turnover markers in women with established osteoporosis previously treated with teriparatide: a randomized controlled trial. Clin Endocrinol (Oxf) 70:522–526
Anastasilakis AD, Polyzos SA, Avramidis A, Papatheodorou A, Terpos E (2009) Effect of strontium ranelate on lumbar spine bone mineral density in women with established osteoporosis previously treated with teriparatide. Horm Metab Res 41:559–562
O’Donnell S, Cranney A, Wells GA, Adachi J, Reginster JY (2006) Strontium ranelate for preventing and treating postmenopausal osteoporosis. Cochrane Database Syst Rev 4:CD005326. doi:10.1002/14651858.CD005326.pub3
Reginster JY, Seeman E, De Vernejoul MC, Adami S, Compston J, Phenekos C et al (2005) Strontium ranelate reduces the risk of nonvertebral fractures in postmenopausal women with osteoporosis: Treatment of Peripheral Osteoporosis (TROPOS) study. J Clin Endocrinol Metab 90:2816–2822
Arlot ME, Jiang Y, Genant HK, Zhao J, Burt-Pichat B, Roux JP et al (2008) Histomorphometric and microCT analysis of bone biopsies from postmenopausal osteoporotic women treated with strontium ranelate. J Bone Miner Res 23:215–222
Roschger P, Manjubala I, Zoeger N, Meirer F, Simon R et al (2010) Bone material quality in transiliac bone biopsies of postmenopausal osteoporotic women after 3 years of strontium ranelate treatment. J Bone Miner Res 25:891–900
Boivin G, Farlay D, Khebbab MT, Jaurand X, Delmas PD, Meunier PJ (2010) In osteoporotic women treated with strontium ranelate, strontium is located in bone formed during treatment with a maintained degree of mineralization. Osteoporos Int 21:667–677
Tankó LB (2007) Effect of RANKL-specific denosumab on osteoclast number and function: a potential friend or foe? Curr Opin Investig Drugs 8:830–835
Cummings SR, San Martin J, McClung MR, Siris ES, Eastell R, Reid IR, FREEDOM Trial et al (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765
Beck TJ, Lewiecki EM, Miller PD, Felsenberg D, Liu Y, Ding B (2008) Effects of denosumab on the geometry of the proximal femur in postmenopausal women in comparison with alendronate. J Clin Densitom 11:351–359
Kendler DL, Roux C, Benhamou CL, Brown JP, Lillestol M, Siddhanti S et al (2009) Effects of denosumab on bone mineral density and bone turnover in postmenopausal women transitioning from alendronate therapy. J Bone Miner Res 25:72–81
Delmas PD, Licata AA, Reginster JY, Crans GG, Chen P, Misurski DA et al (2006) Fracture risk reduction during treatment with teriparatide is independent of pretreatment bone turnover. Bone 39:237–243
Boonen S, Marin F, Obermayer-Pietsch B, Simoes ME, Barker C, Glass EV et al (2008) Effects of previous antiresorptive therapy on the bone mineral density response to two years of teriparatide treatment in postmenopausal women with osteoporosis. J Clin Endocrinol Metab 93:852–860
Miller PD, Delmas PD, Lindsay R, Watts NB, Luckey M, Adachi J et al (2008) Early responsiveness of women with osteoporosis to teriparatide after therapy with alendronate or risedronate. J Clin Endocrinol Metab 93:3785–3793
Middleton ET, Steel SA, Doherty SM (2007) The effect of prior bisphosphonate exposure on the treatment response to teriparatide in clinical practice. Calcif Tissue Int 81:335–340
Obermayer-Pietsch BM, Marin F, McCloskey EV, Hadji P, Farrerons J, Boonen S, EUROFORS Investigators et al (2008) Effects of two years of daily teriparatide treatment on BMD in postmenopausal women with severe osteoporosis with and without prior antiresorptive treatment. J Bone Miner Res 10:1591–1600
