Abstract
Objective
To review our surgical experience with hilar cholangiocarcinoma in the “new era.”
Methods
The medical records of 428 patients with hilar cholangiocarcinoma who underwent treatment between 2001 and 2008 at the First Department of Surgery, the Nagoya University Hospital, were retrospectively reviewed.
Results
Of the 428 patients, 298 (70%) underwent surgical resection (R0, n = 220; R1, n = 70; R2, n = 8). Portal vein resection was performed in 111 (37%) patients, and hepatic artery resection was performed in 53 (18%) patients. Several different types of postoperative complications occurred in a total of 129 (43%) patients and led to 6 (2%) deaths. Of the 298 resected tumors, 206 (69%) were extrahepatic type tumors, and the remaining 92 (31%) were intrahepatic type tumors. Using the Bismuth classification criteria, we identified 15 (5%) type I, 21 (7%) type II, 120 (40%) type III, and 142 (48%) type IV tumors. The overall 1-, 3-, and 5-year survival rates for all 298 patients were 77, 49, and 42%, respectively. The survival rates were highest among the 197 patients with pM0 disease who underwent R0 resection. Patients in this subgroup had a 5-year survival rate of 52%. The 5-year overall survival rate for the 55 patients with pM0 disease who underwent R1 resection was 32%. The survival rate for patients who had pM1 disease and/or underwent R2 resection was the worst of all the subgroups, but was nonetheless significantly better than that of patients with unresectable tumors. The survival rate for patients who underwent vascular resection and reconstruction was unexpectedly better, with 5-year survival of >20%.
Conclusions
The surgical approach to hilar cholangiocarcinoma has become more challenging in the new era. Nevertheless, surgical outcomes have been improved, with decreased morbidity and mortality rates being observed. Long-term survival has also steadily improved. These findings indicate that biliary surgeons should use an aggressive surgical strategy to treat this intractable disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many previous studies on hilar cholangiocarcinoma have shown that aggressive surgery with the aim of performing a curative resection can offer a better chance for long-term survival than conservative therapy [1–10]. In this “new era,” the perioperative management of hilar cholangiocarcinoma has improved markedly. Several advances in surgical techniques and technology have contributed to these improvements. For example, multidetector-row computed tomography (MDCT) has made it possible to accurately diagnose the extent of cancer [11, 12]. Portal vein embolization (PVE) has certainly increased the safety of extended hepatectomy [13–15]. Preoperative bile replacement during external drainage [16] and perioperative symbiotic treatment [17, 18] have reduced postoperative infectious complication rates. Thanks to these recent advances in perioperative management, the surgical outcomes of patients with hilar cholangiocarcinoma may have improved. Therefore, the aim of this study was to review our surgical experiences with hilar cholangiocarcinoma in the “new era” by focusing on the outcomes of patients treated over the past 8 years.
Patients
Between 2001 and 2008, 428 patients with hilar cholangiocarcinoma were treated at the First Department of Surgery, Nagoya University Hospital. Of them, 272 were men and 156 were women, with an average age of 65 years (range 30–84 years). There are two types of hilar cholangiocarcinoma: one is “extrahepatic” cholangiocarcinoma, which arises from the large hilar bile ducts, and the other is “intrahepatic” cholangiocarcinoma, which has an intrahepatic component and involves the hepatic hilus. These two tumor types have similar features on cholangiography and require similar types of surgical management that involve resection of the hepatic duct confluence [19]. Therefore, the present study included patients with both extrahepatic and intrahepatic type cholangiocarcinoma [10, 23–25, 27].
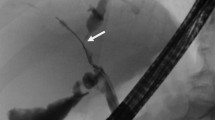
Ultrasonography and MDCT were used in all patients for preoperative tumor staging [11, 12]. Percutaneous transhepatic biliary drainage (PTBD) or endoscopic nasobiliary drainage (ENBD) was performed in all of patients with obstructive jaundice. Previously multiple bilateral drainage was often performed using PTBD [20]. In the past 2–3 years, however, unilateral drainage by ENBD was used whenever possible. Most patients who were planned to undergo extended hepatectomy (resection of 60% or more of the liver) underwent PVE 2–3 weeks before surgery, according to the previously reported method [13–15].
