Abstract.
Background: Surgical resection provides the only chance of cure for patients suffering from hilar cholangiocarcinoma. Although appropriate procedures are not agreed upon, an increase in radicality has been observed during the past 20 years.
Methods: The literature as well as our own experience after 133 resections of hilar cholangiocarcinomas were reviewed.
Results: Tumor-free margins represent the most important prognostic parameter. Hilar resections as least radical resective procedure will generate rates of formally curative resections of less than 50%. Even after these formally curative resections, long-term survival cannot be achieved. Only additional liver resections will increase the number of long-term survivors to significant figures. In our series, the best 5-year survival rate of 72% was achieved after right trisegmentectomy with concomitant resection of the portal vein bifurcation.
Conclusion: Right trisegmentectomy and combined portal vein resection represent the best way to comply with basic rules of surgical oncology for hilar cholangiocarcinoma. This procedure will provide the most pronounced benefit among various types of liver resection, whereas local resections of the extrahepatic bile duct must be considered as an oncologically inefficient procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biliary tract cancer originates in more than 50% of the patients from the bile duct bifurcation within the hepatic hilum. It must be distinguished from carcinomas arising within the biliary epithelium in the periphery of the liver or distal to the cystic duct down to the Papilla Vateri. The surgical strategy for intrahepatic cholangiocarcinomas follows the principles established for other mass-forming tumors in non-cirrhotic livers, such as, for example, colorectal liver metastasis or some forms of hepatocellular carcinoma. This strategy will generally result in an extended liver resection, because most of these tumors will only be diagnosed in an advanced stage, as early symptoms are usually absent. This is, for example, in contrast to hepatocellular carcinoma, in which screening of cirrhotic livers will result in the detection of a considerable share of early tumors.
Biliary tract cancers located distal to the cystic duct mostly have a close proximity to the pancreatic head; therefore, their surgical management involves many of the principles which are also applied for pancreatic head cancer. In addition, patients suffering from these distal cholangiocarcinomas undergo resection of the extrahepatic biliary tract up to the hepatic hilum.
The principal goal for hilar or central cholangiocarcinomas, which means tumors at the bifurcation, is to achieve not only a formally curative resection, but also to apply established guidelines for oncological surgery in general. These guidelines are mainly to achieve wide tumor-free margins, to use no-touch techniques and to avoid intraoperative open tumor biopsies. The close vicinity of these tumors to the portal vein, to the liver arteries, and to the liver parenchyma is one of the main obstacles to accomplishing this goal. Moreover, lateral infiltration occurs early, because of a late diagnosis. This late diagnosis results from the fact that a lateral extension of epithelial biliary tract tumors is not compromised by a strong muscular layer which is almost lacking in the bile duct. On the other hand, the detergent properties of the bile allows a sufficient flow even shortly before a complete luminal obstruction [1]. The growth pattern of hilar cholangiocarcinomas adds to the technical difficulties of a resection, because nodular and well-demarcated or even encapsulated tumors are a rarity, whereas a periductal infiltration is typical. Irrespective of a local growth along lymphatic tracts, a microscopic infiltration of perineural sheaths occurs [2, 3]. Identification of tumor boundaries is hardly possible by digital palpation. As a consequence, a surgical strategy based on principles trying to achieve a wide margin, rather than limited resections based on a possibly misleading intraoperative personal impression, should be favored.
One advantageous feature of hilar cholangiocarcinomas seems to be their low propensity for distant metastasis, which may be regarded as an additional argument for principally extended resections.
Extrahepatic bile duct resection
Extrahepatic bile duct resections, including only parts of the hilar liver parenchyma, must be considered as an oncologically inefficient procedure over the long term. They have been applied, and in some institutions still are, in curative as well as in palliative intention. Probably they are warranted in neither of the two approaches. The mainstay of palliative treatment are endoscopic or transhepatic interventions such as endoscopic retrograde cholangiography (ERC) with stent implantation or percutaneous transhepatic cholangiography and drainage (PTCD) with the possibility of internalization by transtumoral drainages [4, 5]. Various types of surgical bypass operations turned out to result only rarely in a complete decompression of the biliary tree while bearing a considerable morbidity and mortality when applied in a palliative intention [6].
