Abstract
Parkinson’s disease (PD), dementia with Lewy Bodies (DLB), and multiple system atrophy (MSA) are three major synucleinopathies characterized by α-synuclein-containing inclusions in the brains of patients. Because the cell types and brain structures that are affected vary markedly between the disorders, the patients have different clinical manifestations in addition to some overlapping symptoms, which are the basis for differential diagnosis. Cognitive impairment and depression associated with hippocampal dysfunction are frequently observed in these disorders. While various α-synuclein-containing inclusions are found in the hippocampal formation, increasing evidence supports that small α-synuclein aggregates or oligomers may be the real culprit, causing deficits in neurotransmission and neurogenesis in the hippocampus and related brain regions, which constitute the major mechanism for the hippocampal dysfunctions and associated neuropsychiatric manifestations in synucleinopathies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Synucleinopathies are a group of neurodegenerative disorders characterized by the formation of α-synuclein (α-syn)-containing inclusions in selective populations of neurons and/or glia. These disorders consist of Parkinson’s disease (PD), dementia with Lewy bodies (DLB), multiple system atrophy (MSA), and some other rarer disorders such as neurodegeneration with brain iron accumulation type 1 and other neuroaxonal dystrophies [1]. There are three major pathological forms of α-syn-containing inclusions associated with synucleinopathies. These consist of Lewy bodies (LBs) and Lewy neurites (LNs) found in neurons of patients with PD and DLB [2, 3], and glial cytoplasmic inclusions (GCIs) present in oligodendrocytes of patients with MSA [4]. Despite all these disorders have α-syn-containing inclusions deposited in the brain, the cell types and brain structures that are affected vary markedly between the disorders. This leads to different clinical manifestations, which are the basis for differential diagnosis. However, these disorders also present some shared symptoms such as chronic and progressive decline in motor, cognitive, behavioral, and autonomic functions [5].
In this review article, we concentrate on PD, DLB, and MSA, the three major synucleinopathies. We first compare the clinical features and pathological changes of these disorders. We then discuss how these disorders affect hippocampal functions, causing neuropsychiatric manifestations associated with hippocampal abnormalities.
Common features of the synucleinopathies
The synucleinopathies share some common features in both clinical manifestations and pathological changes. Clinically, they all present a chronic and progressive decline in motor, cognitive, behavioral, and autonomic functions. Pathologically, they all have α-syn-containing intracellular inclusions, with LBs and LNs present in neurons of PD and DLB patients and GCIs in oligodendrocytes of MSA patients [1, 6, 7]. However, there are also subtle differences between these disorders in either clinical manifestations and pathological changes, which are the basis for differential diagnosis.
Clinical features
PD PD is one of the most common neurodegenerative diseases, affecting about 1.5% of people over the age of 65 years in Europe [8] with considerable worldwide variation in prevalence [9]. The cardinal clinical manifestations are motor symptoms, including bradykinesia, rigidity, rest tremor, and postural and gait impairments [10], by which PD is diagnosed. Based on the features of motor symptoms, PD can be classified into the tremor-dominant PD, which is relatively absent of other motor symptoms, and the non-tremor-dominant (akinetic/rigid) PD, which includes phenotypes described as akinetic-rigid syndrome and postural instability gait disorder. In addition, a subgroup of PD patients manifest as a mixed or an indeterminate phenotype with several motor symptoms of comparable severity [11, 12]. The tremor-dominant PD is often associated with a slower rate of progression and less functional disability than the non-tremor-dominant PD [13].
In addition to motor symptoms, PD patients also exhibit various non-motor symptoms. These include olfactory dysfunction, cognitive impairment, psychiatric symptoms (depression, visual hallucinations and anxiety), insomnia, rapid eye movement (REM) sleep disorder (RBD) [14], autonomic dysfunction (constipation, orthostatic hypotension, and urinary incontinence),Kibnd pain, and fatigue (Table 1). Some of the non-motor symptoms, such as impaired olfaction, constipation, depression, excessive daytime sleepiness, and RBD, occur before the onset of the motor symptoms [15]. Autonomic deficits preferentially occur in individuals with non-tremor-dominant PD subtype early in the disease [16, 17]. Although the non-motor symptoms are not used for disease diagnosis, they are important prognosis markers and subtype defining features [17].
DLB DLB is the second major synucleinopathy, accounting for around one in 25 dementia cases diagnosed in the community and one in 13 cases in secondary care. However, the true prevalence of DLB is likely to be much higher because its diagnosis is often missed, although there is evidence that new criteria aid case identification [18]. Clinically, DLB can be differentiated from PD with dementia (PDD) depending on the time that the dementia occurs. DLB is diagnosed when cognitive impairment precedes parkinsonism or begins within a year of parkinsonism. PDD is diagnosed when parkinsonism precedes cognitive impairment by more than 1 year [19]. Despite of refined diagnostic criteria for DLB, large autopsy studies indicate that DLB is often misdiagnosed in the clinical setting [20]. One of the reasons is that many older individuals have more than one neurodegenerative syndrome. For example, around one-half of DLB cases have visual hallucinations and RBD prior to or around the onset of memory loss [21–23]. In addition, around one-quarter of patients have anxiety and depression [22, 23]. Retrospective case–control studies have shown that a history of depression [24] or delirium [25] prior to the diagnosis of dementia is more common in DLB than in AD.
The motor symptoms in DLB are similar to those in PD and are usually assessed using the Unified Parkinson’s Disease Rating Scale (UPDRS) [26]. Compared to patients with PDD, patients with DLB have less asymmetry and resting tremor, a more rapid progression of motor symptoms and a poorer response to levodopa [19, 20, 27]. Moreover, DLB patients are particularly sensitive to developing extrapyramidal symptoms (EPS) and also to the potentially fatal complication of neuroleptic sensitivity, which affects approximately 50% of DLB patients [28]. In addition, gait abnormality and postural instability can be prominent in DLB [29] (Table 1).
Autonomic dysfunction is frequent in DLB and the severity is intermediate between those of MSA and PD. Most of patients with DLB have autonomic disorders, such as orthostatic hypotension, heat intolerability, dryness of cutaneous epithelium, mouth mucous membranes, and urination disorders [30].
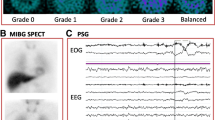
MSA MSA is an adult-onset sporadic, progressive neurodegenerative disorder characterized by any combination of autonomic failure, parkinsonism, cerebellar ataxia [31]. The prevalence of MSA is 4.4 per 100,000 [32]. MSA, together with progressive supranuclear palsy (PSP), is called Parkinson Plus Syndrome. The Neuroprotection and Natural History in Parkinson Plus Syndromes (NNIPPS) diagnostic criteria are consistent and valid. They can be used to distinguish MSA from PSP with high accuracy [33]. MSA is usually diagnosed based on clinical features (autonomic failure/urinary dysfunction plus either parkinsonism poorly responsive to levodopa or cerebellar ataxia) [34]. However, the accuracy of the clinical diagnosis of MSA is unsatisfactory due to the complexity of the clinical features and pathological changes, which sometimes overlap with those of other synucleinopathies [34]. The positive predictive value (PPV) at the later stage of MSA is reported to range from 60 to 90% [35]. A definite diagnosis relies on postmortem pathological examinations [36]. According to clinical features, MSA is subdivided into MSA-C, for those with predominant degeneration in cerebellar circuitry with ataxia, and MSA-P for those with predominant degeneration in the basal ganglia with parkinsonism [37, 38]. The MSA-P phenotype is the most common variant in Europe and USA, accounting for about 65% of all cases [39, 40, 41]. The most frequently occurring motor symptom in this phenotype is rigidity, followed by bradykinesia, tremor and postural instability [42]. Patients with this phenotype usually show poor response to levodopa. In Japanese population, MSA-C phenotype is present in 83.8% of MSA patients at first examination and in 48.6% of the patients at last follow-up [43]. These patients usually present ataxia of gait, instability, and falls but also with ataxia of limbs and speech, intention tremor, and disorders of extraocular movements such as square wave jerks, saccadic pursuit, nystagmus, overshoot or undershoot dysmetria, or slow pursuit (Table 1).
Like PD and DLB, MSA patients also develop various non-motor symptoms, with the most common one being the autonomic failure. The symptoms associated with the autonomic failure include orthostatic hypotension and urogenital disturbances such as increased frequency, enhanced urgency, incontinence and/or retention associated with male erectile dysfunction and female genital hyposensitivity [44]. Pyramidal signs such as Babinski signs, spasticity, hyperreflexia due to pyramidal tract degeneration are found in around half of the patients [45]. More than one-thirds of patients have sleep disorders and dementia [46]. The sleep disorder is accompanied by the specific sleep-related inspiratory stridor. The patterns of cognitive deficits are widely overlapped with those in other parkinsonian disorders [46].
Pathological features
PD Pathologically, PD is characterized by the loss of pigmented dopaminergic neurons in the substantia nigra pars compacta (SNpc) and the formation of α-syn-containing inclusions in neuronal somata and neurites designated LBs and LNs, or collectively known as Lewy-related α-syn pathologies (LRP) [1, 6]. Although the motor symptoms of PD are attributed to the loss of dopaminergic neurons within the area of the substantia nigra pars compacta (SNpc) [1], neuronal loss is also found in many other brain regions, such as the ventral tegmental area (VTA), the locus coeruleus (LC), nucleus basalis of Meynert (NBM), pedunculopontine nucleus (PPN), raphe nucleus, dorsal motor nucleus of the vagus, amygdala, and hypothalamus [5, 47].
The distribution and progression of LRP in PD was first investigated by Braak and his colleagues [2], who proposed a staging scheme based on the topographical location of LRP in a large cohort [2], which has been improved by subsequent studies. According to Braak staging, LRP initially occur in the olfactory mucosa and enteric nervous system, travel into the brain via the vagal and olfactory nerves, and progress to particular brain structures in a predictable pattern [2, 47]. This pattern begins in the dorsal motor nucleus of the glossopharyngeal and vagal nerves and olfactory bulb (stage one), ascending to the pontine tegmentum (stage two), midbrain (stage three), mesocortex and allocortex (stage 4), and finally culminating in widespread neocortical regions (Stages 5 and 6) [2, 47]. Prospective assessment of PD patients to autopsy reveals that the progression of LRP in typical cases (excluding early-onset cases) is consistent with Braak staging, where brainstem LRP dominates in those surviving to 5 years, by 13 years 50% of cases have a transitional distribution to limbic regions, and by 18 years all have at least this pathological phenotype [6]. It is thought that the earliest stages represent a preclinical disease phase in the absence of any motor disability [2]. The pattern and severity of LRP were found to be correlated with different clinical phenotypes. The more rapid disease course, along with higher amounts of pathological deposits and additional neuropathology, suggests an even faster rate of LRP deposition that appears to be linked to multiple pathologies in older-onset PD patients. These cases have similarities to those described below with a dementia dominant phenotype.
DLB The frequency and density of LRP in DLB patients have little difference from those in PD and PDD patients [48]. Compared with PD patients, the majority of DLB cases are found to have an advanced Braak stage, with cortical involvement [48]. In contrast, DLB patients have a less marked loss of the dopaminergic neurons in the substantia nigra and a relative lack of D2 receptor upregulation in the striatum [49]. In addition, many patients with DLB have substantial amyloid deposition in the striatum, hippocampus and cortex [1, 5, 50], much like the older-onset group of PD patients mentioned above. Coexisting LRP and AD pathology (Aβ and tau) is frequently found in DLB at postmortem [51, 52].
