Abstract
Hilar cholangiocarcinoma is a difficult technical challenge for the hepatobiliary surgeon. Achieving negative surgical margins with tumor resection is demanding due to the close proximity of the bile duct bifurcation to the vascular inflow of the liver. As recently as 2001, patients with main portal vein involvement proximal to the bifurcation were considered to be unresectable [1]. However, as portal vein resection was employed in the resection of other hepatobiliary and pancreatic tumors with success, the same principles were extended to hilar cholangiocarcinoma. Although portal vein resection may increase the risks of the resection, this procedure increases the number of patients with potentially resectable disease, and remains the only hope for long-term survival in this uncommon cancer. This chapter will review the indications, surgical technique, and outcomes of portal vein resection for hilar cholangiocarcinoma, as well as a brief review of arterial resection.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
21.1 Introduction
Hilar cholangiocarcinoma is a difficult technical challenge for the hepatobiliary surgeon. Achieving negative surgical margins with tumor resection is demanding due to the close proximity of the bile duct bifurcation to the vascular inflow of the liver. As recently as 2001, patients with main portal vein involvement proximal to the bifurcation were considered to be unresectable [1]. However, as portal vein resection was employed in the resection of other hepatobiliary and pancreatic tumors with success, the same principles were extended to hilar cholangiocarcinoma. Although portal vein resection may increase the risks of the resection, this procedure increases the number of patients with potentially resectable disease, and remains the only hope for long-term survival in this uncommon cancer. This chapter will review the indications, surgical technique, and outcomes of portal vein resection for hilar cholangiocarcinoma, as well as a brief review of arterial resection.
As previously described, hilar cholangiocarcinoma is a relatively rare tumor, and only one third of patients diagnosed with cholangiocarcinoma are candidates for resection. With a small number of patients considered resectable, only a few surgeons at highly specialized centers have developed experience in the surgical management of this formidable disease. However, advances over the last two decades in hepatic surgical techniques have led to a more aggressive approach to the treatment of cholangiocarcinoma. Early reports of biliary resection and biliary enteric anastomosis have advanced to partial and subtotal hepatic resection, combined hepatopancreaticoduodenectomy, and vascular resection (Fig. 21.1), of either portal vein or hepatic artery, or even both. The first Western description of portal vein resection for hilar cholangiocarcinoma was by Hadjis and Blumgart, who suggested the need for portal vein resection in order to achieve tumor clearance [2]. The combination of extended right hepatic resection and portal vein resection was first described in the west by Klempnauer et al. in 1997 [3] and was taken further by Neuhaus et al. in 1999 [4] to include standard resection of the portal bifurcation in a “no touch” technique to minimize tumor dissemination at the time of surgery as well as to improve the rate of negative margin resections. This is often referred to as the Berlin concept [5].
The anatomic juxtaposition of the hepatic duct bifurcation to the bifurcation of the portal vein continues to be a technical challenge in resection of hilar cholangiocarcinoma due to tumor adherence or involvement of the portal vein at the bifurcation. In many cases the tumor may not have truly invaded the portal vein or hepatic artery, however the desmoplastic response to the tumor that is made up of fibrous tissue containing tumor cells extends to the vessel and cannot be separated from the vessel without potential injury and an increased probability of leaving tumor cells adherent to the exterior vessel wall. Portal vein resection may increase the ability to resect with negative margins and improve subsequent long-term survival, however the risk of the procedure may be increased and should not be minimized.
21.2 Indications for Portal Vein Reconstruction
-
1.
The hilar cholangiocarcinoma tumor must meet standard criteria for an anatomic resection outside of portal vein involvement, including the potential for negative margins.
-
2.
The future liver remnant (FLR) volume must be sufficient for post-operative hepatic function, usually 25 % or greater of total liver volume (TLV). Portal vein embolization should be considered in patients to increase FLR to >25 % TLV
-
3.
Venous involvement can be central and at the bifurcation of the portal vein, however the distal portal vein on the liver remnant must have enough length clear of tumor to proceed with venous resection. On the left approximately 1 cm of left portal vein is required prior to segmental branching in order to have sufficient length for clamp placement. On the right, the right posterior branch needs to be clear of tumor. Venous anatomy to the right liver is more variable than the left and should be assessed by imaging prior to surgery. Arterial involvement and the potential for resection will be discussed below.
-
4.
Extra-hepatic disease confined to porta hepatis or intra-pancreatic portion of the bile duct. A complete portal lymphadenectomy should be completed at the time of resection. Portal lymph node spread decreases the chance of long term survival, but is not a contraindication to resection. Involvement of the common hepatic artery lymph node or aorto-caval lymph nodes is considered metastatic disease with less than 5 % 5-year survival. These patients likely should not be considered as candidates for resection. Intrahepatic metastases have a poor prognosis even if encompassed by hepatic resection and we would consider that a contraindication to resection.
-
5.
Extrahepatic metastatic disease is a clear contraindication to resection.
21.3 Pre-operative Evaluation
The standard pre-operative work-up consists of a triphasic-computed tomography (CT) to assess biliary, portal, and hepatic arterial involvement as well as to perform liver volumetry and assess FLR. Patients are also staged with chest and abdominal CTs to exclude extra hepatic and metastatic disease. In many patients, potential resectability can be determined by this evaluation alone, however; additional information may be obtained in some patients with magnetic resonance cholangiopancreatography (MRCP) and contrast enhanced MRI to further delineate biliary anatomy and tumor extension.
