Abstract
Robotic-assisted knee arthroplasty has become increasingly commercially available as both technology developers and surgeons attempt to address specific limitations of conventional jig-based alignment techniques in order to improve resection accuracy and precision. Semi-active and passive systems predominate in the North American and European markets and can provide surgeons additional instruments for intraoperative calibration and balance assessment or directly assist in performing personalized resections. Recently published and ongoing clinical investigations seek to determine if robotic assistance may result in improved radiographic or clinical outcomes for patients undergoing either unicompartmental or total knee arthroplasty. A number of studies evaluating conventional and robotic-assisted knee arthroplasty did not identify significant radiographic or clinical outcome differences, though heterogeneity in robotic system design and application may limit the generalization of focused studies. Conversely, some studies that identified significant differences noted that robotic-assisted knee arthroplasty may be associated with fewer alignment outliers as well as increased surgical time—at least initially for unfamiliar surgeons. Further limitations include limited follow-up for newer systems on the market as well as the associated variety of arthroplasty implants and authors’ surgical techniques. Future studies will help surgeons and patients determine if intraoperative robotic assistance may be beneficial in total knee arthroplasty.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Robotics
- Robotic surgery
- Robotic assisted
- Total knee arthroplasty
- Unicompartmental knee arthroplasty
- Robot-assisted total knee arthroplasty
- Robot-assisted unicompartmental knee arthroplasty
- TKA
- UKA
- RATKA
3.1 Evolution of Robotic Arthroplasty
Surgical technology has developed increasing capabilities over the past 30 years, and robotic-assisted arthroplasty is one of many areas that have attracted significant interest from both patients and surgeons alike. Historically, alignment in total knee arthroplasty (TKA) has been based on preoperative radiographs combined with intraoperative assessments of deformity and alignment jigs that utilize either the anatomic axis—provided by intramedullary guides—or extramedullary and anatomic bony landmarks. While practical, conventional jigs and alignment techniques may be limited by variation in patient anatomy secondary to natural changes or progressive deformity from osteoarthritis [1]. Since the implementation of ROBODOC in 1992 for hip arthroplasty, proponents and creators of robotic systems for joint arthroplasty claim that implementation of these systems improves accuracy in bone cut selection and improves precision in cut execution [2]. Current robotic and computer-navigated knee arthroplasty systems available on the market today encompass a number of different technologies designed to assist surgeons with implanting components in the optimal alignment for a balanced knee with restored kinematics. With a prevalence of 4.7 million individuals with knee arthroplasties in the US population and increasing annual numbers, the evolution and adoption of technologically assisted surgery have broad potential to impact arthroplasty outcomes for thousands of patients every year [3].
3.1.1 Patient Satisfaction and Goals of Robotic Design
Patient satisfaction after total knee arthroplasty may be dependent on a number of patient-specific and technical factors. Despite decades of component design improvements and pre- and postoperative pathway optimization, 10–20% of patients in many studies still endorse dissatisfaction [4,5,6,7]. Common causes of dissatisfaction include persistent pain, stiffness, swelling, as well as subjective feelings of poor function [8]. The surgeon’s role for maximizing patient satisfaction, in addition to setting appropriate expectations regarding the surgical recovery, rehabilitation process, and functional goals, is to provide a technically precise and well-balanced knee that provides near-native kinematics while minimizing soft-tissue injury and complication risks [9]. Robotic assistance thus aims to facilitate the surgeon’s task through evaluation and planning as well as surgical execution.
3.1.2 Surgeon Interest
Unicompartmental knee arthroplasty (UKA) is reported to have higher rates of patient satisfaction and return to sport than TKA but overall is less commonly performed [10, 11]. Surgeons and patients may have concerns regarding the longevity of UKAs compared to TKAs, as analyses of the English/Welsh, Australian, Swedish, and Finnish arthroplasty registries have each revealed lower revision-free survival of UKAs, ranging from 80% to 90% survival rates at 7–10-year follow-up [12,13,14]. Additional studies of English/Welsh and Nordic registries noted volume-dependent outcomes, with high-volume centers achieving improved UKA survival at 10 years [15, 16]. Whether loosening occurs due to implant design, surgeon technique, or excessive overcorrection or undercorrection of deformity, proponents of robot-assisted arthroplasty claim improved accuracy and precision with component implantation may help surgeons make and execute their intraoperative alignment plan and improve implant survival for patients [17].
3.1.3 Robotic Technologies
Robotic-assisted total knee arthroplasty (RATKA) has been used to describe active (autonomous), semi-active (semi-autonomous, haptic, or tactile systems), and passive systems for assistance with the distal femur and proximal tibia bone cuts in unicompartmental and total knee arthroplasty [18, 19]. Understanding the differences in development, technique, and the unique evidence supporting each technology is important for informed decision-making for both patients and surgeons (Table 3.1).
Passive systems include navigation for surgical planning or active cutting guides and may also provide intraoperative feedback. Adoption of robotic systems overall has progressed slowly as surgeons and patients look for results of early implementation before investing in costly technology with potentially limited returns [20], indicating to many the profound impact that robotic arthroplasty has had in orthopedic surgery markets and likely will continue to have for the foreseeable future.
