Abstract
Robotic-assisted surgery for total knee arthroplasty (TKA) continues to gain popularity as orthopedists seek to enhance their abilities to place implants more precisely and consistently. However, the benefits of robotic assistance must be weighed against factors such as increased surgical time, cost, and learning curve challenges. Furthermore, due to the paucity of data on many of these newer systems, clinical studies have yet to determine their long-term benefits. Robotic-assisted navigation does provide distinct 3D data during preoperative planning that allows the surgeon to increase implant placement accuracy. The use of robotic technology is a valuable technological development that can help to improve surgical technique and potentially clinical results in total knee arthroplasty.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Although conventional total knee arthroplasty (TKA) remains a successful intervention for end-stage arthritis , some patients still experience reduced functionality and require revision procedures related to component malposition or soft tissue imbalance [1]. Robotic-assisted TKA has gained increasing popularity as orthopedic surgeons aim to increase accuracy and precision of implant positioning and quantified ligament balance [2]. Postoperative alignment of TKA components may influence clinical outcomes, range of motion, and implant longevity [3]. The use of robotics in orthopedic surgery has helped to minimize human error, which may in turn reduce implant wear and theoretically lead to longer prosthesis survivorship [4, 5]. The following chapter is meant to provide a framework of the surgical techniques for using the NAVIO robotic system to perform total knee arthroplasty (TKA).
Traditional surgical instrumentation has been challenged by robotic systems as a method to decrease mechanical alignment outliers, optimize soft tissue balancing, and restore normal knee kinematics [6,7,8,9]. Robotic-assisted surgery has been available for nearly 15 years, with current systems using various navigation platforms that typically provide a haptic window that allows the surgeon to conduct a total knee arthroplasty (TKA) based on preoperative planning [10]. NAVIO (Smith & Nephew, Inc., Memphis, TN, United States) is a semiautonomous handheld robotic tool that is held and moved by the surgeon, restricting the bone cutting to within the confines of the planned resection area by providing robotic control of the speed or exposure of the tool. It is intended to assist the surgeon in providing spatial boundaries for orientation and reference information to anatomical landmarks during TKA. In the following chapter, we will provide an overview of our preferred surgical techniques for using the NAVIO surgical robotic system for TKA. We will summarize the NAVIO technique for TKA as follows: (1) patient and system setup, (2) surgical preferences, (3) bone tracking hardware, (4) registration, (5) implant planning, (6) bone cutting and soft tissue balance, and (7) trialing and implantation.
Patient and System Setup
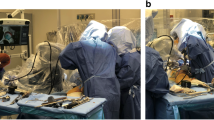
Proper assembly of the NAVIO system is a critical first step to ensuring unimpeded workflow during surgery. The NAVIO computer should be placed to allow the surgeon to easily operate the graphical user interface during the planning stage and to provide visual feedback and guidance during surgery. After the system is well-positioned and the patient has been properly prepped and draped, sterile drapes should be applied to the monitor to allow the surgeon to manipulate the touchscreen intraoperatively. The NAVIO handpiece should also be assembled according to the surgeon’s preference, but the configuration we find most conducive to bone removal is typically 5 mm spherical burr and speed control guard. During patient setup, care should be taken to avoid wrapping the ankle with bulky drapes since this can make it difficult to locate malleolar reference points needed during patient registration. Next, with the help of a leg positioner, elevate the femur to approximately 45°, and flex the knee to 90° (Figs. 15.1 and 15.2). After incision, carefully inspect the joint to remove any prominent spurs or osteophytes. Remove all peripheral osteophytes that can interfere with exposure as this can affect the surgeon’s ability to reliably assess joint stability during virtual mapping and gap balancing. Following resection and excision of osteophytes, ensure that the knee is able to achieve approximately 120° of flexion.
Surgical Preferences
The NAVIO system allows the surgeon to decide on a femur-first or tibia-first workflow (Fig. 15.3). In order to define rotational preferences, the application allows the surgeon to choose landmark preferences on the femur and tibia, which calculates the implant component placement and ligament balancing. For the femur, the rotational references can be defined as follows: transepicondylar, femoral anteroposterior (AP), or posterior condylar axis. For the tibia, the reference options for computing its rotation are the tibial AP axis, mediolateral axis, axis rotationally aligned to the femoral mechanical axis, or axis aligned with the medial third of the tibia tubercle. After deciding preferences for rotational references, the collection stage of registration points and surface mapping based on patient anatomy precedes.
