Abstract
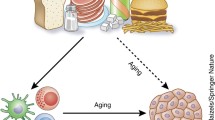
Changes in immunological pathways are involved in all stages of cancer. The immune system is composed of cells which are extremely sensitive to environmental changes. Antitumor immune response involves several pathways. The innate immune response is carried out by neutrophils, macrophages, eosinophils, mast cells, and natural killer (NK) cells, while the adaptive immune response is carried out by B-lymphocytes (B-cells) and T-lymphocytes (T-cells). Overall, lymphocytes act through the recognition of specific antigens circulating in the blood or on the cell surface. Connections between the innate and adaptive immune systems are made either by direct cell contact or by release of cytokines. Under normal conditions, inflammatory response is self-limiting because the production of pro-inflammatory cytokines (TH1 cytokines) is followed by generation of anti-inflammatory (TH2) cytokines such as interleukin (IL)-1, IL-10, or IL-13. Under special circumstances and defects in the resolution process or if its underlying factors continue, then inflammation will turn into chronic inflammation linked to increased risk of cancer. Chronic inflammation can increase the risk of cancer through promoting tumor initiation, the rate and extent of cell division, neovascularization, and angiogenesis. In addition, chronic inflammation results in an overload of reactive oxygen species (ROS), which, in turn, may lead to the development and progression of chronic diseases like cancer. Upregulation of cyclooxygenase (COX)-2, which is not expressed in most cells, may contribute to cancer development and progression through the release of prostaglandins (PGs). Signal transduction pathways like nuclear factor-kappa B (NF-κB) promote inducible expression of several proteins, such as cytokines, chemokines, acute-phase response proteins, cell adhesion molecules, antimicrobial peptides, inducible nitric oxide synthase (iNOS), and COX-2. Antitumoral immune response is mainly produced by T-cells to destroy tumor cells. However, immune escape mechanisms are a hallmark of tumor progression. Recent efforts have been devoted to develop small-molecule drugs that stimulate antitumoral immunity. While immunotherapy alone seems not to be sufficient to eradicate tumors, results of adjuvant immunotherapy are becoming ever more convincing. Bioactive dietary components that antagonize immune escape mechanisms would have potential to prevent tumor development or enhance tumor regression.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Points-
Under special circumstances and defects in resolution process or if its underlying factors continue, then inflammation will turn into chronic inflammation.
-
Chronic inflammation can increase the risk of cancer through promoting tumor initiation, the rate, and extent of cell division, neovascularization, and angiogenesis.
-
Chronic inflammation results in an overload of reactive oxygen species (ROS), which, in turn, may lead to the development and progression of cancer.
-
Immune escape mechanisms are a hallmark of tumor progression.
-
Bioactive dietary components that antagonize immune escape mechanisms would have potential to prevent tumor development or enhance tumor regression.
Dietary Components, Immunity, and Cancer
Acetylsalicylic acid is a nonsteroidal anti-inflammatory drug (NSAID) that has shown chemopreventive effects in animal models and to reduce both inflammation and cancer risk in humans [1]. Salicylic acids exist in a wide range of fruits, vegetables, herbs, and spices. It has been shown that regular intake of salicylates may be causally associated with reduced incidence of certain cancers, especially colon cancer [2].
Macronutrients and Immune System Modulation
Amino Acids
Arginine and glutamine are depleted during the immune response. Arginine is a precursor of polyamine, which is necessary for fidelity of DNA transcription. In addition, arginine is the only substrate for iNOS. Because of reduced arginine concentrations in plasma, T-cells are downregulated by the accumulation of myeloid-derived suppressor cells (MDSCs) and arginase-1 secretion. Glutamine plays a role to sustain lymphocyte proliferation, increase phagocytosis by onocytes/macrophages, and enhance neutrophil cytotoxicity [3]. On the other hand, sulfur amino acids are essential for the generation of glutathione, acting against prooxidant effects of inflammation and aiding cytotoxic T (TC)-cell activation [4].Tryptophan is another important anti-inflammatory molecule, which is found in various types of vegetables and fish. Tryptophan is converted into indole-3-aldehyde, the ligand of aryl hydrocarbon receptor (AhR), by bacterial enzymes (e.g., lactobacilli). AhR functions as a receptor for dietary components and as a transcription factor expressed in epithelial and immune cells and some tumor cells. Several phytochemicals and plants from the Brassicaceae family have been shown to influence AhR ligands. Anti-inflammatory effects of tryptophan can occur through conversion of indoleamine-2,3-dioxygenase to kynurenine. Both indoleamine-2,3-dioxygenase (IDO) and kynurenine modulate T-cell function. Moreover, kynurenine which is produced by cancer cells can suppress antitumor immune responses [5, 6]. AhR can mediate the effects of diet to produce anti-inflammatory effects by affecting microbiota and gut immunity.
Lipids
Increasing the ratio of n-3 to n-6 polyunsaturated fatty acids (PUFA) (n-3/n-6) is generally in favor of human health. High n-3/n-6 ratio has been associated with increased anti-inflammatory responses and decreased risk of cancer. Inflammatory cells display high proportions of n-6 PUFA and low proportions of n-3 PUFA; thus, enhancing the dietary intake of n-3 PUFA could affect the amount and type of endogenously produced eicosanoids [7]. High intake of n-3 PUFA causes replacement of arachidonic acid (AA) in inflammatory cell membranes by eicosapentaenoic acid (EPA) and decreased generation of AA-derived mediators that regulate the secretion of cytokines. Other possible effects may occur through modification of membrane fluidity and lipid rafts and also changes in the gene expression and antigen production associated with signal transduction [8]. For instance, a highly purified form of n-3 PUFA, docosahexaenoic acid (DHA), not only altered the composition of T-cell membrane but also downregulated signaling pathways of activator protein-1 (AP-1), NF-κB, and IL-2 and lymphoproliferation. Also, it has been reported that omega-3 can decrease the expression of pro-inflammatory adhesion molecules, including vascular cell adhesion molecule (VCAM)-1, intracellular adhesion molecule (ICAM)-1, and E-selectin [9]. Short-chain fatty acids (SCFAs), e.g., acetate, butyrate, and propionate, which are produced by colonic bacteria appear beneficial for regulatory T (Treg)-cell proliferation [10, 11]. Phase III clinical trials have been published confirming the efficacy of omega-3 supplementation in some types of cancer.
Minerals
Trace elements, in particular, zinc, iron, and selenium, play a key role in the regulation of immune responses [12]. Zinc deficiency can cause a shift from TH1 to TH2 immune responses, result in the activation of macrophages and monocytes, and increase the production of pro-inflammatory cytokines (tumor necrosis factor-alpha (TNF-α), IL-1β, IL-6, and IL-8) [13, 14]. Selenium has been most strongly associated with cancer risk [15]. Selenium not only does act as an antioxidant by participating in the structure of glutathione peroxidase but also can decrease the sensitivity of lymphocytes to oxidative stress (OS). Its deficiency decreases neutrophil chemotactic activity and antibody generation by B-cells. By contrast, supplementation with selenium would increase phagocytosis, NK cell activity, and T-cell responses [16].
Vitamins
Retinoic acid, the active metabolite of vitamin A, contributes to the activation of nuclear factor receptors-α (RARα), RARβ, and RARγ, which are essential for the stability of TH1 cells and for controlling conversion from TH1 cells to TH17 cells. Antioxidant vitamins like vitamins C and E are able to scavenge free radicals [17]. Vitamin B6 significantly affects the expression of iNOS and COX-2 induced by lipopolysaccharide (LPS). This vitamin inhibits the induction of NF-κB by LPS and leads to a reduction of LPS-induced I-B degradation in RAW cells. Vitamin D and calcium deficiencies interfere with cellular functions in multiple tissues and organs, including the immune system [18]. Betaine (trimethylglycine) is a vitamin-like substance that acts as a methyl donor. Study of aged Sprague Dawley (SD) rats showed that this nutrient has the ability to reduce renal expression of genes encoding inflammatory mediators such as NF-κB, COX-2, iNOS, VCAM-1, and ICAM-1 [19].
The relation of vitamin D3 to immune function and cancer has been the subject of numerous studies. Besides immune cells (macrophages, monocytes, dendritic cells (DCs), and dermal cells), the 25-hydroxyvitamin D3 is metabolized to 1,25-dihydroxyvitamin D3 in the kidneys. Genes that show differential expression in response to vitamin D include nuclear factor of activated T-cells (NFAT), nuclear factor of activated B-cells (NFAB), epidermal growth factor receptor (EGFR), c-myc, and keratin (K16). Vitamin D as an alternative to classical immunosuppressive agents is used in secondary malignancies. Vitamin D supplement has been beneficial for patients with prostate, breast, and colorectal cancer (CRC) and melanoma. Studies support its potential as an adjuvant for cancer [20, 21]. Vitamin D supplement improved disease-free survival in patients with early-diagnosed breast cancer and metastatic CRC. There was a positive association between disease-free survival and plasma 25-(OH) D3 levels [22].