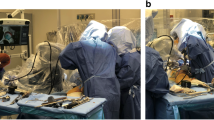
Semi-active systems are currently the most prevalent within the US market and are commonly referred to as haptic or tactile systems, as they utilize robotic guidance while retaining surgeon control within the planned resection [21]. Semi-active systems currently in production include Mako (Stryker, Mahwah, NJ; FDA cleared in 2015), Navio PFS (designed by Blue Belt Technologies, Plymouth, MN, and subsequently bought by Smith & Nephew, Memphis, TN; FDA cleared in 2017), as well as Smith & Nephew’s second-generation system, CORI. The Mako system is approved for both hip and knee arthroplasty, has both saw and burr end-instrument capabilities, and is based on a preoperative computed tomography (CT) scan for resection planning. Alternatively, the Navio PFS and subsequently the CORI systems marketed by Smith & Nephew do not require preoperative imaging; rather, surface mapping of the patient’s anatomy is performed intraoperatively in conjunction with balance assessment in order to guide resection performed selectively with a burr as the end instrument. Recently, the Velys system (DePuy Synthes, subs. of Johnson & Johnson, Warsaw, IN) received FDA 510(k) clearance in 2021, originally designed by French company Orthotaxy (Paris, France). The Velys system also does not require preoperative imaging. Similar to the Navio PFS and CORI systems , it uses a saw for its end instrument compared to the burr used by the two Smith & Nephew systems. Most semi-active systems use a robotic arm attached to an oscillating saw or burr, together providing a constrained resection path for the surgeon to employ. All the above systems currently in production, Mako, Navio PFS, Cori, and Velys, are closed systems that exclusively use implants from their distributors.
Two other semi-active systems currently in production, ROSA (Zimmer Biomet, Warsaw, IN) and OMNIBotics (Corin, Tampa, FL), use cutting guides as their end instrument, rather than cutting instruments such as saws or burrs used by the other semi-active systems. The ROSA system was originally designed by Medtech (Montpellier, France) for navigational use in orthopedic surgery, including spinal instrumentation, and for knee arthroplasty and is able to guide resection based on preoperative radiographs or be used in an imageless fashion. The OMNIBotics system was also initially developed in France, known as the Praxiteles system by Praxim, before it was purchased by OMNIlife (East Taunton, MA) and subsequently by Corin.
Active, autonomous robotic systems are able to perform bone cuts independently under observation of the surgeon, who first performs the approach and calibration. Active RATKAs are less commonly used, as early results with the CASPAR and ROBODOC systems in Europe and Korea in the 2000s reported prolonged operative times and concerns regarding early postoperative complications [22, 23]. Current autonomous systems include iBlock (formerly Praxiteles; OMNIlife Science, East Taunton, MA) and TSolution-One (formerly ROBODOC; Think Surgical Inc., Fremont, CA; previously Curexo Technology; FDA cleared in 2019). Currently, there is no available clinical data published for the TSolution-One.
3.1.4 Other Technologies
In addition to proper bony resection, soft-tissue and ligamentous balancing is essential for restorative knee function. Instability and stiffness are commonly cited reasons for dissatisfaction by patients after total knee arthroplasty [4,5,6, 8, 9]. As most prosthetic implants are designed with fixed medial and lateral widths, it is paramount for the surgeon to properly assess and balance the medial and lateral resection gaps. Most commonly this can be performed with variable-thickness blocks that can be subjected to varus and valgus stress to assess for opening or gapping greater on either medial or lateral aspects as an indicator for an inadequately balanced knee. Manual techniques relying on tactile feel may be subject to inter-surgeon variability [24, 25]. New technologies have been developed to assist with this portion of total and unicompartmental knee arthroplasty as well, with products currently commercially available to quantify the force transmitted across the knee. Verasense (Orthosensor Inc., Dania Beach, FL) is a device that provides force data when used in place of the polyethylene liner insert, as well as dynamic measurements of rollback and stability. Verasense may be used with trial components prior to final component implantation to determine if additional bony resection needs to be made or after final component implantation to determine necessity of soft-tissue releases.
In a trial of 84 patients who underwent TKA using Verasense, Cho et al. found that 36% of patients after standard measured resection had a balanced knee with <15 lbs. difference between medial and lateral compartments. After force assessment with Verasense and subsequent modified gap balancing in 66 patients based on Verasense results, 94% of knees were balanced [26]. No comparison was made for gap balancing between Verasense and tactile assessment, and further studies may be helpful in determining the accuracy and reliability of tactile assessment compared to quantitative force measurements with systems such as Verasense. In another study, Geller et al. compared rates of arthrofibrosis requiring manipulation under anesthesia (MUA), a nonsurgical treatment for postoperative stiffness, and found lower rates of MUA in 252 TKAs using Verasense compared to 699 standard TKAs—1.6 vs. 5%, p = 0.004 [27]. A clinical trial for Verasense by the authors and Columbia University is ongoing and expected to report patient-reported outcomes from 130 patients enrolled between 2017 and 2020.
3.2 Limitations
While robotic-assisted TKA has made great advances in recent years, there are still some limitations to the technology that are inherent to the cycle of disruptive technology development described by Christensen [28].
