Abstract
Abnormally modified α-synuclein is a pathological hallmark of Parkinson’s disease and the other α-synucleinopathies. Since proteinase K (PK) treatment is known to enhance the immunoreactivity of abnormal α-synuclein, we immunohistochemically examined the brain of transgenic (Tg) mice expressing human mutant A53T α-synuclein using this retrieval method. PK treatment abolished the immunoreactivity of α-synuclein in abnormal inclusions as well as of endogenous α-synuclein in Tg mice, whereas PK-resistant α-synuclein was found in the presynaptic nerve terminals, especially in the hippocampus and temporal cortex. In human Lewy body disease, PK-resistant α-synuclein was deposited in Lewy bodies and Lewy neurites, as well as in the presynapses in distinct brain regions, including the hippocampus, temporal cortex and substantia nigra. Biochemical analysis revealed that PK-resistant α-synuclein was detected in the presynaptic fraction in Tg mice and human Lewy body disease. Although PK-resistant α-synuclein was found in the presynapse in Tg mice even at 1 week of age, it was not phosphorylated until at least 8 months of age. Moreover, PK-resistant α-synuclein in the presynapse was not phosphorylated in human Lewy body disease. These findings suggest that phosphorylation is not necessary to cause the conversion of soluble form to PK-resistant α-synuclein. Considering that native α-synuclein is a soluble protein localized to the presynaptic terminals, our findings suggest that PK-resistant α-synuclein may disturb the neurotransmission in α-synucleinopathies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
α-Synuclein is a soluble protein abundantly expressed throughout the brain, especially enriched in the presynaptic nerve terminals [11, 22]. Although physiological functions of α-synuclein remain undefined, mounting evidences suggest that α-synuclein plays a role in modulation of synaptic vesicle pools of various neurotransmitters such as dopamine and glutamate [1, 20, 38, 39].
α-Synucleinopathies comprise a group of neurodegenerative disorders that share abnormal α-synuclein in selected vulnerable neurons and glial cells. Abnormal α-synuclein is accumulated and fibrillated in the neuronal cytoplasm and processes as Lewy bodies and Lewy neurites, respectively, in the brain of patients with Parkinson’s disease (PD) and dementia with Lewy bodies (DLB) [17, 30, 40], as well as in glial cytoplasmic inclusions in multiple system atrophy (MSA) [37]. These aggregates consist of insoluble and polymerized α-synuclein, which are modified by phosphorylation, ubiquitination and nitration [6, 8, 10]. Importantly, immunoreactivity of abnormal α-synuclein is enhanced by pretreatment with proteinase K (PK) [33, 34], suggesting that fibrillization, modifications and proteinase resistance of α-synuclein are implicated in the pathogenesis of α-synucleinopathies.
Transgenic (Tg) α-synucleinopathy rodent models have been generated under several different promoters such as Thy-1, prion, tyrosine hydroxylase and platelet-derived growth factor [9, 14, 19, 23, 24, 31, 32, 36]. These experiments have demonstrated that both wild-type and mutant α-synucleins have potential to form abnormal inclusions resembling Lewy bodies. In particular, Tg mice expressing human mutant A53T α-synuclein under prion promoter (SNCA Tg mice) developed a severe and complex motor impairment, leading to paralysis and death, and pathologically showed Lewy body-like inclusions [9, 19].
In the present study, we performed immunohistochemical and biochemical analyses of SNCA Tg mice using anti-α-synuclein antibodies with PK treatment. Unexpectedly, we found that PK treatment abolished immunoreactivity of α-synuclein in abnormal inclusions as well as of endogenous α-synuclein in SNCA Tg mice. Instead, PK-resistant α-synuclein was deposited in the presynaptic nerve terminals in Tg mice. Furthermore, PK-resistant α-synuclein was present in presynaptic terminals in PD and DLB and, to a lesser extent, in MSA, but not in control subjects. These findings suggest that PK-resistant α-synuclein may disturb the neurotransmission in α-synucleinopathies.
Materials and methods
Animals
Tg mice expressing human mutant A53T α-synuclein protein under the control of the prion promoter (Jackson Laboratories, Bar Harbor, ME) [9] and their wild-type littermates were used in this study. Animals were handled and killed in compliance with institutional and national regulations and policies. The protocol was approved by the Institutional Animal Care and Use Committee at Hirosaki University Graduate School of Medicine, Japan. Tg and control mice were transcardially perfused with phosphate-buffered saline and the brain and spinal cord were removed and fixed with 4% paraformaldehyde for 48 h or 2 weeks. Tissues were dehydrated through a graded ethanol series, embedded in paraffin and cut into 4-μm thick sections.