Vitamin E improves immune function through its antioxidant property. Antioxidant parameters including superoxide dismutase (SOD), catalase (CAT), glutathione (GSH) enzyme family, and vitamins C and E have the potential to serve as biomarkers of prostate cancer [23]. Daily intake of greater than 100 IU vitamin E has been demonstrated to reverse T-cell function impaired by senescence [24]. Additionally, a Bayesian meta-analysis has clearly proved the safety of vitamin E [25]. In vitamin C deficiency, phagocytic activity is impaired because of low neutrophil numbers and reduced NK cell functions [26]. Results from a meta-analysis point to the benefit of decreased mortality that patients diagnosed with breast cancer obtain from vitamin C supplement.
Dietary Bioactive Compounds and Cancer Prevention Through γδ-T-Cells
About 30% of all malignancies in the Western world are estimated to be diet related, where overconsumption of definite food items or not enough of others in whole diet may contribute to cancer incidence [27]. Thus, cancer appears to be potentially preventable or modifiable by suitable dietary interventions. For example, fruit and vegetable consumption reduces the risk of bladder [28, 29] and gastric cancer [30, 31]. Also, reduced risk of prostate cancer has been reported to be in association with cruciferous vegetable consumption and high vitamin C intake [32, 33]. Dietary components can modify the risk of cancer by affecting various processes, including DNA repair, differentiation, apoptosis, angiogenesis, and modification of immune responses. As suppression of immunity is associated with increased risk of cancer, maintenance of immune homeostasis may have the potential to decrease cancer risk [34]. This part will address γδ-T-cells, their ability against malignant cells, and diet-mediated changes in γδ-T-cell function. Several in vivo and in vitro studies reported that certain food components might modify γδ-T-cell differentiation and function. We will discuss the possible effect of dietary bioactive compounds in preventing cancer through γδ-T-cell-based mechanisms.
Based on the T-cell receptor (TCR) on their surface, there are two main subgroups of T-cells: αβ-T-cells that account for about 95% of T-cells in peripheral blood and γδ-T-cells that account for 0.5–5% of all T-lymphocytes [35, 36]. αβ-T-cells commonly express CD4 or CD8 lineage markers [35]. αβ-T-lymphocytes mostly belong to helper or cytotoxic/effector subsets [37, 38]. On the contrary, γδ-T-cells do not generally express CD4 or CD8 lineage markers. T-lymphocytes usually recognize antigenic peptides by major histocompatibility complex (MHC). However, γδ-T-cells do neither require conventional MHC antigen presentation [35] nor recognize peptide antigens on antigen-presenting cell (APC) surfaces. In fact, these cells are activated in the way similar to that of the innate immune cells, meaning through recognition of pathogen-associated molecular patterns (PAMPs) [39, 40], damaged tissue [41, 42], and targets of NK-associated receptors [43, 44]. Phosphorylated uridine and thymidine compounds [45], non-protein prenyl pyrophosphates [46, 47], bisphosphonates [47, 48], and alkylamines [49, 50] have all been reported to activate or prime γδ-T-lymphocytes. Alkylamines can be obtained from the diet and include compounds such as ethylamine, butylamine, and propylamine. Other PAMPs include heat shock proteins [51] and intermediates from the mevalonate pathway which is induced in response to self’s distress signals [52]. The mevalonate pathway is common to all cells, particularly malignant cells, which can be influenced by several dietary factors such as cholesterol, isoprenoids, and genistein [53].
There are two main subsets of γδ-T-cells in mammalian species: Vδ2-T-cells which are mainly found in circulation and Vδ1-T-cells which are specific to mucosal surfaces lining the respiratory, gastrointestinal, urinary, and reproductive tracts [54]. Circulating γδ-T-cells produce effector functions against invading pathogens and malignant cells and could migrate to sites of infection [55]. The mucosal population assists in the maintenance of epithelial barrier integrity through diminishing inflammatory responses and healing of the damaged tissue [57,58,58]. γδ-T-cells are on the frontline to respond to invading pathogens and pave the way for the rest of the immune cells to participate in the elimination of invading pathogens.
γδ-T-cells share features of both innate and adaptive immune cells [59]. These cells produce high amounts of cytokines, chemokines, and growth factors. In this respect, the most important cytokine is interferon (IFN)-γ which is involved in antitumor immune responses [60]. In addition, γδ-T-cells support humoral immunity by the production of IgA, IgM, and IgG antibodies [61]. Other important roles include recruiting macrophages and inducing cytotoxicity in malignancies by producing a variety of chemokines like perforin-granzyme and TNF-related apoptosis-inducing ligand (TRAIL)/TRAIL receptor (TRAILR) system [62].
γδ-T-Cells in Cancer
γδ-T-cells can directly reject tumor cells through different ways. They have the ability to secrete cytokines such as IL-4, IL-10, TNF-α, and IFN-γ [61, 63, 64] which promote antitumor immunity. By increasing the expansion of CD8+ T-cell, monocytes, and neutrophils and upregulating the expression of Fas ligand (FasL) and TRAIL, γδ-T-cells enhance tumor killing activity in the Fas- or TRAIL receptor-sensitive tumors [65, 66]. CD16 is a receptor for the Fc portion of immunoglobulin G (Fcγ receptors). γδ-T-cells by expression of CD16 can increase antibody-dependent cellular cytotoxicity (ADCC) [67]. In addition, γδ-T-cells elicit the release of granzymes and perforin that mediate cellular apoptosis [68] and interact with professional APCs that process antigens important for the killing of target cells [69]. Another function of the γδ-T-cells is the ability to moderate or end inflammation by inhibition of macrophage activation [70, 71]. Interestingly, antigens in bioactive dietary compounds that resemble PAMPs can prime γδ-T-cells, thereby attenuating inflammation and cell damage, which have been implicated in cancer.
Bioactive Dietary Compounds and Possible γδ-T-Cell Activity Against Cancer
The modified function of γδ-T-cells by dietary bioactive compounds may cause favorable immunological response. Information regarding the effect of dietary compounds on differentiation of γδ-T-cells is limited. Vitamins A and D have been reported to play a role in γδ-T-cell differentiation [72]. Vitamin D receptor on the surface of γδ-T-cells is upregulated via a protein kinase C (PKC)-related mechanism [73]. The relationship between diet and γδ-T-cells was first drawn in 1999 [74], when drinking tea increased γδ-T-cell proliferation and IFN-γ secretion compared with coffee. L-Theanine is a bioactive compound available in tea. L-Theanine is hydrolyzed to glutamic acid and ethylamine, a nonmicrobial antigen that interacts with γδ-T-cells [75, 76]. Two classes of plant metabolites have been characterized with defined effects on γδ-T-cells, including non-protein prenyl pyrophosphates [77] and procyanidins [78] that induce Vδ2-T- and Vδ1-T-cells, respectively. Many other bioactive compounds are being investigated.
The hypothesis of nonmicrobial priming implies that though food phytochemicals cannot activate cells, they can prime the cells to respond better and more rapidly to a secondary antigen [79]. Previous in vitro experiments indicated that proanthocyanidins interact with γδ-T-cells and increase their proliferation and activation [80].
In a previous study, consumption of fruit and vegetable concentrate increased γδ-T-cells in the blood while decreasing circulating IFN-γ concentrations [81]. In another study, a capsule containing a standardized mixture of tea components, L-theanine and catechins, was reported to influence γδ-T-cell function. People consumed a distinct amount of L-theanine and catechins for 10 weeks. White blood cells (WBC) from the participants were incubated ex vivo, with the compound responsible for priming, ethylamine. Greater activation and proliferation of γδ-T-cells and greater concentration of IFN-γ were observed in subjects consuming L-theanine compared with placebo. As a side note, subjects taking the capsule experienced fewer cold and flu symptoms during the study [82, 83].
Mistletoe has been reported to increase levels of IL-12 [84], a cytokine that supports the proliferation and cytotoxicity of γδ-T-cells [85]. In another study, mistletoe extracts (50–500 mg/L) increased proliferation of γδ-T-lymphocytes in vitro in a dose-dependent manner [86]. In two strains of mice, at first food allergy was established with ovalbumin sensitization; and then feeding apple condensed tannins (ACT) resulted in much less severe anaphylaxis, lower histamine levels, and decreased serum levels of IgE, IgG1, and IgG2a. γδ-T-lymphocytes were significantly increased in the intestinal epithelium of those consuming ACT [87]. In another in vitro experiment, a quite low concentration (20–40 mg/ml) of apple polyphenols upregulated CD11b on γδ-T-cells [88].
Dietary nucleotides have been indicated to change the percentage of intestinal intraepithelial γδ-T-cells [89]. Adding 0.4% nucleotides to the regular diets of weanling mice for 2 weeks increased γδ-T-cell proportion from 50.6% to 58.7% and increased secretion of IL-7, but not IL-2 or IFN-γ.