The primary barrier to more widespread adoption of this technology is the cost of implementation. The cost of the hardware alone ranges from $400,000 to well over $1,000,000 [20]. Costs are even more prohibitive when considering annual maintenance fees, software upgrades, and per-case disposable costs [20, 29]. Moreover, image-based robotic cases also require advanced preoperative imaging with CT or magnetic resonance imaging (MRI). Finally, Siddiqi et al. offered a thorough cost-benefit analysis including detailed indirect costs that need to be considered in a holistic cost model [20]. As healthcare increasingly trends toward value-based care and bundled payment models, designing comprehensive packages that are inclusive of all ancillary costs will be critical [29].
Working with existing reimbursement schemes, Moschetti et al. performed a Markov decision analysis of robotic unicompartmental knee arthroplasty to explore the current break-even point for robotic knee procedures [30]. The team found that, assuming an image-based system at a cost of $1.362 million, a return on investment can be made once volume surpasses 94 cases per year. For cheaper imageless systems, this break-even point was achieved at 25 cases annually [30]. As such, this technology is presently only a feasible strategy at high-volume centers. Further analyses will need to be performed for TKA and for promising new technology like handheld accelerometer-based navigation systems.
The other important major limitation of robotic-assisted TKA technology is with regard to soft-tissue manipulation. Current versions of orthopedic TKA robots still require the surgeon to perform the dissection and exposure. Once there, systems still require surgeons to retract tissues appropriately to enable cut paths without neurovascular or ligamentous damage [20, 21]. Moreover, current systems cannot actually perform soft-tissue balancing (although they assist in planning gap and ligament balancing) [20, 31]. Future iterations of robotic systems will have better feedback and adaptation mechanisms for mid-cut adjustments and better differentiation of soft-tissue types.
There are other notable limitations when considering this technology. Registration and navigation of the robot require additional or longer incisions for placement of femoral and tibial registration pins [32]. This increases risk for infection, stress risers and periprosthetic fractures, and neurovascular injury due to poor pin placement [20]. Length of surgery is also a concern, as robotic-assisted TKA is still generally longer due to intrinsic workflow delays, OR setup time, implant templating, and intraoperative plan adjustment [20, 21]. Notably, there has been substantial improvement in robotic-assisted TKA efficiency, and there are some studies where surgeons have performed the procedure in comparable time to a conventional TKA [33, 34]. Another concern is that current robotic-assisted TKA systems are implant specific, which limits surgeon options and increases acquisition costs as different surgeons prefer different platforms [21]. Additionally, there are equivocal results on other outcomes such as blood loss, nerve damage, and infection rates, which are all also partially distorted by the learning curves for these techniques [18]. Finally, there are legal concerns, as there is some evidence of an increased rate of litigation with robotic-assisted TKA procedures [35].
While the challenges are not insurmountable, there are still substantial limitations for the widespread adoption of robotic-assisted TKA. Product development with dedicated collaborators will be crucial to expand the use of these systems from a small group of early adopters into standard-of-care practice.
3.3 Outcomes
Whether or not robotic total knee arthroplasty leads to improved radiographic and clinical outcomes remains the subject of significant controversy [36]. Stated broadly, outcomes after robotic-assisted TKA can be grouped into either those related to accuracy and precision of component positioning and alignment or those related to clinical improvement, patient-reported outcomes (PROs) , and functionality metrics. These two groups of outcomes are related but occasionally divergent, and where one study may find significant results related to one or both groups, other studies have failed to differentiate. Investigations into accuracy and precision of component positioning and postoperative limb alignment have evaluated both unicompartmental and TKA cohorts.
3.3.1 Radiographic/Alignment Outcomes After Robotic-Assisted TKA
Robotic-assisted TKA has been touted a s allowing a surgeon to better replicate the anatomy of the native knee. Banger et al. found improved preservation of native knee anatomy in the coronal, sagittal, and axial planes in robotic-assisted TKA [37]. They did not correlate this finding to PROs. In a randomized controlled trial of 72 patients undergoing either conventional TKA or robotic-assisted implantation, Park et al. evaluated femoral flexion angle (gamma angle) and tibial flexion angle (delta angle) in the lateral x-ray and the femoral flexion angle (alpha angle) in the anteroposterior x-ray postoperatively. Both gamma angle and delta angle were significantly improved both with regard to accuracy to anatomic ideal and precision, with standard deviation being lower in the robotic-assisted cohort across all measured angles. With regard to gamma angle, in particular, the robotic-assisted cohort average was 0.17 degrees, representing the achievement of a near-perfect femoral flexion angle [22]. In congruence with these results, Liow et al. found that there were no mechanical axis outliers in a robot-assisted TKA cohort as compared with a 19.4% rate in a conventional cohort. Furthermore, the robotic-assisted TKA group had 3.23% joint-line malposition outliers as compared to 20.6% in the conventional group [38]. Further bolstering the assertion that robotic-assisted TKA results in fewer radiographic outliers, Yang et al. determined that robotic assistance resulted in significantly fewer postoperative leg alignment outliers with regard to femoral coronal inclination, tibial coronal inclination, femoral sagittal inclination, tibial sagittal inclination, and mechanical axis [39]. This data, taken together, leads to the conclusion that robotic-assisted TKA successfully reduces radiographic outliers with respect to postoperative component alignment.