Subjects
Twenty-seven post-mortem cases were utilized for immunohistochemical analysis in the present study: Lewy body disease (n = 17), MSA (n = 5) and normal control subjects (n = 5). Seventeen patients had Braak PD stages between II and VI (three were stage II; four were stage III; three were stage IV; three were stage V; and four were stage VI) [3]. The severity of the concomitant Alzheimer-related neurofibrillary pathology did not go beyond that regularly encountered in stages I–III in all the cases. Tissues were fixed with 10% buffered formalin for 2 weeks and embedded in paraffin. Serial 4-μm sections were cut from block samples of the following areas in each case: frontal and temporal cortices, amygdala, hippocampus, basal ganglia, thalamus, midbrain, pons, medulla oblongata and cerebellum.
For biochemical analysis, frozen brain tissues (middle temporal cortex) from patients with DLB (Braak PD stage VI; n = 3) and age-matched control subjects (n = 3) were obtained from Brain Research Institute, University of Niigata, Japan. Human brain tissues were dissected at autopsy and frozen rapidly at −70°C.
Immunohistochemistry
Immunohistochemical analysis was carried out using the above paraffin-embedded sections. The sections were pretreated with PK (Gibco BRL, Gaithersburg, MD; 50 μg/ml) in PK buffer containing 10 mM Tris–HCl, pH 7.8, 100 mM NaCl, 0.1% Nonidet-P40 at 37°C for 30 min in mouse section or for 10 min in human section. The sections were then subjected to immunohistochemical processing using the avidin–biotin–peroxidase complex method with diaminobenzidine. Monoclonal antibodies against phosphorylated α-synuclein (pSyn#64; WAKO, Osaka, Japan; 1:5000) [6], human α-synuclein (LB509; Zymed, South San Francisco, CA; 1:1000) [13] and synaptophysin (SY-38; Boehringer Mannheim, Mannheim, Germany; 1:1000) and a polyclonal antibody against α-synuclein (NACP6; 1:2000) [29] were used. The immunolabeled sections were counterstained with hematoxylin.
Cell culture, transfection and protein samples
Human embryonic kidney (HEK) 293T cells were maintained in Dulbecco’s modified Eagle’s medium supplemented with 10% fetal calf serum and antibiotics. Human α-synuclein cDNA was amplified from human fetal brain cDNA library using polymerase chain reaction. Following DNA sequencing, it was subcloned into the pcDNA3 vector (Invitogen, Carlsbad, CA) tagged with RGSHHHHHH at C terminus. A plasmid was transfected into HEK293T cells using Fugene 6 (BD Biosciences, San Jose, CA). α-Synuclein-RH was precipitated by TALON-beads system as previously described [35]. Samples from human and mouse brains were weighed and homogenized with 20 volumes of sample treatment solution containing 4% sodium dodecyl sulfate (SDS).
Western blot analysis
After SDS-polyacrylamide gel electrophoresis, Western blot analysis was performed as previously described [41]. Transfer and detection were carried out according to the protocol provided with the ECL detection system (Amersham Pharmacia Biotech, Piscataway, NJ). In addition to the antibodies used for immunohistochemistry, a monoclonal antibody against synaptosomal-associated protein of 25 kDa (SNAP25; Millipore, Bedford, MA; 1:2,000) was used. Horseradish peroxidase-conjugated anti-mouse IgG or anti-rabbit IgG (Santa Cruz Biotechnology, Santa Cruz, CA) was used as a secondary antibody.
Sucrose gradient analysis
We modified the sucrose gradient method described previously [12, 15]. Briefly, the temporal cortex (0.5 g) from DLB and age-matched control subjects was homogenized in Tris-based buffer (TBS; Tris–HCl, pH 7.5, 150 mM NaCl) containing 3 mM CaCl2, 1 mM EDTA, 1 mM EGTA by a Dounce homogenizer for 12 strokes and was adjusted to a final concentration of 1.0 M sucrose by the addition of 2.2 M sucrose solution. The samples were homogenized again by more eight strokes. Tissue homogenates were layered on a linear sucrose gradient (1.2–2.2 M) and centrifuged at 160,000×g for 2 h at 4°C using a S40T swing rotor (Himac CP-56, Hitachi, Japan). After centrifugation, 0.5 ml of each fraction of the gradient was collected from the bottom.
Filter-trap analysis
For detection of PK-resistant α-synuclein, we modified filter-trap analysis previously described [35]. Briefly, each fraction of sucrose gradient analysis was subjected to digestion with DNase I (10 μm/ml) (Applichem, Darmstadt, Germany) in TBS for 15 min at 37°C, and lysed in PK buffer with PK (10 μg/ml) at room temperature for 10 min. The samples were immediately applied to a 0.22 μm cellulose acetate membrane (Millipore) on a slot blot apparatus (Bio-Rad, Hercules, CA) using a vacuum manifold. After washing with TBS containing 0.1% tween-20, the membrane was removed and incubated with LB509 or NACP6. Detection was carried out by the ECL detection system described above.
