Abstract
Despite advances in surgical techniques, recurrent tears of the rotator cuff following repair remain a major challenge. As the endogenous healing potential of the repaired tendon appears to be limited, augmentation techniques using biologic adjuvants have garnered recent attention, including the application of growth factors, platelet-rich plasma (PRP), or mesenchymal stem cells (MSCs). Although bone marrow still remains the traditional source for MSCs used for biologic augmentation of rotator cuff repair, recent studies have highlighted subacromial bursal tissue to be an alternative, easily accessible, inexpensive source of MSCs.
Despite strong in vitro results regarding the stimulating effects of PRP on tenocytes and myocytes, clinical outcomes following PRP application have been inconsistent. Additionally, reported clinical outcomes of concentrated bone marrow aspirate (BMAC) applications should be interpreted with caution, with the actual clinical efficacy of BMAC still remaining a matter of debate. In vitro studies of human subacromial bursa-derived cells (SBDCs) have shown strong results, demonstrating superior differentiation and proliferation potential compared to BMAC. Thus, SBDCs may be a promising biological augment for rotator cuff surgery, however, clinical outcomes following repair augmentation are yet to be reported.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
Despite advances in surgical techniques, recurrent tears of the rotator cuff following repair remain a major challenge [1]. A series of arthroscopic rotator cuff repairs has demonstrated that postoperative healing of the tendon usually occurs between 71% and 89% of cases [2, 3]. However, this rate of tendon healing may decrease to only 47% or 50% of cases in the treatment of massive rotator cuff tears [2, 3]. Consequently, (re)-tear size can directly affect tendon healing and subsequent shoulder function [2,3,4]. Even though a “hypovascular zone” within the supraspinatus tendon has been hypothesized to lead to initial degenerative tears with further implication to poor tendon healing following repair, the complexity of the healing process has not yet been fully understood [5].
The cells contributing to natural tendon healing have been found to originate from loose connective tissue surrounding the tendon fascicles and tendon body [6]. In response to the injury, these cells proliferate and migrate toward the tear site, in order to form collagenous healing tissue [6,7,8]. As the endogenous healing potential of the tendon appears to be limited, augmentation techniques using biologic adjuvants have recently garnered more attention, including the application of growth factors, platelet-rich plasma (PRP), or mesenchymal stem cells (MSCs) [9, 10]. Despite bone marrow being the traditional source for MSCs used for biologic augmentation of tendon injuries over the last years, recent studies have highlighted subacromial bursal tissue to be an alternative, easily accessible, inexpensive source for MSCs, demonstrating superior proliferation potential, tissue engraftment, and survival, when compared to bone marrow-derived MSCs [6, 10,11,12,13].
2 Biologic Adjuvants for Repair Augmentation
2.1 Platelet-Rich Plasma
Platelet-rich plasma (PRP) is derived from autologous peripheral blood that is centrifuged to isolate a higher concentration of growth factors contained within alpha-granules of the platelets (Fig. 4.1) [14]. Due to the potential of promoting tendon healing along with the relatively low risk profile, this biologic adjuvant is appealing in the treatment of rotator cuff tears [14, 15]. Generally, there are two types of PRP based on the concentration of white blood cells: leukocyte-poor and leukocyte-rich PRP. As leukocytes are important for wound healing and tissue restoration, they may also induce an excessive inflammatory response [16].
2.1.1 Basic Science Evidence
In vitro studies have demonstrated that tenocytes exposed to PRP have increased cell proliferation and matrix synthesis, potentially leading to improved tendon regeneration or healing [15, 17]. In addition, application of PRP was found to induce the differentiation of tendon stem cells into active tenocytes, exhibiting high proliferation rates and collagen production capability [18]. However, the final PRP-composite is influenced by numerous patient-specific factors, including age, sex, diet, and activity level [19]. Preparation-specific factors comprise the type of collecting tube as well as speed and number of cycles during the centrifugation process [15, 16]. Even in separate samples harvested from the same patient, PRP has been shown to vary widely, making generalization of clinical and in vitro findings difficult [16].