Bone Tracking Hardware
A successful NAVIO-assisted surgery is highly dependent on rigid independent fixation of the femoral and tibial tracking frames to the bones. NAVIO utilizes a two-pin bi-cortical fixation system. To place the tibia tracker, percutaneously place the first bone screw approximately one handbreadth inferior to the tibial tubercle on the medial side of the tibial crest. Slowly drill the bone screw into the tibia, perpendicular to the bony surface, stopping once the opposing cortex has been engaged. Then, use the tissue protector to mark the position of the second bone screw inferior to the initial placement and engage the second screw with the bone. Slide the bone clamps over the two bone screws until the bottom of the clamp is within 1 cm of the patient’s skin. Clamp the tibia array, orienting the reflective markers toward the camera, and then slide the array away from the incision site. Next, percutaneously place the first bone screw one handbreadth superior to the patella in the center of the femoral shaft. This can be done after the arthrotomy to ensure the quadriceps tendon is not tethered. If placing the array prior to arthrotomy, ensure the pins are placed laterally to the quadriceps tendon and with the knee in deep flexion to minimize tethering of the quadriceps. Clamp the femoral tracker frame onto the bone clamp. Confirm that the position of the optical tracking arrays is fully in line of sight with the camera through a full range of motion to optimize the flow of the registration and cutting processes (Fig. 15.4). With the leg in deep flexion, then in full extension, advance the camera orientation adjustment screen to confirm the visibility of the femur and tibia tracker frames (Fig. 15.5). Checkpoint pins should also be placed in the femur/tibia so that these points can be used throughout the procedure to determine if bone tracking frames have moved. Be sure to place the checkpoint pins away from the bone surfaces that are to be prepared in order to avoid cutting or shifting them. On the tibial side, this pin must be placed far enough below the resection level; on the femoral side, this pin is placed on the medial condyle, posteriorly toward the epicondyle to avoid being disturbed by the femoral chamfer cuts (Fig. 15.6).
Registration
NAVIO utilizes a CT-free registration process that relies on standard image-free principles to construct a virtual representation of the patient’s anatomy and kinematics. The first step in registration is to use the point probe to identify the most prominent points on the medial and lateral malleoli in order to register the ankle center. The next step, hip center calculation, follows the femoral tracker array through circular movements of the hip. A key point at this stage is to avoid pelvic movement, which can serve as a source of error. The femur should start in approximately 20° of flexion (avoid hip flexion greater than 45°), and then slowly rotate the hip until all sectors of the graphic on the screen have turned green (Fig. 15.7). Then place the leg in full extension, press and hold the right foot pedal, which will calculate the patient’s varus/valgus alignment. The Preoperative Knee Motion Collection screen then allows the user to record normal flexion motion. Move the leg through a normal (unstressed) range of motion to maximum flexion, making sure to collect all possible sectors between 20° and 50° at minimum. Then, apply constant varus and valgus stress to the collateral ligaments and collect data throughout flexion. The system turns orange for the medial compartment and purple for the lateral compartment. This data will be used to identify how much laxity will be built into the respective medial and lateral gaps for proper joint balancing.
In order to register the femoral condylar surfaces, there are four landmark points that must be collected. Using the point probe, collect the knee center, most posterior medial point, most posterior lateral point, and the anterior notch point (Fig. 15.8). Based on surgeon preference, there are three options for defining the femoral reference for rotational alignment: transepicondylar axis, femoral AP axis, or posterior condylar axis. At this stage, femoral condylar surface mapping is performed by “painting” the probe over the entire femoral surface while holding down the foot pedal (Fig. 15.7). After mapping the femoral surfaces, if the surgeon does not feel that the rotational axis is properly established, then femoral axis redefinition can be performed to redefine the rotational axis of the femur.
Following successful femoral registration, there are three tibial landmarks to collect: knee center, medial plateau, and lateral plateau points (Fig. 15.9). Then, as defined during previous surgical preference selection, there are four options to define the tibial rotational axis: tibia AP axis, mediolateral axis, transfer femoral mechanical axis, and medial third of the tibial tubercle collection. The last registration step, tibial condyle surface mapping, offers visualization of the previously collected tibial mechanical and rotational axes. The user should also digitize the tibial condylar surfaces by “painting” the point probe over the surface while holding down the foot pedal until the virtual model is formed. To ensure accuracy, it is encouraged to “paint” over the edges to help with sizing of the model. Similar to above, the rotational axis can be redefined at this stage if the surgeon feels that the axis is not properly defined.