Although controversial, we feel that complete drainage and decompression of the remnant liver biliary tree is mandatory prior to resection, to decrease the risk of postoperative morbidity and mortality [6–8]. We consider an internally placed endoscopic cholangiopancreatography (ERCP) stent to be the first choice, but if adequate drainage is not achieved, percutaneous transhepatic drainage (PTCD) is required.
In many patients with hilar cholangiocarcinoma with vascular involvement, the FLR may already have experienced compensatory hypertrophy. However, if the hypertrophy has not occurred or if it is inadequate then pre-operative portal vein embolization should be performed (Fig. 21.2) on the side of the liver that is to be resected 4–6 weeks prior to surgery [9]. The importance of hypertrophy of the remnant liver in surgery for hilar cholangiocarcinoma has been demonstrated by multiple reports [10–14].
21.4 Procedure
21.4.1 Surgical Technique
-
1.
The first step of this operation includes an abdominal exploration to detect disseminated abdominal disease. This may be completed using minimally invasive techniques such as laparoscopy, particularly for those patients with bulky portal disease [15], or a mini laparotomy using a portion of the potential incision. If no contraindications to resection are initially seen the incision is widened and aorto-caval and common hepatic artery lymph nodes are sampled. If positive the patient is unlikely to benefit from resection.
-
2.
Patients without disseminated disease undergo a standardized assessment of resectability, including an intra-operative ultrasound directed examination of the tumor and the relationship of the tumor to the major vascular structures.
-
3a.
If the tumor is predominately right-sided and a right trisegmentectomy is contemplated, then dissection of the left hepatic duct and left portal vein at the base of the falciform ligament is performed. If the hepatic duct is clear at the segment 2/3 junction along with a patent left portal vein distally then a right trisegmentectomy can be performed. The left hepatic duct and left portal vein are accessible by dissecting the falciform ligament to the left portal vein capitalizing on the knowledge that the remnant of the umbilical vein (that during fetal circulation flowed into the left portal vein) runs within the round ligament of the falciform and will lead directly to the left portal vein at the portion just before the branching into segment 2, 3. This allows assessment of resectability before committing to bile duct division or hepatic resection. Even if the proximal portal vein and bile duct are involved, reconstruction can occur to the uninvolved distal structures.
-
3b.
If the tumor is predominately left-sided and a left trisegmentectomy is contemplated, intraoperative ultrasound plays a more important role. In particular tumor involvement along the right posterior hepatic duct (segments 6/7) must be assessed. The bifurcation of the anterior and posterior branches of both the portal vein and hepatic ducts are relatively intrahepatic and is a difficult area to assess for definitive evidence of tumor by either ultrasound or by the manual and visual assessment of the surgeon. Although lowering of the hilar plate facilitates the assessment of the segment 6, 7, take off it is not recommended because of the potential to broach the tumor plane. There is no doubt that in many cases the surgeon must commit to resection and hepatic division without certainty regarding margins and vessel involvement which is more frequently encountered in performing a left trisegmentectomy than a right sided resection. An assessment of the portal venous anatomy as well an assessment of the position of the posterior branch of the hepatic artery and its position relative to the portal vein branches on the right should also be undertaken during intraoperative ultrasound examination.
-
4.
After it has been determined that resection will proceed, the next step is dissection of the hepatic artery to ensure the hepatic arterial supply to the remnant liver is not involved by tumor. The common hepatic artery and left hepatic artery can be dissected out without committing to resection by dissecting along the medial side of the artery. In general, involvement of the common hepatic artery or major hepatic branch to the remnant liver is considered a contraindication to resection, however; there has been some success reported with hepatic arterial resection in selected cases, which will be discussed later in this chapter. The right hepatic artery, if in a standard position anterior to the portal vein but posterior to the bile duct is difficult to dissect out until after the bile duct has been divided and flipped superiorly.
-
5.
The common bile duct is then divided at the level of the pancreas and reflected superiorly (Fig. 21.3). A margin is sent from the distal common bile duct to assess for tumor involvement. Additional margin on the distal bile duct can be obtained by dissecting out the intra-pancreatic portion of the bile duct however pancreaticoduodenectomy may be considered if the margin is positive. A positive margin at this time requires a decision of how a negative distal margin can be obtained. If the patient is not a candidate for HPD then liver resection should not be considered in the face of a persistently positive distal margin. Lymph nodes of the hepatoduodenal ligament are resected either en-bloc with the bile duct as it is reflected superiorly along with the portal lymphatics or if the nodes must be removed separately then the level and position of the node is noted when the nodes are sent for permanent section. Reflecting the bile duct superiorly allows completion of the dissection of the right hepatic artery to its anterior/posterior division for a left sided resection and during that dissection possible involvement of the right hepatic artery or the posterior branch may preclude resection or necessitate resection and reconstruction. At this point the need for portal vein resection can be identified.
-
6.