2.1.2 Clinical Outcomes
Despite strong in vitro results regarding its stimulating effects on tenocytes and myocytes, clinical outcomes following PRP application have been inconsistent. Recent meta-analyses of randomized controlled trials have reported mixed results, with some showing decreased failure-to-heal rate for small- to medium-sized tears as well as decreased re-tear rates for large tears treated with PRP [20, 21], and others finding no difference in outcome scores and structural healing rates [22, 56]. A study by Malavolta et al. found that PRP application did not significantly improve clinical outcomes, pain, and structural healing in 51 prospectively randomized patients undergoing arthroscopic single-row rotator cuff repair at 5-year follow-up [39]. In contrast, Randelli et al. performed a prospective, double-blinded, randomized controlled trial and reported short-term benefits following repair augmentation using PRP, including significantly lower pain scores 1 month after surgery and greater functional improvement at 3-month follow-up [51]. However, there was no difference in clinical outcome measures at 6, 12, and 24 months, postoperatively [51].
The use of PRP for clinical application is limited to the variability in the final composite and the heterogeneity of studies, compromising direct comparisons between studies. This includes differences in underlying tendon pathology, repair technique, postoperative rehabilitation, PRP composition, and comorbidities such as smoking status and diabetes [15].
3 Cell-Based Therapies
Concentrated bone marrow aspirate (BMAC) and subacromial bursa-derived cells (SBDCs) have been described as viable sources of cell populations with MSC and progenitor characteristics for the use in regenerative orthopedic surgery [11, 13, 40, 44, 45, 47, 49]. However, it should be considered that these minimally manipulated cell preparations have to be distinguished from laboratory-prepared cell populations undergoing cell sorting and culture expansion [15]. In contrast to culture-expanded bone marrow-derived MSCs, BMAC only comprises a very low concentration of MSCs by formal criteria [28], which has been shown to range only from 0.001% to 0.01% of total cells [50]. These minimal criteria proposed by the International Society for Cell Therapy include the adherence to tissue culture plastic, the ability to form colonies, positive fluorescence-activated cell sorting (FACS) analysis for MSC-specific surface markers, and the ability of multilineage differentiation [28]. Thus, it has been recommended to abandon the term “mesenchymal stem cell” for these minimally manipulated cell preparations, which are allowed for clinical application [15]. As a result, the term “connective tissue progenitors” (CTPs) has been proposed, which more accurately describes the heterogeneous population of tissue-resident proliferative stem and progenitor cells [47, 49].
4 Concentrated Bone Marrow Aspirate (BMAC)
Bone marrow still remains the most commonly used source of MSCs for biological augmentation, as its application in patients with rotator cuff injuries has shown promising results including decreasing re-tear rates and improved healing outcomes [9, 10, 29]. However, Muschler et al. found that progenitor cells only averaged about 1 per 30,000 nucleated cells in BMA obtained from the iliac crest [46].
Although aspiration of bone marrow from the iliac crest is still considered the gold standard [35, 42, 49, 58], complications such as hematoma and nerve palsy have been reported [31]. While the proximity of the axillary nerve and artery make the proximal humerus amenable to similar risks, the ability to obtain the sample under direct visualization during rotator cuff repair makes this an ideal location. Mazzocca et al. first described the proximal humerus to be a more desirable source of MSCs for rotator cuff repair due to its ease of attainment (Fig. 4.2) [40]. In addition, BMAC has been shown to contain more growth factors with anti-inflammatory and anabolic effects as well as up to three times more nucleated cells when compared to PRP [57]. However, harvesting BMAC remains an expensive procedure with debatable cost-effectiveness [15].