MSA The core pathological feature of all clinical subtypes of MSA is the presence of α-syn-positive glial cytoplasmic inclusions (GCIs) in oligodendroglia, which are widely observed throughout the brain [53]. Other α-syn-containing inclusions found in the brain of MSA patients include glial nuclear inclusions (GNIs), neuronal cytoplasmic inclusions (NCIs), neuronal nuclear inclusions (NNIs) [7]. Although neuronal loss and GCIs are key pathological findings in MSA, the severity of these lesions and their regional distribution can be highly variable, resulting in clinical heterogeneity. Pathologically, MSA cases were separated into those with predominately olivopontocerebellar (OPC) and striatonigral (StrN) involvement, corresponding to the clinical phenotypes of MSA-C and MSA-P. Historically, these pathological variants were termed striatonigral degeneration (SND) [54] and olivopontocerebellar atrophy (OPCA) [55], respectively. An earlier study described two clinically diagnosed MSA-P cases with widespread GCIs and neuronal loss restricted to the substantia nigra and locus coeruleus; such cases are examples of pure SND and were coined “minimal change” MSA [56]. In all the cases described by Ozawa et al. [57, 58], neuronal loss was present in at least one StrN and OPC region, with no cases being “pure” SND or “pure” OPCA. A report has also reported that a case of “minimal change of OPCA”, with neuronal loss being confined to OPC structures [59]. Like most sporadic neurodegenerative diseases, the strongest known risk factor for MSA is ageing. Therefore, it is not surprising that the pathological hallmarks of other age-associated disorders are sometimes found in conjunction with MSA, termed concomitant pathologies. In 94 of MSA cases from the UK, screening of the dorsal motor nucleus of the vagus and substantia nigra revealed the presence of LBs, the pathological hallmark of PD and DLB, in approximately 10% cases [57]. These studies suggest that LBs may represent an independent disease process in MSA, although a similar study in 50 cases of Japanese MSA reported no cases with LBs [58]. However, significant correlation was mainly observed between the frequency of GCIs and the severity of neuronal cell loss, and between these pathological changes and disease duration [57]. Grading systems have been proposed with cases assigned a separate severity grade between 0 and 3 for both MSA-P and MSA-C pathology, reflecting the considerable overlap between these subtypes [1].
Hippocampal manifestations
The hippocampus is a major component of the brain that plays important roles in the consolidation of new memory, emotional responses, navigation, and spatial orientation. It belongs to the limbic system and consists of several structures, including the dentate gyrus, the CA1-CA3 layers, and the subiculum [60]. The entorhinal cortex (EC), located in the parahippocampal gyrus, is considered to be part of the hippocampal region because it serves as the main “interface” between the hippocampus and other parts of the brain. The hippocampus is one of the most vulnerable brain regions affected by synucleinopathies, and the hippocampal dysfunction may cause various neuropsychiatric manifestations such as cognitive deficits, depression, anxiety, hyposmia, anhedonia, and psychosis, which have described above. In this section, we will discuss the pathological changes in the hippocampus and the possible mechanisms underlying the hippocampal dysfunctions associated with depression and cognitive deficits, the most frequently occurring symptoms observed in the three major synucleinopathies [61–67].
Pathological changes
Hippocampal atrophy
There is a controversy on the volume loss of the hippocampus in PD patients with normal cognition (PD-NC). Some studies described the volume loss of the hippocampus in PD-NC as compared with normal controls [68–71]. Some others reported the lack of difference in the hippocampal volume between PD-NC and normal controls [72, 73]. Different from PD-NC, PD patients with mild cognitive impairment (PD-MCI) and dementia (PDD) show a significant reduction in the hippocampal volume [68, 69, 71–77]. Patients with DLB also have a reduced hippocampal volume as those with PDD. However, this volume reduction is not significantly different between DLB and PDD, although it is smaller than that in AD [71, 78–82]. In patients with MSA, only the MSA-P phenotype was shown to have a reduction in the hippocampal volume as compared with control subjects [83–85].
There is a body of evidence suggesting the correlation between hippocampal volume loss and cognitive impairment in synucleinopathies. For example, memory impairment is an important feature of cognitive dysfunction in PD. It can be observed since early stages [86], is more pronounced in patients with visual hallucinations [87, 88] and predicts conversion to dementia [89]. The results that significant hippocampal volume loss is only observed in PD-MCI and PDD but not in PD-NC indicate the association between hippocampal volume loss and cognitive impairment. Direct evidence showing the relationship between hippocampal volume loss and cognitive impairment in PD patients has been obtained by volumetric magnetic resonance imaging [71, 90–92], which showed a pattern (control > PD > PDD > AD) of changes in the hippocampal volume. It is suggested that low hippocampal volume can be an important predictive factor for the progression from PD-NC to PD-MCI and also from PD-MCI to PDD [75]. Discriminant analysis and a receiver operating characteristics approach showed that mean cortical thickness and hippocampus volume have 80% accuracy in identifying PD patients with dementia [93]. In addition, white matter hyperintensity (WMH) is demonstrated to be an additional factor determining the progression of cognitive impairment in PD [75]. The finding that both hippocampal volume and WMH contribute to the development of cognitive impairment and dementia in PD is important as it would allow further studies to investigate the mechanisms by which hippocampal volume and WMH act synergistically in PD dementia.
The DLB patients also show the correlation between hippocampal volume loss and cognitive decline. For example, voxel-based morphometry results showed that the right hippocampus and amygdala volume correlated with Visual Memory Test in DLB patients [82]. In a study with 3T T1-weighted imaging, DLB patients were shown to have milder hippocampal atrophy that was accompanied by preservation of the CA1 compared with AD patients. Among DLB subjects, CA1 was correlated with the Recent Memory Score of the Cambridge Cognitive Examination (CAMCOG) and Delayed Recall subscores of the The Hopkins Verbal Learning Test (HVLT) [94]. These findings highlight the promising role of hippocampal subfield volumetry, particularly that of the CA1, as a biomarker for the distinction between AD and DLB. Compared with pure DLB patients, the mixed DLB/AD patients displayed greater atrophy rates in the whole brain, temporoparietal cortices, hippocampus and amygdala, and ventricle expansion, similar to AD patients. In the DLB and DLB/AD patients, the atrophy rates correlated with Braak neurofibrillary tangle stage, cognitive decline, and progression of motor symptoms [95].
The MSA patients also manifest cognitive impairment, with prevalence rates being up to 31%. The patterns of cognitive deficits are widely overlapped with those of parkinsonian disorders, with some suggestive of hippocampal dysfunction [46, 96]. However, direct data showing the correlation between cognitive impairment and hippocampal atrophy in MSA remain to be collected.
It is well established that reduced hippocampal volumes are consistently associated with major depression [97–99]. Studies have shown that about 90% of PD patients have at least one neuropsychiatric symptom, among which, depression is considered as the frequent one. Studies with magnetic resonance imaging (MRI) detection have revealed that the patients with a history of several depressive episodes have significantly smaller hippocampal volumes in comparison to controls [100, 101]. This observation was further confirmed in meta-analyses of MRI studies of hippocampal volume in depression [102, 103]. Depression was also found in patients with DLB and MSA [104]. Since the hippocampal volume loss is also present in both diseases, it may also contribute to the depression, although studies for the direct link have not been reported.
Hippocampal α-syn pathology
Since α-syn-containing inclusions (LBs, LNs, GCIs, GNIs and NCIs) are hallmark pathologies of synucleinopathies, it is reasonable to assume that the presence and density of these protein inclusions in the hippocampus and related brain regions are associated with neuropsychiatric impairments in these disorders. Attempts have been made to relate cortical LBs and LNs with cognitive impairment in PD. It was demonstrated in demented PD patients that the densities of LBs, LNs, and LGs (Lewy grains) were significantly greater in amygdala, entorhinal cortex (EC), and sectors CA2/CA3 of the hippocampus, whereas middle frontal gyrus, sector CA1, and dentate gyrus were least affected [105]. In patients with a long disease duration where sufficient time for the slow accumulation of LRPs can occur, limbic and cortical LRPs correlates with the presence and severity of cognitive impairment in PD [106–110]. In a study performed on elderly PD patients in whom parkinsonism preceded cognitive decline by at least 3 years, Kövari and colleagues found that LB densities in the entorhinal and anterior cingulate cortex may predict cognitive deficits in PD. They suggested that LB formation in limbic areas may be crucial for the development of PD dementia [111]. Harding and Halliday indicated that high densities of parahippocampal LBs could separate demented from non-demented PD cases with high sensitivity and specificity [108]. In a study where α-syn, phosphorylated tau (phosphotau) and Aβ plaque pathology in PDD and DLB patients was assessed semi-quantitatively in four regions of the neocortex, the decline in cognition, assessed by Mini Mental State Examination, was found to correlate positively with the cortical α-syn load. Patients also had varying degrees of senile Aβ plaque and phosphor-tau pathology. Regression analyses pointed to a combined pathology (Aβ plaque plus phosphor-tau plus α-syn-positive features), particularly in the prefrontal cortex and temporal lobe neocortex with the superior and middle temporal gyrus being a major determining factor in the development of dementia. This study suggests that cognitive decline in LB dementia is not a consequence of α-syn-induced neurodegeneration alone, and senile plaque and phosphor-tau pathology also contribute to the overall deficits.
In typical MSA patients, the oligodendrocyte GCIs and GNIs are seldom observed in the hippocampus, although their presence in the temporal lobe has been reported in some rarer cases [85, 112, 113]. Atypical MSA (aMSA) is a term recently introduced by Aoki and his colleagues [114] to describe cases that show hallmark GCI pathological changes while clinically present with frontotemporal dementia (FTD) syndromes associated with frontotemporal lobar degeneration and severe limbic and cortical α-syn neuronal pathology [114]. Compared with typical MSA, the atypical MSA has significantly more neuronal inclusions in anteromedial temporal lobe and limbic structures (e.g., hippocampus and amygdala) [114]. However, if the increased neuronal inclusions correlate with the severity of cognitive deficit in MSA remains to be investigated.
While the above studies suggest an association between cortical LBs and cognitive impairment, other studies have not confirmed this assumption [115–117]. As have been stated, LB pathology may be a structural manifestation of a cytoprotective response or a failed cellular self-preservation mechanism to confine and eliminate cytotoxic proteins, and the real pathogenic form of α-syn is its aggregates and oligomers. For example, although incidental LB disease (iLBD) is often assumed to represent preclinical PD [29], in some PD patients, significant neurodegeneration and cellular dysfunction precedes LB pathology in the SNpc, challenging the pathogenic role of LB pathology in PD [30]. Studies using protein-fragment complementation assays have demonstrated that α-syn oligomers are associated with enhanced cytotoxicity in living cells, which can be rescued by Hsp70 in a process that reduces the formation of α-syn oligomers [118]. Other convictive evidence comes from a study on α-syn-overexpressing cells, showing that the toxicity of α-syn was alleviated by a single chain antibody (scFv) targeting the clearance of oligomeric but not monomeric α-syn [119]. The neurotoxicity of α-syn oligomers has also been demonstrated in animal models using mutant forms of α-syn with decreased capacity to form fibrils but increased propensity to form soluble oligomers [120]. In these animals, α-syn accumulation in the hippocampus was accompanied by cognitive deficits [121, 122]. In accordance with the findings in cells and animals, patients with parkinsonism (PD, DLB, and MSA) have increased levels of α-syn oligomers in the brain compared to those without parkinsonism or to healthy controls [123–126]. The above findings suggest a relationship between endogenous α-syn oligomers and neurodegeneration in synucleinopathies. To support this notion, neuropathological studies in a large series have confirmed that staging of LB pathology is barely applicable to cognitive impairment and dementia. Only a percentage of cases showed a relationship between cortical LBs and cognitive impairment and dementia [115], indicating that cortical LBs are not per se causative of dementia, but rather indicators of pathological α-syn aggregates. While the pathophysiology of the neurodegenerative process can hardly be explained by LBs, the clinical symptoms do indicate a degenerative process located at the presynapses resulting in a neurotransmitter deficiency. It was shown that 90% or even more of α-syn aggregates in DLB cases were located at the presynapses, which was shown as Proteinase K-resistant in distinct brain regions, including the hippocampus, temporal cortex and substantia nigra [127]. The PK-resistant α-syn aggregates were also found in the presynaptic nerve terminals in the hippocampus and temporal cortex in A53T α-syn transgenic mice [127]. To further support the neurotoxicity of insoluble α-syn aggregates, recent studies showed that perturbing normal α-syn repeat motifs, which occurs in α-syn mutations such as E46 K, promotes a conversion of α-syn from physiological tetramers into monomers [128]; this conversion decreases α-syn solubility and increases its aggregation and neurotoxicity [128]. By examining the insoluble α-syn aggregates-accumulated presynaptic sites in both transgenic mice [127] and PD brains, it was found that the dendritic spines were retracted, whereas the presynapses were relatively preserved, suggesting a neurotransmitter deprivation. These findings give rise to the notion that not only cell death but also α-syn aggregate-related synaptic dysfunction may cause clinical symptoms in synucleinopathies [129].