The portal vein resection can be performed at two different time points during the procedure depending on the extent of mobility of the portal vein, extent of tumor and accessibility in the patient. In the majority of patients undergoing right-sided trisegmentectomies where access is reasonable and the amount of portal vein expected to be resected relatively short, the portal vein resection and reconstruction can be performed prior to hepatic transection. After dissection of the left hepatic artery to its segmental branches and ligation of the right hepatic artery, the main portal vein below the tumor is isolated. The left portal vein above the tumor is dissected out past the transverse portion of the vein up to the ascending segment just before branching into main segmental branches. Multiple caudate branches require division in order to free up enough left portal vein to work with. The area of the main portal venous bifurcation is left en bloc with the tumor. Vascular clamps are placed on the main portal vein and left portal vein just before it’s branching to main segmental branches (Fig. 21.4). The vein is then divided and left attached to the tumor. The left portal vein is then brought down to the main portal vein with a primary end to end anastomosis using 6-0 or 7-0 vascular sutures. Arterial perfusion can be maintained throughout the resection and reconstruction, minimizing ischemia to the FLR. The hepatic transection and specimen removal occurs after reconstruction with maintenance of both portal and hepatic arterial flow.
Fig. 21.4 In some patients where access is difficult or the tumor extensive, the portal vein is dissected as much as possible to prior hepatic transection, however it is not divided until hepatic parenchymal transection is completed. Dividing the portal vein at this later stage mobilizes the specimen and allows a tremendous improvement in mobility of the hepatic side of the portal vein, which can be rotated down significantly from its original position to minimize tension on the venous anastomosis (Fig. 21.5). The majority of left sided (Fig. 21.6) resections with anastomosis of the main portal vein to either right portal vein branch or posterior sectoral portal vein branch are more easily performed after hepatic parenchymal transection in our experience. In general the use of interposition grafts should not be required. If it appears that there will be excessive tension on the reconstruction by performing the reconstruction prior to hepatic parenchymal division then the reconstruction should be performed after the hepatic division when the additional mobility of the liver allows anastomosis. If even after hepatic transection a graft appears to be needed, hepatic vein from the resected side of the liver can be used to bridge the gap (Fig. 21.7) or if necessary the portion of the left renal vein between gonadal vein and IVC can be harvested and used as a graft. Both internal jugular vein and superficial femoral vein have been used as interposition grafts for the portal vein reconstruction, however the need for an interposition graft should be rare.
Fig. 21.5 Fig. 21.6 Fig. 21.7 Right hepatectomy with portal vein resection and reconstruction of the main portal vein to left portal vein. The right hepatic vein has been removed from the resected right lobe and used as an interposition graft. LHA left hepatic artery, LPV left portal vein, PV portal vein, Vein graft right hepatic vein used as an interposition graft
-
7.
Liver resection should then be performed using techniques familiar to the operating surgeon. The general consensus is that the caudate lobe should be resected routinely. In general we attempt to perform the parenchymal transection with maintenance of flow in both portal vein and hepatic artery in attempts to limit ischemia to what is considered an “damaged” liver from biliary obstruction and because of the requirement of additional ischemia during the portal vein resection and reconstruction phase of the procedure. However if bleeding is encountered we have little hesitation in applying inflow occlusion to the liver irrespective of whether the portal vein resection is performed initially prior to parenchymal division, or it is done at the completion of the parenchymal transection. If inflow occlusion is required we apply occlusion for periods of 15 min followed by 5 min of reperfusion [16].
-
8.
Frozen section analysis of margins should be used to guide resection, and if positive margins are encountered, additional resection should be performed if possible. Negative margins are the most important factor in long-term survival of this disease.
-
9.
In the majority of right trisegmentectomies, left portal vein resection can be completed prior to completion of the hepatic transection if there is a sufficient length of intrahepatic left portal vein that is tumor free [11, 17]. In left trisegmentectomies and in right trisegmentectomies involving cases where the left portal vein is more substantially involved, venous resection and reconstruction can be completed after resection. Resection without immediate reconstruction is not recommended, as it leaves the remnant liver with prolonged ischemia.
-
10.
Reconstruction is completed end to end with 5-0/6-0 running prolene suture, being careful to incorporate a growth factor as in liver transplantation. We generally “parachute” down the posterior wall to distribute tension along the venous anastomosis prior to bring the ends together and then run the anterior wall of the anastomosis. Alternatively the posterior wall can be parachuted down with a continuous suture and the front wall interrupted. As mentioned previously, if primary reconstruction is not feasible, hepatic vein from the side resected, left renal vein, superficial femoral vein or jugular vein can be considered for a conduit. Synthetic and cryopreserved grafts are not recommended due to the risk of infection and thrombosis. An important point is that arterial inflow to the remnant liver is maintained during reconstruction.
-
11.
The biliary system should be reconstructed using a 60 cm roux-en-Y limb of jejunum.
-
12.
Post-operative care is similar to a standard liver resection. Ultrasound should be used to confirm patency of the reconstructed vasculature, both intra- and post-operatively. At our center postoperative anticoagulation is reserved for patients at increased risk for thrombosis (hypercoaguable state, intraoperative thrombosis), complex reconstruction, or arterial reconstruction with small vessels (heparin, long-term aspirin). Other published series range from no anticoagulation [18] to catheters dripping heparin into the portal vein postoperatively [19].