Different dietary oils have been investigated regarding their possible effect on γδ-T-cells. In one study, splenic γδ-T-cells were statistically higher in the safflower oil diet compared with the fish oil diet. The possible response to n-6/n-3 fatty acid ratio has been suggested [90]. Conjugated linoleic acid (CLA) has also been reported to almost double the number of γδ-T-cells in pigs fed 1.33 g CLA/100 g diet for 72 days [91]. Vaccination combined with CLA increased γδ-T-cell numbers largely (sixfold).
Alkylamine compounds produced by gut microbiota have been shown to prime γδ-T-cells [50, 92]. Furthermore, they can be obtained from dietary sources, such as kola nuts [93], tea, apple skins, mushrooms, and cucumbers [92]. Drinking tea increases urinary ethylamine [75]. When mixed with peripheral blood mononuclear cells (PBMCs), ethylamine could cause a 15-fold increase in the number of γδ-T-cells [92]. In addition, the secretion of IFN-γ in PBMCs incubated with ethylamine and challenged with bacteria was shown to be stimulated by alkylamines [50, 92]. Consumption of tea caused a two- to threefold increase in the capacity of γδ-T-cells to secrete IFN-γ in response to bacterial pathogens or nonpeptide antigens.
A trial in healthy individuals showed that regular consumption of Concord grape juice for 9 weeks significantly increased the number of circulating γδ-T-cells [94]. Consumption of Lentinula edodes (shiitake) mushrooms for 4 weeks also led to an increase in ex vivo proliferation of γδ-T- and NK T-cells and in sIgA production [95]. Studies also investigated the effects of aged garlic extract (AGE) in healthy subjects [96] and patients with cancer [97]. Although not many γδ-T-cells were found in the serum, they were expanded in the epithelial linings of the gastrointestinal, respiratory, and genitourinary tracts [96]. A trial in healthy subjects revealed that the proliferation index of γδ-T-cells was almost five times increased after a 10-week cranberry juice consumption [98]. Other plant preparations with γδ-T-cell agonist activity include compounds from Funtumia elastica bark, Angelica sinensis root, cocoa, cat’s claw bark, grape seed extract, and safflower oil [100,101,102,102]. Recent evidence reveled that grape seed extract has potent γδ-T-cell agonist activity. On the other hand, cocoa extracts caused expansion of rat γδ-T-cells in vivo [101] to some degree similar to that observed with apple-derived procyanidins [87]. Of note, the expansion of γδ-T-cell population particularly occurred in intestinal and Peyer’s patches after oral administration of procyanidins. Rats feeding cocoa showed an increase in intestinal γδ-T-cells and a decrease in production of secretory IgA [87, 101].
In one study in mice, the effect of methanol extract from Chelidonium majus was investigated in collagen-induced arthritis. Chelidonium majus decreased B-cell and γδ-T-cell numbers (in spleen) while increasing the proportion of CD4+CD25+ Treg cells [103]. The production of cytokines (TNF-α, IL-6, and IFN-γ) and the levels of IgG and IgM RA factors were decreased as well [103]. One experiment showed that condensed tannins derived from the unripe peel of the apple fruit act as agonist for both human Vδ1- and Vδ2-T-cells and increase the expression of IL-2R and cell proliferation. Previous studies reported that glutamine prevents apoptosis of small intestinal γδ-T-cells and downregulates the expression of inflammatory mediators by γδ-T-cells in septic mice [104, 105].
However, it has been discussed that many of the bioactive compounds in diet are only absorbed minimally, and their ability to influence immune responses throughout the body is therefore argued. However, it must be noted that several bioactive compounds do not need to be absorbed by the body to modify immune cells. For example, such compounds may be metabolized by the microbiota, and intermediates which are absorbed in the colon influence circulating immune cells. However, this has not been proven yet. Furthermore, Peyer’s patches and intraepithelial cells lining the microvilli contain several immune cells, many of which express γδ-TCR. In addition, gut immune cells are able to move in and out of tissues via the circulation and the lymphatic system [106]. In this manner, blood-borne γδ-T-cells would be influenced by bioactive compounds which have not yet been absorbed.
Although tumoricidal activity of bioactive food compounds has not been clearly shown, certain food components are known to prime γδ-T-cells. When primed cells encounter a malignant cell, they can respond faster and more efficiently in terms of increased production of cytokines. However, enhancement of immune function is not always favorable; it is associated with decreased risk of cancer on one side, and on the other side, it has the potential to increase the risk of autoimmune diseases such as inflammatory bowel disease [107] and celiac disease [108]. Further research is necessary to investigate the relevance of using bioactive food components as regulators of γδ-T-cell function. If results support the hypothesis of priming γδ-T-cells, then this would propose a mechanism by which dietary factors can reduce the risk of cancer.
Cocoa, Immunity, and Cancer
Cocoa, the dried, roasted, and either unfermented or fermented seeds derived from Theobroma cacao tree, has been consumed by ancient civilizations such as the Mayans and Aztecs [109, 110]. Cocoa or cacao contains the highest flavanol content of all foods on a weight basis and is a significant contributor to total dietary flavonoid intake [111]. It is worth mentioning that manufacturing processes increase flavonoid contents of cocoa four times greater than in conventional cocoa powder [112]. In this respect, fermented cocoa contains high quantities of flavonoids, flavanols (also called flavan-3-ols), (−)-epicatechin (EC), and (+)-catechin and to a lesser extent other polyphenols such as quercetin, naringenin, luteolin, and apigenin [113]. When compared to other flavonoid-containing foodstuffs, cocoa and its derivatives contain high concentrations of procyanidins, which are weakly absorbed through the gut barrier [114, 115]. The procyanidins in cocoa are unique because they exist as long polymers, prepared through polymeric condensation by two, three, or up to ten linked units of catechin or epicatechin [116] formed during fermentation [117]; thus, their favorable effects would be restricted to the gastrointestinal tract. These compounds represent 60% of the total polyphenol content in cocoa products [118, 119]. Cocoa and its products are generally consumed around the world because of highly attractive organoleptic characteristics [118]. Absolutely, cocoa and its derivatives constitute a larger proportion of the diet of many individuals than green tea, wine, or soybeans [118]. However, health benefits of cocoa flavonoids depend on their bioavailability (absorption, metabolism, and elimination) [120]. Of note, oligomers and polymers of flavanols that are not absorbed in the intestine can be metabolized by gut microbiota into various metabolites with low molecular weight, which tend to be well-absorbed through the colon and possess biological properties [121].
Intake of flavonoid-rich foods that possess antioxidant properties can have health effects [122]. Over the last few years, evidence emerged suggesting health benefits of cocoa phenolics, especially prominent for their metabolic and cardiovascular effects. These effects may be due to antioxidant and antiradical properties of cocoa bioactive compounds. Along with their antiplatelet effects [123], cocoa phenolics can be protective against heart diseases [124]. In addition, they have the capacity to modify the immune responses and produce anti-inflammatory and anticarcinogenic effects [125].
Below is an overview of evidences suggesting cocoa products as a cancer-protective factor. In particular, data from epidemiological studies support protective effects of cocoa and chocolate against cancer. Then, it would be also interesting to unravel potential biologic mechanisms through which cocoa phenolics can modify immune processes, thereby protecting against cancer. The focus is mainly to show anti-inflammatory and antioxidant effects of cocoa, which are known to decrease cancer risk. Inflammation provides a microenvironment appropriate for angiogenesis and therefore tumor growth [126]. Consistently, prospective studies have linked high levels of pro-inflammatory mediators such as IL-6, CRP, and TNF-α to increased risk of cancer in [127, 128]. An inflammatory response can result in the overproduction of ROS, which, in turn, would exacerbate the condition through oxidative stress.
Epidemiological Studies
Exposure to low doses of carcinogens may happen continuously during a lifetime. Furthermore, the body’s response to carcinogens and chemoprotective agents depends upon several factors such as genetic polymorphisms and epigenetic modifications [129]. Few epidemiological studies have investigated the link between cancer-related mortality and cocoa, and consequently there is a limited support for the efficacy of cocoa for cancer-related mortality. Therefore, large-scale and long-term controlled trials are necessary to confirm cancer preventive effects of foodstuffs. Below provides a summary of existing studies by type. A review of epidemiological studies on polyphenols has previously addressed the link between catechin intake and cancer risk [130].
Case-Control Studies
Data supporting cancer preventive effects of cocoa in humans come mostly from the Kuna tribe in Panama. Kuna islanders drink flavanol-rich cocoa as their major cocktail. Studies have found lower mortality rates for cancer and other chronic diseases among islanders than in mainland Panama. However, the finding should be treated with caution due to uncertainties arising from confounding factors [131]. Case-control studies have frequently investigated the relation between cocoa and cancer. They linked flavonoid consumption and procyanidin intake to decreased risk of gastric cancer [132]. In addition, higher catechin intake reported to be associated with lower rectal cancer incidence in postmenopausal women [133]; and higher consumption of epicatechin, anthocyanidin, and procyanidin was protective against non-Hodgkin lymphoma [134]. Although intake of these phenolic compounds has been associated with reduced risk of cancers [130, 135], the nutrition source for these bioactive compounds remains to be identified. Moreover, there are studies that failed to show the efficacy of cocoa intake in decreasing risk of cancer. For example, there was no relation between chocolate and cocoa intake and the incidence of any stage of colorectal diseases ranging from polyps and adenomas to CRC [136]. Lack of correlation might lie in the lower intake of flavanols (with a small percentage of cocoa-like milk chocolate) and/or low study power [136]. In another study, CRC risk was decreased by about 26% for epicatechin and by about 22% for procyanidins [136]. In a case-control study, procyanidins were associated with a lower risk of CRC. Interestingly, the higher the degree of polymerization of procyanidins, the lower the risk of CRC [137].