Several studies have attempted to correlate these radiographic findings to PROs and complication rates. Song et al. prospectively randomized 100 patients who underwent unilateral TKA into a robot-assisted arm and a conventional arm and analyzed mechanical axis alignment, flexion/extension gap balance, and PRO scores across the cohorts. They noted a significant decrease in flexion and extension gap imbalance as well as mechanical axis alignment outliers in the robotic-assisted cohort. We will discuss the outcome metrics from this study in more detail in the following section, but despite the reduction in mechanical axis outliers, there was no improvement in postoperative PRO scores. The robotic-assisted procedure did take 25 minutes longer on average than the conventional but had less postoperative blood drainage [40]. Similarly, Kim et al. compared a single surgeon’s robotic-assisted TKA to conventional technique with regard not only to radiographic parameters but also to PROs and complication rates across 1406 patients. These authors failed to find any significant difference between the two cohorts, not only with regard to PROs, survivorship, and complication rates but also with regard to mechanical and radiographic alignment parameters. Thus, they concluded that robotic-assisted TKA was not superior to conventional and, therefore, not cost-effective. These results are poorly generalizable, however, given their single-surgeon sample. It may be reasonable to assume that for an extremely high-volume adult reconstruction surgeon, performing several hundred TKAs yearly, robotic assistance may be unnecessary to achieve adequate alignment. However, for the lower-volume surgeon, robotic assistance may pay dividends in ensuring accuracy and precision of component alignment [41].
3.3.2 Radiographic/Alignment Outcomes After Robotic-Assisted UKA
Studies with methodologies similar to those listed previously have evaluated alignment parameters in unicompartmental knee arthroplasty (UKA) performed using robotic assistance versus the conventional technique. Ollivier et al. found no difference between the two cohorts in regards to lower limb alignment or implant positioning on mediolateral and anteroposterior radiographs. Functionality outcomes differed only marginally between cohorts, and the authors concluded that robotic assistance conferred no real benefit over conventional UKA [42]. In contrast with these results, Bell et al. noticed an improvement in the accuracy of component positioning with robotic-assisted UKA. These authors noted substantial effect sizes, with the percent of cases with femoral component coronal position within 2 degrees of the target position being 70% in the robotic-assisted group versus 28% in the conventional group. These authors did not assess PROs to observe whether or not this discrepancy leads to differential functional outcomes [43].
3.3.3 Radiographic/Alignment Outcomes After Robotic-Assisted TKA Using Adjustable Versus Conventional Cutting Blocks
In a unique study comparing differing techniques within robotic-assisted TKA, Suero et al. compared adjustable cutting blocks to conventional cutting blocks in computer-navigated TKA in 94 patients. These authors found that postoperative mechanical alignment variability and tourniquet time were significantly less in the adjustable cutting block group. Component alignment did not significantly vary between groups [44]. More data is needed to further delineate differences between various protocols for robotic-assisted TKA.
3.4 Clinical/Patient-Reported Outcomes
Patient satisfaction after total knee arthroplasty is dependent on several patient-specific and technical factors. Despite decades of component design improvements and pre- and postoperative pathway optimization, 10–20% of patients in many studies still endorse dissatisfaction [4,5,6,7]. Clinical and PROs after robotic-assisted TKA can be related to accuracy and precision of component positioning and alignment; however, there are other contributing factors. Thus, a surgeon’s role for maximizing patient satisfaction after TKA is twofold: first, setting appropriate expectations regarding surgical recovery, rehabilitation process, and functional goals and, second, providing a technically precise and well-balanced knee with near-native kinematics while minimizing soft-tissue injury and complication risks [9]. Robotic assistance aims to facilitate the surgeon’s task and improve postoperative outcomes through evaluation and planning as well as surgical execution. In this section, we will continue the discussion of outcomes after robotic-assisted TKA by focusing on clinical and PROs.
There are several metrics used to evaluate clinical and patient-reported outcomes. The Oxford Knee Score (OKS) is a knee joint-specific 12-item questionnaire originally developed and validated in 1998 for use in randomized controlled trials in TKA [45]. The OKS has 12 items, five for assessing pain and seven for assessing function. Each item is worth equal weighting [1–5] for a total possible score ranging from 12 to 60. A lower score indicates a better outcome. It is designed specifically for measuring outcomes in knee replacement.
The Knee Injury and Osteoarthritis Outcome Score (KOOS) is a knee joint-specific questionnaire developed in 1998 originally for the purpose of evaluating short-term and long-term symptoms and functioning in subjects with knee injury and osteoarthritis (OA). It was originally validated in patients undergoing anterior cruciate ligament (ACL) reconstruction [46]. The KOOS is a 42-item survey designed to assess people’s opinions about the difficulties they experience with activity due to problems with their knees. A higher score indicates a better outcome.
The Western Ontario and McMaster Universities Arthritis Index (WOMAC) was initially developed in 1982 and was first validated for the purpose of evaluating response to treatment in patients with hip and knee OA in 1998 [47, 48]. The WOMAC underwent multiple subsequent revisions and refinements between 1996 and 1999 [49]. The WOMAC is a 24-item questionnaire with three subscales measuring pain (five items), stiffness (two items), and physical function (17 items). A lower score indicates a better outcome.
Finally, the Knee Society Clinical Rating System (KSS) is a knee joint-specific questionnaire originally developed and validated in 1989 for use in assessing the outcome of TKA [47]. The KSS has two components: a knee rating (0–100 points) and function (0–100 points) worth a total of 200 points. The knee rating is divided into pain (0–50 points) and a knee score that assesses range of motion, stability, and alignment (0–50 points). A higher score indicates a better outcome.