The perspective of local resections as a curative approach are even more worse as has recently been reported by several centers. Jarnagin et al. from the Memorial Sloan Kettering Cancer Center have described 80 patients undergoing resection of a hilar cholangiocarcinoma [7]. Among these 80 patients, an extrahepatic biliary tract resection or a partial hepatic resection had been performed in 18 and 62 patients, respectively. The rate of formally curative resections was considerably high (78%). Within the group of formally curative resections, liver resection was the only independent prognostic parameter. After a follow-up period of 5 years, only 9 patients were alive. All of these 9 patients had undergone a liver resection, whereas no patient after an extrahepatic biliary tract resection had survived.
A similar result has been published by Miyazaki et al. from Chiba University in Japan [8]. Extrahepatic biliary tract resections or liver resections had been performed in 11 and 65 patients, respectively. The respective rates of formally curative resections in these two groups were 45 and 75%. There was no 5-year survival after extrahepatic biliary tract resections, compared with a 27% survival rate after additional liver resection.
The largest series thus far originates from Nimura and his group from Nagoya Medical School in Japan, comprising 142 patients including 108 formally curative resections (76%) [9]. Nimura et al. had achieved a formally curative resection in only 8 patients by an extrahepatic biliary tract resection, compared with 100 patients who had undergone a liver resection. In the group of extrahepatic biliary tract resections, all patients had died after 65 months. Ten-year survival after formally curative liver resection was 20%. The results after extrahepatic bile duct resection for hilar cholangiocarcinoma are summarized in Table 1.
Another factor, indicating that an extrahepatic biliary tract resection is insufficient in achieving a local tumor control, is a high local recurrence rate of 76% [10]. Local recurrence mostly occurred at the resection margins, predominantly on the side of the liver. In other gastrointestinal cancers a local recurrence rate of 80% would be considered unacceptable. Such a high figure may occur, for example, after resection of rectal cancer in case of an intraoperative tumor perforation with consecutive dissemination of tumor cells.
The most promising strategy to overcome the problem of high local recurrence rates, after resection of hilar cholangiocarcinoma, is an extension of the resection margins especially at the side of the liver. In the experience of our institution from 1988 to 2000, only 6 R0 resections in the extrahepatic bile duct resection group can be compared with 66 R0 liver resections resulting in 5-year survival rates of 0 and 35%, respectively.
It is noted that in the group of extrahepatic biliary tract resections half of the patients were suffering from type-I or type-II tumors, according to the Bismuth-Corlette classification. These patients originate from the early phase of our experience and had been treated with a curative intent. The remaining patients in this group were suffering from locally advanced tumors in whom palliation was the primary goal. In all the other groups, patients were almost exclusively suffering from type-III or type-IV tumors, according to the Bismuth-Corlette classification. In these patients, resection was only possible because of an additional liver resection and would not have been attempted without it. As a consequence, an additional hepatic resection increases the resectability rate.
Central hepatic resections
Especially in the Japanese literature, some authors advocated a central hepatic resection [9, 11]. The concept of resecting the medial sectors of the liver, which means the segments IV, V, and VIII, or at least the inferior parts of these sectors, creates two resection lines on each side of the hepatic hilum. It is an attempt to achieve a wide tumor-free margin and to overcome the problem of tumor-free margins which sometimes do not exceed 1–2 mm.
The criticism to such a central bisectionectomy is that the left and the right liver artery, as well as the left and the right portal vein branch, have to be preserved. This is a problem, because especially the portal bifurcation and the right liver artery run in close proximity to a hilar cholangiocarcinoma. Frequently, an inflammatory induration of the tissue cannot be distinguished from an infiltration of these vessels. As a consequence, tumor cells are likely to be spilled into the operative field by dissecting these structures.