Cohort Studies
Four prospective cohort studies assessed the effect of cocoa and chocolate intake on mortality and cancer outcomes: Iowa Women’s Study [133], the Zutphen Elderly Study from the Netherlands [138], the Harvard Alumni Study [139], and the Leisure World Cohort Study [140]. In the first study, no separate risk estimates of rectal cancer were shown for chocolate [133]. In the study [141], no association was found between chocolate intake and non-Hodgkin lymphoma, though total procyanidin consumption was protective, with a 30% lower hazard for the category with the highest consumption. Overall catechin consumption was associated neither with epithelial cancer nor with lung cancer after adjustment for confounders. However, nonsignificant inverse association was present between intake of catechins from cocoa and chocolate and incidence of lung and all epithelial cancers. In the Harvard Alumni Study, individuals who consumed candy 1–3 times per month had a 27% lower risk of mortality [139]. In the study [140], frequent chocolate consumption was not associated with lower mortality risk, but mortality seemed to decrease (about 6%) in people with occasional chocolate intake.
Intervention Studies
To our knowledge, no clinical trial on the effectiveness of cocoa and chocolate intake for cancer prevention is available. However, few human studies report that cocoa favorably affects intermediary factors in cancer progression, in particular inflammation and oxidative stress [143,144,145,145]. Recent studies focused on the modification of antioxidant and anti-inflammatory status by consumption of cocoa derivatives. One trial [146] has demonstrated that dark chocolate intake significantly improved DNA resistance against oxidative stress. Cocoa consumption reduced NF-κB activation in PBMCs of healthy volunteers [147]; but other biomarkers of inflammation, including IL-6, remained unaltered in a group of patients with cardiovascular diseases after cocoa powder intake [146].
Evidence for cancer chemoprevention by flavonoids comes from different study types. Antitumoral effects of flavonoids occur through induction of apoptosis and inhibition of several kinases and transcription factors, angiogenesis, and cell proliferation. Further, cocoa and its bioactive compounds have shown antitumoral effects independent of antioxidant function [115, 148, 149]. However, whether it works in humans remains to be addressed. Below different pathways and molecular targets whereby cocoa and their bioactive compounds interfere with cancer cells are reviewed.
Antioxidant and Antiradical Activities of Cocoa
Polyphenols are able to capture ROS which have been implicated in carcinogenesis. One serving of cocoa or chocolate has antioxidant capacity (AOC) that exceeds the antioxidant capabilities of many foodstuffs [118]. The cocoa procyanidins, epicatechin, and catechin have important antioxidant abilities [150, 151]. Genome analysis of human colon adenocarcinoma cell line (Caco-2 cells) revealed that polyphenolic cocoa extract can modulate the expression of numerous genes involved in cellular response to OS [152]. Phenolic compounds from cocoa inhibit lipid peroxidation in microsomes and liposomes. The polyphenolic cocoa extract increased mRNA levels, protein levels, and enzymatic activity of CYP1A1 in MCF-7 and SKBR3 breast cancer cells [153]. The cocoa polyphenolic extract led to inhibition of ROS generation and xanthine oxidase activity in stimulated myelocytic leukemia HL-60 cells [154]. In vivo studies also demonstrated the protective effect of cocoa in rodent models of CRC and lung cancer and liver injury [155, 156]. In a lymphoma model, the albumin fraction of semifermented dry cacao showed free radical scavenging capacity [157]. The cacao is, therefore, the source of potential antitumor agents. Upregulation of cytoprotective enzymes like Kelch-like ECH-associated protein 1 (Keap1) and its binding partner, transcription factor NF-E2-related factor-2 (Nrf2), which are involved in antioxidant response element (ARE), by therapeutic agents like cocoa and its phenolic compounds can subsequently activate ARE [158]. Epicatechin has been described to act through this pathway as well [159]. Human studies also showed similar results with an increase in plasma AOC and a decrease in plasma lipid oxidation [143, 160].
Cocoa and Immunity
Several studies of cocoa’s effects on the immune system have been published in recent years. In vitro and in vivo models have investigated both the innate and adaptive immunity. Most in vitro experiments of cocoa and its components have focused on inflammatory mediators released by macrophages. Some studies tested the effects of cocoa administration in several models of inflammation. Human studies investigating the relation between cocoa and innate immune responses are scarce and provide inconsistent results. One study showed no significant effect of cocoa on inflammatory markers in a group of healthy subjects [142]. However, another study reported that regular intake of dark chocolate by healthy humans was inversely associated with serum C-reactive protein (CRP) concentrations [161]. In vitro, on cultured lymphoid cells or PBMCs, and in vivo models also have investigated the influence of cocoa on adaptive immune response.
An Overview of Inflammation in Cancer
Inflammation is a feature of innate immunity, and chronic inflammation is a contributing factor to the initiation and progression of cancer. Chronic inflammation acts as a trigger for premalignant and malignant transformation of cells. About 20% of all cancers are related to chronic inflammation resulting from infections and autoimmune diseases [162]. The association between inflammation and cancer involves key inflammatory mediators. Several inflammatory mediators, like NF-κB, TNF-α, and COX-2, have been related to cell proliferation, antiapoptotic activity, angiogenesis, and metastasis [163, 164]. Inflammatory cytokines and cells have been broadly recognized in cancers of the stomach, colon, skin, liver, breast, lung, and head/neck [165]. Inhibition of COX-2 and iNOS has shown protective effects against tumor development in animal models, suggesting that they are crucial targets for tumorigenesis. Inflammation can enhance mutation rates and proliferation of mutated cells. Inflammatory cells are sources of ROS that are able to induce genomic instability and DNA damage. More precisely, cells may use cytokines such as TNF-α to increase ROS in adjacent epithelial cells [166, 167]. On the other hand, NF-κB, which regulates the expression of iNOS and COX-2, is constitutively active in neoplastic cells, posing a hazard to the development of cancer. The pro-tumorigenic function of TNF-α and IL-6 released by immune cells is well established. The role of TNF-α and IL-6 as master regulators of tumor-associated inflammation and tumorigenesis makes them striking targets for adjuvant therapy in cancer [163]. Diet can also contribute to chronic inflammation that facilitates the development of gastrointestinal cancers. Chronic consumption of alcohol activates mast cells, causes polyp formation, and enhances tumor formation and invasion in a mouse model of colon cancer. In addition, red meat contains high levels of N-glycolylneuraminic acid. This foreign antigen can get incorporated into tissue and attract inflammatory cells [165]. Inflammation can also modulate composition of the gut microbiota, assisting growth of harmful bacteria such as Escherichia coli, which are present in higher concentrations in patients with CRC. Colitis can cause tumorigenesis by changing microbiome toward a population more capable of inducing gene damage and mutagenesis [165]. Therefore, the use of chemopreventive substances that decrease inflammation seems to be a helpful approach to control the development and progression of cancers. For example, NSAIDs or selective blockers by inhibition of COX activity, which fuels cancer-related inflammation through prostaglandin E2, decrease the risk of some type of cancers including colon and lung cancer. However, further clinical studies are necessary to determine the possible benefits and risks of long-term NSAID use for cancer prevention and treatment [165]. For more information about the role of inflammation in cancer, see comprehensive reviews [162, 164, 168].
Anti-inflammatory Effects of Cocoa and Cancer
Different anti-inflammatory effects of cocoa extracts have been reported. Cocoa extract and EC decreased TNF-α, IL-1a, IL-6 expression and NO secretion in different cells. Cocoa phenolic extract inhibited phosphorylation of AKT and ERK induced by TNF-α and suppressed MEK1 (mitogen-activated protein kinase kinase-1) and phosphatidylinositol-3-kinase (PI3K) activity induced by TNF-α, suggesting a potential chemopreventive effect against pro-inflammatory cytokine-mediated skin cancer and inflammation [169]. Cocoa polyphenols reduced phosphorylation of TNF-α-induced c-Jun N-terminal kinase (JNK) and nuclear translocation of NK-κB [170]. High-molecular-weight polymeric procyanidins from cocoa decreased TNF-α-induced IL-8 in human colon cancer HT-29 cells [171]. Cocoa flavanols have demonstrated a critical role in the prevention of neoplastic lesions in CRC [172]. Feeding animals with a 12% cocoa-enriched diet suppressed intestinal inflammation induced by AOM through the inhibition of NF-κB signaling and downregulation of COX-2 and iNOS [170]. These effects suggest the chemopreventive effect of a cocoa-rich diet on colon inflammation and preneoplastic lesions. In another study, supplementation with dark chocolate decreased cell proliferation and downregulated transcription levels of COX-2 and RelA resulting in a lower number of preneoplastic lesions [173].