Results
Specificity of the primary antibodies
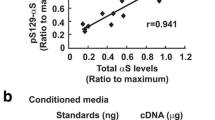
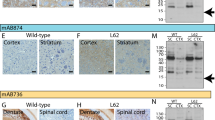
We used three primary antibodies against α-synuclein: NACP6, LB509 and pSyn#64. NACP6 is a polyclonal antibody raised against full-length human α-synuclein and specifically recognizes α-synuclein, but not β-synuclein [29]. As shown in Fig. 1, NACP6 reacted with both human and mouse α-synuclein. LB509 reacted with human α-synuclein, but not with mouse α-synuclein, as reported previously [13] (Fig. 1). pSyn#64 is known to specifically recognize α-synuclein phosphorylated at Serine 129 [6].
Specificity of anti-α-synuclein antibodies. Recombinant human α-synuclein is recognized with LB509 and NACP6 (lane 1). LB509 detects α-synuclein in the lysate from normal human brain (lane 2) and Tg mouse expressing human mutant A53T α-synuclein (lane 4), but not normal mouse α-synuclein (lane 3). NACP6 recognizes both human and mouse α-synucleins (lanes 2–4)
Distribution of PK-resistant α-synuclein in Tg mice
NACP6 immunostained the neuropil throughout the brain in both control and Tg mice at 12 weeks of age (Fig. 2a–d). Consistent with previous studies [9], α-synuclein-immunoreactive inclusions observed in Tg mice were immunolabeled with pSyn#64 (Fig. 2e, f).
α-Synuclein immunoreactivity in control (a, c, e) and Tg mice (b, d, f). NACP6 immunolabels the gray matter throughout the brain of control (a) and Tg mice (b). The cerebral cortex showing diffuse neuropil staining in control (c) and Tg mice (d). The thalamus showing no abnormality in control mice (e) and phosphorylated α-synuclein-positive inclusions in Tg mice (f). a–d NACP6, e, f pSyn#64. Bars 1 mm in a, b, 20 μm in c–f
Since PK is used for the enhancement of immunostaining of abnormal α-synuclein [25–27, 33, 34], we applied PK treatment to the mouse brain fixed for 48 h or 2 weeks. Immunoreactivity of endogenous α-synuclein in the neuropil was almost completely disappeared in control mice by this treatment (Fig. 3a, c), whereas NACP6 immunoreactivity was relatively preserved in Tg mice (Fig. 3b, d). Interestingly, PK-resistant α-synuclein in the neuropil was not phosphorylated (Fig. 3e, f) and NACP6- and pSyn#64-positive inclusions were disappeared after PK treatment (Fig. 3g, h). Similarly, LB509 immunohistochemistry showed that PK-resistant α-synuclein was deposited in the neuropil of Tg mice, but not in controls (Fig. 3i–l). These findings suggest that human α-synuclein is over-expressed in the neuropil in Tg mice and is, at least in part, PK-resistant.
The effect of proteinase K (PK) treatment on α-synuclein immunoreactivity. PK treatment for 30 min diminishes neuropil staining in control mice (a), whereas PK-resistant α-synuclein is detected in Tg mice (b). Boxed areas in a and b are shown at higher magnification in c and d, respectively. The hippocampus showing PK-resistant α-synuclein in Tg mice (d), but not in control (c). PK-resistant α-synuclein in the hippocampus is not phosphorylated in control (e) and Tg mice (f). pSyn#64-positive inclusions are not found in control (g) and Tg mice (h) after PK treatment. PK treatment for 30 min diminishes neuropil staining in the control hippocampus (i, k), whereas PK-resistant α-synuclein is detected in Tg mice (j, l). Boxed areas in i and j are shown at higher magnification in k and l, respectively. a–d NACP6, e–h pSyn#64, i–l LB509. Bars 1 mm in a, b, i, j, 20 μm in c–h, k, l
Since PK-resistant α-synuclein-immunoreactive structures were seen as fine granular or dot-like structures around the neuronal cytoplasm and proximal dendrites (Fig. 3d, l), we used an antibody against synaptophysin, a marker of presynaptic nerve terminals. As shown in Fig. 4, immunohistochemical localization of PK-resistant α-synuclein was identical to that of synaptophysin, suggesting that PK-resistant α-synuclein is located to the presynaptic terminals.