Other functional outcomes of interest include the International Knee Documentation Committee [50], the Lower Extremity Functional Scale [51], and the UCLA activity-level rating [52]. Furthermore, many global health scores are available including the Nottingham Health Profile [53], the SF-12 [54], the SF-36 [55], and the Sickness Impact Profile [56].
3.4.1 Clinical and Patient-Reported Outcomes After TKA
The ROBODOC system (Curexo Technology, Fremont, CA) was the first robotic system to be used in orthopedic surgery in 1992. ROBODOC is an active-autonomous, image-based, robotic milling system that can reproduce accurate component placement and an ideal hip-knee-ankle (HKA) mechanical axis (MA) through an image-based preoperative planning system [38, 57]. ROBODOC was subsequently changed to TSolution-One®. As it has been used for several years, there are several studies in the literature that comment on patient satisfaction after RATKA with ROBODOC.
Liow et al. [57] compared patients undergoing RATKA with ROBODOC to those undergoing conventional TKA [57]. Patients in both groups received Zimmer NexGen LPS-Flex posterior stabilized implants. The RATKA group showed significant improvement in outcome scores for several SF-36 parameters (general health, vitality, and role emotional) and a nonsignificant trend toward higher functional scores. However, they did not demonstrate differences in clinical outcome measures of OKS and KSS knee and function scores.
Kim et al. [41] randomized subjects to a robotic-assisted or conventional jig-based TKA [41]. Robotic-assisted TKA was carried out in two steps with CT-based preoperative planning using ORTHODOC (Integrated Surgical Technology Corp., Davis, CA, USA) and robotic-assisted surgery using the ROBODOC surgical assistance. A Duracon® posterior cruciate-substituting total knee prosthesis (Stryker Orthopaedics, Mahwah, NJ, USA) was used in each knee. There was no difference in any clinical outcome measure at the latest follow-up for patients who received robotic-assisted TKAs when compared to those who received conventional TKAs. This included KSS scores, residual pain, WOMAC scores, knee range of motion (ROM), and UCLA activity scores. Furthermore, at a minimum follow-up of 10 years, they found no differences between robotic-assisted TKA and conventional TKA in terms of functional outcome scores, aseptic loosening, overall survivorship, and complications. Their group ultimately did not recommend robotic-assisted surgery, stating that any technique like robotic-assisted surgery which adds cost to the procedure should deliver results that patients can perceive as improvements.
Finally, Song et al. assessed intermediate-term outcomes of patients undergoing RATKA with the ROBODOC in comparison to those undergoing conventional TKA [40]. They found HSS and WOMAC scores were similar to those previously reported in the literature, with no significant differences between the two.
Within the ROBODOC system , studies have been done to compare outcomes when using the classical (or mechanical) alignment method versus the anatomic (or kinematic) alignment method. Yim et al. [58] compared clinical outcomes between these methods when using ROBODOC with preoperative ORTHODOC planning [58]. They found no significant postoperative differences in knee ROM, HSS, and WOMAC scores. Yeo et al. [59] also evaluated the two alignment methods in patients undergoing ROBODOC-assisted TKA [59]. They also found no significant difference in mean HSS, WOMAC, and KSS scores at final follow-up.
Though there are fewer studies comparing intraoperative alignment methods used during RATKA, there appears to be no difference in clinical outcomes between the two approaches.
MAKO (Stryker, Mahwah, NJ) is a semi-active robotic system and is one of the most prevalent within the US market. It is a haptic or tactile system as it utilizes robotic guidance while retaining surgeon control within the planned resection. Given its recent FDA approval and recent popularity, numerous studies have been published on patient-reported outcomes after RATKA with MAKO. While PROs appear to be relatively similar in the literature focused on RATKA with ROBODOC, the literature demonstrates a trend toward improved PROs when MAKO is used.
Given the brief history of MAKO with its recent FDA approval in 2015, most studies are centered around early postoperative outcomes. Khlopas et al. conducted a prospective randomized controlled trial of early postoperative outcomes in patients undergoing conventional TKA versus those undergoing robotic-arm-assisted TKA with MAKO [60]. Both groups had a cemented Triathlon Cruciate Retaining Total Knee System (Stryker Orthopaedics, Mahwah, NJ) implanted. Functional activity walking and standing scores as well as pain scores were both improved in the RATKA group at 6 weeks and 3 months postoperatively. Importantly, patient satisfaction scores were also improved at 6 weeks and 3 months in the RATKA cohort. Kayani et al. also found improved early postoperative pain scores at four time intervals following surgery [61]. Patients in the RATKA cohort also had decreased opiate analgesia requirements. Finally, Naziri et al. found improved 90-day ROM but comparable complication rates, KSS, and PROs at all early postoperative time points [62]. They found no difference in hospital satisfaction rates.
Marchand et al. in 2017 used the WOMAC patient satisfaction outcome survey to compare 6-month postoperative mean pain, physical function, and total patient satisfaction scores in patients who underwent conventional versus RATKA with MAKO [63]. In their series, patients who underwent robotic-assisted surgery reported significantly better 6-month mean pain and overall satisfaction scores. The same group repeated this study in 2019, assessing 1-year PROs [64]. They found that WOMAC scores were significantly lower in the RATKA group with improved function and decreased pain. Mahoney et al. [65] and Smith et al. [66] both compiled 1-year postoperative clinical outcomes, with both demonstrating clinical improvements of postoperative physical status and function, specifically in KSS score.