Based on the results of the diagnostic imaging, the type of hepatectomy was planned as follows: right hemihepatectomy was applied to Bismuth type I, II, and IIIa tumors [21]; left hemihepatectomy or trisectionectomy to type IIIb tumors; and right or left trisectionectomy or central bisectionectomy to type IV tumors [22]. Applied standard surgical technique involved resection of the connective tissue in the hepatoduodenal ligament with lymph node dissection [23, 24], hepatectomy with en bloc resection of the caudate lobe and extrahepatic bile duct [25], aggressive vascular resection when macroscopic tumor invasion was suspected at surgery [26–28], and transection of the intrahepatic bile duct with an optimal margin of 1 cm [29] or else at the most proximal point that was possible. When cancer extended to the lower bile duct, combined pancreatoduodenectomy was also performed [30, 31]. Surgery was usually abandoned if paraaortic lymph node metastasis, liver metastasis, and/or peritoneal seeding was found, but resection was done under these circumstances in some patients when it was deemed not too risky and likely to improve the patient’s quality of life.
All tumors were staged according to the latest AJCC tumor (T) node (N) metastasis (M) classification system for “extrahepatic bile duct cancer” [32]. Therefore, the tumors of patients with intrahepatic type cholangiocarcinoma who had intrahepatic metastases were classified as having distant metastasis (M1).
Categorical variables were compared using Fisher’s exact test. Survival was calculated using the Kaplan–Meier method and compared by the log-rank test. A p value <0.05 was considered statistically significant.
Results
Surgery
Of the 428 study patients, 130 patients underwent conservative treatment with or without biliary drainage, due to distant metastasis, locally far advanced tumors, and/or poor hepatic function. The remaining 298 patients underwent surgical resection with curative intent, resulting in a resectability rate of 70%.
The surgical procedures performed are summarized in Table 1. Several different types of hepatectomy were performed in 293 (98%) patients, while bile duct resection without hepatectomy was performed in only 5 (2%) patients. Concomitant portal vein resection and reconstruction was performed in 111 (37%) patients, and hepatic artery resection and reconstruction were performed in 53 (18%) patients. In the 293 patients who underwent hepatectomy, operative time was 644 ± 146 min (range 353–1150 min), and blood loss was 1862 ± 1186 ml (range 385–11115 ml). Thanks to preoperative blood donation [33], 205 (70%) of the 293 hepatectomized patients did not require transfusions of unheated blood products (i.e., MAP and/or FFP) during the intra- and postoperative period.
According to surgical curability, R0, R1, and R2 resections were performed in 220 (74%), 70 (23%), and 8 (3%), respectively.
Morbidity and mortality
Several kinds of postoperative complications occurred in a total of 129 (43%) patients (Table 2). Intraabdominal abscess, observed in 53 (18%) patients, was the most common complication, followed by wound sepsis (13%) and bile leakage from the liver stump (11%). Liver failure, defined as a serum total bilirubin concentration of >10 mg/dl [34], was observed in 18 (6%) patients. Portal vein thrombosis following portal vein resection and reconstruction occurred in five (2%) patients. Of these five patients, three underwent re-laparotomy with thrombectomy. Six (2%) patients died of postoperative complication(s) on days 7, 15, 20, 56, 71, and 80, respectively, while the remaining 292 patients were discharged from the hospital in good condition. The cause of death among the six nonsurvivors was liver failure following portal vein thrombosis (n = 4), liver failure with sepsis (n = 1), and intraabdominal hemorrhage (n = 1).
Tumor type, pathology, and stage
Of the 298 resected tumors, 206 (69%) were extrahepatic type tumors, and the remaining 92 (31%) were intrahepatic type tumors [12]. According to the Bismuth classification criteria, types I, II, III, and IV tumors were found in 15 (5%), 21 (7%), 120 (40%), and 142 (48%) patients, respectively. The histological differentiation of the tumors was G1 in 86 (29%) patients, G2 in 176 (59%) patients, and G3 in 36 (12%) patients.
According to the TNM staging system, pT1 disease was identified in 15 (5%) patients, pT2 disease in 63 (21%) patients, pT3 disease in 120 (40%) patients, and pT4 disease in 100 (34%) patients. One hundred thirty-one (44%) patients had pN1 disease, and 42 (14%) patients had pM1 disease. The final tumor stage was IA in 15 (5%) patients, IB in 44 (15%), IIA in 58 (19%), IIB in 53 (18%), III in 86 (29%), and IV in 42 (14%).