Other studies reported several possible immunological effects of cocoa and cocoa flavonoids on cancer models.
Cancer Immunity Cycle
The immune system is able to recognize tumor antigens. However, mechanisms for immune escape are a hallmark of cancer progression [174]. Antitumoral activity of the immune system involves different immune cells such as NK cells, dendritic cells (DCs), macrophages, and T-cells [175]. DCs capture tumor antigens, leading to activation and priming of effector T-cells (Teff) against tumor-specific antigens in lymph nodes [176]. DCs present antigens bound to major histocompatibility complex (MHC) molecules. Activated Teff infiltrate in tumor, recognize malignant cells, and kill them. DCs capture antigens from dying tumor cells, and this would trigger the cycle over again. Naïve T-cells cannot be activated exclusively by recognition of cancer-specific peptide-MHC I complexes by T-cell receptor (TCR). Additional activator signals must be present involving pro-inflammatory cytokines (e.g., TNF-α, IL-1, IFN-α) [177], factors released by killed cancer cells such as high mobility group box 1 (HMGB1) and cyclic dinucleotide (CDN) [178], and Toll-like receptor (TLR) signaling. Because killing of cancer cells is accompanied by release of tumor-associated antigens and increased activation of Teff, it is expected that antitumor responses should occur repeatedly. However, different mechanisms help tumor cells to escape the immune system. For example, many tumors suppress MHC expression, thus masking their presence from TCR. In addition, after infiltration of Teff into cancer cells, activation of inhibitory signaling pathways in local microenvironment would reduce T-cell function. Inhibition of these pathways by immunological drugs removes cell intrinsic inhibitory pathways that block effective antitumor cell response [180,181,181].
Recent studies have suggested paradoxical roles of regulatory T (TREG) cells in cancer [182]. FOXP3C CD4C CD25C/high TREG cells are involved in the modulatory action of the immune system and, in particular, are valuable for coordinating control of peripheral immunological tolerance [183, 184]. The transcription factor FOXP3 is a critical regulator of TREG cell function. TREG cells provide the machinery for immune homeostasis during infections by inducing useful inflammatory responses while minimizing collateral tissue injury. However, TREG cell function in cancers is widely regarded as negative [185,186,187]. In fact, an increased number of TREG cells have been reported in patients with head and neck, pancreatic, stomach, breast, and liver cancers [181]. Tumor-associated TREG cells pose a major challenge in vaccine therapy for cancers [185, 187, 188]. Therefore, several anti-TREG regimens have been developed that rely on depletion of TREG cells and inhibition of their suppressive function, their residence into tumors, and/or their differentiation/proliferation [185, 186]. For instance, anti-CTLA-4 (cytotoxic T-lymphocyte-associated antigen-4) immunotherapy that has shown promising results [189] depletes TREG cells from tumor tissues [189]. Chronic inflammation mediated by cytokines and ROS may cause cell injury in target cells and therefore may contribute to cancer development. Mounting evidence suggests that tumor-associated inflammation is a tumor-promoting event. The reason is that inflammation can support cancer cell survival through DNA damage and development of a tumor stroma.
Almost immediately after birth, the gastrointestinal (GI) tract changes from sterility to a large ecosystem with hundred trillion microbial organisms, representing the most densely populated ecosystem known so far [190]. The overall population of intestinal colonies including bacterial, fungal, and viral communities is referred to as the gut microbiota. The microbiota include more than 1500 bacterial species, which are estimated to encode more than 150 times more genes than human genome. The gut microbiota is in intricate and reciprocal interaction with the human host and nutrients, providing a metabolic engine important for GI health and disease. This highly regulated and complex ecosystem plays an important role in priming the immune system and maintenance of intestinal immune homeostasis [191, 192]. Besides metabolic effects, the gut microbiota affects tissue development and inflammation [193,194,195,196]. Providing a physical barrier against pathogens and supplying immunological surveillance signals are other functions of the gut microbiota. There should be an ability to maintain the balance between tolerance toward microbiota and surveillance against pathogens. Such ability comes from the cross talk between the intestinal microbiota and host that involves both innate and adaptive immunity [197,198,199]. The hygiene hypothesis reflects the fact that the lack of exposure of the gut to harmless microorganisms, called “old friends,” in infancy causes certain deficiencies in the immune system at later age. A number of immunological disorders such as allergic diseases, inflammatory bowel diseases, type 1 diabetes, and multiple sclerosis are thought to result from an imbalance in the function of the regulatory immune system. Proper discrimination between harmful and harmless pathogens involves a family of cell surface and cytosolic receptors of the innate immunity, called pattern recognition receptors (PRRs). PRRs including Toll-like receptors (TLRs), C-type lectin receptors (CLRs), and nucleotide-binding oligomerization domain proteins (NOD proteins) recognize PAMPs and damage-associated molecular pattern (DAMPs). Interestingly, both harmful and harmless bacteria express these PAMPs. In this manner, pathogenic bacteria can pass through the epithelial barrier and activate inflammatory cascade through increased NF-κB translocation, on one side, and on the other side, commensal bacteria do not invade epithelial cells and do not stimulate inflammatory responses [200,201,202,203].
Commensal bacteria colonization results in Paneth cell expression of an antimicrobial peptide, regenerating islet-derived 3 gamma (Reg III-γ) [204, 205], which is involved in innate immune protection against enteric pathogens [206]. Moreover, the gut microbiota helps with maintaining the balance between Teff and Treg cell function. Expansion and differentiation of T-cells into TREG cells occur in the colon in the presence of microbiota. TREG cells suppress inflammatory response via the production of anti-inflammatory cytokines IL-10 and transforming growth factor (TGF)-β. A mixture of Clostridia strains induces the accumulation of TREG cells in the colon and expression of IL-10 and CTLA-4 by Treg cells. Lactobacillus reuteri, L. murinus, and Helicobacter hepaticus have also been implicated in TREG function [207,208,209,210].
Cancer Prevention and Treatment, Immunity, and Probiotics
Epidemiological Studies
The preventive effect of probiotics or fermented products containing probiotics on animal and human cancers has been frequently investigated. However, epidemiological evidence is scarce. Studies on humans showed a reverse association between yogurt intake and the risk of breast cancer [211]. In another case-control study in the United States, yogurt consumption was reported to be protective against colon cancer [212]. Similar results were found by Dutch researchers for breast cancer [213]. There are clinical trials investigating the possible role of probiotics in cancer prevention. In one trial, recurrence rate of superficial bladder cancer was lower in subjects who received L. casei Shirota (LcS) in comparison with subjects receiving placebo [214]. However, it must be clarified if long-term supplementation of probiotics can significantly reduce the risk of CRC in humans. A cohort study with 12 years of follow-up on 45,241 volunteers determined that high yogurt consumption was significantly related to lower risk of CRC [215]. However, these studies have limitations concerning selection and standardization of microorganisms, control of food intake, time, and dosing of microorganism administration.
Clinical studies have also investigated the beneficial effect of probiotics in preventing GI disorders, including viral diarrhea and chemotherapy, radiotherapy, or antibiotic-associated diarrhea. In addition, chronic treatment with probiotics effectively reduced the urinary excretion of aflatoxin B(1)-N(7)-guanine (AFB-N(7)-guanine), a marker for hepatocyte carcinogenesis, and the risk of CRC [216]. It is commonly believed that probiotic supplementation can decrease the risk of breast cancer in perimenopausal women. However, clinical studies report inconsistent results. It seems that long-term use of probiotics is needed to achieve chemopreventive effect on the development of malignant tumors. For instance, L. casei supplementation for 4 years could prevent atypical CRC [217]. Usual consumption of L. casei Shirota (LcS) and soy isoflavone in adolescents was inversely related to the incidence of breast cancer in Japanese women [218]. In contrast, the 3-month yogurt consumption could not improve cell-mediated immune function in women [219]. Altogether, evidence for the efficacy of probiotics in human tumorigenesis is ambiguous. However, there is mounting evidence from experimental models indicating antineoplastic effects of probiotics. In addition, as shown through a meta-analysis study, data from epidemiological studies reveal a decreased risk of CRC and precursor lesions in association with consumption of probiotics. However, interventional studies are necessary to confirm the efficacy of probiotics [220]. Coupled to the above is the need for long-term high-quality studies that assess the efficacy of probiotics in subjects with different types and stages of cancer.
Cancer Prevention
Study of proto-oncogene human epidermal growth factor receptor-2 (HER2)/neu -driven transgenic mice showed that extended contact to metronidazole in combination with ciprofloxacin increases the risk of breast cancer [221]. In fact, altered composition of the gut microbiota may influence the development and progression of cancer through inflammatory and metabolic pathways [222, 223]. However, not all probiotics have the ability to modulate the immune system and thereby play a role in cancer prevention. Previously, it has been reported that a dose of 108–109 colony-forming unit (CFU)/day of a strain with immunomodulatory effect and a duration of 48–72 h is required to influence the host immune homeostasis [224, 225].