Another criticism is the creation of two resection lines, thus increasing the risk of morbidity, especially complications from a postoperative bile leakage. Due to the high variability of the segmental ramification between the right lateral section (segments VI/VII) and the right medial section (segments V/VIII), on the one hand, and a sometimes high number of small orifices on the right side, a multitude of biliodigestive anastomoses has to be created. Moreover, the real oncological advantage of shifting the resection line to the right side may be doubted, because the distance from the midline of the liver towards the right intersection is relatively wide only in the periphery. Centrally, that means around the hepatic hilum, all the intersections almost converge and hardly allow for a considerable additional distance to the tumor.
Extended right lobe resection
In our perception, oncological surgery for hilar cholangiocarcinoma, including wide tumor-free margins and no-touch techniques, can only be realized by performing right-sided resections together with the resection of the portal vein. The advantages can easily be exemplified by comparing this procedure to the central bisectionectomy.
Firstly, it is not necessary to dissect any structures in vicinity to the tumor. The right liver artery can be divided close to its origin at the arteria hepatica propria. The necessity of the left hepatic artery to be preserved is no disadvantage, because of the generally extratumoral course of this artery at the left margin of the hepatoduodenal ligament. The portal bifurcation will be principally resected and therefore does not need not to be dissected, either. An end-to-end anastomosis of the portal trunk to the left portal vein branch will result in a more stretched course of this vessel and may avoid a kinking which can sometimes be observed after extended right-sided resection with preservation of the portal bifurcation.
Secondly, a parenchymal dissection between the left lateral (segments II and III) and left medial section (segments IV) will result in a small parenchymal dissection area. Moreover, the anatomical variability of the segmental ramification in this area is low. It is hardly ever necessary to anastomose more than the two orifices to the segments II and III, respectively.
Thirdly, the distance from the bifurcation of the main hepatic ducts to the ramification into the left lateral section may be as wide as 5 cm, whereas the corresponding distance on the right side usually measures less than 1 cm [12].
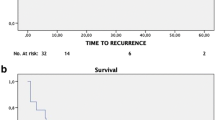
A multivariate analysis of 133 patients who had undergone resection of a hilar cholangiocarcinoma from September 1988 to January 2001 at our institution revealed the surgical radicality as the most important prognostic parameter. In addition, a lymphangiosis carcinomatosa, a perineural sheath infiltration, and the histopathological grading could be identified as significantly relevant for long-term survival. Figure 1 shows the actual survival rates after 133 resections of hilar cholangiocarcinomas according to the surgical radicality. Taking into account only those patients who had undergone a formally curative resection, a multivariate analysis revealed only one favorable prognostic parameter: a portal vein resection. In contrast, lymphangiosis carcinomatosa, perineural sheath infiltration, and histopathological grading did not have a significant impact on survival once a curative resection had been accomplished.
We have previously reported on the advantage of an additional resection of the portal vein bifurcation [13]. At that time, this finding was surprising because comparable analyses of, for example, pancreatic head resections with concomitant portal vein resections had frequently revealed an impaired prognosis and never a significant survival benefit in any multivariate analysis. Our favorable experience was all the more astonishing as we had generally not intended a no-touch technique by resecting the portal vein bifurcation, but we were driven to do so by a suspected portal vein infiltration; however, a true carcinomatous infiltration could only be substantiated in 20% of the respective specimens on histopathological examination, whereas perivascular fibrosis accounted for the remaining indurations. As a consequence, we have conceptualized this concomitant resection of the portal vein henceforth. Figure 2 shows the outcome after all right trisectionectomies, either with or without a concomitant portal vein resection. Meanwhile, a 5-year survival rate in the group of R0 right trisectionectomies with concomitant portal vein resection reaches an unexpectedly favorable figure of 72%. R0 right trisectionectomies without concomitant portal vein resection fares worse but still achieves a 5-year survival rate of 52% (data not shown).
The 5-year survival rates after right hemihepatectomies or left-sided liver resections were 23 and 18%, respectively (Fig. 3). These rates did not differ significantly and demonstrate that the resection margin has to be extended beyond the boundaries of a right hemihepatectomy towards the left hemiliver in order to achieve a benefit towards left-sided resections.
Formally, non-curative R1 resections did not fare worse in the hemihepatectomies when compared with R0 resections (data not shown). After right trisectionectomies with concomitant portal vein resection, 5-year survival figures were lower after R1 resections than after R0 resections but still reached 45%, which may raise doubts regarding the term non-curative resection or at least its clinical significance. The phenomenon of similar survival rates after R0 and R1 resections has already been described for solid liver tumors.