21.5 Outcomes
21.5.1 Perioperative Morbidity and Mortality
21.5.1.1 Mortality
Early series with small numbers of patients with portal vein resection (PVR) for hilar cholangiocarcinoma had high mortality rates ranging from 8 to 33 %. This discouraged wide spread use of the described techniques [20–26]. In 2000, Gerhards et al. [21] also found vascular reconstruction to be an independent predictor of increased mortality. With increasing experience with extended hepatectomies, vascular reconstruction, and living donor liver transplantation [27], the mortality rates at specialized high volume centers have decreased dramatically and are now equivalent to non-vascular resections. Recent series demonstrate mortality of 2 % or less with portal vein and combined resections [11, 13, 18, 28]. Nagino et al. [18] published a series of 50 combined hepatic artery resections with a perioperative mortality of 2 %, which is decreased significantly from a 9.6 % mortality from the same group in 2003 [24]. Lee et al. [27] also reported a mortality of 0 in 40 consecutive patients with PVR from 2005 to 2008 compared to 9.8 % from 1989 to 2005. The authors of both of these studies concluded that general improvement of technique, including use of microvascular techniques, and improved perioperative management utilizing portal vein embolization and remnant liver biliary drainage resulted in improved outcomes.
Hemming et al. [11, 14] demonstrated a trend toward decreased mortality in patients undergoing PVR. In 95 patients undergoing resection for hilar cholangiocarcinoma, 42 patients who underwent PVR had a perioperative mortality of 2 % compared to 8 % for the 53 patients undergoing resection alone. The authors postulated that portal vein involvement mimics portal vein embolization, creating hypertrophy of the remaining hepatic lobe, and decreasing the risk of post-operative liver failure. With experience, there was also a significant decrease in 30-day mortality as a consequence of improvements in perioperative management (portal vein embolization, biliary drainage of the future liver remnant). In the first half of the study the operative mortality was 10 % and subsequently there were no perioperative mortalities in the second half of the study (P = 0.04) [14].
21.5.1.2 Morbidity
Despite improvement in mortality, these procedures continue to have a high morbidity, as do all major hepatic resections for hilar cholangiocarcinoma. Complications range from 43 to 100 % [13, 14, 25, 27]. Morbidity does not appear to differ between vascular and non vascular resections [23, 29], and in some cases may be decreased when compared to non vascular resections [19]. The most common complications are wound infection, bile leak, intra-abdominal abscess, sepsis, hemorrhage, reoperation and liver failure. The initial series demonstrated a high risk of postoperative liver insufficiency (defined in most series as hyperbilirubinemia, usually of serum bilirubin greater then 8–10 mg/dl) of up to 20 %. The more recent series using routine perioperative portal vein embolization showed liver failure to occur less frequently in 5–10 % of patients after resection [13], and most patients recovered with time.
The risk of complications directly related to vascular reconstruction is low. In one of the largest series of 111 patients who underwent portal vein reconstruction, five patients developed portal vein thrombosis intra- or post-operatively, and three requiring reoperation and thrombectomy. The paper reported four deaths from portal vein thrombosis and subsequent liver failure, but it is unclear if these were all related to portal vein resection and reconstruction [13]. Hirano et al. [19] reported 4 (10.8 %) intra-operative portal vein thromboses including two patients who received interposition grafts. All four were reconstructed intra-operatively without any long-term consequences. In a subsequent paper reporting on 50 more recent consecutive patients who received combined portal vein and hepatic arterial reconstructions by the same group, only one patient developed portal venous thrombosis postoperatively [18]. Hemming et al. [14] reported no anastomotic complications or thromboses in a review of 42 portal vein resections without the use of interposition grafts. There are several case reports of thrombosis with the use of interposition grafts [17, 19]. Although this is not a conclusive evidence, interposition grafts should only be used if absolutely necessary due to these concerns.
21.6 Survival
21.6.1 Overall Survival
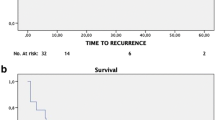
The 1, 3, and 5-year survival after hepatic resection and portal vein resection have been reported in many series. It is clear that survival of patients undergoing vascular resection is higher than that of a cohort of unresectable tumors [13, 18, 23]. In addition, vascular resection increases the number of potentially resectable tumors [24]. These facts alone validate the use of vascular resection if technically feasible in suitable patients. Reports on long-term survival after portal vein resection for hilar cholangiocarcinoma are conflicting. When comparing patients who underwent portal vein resection to patients who underwent resection only, most studies showed inferior long-term survival [18, 23, 24, 26]. For example, Igmai et al. [13] found that the survival rates of patients undergoing portal vein resection were 37 % at 3 years and 23 % at 5 years, which were less than the survival of non vascular resections (42 % at 5 years, 52 % if R0), but it was still better than the survivals of R2/pM1 resections and unresectable disease, and the survival was equivalent to R1 resections.
Ebata et al. [24] also reported on a worse long-term survival in patients requiring portal vein resection. However multivariate analysis demonstrated that portal vein resection itself did not worsen survival, but it was the presence of transluminal tumor or positive margins that had a negative impact. In many series, multivariate analysis showed portal vein resection to be a negative prognostic factor [24, 26], but more recent studies demonstrated otherwise [19]. Using the “no touch” technique, Neuhaus et al. [30] reported improved survival when compared to standard hepatic resection, with portal vein resection being a positive predictor of long-term survival. With improvement in perioperative mortality as centers gain more experience with these procedures, the long-term survival is also improved. Dinant et al. [25] demonstrated an increased 2 year survival from 33 % (1998–1993) to 60 % (1998–2003) by adopting aggressive surgical techniques including trisectionectomies, vascular reconstruction, and caudate resection to achieve negative margins.