The distribution and staining intensity of synaptic PK-resistant α-synuclein is shown in Fig. 5. In Tg mice, an intense immunoreactivity of presynapses was found in the hippocampus, especially in the dentate hilus, as well as in the temporal cortex. A moderate immunoreactivity was also found in the frontal cortex, thalamus, hypothalamus, brainstem, cerebellar cortex and spinal gray matter. Because similar distribution pattern of PK-resistant α-synuclein was found both in hemizygous and homozygous Tg mice, hemizygous Tg mice were preferentially used in the following examinations.
To examine when the accumulation of PK-resistant α-synuclein occurs in the developmental stage of Tg mice, we immunohistochemically examined the brain sections from 1-, 3-, 6-, 8-, 10-, 12- and 34-week-old Tg mice. Surprisingly, PK-resistant α-synuclein occurred in presynapses of hemizygous Tg mice even at 1 week of age (data not shown). These presynaptic PK-resistant α-synucleins were not immunostained with pSyn#64 until at least 34 weeks of age. Abnormal inclusions were observed from 2 weeks of age, which were immunolabelled with pSyn#64.
Similar findings were observed in the mouse brain fixed for 48 h and 2 weeks.
Distribution of PK-resistant α-synuclein in human α-synucleinopathies
We first examined the temporal lobe including the hippocampus from patients with DLB (PD stages V and VI) and control subjects. In general, intensity of LB509 immunoreactivity was weakened in controls with increasing time of PK treatment and the positive staining was almost entirely disappeared after 10 min of PK treatment (Fig. 6a–c, g–i). In contrast, LB509 immunoreactivity was preserved in the temporal lobe of DLB patients after 10 min of PK treatment (Fig. 6d–f, j–l). These PK-resistant α-synuclein-immunoreactive structures were recognized as abnormal inclusions (Lewy bodies, Lewy neurites and Lewy dots) or diffuse neuropil staining, corresponding to the presynaptic terminals. The PK-resistant α-synuclein observed in the abnormal inclusions was immunolabeled with pSyn#64, whereas PK-resistant α-synuclein in the presynaptic terminals was not phosphorylated (data not shown).
LB509 immunoreactivity in the brain of dementia with Lewy bodies (DLB) without PK treatment (a, d, g, j) or PK treatment for 5 min (b, e, h, k) or 10 min (c, f, i, l). PK treatment for 10 min diminishes neuropil staining in the temporal neocortex in controls (a–c), whereas α-synuclein immunoreactivity is preserved in DLB (d–f). PK treatment diminishes α-synuclein immunoreactivity in the hippocampal CA2/3 regions in controls (g–i), whereas α-synuclein immunoreactivity is the neuropil and Lewy neurites is preserved in DLB (j–l). Bars 100 μm
Based on the above findings, we hypothesized that PK-resistant α-synuclein is also deposited in the presynapses in certain brain regions in human α-synucleinopathies. Then, we systemically examined the brain of patients with Lewy body disease (PD stages II–VI), MSA and control subjects. In controls, no synaptic staining was noted after PK treatment (Fig. 7a–e). In stage II (Lewy pathology confined to the medulla oblongata and pontine tegmentum), PK-resistant synaptic staining was not found in the medulla oblongata (Fig. 7f), pontine tegmentum (Fig. 7g) and hippocampal CA2-3 region (Fig. 7i), whereas weak synaptic staining was found in the substantia nigra (Fig. 7h) and CA4 region (Fig. 7j). In stage III (Lewy pathology confined to the brainstem in the absence of cortical lesions), synaptic staining was also found in the substantia nigra and hippocampal CA4 region. In stage IV (Lewy pathology in the brainstem and antero-medial temporal mesocortex), synaptic staining in the substantia nigra and hippocampal CA4 region was more intense than that in stage III (Fig. 7k–o). In stages V and VI (Lewy pathology in the brainstem, limbic system and cerebral neocortex), synaptic staining was found in the tegmentum of the medulla oblongata and pons, substantia nigra and hippocampus (Fig. 7p–t). The staining intensity of the hippocampus was much stronger than that in stage IV (Fig. 7f). In stages V and VI, PK-resistant synaptic staining was also found in the cerebellar cortex and inferior olivary nucleus (data not shown). Abnormal accumulation of synaptic PK-resistant α-synuclein was also found in the hippocampus in 2 out of 5 patients with MSA, both of whom contained neuronal cytoplasmic inclusions in the medial temporal region (data not shown).