Implant Planning
The implant planning stage provides a virtual reconstruction of the patient’s femoral and tibial anatomy, soft tissue ligament tension, and joint balance. There are three stages: (1) initial sizing and placement, (2) gap planning/balancing, and (3) cut guide placement (if that is the preferred method of bone preparation). Landmark points collected during registration are used to adjust the size and placement of the components. For the femoral component, using the cross-section mode, first confirm that the component size provides adequate coverage on the digitized femur bone surface. To avoid notching, be sure to assess the transition of the implant’s anterior/proximal tip with the bone surface (Fig. 15.10). Then, verify the transition of the implant component in the sagittal view screen and adjust the component in the AP position and flexion to achieve the desired anterior transition. Assess the posterior coverage of the component in both the sagittal and transverse views. The implant components for NAVIO are anteriorly referenced. Therefore in order to have greater resection on the posterior bone and to increase the posterior gap, the component may be downsized, without any change to the anterior transition of the component on to the bone. In order to assess size coverage, implant anterior transition, and the bone resection plan, toggle on the virtual cut to visualize the implant component on the bone surface. The user should also confirm that the component is not overhanging medially or laterally.
For the tibial component, the NAVIO software provides a starting size and initial placement based on the tibia free point collection. Begin by confirming and adjusting the implant size using the transverse view. Next, confirm the posterior slope, which reflects the slope of the tibial component with respect to the mechanical axis defined during registration. The rotation of the tibial component is initialized to 0° with respect to the tibial AP axis. Placement of the tibial component is not constrained by NAVIO cut guides since the final implant rotation and placement is performed manually. Initially, the tibial component will default to the thinnest bearing, but thicker inserts can be selected by changing the polyethylene component. The user can also choose to move the component proximally, which will decrease the resection depth based on the two plateau points collected on the tibia during the Tibia Landmark Point Collection stage.
The second stage of implant planning allows the user the ability to dial in the virtual soft tissue laxity for the patient through a full range of flexion based on the prior ligament balancing section. There are four interactive views for translating and rotating the components with respect to the patient’s virtualized joint. The goal of this stage is to have balanced extension and flexion gaps with no virtual overlap in either the medial or lateral compartments. The surgeon can choose to perform various cruciate or collateral/capsular soft tissue releases and then re-collect laxity information by clicking on the Re-collect Joint Laxity button in order to depict what the joint space will actually look like once the initial balancing is performed. The surgeon can also manipulate the virtual coronal, sagittal, translational, or rotational positions of the implants to adjust gap balance, such that the resulting gap is approximately 2–3 mm above the zero line through a range of motion (Fig. 15.11). Balancing of the flexion gap in the medial and lateral compartments can be performed by rotating the femur component internally or externally. Adjustments to femoral component rotation should be carefully considered relative to prior parameters such as anterior notching and patellofemoral tracking. Adjustments to femoral flexion should also be considered against prior considerations regarding anterior fit and alignment to the intramedullary (IM) axis.
The joint laxity assessment consists of collecting information on ligament stress or laxity throughout the full range of knee motion. First, while keeping the operative leg in full extension and maintaining knee flexion between −10° and +10°, apply constant and maximal stress to the contralateral ligaments to collect varus and valgus data. A graph is then generated that depicts the tightness or laxity in the medial or lateral knee compartments based on the stress collections. This graphic illustration allows the user to determine the degree of ligament release that is required to restore equal gaps in the medial and lateral compartments in full extension. Next, flex the operative knee to 90° and apply constant and maximal stress to the contralateral ligaments to collect varus/valgus data within 80°–100° of knee flexion. The surgeon may want to use a Z-retractor or laminar spreader to open up the medial and lateral compartment spaces to capture the maximum joint laxity to varus and valgus stresses in flexion .
Bone Cutting
While the entirety of the bone preparation can be performed with a 5 mm burr, for efficiency purposes, most NAVIO users utilize a hybrid approach, with the use of burrs and saws, for complete bone preparation in TKA. In accordance with the implant placement plan, the robotic handpiece is used to create locking lug slots in the patient’s bones that securely position the cutting guides in place (Figs. 15.12 and 15.13). The femoral distal cut guide is then mounted onto the anterior femur via the prepared anterior lug holes and locked into position using a stabilizer block and additional pins. A manually controlled saw is used to resect the distal femur through the robotically positioned cut guide. Based on the virtual preoperative implant sizing plan, the drill guide adapter is attached to the distal cut guide and drill holes made at the predetermined size. The appropriately sized 5-in-1 cutting guide is then impacted and pinned into position. A plate probe can be used to ensure that the cut guide is placed in its intended position prior to resection, and it can also be used after saw cuts are made to confirm precision of the resections. The remaining femoral resections are made through the cutting block (Fig. 15.14).
For tibial resection, precise positioning and mounting of the tibial cutting guide is facilitated by using the robotic tool to make four recipient lug slots on the tibia, as directed based on the virtually modeled plan. The tibia cut guide is inserted into the prepared bone lug holes and further secured with additional pins. The tibia is then resected with a saw, with care taken to use soft tissue protectors to prevent the saw (or burr) from causing inadvertent damage to the collateral ligaments and other soft tissues .