Demonstrating harvest and processing of bone marrow aspirate (BMA). BMA is obtained from the proximal humeral head during arthroscopic rotator cuff repair using a non-fenestrated trocar (a). The harvested BMA, consisting of blood, bone marrow, and arthroscopic fluid is transferred to a centrifugation system (b) and concentrated (c)
4.1 Basic Science Evidence
Basic science evidence for the use of BMAC in rotator cuff healing augmentation is limited. In a rabbit model, Liu et al. studied the healing potential of supraspinatus tendon repairs augmented with PRP and BMAC [38]. The authors found that repairs augmented with BMAC alone or with a combination of BMAC and PRP demonstrated superior biomechanical properties compared to repairs augmented with PRP alone or pure saline solution [38]. Treatment with BMAC enhanced tendon-to-bone healing along with superior collagen fiber continuity and orientation compared to the control group and presented with significantly higher levels of growth factors compared to PRP [38].
Additionally, Kim et al. investigated the effects of a combined BMAC and PRP application on tendon-derived stem cells and found enhanced proliferation and migration of tendon-derived stem cells, while preventing aberrant chondrogenic and osteogenic differentiation [36].
4.2 Clinical Outcomes
Concentration of a harvested aspirate can easily be performed with only minimal manipulation of cells, allowing for subsequent clinical application in the setting of rotator cuff repair (Fig. 4.2). However, only a few studies with small case series have investigated the effectiveness of bone marrow aspirate for augmenting single-row rotator cuff repairs, with most reporting on bone marrow stimulation techniques, rather than direct application of BMAC [9, 29, 43, 53]. Hernigou et al. reported long-term results of primary rotator cuff repairs augmented using cBMA showing improved healing rates on MRI compared to a non-augmented control group [9]. At 10-year follow-up, 87% of augmented repairs remained intact compared to 44% of repairs in the control group [9].
In 14 patients with a minimum follow-up of 1 year, Ellera Gomes et al. described improved clinical outcomes along with tendon integrity in all patients following augmentation of mini-open transosseous suture repair for full-thickness rotator cuff tears [29]. However, current literature does not allow for drawing definite conclusions regarding the clinical efficacy of BMAC applications, which is mainly due to inconsistent relationships between successful rotator cuff healing and clinical outcomes scores as well as disparities in underlying pathologies, repair techniques, lack of control groups, and patient demographics [15].
In conclusion, reported clinical outcomes of BMAC applications should be interpreted with caution [9, 10, 15, 29, 35, 37]. Further, the actual clinical efficacy of BMAC remains a matter of debate and may rather be explained by its high concentration of growth factors, having anabolic and anti-inflammatory effects [15, 41]. Further, the clinical efficacy of autologous BMAC is dependent on the concentration of necessary progenitor cells [33]. While certain patient characteristics, such as alcohol abuse [32] and smoking [26] can negatively affect BMAC quality, optimizing surgical technique is essential for a successful treatment.
5 Subacromial Bursa-Derived Cells (SBDCs): The Future?
Although bone marrow is still considered the most commonly used source of MSCs for biologic augmentation, recent literature has shown MSCs to be present in subacromial bursal tissue, which is often discarded during arthroscopic surgery to ensure visualization of the rotator cuff tear, suggesting its use as an easily accessible, inexpensive, and viable augment for arthroscopic rotator cuff repair [6, 9,10,11,12,13, 29, 35]. Previous studies found that the cells forming collagenous healing tissue at the tear site originate from originate from loose connective tissue surrounding the tendon fascicles and body, especially the paratenon [7, 8, 55]. As the rotator cuff tendon does not seem to be enclosed by a typical paratenon, the surrounding bursal tissue may be one of the main contributors to endogenous tendon healing. Thus, in the presence of tendon injury and degeneration, these cells may be stimulated to migrate toward and induce healing at the tear site. This may be further supported by the suggestion of Uhthoff et al. that the extension of subacromial bursa should rather be considered a reparative response than a degenerative change [54].
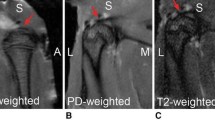
Morikawa et al. described a novel, non-enzymatic, mechanical method for isolating SBDCs for clinical use [45]. According to their technique, subacromial bursa is obtained from over the rotator cuff tendon using an arthroscopic grasper device [45]. The sample is then mechanically digested for 60 s using sterile tenotomy scissors until the tissue resembles a finely minced, liquified particulate (Fig. 4.3) [45].