LB509 immunohistochemistry with PK treatment showing presynaptic PK-resistant α-synuclein in the dorsal vagal nucleus (DVN) (a, f, k, p), locus ceruleus (LC) (b, g, l, q), substantia nigra (SN) (c, h, m, r), and hippocampal CA2-3 (d, i, n, s) and CA4 regions (e, j, o, t) in controls, and stages II, IV and VI of human Lewy body disease. No synaptic staining in controls (a–e). Weak synaptic staining in the substantia nigra and CA4 in stage II (f–j). Modeate synaptic staining in the substantia nigra and CA4 in stage IV (k–o). Diffuse synaptic staining in the brainstem and hippocampus in stage VI (p–t). Bar 20 μm
Detection of PK-resistant α-synuclein by biochemical analysis
In order to confirm that PK-resistant α-synuclein exists in the presynapse in patients with DLB, biochemical analysis was performed using brain tissues from DLB (n = 3) and age-matched control subjects (n = 3). Sucrose gradient analysis clearly demonstrated that α-synuclein was distributed in presynaptic fractions 15–18, where synaptic proteins such as synaptophysin and SNAP25 exist (Fig. 8a). Subsequently, each fraction was digested with PK for 10 min, and applied to SDS-PAGE. However, immunoblot data have not been convincingly demonstrated that PK-resistant α-synuclein exists in the samples (data not shown). Alternatively, filter-trap assay was performed to detect PK-resistant α-synuclein. In this method, α-synuclein-rich fraction (No. 17) was subjected to various concentration of PK. The intensity of LB509-positive signal weakened with increasing concentration of PK in samples from control subjects, whereas LB509-positive signal remained detectable in samples from DLB even with 10 μg/ml of PK concentration (Fig. 8b). Without PK treatment, our filter-trap analysis demonstrated that α-synuclein is detected in samples from both control and DLB (Fig. 8c). Consistent with previous results [16], α-synuclein in DLB was detected throughout the almost all fractions (Fig. 8c). In contrast, α-synuclein in control was detected in fractions 13–18. Next, each fraction was subjected to PK digestion to examine which fraction contains PK-resistant α-synuclein. Filter-trap analysis clearly showed that PK-resistant α-synuclein exists in fractions 16–18, which is corresponding to synaptic protein-rich fractions in samples from DLB. In separate experiments, we obtained similar results in another samples from DLB and control subjects. Furthermore, PK-resistant α-synuclein was detected only in samples from Tg mice, but not in control mice under this condition (Fig. 8c). Collectively, these results suggest that PK-resistant α-synuclein was mainly located to the presynapses in human Lewy body disease and A53T α-synuclein Tg mice.
Biochemical analysis showing that α-synuclein is distributed to fractions 15–18 after sucrose gradient centrifugation. A marker protein of presynaptic nerve terminals, synaptophysin, is distributed to fractions 13–18. SNAP25, which is known to be localized to presynapses, is similarly distributed to fractions 13–18 in both DLB and control subjects (upper panel a). Arrowhead indicates that high-molecular weight bands are slightly detected in fractions 15–18 from DLB using LB509 antibody (lower panel a). Filter-trap analysis showing that α-synuclein in DLB is more resistant to PK treatment than that in control (b). Samples from fraction 17 of DLB and control were subjected to DNase I digestion (10 μg/ml) to avoid clogging the filter membrane. Following PK treatment (10 μg/ml) at room temperature for 10 min, 80 μl of each sample was immediately applied to the filter-trap apparatus and detected using LB509 antibody. Filter-trap analysis demonstrated that α-synuclein is distributed to fractions 13–18 in control subject and fractions 1 and 4–18 in DLB patient. Following PK treatment as described previously, α-synuclein in all fractions of control subject is diminished, whereas α-synuclein remains detectable in fractions 14 and 16–18 of DLB and 13–18 in Tg mice (c)
Discussion
Since PK treatment is useful for the evaluation of cytoplasmic and neuritic pathology in α-synucleinopathies [25–27, 33, 34], this retrieval method has been recommended to apply to routine α-synuclein immunostaining [2]. Here, we applied PK treatment for immunohistochemical examination of SNCA Tg and control mice. Immunohistochemical analysis using two antibodies against α-synuclein (NACP6 and LB509) demonstrated that PK-resistant α-synuclein is deposited in the presynaptic nerve terminals in Tg mice, but not in control mice. Considering that LB509 recognizes human α-synuclein, but not mouse α-synuclein, this finding indicates that human α-synuclein is over-expressed in the presynapses in Tg mice and is, at least in part, PK-resistant. Neumann et al. [27] reported that PK-resistant α-synuclein was deposited in the neuronal somata and processes in the central nervous system, predominantly in the brainstem and spinal cord, in aged Tg mice expressing human mutant A30P α-synuclein under Thy1 promoter. In A53T α-synuclein Tg mice we used, prion promoter was utilized to express human α-synuclein. The differences of expressed level and pattern of PK-resistant α-synuclein between A30P and A53T Tg mice may be due to the differences of mutant protein or promoter used.