Survival
The overall 1-, 3-, and 5-year survival rates were 77, 49, and 42% for all 298 patients who underwent resection, all of which were significantly better than the survival rates of the 130 patients who had unresectable tumors (Fig. 1).
Of the 298 resected patients, the survival rate was highest among the 197 patients with pM0 disease who underwent R0 resection. This subgroup had a 5-year survival rate of 52%. The 5-year survival rate for the 55 patients with pM0 disease who underwent R1 resection was somewhat lower at 32%. The survival rate for patients who had pM1 disease and/or underwent R2 resection was worst, but significantly better than that for patients with unresectable tumors (Fig. 2). In patients with pM0 disease, the survival rates were significantly different according to presence or absence of lymph node metastasis: when no lymph node metastases were observed, the survival rates were satisfactory, with a 5-year survival of 62% (Fig. 3).
Survival rates for patients who underwent vascular resection were unexpectedly better: the 3- and 5-year survival rates were 37 and 23%, respectively, for the 69 patients who underwent portal vein resection alone and 38 and 33%, respectively, for the 53 patients who underwent hepatic artery resection with (n = 42) or without portal vein resection (n = 11) (Fig. 4).
Discussion
Ever since one (YN) of the authors first began performing surgical treatment for hilar cholangiocarcinoma in 1977, we have performed aggressive surgeries to treat this intractable disease. In this “new era,” we have further expanded the surgical indications for hilar cholangiocarcinoma. PVE has made a remarkable contribution to the expansion of surgical indications [13–15]. This radiological intervention has certainly increased the safety of extended hepatectomy, and, as a result, posthepatectomy liver failure, the most serious complication observed after extended hepatectomy, has markedly decreased. In the present study, 174 (58%) patients underwent extended hepatectomy including right or left trisectionectomy and right hepatectomy (i.e., resection of >50% of the liver). The incidence of liver failure after hepatectomy was only 6% in this study, which was significantly lower than the previous incidence of >20% that we reported in previous studies [10, 30, 34].
Another contribution that allowed expansion of the surgical indications was the addition of aggressive vascular resections. Portal vein resection and reconstruction are now considered a routine procedure that is performed, when necessary, in high-volume centers. So far we have also performed portal vein resection in more than 200 patients with hepatobiliary malignancies and have reported their surgical outcomes [26, 27]. In addition to portal vein resection, the hepatic artery resection and reconstruction procedure was adopted about 10 years ago, and its use has increased each year. In the present series, a total of 53 (17%) patients underwent concomitant hepatic artery resection and reconstruction with or without portal vein resection. Despite the risky nature of this procedure, only 1 of the 53 patients died of complications postoperatively, and 2 patients survived more than 5 years after surgery. Several authors reported dismal surgical outcomes of hepatectomy with concomitant hepatic artery resection [28, 35, 36]. However, our satisfactory results may encourage hepatobiliary surgeons to attempt this challenging surgical procedure.
In patients with pM0 disease who underwent R0 resection, 31 patients survived for more than 5 years, resulting in a 52% 5-year survival rate. When no lymph node metastases were observed, the survival rate was higher, with 5-year survival of over 60%. In contrast, in patients with lymph node metastases, the 5-year survival rate was only 21%. Previously, we reported that lymph node micrometastasis has no impact on survival in patients with otherwise negative lymph nodes and that extended lymph node dissection may provide a survival benefit in patients with hilar cholangiocarcinoma [23, 24]. However, these results suggest that surgery alone may be insufficient to successfully treat hilar cholangiocarcinoma with lymph node metastases, even if an R0 resection is achieved. Therefore, we are now conducting a nationwide randomized controlled trial to examine the efficacy of adjuvant chemotherapy (Bile duct Cancer Adjuvant Trial, BCAT).
In summary, the surgical approach to hilar cholangiocarcinoma in the “new era” has become more challenging with the addition of concomitant portal vein and/or hepatic artery resection. Nevertheless, thanks to advances in perioperative management, surgical outcomes have improved, and morbidity and mortality rates have decreased. Long-term survival has also steadily improved. These findings indicate that we, as biliary surgeons, should use an aggressive surgical strategy to treat this intractable disease.