Jobke B, Pfeifer M, Minne HW (2009) Teriparatide following bisphosphonates: initial and long-term effects on microarchitecture and bone remodeling at the human iliac crest. Connect Tissue Res 50:46–54
Dobnig H, Stepan JJ, Burr DB, Li J, Michalska D, Sipos A et al (2009) Teriparatide reduces bone microdamage accumulation in postmenopausal women previously treated with alendronate. J Bone Miner Res 24:1998–2006
Leder BZ, Neer RM, Wyland JJ, Lee HW, Burnett-Bowie SA, Finkelstein JS (2009) Effects of teriparatide treatment and discontinuation in postmenopausal women and eugonadal men with osteoporosis. J Clin Endocrinol Metab 94:2915–2921
Finkelstein JS, Wyland JJ, Leder BZ, Burnett-Bowie SM, Lee H, Jüppner H et al (2009) Effects of teriparatide retreatment in osteoporotic men and women. J Clin Endocrinol Metab 94:2495–2501
Rittmaster RS, Bolognese M, Ettinger MP, Hanley DA, Hodsman AB, Kendler DL et al (2000) Enhancement of bone mass in osteoporotic women with parathyroid hormone followed by alendronate. J Clin Endocrinol Metab 85:2129–2134
Black DM, Greenspan SL, Ensrud KE, Palermo L, McGowan JA, Lang TF, PaTH Study Investigators et al (2003) The effects of parathyroid hormone and alendronate alone or in combination in postmenopausal osteoporosis. N Engl J Med 349:1207–1215
Black DM, Bilezikian JP, Ensrud KE, Greenspan SL, Palermo L, Hue T et al (2005) One year of alendronate after one year of parathyroid hormone (1–84) for osteoporosis. N Engl J Med 353:555–565
Keaveny TM, Hoffmann PF, Singh M, Palermo L, Bilezikian JP, Greenspan SL et al (2008) Femoral bone strength and its relation to cortical and trabecular changes after treatment with PTH, alendronate, and their combination as assessed by finite element analysis of quantitative CT scans. J Bone Miner Res 23:1974–1982
Acknowledgment
This study was supported by Eli-Lilly and Co., which provided a fee for one of the authors (T. D.).
Author information
Authors and Affiliations
Corresponding author
Additional information
S. J. Gallacher has received honoraria and conference support from Amgen, Eli Lilly and Company Limited, Novartis, ProStrakan, Roche Pharmaceuticals, Shire, and Warner Chilcott. T. Dixon is a director of JB Medical Ltd. JB Medical Ltd has received funding from Eli Lilly and Company Limited for this project and has also received consultancy fees from Merck & Co, Merck Sharp & Dohme Limited, Nycomed, Roche Products, and Lilly for other projects related to osteoporosis. The sponsor (Eli Lilly and Company Limited) did not have any input into the content of the manuscript and did not see a copy of the manuscript prior to submission.
Appendix: Search Strategy
Appendix: Search Strategy
-
1.
Alendronate
-
2.
Risedronate
-
3.
Ibandronate
-
4.
Zoledronate
-
5.
1 or 2 or 3 or 4
-
6.
Strontium ranelate
-
7.
Teriparatide
-
8.
Preotact
-
9.
hPTH
-
10.
1–84
-
11.
1–34
-
12.
7 or 8 or 9 or 10 or 11 or 12
-
13.
Denosumab
-
14.
Bone quality
-
15.
Bone strength
-
16.
Bone microarchitecture
-
17.
Bone histomorphometry
-
18.
Osteocalcin
-
19.
Alkaline phosphatase
-
20.
Ctx
-
21.
Ntx
-
22.
Bone turnover
-
23.
Osteoporosis
-
24.
5 or 6 or 12 or 13
-
25.
14 or 15 or 16 or 17 or 18 or 19 or 20 or 21 or 22
-
26.
24 and 25
-
27.
26 and osteoporosis
Limit to humans and adults.
Rights and permissions
About this article
Cite this article
Gallacher, S.J., Dixon, T. Impact of Treatments for Postmenopausal Osteoporosis (Bisphosphonates, Parathyroid Hormone, Strontium Ranelate, and Denosumab) on Bone Quality: A Systematic Review. Calcif Tissue Int 87, 469–484 (2010). https://doi.org/10.1007/s00223-010-9420-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-010-9420-x