Synaptic PK-resistant α-synuclein was widely distributed in the brain of A53T Tg mice, although it was preferentially accumulated in the hippocampus and temporal cortex. Some of the affected brain regions in Tg mice were implicated in human Lewy body disease. In addition to the PK-resistant cytoplasmic and neuritic pathology [28], PK-resistant α-synuclein was deposited in the presynaptic terminals in PD (stages III and IV) and DLB (stages V and VI). The distribution of presynaptic PK-resistant α-synuclein was more widespread in DLB than in PD and the staining intensity was most prominent in the dentate hilus (hippocampal CA4 region). Galvin et al. [7] reported that α- and β-synucleins were abnormally accumulated in the axon terminals of the dentate hilus in DLB, although they did not mention about PK-resistance of the accumulated α- and β-synucleins. Kramer et al. [16] also demonstrated diffuse neuropil staining of PK-resistant α-synuclein in the frontal and cingulate cortex in patients with DLB. The latter authors further showed that using the protein aggregate filtrate assay, the absolute majority of α-synuclein aggregates is located at the presynaptic terminals. Consistent with this observation, our filter-trap analysis demonstrated that PK-resistant α-synuclein is detected in synaptic protein-rich fractions in DLB. These findings suggest that presynaptic PK-resistant α-synuclein is deposited more extensively than has previously been appreciated.
Regarding phosphorylation and PK-resistance of α-synuclein, the character of α-synuclein deposited in A53T Tg mice and human α-synucleinopathies is summarized in Table 1. Although PK-resistant α-synuclein was found in the presynapse in A53T Tg mice even at 1 week of age, it was not phosphorylated until at least 8 months of age. Moreover, PK-resistant α-synuclein in the presynapse was not phosphorylated in human α-synucleinopathies. These findings suggest that phosphorylation is not necessary to cause the conversion of soluble form to PK-resistant α-synuclein. Furthermore, it is noteworthy that PK-resistant synaptic staining was found in the substantia nigra and hippocampus even in stage II (Lewy pathology confined to the medulla oblongata and pontine tegmentum). These findings suggest that PK-resistant synaptic staining precedes the deposition of phosphorylated α-synuclein in the substantia nigra and hippocampus.
α-Synuclein deposited in Lewy bodies in PD and DLD was phosphorylated and PK-resistant. By contrast, α-synuclein deposited in abnormal inclusions in A53T Tg mice was phosphorylated but not PK-resistant. Almost all of Lewy bodies are immunopositive for ubiquitin [18]. However, approximately 10–25% of abnormal inclusions found in A53T Tg mice are ubiquitinated [9]. Ultrastructurally, Lewy bodies consist of 10–20 nm non-constricted filaments [4]. Neuronal perikaryal inclusions in A53T Tg mice are also composed of filamentous structures, 10–16 nm in diameter [9]. These findings may imply that fibril formation does not participate in acquiring PK-resistance of α-synuclein.
In A53T Tg mice, α-synuclein in the abnormal inclusions was phosphorylated but not PK-resistant, whereas presynaptic α-synuclein was PK-resistant but not phosphorylated. In human Lewy body disease, α-synuclein deposited both in the abnormal inclusions and presynapse was PK-resistant. However, α-synuclein in the abnormal inclusions, but not in presynapse, was phosphorylated. It is likely that there are some differences in the mechanism of α-synuclein accumulation between the cytoplasm and presynapse in both A53T Tg mice and human Lewy body disease.
What causes PK-resistance of α-synuclein? Although we do not have clear answers to explain it, over-expression of α-synuclein may be necessary to change the property of α-synuclein. Fernagut et al. [5] reported that long-term exposure of paraquat, one of the pesticides, markedly increased the number of PK-resistant α-synuclein inclusions in the substantia nigra of Tg mice over-expressing wild-type human α-synuclein. Furthermore, Lu et al. [21] described age-dependent PK-resistant α-synuclein in the neuronal somata in the substantia nigra in Tg mice expressing C-terminal truncated human mutant parkin (Parkin-Q311X). Parkin gene is the most frequently mutated gene in familial early-onset recessive PD. Collectively, it is suggested that both environmental and genetic factors, along with increased level of α-synuclein are associated with the formation of PK-resistant α-synuclein.
In conclusion, we showed that PK-resistant α-synuclein accumulates in the presynaptic nerve terminals in distinct regions in A53T Tg mice and human Lewy body disease. Considering that native α-synuclein is a soluble protein localized to the presynaptic terminals, our findings suggest that PK-resistant α-synuclein may disturb the physiological functions of α-synuclein.