Obviously a decreased survival after portal vein resection may be secondary to invasion of the portal vein by tumor. Hilar cholangiocarcinomas typically manifest an intense fibrotic response around the hilar plate and vessels. Portal vein involvement may be directly related to tumor involvement, or indirectly related to entrapment in the fibrotic reaction. In most series, only 30–50 % of resected veins actually have microscopic or histologic tumor involvement [18, 24, 31, 32]. Other series reported up to 80 % involvement [14, 23], and there is obviously some difference between studies in the definition of histologic involvement. Whether or not histologic portal vein involvement influences survival is also controversial. Several series reported that histologic portal vein invasion is a negative prognostic factor for long-term survival [23, 32, 33], while other studies did not demonstrate this effect [14, 19]. A negative margin or R0 resection remains the best chance for long-term survival, and not surprisingly tumors requiring portal vein resection are also less likely to achieve an R0 resection [29].
In addition, several series have report on some patients surviving over 3 years [22, 34]. Nagino et al. [18] reported on six patients who lived longer than 3 years, and two patients who were alive after 5 years with combined portal vein and hepatic artery resection. Lee et al. [27] reported on ten patients who survived longer than 5 years after portal vein resection, including six patients who were alive and disease free at the time of publication, and they estimated that portal vein resection could offer long-term survival in more than one of ten patients with locally advanced hilar cholangiocarcinoma.
21.7 “No Touch” Resections
Some authors have advocated a “no touch” method resection for hilar cholangiocarcinoma [30, 31]. As mentioned above, hilar cholangiocarcinoma is challenging because of the proximity of the hepatic duct bifurcation to the major vascular inflow of the liver. Even if the portal vein is not directly involved with the tumor, the tumor may involve the perihilar lymphatics and neural tissue. To decrease the potential of locoregional recurrence for microscopic tumor spread and increase the likelihood of an R0 resection require an en bloc resection including right hepatectomy, caudate lobectomy, bile duct resection, and portal vein resection. Neuhaus et al. [30] championed this technique, with a 5-year survival of 72 % for patients who underwent en bloc vascular resection, which was significantly higher than patients undergoing non-vascular resection.
Subsequently, Hirando et al. [31] published a series of 64 patients, in which 25 patients underwent en bloc resection. Forty-three patients underwent conventional resection, including 18 patients with portal vein resection. Intra-operative thrombosis occurred in four patients, two patients in each of the portal vein resection and the en bloc groups. These were all revised intra-operatively and there were no post-operative portal vein complications. Two-year survival was not significantly different between the no resection, conventional, and en bloc groups (73.7 %/39.7 %/69.6 %), but trended down in the conventional resection group. Morbidity and in hospital mortality also did not differ between the groups. In contrast, Lee et al. [27] reported that in actual clinical practice, the “no-touch technique” for extensive surgical resection of hepatopancreatobiliary malignancies has failed to show a short-term survival benefit because of the high postoperative mortality [27]. Of course, the ultimate “no touch” technique is liver transplantation, which has encouraging results in very select patients [35].
21.8 Right Versus Left Resections
Some centers would argue that portal vein resection and aggressive liver resection for hilar cholangiocarcinoma should be limited to right trisegmentectomies, and left hepatectomies with left trisegmentectomies in particular to be avoided due to the anatomic differences in the right hepatic lobe [4, 36] and the difficulty in getting negative margins. In particular, the early ramifications of the right portal vein and biliary system require dissection that may broach microscopic tumor planes. The course of the right hepatic artery and in particular the position of the posterior right hepatic artery relative to both the posterior branches of the duct and relative position to the portal vein branches makes achieving a negative margin without broaching tumor planes more difficult. Left trisectionectomies have been reported to have an increased mortality, decreased R0 resections, and as a result decreased long term survival in some series when compared to right sided trisectionectomies [5].
However, as surgeons continue to push boundaries, experience with left sided hepatectomies for hilar cholangiocarcinoma with combined vascular resection continues to grow. Shimizu et al. [37] recently published a series of 224 patients of whom 88 underwent left hepatectomies and 84 underwent right hepatectomies. Portal vein resection was carried out in 23 of 88 left hepatectomies (26 %) and 25 of 84 right hepatectomies (30 %). Overall R0 resection, morbidity, and survival were equivalent between the two groups, except that left hepatectomies had an increased risk of bile leakage, and right hepatectomies had an increased risk of liver insufficiency and mortality as a result of the smaller remnant liver. However, there was a significantly decreased chance of an R0 resection with a left hepatectomy and portal vein resection compared to the right hepatectomy, and a subsequent decrease in long-term survival. If an R0 resection was achieved, survival was the same. There was also a significant increase in the use of partial wedge resections with vein patching versus a segmental vein resection and end-to-end venous anastomosis in left hepatectomies, due to the limited mobility and early ramifications of the right portal vein [37]. The authors concluded that while extended left or left trisegmentectomies are technically more demanding than right sided resections for hilar cholangiocarcinoma, in many cases they are the only option available to perform a curative resection.
21.9 Hepatic Artery Resection
Until recently hepatic arterial involvement was considered a contraindication to resection for hilar cholangiocarcinoma. However, as more experience is gained in these complex combined vascular and hepatic resections, aggressive centers are resecting and reconstructing both the right, left, and main hepatic artery with acceptable outcomes. These innovations may continue to extent the limits of resection with hilar cholangiocarcinoma, particularly in extended left trisegmentectomies where the right hepatic artery can often be involved with tumor as the artery runs close to the hepatic hilus.