Some literature does not specify what robot was used to assist with TKA. Hozack et al. found that patients undergoing RATKA had significantly higher functional activity scores at 6 weeks and 1 year postoperatively [67]. A meta-analysis done by Zhang et al. included seven clinical studies that reported functional outcomes when comparing RATKA using different robotic devices to conventional TKA [68]. Different outcome scores were utilized across the included studies, with the KSS being the most reported followed by Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores . Meta-analysis of outcome data from the studies demonstrated RATKA resulted in a significantly better KSS scores in short to mid-term follow-up.
3.4.2 Clinical and Patient-Reported Outcomes After UKA
There are significantly fewer studies in the literature that assess clinical and PROs after robotic-assisted unicompartmental knee arthroplasty (RAUKA). Gilmour et al. reported on patients undergoing conventional or RAUKA with MAKO [69]. Primary outcomes in the study were OKS and KSS which were not significantly different in the two groups at 2-year follow-up. These findings were supported by Pearle et al. who also reported on patients undergoing RAUKA with MAKO [70]. They found no significant difference in KSS, change in KSS, or Marmor rating between the two cohorts at final follow-up.
Finally, Motesharei et al. compared gait analysis between patients undergoing conventional Oxford UKA and RAUKA with MAKO [71]. At 1-year follow-up, there was a significant difference in the gait of patients in each cohort, with the RAUKA patients demonstrating similar knee excursion compared with native knees, and the conventional Oxford UKA patients demonstrating decreased knee excursion. The authors noted they were unable to specifically attribute this difference to the technique, and other factors may have played a role such as the design of the different implants used for each cohort. Despite these differences, there were no significant differences in OKS and KSS between the two groups.
3.5 Summary
In the coming years, patients and surgeons can expect to see an increase in both the number and variety of robotic technologies commercially available for knee arthroplasty. For both unicompartmental and TKA, the use of robotic assistants to personalize bone resection and knee balancing may be performed in a versatile manner using intraoperative calibration and feedback, with or without the need for preoperative imaging. Since the implementation of early robotic assistants such as ROBODOC, it has been a challenge for many robotic-assistant developers to reduce some of the limitations to broad implementation, particularly with regard to cost, the surgeon’s learning curve, and associated prolongation of intraoperative time. As more types of semi-active robotic assistants come to market after their FDA 510(k) clearance in the past 5 years, more patients and surgeons may demonstrate interest in these technologies and refer to the clinical results of early adopters, some of which demonstrate improvements in radiographic, kinematic, and clinical outcomes.
References (EndNote Traveling Library)
Gatti CJ, Hallstrom BR, Hughes RE. Surgeon variability in total knee arthroplasty component alignment: a Monte Carlo analysis. Comput Methods Biomech Biomed Engin. 2014;17(15):1738–50.
Bargar WL, Bauer A, Börner M. Primary and revision total hip replacement using the Robodoc system. Clin Orthop Relat Res. 1998;354:82–91.
Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97(17):1386–97.
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KDJ. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. 2010;468(1):57–63.
Clement ND, Burnett R. Patient satisfaction after total knee arthroplasty is affected by their general physical well-being. Knee Surg Sports Traumatol Arthrosc. 2013;21(11):2638–46.
Nam D, Nunley RM, Barrack RL. Patient dissatisfaction following total knee replacement. The Bone & Joint Journal. 2014;96-B(11_Supple_A):96–100.
Von Keudell A, Sodha S, Collins J, Minas T, Fitz W, Gomoll AH. Patient satisfaction after primary total and unicompartmental knee arthroplasty: an age-dependent analysis. Knee. 2014;21(1):180–4.
Noble PC, Conditt MA, Cook KF, Mathis KB. The John Insall Award: patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res. 2006;452:35–43.
Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW. Patient dissatisfaction following total knee arthroplasty: a systematic review of the literature. J Arthroplasty. 2017;32(12):3854–60.
Naal FD, Fischer M, Preuss A, Goldhahn J, von Knoch F, Preiss S, et al. Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med. 2007;35(10):1688–95.
Hopper GP, Leach WJ. Participation in sporting activities following knee replacement: total versus unicompartmental. Knee Surg Sports Traumatol Arthrosc. 2008;16(10):973.
Liddle AD, Judge A, Pandit H, Murray DW. Adverse outcomes after total and unicompartmental knee replacement in 101 330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet. 2014;384(9952):1437–45.
W-Dahl A, Robertsson O, Lidgren L, Miller L, Davidson D, Graves S. Unicompartmental knee arthroplasty in patients aged less than 65. Acta Orthop. 2010;81(1):90–4.
Koskinen E, Paavolainen P, Eskelinen A, Pulkkinen P, Remes V. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007;78(1):128–35.
Liddle AD, Pandit H, Judge A, Murray DW. Effect of surgical caseload on revision rate following total and unicompartmental knee replacement. JBJS. 2016;98(1):1–8.
Badawy M, Fenstad AM, Bartz-Johannessen CA, Indrekvam K, Havelin LI, Robertsson O, et al. Hospital volume and the risk of revision in Oxford unicompartmental knee arthroplasty in the Nordic countries -an observational study of 14,496 cases. BMC Musculoskelet Disord. 2017;18(1):388.