References
Abeliovich A, Schmitz Y, Farinas I et al (2000) Mice lacking alpha-synuclein display functional deficits in the nigrostriatal dopamine system. Neuron 25:239–252
Beach TG, White CL, Hamilton RL et al (2008) Evaluation of alpha-synuclein immunohistochemical methods used by invited experts. Acta Neuropathol 116:277–288
Braak H, Del Tredici K, Rub U et al (2003) Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging 24:197–211
Duffy PE, Tennyson VM (1965) Phase and electron microscopic observations of Lewy bodies and melanin granules in the substantia nigra and locus caeruleus in Parkinson’s disease. J Neuropathol Exp Neurol 24:398–414
Fernagut PO, Hutson CB, Fleming SM et al (2007) Behavioral and histopathological consequences of paraquat intoxication in mice: effects of alpha-synuclein over-expression. Synapse 61:991–1001
Fujiwara H, Hasegawa M, Dohmae N et al (2002) Alpha-synuclein is phosphorylated in synucleinopathy lesions. Nat Cell Biol 4:160–164
Galvin JE, Uryu K, Lee VM, Trojanowski JQ (1999) Axon pathology in Parkinson’s disease and Lewy body dementia hippocampus contains alpha-, beta-, and gamma-synuclein. Proc Natl Acad Sci USA 96:13450–13455
Giasson BI, Duda JE, Murray IV et al (2000) Oxidative damage linked to neurodegeneration by selective alpha-synuclein nitration in synucleinopathy lesions. Science 290:985–989
Giasson BI, Duda JE, Quinn SM et al (2002) Neuronal alpha-synucleinopathy with severe movement disorder in mice expressing A53T human alpha-synuclein. Neuron 34:521–533
Hasegawa M, Fujiwara H, Nonaka T et al (2002) Phosphorylated alpha-synuclein is ubiquitinated in alpha-synucleinopathy lesions. J Biol Chem 277:49071–49076
Iwai A, Masliah E, Yoshimoto M et al (1995) The precursor protein of non-Abeta component of Alzheimer’s disease amyloid is a presynaptic protein of the central nervous system. Neuron 14:467–475
Iwatsubo T, Yamaguchi H, Fujimuro M et al (1996) Purification and characterization of Lewy bodies from the brains of patients with diffuse Lewy body disease. Am J Pathol 148:1517–1529
Jakes R, Crowther RA, Lee VM et al (1999) Epitope mapping of LB509, a monoclonal antibody directed against human alpha-synuclein. Neurosci Lett 269:13–16
Kahle PJ (2008) Alpha-synucleinopathy models and human neuropathology: similarities and differences. Acta Neuropathol 115:87–95
Kahle PJ, Neumann M, Ozmen L et al (2000) Subcellular localization of wild-type and Parkinson’s disease-associated mutant alpha-synuclein in human and transgenic mouse brain. J Neurosci 20:6365–6373
Kramer ML, Schulz-Schaeffer WJ (2007) Presynaptic alpha-synuclein aggregates, not Lewy bodies, cause neurodegeneration in dementia with Lewy bodies. J Neurosci 27:1405–1410
Kruger R, Kuhn W, Muller T et al (1998) Ala30Pro mutation in the gene encoding alpha-synuclein in Parkinson’s disease. Nat Genet 18:106–108
Kuzuhara S, Mori H, Izumiyama N, Yoshimura M, Ihara Y (1988) Lewy bodies are ubiquitinated. A light and electron microscopic immunocytochemical study. Acta Neuropathol 75:345–353
Lee MK, Stirling W, Xu Y et al (2002) Human alpha-synuclein-harboring familial Parkinson’s disease-linked Ala-53→Thr mutation causes neurodegenerative disease with alpha-synuclein aggregation in transgenic mice. Proc Natl Acad Sci USA 99:8968–8973
Liu S, Ninan I, Antonova I et al (2004) Alpha-synuclein produces a long-lasting increase in neurotransmitter release. EMBO J 23:4506–4516
Lu XH, Fleming SM, Meurers B et al (2009) Bacterial artificial chromosome transgenic mice expressing a truncated mutant parkin exhibit age-dependent hypokinetic motor deficits, dopaminergic neuron degeneration, and accumulation of proteinase K-resistant alpha-synuclein. J Neurosci 29:1962–1976
Maroteaux L, Scheller RH (1991) The rat brain synucleins; family of proteins transiently associated with neuronal membrane. Brain Res Mol Brain Res 11:335–343
Masliah E, Rockenstein E, Veinbergs I et al (2000) Dopaminergic loss and inclusion body formation in alpha-synuclein mice: implications for neurodegenerative disorders. Science 287:1265–1269
Matsuoka Y, Vila M, Lincoln S et al (2001) Lack of nigral pathology in transgenic mice expressing human alpha-synuclein driven by the tyrosine hydroxylase promoter. Neurobiol Dis 8:535–539