Other pathologies
DLB and PDD are characterized by the presence of α-syn-containing LBs and LNs. However, they also show variable degrees of AD pathology, such as senile plaques and neurofibrillary tangles, particularly in areas of the cortex associated with higher cognitive functions [108, 130]. Although the decline in cognition in both dementias was found to correlate positively with the cortical α-syn load, patients also had varying degrees of senile Aβ plaque and phosphor-tau pathology. Regression analyses pointed to a combined pathology (Aβ plaque plus phosphor-tau plus α-syn-positive features), particularly in the prefrontal cortex (BA9) and temporal lobe neocortex with the superior and middle temporal gyrus (BA21, 22), being a major determining factor in the development of dementia [131]. Thus, cognitive decline in Lewy body dementias is not a consequence of α-syn-induced neurodegeneration alone but senile plaque and phosphor-tau pathology also contribute to the overall deficits. In atypical MSA, except GCIs and NCIs, numerous Pick body-like inclusions in hippocampus and amygdala associated with neuronal loss and atrophy are the most specific features of atypical MSA [114].
Mechanisms underlying hippocampal dysfunctions in synucleinopathies
The hippocampal formation receives information from widely spread cortical and subcortical regions, and in turn sends signals through efferent nerves to many of the cortical regions as well as subcortical nuclei [132]. Previous studies have demonstrated impairments of the dopaminergic, serotonergic, cholinergic, and adrenergic neurons from the subcortical nuclei and their association with hippocampal dysfunction in patients with PD-MCI, PD-D, and DLB, which have been well reviewed elsewhere [133, 134]. Here, we will focus on recent progresses for the potential mechanisms underlying the deficits in synaptic transmission and neurogenesis induced by α-syn abnormalities and discuss their possible roles for the hippocampus-mediated depression and cognitive deficits in synucleinopathies.
α-Syn-induced deficits in synaptic transmission
The connectivity between neurons in the brain depends on the number of synapses and their plasticity. The synaptic plasticity mainly refers to a persistent strengthening and weakening of the synaptic transmission efficacy. There is a body of evidence supporting that α-syn abnormalities can affect the efficacy of synaptic transmission by both the presynaptic and postsynaptic mechanisms. One way that α-syn affects synaptic transmission is to modulate neurotransmitter release. This effect is likely mediated by affecting the spatial organization of distinct synaptic vesicle pools within the presynaptic terminal, possibly via α-syn multimerization [135, 136] or by modulating intersynaptic vesicular dynamics [137]. α-Syn may exert its effect on synaptic vesicle recycling by its ability to bind membrane and potentiate SNARE-complex assembly [138, 139]. Another way that α-syn affects synaptic transmission is to modulate the trafficking and activity of neurotransmitter transporters, which serve to remove neurotransmitters from the synaptic cleft and reuptake the transmitters into cytosol from which they are sequestered into vesicles for storage and later release. The transporters found to be regulated by α-syn include dopamine, serotonin, and norepinephrine transporters [133]. In line with the results for the presynaptic impairments observed in experimental models, in vivo imaging studies on synaptic functions of the central nervous system provide compelling evidence for presynaptic neurotransmitter deficiencies in PD, PDD and DLB [140]. In addition to the presynaptic mechanisms, α-syn can also affect synaptic transmission by modulating the activity and expression of postsynaptic receptors. For example, extracellular α-syn oligomers have been shown to impair long-term potentiation by activating NMDA receptors [141, 142]. Besides, extracellular α-syn and overexpressed α-syn have been demonstrated to promote clathrin-mediated NMDA receptor endocytosis, leading to the reduction in the level of membrane NMDA receptors and the NMDA receptor-mediated Ca2+ influx upon stimulation [143, 144]. In accordance with the in vitro findings, α-syn transgenic mice showed reduced surface NMDA receptor levels and NR2A/NR2B subunit ratio in the hippocampus and altered hippocampus-related memory and long-term potentiation (LTP) [143, 145].
As have mentioned above, the connectivity between neurons depends on not only the synaptic plasticity but also the number of synapses. Loss of synapses has been observed in the frontal and temporal cortex as well as the hippocampus in patients with DLB, which correlates well with the cognitive impairment [146, 147]. Significant loss of presynaptic terminals are also demonstrated a few months after small α-syn aggregates begin to appear in the hippocampus of an α-syn overexpressing mouse model of DLB [148]. When the overexpressing transgene was switched off, the synapse loss was reversed, with a simultaneous clearance of the α-syn pathology, indicating a toxicity of the α-syn aggregates to the synapse. In line with the results obtained in animal models, in human LBD brains, the accumulation of protease K (PK)-resistant small α-syn aggregates can be observed at presynaptic terminals [129, 149, 150]. How might these α-syn aggregates or oligomers damage the synapse or cause synaptotoxicity? Based on the evidence obtained so far, several potential mechanisms are suggested. First, α-syn oligomers may directly change the permeability of the synaptic membrane by forming α-syn pores [151, 152] or inducing membrane thinning [153–155]. Second, α-syn oligomers may induce synaptotoxicity by damaging mitochondria [156], reducing synaptic proteins [157–159] or interfering with synaptic vesicle recycling [144, 160]. Third, in addition to acting on presynaptic terminals, α-syn oligomers may damage spine morphogenesis by affecting the function of NMDA receptors [141] since the latter plays an important role in spine morphogenesis [161]. Given the importance of NMDA receptors in synaptic signaling and spine morphogenesis, it is no surprise to find in human post-mortem tissue and numerous models of PD that spine densities are altered [161, 162].
Taken together, α-syn abnormalities can cause either the impairment of synaptic plasticity or the loss of synapses, leading to deficits in synaptic transmission. The toxic effect of α-syn on synaptic transmission can disrupt the connectivity between either the neurons within the hippocampus or the hippocampal neurons with those from the subcortical nuclei. This will impair hippocampal function, causing the hippocampus-mediated cognitive deficits and depression. It is well established that hippocampal LTP represents the major experimental model for the synaptic changes underlying learning and memory. It has been demonstrated that the LTP in the CA3/CA1 Schaffer collateral/commissural pathway of the hippocampus are affected by exogenously applied α-syn oligomers [141, 142]. Because the synaptic plasticity of this pathway is modulated by the mesolimbic dopaminergic neurons in the medial substantia nigra (A9 neurons) and nearby ventral tegmental area (A10 neurons) through dopamine D1/D5 receptors [163–166], deficits in synaptic transmission between the dopaminergic neurons and the hippocampal neurons will impair the hippocampal function. As the evidence for this, in mice transgenic for truncated α-syn (1–120), the hippocampal LTP was found to change, which was associated with an impaired dopaminergic transmission and a decrease of NR2A/NR2B subunit ratio in synaptic NMDA receptors. Deficits in hippocampus-dependent learning were also found in this animal model. Interestingly, the dopamine precursor L-DOPA was able to restore the hippocampal synaptic potentiation via D1/D5 receptors and to ameliorate the cognitive deficit in the parkinsonian animals [143]. In consistent with the results of animal experiments, a single serial section study assessing the mesocortical A10 dopamine neurons proper revealed limited degeneration in the A10 dopamine cell groups in PD and PDD patients [167]. Despite this, in vivo imaging suggests a reduction in cortical dopamine in patients with PDD [168], indicating a functional rather than structural depletion of dopamine in the mesocortical system.
Except the dopaminergic innervation, the hippocampal formation also receives the serotonergic and noradrenergic projections from the raphe nucleus and locus coeruleus, the two nuclei that are vulnerable to α-syn pathology. Deficits in the serotonergic and noradrenergic innervation to the hippocampus have been reported in PD patients [169], which are believed to contribute to the development of dementia and depression. In BAC α-syn transgenic rat model, a serotonergic deficit in the hippocampus as defined by reduced levels of serotonin (5-HT) 1B receptor, decreased 5-HT neurotransmitter levels, and a loss of serotonergic nerve terminals innervating the DG/CA3 subfield were observed, while the number of serotonergic neurons in the raphe nuclei remained unchanged. Importantly, the BAC α-syn rats showed an early anxiety-like phenotype consisting of reduced exploratory behavior and feeding [170]. Decreased 5-HT1A receptor availability is found in limbic regions including the hippocampus in depressed PD patients [171, 172]. These findings are in agreement with post-mortem evidence and support the hypothesis that reductions in postsynaptic 5-HT1A receptors availability could be an underlying mechanism for the development of depression in PD [171]. In addition, preferential degeneration of noradrenergic terminals is reported in transgenic mice overexpressing mutant human A53T α-syn [173]. Moreover, α-syn has been demonstrated to attenuate the norepinephrine transporter activity and trafficking [174]. Therefore, there is also a possibility that α-syn abnormalities in the noradrenergic neurons of the locus coeruleus may also affect the hippocampal function.
α-Syn-induced deficits in hippocampal neurogenesis
Adult hippocampal neurogenesis occurs in a relatively limited area, the subgranular zone (SGZ) of the dentate gyrus (DG). There are numerous studies supporting the role of adult hippocampal neurogenesis in memory formation and emotion processing. For example, early studies specifically ablating adult hippocampal neurogenesis suggest the role of newly generated granule cells in memory formation [175–178], which are confirmed by recent advanced technologies such as conditional gene targeting, viral injection, and optogenetic approaches. Besides, reduced hippocampal neurogenesis has been observed in animal models and some patients with depression. There is evidence that antidepressant treatment can improve the adult hippocampal neurogenesis and the depression symptom [179–182]. Because postmortem analyses of adult neurogenesis are limited, direct investigation of alterations in adult hippocampal neurogenesis has been carried out in only a few samples of PD and DLB patients. These studies have revealed changes in some proteins in the patients that are implicated in adult hippocampal neurogenesis. For example, the number of cells positive for proliferating cell nuclear antigen (PCNA), epidermal growth factor (EGF) receptor, nestin, and 3-tubulin was found to reduce in the SGZ and the subventricular zone (SVZ) of PD patients when compared to controls [183]. In addition, a reduction of Musashi-positive cells within the hippocampal SVZ, subgranular layer (SGL) and ependymal cell layer (EPL) SVZ (representing neural stem and progenitor cells within this area) was noted in specimen of DLB [184]. The observed decrease in the SGV and SVZ proliferation of patients with LB disease is speculated to be a consequence of dopamine depletion [183].