Maintenance and Enhancement of Intestinal Barrier Function
Mucin 2 (MUC2) is the main mucin secreted by intestinal goblet cells. MUC2-deficient mice have increased risk for CRC [226]. Treatment with probiotics was reported to be effective to promote the restoration of colonic tissue through an increased MUC2 expression, extracellular mucin secretion, and inhibition of enteropathogenic adherence. Increased epithelial permeability has been implicated in early stages of CRC. L. plantarum MB452 was shown to enhance Caco-2 tight junction (TJ) integrity, possibly through encoding TJ-related genes including occludin and scaffold protein zonula occludens [226,227,228]. Probiotics are also capable of preventing epithelial barrier damage by stimulating the production of cytoprotective heat shock proteins in stressed epithelial cells to maintain hemostasis [229] and promote cell survival [230]. Components of E. coli strain Nissle 1917 can decrease intestinal permeability by restoring a disrupted epithelial barrier [231]. Combination of L. rhamnosus GG (LGG) and B. lactis Bb12 could also improve epithelial integrity in patients with CRC [232].
Recognition of Probiotics by the Immune System: Toll-Like Receptors
TLR2 plays a protective role in colitis-associated CRC. TLR2-deficient mice demonstrated increased inflammation and elevated serum levels of inflammatory markers such as IL-6 and IL-17A. Probiotics can modify the risk of CRC through a TLR2-dependent pathway. TLR2 recognizes gram-positive bacteria, such as lactobacilli and bifidobacteria [233, 234]. Peptidoglycan from lactobacilli blocks the production of pro-inflammatory cytokine IL-12 by macrophages via TLR2 [235]. In addition, mixture of L. plantarum and L. casei synergistically stimulate IL-10 production in macrophages through a TLR2-dependent pathway [233].
Modulation of DCs
IL-10 suppresses the production of pro-inflammatory cytokines while promoting the development of TREG cells. Studies showed a strong association between probiotics and induction of IL-10 by DCs [236]. Administration of probiotics also induced regulatory DCs, which, in turn, could promote the induction of CD4+Foxp3+ TREG cells in vivo [237]. Thereby, mice showed a reduction in the production of pro-inflammatory cytokines IL-17, IFN-γ, and TNF-α and an amelioration of disease progression. In the study [238], the authors investigated the ability of three Lactobacillus species to influence DC to drive TREG cell development. Human monocyte-derived DC matured in the presence of L. rhamnosus showed decreased capacity to support T-cell proliferation and attenuate CD3/CD28-induced cytokine production.
L. rhamnosus GG, B. lactis Bb12, and/or inulin enriched with oligofructose demonstrated immune stimulatory effects by inducing the maturation of DC [239], supporting the immune response against tumor cells [240]. Activation of IL-10-secreting cells was accompanied by the induction of apoptosis in colon cancer cells and suppression of pro-carcinogenic factors [241]. Bifidobacterium in a mice model has been shown to alter DC activity, leading to improved tumor-specific CD8+ T-cell function.
NK Cell Proliferation and Activity
Probiotics are also able to increase NK cell numbers and their cytotoxic activity [242]. Oral administration of L. casei Shirota (LcS) to tumor-bearing mice stimulated splenic NK cell activity, thus leading to postponed tumor formation [243,244,245]. Probiotics exert desmutagenic effects on myeloid DC maturation through IL-12 production and shifting T-cell activity toward TH1, TH2, or even TREG type of responses [244, 246, 247]. Later, this molecule, IL-12, activates NK cells to produce IFN-γ [248]. In this manner, LcS is able to suppress murine tumorigenesis via increased IL-12 production by bone marrow-derived cells in vitro [249] and inhibition of IL-6 production in the colonic mucosa [250, 251]. Previous studies demonstrated that Lactobacillus strains with a firm cell wall resistant to intracellular digestion can stimulate high levels of IL-12 [252].
Lactobacillus and Bifidobacterium strains and their mixture differentially initiated NK/DC interactions via induction of DC maturation and cytolytic potential of NK cells [253]. NK cells play a critical role in tumor surveillance and production of IFN-γ and TNF-α, which induce cell-mediated immunity and lead to further activation of APCs (DCs and macrophages) [248]. NK cells also are indirectly activated by DCs which secrete soluble factors, such as IL-12, IL-18, and type I interferons. Probiotic Lactobacillus strains can induce secretion of pro-inflammatory cytokines, IL-12 and TNFα [254], which are positively correlated with NK cell activity.
IL-12 produced by DC and APC primes NK cell activation and subsequent secretion of TNF-α. Therefore, LcS and Lactobacillus strains may indirectly activate NK effector cells through DCs and APCs, respectively. NK-derived IFN-γ secretion has been implicated not only in innate antitumor immune responses but also in cell-mediated antitumor immune responses [253, 255]. In one trial, intake of fermented milk containing LcS enhanced NF-κB activity in subjects. The effect was reduced in the presence of anti-IL-12 monoclonal antibody [256]. DCs, TREG cells, and NK cells are important immune cells in defense against cancer [251, 257]. However, supplementation with synbiotics containing LGG, B. lactis, and oligofructose for 12 weeks showed little effects on systemic immune responses in patients with CRC [239].
Inhibitory Effect of Probiotics on TLR4 and COX-2 Expression
COX-2 has been implicated in inflammatory diseases and CRC. TLR4 is mandatory for the induction of COX-2 and therefore CRC development [258]. Overexpression of TLR4 upregulates NF-κB activation and COX-2 expression [259]. The probiotic combination VSL#3 has been reported to downregulate COX-2 expression in Colo320 and SW480 intestinal epithelial cells (IECs). COX-2 has been associated with an increased risk of CRC because it stimulates cell proliferation and triggers inflammatory pathways [35]. Milks fermented with different strains of probiotics have been investigated in HT-29 colon cancer cells. Almost all of them induced a significant, although variable, reduction in the growth of HT-29 cells [260, 261].
Probiotics Enhance Innate Immune Functions
Defensins through membrane lysis and DNA damage exert cytotoxic activity on tumor cells. Murine b-defensin 2 has been shown to promote DC maturation, which initiates type I polarized immune responses through the production of pro-inflammatory cytokines such as IL-12, IL-1α, IL-1β, and IL-6 [262]. Treatment of Caco-2 colorectal adenocarcinoma cells with L. plantarum through the induction of TLR2 significantly upregulated the mRNA expression and secretion of human b-defensin 2 (HBD-2) in a dose-dependent manner [263]. A probiotic mixture, including several E. coli strains, VSL#3, and lactobacilli, increased HBD-2 synthesis in human and Caco-2 cells [264]. In addition, probiotic products enhanced host immune function by increasing phagocytic activity of macrophages [265].
Immunoglobulins
IgA exerts anti-inflammatory and also cytotoxic effects on tumor cells [266]. It is resistant to proteolysis and can limit contact between potentially carcinogenic compounds and colon cells [225]. A study of mice treated with carcinogen showed that consumption of yogurt containing probiotics was efficient to downregulate cancer progression in the large intestine through upregulation of IgA, T-cell function, and colonic macrophage activities [234]. However, the effect of probiotic supplementation on the production of IgA remains controversial [265, 267]. LcS has been shown to inhibit tumor development and IgE production in mice [268].
Administration of L. acidophilus SNUL, L. casei YIT9029, and B. longum HY8001 improved the survival of tumor-bearing mice. The effect was associated with enhanced cellular immune responses as reflected in increased numbers of total T-cells, NK cells and MHC class II+ cells, and CD4−CD8+ T-cells [269]. Lactobacillus rhamnosus strain GG (LGG) was reported to delay the onset of cancer through mitigating CD3 T-cell depletion in tumor-bearing mice while enhancing activation of CD8 and CD4− T-cells without significant effect on NK cell function [270]. Furthermore, L. acidophilus suppressed MHC class I expression and also induced a decrease in mRNA expression of stromal-derived factor-1 receptor, CXCR4, suggesting a role in cancer metastasis prevention [271]. In DSS-induced CRC mice, Lactobacillus and the VSL#3 mixture increased levels of angiostatin, an endogenous inhibitor of angiogenesis and regulatory T-cells [272]. In contrast, there was an increase in the number of memory CD4+ T-cells and pro-inflammatory cytokines IL-17 and TNF-α [272].
Pre-inoculation with L. plantarum significantly reduced tumor growth and activated innate immunity while increasing the intratumoral levels of CD8+ T-cells and NK cells in the tumor microenvironment [273]. Probiotic administration significantly increased the CD8+/CD4+ T-lymphocyte ratio. CD4 cells induce production of cytokines such as IL-6 and IL-10. Thus, increasing the CD8+/CD4+ T-lymphocyte ratio might explain lowering of IL-6 and delayed tumor growth by probiotics [274]. Indeed, L. reuteri was shown to delay the onset of neoplastic features through the induction of anti-inflammatory CD4+CD25+ TREG cells. Stimulated TREG cells would direct immune networks in a manner to resist against inflammatory diseases, including early stage of malignant transformation [275]. L. rhamnosus GG has been demonstrated to be effective in reducing the recurrence of bladder cancer [276]. The effect may be mediated by increased levels of chemokine (C motif) ligand (XCL1); this chemokine produced by activated CD8+ cells and γδ-T-cells, NK cells, and master cells, which helps in chemotaxis by T-cells and NK cells and thus assists in tumor regression [276]. Activation of phagocytes by probiotics can inhibit cancer cells in early stage. Kefir consumption caused stimulation of phagocytes present in Peyer’s patches and in the peritoneum [277].