Christ AB, Pearle AD, Mayman DJ, Haas SB. Robotic-assisted unicompartmental knee arthroplasty: state-of-the art and review of the literature. J Arthroplasty. 2018;33(7):1994–2001.
Lang JE, Mannava S, Floyd AJ, Goddard MS, Smith BP, Mofidi A, et al. Robotic systems in orthopaedic surgery. J Bone Joint Surg Br. 2011;93(10):1296–9.
Schneider O, Troccaz J. A six-degree-of-freedom passive arm with dynamic constraints (PADyC) for cardiac surgery application: preliminary experiments. Comput Aided Surg. 2001;6(6):340–51.
Siddiqi A, Mont MA, Krebs VE, Piuzzi NS. Not all robotic-assisted total knee arthroplasty are the same. J Am Acad Orthop Surg. 2021;29(2):45–59.
Jacofsky DJ, Allen M. Robotics in arthroplasty: a comprehensive review. J Arthroplasty. 2016;31(10):2353–63.
Park SE, Lee CT. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplasty. 2007;22(7):1054–9.
Siebert W, Mai S, Kober R, Heeckt PF. Technique and first clinical results of robot-assisted total knee replacement. Knee. 2002;9(3):173–80.
Elmallah RK, Mistry JB, Cherian JJ, Chughtai M, Bhave A, Roche MW, et al. Can we really “Feel” a balanced total knee arthroplasty? J Arthroplasty. 2016;31(9, Supplement):102–5.
D'Lima DD, Patil S, Steklov N, Colwell CW Jr. An ABJS best paper: dynamic intraoperative ligament balancing for total knee arthroplasty. Clin Orthop Relat Res. 2007;463:208–12.
Cho KJ, Seon JK, Jang WY, Park CG, Song EK. Objective quantification of ligament balancing using VERASENSE in measured resection and modified gap balance total knee arthroplasty. BMC Musculoskelet Disord. 2018;19(1):266.
Geller JA, Lakra A, Murtaugh T. The use of electronic sensor device to augment ligament balancing leads to a lower rate of arthrofibrosis after total knee arthroplasty. J Arthroplasty. 2017;32(5):1502–4.
Christensen CM. The innovator's dilemma : when new technologies cause great firms to fail. Boston: Harvard Business Review Press; 2013. xxvii, 252 pages p.
Lonner JH, Klement MR. Robotic-assisted medial unicompartmental knee arthroplasty: options and outcomes. J Am Acad Orthop Surg. 2019;27(5):e207–e14.
Moschetti WE, Konopka JF, Rubash HE, Genuario JW. Can robot-assisted unicompartmental knee arthroplasty be cost-effective? A Markov decision analysis. J Arthroplasty. 2016;31(4):759–65.
Pearle AD, Kendoff D, Musahl V. Perspectives on computer-assisted orthopaedic surgery: movement toward quantitative orthopaedic surgery. J Bone Joint Surg Am. 2009;91 Suppl 1:7–12.
Kayani B, Konan S, Ayuob A, Onochie E, Al-Jabri T, Haddad FS. Robotic technology in total knee arthroplasty: a systematic review. EFORT Open Rev. 2019;4(10):611–7.
Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1132–41.
Grau L, Lingamfelter M, Ponzio D, Post Z, Ong A, Le D, et al. Robotic arm assisted total knee arthroplasty workflow optimization, operative times and learning curve. Arthroplast Today. 2019;5(4):465–70.
Davies BL, Rodriguez y Baena FM, Barrett AR, Gomes MP, Harris SJ, Jakopec M, et al. Robotic control in knee joint replacement surgery. Proc Inst Mech Eng H. 2007;221(1):71–80.
Shatrov J, Parker D. Computer and robotic – assisted total knee arthroplasty: a review of outcomes. J Exp Orthop. 2020;7(1):70.
Banger MS, Johnston WD, Razii N, Doonan J, Rowe PJ, Jones BG, et al. Robotic arm-assisted bi-unicompartmental knee arthroplasty maintains natural knee joint anatomy compared with total knee arthroplasty: a prospective randomized controlled trial. Bone Joint J. 2020;102-B(11):1511–8.
Liow MH, Xia Z, Wong MK, Tay KJ, Yeo SJ, Chin PL. Robot-assisted total knee arthroplasty accurately restores the joint line and mechanical axis. A prospective randomised study. J Arthroplasty. 2014;29(12):2373–7.
Yang HY, Seon JK, Shin YJ, Lim HA, Song EK. Robotic total knee arthroplasty with a cruciate-retaining implant: a 10-year follow-up study. Clin Orthop Surg. 2017;9(2):169–76.
Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. 2013;471(1):118–26.
Kim YH, Yoon SH, Park JW. Does robotic-assisted TKA result in better outcome scores or long-term survivorship than conventional TKA? A randomized. Controlled Trial Clin Orthop Relat Res. 2020;478(2):266–75.
Ollivier M, Parratte S, Lunebourg A, Viehweger E, Argenson JN. The John Insall Award: no functional benefit after unicompartmental knee arthroplasty performed with patient-specific instrumentation: a randomized trial. Clin Orthop Relat Res. 2016;474(1):60–8.
Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M. Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am. 2016;98(8):627–35.