In contrast to the limited amount of data and materials from human LB brains, many studies have been conducted in PD animal models, mainly in rodents. Studies on dopaminergic lesion models using 6-hydroxydopamine (6-OHDA) or 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) have revealed a negative impact of dopaminergic deafferentation on neural progenitor cell (NPC) proliferation in SVZ, and dopaminergic stimulation increases proliferation in non-lesioned and lesioned rodents [183, 185, 186]. These results reinforce the speculation for the role of dopaminergic innervation in SVZ proliferation. In addition to lesioned PD models, adult neurogenesis has been studied in different transgenic mice that overexpress wild type or mutant α-syn. In these mice, neurogenetic deficits can be observed in the hippocampus [67, 170, 187–189]. Although there is possibility that impaired dopaminergic innervation may contribute to the hippocampal neurogenetic deficits since degeneration of dopaminergic neurons also occurs in these animals [187, 190], evidence obtained also supports the direct effect of α-syn on neurogenesis. For example, in a tetracycline-suppressive (tet-off) transgenic mouse model, reduced neurogenesis in the hippocampus and olfactory bulb was observed when the A30P mutant α-syn was overexpressed, which was restored to control levels after the A30P α-syn was abrogated [191, 192]. In addition, the induced pluripotent stem cells that derived from PD patients with SNCA gene triplication exhibited elevated α-syn expression and impaired neuronal differentiation and maturation [193], further supporting that the abnormal accumulation of α-syn may directly affect the neurogenesis in the hippocampus.
Due to the potential roles of adult hippocampal neurogenesis in memory formation and emotion processing, its defect may contribute to the manifestations of neuropsychiatric impairments such as cognitive deficits and depression in synucleinopathies.
Concluding remarks
While all the three synucleinopathies (PD, DLB, MSA) have α-syn-containing inclusions found in the brains of patients, the cell types and structures affected vary between different disorders. This determines the distinctive clinical features of each disease, although they all manifest as a chronic and progressive decline in motor, cognitive, behavioral, and autonomic functions. The formation of α-syn-containing inclusions is frequently observed in the hippocampus and related brain regions of patients with synucleinopathies, which are accompanied by hippocampal atrophy and dysfunction as well as neuropsychiatric symptoms such as cognitive deficits and depression. Although the α-syn-containing inclusions are hallmark pathological changes in synucleinopathies, increasing evidence supports that small α-syn aggregates or oligomers are toxic species that induce neurodegeneration initially starting at the synaptic site. Both neuronal functional change and degeneration in the hippocampus and some subcortical neurons with projections to the hippocampus and related regions can lead to the manifestations of neuropsychiatric abnormalities in synucleinopathies.
References
McCann H, Stevens CH, Cartwright H, Halliday GM (2014) alpha-Synucleinopathy phenotypes. Parkinsonism Relat Disord 20(Suppl 1):S62–S67
Braak H, Del TK, Rub U, de Vos RA, Jansen Steur EN, Braak E (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Spillantini MG, Schmidt ML, Lee VM, Trojanowski JQ, Jakes R, Goedert M (1997) Alpha-synuclein in Lewy bodies. Nature 388:839–840
Gai WP, Power JH, Blumbergs PC, Blessing WW (1998) Multiple-system atrophy: a new alpha-synuclein disease? Lancet 352:547–548
Halliday GM, Holton JL, Revesz T, Dickson DW (2011) Neuropathology underlying clinical variability in patients with synucleinopathies. Acta Neuropathol 122:187–204
Halliday GM, McCann H (2010) The progression of pathology in Parkinson’s disease. Ann N Y Acad Sci 1184:188–195
Wenning GK, Colosimo C, Geser F, Poewe W (2004) Multiple system atrophy. Lancet Neurol 3:93–103
von Campenhausen S, Bornschein B, Wick R, Botzel K, Sampaio C, Poewe W, Oertel W, Siebert U, Berger K, Dodel R (2005) Prevalence and incidence of Parkinson’s disease in Europe. Eur Neuropsychopharmacol 15:473–490
Muangpaisan W, Mathews A, Hori H, Seidel D (2011) A systematic review of the worldwide prevalence and incidence of Parkinson’s disease. J Med Assoc Thai 94:749–755
Jankovic J (2008) Parkinson’s disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry 79:368–376
Fereshtehnejad SM, Shafieesabet M, Farhadi F, Hadizadeh H, Rahmani A, Naderi N, Khaefpanah D, Shahidi GA, Delbari A, Lokk J (2015) Heterogeneous determinants of quality of life in different phenotypes of Parkinson’s disease. PLoS One 10:e0137081
Kalia LV, Lang AE (2015) Parkinson’s disease. Lancet 386:896–912
Rajput AH, Voll A, Rajput ML, Robinson CA, Rajput A (2009) Course in Parkinson disease subtypes: a 39-year clinicopathologic study. Neurology 73:206–212
Rodrigues TM, Castro CA, Ferreira JJ (2016) Pharmacological interventions for daytime sleepiness and sleep disorders in Parkinson’s disease: systematic review and meta-analysis. Parkinsonism Relat Disord 27:25–34
Jellinger KA (2015) Neuropathobiology of non-motor symptoms in Parkinson disease. J Neural Transm 122:1429–1440
Espay AJ, LeWitt PA, Kaufmann H (2014) Norepinephrine deficiency in Parkinson’s disease: the case for noradrenergic enhancement. Mov Disord 29:1710–1719
Marras C, Chaudhuri KR (2016) Nonmotor features of Parkinson’s disease subtypes. Mov Disord 31:1095–1102
Vann Jones SA, O’Brien JT (2014) The prevalence and incidence of dementia with Lewy bodies: a systematic review of population and clinical studies. Psychol Med 44:673–683
Burn DJ, Rowan EN, Allan LM, Molloy S, O’Brien JT, McKeith IG (2006) Motor subtype and cognitive decline in Parkinson’s disease, Parkinson’s disease with dementia, and dementia with Lewy bodies. J Neurol Neurosurg Psychiatry 77:585–589
Burn DJ, Rowan EN, Minett T, Sanders J, Myint P, Richardson J, Thomas A, Newby J, Reid J, O’Brien JT, McKeith IG (2003) Extrapyramidal features in Parkinson’s disease with and without dementia and dementia with Lewy bodies: a cross-sectional comparative study. Mov Disord 18:884–889
Fujishiro H, Iseki E, Nakamura S, Kasanuki K, Chiba Y, Ota K, Murayama N, Sato K (2013) Dementia with Lewy bodies: early diagnostic challenges. Psychogeriatrics 13:128–138
Auning E, Rongve A, Fladby T, Booij J, Hortobagyi T, Siepel FJ, Ballard C, Aarsland D (2011) Early and presenting symptoms of dementia with lewy bodies. Dement Geriatr Cogn Disord 32:202–208
Chiba Y, Fujishiro H, Iseki E, Ota K, Kasanuki K, Hirayasu Y, Satoa K (2012) Retrospective survey of prodromal symptoms in dementia with Lewy bodies: comparison with Alzheimer’s disease. Dement Geriatr Cogn Disord 33:273–281
Boot BP, Orr CF, Ahlskog JE, Ferman TJ, Roberts R, Pankratz VS, Dickson DW, Parisi J, Aakre JA, Geda YE, Knopman DS, Petersen RC, Boeve BF (2013) Risk factors for dementia with Lewy bodies: a case-control study. Neurology 81:833–840
Vardy E, Holt R, Gerhard A, Richardson A, Snowden J, Neary D (2014) History of a suspected delirium is more common in dementia with Lewy bodies than Alzheimer’s disease: a retrospective study. Int J Geriatr Psychiatry 29:178–181
Ballard C, McKeith I, Burn D, Harrison R, O’Brien J, Lowery K, Campbell M, Perry R, Ince P (1997) The UPDRS scale as a means of identifying extrapyramidal signs in patients suffering from dementia with Lewy bodies. Acta Neurol Scand 96:366–371
Dodel R, Csoti I, Ebersbach G, Fuchs G, Hahne M, Kuhn W, Oechsner M, Jost W, Reichmann H, Schulz JB (2008) Lewy body dementia and Parkinson’s disease with dementia. J Neurol 255(Suppl 5):39–47
Baskys A (2004) Lewy body dementia: the litmus test for neuroleptic sensitivity and extrapyramidal symptoms. J Clin Psychiatry 65(Suppl 11):16–22
McKeith IG, Dickson DW, Lowe J, Emre M, O’Brien JT, Feldman H, Cummings J, Duda JE, Lippa C, Perry EK, Aarsland D, Arai H, Ballard CG, Boeve B, Burn DJ, Costa D, Del ST, Dubois B, Galasko D, Gauthier S, Goetz CG, Gomez-Tortosa E, Halliday G, Hansen LA, Hardy J, Iwatsubo T, Kalaria RN, Kaufer D, Kenny RA, Korczyn A, Kosaka K, Lee VM, Lees A, Litvan I, Londos E, Lopez OL, Minoshima S, Mizuno Y, Molina JA, Mukaetova-Ladinska EB, Pasquier F, Perry RH, Schulz JB, Trojanowski JQ, Yamada M (2005) Diagnosis and management of dementia with Lewy bodies: third report of the DLB Consortium. Neurology 65:1863–1872
Thaisetthawatkul P, Boeve BF, Benarroch EE, Sandroni P, Ferman TJ, Petersen R, Low PA (2004) Autonomic dysfunction in dementia with Lewy bodies. Neurology 62:1804–1809
Stefanova N, Bucke P, Duerr S, Wenning GK (2009) Multiple system atrophy: an update. Lancet Neurol 8:1172–1178
Schrag A, Ben-Shlomo Y, Quinn NP (1999) Prevalence of progressive supranuclear palsy and multiple system atrophy: a cross-sectional study. Lancet 354:1771–1775
Bensimon G, Ludolph A, Agid Y, Vidailhet M, Payan C, Leigh PN (2009) Riluzole treatment, survival and diagnostic criteria in Parkinson plus disorders: the NNIPPS study. Brain 132:156–171
Kim HJ, Jeon BS, Jellinger KA (2015) Diagnosis and differential diagnosis of MSA: boundary issues. J Neurol 262:1801–1813
Joutsa J, Gardberg M, Roytta M, Kaasinen V (2014) Diagnostic accuracy of parkinsonism syndromes by general neurologists. Parkinsonism Relat Disord 20:840–844
Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias CJ, Trojanowski JQ, Wood NW, Colosimo C, Durr A, Fowler CJ, Kaufmann H, Klockgether T, Lees A, Poewe W, Quinn N, Revesz T, Robertson D, Sandroni P, Seppi K, Vidailhet M (2008) Second consensus statement on the diagnosis of multiple system atrophy. Neurology 71:670–676