Mori F, Piao YS, Hayashi S et al (2003) Alpha-synuclein accumulates in Purkinje cells in Lewy body disease but not in multiple system atrophy. J Neuropathol Exp Neurol 62:812–819
Mori F, Tanji K, Yoshimoto M, Takahashi H, Wakabayashi K (2002) Demonstration of alpha-synuclein immunoreactivity in neuronal and glial cytoplasm in normal human brain tissue using proteinase K and formic acid pretreatment. Exp Neurol 176:98–104
Neumann M, Kahle PJ, Giasson BI et al (2002) Misfolded proteinase K-resistant hyperphosphorylated alpha-synuclein in aged transgenic mice with locomotor deterioration and in human alpha-synucleinopathies. J Clin Invest 110:1429–1439
Neumann M, Muller V, Kretzschmar HA, Haass C, Kahle PJ (2004) Regional distribution of proteinase K-resistant alpha-synuclein correlates with Lewy body disease stage. J Neuropathol Exp Neurol 63:1225–1235
Piao YS, Mori F, Hayashi S et al (2003) Alpha-synuclein pathology affecting Bergmann glia of the cerebellum in patients with alpha-synucleinopathies. Acta Neuropathol 105:403–409
Polymeropoulos MH, Lavedan C, Leroy E et al (1997) Mutation in the alpha-synuclein gene identified in families with Parkinson’s disease. Science 276:2045–2047
Richfield EK, Thiruchelvam MJ, Cory-Slechta DA et al (2002) Behavioral and neurochemical effects of wild-type and mutated human alpha-synuclein in transgenic mice. Exp Neurol 175:35–48
Rockenstein E, Mallory M, Hashimoto M et al (2002) Differential neuropathological alterations in transgenic mice expressing alpha-synuclein from the platelet-derived growth factor and Thy-1 promoters. J Neurosci Res 68:568–578
Takeda A, Hashimoto M, Mallory M et al (2000) C-terminal alpha-synuclein immunoreactivity in structures other than Lewy bodies in neurodegenerative disorders. Acta Neuropathol 99:296–304
Takeda A, Hashimoto M, Mallory M et al (1998) Abnormal distribution of the non-Abeta component of Alzheimer’s disease amyloid precursor/alpha-synuclein in Lewy body disease as revealed by proteinase K and formic acid pretreatment. Lab Invest 78:1169–1177
Tanji K, Tanaka T, Mori F et al (2006) NUB1 suppresses the formation of Lewy body-like inclusions by proteasomal degradation of synphilin-1. Am J Pathol 169:553–565
van der Putten H, Wiederhold KH, Probst A et al (2000) Neuropathology in mice expressing human alpha-synuclein. J Neurosci 20:6021–6029
Wakabayashi K, Yoshimoto M, Tsuji S, Takahashi H (1998) Alpha-synuclein immunoreactivity in glial cytoplasmic inclusions in multiple system atrophy. Neurosci Lett 249:180–182
Yavich L, Oksman M, Tanila H et al (2005) Locomotor activity and evoked dopamine release are reduced in mice overexpressing A30P-mutated human alpha-synuclein. Neurobiol Dis 20:303–313
Yavich L, Tanila H, Vepsalainen S, Jakala P (2004) Role of alpha-synuclein in presynaptic dopamine recruitment. J Neurosci 24:11165–11170
Zarranz JJ, Alegre J, Gomez-Esteban JC et al (2004) The new mutation, E46K, of alpha-synuclein causes Parkinson and Lewy body dementia. Ann Neurol 55:164–173
Zhang HX, Tanji K, Mori F, Wakabayashi K (2008) Epitope mapping of 2E2-D3, a monoclonal antibody directed against human TDP-43. Neurosci Lett 434:170–174
Acknowledgments
This work was supported by Grants-in-Aid 20590335 (K.T.), 20591361 (F.M.) and 20300123 (K.W.) for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology, Japan, a Grant for Hirosaki University Institutional Research (K.W.), a Hirosaki University Grant for Exploratory Research by Young Scientists (K.T.), and a Grant-in-Aid for Studies on the Development of Diagnostic Technique and Therapies for Lewy Body Disease, the Ministry of Health, Labour and Welfare, Japan (K.W.). The authors wish to express their gratitude to M. Nakata for her technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tanji, K., Mori, F., Mimura, J. et al. Proteinase K-resistant α-synuclein is deposited in presynapses in human Lewy body disease and A53T α-synuclein transgenic mice. Acta Neuropathol 120, 145–154 (2010). https://doi.org/10.1007/s00401-010-0676-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00401-010-0676-z