5.1 Basic Science Evidence
In vitro characterizations of human SBDCs have shown that these cells fulfill all characteristics of MSCs, including similar surface antigen expression profiles and multilineage differentiation [11,12,13]. Furthermore, Utsunomiya et al. reported superior proliferation and differentiation potential of SBDCs compared to other tissues within the shoulder [13]. In an immunodeficient murine patellar tendon defect model, SBDCs showed superior engraftment to host tendon along with survival when compared to bone marrow-derived MSCs (bMSCs) [6]. Further, Morikawa et al. demonstrated superior differentiation and proliferation potential of SBDCs compared to BMAC [44].
Several studies have suggested that the subacromial bursa may play an influential role in bone-tendon healing [34, 54, 55]. Uhthoff and Sarkar reported that rotator cuff healing was most noticeable along the subacromial bursal wall in rotator cuff biopsy specimens and recommended against radical removal of bursa, as total debridement of the bursa may remove a primary source of neovascularizing signals and fibroblastic cells necessary for biological repair of the torn tendon [54]. Further evidence of the biological activity of native bursa was reported by Hirose et al. who determined that spontaneous healing occurred along the bursal side of the rotator cuff tendon in a rabbit model and that the cells that infiltrated the defects were observed to be continuous with the epitenon of the bursa [34]. Yoshida et al. identified the cellular origins of rotator cuff healing after labeling tissue in a murine model, reporting robust involvement of bursal-sided tendon cells with minimal contribution from the enthesis [55]. These studies suggest that subacromial bursa exhibits biological activity within in vitro rotator cuff repair models.
5.2 Clinical Experience and Future
While there is currently no proof regarding the long-term efficacy of bursa augmentation during rotator cuff repair, Hernigou et al. have reported on the clinical results of MSC adjunctive therapy in arthroscopic rotator cuff repair [40]. Patients in the study group received MSCs from BMAC, while those in the control group did not. At 10 years follow-up, 87% of patients in the MSC group had intact rotator cuffs compared with 44% in the control group. Similar clinical outcomes for bursa-augmented repairs is lacking. However, Morikawa et al. showed that the proliferation and differentiation capabilities of MSCs derived from subacromial bursa are at least the same if not superior to those from BMAC [20]. These data suggest that subacromial bursa is a viable, easily accessible source of MSCs that may be a promising biological augment for rotator cuff repairs. However, clinical outcomes following rotator cuff repair augmented with subacromial bursa are yet to be reported.
Additionally, it remains unclear whether there are any metrics that can predict the potential success of subacromial bursa in augmenting rotator cuff healing, including the relation of patient demographics and rotator cuff pathology to the healing potential of subacromial bursa. Further studies are necessary to examine the effects of local and systemic disease on the biological viability of this tissue. Understanding variations in subacromial bursa tissue and how they relate to biological factors involved in healing may assist surgeons in predicting tendon healing and determining both repair type and the need for possible augmentation. Clinical and radiographic outcomes studies are needed to understand the role of bursal augmentation in arthroscopic rotator cuff repair.
6 Further Considerations
Preliminary basic science and clinical evidence has suggested that various nutrients, including vitamin D, proteins, amino acids, and trace minerals may have a positive effect on tendon growth and healing, mainly by engaging with the metabolism of collagen [27]. As collagen forms the major extracellular protein in tendons and muscles, dietary interventions to improve collagen synthesis may be helpful in restoring tendon integrity [27].