Suero EM, Plaskos C, Dixon PL, Pearle AD. Adjustable cutting blocks improve alignment and surgical time in computer-assisted total knee replacement. Knee Surg Sports Traumatol Arthrosc. 2012;20(9):1736–41.
Dawson J, Fitzpatrick R, Murray D, Carr A. Questionnaire on the perceptions of patients about total knee replacement. J Bone Joint Surg Br. 1998;80(1):63–9.
Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS) - validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1:17.
Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop Relat Res. 1989;248:13–4.
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40.
Bellamy N. WOMAC: a 20-year experiential review of a patient-centered self-reported health status questionnaire. J Rheumatol. 2002;29(12):2473–6.
Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken). 2011;63 Suppl 11:S208–28.
Binkley JM, Stratford PW, Lott SA, Riddle DL. The Lower Extremity Functional Scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999;79(4):371–83.
Naal FD, Impellizzeri FM, Leunig M. Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res. 2009;467(4):958–65.
Dunbar MJ, Robertsson O, Ryd L, Lidgren L. Appropriate questionnaires for knee arthroplasty. Results of a survey of 3600 patients from the Swedish Knee Arthroplasty Registry. J Bone Joint Surg Br. 2001;83(3):339–44.
Ware J Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83.
Bergner M, Bobbitt RA, Carter WB, Gilson BS. The sickness impact profile: development and final revision of a health status measure. Med Care. 1981;19(8):787–805.
Liow MHL, Chin PL, Pang HN, Tay DK, Yeo SJ. THINK surgical TSolution-one((R)) (Robodoc) total knee arthroplasty. SICOT J. 2017;3:63.
Yim JH, Song EK, Khan MS, Sun ZH, Seon JK. A comparison of classical and anatomical total knee alignment methods in robotic total knee arthroplasty: classical and anatomical knee alignment methods in TKA. J Arthroplasty. 2013;28(6):932–7.
Yeo JH, Seon JK, Lee DH, Song EK. No difference in outcomes and gait analysis between mechanical and kinematic knee alignment methods using robotic total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2019;27(4):1142–7.
Khlopas A, Sodhi N, Hozack WJ, Chen AF, Mahoney OM, Kinsey T, et al. Patient-reported functional and satisfaction outcomes after robotic-arm-assisted total knee arthroplasty: early results of a prospective multicenter investigation. J Knee Surg. 2020;33(7):685–90.
Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J. 2018;100-B(7):930–7.
Naziri Q, Cusson BC, Chaudhri M, Shah NV, Sastry A. Making the transition from traditional to robotic-arm assisted TKA: what to expect? A single-surgeon comparative-analysis of the first-40 consecutive cases. J Orthop. 2019;16(4):364–8.
Marchand RC, Sodhi N, Khlopas A, Sultan AA, Harwin SF, Malkani AL, et al. Patient satisfaction outcomes after robotic arm-assisted Total knee arthroplasty: a short-term evaluation. J Knee Surg. 2017;30(9):849–53.
Marchand RC, Sodhi N, Anis HK, Ehiorobo J, Newman JM, Taylor K, et al. One-year patient outcomes for robotic-arm-assisted versus manual total knee arthroplasty. J Knee Surg. 2019;32(11):1063–8.
Mahoney O, Kinsey T, Sodhi N, Mont MA, Chen AF, Orozco F, et al. Improved component placement accuracy with robotic-arm assisted total knee arthroplasty. J Knee Surg. 2020.
Smith AF, Eccles CJ, Bhimani SJ, Denehy KM, Bhimani RB, Smith LS, et al. Improved patient satisfaction following robotic-assisted total knee arthroplasty. J Knee Surg. 2021;34(7):730–8.
Hozack WJ. Multicentre analysis of outcomes after robotic-arm assisted total knee arthroplasty. Orthop Proc. 2018;100-B(SUPP_12):38.
Zhang J, Ndou WS, Ng N, Gaston P, Simpson PM, Macpherson GJ, et al. Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2021.
Gilmour A, MacLean AD, Rowe PJ, Banger MS, Donnelly I, Jones BG, et al. Robotic-arm-assisted vs conventional unicompartmental knee arthroplasty. The 2-year clinical outcomes of a randomized controlled trial. J Arthroplasty. 2018;33(7S):S109–S15.
Pearle AD, van der List JP, Lee L, Coon TM, Borus TA, Roche MW. Survivorship and patient satisfaction of robotic-assisted medial unicompartmental knee arthroplasty at a minimum two-year follow-up. Knee. 2017;24(2):419–28.
Motesharei A, Rowe P, Blyth M, Jones B, Maclean A. A comparison of gait one year post operation in an RCT of robotic UKA versus traditional Oxford UKA. Gait Posture. 2018;62:41–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kerr, D.L., Cochrane, N.H., Anastasio, A.T., Charalambous, L.T., Wu, M., Seyler, T.M. (2022). Advances in Surgical Techniques for Robotic Computer-Navigated Total and Unicompartmental Knee Arthroplasty. In: Noyes, F.R., Barber-Westin, S. (eds) Critical Rehabilitation for Partial and Total Knee Arthroplasty. Springer, Cham. https://doi.org/10.1007/978-3-030-87003-4_3
Download citation
DOI: https://doi.org/10.1007/978-3-030-87003-4_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-87002-7
Online ISBN: 978-3-030-87003-4
eBook Packages: MedicineMedicine (R0)