In colorectal metastases, the survival curves of 167 patients with a tumor-free liver resection margin exceeding 10 mm, 78 patients in whom it ranged from 5–9 mm, and 133 patients with a non-infiltrated resection margin of less than 4 mm, ran almost in parallel [14]. The most likely explanation for these findings is a too stringent criterion for a formally curative or R0 resection. The margin of the specimen which is finally evaluated histopathologically forms only part of a surgical safety area around a hepatic tumor mass. In addition, there are two more layers around the tumor contributing to the safety zone: the parenchymal dissection line and a coagulation field along the resection line of the liver remnant, each measuring approximately 1–3 mm. The tissue destruction within the parenchymal dissection line is usually created by an ultrasound tip and the coagulation field on the remnant liver tissue by infrared light. This additional resection margin can hardly be quantified and has not been considered in former retrospective analyses.
Caudate lobe resection
In centers of hepatobiliary surgery, it is widely accepted that liver resections for hilar cholangiocarcinoma should always include the caudate lobe (segment I) [15, 16]. Although it has never been proven that the concomitant resection of the caudate lobe resulted in a substantial survival benefit over the long term, it was a prime area of local recurrence after local resections. Again, the close proximity to the tumor is the most likely explanation for this phenomenon. The segment-I bile duct almost always drains directly into the hilar bifurcation or at least within a distance of 1 cm. Exceptions to this rule account for only 3% of all cases. Moreover, it is our impression that concomitant resections of the caudate lobe reduce the risk of a bile leakage from the parenchymal dissection field after extended right hepatic resections.
Perioperative mortality
Before considering extrahepatic bile duct resections without major liver resections as widely inefficient in the treatment of hilar cholangiocarcinoma, they found a wider application due to a low postoperative mortality. In fact, higher resectability and radicality rates after concomitant liver resection still go along with increased mortality rates. In our experience, the mortality rates after extrahepatic bile duct resections, hemihepatectomies and right trisectionectomies with portal vein resection are 0, 10, and 13%, respectively. The main cause of death after extended liver resection is liver insufficiency due to a lack of functioning parenchyma, all the more if a cholestatic alteration of the tissue is present.
Attempts to overcome this obstacle have aimed at enlarging the anticipated liver remnant volume already preoperatively in order to alleviate the postoperative nadir of liver function and to shorten the gap until its restoration.
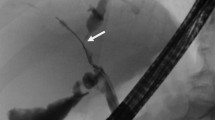
A preoperative hypertrophy of the future remnant liver, induced by unilateral portal vein embolization, has been shown to minimize the associated risk of postoperative liver failure [17]. Decompression of the biliary system may also be indicated to improve hepatocellular function. Former randomized trials did not demonstrate an advantage associated with preoperative external biliary drainage [18]; however, older studies were mainly comprised of bypass surgery and suffer from a low share of hepatectomies, i.e., the group which is most likely to have a benefit from preoperative biliary decompression. We use a modified approach with either internal or external biliary decompression exclusively of the remnant left lobe [19]. In addition, embolization of the right liver artery has been performed and demonstrated together with selective biliary decompression a significant effect on hypertrophy [20]; however, we cannot discriminate between the effects of unilateral biliary decompression and contralateral arterial embolization. In patients with particularly small left lateral sections, we use increasingly unilateral portal vein embolization which is the more substantial method.
Another strategy aims at preserving more liver tissue during resection while avoiding concessions to radicality; therefore, we have sometimes attempted to combine an extended right-sided resection in the inferior and perihilar regions of the liver with a parenchyma-sparing almost right hemihepatectomy-like resection in the superior parts of the liver. Such a combination is frequently possible because the segment-IV ramification of the right hepatic duct, the portal vein branch and the arterial supply to segment IV generally run to the left first reaching the umbilical fissure where these structures then enter the parenchyma and run towards the right into segment IV; therefore, an extension of the resection line towards the umbilical fissure, i.e., the left-sided intersection, is feasible as in a right trisectionectomy while maintaining considerable portions of segment IV distant to the hilum.