In a rat model, Angeline et al. found that a diet-induced vitamin D deficiency had negative effects on early healing at the rotator cuff repair site, showing a significant decrease in load to failure along with less bone formation and collagen fiber organization [23]. However, clinical data regarding the effect of vitamin D supplementation on postoperative rotator cuff healing remains inconsistent. Ryu et al. demonstrated that low serum vitamin D levels were not related to preoperative tear size, extent of tendon retraction, or fatty infiltration of the cuff muscles [52]. More importantly, the authors found that there were no significant relationships with postoperative structural integrity and functional outcomes after arthroscopic rotator cuff repair [52]. Contrary, Oh et al. showed that serum vitamin D levels had a significant negative correlation with fatty muscle degeneration and a positive correlation with isokinetic muscle torque [48]. Further, vitamin D deficiency has been reported to be associated with a greater risk of postoperative surgical complications following rotator cuff repair [30].
Additionally, recent studies have identified matrix metalloproteinases (MMPs) to be critical in maintaining and remodeling the extracellular tissue matrix after rotator cuff repair [24, 25]. The tetracycline family of antibiotics has been demonstrated to inhibit MMPs by a mechanism being independent of their antimicrobial activity, with its local or systemic administration demonstrating reduced severity of tendon degeneration associated with increased MMP activity [24, 25]. Bedi et al. further found that doxycycline-mediated inhibition of interstitial collagenase (MMP-13) enhanced early healing after rotator cuff repair in a rat model, resulting in improved collagen organization and greater strength of the healing enthesis [24]. Although this may offer a novel biologic pathway of repair augmentation, clinical studies regarding the effectiveness of doxycycline administration in the setting of rotator cuff repair are still lacking [24].
7 Summary
Despite advances in surgical techniques, recurrent rotator cuff tears following repair remain a major challenge [1]. As the endogenous healing potential of the tendon appears to be limited, augmentation techniques using biologic adjuvants have recently garnered more attention, including the application of growth factors, PRP, or MSCs [9, 10]. Although bone marrow still remains the traditional source for MSCs used for biologic augmentation of rotator cuff repair, recent studies have highlighted subacromial bursal tissue to be an alternative, easily accessible source of MSCs [6, 10,11,12,13]. Despite strong in vitro results regarding its stimulating effects on tenocytes and myocytes, clinical outcomes following PRP application have been inconsistent. Additionally, reported clinical outcomes of BMAC applications should be interpreted with caution, with the actual clinical efficacy of BMAC still remaining a matter of debate [9, 10, 15, 29, 35, 37]. In vitro characterizations of human SBDCs have shown strong results [11,12,13], demonstrating superior differentiation and proliferation potential compared to BMAC [44]. Thus, SBDCs may be a promising biological augment for rotator cuff repairs; however, clinical outcomes following repair augmentation are yet to be reported.
References
Galatz L, Ball C, Teefey S. The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg Am. 2004;86:219–24.
Bigliani LU, Cordasco FA, McIlveen SJ, Musso ES. Operative treatment of failed repairs of the rotator cuff. J Bone Joint Surg Am. 1992;74(10):1505–15.
Nho SJ, Delos D, Yadav H, et al. Biomechanical and biologic augmentation for the treatment of massive rotator cuff tears. Am J Sports Med. 2010;38(3):619–29.
Bennett WF. Arthroscopic repair of massive rotator cuff tears: a prospective cohort with 2- to 4-year follow-up. Arthroscopy. 2003;19(4):380–90.
Gamradt SC, Gallo RA, Adler RS, et al. Vascularity of the supraspinatus tendon three months after repair: characterization using contrast-enhanced ultrasound. J Shoulder Elb Surg. 2010;19(1):73–80.
Dyrna F, Zakko P, Pauzenberger L, McCarthy MB, Mazzocca AD, Dyment NA. Human subacromial bursal cells display superior engraftment versus bone marrow stromal cells in murine tendon repair. Am J Sports Med. 2018;46(14):3511–20.
Dyment NA, Galloway JL. Regenerative biology of tendon: mechanisms for renewal and repair. Curr Mol Biol Rep. 2015;1(3):124–31.
Dyment NA, Hagiwara Y, Matthews BG, Li Y, Kalajzic I, Rowe DW. Lineage tracing of resident tendon progenitor cells during growth and natural healing. PLoS One. 2014;9(4):e96113.