Hepatic artery reconstructions can be completed in a segmental fashion with reconstruction using either an end-to-end anastomosis to the left gastric, right gastric or gastroduodenal or other alternative inflow, or an interposition graft (including greater saphenous vein or radial artery, or proximal splenic artery (Fig. 21.8)) [38]. As with portal vein resection, a distal hepatic artery clear of tumor is necessary. If portal vein resection is also required, hepatic arterial resection should be done in a sequential fashion before or after portal vein resection to protect the liver from ischemia. If this cannot be done, cold perfusion techniques may be necessary.
21.9.1 Combined Hepatic Artery and Portal Vein Resection
Early results from hepatic artery resection for hilar cholangiocarcinoma were dismal. Some early series including hepatic arterial resections with or without portal vein reconstruction had a high mortality of 33.3–55.6 % [23, 39, 40] with no long term survivors. Gerhards et al. [21] found in an univariate analysis that hepatic arterial resection increased mortality in extended liver resections for hilar cholangiocarcinoma. Miyazaki et al. [23] reported the results of nine combined hepatic artery and portal vein resections. There was no benefit in terms of survival (1- and 3-year survival rate; 17 % and 0, respectively) and it led to an increase in operative mortality (33 %) and morbidity (78 % compared to 36 %). A recent series comparing right and left hepatectomies found that hepatic arterial resection for both right and left hepatectomies (11 patients) decreased survival, and there were no survivors beyond 3 years [37].
However, recent advances in microsurgical techniques and increasing experience with vascular resections have improved outcomes in patients undergoing hepatic artery resection. Several series on portal vein reconstruction have included small numbers of patients with concomitant hepatic artery resection without any significant complications [11, 12, 32, 41]. In a series published by Yamanaka et al., 25 patients underwent major hepatic resection with vascular reconstruction for hilar cholangiocarcinoma. The series included: ten patients who underwent hepatic arterial reconstruction (nine right and one left hepatic artery) [20]. The reconstructions were all done in an end to end fashion to the proper hepatic artery or gastroduodenal artery, and 80 % were done using microsurgical techniques. Perioperative mortality was 8.8 %. Although survival was lower in the left trisegmentectomy group with vascular resections, the complications were not directly related to the vascular reconstruction. In a similar series, Shimada et al. looked at 39 patients with hilar cholangiocarcinoma and gallbladder cancer, of which 17 underwent hepatic arterial resection with or without portal vein resection [22]. Patency was achieved in 83 % of the reconstructed hepatic artery, and two patients developed multiple hepatic abscesses from hepatic arterial thrombosis. The results improved after they adopted microsurgical techniques. Perioperative mortality in the patients with vascular reconstruction was 13.3 % compared to 8.3 %, alone in the non-reconstruction cohorts. Two patients with combined HA/PV reconstruction survived more than 3 years.
In the largest series published to date, Nagino et al. [18] reported a series of 50 patients who underwent simultaneous resection of hilar cholangiocarcinoma, including 26 left trisegmentectomies, 23 left hepatectomies, and one right hepatectomy. R0 resection was achieved in 33 (66 %) patients. The 1, 3 and 5 year survivals were 78.9, 36.3, and 30.3 %, respectively. Twenty-seven (54 %) patients developed complications and one patient died perioperatively. All reconstructions were done with the assistance of a surgical microscope, and these included 32 end-to-end anastomoses, 11 greater saphenous vein or radial artery interpositions, and 2 reconstructions using the left or right gastric artery. Three patients were unable to be reconstructed. One patient with a vein graft thrombosed intra-operatively and was thrombectomized and revised without any complication. There were no long-term complications from the arterial reconstructions. The authors of this series believe that the microsurgical techniques offered an improvement over their earlier studies.
In some cases, reconstruction may not be necessary. Miyake et al. [42] reported a case where the right hepatic artery was unable to be reconstructed, but there was good collateral flow through the right phrenic artery and the patient recovered. If the branch of the hepatic artery supplying segment IV (or middle hepatic artery, which arises from the left hepatic artery in 75 % of cases) is the only artery which is involved by tumor, it can be resected without any significant complications, including biliary leaks and abscesses [19].
In preparation for hepatic arterial resection, some authors have advocated pre-operative hepatic arterial embolization to allow for the development of collaterals prior to resection. Yasuda et al. [34] described pre-operative embolization of the right hepatic artery to allow collateralization of the right liver remnant for left trisectionectomies with tumors involving the right and proper hepatic arteries. A series of six patients underwent left trisegmentectomy 3 weeks after arterial embolization for hilar cholangiocarcinoma. All six patients underwent R0 resection, and there were no liver failure or perioperative death. Two patients remain alive after 7 years.
In some cases, it may not be technically possible to reconstruct the hepatic artery, due to the extent of tumor involvement or its small caliber. In the largest series of hepatic arterial resection reported to date, Nagino et al. [18] described three patients in whom the artery was unable to be reconstructed. In one patient, it was a small segment 6 artery that did not require reconstruction. The other two patients underwent arterioportal shunting, which resulted in liver failure in one patient, and liver abscess in the other. Kondo et al. [43] reported better results in using arterioportal shunting in ten patients (6 HCCA and 4 GBCA). There were no deaths, and three patients developed complications including bile leakage and liver abscesses. Angiography performed 1 month after surgery showed shunt occlusion in 30 % of the patients. The remainder of the shunts was occluded by coil embolization after collateralization was confirmed.