Researchers have argued that stimulation rather than suppression of the innate immune system can contribute to cancer development. Yogurt feeding was correlated with altered levels of cytokines, such as TNF-α, IFN-γ, and interleukins [278, 279]. Intrapleural injection of LcS in mice could improve immunity against tumor development through release of TNF-α, an antitumor agent. In line with these observations, other studies also noted that intrapleural administration of LcS in tumor-bearing mice induced the production of IFN-γ, IL-1β, and TNF-α, leading to the inhibition of tumor growth and therefore an increased survival [280, 281]. Similar results have been reported for L. acidophilus SNUL, L. casei YIT9029, and B. longum HY8001 strains [269]. Urbanska and colleagues [279] investigated the effect of microencapsulated probiotic Lactobacillus acidophilus in a model of CRC. Daily oral administration of the microorganism significantly induced suppression in tumor growth, tumor multiplicity, and tumor size. In a study by de Leblanc et al. [282], LcS induced the secretion of inflammatory cytokines such as TNF-α, IL-1β, and IFN-γ, resulting in reduced tumor development and improved survival of mice treated with a carcinogen [281]. IFN-γ is involved in activation of NK cells and macrophages. Consequently, it plays a significant role in cancer prevention. Humans and animals continuously produce IFN-γ in the defense against cancer [283]. Excessive inflammatory response is not desirable, and probiotics are able to induce and control TREG cell function [284]. Direct immune modulatory effects of B. lactis and L. rhamnosus have been reported to be mediated through reduction of IL-2 and inducible NO synthase [285, 286]. Antitumoral and immunoregulatory effects of LcS have been investigated in various models. Of note, oral administration of LcS has demonstrated antitumoral activity against bladder cancer cells in clinical trials [287].
Modulation of Inflammatory Response
Chronic inflammation has been recognized as a risk factor for cancer. Inflammation plays a causative role in colitis-associated colon cancer, sporadic colon cancer, and hepatocellular carcinoma (HCC) [288,289,290]. Previous studies have reported antitumoral and anti-inflammatory effects of probiotics [291, 292]. LGG was reported to prevent colon cancer, accompanied by suppression of NF-κB pathway [293]. Li et al. showed a reduction in the level of IL-17 by probiotics in an HCC model. It suggests an association between immunomodulatory and antitumoral effects of probiotics [290]. Mounting evidence suggests the IL-6-lowering effect of L. casei CRL431. The proangiogenic role of IL-6 is consistent with impaired tumor growth by probiotic supplementation [274].
The Lactobacillus casei BL23, recognized for its anti-inflammatory characteristics, was tested for its protective effects on CRC in mice [294]. Mice in probiotic group substantially showed reduced levels of the monocyte chemoattractant protein-1 (MCP-1) and TNF-α with high levels of anti-inflammatory ones, such as IL-10 [294].
IL-17A produced by TH17 cells would assist angiogenesis. Although the role of TH17 cells and IL-17 in cancer is still inconsistent, but it has been suggested that reduction of TH17 cell population and IL-17 level may inhibit progression of cancer [295, 296]. Noteworthy, ex vivo studies on splenic cells incubated with L. casei BL23 showed reduced numbers of TREG cells and increased percentage of TH17 cells and higher production of IL-17, IL-6, and TGF-β, together providing a microenvironment favorable to TH17 differentiation [294]. As mentioned before, a probiotic mixture led to reduction in the proportion of TH17 cells and in the production of IL-17 in an HCC model. In contrast, L. casei BL23 caused an increase in the proportion of TH17 cells and in the production of IL-17 in a model of CRC [290]. However, both studies revealed an increase in the levels of anti-inflammatory cytokine IL-10 and anti-angiogenic cytokine IL-22. This would reflect a TH17-mediated response.
IFN-γ plays a role in cancer immunity by increasing MHC I expression, T-cell infiltration, differentiation to cytotoxic T-lymphocytes, and TH1 polarization, orchestrating different antitumoral immune responses [297, 298]. IFN-γ also has been used clinically for its antitumoral effect, leading to improved survival. Studies of mice reveal the role of IFN-γ in mediating the protective effect of probiotics against cancer [299, 300].
Production of Active Compounds Which May Be Involved in Immunity
Short-chain fatty acids (SCFAs) are the products of bacterial fermentation of nondigestible carbohydrates. Butyrate is a SCFA that can contribute to cancer prevention in different ways. It has the ability to increase mucus production and improve intestinal barrier function. It is also able to stimulate the production of anti-inflammatory cytokines, such as IL-10, while decreasing the production of pro-inflammatory cytokines by inhibiting the activation of NF-κB. More interestingly, butyrate can increase the immunogenicity of tumor cells by monitoring neutrophils and antigen-presenting cells and through regulation of chemotaxis by neutrophils, DCs, and macrophages [301] and suppressing COX-2 activity [302, 303]. Other SCFAs like acetic and propionic acids also exhibit the same anti-inflammatory activity through suppression of NF-κB signaling pathway [304, 305].
Some species of probiotic bacteria, such as Lactobacillus acidophilus, are able to produce conjugated linoleic acid (CLA) from linoleic acid. CLA can suppress the production of eicosanoids in colon cells through replacement of arachidonic acid by CLA in the cell membrane and through interference with cyclooxygenase and lipoxygenase (LOX) enzymes. Probiotic supplementation can increase the production of CLA to promote antitumor immunity in a dose-dependent manner [241, 306].
Immunological Effects of Probiotics Combined with Chemotherapy
Probiotics also can be used in combination with conventional cancer therapies. In particular, disruption of the gut microbiota can impair the cancer cell response to platinum salts as chemotherapy. Supporting this, mice treated with an antibiotic mixture (including vancomycin, imipenem, and neomycin) displayed reduced therapeutic response to oxaliplatin and cisplatin in a colon carcinoma (MC38) and lymphoma (EL4) model, respectively. Interestingly, it has been reported that combination antibiotic therapy reduces oxaliplatin-induced DNA damage and apoptosis in tumor-bearing mice. In addition, Ruminococcus, Alistipes, and Lactobacillus fermentum are capable of affecting tumor response to CpG oligodeoxynucleotide (ODN), probably through regulation of TNF production [307, 308].
The study [309] proved that the efficacy of cyclophosphamide as an anticancer immunomodulatory agent, at least in part, relies on the gut microbiota. Tumor-bearing mice that were either germ-free or antibiotics-treated showed a reduction in “pathogenic” T-helper (pTH17) responses, and their tumors were more resistant to cyclophosphamide-based therapy. It seems that this cyclophosphamide would stimulate pTH17 cells through a complex circuitry that involves the gut microbiota [309]. More precisely, treatment with cyclophosphamide causes a reduction in the abundance of lactobacilli and enterococci in the gut [309]. Gram-positive bacteria, such as L. johnsonii and E. hirae, promote differentiation of CD4+ T-cells into TH1 and TH17 cells. Broad-spectrum antibiotics suppressed cyclophosphamide-induced production of IL-17 and IFN-γ [309]. Consistently, another study [310] showed that two bacterial species, Enterococcus hirae and Barnesiella intestinihominis, are involved in response to cyclophosphamide therapy. After cyclophosphamide treatment, E. hirae migrates to secondary lymphoid organs, followed by mounting pTH17 immune responses and accumulation of IFN-γ+ IL-17+ cells and CCR6+ CXCR3+ CD4+ T-cells and TREG cells in the spleen [309].
Studies have demonstrated the significance of Bifidobacterium to natural antitumor immunity and also in response to anti-PD-L1 antibody therapy and CTLA-4 therapy in tumor settings [311, 312]. Furthermore, Bacteroides fragilis improved response to CTLA-4 blockade, by affecting IL-12-dependent TH1 immune response. Bifidobacterium in combination with anti-PD-L1 antibody enhanced antitumor immunity through activation of DCs [312].
Altogether, finding bacterial genera linking intestinal immune homeostasis and anticancer immune responses is essential to shed light on the possibility of using selected bacteria to improve cancer therapy by enriching the gut microbiota. In patients with metastatic melanoma, an increased delivery of bacteria belonging to the Bacteroidetes phylum is associated with an increased resistance to the development of checkpoint blockade-induced colitis [313]. Recent advances in this field such as fecal transplant open up new avenues in cancer therapy [314, 315].