Hernigou P, Flouzat Lachaniette CH, Delambre J, et al. Biologic augmentation of rotator cuff repair with mesenchymal stem cells during arthroscopy improves healing and prevents further tears: a case-controlled study. Int Orthop. 2014;38(9):1811–8.
Imam MA, Holton J, Horriat S, et al. A systematic review of the concept and clinical applications of bone marrow aspirate concentrate in tendon pathology. SICOT J. 2017;3:58.
Song N, Armstrong AD, Li F, Ouyang H, Niyibizi C. Multipotent mesenchymal stem cells from human subacromial bursa: potential for cell based tendon tissue engineering. Tissue Eng Part A. 2014;20(1–2):239–49.
Steinert AF, Kunz M, Prager P, et al. Characterization of bursa subacromialis-derived mesenchymal stem cells. Stem Cell Res Ther. 2015;6:114.
Utsunomiya H, Uchida S, Sekiya I, Sakai A, Moridera K, Nakamura T. Isolation and characterization of human mesenchymal stem cells derived from shoulder tissues involved in rotator cuff tears. Am J Sports Med. 2013;41(3):657–68.
Lubkowska A, Dolegowska B, Banfi G. Growth factor content in PRP and their applicability in medicine. J Biol Regul Homeost Agents. 2012;26:3S–22S.
Carr JB 2nd, Rodeo SA. The role of biologic agents in the management of common shoulder pathologies: current state and future directions. J Shoulder Elb Surg. 2019;28(11):2041–52.
Mazzocca AD, McCarthy MB, Chowaniec DM, et al. Platelet-rich plasma differs according to preparation method and human variability. J Bone Joint Surg Am. 2012;94(4):308–16.
Kia C, Baldino J, Bell R, Ramji A, Uyeki C, Mazzocca A. Platelet-rich plasma: review of current literature on its use for tendon and ligament pathology. Curr Rev Musculoskelet Med. 2018;11(4):566–72.
Zhang J, Wang JHC. Platelet-rich plasma releasate promotes differentiation of tendon stem cells into active tenocytes. Am J Sports Med. 2010;38(12):2477–86.
Xiong G, Lingampalli N, Koltsov JCB, et al. Men and women differ in the biochemical composition of platelet-rich plasma. Am J Sports Med. 2018;46(2):409–19.
Hurley ET, Lim Fat D, Moran CJ, Mullett H. The efficacy of platelet-rich plasma and platelet-rich fibrin in arthroscopic rotator cuff repair: a meta-analysis of randomized controlled trials. Am J Sports Med. 2019;47(3):753–61.
Warth RJ, Dornan GJ, James EW, Horan MP, Millett PJ. Clinical and structural outcomes after arthroscopic repair of full-thickness rotator cuff tears with and without platelet-rich product supplementation: a meta-analysis and meta-regression. Arthroscopy. 2015;31(2):306–20.
Saltzman BM, Jain A, Campbell KA, et al. Does the use of platelet-rich plasma at the time of surgery improve clinical outcomes in arthroscopic rotator cuff repair when compared with control cohorts? A systematic review of meta-analyses. Arthroscopy. 2015;32(5):906–18.
Angeline ME, Ma R, Pascual-Garrido C, et al. Effect of diet-induced vitamin D deficiency on rotator cuff healing in a rat model. Am J Sports Med. 2014;42(1):27–34.
Bedi A, Fox AJ, Kovacevic D, Deng XH, Warren RF, Rodeo SA. Doxycycline-mediated inhibition of matrix metalloproteinases improves healing after rotator cuff repair. Am J Sports Med. 2010;38(2):308–17.
Bedi A, Kovacevic D, Hettrich C, et al. The effect of matrix metalloproteinase inhibition on tendon-to-bone healing in a rotator cuff repair model. J Shoulder Elb Surg. 2010;19(3):384–91.
Beyth S, Mosheiff R, Safran O, Daskal A, Liebergall M. Cigarette smoking is associated with a lower concentration of CD105(+) bone marrow progenitor cells. Bone Marrow Res. 2015;2015:914935.