21.10 Conclusion
Multiple series have now confirmed that an aggressive surgical approach to hilar cholangiocarcinoma is beneficial. Portal vein resection can be performed safely with low mortality and acceptable morbidity at high volume specialized centers. While routine en bloc portal vein resection of all hilar cholangiocarcinomas has been advocated by some centers it is difficult to recommend routine resection of the portal vein at this time. It is our recommendation that portal vein resection be carried out in cases where the portal vein cannot be separated from the tumor either because of direct tumor spread or peri-tumoral fibrosis. There is no doubt that combined portal vein resection offers improved survival when compared to no resection or a resection with positive margins. In selected patients, vascular resection increases the chance of obtaining negative resection margin, and may increase the number of patients who can be consider for resection. Recently the reported 5-year survival rate for hilar cholangiocarcinoma of 50 % exceeds the survival reported for pancreatic cancer. Portal vein resection for hilar cholangiocarcinoma in experienced hand should no longer be considered controversial. Hepatic arterial resection is also evolving and while it should not considered as routine at present, it may become a standard aggressive treatment of hilar cholangiocarcinoma in the future as techniques and experience continue to improve.
References
Jarnagin WR, Fong Y, DeMatteo RP, et al. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001;234(4):507–17; discussion 17–9.
Hadjis NS, Blenkharn JI, Alexander N, et al. Outcome of radical surgery in hilar cholangiocarcinoma. Surgery. 1990;107(6):597–604.
Klempnauer J, Ridder GJ, Werner M, et al. What constitutes long-term survival after surgery for hilar cholangiocarcinoma? Cancer. 1997;79(1):26–34.
Neuhaus P, Jonas S, Bechstein WO, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg. 1999;230(6):808–18; discussion 19.
Thelen A, Scholz A, Benckert C, et al. Microvessel density correlates with lymph node metastases and prognosis in hilar cholangiocarcinoma. J Gastroenterol. 2008;43(12):959–66.
Grandadam S, Compagnon P, Arnaud A, et al. Role of preoperative optimization of the liver for resection in patients with hilar cholangiocarcinoma type III. Ann Surg Oncol. 2010;17(12):3155–61.
Nimura Y. Preoperative biliary drainage before resection for cholangiocarcinoma (Pro). HPB (Oxford). 2008;10(2):130–3.
Laurent A, Tayar C, Cherqui D. Cholangiocarcinoma: preoperative biliary drainage (Con). HPB (Oxford). 2008;10(2):126–9.
Hemming AW, Reed AI, Howard RJ, et al. Preoperative portal vein embolization for extended hepatectomy. Ann Surg. 2003;237(5):686–91; discussion 91–3.
Kennedy TJ, Yopp A, Qin Y, et al. Role of preoperative biliary drainage of liver remnant prior to extended liver resection for hilar cholangiocarcinoma. HPB (Oxford). 2009;11(5):445–51.
Hemming AW, Kim RD, Mekeel KL, et al. Portal vein resection for hilar cholangiocarcinoma. Am Surg. 2006;72(7):599–604; discussion 604–5.
Lee SG, Lee YJ, Park KM, et al. One hundred and eleven liver resections for hilar bile duct cancer. J Hepatobiliary Pancreat Surg. 2000;7(2):135–41.
Igami T, Nishio H, Ebata T, et al. Surgical treatment of hilar cholangiocarcinoma in the “new era”: the Nagoya University experience. J Hepatobiliary Pancreat Sci. 2010;17(4):449–54.
Hemming AW, Mekeel K, Khanna A, et al. Portal vein resection in the management of hilar cholangiocarcinoma. J Am Coll Surg. 2011;212(4):604–13; discussion 613–6.
D’Angelica M, Fong Y, Weber S, et al. The role of staging laparoscopy in hepatobiliary malignancy: prospective analysis of 401 cases. Ann Surg Oncol. 2003;10(2):183–9.
Petrowsky H, McCormack L, Trujillo M, et al. A prospective, randomized, controlled trial comparing intermittent portal triad clamping versus ischemic preconditioning with continuous clamping for major liver resection. Ann Surg. 2006;244(6):921–8; discussion 8–30.
Kondo S, Katoh H, Hirano S, et al. Portal vein resection and reconstruction prior to hepatic dissection during right hepatectomy and caudate lobectomy for hepatobiliary cancer. Br J Surg. 2003;90(6):694–7.
Nagino M, Nimura Y, Nishio H, et al. Hepatectomy with simultaneous resection of the portal vein and hepatic artery for advanced perihilar cholangiocarcinoma: an audit of 50 consecutive cases. Ann Surg. 2010;252(1):115–23.
Hirano S, Kondo S, Tanaka E, et al. Safety of combined resection of the middle hepatic artery in right hemihepatectomy for hilar biliary malignancy. J Hepatobiliary Pancreat Surg. 2009;16(6):796–801.
Yamanaka N, Yasui C, Yamanaka J, et al. Left hemihepatectomy with microsurgical reconstruction of the right-sided hepatic vasculature. A strategy for preserving hepatic function in patients with proximal bile duct cancer. Langenbecks Arch Surg. 2001;386(5):364–8.