Gilman S, Koeppe RA, Junck L, Little R, Kluin KJ, Heumann M, Martorello S, Johanns J (1999) Decreased striatal monoaminergic terminals in multiple system atrophy detected with positron emission tomography. Ann Neurol 45:769–777
Gilman S, Low PA, Quinn N, Albanese A, Ben-Shlomo Y, Fowler CJ, Kaufmann H, Klockgether T, Lang AE, Lantos PL, Litvan I, Mathias CJ, Oliver E, Robertson D, Schatz I, Wenning GK (1999) Consensus statement on the diagnosis of multiple system atrophy. J Neurol Sci 163:94–98
Kollensperger M, Geser F, Ndayisaba JP, Boesch S, Seppi K, Ostergaard K, Dupont E, Cardozo A, Tolosa E, Abele M, Klockgether T, Yekhlef F, Tison F, Daniels C, Deuschl G, Coelho M, Sampaio C, Bozi M, Quinn N, Schrag A, Mathias CJ, Fowler C, Nilsson CF, Widner H, Schimke N, Oertel W, Del SF, Albanese A, Pellecchia MT, Barone P, Djaldetti R, Colosimo C, Meco G, Gonzalez-Mandly A, Berciano J, Gurevich T, Giladi N, Galitzky M, Rascol O, Kamm C, Gasser T, Siebert U, Poewe W, Wenning GK (2010) Presentation, diagnosis, and management of multiple system atrophy in Europe: final analysis of the European multiple system atrophy registry. Mov Disord 25:2604–2612
Geser F, Seppi K, Stampfer-Kountchev M, Kollensperger M, Diem A, Ndayisaba JP, Ostergaard K, Dupont E, Cardozo A, Tolosa E, Abele M, Dodel R, Klockgether T, Ghorayeb I, Yekhlef F, Tison F, Daniels C, Kopper F, Deuschl G, Coelho M, Ferreira J, Rosa MM, Sampaio C, Bozi M, Schrag A, Hooker J, Kim H, Scaravilli T, Mathias CJ, Fowler C, Wood N, Quinn N, Widner H, Nilsson CF, Lindvall O, Schimke N, Eggert KM, Oertel W, del Sorbo F, Carella F, Albanese A, Pellecchia MT, Barone P, Djaldetti R, Meco G, Colosimo C, Gonzalez-Mandly A, Berciano J, Gurevich T, Giladi N, Galitzky M, Ory F, Rascol O, Kamm C, Buerk K, Maass S, Gasser T, Poewe W, Wenning GK (2005) The European Multiple System Atrophy-Study Group (EMSA-SG). J Neural Transm (Vienna) 112:1677–1686
Wenning GK, Geser F, Krismer F, Seppi K, Duerr S, Boesch S, Kollensperger M, Goebel G, Pfeiffer KP, Barone P, Pellecchia MT, Quinn NP, Koukouni V, Fowler CJ, Schrag A, Mathias CJ, Giladi N, Gurevich T, Dupont E, Ostergaard K, Nilsson CF, Widner H, Oertel W, Eggert KM, Albanese A, del Sorbo F, Tolosa E, Cardozo A, Deuschl G, Hellriegel H, Klockgether T, Dodel R, Sampaio C, Coelho M, Djaldetti R, Melamed E, Gasser T, Kamm C, Meco G, Colosimo C, Rascol O, Meissner WG, Tison F, Poewe W (2013) The natural history of multiple system atrophy: a prospective European cohort study. Lancet Neurol 12:264–274
Roncevic D, Palma JA, Martinez J, Goulding N, Norcliffe-Kaufmann L, Kaufmann H (2014) Cerebellar and parkinsonian phenotypes in multiple system atrophy: similarities, differences and survival. J Neural Transm (Vienna) 121:507–512
Yabe I, Soma H, Takei A, Fujiki N, Yanagihara T, Sasaki H (2006) MSA-C is the predominant clinical phenotype of MSA in Japan: analysis of 142 patients with probable MSA. J Neurol Sci 249:115–121
Kuzdas-Wood D, Stefanova N, Jellinger KA, Seppi K, Schlossmacher MG, Poewe W, Wenning GK (2014) Towards translational therapies for multiple system atrophy. Prog Neurobiol 118:19–35
da Rocha AJ, Maia AC Jr, da Silva CJ, Braga FT, Ferreira NP, Barsottini OG, Ferraz HB (2007) Pyramidal tract degeneration in multiple system atrophy: the relevance of magnetization transfer imaging. Mov Disord 22:238–244
Stankovic I, Krismer F, Jesic A, Antonini A, Benke T, Brown RG, Burn DJ, Holton JL, Kaufmann H, Kostic VS, Ling H, Meissner WG, Poewe W, Semnic M, Seppi K, Takeda A, Weintraub D, Wenning GK (2014) Cognitive impairment in multiple system atrophy: a position statement by the Neuropsychology Task Force of the MDS Multiple System Atrophy (MODIMSA) study group. Mov Disord 29:857–867
Braak H, Rub U, Gai WP, Del TK (2003) Idiopathic Parkinson’s disease: possible routes by which vulnerable neuronal types may be subject to neuroinvasion by an unknown pathogen. J Neural Transm 110:517–536
Beach TG, Adler CH, Lue L, Sue LI, Bachalakuri J, Henry-Watson J, Sasse J, Boyer S, Shirohi S, Brooks R, Eschbacher J, White CL, Akiyama H, Caviness J, Shill HA, Connor DJ, Sabbagh MN, Walker DG (2009) Unified staging system for Lewy body disorders: correlation with nigrostriatal degeneration, cognitive impairment and motor dysfunction. Acta Neuropathol 117:613–634
Piggott MA, Marshall EF, Thomas N, Lloyd S, Court JA, Jaros E, Burn D, Johnson M, Perry RH, McKeith IG, Ballard C, Perry EK (1999) Striatal dopaminergic markers in dementia with Lewy bodies, Alzheimer’s and Parkinson’s diseases: rostrocaudal distribution. Brain 122(Pt 8):1449–1468
Jellinger KA, Attems J (2006) Does striatal pathology distinguish Parkinson disease with dementia and dementia with Lewy bodies? Acta Neuropathol 112:253–260
Ballard C, Ziabreva I, Perry R, Larsen JP, O’Brien J, McKeith I, Perry E, Aarsland D (2006) Differences in neuropathologic characteristics across the Lewy body dementia spectrum. Neurology 67:1931–1934
Lopez OL, Becker JT, Kaufer DI, Hamilton RL, Sweet RA, Klunk W, DeKosky ST (2002) Research evaluation and prospective diagnosis of dementia with Lewy bodies. Arch Neurol 59:43–46
Jellinger KA (2014) Neuropathology of multiple system atrophy: new thoughts about pathogenesis. Mov Disord 29:1720–1741
Adams RD, Vanbogaert L, Vandereecken H (1964) Striato-nigral degeneration. J Neuropathol Exp Neurol 23:584–608
Savoiardo M, Strada L, Girotti F, Zimmerman RA, Grisoli M, Testa D, Petrillo R (1990) Olivopontocerebellar atrophy: MR diagnosis and relationship to multisystem atrophy. Radiology 174:693–696
Wenning GK, Quinn N, Magalhaes M, Mathias C, Daniel SE (1994) “Minimal change” multiple system atrophy. Mov Disord 9:161–166
Ozawa T, Paviour D, Quinn NP, Josephs KA, Sangha H, Kilford L, Healy DG, Wood NW, Lees AJ, Holton JL, Revesz T (2004) The spectrum of pathological involvement of the striatonigral and olivopontocerebellar systems in multiple system atrophy: clinicopathological correlations. Brain 127:2657–2671
Ozawa T, Tada M, Kakita A, Onodera O, Tada M, Ishihara T, Morita T, Shimohata T, Wakabayashi K, Takahashi H, Nishizawa M (2010) The phenotype spectrum of Japanese multiple system atrophy. J Neurol Neurosurg Psychiatry 81:1253–1255
Wakabayashi K, Mori F, Nishie M, Oyama Y, Kurihara A, Yoshimoto M, Kuroda N (2005) An autopsy case of early (“minimal change”) olivopontocerebellar atrophy (multiple system atrophy-cerebellar). Acta Neuropathol 110:185–190
Lavenex P, Lavenex PB, Amaral DG (2007) Spatial relational learning persists following neonatal hippocampal lesions in macaque monkeys. Nat Neurosci 10:234–239
Bannerman DM, Rawlins JN, McHugh SB, Deacon RM, Yee BK, Bast T, Zhang WN, Pothuizen HH, Feldon J (2004) Regional dissociations within the hippocampus–memory and anxiety. Neurosci Biobehav Rev 28:273–283
Fanselow MS, Dong HW (2010) Are the dorsal and ventral hippocampus functionally distinct structures? Neuron 65:7–19
Lauterbach EC (2004) The neuropsychiatry of Parkinson’s disease and related disorders. Psychiatr Clin North Am 27:801–825
Lee JS, Chun JW, Kang JI, Kang DI, Park HJ, Kim JJ (2012) Hippocampus and nucleus accumbens activity during neutral word recognition related to trait physical anhedonia in patients with schizophrenia: an fMRI study. Psychiatry Res 203:46–53
Adhikari A, Topiwala MA, Gordon JA (2010) Synchronized activity between the ventral hippocampus and the medial prefrontal cortex during anxiety. Neuron 65:257–269
Adhikari A, Topiwala MA, Gordon JA (2011) Single units in the medial prefrontal cortex with anxiety-related firing patterns are preferentially influenced by ventral hippocampal activity. Neuron 71:898–910
Marxreiter F, Regensburger M, Winkler J (2013) Adult neurogenesis in Parkinson’s disease. Cell Mol Life Sci 70:459–473
Danti S, Toschi N, Diciotti S, Tessa C, Poletti M, Del DP, Lucetti C (2015) Cortical thickness in de novo patients with Parkinson disease and mild cognitive impairment with consideration of clinical phenotype and motor laterality. Eur J Neurol 22:1564–1572
Jokinen P, Bruck A, Aalto S, Forsback S, Parkkola R, Rinne JO (2009) Impaired cognitive performance in Parkinson’s disease is related to caudate dopaminergic hypofunction and hippocampal atrophy. Parkinsonism Relat Disord 15:88–93
Noh SW, Han YH, Mun CW, Chung EJ, Kim EG, Ji KH, Seo JH, Kim SJ (2014) Analysis among cognitive profiles and gray matter volume in newly diagnosed Parkinson’s disease with mild cognitive impairment. J Neurol Sci 347:210–213
Camicioli R, Moore MM, Kinney A, Corbridge E, Glassberg K, Kaye JA (2003) Parkinson’s disease is associated with hippocampal atrophy. Mov Disord 18:784–790
Rektorova I, Biundo R, Marecek R, Weis L, Aarsland D, Antonini A (2014) Grey matter changes in cognitively impaired Parkinson’s disease patients. PLoS One 9:e85595
Melzer TR, Watts R, MacAskill MR, Pitcher TL, Livingston L, Keenan RJ, Dalrymple-Alford JC, Anderson TJ (2012) Grey matter atrophy in cognitively impaired Parkinson’s disease. J Neurol Neurosurg Psychiatry 83:188–194
Xia Y, Luo C, Dai S, Yao D (2013) Increased EphA/ephrinA expression in hippocampus of pilocarpine treated mouse. Epilepsy Res 105:20–29
Kandiah N, Zainal NH, Narasimhalu K, Chander RJ, Ng A, Mak E, Au WL, Sitoh YY, Nadkarni N, Tan LC (2014) Hippocampal volume and white matter disease in the prediction of dementia in Parkinson’s disease. Parkinsonism Relat Disord 20:1203–1208
Summerfield C, Junque C, Tolosa E, Salgado-Pineda P, Gomez-Anson B, Marti MJ, Pastor P, Ramirez-Ruiz B, Mercader J (2005) Structural brain changes in Parkinson disease with dementia: a voxel-based morphometry study. Arch Neurol 62:281–285
Wiseman RM, Saxby BK, Burton EJ, Barber R, Ford GA, O’Brien JT (2004) Hippocampal atrophy, whole brain volume, and white matter lesions in older hypertensive subjects. Neurology 63:1892–1897
Burton A (2004) 9th International Conference on AD and related disorders (ICAD). Lancet Neurol 3:510