Curtis L. Nutritional research may be useful in treating tendon injuries. Nutrition. 2016;32(6):617–9.
Dominici M, Le Blanc K, Mueller I, et al. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy position statement. Cytotherapy. 2006;8(4):315–7.
Ellera Gomes JL, da Silva RC, Silla LM, Abreu MR, Pellanda R. Conventional rotator cuff repair complemented by the aid of mononuclear autologous stem cells. Knee Surg Sports Traumatol Arthrosc. 2012;20(2):373–7.
Harada GK, Arshi A, Fretes N, et al. Preoperative vitamin D deficiency is associated with higher postoperative complications in arthroscopic rotator cuff repair. J Am Acad Orthop Surg Glob Res Rev. 2019;3(7):e075.
Hernigou J, Picard L, Alves A, Silvera J, Homma Y, Hernigou P. Understanding bone safety zones during bone marrow aspiration from the iliac crest: the sector rule. Int Orthop. 2014;38(11):2377–84.
Hernigou P, Beaujean F. Abnormalities in the bone marrow of the iliac crest in patients who have osteonecrosis secondary to corticosteroid therapy or alcohol abuse. J Bone Joint Surg Am. 1997;79(7):1047–53.
Hernigou P, Mathieu G, Poignard A, Manicom O, Beaujean F, Rouard H. Percutaneous autologous bone-marrow grafting for nonunions. Surgical technique. J Bone Joint Surg Am. 2006;88:322–7.
Hirose K, Kondo S, Choi HR, Mishima S, Iwata H, Ishiguro N. Spontaneous healing process of a supraspinatus tendon tear in rabbits. Arch Orthop Trauma Surg. 2004;124(6):374–7.
Imam MA, Holton J, Ernstbrunner L, et al. A systematic review of the clinical applications and complications of bone marrow aspirate concentrate in management of bone defects and nonunions. Int Orthop. 2017;41(11):2213–20.
Kim SJ, Song DH, Park JW, Park S, Kim SJ. Effect of bone marrow aspirate concentrate-platelet-rich plasma on tendon-derived stem cells and rotator cuff tendon tear. Cell Transplant. 2017;26(5):867–78.
Lamo-Espinosa JM, Mora G, Blanco JF, et al. Intra-articular injection of two different doses of autologous bone marrow mesenchymal stem cells versus hyaluronic acid in the treatment of knee osteoarthritis: multicenter randomized controlled clinical trial (phase I/II). J Transl Med. 2016;14(1):246.
Liu XN, Yang C-J, Kim JE, et al. Enhanced tendon-to-bone healing of chronic rotator cuff tears by bone marrow aspirate concentrate in a rabbit model. Clin Orthop Surg. 2018;10(1):99–110.
Malavolta EA, Gracitelli MEC, Assuncao JH, Ferreira Neto AA, Bordalo-Rodrigues M, de Camargo OP. Clinical and structural evaluations of rotator cuff repair with and without added platelet-rich plasma at 5-year follow-up: a prospective randomized study. Am J Sports Med. 2018;46(13):3134–41.
Mazzocca AD, McCarthy MB, Chowaniec DM, Cote MP, Arciero RA, Drissi H. Rapid isolation of human stem cells (connective tissue progenitor cells) from the proximal humerus during arthroscopic rotator cuff surgery. Am J Sports Med. 2010;38(7):1438–47.
McCarrel T, Fortier L. Temporal growth factor release from platelet-rich plasma, trehalose lyophilized platelets, and bone marrow aspirate and their effect on tendon and ligament gene expression. J Orthop Res. 2009;27(8):1033–42.
McLain RF, Fleming JE, Boehm C, Muschler G. Aspiration of osteoprogenitor cells for augmenting spinal fusion: comparison of progenitor cell concentrations from the vertebral body and iliac crest. J Bone Joint Surg Am. 2005;87(12):2655–61.