Gerhards MF, van Gulik TM, de Wit LT, et al. Evaluation of morbidity and mortality after resection for hilar cholangiocarcinoma—a single center experience. Surgery. 2000;127(4):395–404.
Shimada H, Endo I, Sugita M, et al. Hepatic resection combined with portal vein or hepatic artery reconstruction for advanced carcinoma of the hilar bile duct and gallbladder. World J Surg. 2003;27(10):1137–42.
Miyazaki M, Kato A, Ito H, et al. Combined vascular resection in operative resection for hilar cholangiocarcinoma: does it work or not? Surgery. 2007;141(5):581–8.
Ebata T, Nagino M, Kamiya J, et al. Hepatectomy with portal vein resection for hilar cholangiocarcinoma: audit of 52 consecutive cases. Ann Surg. 2003;238(5):720–7.
Dinant S, Gerhards MF, Rauws EA, et al. Improved outcome of resection of hilar cholangiocarcinoma (Klatskin tumor). Ann Surg Oncol. 2006;13(6):872–80.
Young AL, Prasad KR, Toogood GJ, et al. Surgical treatment of hilar cholangiocarcinoma in a new era: comparison among leading eastern and western centers, Leeds. J Hepatobiliary Pancreat Sci. 2010;17(4):497–504.
Lee SG, Song GW, Hwang S, et al. Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Sci. 2010;17(4):476–89.
Miyazaki M, Kimura F, Shimizu H, et al. One hundred seven consecutive surgical resections for hilar cholangiocarcinoma of Bismuth types II, III, IV between 2001 and 2008. J Hepatobiliary Pancreat Sci. 2010;17(4):470–5.
Kurosaki I, Hatakeyama K, Minagawa M, et al. Portal vein resection in surgery for cancer of biliary tract and pancreas: special reference to the relationship between the surgical outcome and site of primary tumor. J Gastrointest Surg. 2008;12(5):907–18.
Neuhaus P, Jonas S, Settmacher U, et al. Surgical management of proximal bile duct cancer: extended right lobe resection increases resectability and radicality. Langenbecks Arch Surg. 2003;388(3):194–200.
Hirano S, Kondo S, Tanaka E, et al. No-touch resection of hilar malignancies with right hepatectomy and routine portal reconstruction. J Hepatobiliary Pancreat Surg. 2009;16(4):502–7.
Hidalgo E, Asthana S, Nishio H, et al. Surgery for hilar cholangiocarcinoma: the Leeds experience. Eur J Surg Oncol. 2008;34(7):787–94.
Ebata T, Kamiya J, Nishio H, et al. The concept of perihilar cholangiocarcinoma is valid. Br J Surg. 2009;96(8):926–34.
Yasuda Y, Larsen PN, Ishibashi T, et al. Resection of hilar cholangiocarcinoma with left hepatectomy after pre-operative embolization of the proper hepatic artery. HPB (Oxford). 2010;12(2):147–52.
Heimbach JK, Haddock MG, Alberts SR, et al. Transplantation for hilar cholangiocarcinoma. Liver Transpl. 2004;10(10 Suppl 2):S65–8.
Kondo S, Hirano S, Ambo Y, et al. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg. 2004;240(1):95–101.
Shimizu H, Kimura F, Yoshidome H, et al. Aggressive surgical resection for hilar cholangiocarcinoma of the left-side predominance: radicality and safety of left-sided hepatectomy. Ann Surg. 2010;251(2):281–6.
Sakamoto Y, Sano T, Shimada K, et al. Clinical significance of reconstruction of the right hepatic artery for biliary malignancy. Langenbecks Arch Surg. 2006;391(3):203–8.
Ota T, Araida T, Yamamoto M, et al. Operative outcome and problems of right hepatic lobectomy with pancreatoduodenectomy for advanced carcinoma of the biliary tract. J Hepatobiliary Pancreat Surg. 2007;14(2):155–8.
Shimada K, Sano T, Sakamoto Y, et al. Clinical implications of combined portal vein resection as a palliative procedure in patients undergoing pancreaticoduodenectomy for pancreatic head carcinoma. Ann Surg Oncol. 2006;13(12):1569–78.
Madariaga JR, Iwatsuki S, Todo S, et al. Liver resection for hilar and peripheral cholangiocarcinomas: a study of 62 cases. Ann Surg. 1998;227(1):70–9.
Miyake H, Mizuno K, Iyomasa S, et al. Limited hepatectomy with left hepatic vein reconstruction for hepatocellular carcinoma on cirrhosis. Surgery. 2004;135(6):696.
Kondo S, Hirano S, Ambo Y, et al. Arterioportal shunting as an alternative to microvascular reconstruction after hepatic artery resection. Br J Surg. 2004;91(2):248–51.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media Dordrecht and People's Medical Publishing House
About this chapter
Cite this chapter
Mekeel, K., Hemming, A.W. (2013). Combined Liver Resection and Portal Vein Resection. In: Lau, W. (eds) Hilar Cholangiocarcinoma. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-6473-6_21
Download citation
DOI: https://doi.org/10.1007/978-94-007-6473-6_21
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-6472-9
Online ISBN: 978-94-007-6473-6
eBook Packages: MedicineMedicine (R0)