Trialing
Leaving the femoral and tibial tracking arrays in place, after completing all bone cuts and adjustments to the final surfaces, the trial components are provisionally implanted, and their positions, limb alignment, range of knee motion, and varus/valgus balance are assessed throughout a full flexion arc both by clinical assessment and virtual quantification (Fig. 15.15). The Postop Stressed Gap Assessment screen allows the user to quantifiably assess the post-op laxities throughout flexion in both the medial and lateral compartments. At this point, adjustments in bone resections or soft tissue releases can be made to further optimize position, motion, and soft tissue gap balancing. After the dynamic ROM testing is finalized, final surface preparation is completed for manual implantation of the final components (Fig. 15.16).
Data/Outcomes
While there are presently no published data on the radiographic or functional outcomes of TKA performed with assistance of the NAVIO robotic system, the preliminary data of our initial 54 unilateral primary TKA cases show promising results. Mean age was 68 ± 7 years, and gender breakdown was 75% female and 25% male. With regard to preoperative comorbidity risk, the majority of patients were ASA 2 (58%) and ASA 3 (42%). The average hospital length of stay was 3 ± 1.4 days. Intraoperatively, average estimated blood loss (EBL) was 292 ± 85 mL, and surgical time was 130 ± 43 min. Postoperative alignment was within ±3° for all cases. There were no intra- or postoperative complications and no reoperation or revision surgeries.
Conclusions
Robotic-assisted surgery for TKA continues to gain popularity as orthopedists seek to enhance their abilities to place implants more precisely and consistently. However, the benefits of robotic assistance must be weighed against factors such as increased surgical time, cost, and learning curve challenges. Furthermore, due to the paucity of data on many of these newer systems, clinical studies have yet to determine their long-term benefits. Robotic-assisted navigation does provide distinct 3D data during preoperative planning that allow the surgeon to increase implant placement accuracy. The use of robotic technology is a valuable technological development that can help to improve surgical technique and potentially clinical results in total knee arthroplasty.
References
Kim YH, Kim JS, Kim DY. Clinical outcome and rate of complications after primary total knee replacement performed with quadriceps-sparing or standard arthrotomy. J Bone Joint Surg Br. 2007;89:467–70.
Park SE, Lee CT. Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplast. 2007;22:1054–9.
Matsuda S, Kawahara S, Okazaki K, Tashiro Y, Iwamoto Y. Postoperative alignment and ROM affect patient satisfaction after TKA. Clin Orthop Relat Res. 2013;471(1):127–33.
Bellemans J, Vandenneucker H, Vanlauwe J. Robot-assisted total knee arthroplasty. Clin Orthop Relat Res. 2007;464:111–6.
Song EK, Seon JK, Yim JH, Netravali NA, Bargar WL. Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA. Clin Orthop Relat Res. 2013;471:118–26.
Borner M, Wiesel U, Ditzen W. Clinical experiences with Robodoc and the Duracon Total knee. In: Stiehl JB, Konermann WH, Haaker RG, editors. Navigation and robotics in total joint and spine surgery. Berlin: Springer; 2004. p. 362–6.
Mai S, Lorke C, Siebert W. Clinical results with the robot-assisted Caspar system and the search-evolution prosthesis. In: Stiehl JB, Konermann WH, Haaker RG, editors. Navigation and robotics in total joint and spine surgery. Berlin: Springer; 2004. p. 355–61.
Decking J, Theis C, Achenbach T, et al. Robotic total knee arthroplasty: the accuracy of CT-based component placement. Acta Orthop Scand. 2004;75:573–9.
Kharwadkar N, Kent RE, Sharara KH, Naique S. 5 degrees to 6 degrees of distal femoral cut for uncomplicated primary total knee arthroplasty: is it safe? Knee. 2006;13:57–60.
Paul HA, Bargar WL, Mittlestadt B, et al. Development of a surgical robot for cementless total hip arthroplasty. Clin Orthop Relat Res. 1992;(285):57–66.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Elbuluk, A.M., Vigdorchik, J.M. (2019). Total Knee Arthroplasty Technique: NAVIO. In: Lonner, J. (eds) Robotics in Knee and Hip Arthroplasty. Springer, Cham. https://doi.org/10.1007/978-3-030-16593-2_15
Download citation
DOI: https://doi.org/10.1007/978-3-030-16593-2_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-16592-5
Online ISBN: 978-3-030-16593-2
eBook Packages: MedicineMedicine (R0)