Milano G, Saccomanno MF, Careri S, Taccardo G, De Vitis R, Fabbriciani C. Efficacy of marrow-stimulating technique in arthroscopic rotator cuff repair: a prospective randomized study. Arthroscopy. 2013;29(5):802–10.
Morikawa D, Johnson JD, Kia C, et al. Examining the potency of subacromial bursal cells as a potential augmentation for rotator cuff healing: an in vitro study. Arthroscopy. 2019;35(11):2978–88.
Morikawa D, Muench LN, Baldino JB, et al. Comparison of preparation techniques for isolating subacromial bursa-derived cells as a potential augment for rotator cuff repair. Arthroscopy. 2020;36(1):80–5.
Muschler G, Boehm C, Easley K. Aspiration to obtain osteoblast progenitor cells from human bone marrow: the influence of aspiration volume. J Bone Joint Surg Am. 1997;79(11):1699–709.
Muschler G, Midura RJ. Connective tissue progenitors: practical concepts for clinical applications. Clin Orthop Relat Res. 2002;395:66–80.
Oh JH, Kim SH, Kim JH, Shin YH, Yoon JP, Oh CH. The level of vitamin D in the serum correlates with fatty degeneration of the muscles of the rotator cuff. J Bone Joint Surg Br. 2009;91(12):1587–93.
Patterson TE, Boehm C, Nakamoto C, et al. The efficiency of bone marrow aspiration for the harvest of connective tissue progenitors from the human iliac crest. J Bone Joint Surg Am. 2017;99(19):1673–82.
Pittenger MF, Mackay AM, Beck SC, et al. Multilineage potential of adult mesenchymal stem cells. Science. 1999;284(5411):143–7.
Randelli P, Arrigoni P, Ragone V, Aliprandi A, Cabitza P. Platelet rich plasma in arthroscopic rotator cuff repair: a prospective RCT study, 2-year follow-up. J Shoulder Elb Surg. 2011;20(4):518–28.
Ryu KJ, Kim BH, Lee Y, Dan J, Kim JH. Low serum vitamin D is not correlated with the severity of a rotator cuff tear or Retear after arthroscopic repair. Am J Sports Med. 2015;43(7):1743–50.
Taniguchi N, Suenaga N, Oizumi N, et al. Bone marrow stimulation at the footprint of arthroscopic surface-holding repair advances cuff repair integrity. J Shoulder Elb Surg. 2015;24(6):860–6.
Uhthoff H, Sarkar K. Surgical repair of rotator cuff ruptures - the importance of the subacromial Bursa. J Bone Joint Surg Br. 1991;73:399–401.
Yoshida R, Alaee F, Dyrna F, et al. Murine supraspinatus tendon injury model to identify the cellular origins of rotator cuff healing. Connect Tissue Res. 2016;57(6):507–15.
Zhao JG, Zhao L, Jiang YX, Wang ZL, Wang J, Zhang P. Platelet-rich plasma in arthroscopic rotator cuff repair: a meta-analysis of randomized controlled trials. Arthroscopy. 2015;31(1):125–35.
Zhong W, Sumita Y, Ohba S, et al. In vivo comparison of the bone regeneration capability of human bone marrow concentrates vs. platelet-rich plasma. PLoS One. 2012;7(7):e40833.
Zumstein MA, Ladermann A, Raniga S, Schar MO. The biology of rotator cuff healing. Orthop Traumatol Surg Res. 2017;103(1S):S1–S10.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 ISAKOS
About this chapter
Cite this chapter
Muench, L.N., Berthold, D.P., Mazzocca, A.D. (2021). The Failed Rotator Cuff: Diagnosis and Management—New Concepts in Biology of Repair. In: Savoie III, F.H., Calvo, E., Mazzocca, A.D. (eds) The Failed Rotator Cuff. Springer, Cham. https://doi.org/10.1007/978-3-030-79481-1_4
Download citation
DOI: https://doi.org/10.1007/978-3-030-79481-1_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-79480-4
Online ISBN: 978-3-030-79481-1
eBook Packages: MedicineMedicine (R0)