References
Launois B, Terblanche J, Lakehal M, Catheline JM, Bardaxoglou E, Landen S, et al. Proximal bile duct cancer. High respectability rate and 5-year survival. Ann Surg. 1999;230:266–75.
Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, King N, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg. 1999;230:808–19.
Lee SG, Lee YJ, Park KM, Hwang S, Min PC. One hundred and eleven liver resections for hilar cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 2000;7:135–41.
Tsao JI, Nimura Y, Kamiya J, Hayakawa N, Kondo S, Nagino M, et al. Management of hilar cholangiocarcinoma: comparison of an American and a Japanese experience. Ann Surg. 2000;232:166–74.
Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz J, et al. Staging, respectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001;234:507–19.
Seyama Y, Kubota K, Sano K, Noie T, Takayama T, Kosuge T, et al. Long-term outcome pf extended hemihepatectomy for hilar bile duct cancer with no mortality and high survival rate. Ann Surg. 2003;238:73–83.
Kawasaki S, Imamura H, Kobayashi A, Noike T, Miwa S, Miyagawa S, et al. Results of surgical resection for patients with hilar bile duct cancer: application of extended hepatectomy after biliary drainage and hemihepatic portal vein embolization. Ann Surg. 2003;238:84–92.
Kondo S, Hirano S, Ambo Y, Tanaka E, Okushiba S, Morikawa T, et al. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Ann Surg. 2004;240:95–101.
Sano T, Shimada K, Sakamoto Y, Yamamoto J, Yamasaki S, Kosuge T. One hundred two consecutive hepatobiliary resections for perihilar cholangiocarcinoma with zero mortality. Ann Surg. 2006;244:240–7.
Nishio H, Nagino M, Nimura Y. Surgical management of hilar cholangiocarcinoma: the Nagoya experience. HPB. 2005;7:259–62.
Sugiura T, Nishio H, Nagino M, Senda Y, Ebata Y, Yokoyama Y, et al. Value of multidetector-row computed tomography in diagnosis of portal vein invasion by perihilar cholangiocarcinoma. World J Surg. 2008;32:1478–84.
Senda Y, Nishio H, Oda K, Yokoyama Y, Ebata T, Igami T, et al. Value of multidetector row CT in the assessment of longitudinal extension of cholangiocarcinoma-correlation between MDCT and microscopic findings. World J Surg. 2009;33:1459–67.
Nagino M, Nimura Y, Kamiya J, Kondo S, Kanai M. Selective percutaneous transhepatic embolization of the portal vein in preparation for extensive liver resection: the ipsilateral approach. Radiology. 1996;200:559–63.
Nagino M, Nimura Y, Kamiya J, Kondo S, Uesaka K, Kin Y, et al. Right or left trisegment portal vein embolization before hepatic trisegmentectomy for hilar cholangiocarcinoma. Surgery. 1995;117:677–81.
Nagino M, Kamiya J, Nishio H, Ebata T, Arai T, Nimura Y. Two hundred forty consecutive portal vein embolizations before extended hepatectomy for biliary cancer: surgical outcome and long-term follow-up. Ann Surg. 2006;243:364–72.
Kamiya S, Nagino M, Kanazawa H, Komatsu S, Mayumi T, Takagi K, et al. The value of bile replacement during external biliary drainage: an analysis of intestinal permeability, integrity, and microflora. Ann Surg. 2004;239:510–7.
Kanazawa H, Nagino M, Kamiya S, Komatsu S, Mayumi T, Takagi K, et al. Synbiotics reduce postoperative infectious complications: a randomized controlled trial in biliary cancer patients undergoing hepatectomy. Langenbecks Arch Surg. 2005;390:104–13.
Sugawara G, Nagino M, Nishio H, Ebata T, Takagi K, Asahara T, et al. Perioperative symbiotic treatment to prevent postoperative infectious complications in biliary cancer surgery: a randomized controlled trial. Ann Surg. 2006;244:706–14.
Ebata T, Kamiya J, Nishio H, Nagasaka T, Nimura Y, Nagino M. The concept of perihilar cholangiocarcinoma is valid. Br J Surg. 2009;96:926–34.