Barber R, McKeith IG, Ballard C, Gholkar A, O’Brien JT (2001) A comparison of medial and lateral temporal lobe atrophy in dementia with Lewy bodies and Alzheimer’s disease: magnetic resonance imaging volumetric study. Dement Geriatr Cogn Disord 12:198–205
Hashimoto M, Kitagaki H, Imamura T, Hirono N, Shimomura T, Kazui H, Tanimukai S, Hanihara T, Mori E (1998) Medial temporal and whole-brain atrophy in dementia with Lewy bodies: a volumetric MRI study. Neurology 51:357–362
Tagawa R, Hashimoto H, Nakanishi A, Kawarada Y, Muramatsu T, Matsuda Y, Kataoka K, Shimada A, Uchida K, Yoshida A, Higashiyama S, Kawabe J, Kai T, Shiomi S, Mori H, Inoue K (2015) The relationship between medial temporal lobe atrophy and cognitive impairment in patients with dementia with Lewy bodies. J Geriatr Psychiatry Neurol 28:249–254
Sanchez-Castaneda C, Rene R, Ramirez-Ruiz B, Campdelacreu J, Gascon J, Falcon C, Calopa M, Jauma S, Juncadella M, Junque C (2009) Correlations between gray matter reductions and cognitive deficits in dementia with Lewy bodies and Parkinson’s disease with dementia. Mov Disord 24:1740–1746
Brenneis C, Egger K, Scherfler C, Seppi K, Schocke M, Poewe W, Wenning GK (2007) Progression of brain atrophy in multiple system atrophy. A longitudinal VBM study. J Neurol 254:191–196
Messina D, Cerasa A, Condino F, Arabia G, Novellino F, Nicoletti G, Salsone M, Morelli M, Lanza PL, Quattrone A (2011) Patterns of brain atrophy in Parkinson’s disease, progressive supranuclear palsy and multiple system atrophy. Parkinsonism Relat Disord 17:172–176
Shibuya K, Nagatomo H, Iwabuchi K, Inoue M, Yagishita S, Itoh Y (2000) Asymmetrical temporal lobe atrophy with massive neuronal inclusions in multiple system atrophy. J Neurol Sci 179:50–58
Muslimovic D, Post B, Speelman JD, Schmand B (2005) Cognitive profile of patients with newly diagnosed Parkinson disease. Neurology 65:1239–1245
Ramirez-Ruiz B, Junque C, Marti MJ, Valldeoriola F, Tolosa E (2006) Neuropsychological deficits in Parkinson’s disease patients with visual hallucinations. Mov Disord 21:1483–1487
Ozer F, Meral H, Hanoglu L, Ozturk O, Aydemir T, Cetin S, Atmaca B, Tiras R (2007) Cognitive impairment patterns in Parkinson’s disease with visual hallucinations. J Clin Neurosci 14:742–746
Levy RB, Aoki C (2002) Alpha7 nicotinic acetylcholine receptors occur at postsynaptic densities of AMPA receptor-positive and -negative excitatory synapses in rat sensory cortex. J Neurosci 22:5001–5015
Bouchard TP, Malykhin N, Martin WR, Hanstock CC, Emery DJ, Fisher NJ, Camicioli RM (2008) Age and dementia-associated atrophy predominates in the hippocampal head and amygdala in Parkinson’s disease. Neurobiol Aging 29:1027–1039
Junque C, Ramirez-Ruiz B, Tolosa E, Summerfield C, Marti MJ, Pastor P, Gomez-Anson B, Mercader JM (2005) Amygdalar and hippocampal MRI volumetric reductions in Parkinson’s disease with dementia. Mov Disord 20:540–544
Tam CW, Burton EJ, McKeith IG, Burn DJ, O’Brien JT (2005) Temporal lobe atrophy on MRI in Parkinson disease with dementia: a comparison with Alzheimer disease and dementia with Lewy bodies. Neurology 64:861–865
Zarei M, Ibarretxe-Bilbao N, Compta Y, Hough M, Junque C, Bargallo N, Tolosa E, Marti MJ (2013) Cortical thinning is associated with disease stages and dementia in Parkinson’s disease. J Neurol Neurosurg Psychiatry 84:875–881
Mak E, Li S, Williams GB, Watson R, Firbank M, Blamire A, O’Brien J (2016) Differential atrophy of hippocampal subfields: a comparative study of dementia with Lewy bodies and Alzheimer disease. Am J Geriatr Psychiatry 24:136–143
Nedelska Z, Ferman TJ, Boeve BF, Przybelski SA, Lesnick TG, Murray ME, Gunter JL, Senjem ML, Vemuri P, Smith GE, Geda YE, Graff-Radford J, Knopman DS, Petersen RC, Parisi JE, Dickson DW, Jack CR, Kantarci K (2015) Pattern of brain atrophy rates in autopsy-confirmed dementia with Lewy bodies. Neurobiol Aging 36:452–461
Stanzani-Maserati M, Gallassi R, Calandra-Buonaura G, Alessandria M, Oppi F, Poda R, Sambati L, Provini F, Cortelli P (2014) Cognitive and sleep features of multiple system atrophy: review and prospective study. Eur Neurol 72:349–359
Thoma RJ, Monnig M, Hanlon FM, Miller GA, Petropoulos H, Mayer AR, Yeo R, Euler M, Lysne P, Moses SN, Canive JM (2009) Hippocampus volume and episodic memory in schizophrenia. J Int Neuropsychol Soc 15:182–195
Malchow B, Strocka S, Frank F, Bernstein HG, Steiner J, Schneider-Axmann T, Hasan A, Reich-Erkelenz D, Schmitz C, Bogerts B, Falkai P, Schmitt A (2015) Stereological investigation of the posterior hippocampus in affective disorders. J Neural Transm (Vienna) 122:1019–1033
Caetano SC, Hatch JP, Brambilla P, Sassi RB, Nicoletti M, Mallinger AG, Frank E, Kupfer DJ, Keshavan MS, Soares JC (2004) Anatomical MRI study of hippocampus and amygdala in patients with current and remitted major depression. Psychiatry Res 132:141–147
Bremner JD, Narayan M, Anderson ER, Staib LH, Miller HL, Charney DS (2000) Hippocampal volume reduction in major depression. Am J Psychiatry 157:115–118
Sheline YI, Black KJ, Lin DY, Christensen GE, Gado MH, Brunsden BS, Vannier MW (1996) Stereological MRI volumetry of the frontal lobe. Psychiatry Res 67:203–214
Videbech P, Ravnkilde B (2004) Hippocampal volume and depression: a meta-analysis of MRI studies. Am J Psychiatry 161:1957–1966
Campbell S, Marriott M, Nahmias C, MacQueen GM (2004) Lower hippocampal volume in patients suffering from depression: a meta-analysis. Am J Psychiatry 161:598–607
Kao AW, Racine CA, Quitania LC, Kramer JH, Christine CW, Miller BL (2009) Cognitive and neuropsychiatric profile of the synucleinopathies: Parkinson disease, dementia with Lewy bodies, and multiple system atrophy. Alzheimer Dis Assoc Disord 23:365–370
Armstrong RA, Kotzbauer PT, Perlmutter JS, Campbell MC, Hurth KM, Schmidt RE, Cairns NJ (2014) A quantitative study of alpha-synuclein pathology in fifteen cases of dementia associated with Parkinson disease. J Neural Transm 121:171–181
Kempster PA, O’Sullivan SS, Holton JL, Revesz T, Lees AJ (2010) Relationships between age and late progression of Parkinson’s disease: a clinico-pathological study. Brain 133:1755–1762
Apaydin H, Ahlskog JE, Parisi JE, Boeve BF, Dickson DW (2002) Parkinson disease neuropathology: later-developing dementia and loss of the levodopa response. Arch Neurol 59:102–112
Harding AJ, Halliday GM (2001) Cortical Lewy body pathology in the diagnosis of dementia. Acta Neuropathol 102:355–363
Halliday G, Hely M, Reid W, Morris J (2008) The progression of pathology in longitudinally followed patients with Parkinson’s disease. Acta Neuropathol 115:409–415
Halliday G, Lees A, Stern M (2011) Milestones in Parkinson’s disease–clinical and pathologic features. Mov Disord 26:1015–1021
Kovari E, Gold G, Herrmann FR, Canuto A, Hof PR, Bouras C, Giannakopoulos P (2003) Lewy body densities in the entorhinal and anterior cingulate cortex predict cognitive deficits in Parkinson’s disease. Acta Neuropathol 106:83–88
Nishie M, Mori F, Fujiwara H, Hasegawa M, Yoshimoto M, Iwatsubo T, Takahashi H, Wakabayashi K (2004) Accumulation of phosphorylated alpha-synuclein in the brain and peripheral ganglia of patients with multiple system atrophy. Acta Neuropathol 107:292–298
Arnold AE, Protzner AB, Bray S, Levy RM, Iaria G (2014) Neural network configuration and efficiency underlies individual differences in spatial orientation ability. J Cogn Neurosci 26:380–394
Aoki N, Boyer PJ, Lund C, Lin WL, Koga S, Ross OA, Weiner M, Lipton A, Powers JM, White CL, Dickson DW (2015) Atypical multiple system atrophy is a new subtype of frontotemporal lobar degeneration: frontotemporal lobar degeneration associated with alpha-synuclein. Acta Neuropathol 130:93–105
Parkkinen L, Pirttila T, Alafuzoff I (2008) Applicability of current staging/categorization of alpha-synuclein pathology and their clinical relevance. Acta Neuropathol 115:399–407
Parkkinen L, Kauppinen T, Pirttila T, Autere JM, Alafuzoff I (2005) Alpha-synuclein pathology does not predict extrapyramidal symptoms or dementia. Ann. Neurol 57:82–91
Weisman D, Cho M, Taylor C, Adame A, Thal LJ, Hansen LA (2007) In dementia with Lewy bodies, Braak stage determines phenotype, not Lewy body distribution. Neurology 69:356–359
Outeiro TF, Putcha P, Tetzlaff JE, Spoelgen R, Koker M, Carvalho F, Hyman BT, McLean PJ (2008) Formation of toxic oligomeric alpha-synuclein species in living cells. PLoS ONE 3:e1867
Yuan B, Sierks MR (2009) Intracellular targeting and clearance of oligomeric alpha-synuclein alleviates toxicity in mammalian cells. Neurosci Lett 459:16–18
Karpinar DP, Balija MB, Kugler S, Opazo F, Rezaei-Ghaleh N, Wender N, Kim HY, Taschenberger G, Falkenburger BH, Heise H, Kumar A, Riedel D, Fichtner L, Voigt A, Braus GH, Giller K, Becker S, Herzig A, Baldus M, Jackle H, Eimer S, Schulz JB, Griesinger C, Zweckstetter M (2009) Pre-fibrillar alpha-synuclein variants with impaired beta-structure increase neurotoxicity in Parkinson’s disease models. EMBO J 28:3256–3268
Hashimoto M, Kawahara K, Bar-On P, Rockenstein E, Crews L, Masliah E (2004) The Role of alpha-synuclein assembly and metabolism in the pathogenesis of Lewy body disease. J Mol Neurosci 24:343–352
Zhou W, Milder JB, Freed CR (2008) Transgenic mice overexpressing tyrosine-to-cysteine mutant human alpha-synuclein: a progressive neurodegenerative model of diffuse Lewy body disease. J Biol Chem 283:9863–9870
Paleologou KE, Kragh CL, Mann DM, Salem SA, Al-Shami R, Allsop D, Hassan AH, Jensen PH, El-Agnaf OM (2009) Detection of elevated levels of soluble alpha-synuclein oligomers in post-mortem brain extracts from patients with dementia with Lewy bodies. Brain 132:1093–1101