Lymphadenectomy
Bismuth et al. described positive lymph nodes in hilar cholangiocarcinoma to be a less important prognostic parameter than in other gastrointestinal cancers [21]. Other reports, also involving more aggressive approaches, are not conclusive in this respect as well [17, 22].
Even more uncertainty prevails regarding the role of a lymphadenectomy, which is so far hardly supported by clinical data. In our concept, the lymph nodes of the hepatic hilum and the hepatoduodenal ligament are en bloc resected with the tumor. In addition, the pancreatoduodenal and the para-aortal lymph nodes around the celiac trunk are resected for staging. In contrast to previous reports, in our experience there is a significant difference in long-term survival after resection when comparing patients with positive or negative lymph nodes (Fig. 4).
Kitagawa et al., from the Nagoya group of Nimura, showed that an extended lymphadenectomy involving the para-aortal lymph nodes had a benefit in patients in whom these lymph nodes were infiltrated without microscopic signs of an infiltration [23]. Their study involved 110 patients after resection of hilar cholangiocarcinoma with 5-year survival rates of 31%, if the lymph nodes were negative. In patients suffering from a local or a para-aortal lymph node infiltration, the 5-year survival rates were 15 and 12%, respectively. Examining in further detail the group with positive para-aortal lymph nodes, they could identify that in 7 of these 19 patients an infiltration was macroscopically undetectable. Comparing these two groups, i.e., patients with macroscopically detectable infiltration to patients with a macroscopically undetectable infiltration of para-aortic lymph nodes, the authors found no 5-year survival at all compared with a rate of 29%, respectively.
The same group has also provided evidence that lymph node micrometastases do not have a survival impact on patients with otherwise node-negative hilar cholangiocarcinoma [24]. An immunohistochemical examination of lymph nodes has been suggested to improve the pathological staging of gastrointestinal cancers, such as, for example, esophageal cancer [25]. Tojima et al. [24] had detected lymph node micrometastases in 11 of 45 patients or in 13 of 954 lymph nodes (1.4%) examined. Survival curves were essentially similar between patients with and without micrometastases. In addition, the grade of micrometastases did not show any impact on survival in a multivariate analysis; therefore, the authors did not recommend extensive lymph node sectioning with keratin immunostaining for prognostic evaluation.
References
Okuda K, Kubo Y, Okazaki N, Arishima T, Hashimoto M (1977) Clinical aspects of intrahepatic bile duct carcinoma including hilar carcinoma: a study of 57 autopsy-proven cases. Cancer 39:232–246
Bhuiya M-R, Nimura Y, Kamiya J, Kondo S, Fukata S, Hayakawa N, Shionoya S (1992) Clinicopathologic studies on perineural invasion of bile duct carcinoma. Ann Surg 215:344–349
Weinbren K, Mutum S-S (1983) Pathological aspects of cholangiocarcinoma. J Pathol 139:217–238
Born P, Rosch T, Willkomm G, Sandschin W, Fitz N, Weigert N, Ott R, Frimberger E, Allescher H, Classen M (1999) Initial experience with a new Yamakawa-type prosthesis for long-term percutaneous transhepatic drainage. Endoscopy 31:748–750
Kaufman S-L (1995) Percutaneous palliation of unresectable pancreatic cancer. Surg Clin North Am 75:989–999
Schlitt H-J, Weimann A, Klempnauer J, Oldhafer K-J, Nashan B, Raab R, Pichlmayr R (1999) Peripheral hepatojejunostomy as palliative treatment for irresectable malignant tumors of the liver hilum. Ann Surg 229:181–186
Jarnagin W-R, Fong Y, DeMatteo R-P, Gonen M, Burke E-C, Bodniewicz BSJ, Youssef BAM, Klimstra D, Blumgart L-H (2001) Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 234:507–517
Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Shimizu Y, Kato A, Nakamura S, Omoto H, Nakajima N, Kimura F, Suwa T (1998) Aggressive surgical approaches to hilar cholangiocarcinoma: hepatic or local resection? Surgery 123:131–136
Nimura Y, Kamiya J, Kondo S, Nagino M, Uesaka K, Oda K, Sano T, Yamamoto H, Hayakawa N (2000) Aggressive preoperative management and extended surgery for hilar cholangiocarcinoma: Nagoya experience. J Hepatobiliary Pancreat Surg 7:155–162
Mittal B, Deutsch M, Iwatsuki S (1985) Primary cancers of the extrahepatic biliary passages. Int J Radiat Oncol Biol Phys 11:849–855
Kawarada Y, Isaji S, Taoka H, Tabata M, Das B-C, Yokoi H (1999) S4a+S5 with caudate lobe (S1) resection using the Taj Mahal liver parenchymal resection for carcinoma of the biliary tract. J Gastrointest Surg 3:369–373
Bismuth H (1982) Surgical anatomy and anatomical surgery of the liver. World J Surg 6:3–9
Neuhaus P, Jonas S, Bechstein W-O, Lohmann R, Radke C, Kling N, Wex C, Lobeck H, Hintze R (1999) Extended resections for hilar cholangiocarcinoma. Ann Surg 230:808–818
Scheele J, Altendorf-Hofmann A, Stangl R, Schmidt K (1996) Surgical resection of colorectal liver metastases: Gold standard for solitary and radically resectable lesions. Swiss Surg (Suppl) 4:4–17
Iwasaki Y, Okamura T, Ozaki A, Todoroki T, Takase Y, Ohara K, Nishimura A, Otsu H (1986) Surgical treatment for carcinoma at the confluence of the major hepatic ducts. Surg Gynecol Obstet 162:457–464
Mizumoto R, Kawarada Y, Suzuki H (1986) Surgical treatment of hilar carcinoma of the bile duct. Surg Gynecol Obstet 162:153–158
Makuuchi M, Thai BL, Takayasu K, et al (1990) Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery 107:521–527
Hatfield ARW, Tobias R, Terblanche J, et al (1982) Preoperative external biliary drainage in obstructive jaundice: a prospective controlled clinical trial. Lancet 2:896–899
Hintze R-E, Abou-Rebyeh H, Adler A, Veltzke-Schlieker W, Felix R, Wiedenmann B (2001) Magnetic resonance cholangiopancreatography-guided unilateral endoscopic stent placement for Klatskin tumors. Gastrointest Endosc 53:40–46
Vogl T-J, Balzer J-O, Dette K, Hintze R, Pegios W, Maurer J, Keck H, Neuhaus P, Felix R (1998) Initially unresectable hilar cholangiocarcinoma: hepatic regeneration after transarterial embolization. Radiology 208:217–222
Bismuth H, Nakache R, Diamond T (1992) Management strategies in resection for hilar cholangiocarcinoma. Ann Surg 215:31–38
Kosuge T, Yamamoto J, Shimada K, Yamasaki S, Makuuchi M (1999) Improved surgical results for hilar cholangiocarcinoma with procedures including major hepatic resection. Ann Surg 230:663–671
Kitagawa Y, Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H, Hayakawa N, Nimura Y (2001) Lymph node metastasis from hilar cholangiocarcinoma: audit of 110 patients who underwent regional and paraaortic node dissection. Ann Surg 233:385–392
Tojima Y, Nagino M, Ebata T, Uesaka K, Kamiya J, Nimura Y (2003) Immunohistochemically demonstrated lymph node micrometastasis and prognosis in patients with otherwise node-negative hilar cholangiocarcinoma. Ann Surg 237:201–207
Izbicki J-R, Hosch S-B, Pichlmeier U, Rehders A, Busch C, Niendorf A, Passlick B, Broelsch C-E, Pantel K (1997) Prognostic value of immunohistochemically identifiable tumor cells in lymph nodes of patients with completely resected esophageal cancer. N Engl J Med 337:1188–1194
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Neuhaus, P., Jonas, S., Settmacher, U. et al. Surgical management of proximal bile duct cancer: extended right lobe resection increases resectability and radicality. Langenbecks Arch Surg 388, 194–200 (2003). https://doi.org/10.1007/s00423-003-0383-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-003-0383-5