Nagino M, Nimura Y, Kamiya J, Kondo S, Kanai M, Miyachi M, et al. Preoperative management of hilar cholangiocarcinoma. J Hepatobiliary Pancreat Surg. 1995;2:215–23.
Ikeyama T, Nagino M, Oda K, Ebata T, Nishio H, Nimura Y. Surgical approach to Bismuth type I and II hilar cholangiocarcinomas: audit of 54 consecutive cases. Ann Surg. 2007;246:1052–7.
Nagino M, Kamiya J, Arai T, Nishio H, Ebata T, Nimura Y. “Anatomic” right hepatic trisectionectomy (extended right hepatectomy) with caudate lobectomy for hilar cholangiocarcinoma. Ann Surg. 2006;243:28–32.
Kitagawa Y, Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H, et al. Lymph node metastasis from cholangiocarcinoma: audit of 110 patients who underwent regional and paraaortic node dissection. Ann Surg. 2001;233:385–92.
Tojima Y, Nagino M, Ebata T, Uesaka K, Kamiya J, Nimura Y. Immunohistochemically demonstrated lymph node micrometastasis and prognosis in patients with otherwise node-negative hilar cholangiocarcinoma. Ann Surg. 2003;237:201–7.
Nimura Y, Hayakawa N, Kamiya J, Kondo S, Shionoya S. Hepatic segmentectomy with caudate lobe resection for bile duct carcinoma of the hepatic hilus. World J Surg. 1990;14:535–44.
Nimura Y, Hayakawa N, Kamiya J, Maeda S, Kondo S, Yasui A, et al. Combined portal vein and liver resection for carcinoma of the biliary tract. Br J Surg. 1991;78:727–31.
Ebata T, Nagino M, Kamiya J, Uesaka K, Nagasaka T, Nimura Y. Hepatectomy with portal vein resection for hilar cholangiocarcinoma: audit of 52 consecutive cases. Ann Surg. 2003;238:720–7.
Miyazaki M, Kato A Ito H, Kimura F, Shimizu H, Ohtsuka N, et al. Combined vascular resection in operative resection for hilar cholangiocarcinoma: does it work or not? Surgery. 2007;141:581–8.
Ebata T, Watanabe H, Ajioka Y, Oda K, Nimura Y. Pathological appraisal of lines of resection for bile duct carcinoma. Br J Surg. 2002;89:1260–7.
Nimura Y, Hayakawa N, Kamiya J, Maeda S, Kondo S, Yasui A, et al. Hepatopancreatoduodenectomy for advanced carcinoma of the biliary tract. Hepatogastroenterology. 1991;38:170–5.
Ebata T, Nagino M, Nishio H, Arai T, Nimura Y. Right hepatopancreatoduodenectomy: improvements over 23 years to attain acceptability. J Hepatobiliary Pancreat Surg. 2007;14:131–5.
Greene FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, et al., editors. AJCC cancer staging manual. 6th ed. New York: Springer; 2002.
Nagino M, Kamiya J, Arai T, Nishio H, Ebata T, Nimura Y. One hundred consecutive hepatobiliary resections for biliary malignancy: preoperative blood donation, blood loss, transfusion, and outcome. Surgery. 2005;137:148–55.
Nagino M, Kamiya J, Uesaka K, Sano T, Yamamoto H, Hayakawa N, et al. Complications of hepatectomy for hilar cholangiocarcinoma. World J Surg. 2001;25:1277–83.
Gerhards MF, Gulik TM, de Wit LT, Obertop H, Gouma DJ. Evaluation of morbidity and mortality after resection for hilar cholangiocarcinoma—a single center experience. Surgery. 2000;127:395–404.
Sakamoto Y, Sano T, Shimada K, Kosuge T, Kimata Y, Sakuraba M, et al. Clinical significance of reconstruction of the right hepatic artery for biliary malignancy. Langenbeck’s Arch Surg. 2006;391:203–8.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Igami, T., Nishio, H., Ebata, T. et al. Surgical treatment of hilar cholangiocarcinoma in the “new era”: the Nagoya University experience. J Hepatobiliary Pancreat Sci 17, 449–454 (2010). https://doi.org/10.1007/s00534-009-0209-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00534-009-0209-0