Tong J, Wong H, Guttman M, Ang LC, Forno LS, Shimadzu M, Rajput AH, Muenter MD, Kish SJ, Hornykiewicz O, Furukawa Y (2010) Brain alpha-synuclein accumulation in multiple system atrophy, Parkinson’s disease and progressive supranuclear palsy: a comparative investigation. Brain 133:172–188
Choi JH, Stubblefield B, Cookson MR, Goldin E, Velayati A, Tayebi N, Sidransky E (2011) Aggregation of alpha-synuclein in brain samples from subjects with glucocerebrosidase mutations. Mol Genet Metab 104:185–188
Sharon R, Bar-Joseph I, Frosch MP, Walsh DM, Hamilton JA, Selkoe DJ (2003) The formation of highly soluble oligomers of alpha-synuclein is regulated by fatty acids and enhanced in Parkinson’s disease. Neuron 37:583–595
Tanji K, Mori F, Mimura J, Itoh K, Kakita A, Takahashi H, Wakabayashi K (2010) Proteinase K-resistant alpha-synuclein is deposited in presynapses in human Lewy body disease and A53T alpha-synuclein transgenic mice. Acta Neuropathol 120:145–154
Dettmer U, Newman AJ, Soldner F, Luth ES, Kim NC, von Saucken VE, Sanderson JB, Jaenisch R, Bartels T, Selkoe D (2015) Parkinson-causing alpha-synuclein missense mutations shift native tetramers to monomers as a mechanism for disease initiation. Nat Commun 6:7314
Schulz-Schaeffer WJ (2010) The synaptic pathology of alpha-synuclein aggregation in dementia with Lewy bodies, Parkinson’s disease and Parkinson’s disease dementia. Acta Neuropathol 120:131–143
Duda JE (2004) Pathology and neurotransmitter abnormalities of dementia with Lewy bodies. Dement Geriatr Cogn Disord 17(Suppl 1):3–14
Howlett DR, Whitfield D, Johnson M, Attems J, O’Brien JT, Aarsland D, Lai MK, Lee JH, Chen C, Ballard C, Hortobagyi T, Francis PT (2015) Regional multiple pathology scores are associated with cognitive decline in Lewy body dementias. Brain Pathol 25:401–408
Schultz C, Engelhardt M (2014) Anatomy of the hippocampal formation. Front Neurol Neurosci 34:6–17
Buddhala C, Loftin SK, Kuley BM, Cairns NJ, Campbell MC, Perlmutter JS, Kotzbauer PT (2015) Dopaminergic, serotonergic, and noradrenergic deficits in Parkinson disease. Ann Clin Transl Neurol 2:949–959
Halliday GM, Leverenz JB, Schneider JS, Adler CH (2014) The neurobiological basis of cognitive impairment in Parkinson’s disease. Mov Disord 29:634–650
Nemani VM, Lu W, Berge V, Nakamura K, Onoa B, Lee MK, Chaudhry FA, Nicoll RA, Edwards RH (2010) Increased expression of alpha-synuclein reduces neurotransmitter release by inhibiting synaptic vesicle reclustering after endocytosis. Neuron 65:66–79
Wang L, Das U, Scott DA, Tang Y, McLean PJ, Roy S (2014) alpha-synuclein multimers cluster synaptic vesicles and attenuate recycling. Curr Biol 24:2319–2326
Scott D, Roy S (2012) alpha-Synuclein inhibits intersynaptic vesicle mobility and maintains recycling-pool homeostasis. J Neurosci 32:10129–10135
Burre J, Sharma M, Tsetsenis T, Buchman V, Etherton MR, Sudhof TC (2010) Alpha-synuclein promotes SNARE-complex assembly in vivo and in vitro. Science 329:1663–1667
Rizo J, Xu J (2015) The synaptic vesicle release machinery. Annu Rev Biophys 44:339–367
Nikolaus S, Antke C, Muller HW (2009) In vivo imaging of synaptic function in the central nervous system: I. Movement disorders and dementia. Behav Brain Res 204:1–31
Diogenes MJ, Dias RB, Rombo DM, Vicente MH, Maiolino F, Guerreiro P, Nasstrom T, Franquelim HG, Oliveira LM, Castanho MA, Lannfelt L, Bergstrom J, Ingelsson M, Quintas A, Sebastiao AM, Lopes LV, Outeiro TF (2012) Extracellular alpha-synuclein oligomers modulate synaptic transmission and impair LTP via NMDA-receptor activation. J Neurosci 32:11750–11762
Martin ZS, Neugebauer V, Dineley KT, Kayed R, Zhang W, Reese LC, Taglialatela G (2012) alpha-Synuclein oligomers oppose long-term potentiation and impair memory through a calcineurin-dependent mechanism: relevance to human synucleopathic diseases. J Neurochem 120:440–452
Chen Y, Yang W, Li X, Li X, Yang H, Xu Z, Yu S (2015) Alpha-Synuclein-induced internalization of NMDA receptors in hippocampal neurons is associated with reduced inward current and Ca(2+) influx upon NMDA stimulation. Neuroscience 300:297–306
Cheng F, Li X, Li Y, Wang C, Wang T, Liu G, Baskys A, Ueda K, Chan P, Yu S (2011) Alpha-Synuclein promotes clathrin-mediated NMDA receptor endocytosis and attenuates NMDA-induced dopaminergic cell death. J Neurochem 119:815–825
Costa C, Sgobio C, Siliquini S, Tozzi A, Tantucci M, Ghiglieri V, Di FM, Pendolino V, de Iure A, Marti M, Morari M, Spillantini MG, Latagliata EC, Pascucci T, Puglisi-Allegra S, Gardoni F, Di LM, Picconi B, Calabresi P (2012) Mechanisms underlying the impairment of hippocampal long-term potentiation and memory in experimental Parkinson’s disease. Brain 135:1884–1899
Revuelta GJ, Rosso A, Lippa CF (2008) Neuritic pathology as a correlate of synaptic loss in dementia with lewy bodies. Am J Alzheimers Dis Other Demen 23:97–102
Masliah E, Mallory M, DeTeresa R, Alford M, Hansen L (1993) Differing patterns of aberrant neuronal sprouting in Alzheimer’s disease with and without Lewy bodies. Brain Res 617:258–266
Lim Y, Kehm VM, Lee EB, Soper JH, Li C, Trojanowski JQ, Lee VM (2011) Alpha-Syn suppression reverses synaptic and memory defects in a mouse model of dementia with Lewy bodies. J Neurosci 31:10076–10087
Kramer ML, Schulz-Schaeffer WJ (2007) Presynaptic alpha-synuclein aggregates, not Lewy bodies, cause neurodegeneration in dementia with Lewy bodies. J Neurosci 27:1405–1410
Neumann M, Kahle PJ, Giasson BI, Ozmen L, Borroni E, Spooren W, Muller V, Odoy S, Fujiwara H, Hasegawa M, Iwatsubo T, Trojanowski JQ, Kretzschmar HA, Haass C (2002) Misfolded proteinase K-resistant hyperphosphorylated alpha-synuclein in aged transgenic mice with locomotor deterioration and in human alpha-synucleinopathies. J Clin Invest 110:1429–1439
Tsigelny IF, Sharikov Y, Wrasidlo W, Gonzalez T, Desplats PA, Crews L, Spencer B, Masliah E (2012) Role of alpha-synuclein penetration into the membrane in the mechanisms of oligomer pore formation. FEBS J 279:1000–1013
Pacheco CR, Morales CN, Ramirez AE, Munoz FJ, Gallegos SS, Caviedes PA, Aguayo LG, Opazo CM (2015) Extracellular alpha-synuclein alters synaptic transmission in brain neurons by perforating the neuronal plasma membrane. J Neurochem 132:731–741
Ouberai MM, Wang J, Swann MJ, Galvagnion C, Guilliams T, Dobson CM, Welland ME (2013) Alpha-Synuclein senses lipid packing defects and induces lateral expansion of lipids leading to membrane remodeling. J Biol Chem 288:20883–20895
Stockl MT, Zijlstra N, Subramaniam V (2013) Alpha-Synuclein oligomers: an amyloid pore? Insights into mechanisms of alpha-synuclein oligomer-lipid interactions. Mol Neurobiol 47:613–621
Shi Z, Sachs JN, Rhoades E, Baumgart T (2015) Biophysics of alpha-synuclein induced membrane remodelling. Phys Chem Chem Phys 17:15561–15568
Angelova PR, Abramov AY (2016) Alpha-synuclein and beta-amyloid–different targets, same players: calcium, free radicals and mitochondria in the mechanism of neurodegeneration. Biochem Biophys Res Commun. doi:10.1016/j.bbrc.2016.07.103 (online available)
Scott DA, Tabarean I, Tang Y, Cartier A, Masliah E, Roy S (2010) A pathologic cascade leading to synaptic dysfunction in alpha-synuclein-induced neurodegeneration. J Neurosci 30:8083–8095
Chung CY, Koprich JB, Siddiqi H, Isacson O (2009) Dynamic changes in presynaptic and axonal transport proteins combined with striatal neuroinflammation precede dopaminergic neuronal loss in a rat model of AAV alpha-synucleinopathy. J Neurosci 29:3365–3373
Volpicelli-Daley LA, Luk KC, Patel TP, Tanik SA, Riddle DM, Stieber A, Meaney DF, Trojanowski JQ, Lee VM (2011) Exogenous alpha-synuclein fibrils induce Lewy body pathology leading to synaptic dysfunction and neuron death. Neuron 72:57–71
Yu S, Chan P (2014) Role of alpha-synuclein in neurodegeneration: implications for the pathogenesis of Parkinson’s disease. Essays Biochem 56:125–135
Mattison HA, Popovkina D, Kao JP, Thompson SM (2014) The role of glutamate in the morphological and physiological development of dendritic spines. Eur J Neurosci 39:1761–1770
Smith Y, Villalba RM, Raju DV (2009) Striatal spine plasticity in Parkinson’s disease: pathological or not? Parkinsonism Relat Disord 15(Suppl 3):S156–S161
Lisman JE, Grace AA (2005) The hippocampal-VTA loop: controlling the entry of information into long-term memory. Neuron 46:703–713
Lemon N, Manahan-Vaughan D (2006) Dopamine D1/D5 receptors gate the acquisition of novel information through hippocampal long-term potentiation and long-term depression. J Neurosci 26:7723–7729
Wiescholleck V, Manahan-Vaughan D (2014) Antagonism of D1/D5 receptors prevents long-term depression (LTD) and learning-facilitated LTD at the perforant path-dentate gyrus synapse in freely behaving rats. Hippocampus 24:1615–1622
Reyes S, Cottam V, Kirik D, Double KL, Halliday GM (2013) Variability in neuronal expression of dopamine receptors and transporters in the substantia nigra. Mov Disord 28:1351–1359
McRitchie DA, Cartwright HR, Halliday GM (1997) Specific A10 dopaminergic nuclei in the midbrain degenerate in Parkinson’s disease. Exp Neurol 144:202–213
Ito K, Nagano-Saito A, Kato T, Arahata Y, Nakamura A, Kawasumi Y, Hatano K, Abe Y, Yamada T, Kachi T, Brooks DJ (2002) Striatal and extrastriatal dysfunction in Parkinson’s disease with dementia: a 6-[18F]fluoro-L-dopa PET study. Brain 125:1358–1365
Buddhala C, Loftin SK, Kuley BM, Cairns NJ, Campbell MC, Perlmutter JS, Kotzbauer PT (2015) Dopaminergic, serotonergic, and noradrenergic deficits in Parkinson disease. Ann Clin Transl Neurol 2:949–959
Kohl Z, Ben AN, Vogelgsang J, Tischer L, Deusser J, Amato D, Anderson S, Muller CP, Riess O, Masliah E, Nuber S, Winkler J (2016) Severely impaired hippocampal neurogenesis associates with an early serotonergic deficit in a BAC alpha-synuclein transgenic rat model of Parkinson’s disease. Neurobiol Dis 85:206–217
Ballanger B, Klinger H, Eche J, Lerond J, Vallet AE, Le BD, Tremblay L, Sgambato-Faure V, Broussolle E, Thobois S (2012) Role of serotonergic 1A receptor dysfunction in depression associated with Parkinson’s disease. Mov Disord 27:84–89
Ballanger B, Poisson A, Broussolle E, Thobois S (2012) Functional imaging of non-motor signs in Parkinson’s disease. J Neurol Sci 315:9–14
Sotiriou E, Vassilatis DK, Vila M, Stefanis L (2010) Selective noradrenergic vulnerability in alpha-synuclein transgenic mice. Neurobiol Aging 31:2103–2114
Wersinger C, Jeannotte A, Sidhu A (2006) Attenuation of the norepinephrine transporter activity and trafficking via interactions with alpha-synuclein. Eur J Neurosci 24:3141–3152
Lopez-Virgen V, Zarate-Lopez D, Adirsch FL, Collas-Aguilar J, Gonzalez-Perez O (2015) Effects of sleep deprivation in hippocampal neurogenesis. Gac Med Mex 151:99–104
Ernst A, Frisen J (2015) Adult neurogenesis in humans- common and unique traits in mammals. PLoS Biol 13:e1002045
Yu DX, Marchetto MC, Gage FH (2014) How to make a hippocampal dentate gyrus granule neuron. Development 141:2366–2375
Oomen CA, Bekinschtein P, Kent BA, Saksida LM, Bussey TJ (2014) Adult hippocampal neurogenesis and its role in cognition. Wiley Interdiscip Rev Cogn Sci 5:573–587
Boldrini M, Underwood MD, Hen R, Rosoklija GB, Dwork AJ, John MJ, Arango V (2009) Antidepressants increase neural progenitor cells in the human hippocampus. Neuropsychopharmacology 34:2376–2389
Jun H, Mohammed Qasim HS, Rigby MJ, Jang MH (2012) Functional role of adult hippocampal neurogenesis as a therapeutic strategy for mental disorders. Neural Plast 2012:854285
Elder GA, De GR, Gama Sosa MA (2006) Research update: neurogenesis in adult brain and neuropsychiatric disorders. Mt Sinai J Med 73:931–940
Kempermann G, Krebs J, Fabel K (2008) The contribution of failing adult hippocampal neurogenesis to psychiatric disorders. Curr Opin Psychiatry 21:290–295
Hoglinger GU, Rizk P, Muriel MP, Duyckaerts C, Oertel WH, Caille I, Hirsch EC (2004) Dopamine depletion impairs precursor cell proliferation in Parkinson disease. Nat Neurosci 7:726–735
Johnson M, Ekonomou A, Hobbs C, Ballard CG, Perry RH, Perry EK (2011) Neurogenic marker abnormalities in the hippocampus in dementia with Lewy bodies. Hippocampus 21:1126–1136
Park JH, Enikolopov G (2010) Transient elevation of adult hippocampal neurogenesis after dopamine depletion. Exp Neurol 222:267–276
Suzuki K, Okada K, Wakuda T, Shinmura C, Kameno Y, Iwata K, Takahashi T, Suda S, Matsuzaki H, Iwata Y, Hashimoto K, Mori N (2010) Destruction of dopaminergic neurons in the midbrain by 6-hydroxydopamine decreases hippocampal cell proliferation in rats: reversal by fluoxetine. PLoS One 5:e9260
Kohl Z, Winner B, Ubhi K, Rockenstein E, Mante M, Munch M, Barlow C, Carter T, Masliah E, Winkler J (2012) Fluoxetine rescues impaired hippocampal neurogenesis in a transgenic A53T synuclein mouse model. Eur J Neurosci 35:10–19
Winner B, Lie DC, Rockenstein E, Aigner R, Aigner L, Masliah E, Kuhn HG, Winkler J (2004) Human wild-type alpha-synuclein impairs neurogenesis. J Neuropathol Exp Neurol 63:1155–1166
Winner B, Rockenstein E, Lie DC, Aigner R, Mante M, Bogdahn U, Couillard-Despres S, Masliah E, Winkler J (2008) Mutant alpha-synuclein exacerbates age-related decrease of neurogenesis. Neurobiol Aging 29:913–925
Horgusluoglu E, Nudelman K, Nho K, Saykin AJ (2016) Adult neurogenesis and neurodegenerative diseases: A systems biology perspective. Am J Med Genet B Neuropsychiatr Genet. doi:10.1002/ajmg.b.32429 (online available)
Marxreiter F, Nuber S, Kandasamy M, Klucken J, Aigner R, Burgmayer R, Couillard-Despres S, Riess O, Winkler J, Winner B (2009) Changes in adult olfactory bulb neurogenesis in mice expressing the A30P mutant form of alpha-synuclein. Eur J Neurosci 29:879–890
Marxreiter F, Ettle B, May VE, Esmer H, Patrick C, Kragh CL, Klucken J, Winner B, Riess O, Winkler J, Masliah E, Nuber S (2013) Glial A30P alpha-synuclein pathology segregates neurogenesis from anxiety-related behavior in conditional transgenic mice. Neurobiol Dis 59:38–51
Oliveira LM, Falomir-Lockhart LJ, Botelho MG, Lin KH, Wales P, Koch JC, Gerhardt E, Taschenberger H, Outeiro TF, Lingor P, Schule B, Arndt-Jovin DJ, Jovin TM (2015) Elevated alpha-synuclein caused by SNCA gene triplication impairs neuronal differentiation and maturation in Parkinson’s patient-derived induced pluripotent stem cells. Cell Death Dis 6:e1994
Thenganatt MA, Jankovic J (2014) Parkinson disease subtypes. JAMA Neurol 71:499–504
Schrag A, Sauerbier A, Chaudhuri KR (2015) New clinical trials for nonmotor manifestations of Parkinson’s disease. Mov Disord 30:1490–1504
Weintraub D, Simuni T, Caspell-Garcia C, Coffey C, Lasch S, Siderowf A, Aarsland D, Barone P, Burn D, Chahine LM, Eberling J, Espay AJ, Foster ED, Leverenz JB, Litvan I, Richard I, Troyer MD, Hawkins KA (2015) Cognitive performance and neuropsychiatric symptoms in early, untreated Parkinson’s disease. Mov Disord 30:919–927
Williams-Gray CH, Evans JR, Goris A, Foltynie T, Ban M, Robbins TW, Brayne C, Kolachana BS, Weinberger DR, Sawcer SJ, Barker RA (2009) The distinct cognitive syndromes of Parkinson’s disease: 5 year follow-up of the CamPaIGN cohort. Brain 132:2958–2969
Dujardin K, Langlois C, Plomhause L, Carette AS, Delliaux M, Duhamel A, Defebvre L (2014) Apathy in untreated early-stage Parkinson disease: relationship with other non-motor symptoms. Mov Disord 29:1796–1801
Brown RG, Landau S, Hindle JV, Playfer J, Samuel M, Wilson KC, Hurt CS, Anderson RJ, Carnell J, Dickinson L, Gibson G, van Schaick R, Sellwood K, Thomas BA, Burn DJ (2011) Depression and anxiety related subtypes in Parkinson’s disease. J Neurol Neurosurg Psychiatry 82:803–809
Burn DJ, Landau S, Hindle JV, Samuel M, Wilson KC, Hurt CS, Brown RG (2012) Parkinson’s disease motor subtypes and mood. Mov Disord 27:379–386
Romenets SR, Gagnon JF, Latreille V, Panniset M, Chouinard S, Montplaisir J, Postuma RB (2012) Rapid eye movement sleep behavior disorder and subtypes of Parkinson’s disease. Mov Disord 27:996–1003
Yoritaka A, Ohizumi H, Tanaka S, Hattori N (2009) Parkinson’s disease with and without REM sleep behaviour disorder: are there any clinical differences? Eur Neurol 61:164–170
Quinn NP, Koller WC, Lang AE, Marsden CD (1986) Painful Parkinson’s disease. Lancet 1:1366–1369
Wallace VC, Chaudhuri KR (2014) Unexplained lower limb pain in Parkinson’s disease: a phenotypic variant of “painful Parkinson’s disease”. Parkinsonism Relat Disord 20:122–124
Sharma JC, Turton J (2012) Olfaction, dyskinesia and profile of weight change in Parkinson’s disease: identifying neurodegenerative phenotypes. Parkinsonism Relat Disord 18:964–970
Sharma JC, Vassallo M (2014) Prognostic significance of weight changes in Parkinson’s disease: the park-weight phenotype. Neurodegener Dis Manag 4:309–316
McKeith IG, Burn DJ, Ballard CG, Collerton D, Jaros E, Morris CM, McLaren A, Perry EK, Perry R, Piggott MA, O’Brien JT (2003) Dementia with Lewy bodies. Semin Clin Neuropsychiatry 8:46–57
Clark LN, Kartsaklis LA, Wolf GR, Dorado B, Ross BM, Kisselev S, Verbitsky M, Mejia-Santana H, Cote LJ, Andrews H, Vonsattel JP, Fahn S, Mayeux R, Honig LS, Marder K (2009) Association of glucocerebrosidase mutations with dementia with lewy bodies. Arch Neurol 66:578–583
Nelson PT, Schmitt FA, Jicha GA, Kryscio RJ, Abner EL, Smith CD, Van Eldik LJ, Markesbery WR (2010) Association between male gender and cortical Lewy body pathology in large autopsy series. J Neurol 257:1875–1881
Lopez OL, Becker JT, Sweet RA, Martin-Sanchez FJ, Hamilton RL (2006) Lewy bodies in the amygdala increase risk for major depression in subjects with Alzheimer disease. Neurology 67:660–665
Mak E, Su L, Williams GB, O’Brien JT (2014) Neuroimaging characteristics of dementia with Lewy bodies. Alzheimers Res Ther 6:18
Geser F, Wenning GK, Seppi K, Stampfer-Kountchev M, Scherfler C, Sawires M, Frick C, Ndayisaba JP, Ulmer H, Pellecchia MT, Barone P, Kim HT, Hooker J, Quinn NP, Cardozo A, Tolosa E, Abele M, Klockgether T, Ostergaard K, Dupont E, Schimke N, Eggert KM, Oertel W, Djaldetti R, Poewe W (2006) Progression of multiple system atrophy (MSA): a prospective natural history study by the European MSA Study Group (EMSA SG). Mov Disord 21:179–186
Wenning GK, Stefanova N (2009) Recent developments in multiple system atrophy. J Neurol 256:1791–1808
Brown RG, Lacomblez L, Landwehrmeyer BG, Bak T, Uttner I, Dubois B, Agid Y, Ludolph A, Bensimon G, Payan C, Leigh NP (2010) Cognitive impairment in patients with multiple system atrophy and progressive supranuclear palsy. Brain 133:2382–2393
Kawai Y, Suenaga M, Takeda A, Ito M, Watanabe H, Tanaka F, Kato K, Fukatsu H, Naganawa S, Kato T, Ito K, Sobue G (2008) Cognitive impairments in multiple system atrophy: MSA-C vs MSA-P. Neurology 70:1390–1396
Wenning GK, Tison F, Ben SY, Daniel SE, Quinn NP (1997) Multiple system atrophy: a review of 203 pathologically proven cases. Mov Disord 12:133–147
Ozawa T (2007) Morphological substrate of autonomic failure and neurohormonal dysfunction in multiple system atrophy: impact on determining phenotype spectrum. Acta Neuropathol 114:201–211
Acknowledgements
The authors are supported by Grants from the National Basic Research Program (“973” Program) of China (2011CB504101), the Natural Science Foundation of China (81371200, 81071014, 81401042), the National Science and Technology Support Program (2012BAI10B03) and Special Scientific Research Funds for Capital Health Development (2011-1001-01), Natural Science Foundation of Beijing (7122035).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, W., Yu, S. Synucleinopathies: common features and hippocampal manifestations. Cell. Mol. Life Sci. 74, 1485–1501 (2017). https://doi.org/10.1007/s00018-016-2411-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-016-2411-y