Role of Microorganisms in the Development of Cancer
Tumorigenesis is a complex process. As a result, it is difficult to draw a direct association between dysbiosis, inflammation, and tumorigenesis. Adherent/invasive E. coli strains are present in great quantity on the colonic mucosa of patients with CRC but not normal colonic mucosa. This indicates involvement of E. coli colonization in cancer pathophysiology [316]. Long-term colonization of enterotoxigenic Bacteroides fragilis (ETBF) led to colitis and multiple intestinal neoplasia (MIN) in mice [317]. On the other side, IL-10-deficient mice colonized with Bacteroides vulgates displayed low-grade inflammation and more interestingly were less likely to develop colorectal tumors as compared with conventionalized IL-10-deficient mice [318]. The results support the differential role of gut microorganisms in intestinal immune homeostasis and CRC. There is a complex interaction between the gut microbiota and IECs, where innate immune receptors including Nod-like receptors (NLRs) and TLRs play a role. It has been reported that Nod1 pathway could increase tumor-promoting effect of attenuated Wnt signaling. Furthermore, gut microbiota depletion by antibiotics decreases tumor development in Nod1-deficient mice [319]. These data highlight the complicated interaction between the microbiota, inflammation, and cancer and support the hypothesis that susceptibility to cancer would be influenced by the composition of the gut microbiota and by the repertoire of host innate sensors as well. As a result, modification of the intestinal microbiota using probiotics or prebiotics may affect the development of cancer.
Gut Microbiota Induces Potent TREG Cells with Systemic Antineoplastic Properties
The association of tumor-associated cells expressing TREG cell markers including FOXP3 with poor prognosis of human cancers remains inconsistent. Under certain conditions, microbial priming of TREG cells not only protects against cancer development but also helps remission of already established intestinal, mammary, and prostate cancers [320]. However, TREG cells play paradoxical roles in cancer [320, 321]. Actually, Treg-mediated decreased risk of cancer is dependent on microbiota-induced IL-10, which acts to maintain immune system homeostasis and support a protective anti-inflammatory and antineoplastic TREG phenotype. Probiotic consumption in mice shifts immunity toward IFN-γ and CD25 to improve wound healing and promote systemic health [322]. IFN-γ levels increase during TREG-mediated tumor regression in mice. Recent findings show that an unbalanced gut flora would weaken response to immune [307, 309] and nonimmune chemotherapeutic regimens such as cisplatin and oxaliplatin [307].
Based on the “hygiene hypothesis,” hygienic subjects are vulnerable to a redirection of unbalanced resting peripheral TREG to TH17 immune responses, putting them at higher risk of autoimmune diseases and cancer [182]. Furthermore, consumption of beneficial probiotic bacteria led to the expansion of Foxp3+ cells in the periphery [275, 322], improving defense against mammary cancer [275]. Probiotics-induced enhancement of the TREG-dominated arm of the immune system did not interfere with the capability to respond against invading pathogens [322]. Altogether, the gut and its cross talk with the host determine the fate of preneoplastic and neoplastic lesions arising in epithelia throughout the body. It would open up a new avenue in cancer immunotherapy through modulation of beneficial TREG via diet. This concept not only could be considered for fighting cancer, but also arousing these dormant TREG-mediated capabilities may give an alternative approach to reduce cancer risk and promote overall good health and longevity [320].
Lactoferrin, Immunity, and Cancer
Lactoferrin (Lf) is an iron-binding glycoprotein belonging to the transferring family. It contributes to the regulation of iron absorption in the bowel and immune responses, as well as is able to exert antimicrobial, antioxidant, antitumoral, and anti-inflammatory effects [323, 324]. Lf is produced by mucosal epithelial cells and is present in most biological fluids, including tears, saliva, vaginal fluids, semen, and most abundantly milk and colostrum [324]. Moreover, it is present in considerable amounts in polymorphonuclear granules [323]. Recent reports have shown that this multifunctional agent essentially exerts antimicrobial effect, which can be directed against bacteria, fungi, and viruses [325]. Other Lf-mediated activities include immune modulatory functions and tumor growth inhibition [325]. Its bacteriostatic effect is mediated through iron-binding ability, which consequently restricts the use of iron by bacteria and inhibits their growth systemically. Additionally, Lf damages the external membrane of the gram-negative bacteria by interacting with the lipopolysaccharide (LPS) [323]. Therefore, knowledge of the physiological role and possible therapeutic implications of LF is hastily growing. Here, we present possible antitumoral effects of LF through immune modulatory activity.
Antitumor Activity
The first reports suggesting that Lf may possess antitumor effects through depleting tumor cells of glutathione, making them more susceptible to chemotherapy, appeared in 1995 [326]. Since then, in vitro studies have demonstrated antitumor effects of Lf in different cancer cell lines such as breast cancer [327, 328], pancreatic cancer, colon cancer, and oral squamous cell carcinoma [329,330,331]. Suggested mechanisms include increased NK cell cytotoxicity and inhibition of cell growth and metastatic colony formation. Chemopreventive effects of bovine Lf (bLf) also have been implicated in treatment of tumors of the colon, peritoneum, lung, esophagus, mouth, and neck. Moreover, the immune modulatory effect of Lf has been shown in mice [332,333,334]. Oral administration of recombinant human Lf has been investigated in head and neck squamous cell carcinoma in mice. Animals treated with Lf exhibited tumor growth inhibition of 75% concurrent with a 20-fold increase in lymphocyte ratio compared with controls. Of note, when mice were depleted of CD3+ cells, Lf-induced tumor inhibition was abrogated [335].
Other studies investigated the effects of iron-saturated (i-s) bLf on the augmentation of chemotherapy. Results showed that chemotherapy eradicated large lymphomas only in mice fed 100% i-s bLf for at least 2 weeks prior to chemotherapy, but not in mice fed lower saturated forms of bovine Lf or control mice fed no bLf. Lf was nevertheless effective in augmenting chemotherapy at the lowest dose tested, equated to a 70 kg person ingesting 3 grams of Lf per day. In addition, 100% i-s bLf decreased angiogenesis, increased apoptosis, and supported immunomodulation, as reflected in increased production of TH1 (TNF-α, IFN-γ, and IL-18) and TH2 (IL-4, IL-5, IL-6, and IL-10) cytokines, which are necessary for optimal antitumor immune responses. Moreover, 100% i-s bLf also restored both RBC and WBC numbers depleted by chemotherapy [336]. However, the ability of Lf to exert a protective effect at sites far away from the GI tract is less understood [337].
Evidence for Chemopreventive Potential
Anti-inflammatory Activity
Lf possesses potent modulatory properties. It can decrease the production of pro-inflammatory cytokines (IFN-γ, TNF-α, IL-1β, IL-6, and granulocyte-macrophage colony-stimulating factor (GMCSF)) [335, 338,339,340,341] while upregulating the levels of anti-inflammatory cytokines (IL-10) [342, 343]. However, other studies reported inconsistent results: (1) ex vivo upregulation of TNF-α and IFN-γ concurrent with a reduction in IL-5 and IL-10 upon induction with the exotoxin toxic shock syndrome toxin-1 [344] and (2) enhanced IL-12 production and decreased IL-10 release in human immunodeficiency virus (HIV)-infected children [345]. Together, these results indicate that Lf affects the TH1/TH2 cytokine balance independent of the host immune setting. Thus, Lf can increase the production of TH1 cytokines in settings requiring an augmented ability to control infection on one hand and on the other hand may decrease the production of TH1 cytokines to restrict excessive inflammatory responses [346]. Moreover, intravenous administration of bLf 24 h presurgery eased thymectomy- and splenectomy-induced TNF-α and IL-6 generation, suggesting that Lf may have therapeutic application in cases of shock syndromes [347].
Immune Modulatory Activity
As already discussed, Lf also possesses immune-modulating properties. In vivo studies on the oral administration of bLf in mice revealed increased levels of NK cells, CD4+ and CD8+ cells, and IFN-γ+ cells, in both the mucosal layer of the small intestine and the peripheral cells [348,349,350]. In addition, NK cell cytotoxicity is increased both in vitro and in vivo [328, 351, 352]. In humans, CD3+, CD4+, and CD8+ T-cell activation has been observed as well [353].
Endogenous Lf belongs to the innate nonspecific immune system. However, mounting evidence shows that it may also be attributed to acquired immunity and protection against inflammation. As a powerful modulator of inflammatory and immune responses, Lf supports protection against both microbial infections such as septic shock and inflammatory diseases such as arthritis, chronic hepatitis, and cancer [354,355,356]. The modifying activity by Lf is connected to its capability to interfere with both specific cell receptors on a wide range of epithelial and immune cells [357] and pro-inflammatory bacterial components like LPS [358].
At the molecular level, the modulatory characteristics of Lf are mediated through iron binding and interactions with a multitude of compounds such as LPS. At the cellular level, Lf modifies the migration, maturation, differentiation, activation, proliferation, and function of immune cells. Some possible mechanisms include modulation of NF-κB and MAP kinase signaling [354]. Lf has been shown to increase the accumulation of neutrophils to sites of damage, support cell-to-cell interaction by promoting “stickiness,” promote phagocytosis by polymorphonuclear leukocytes (PMNs) and monocyte/macrophages, support motility and superoxide production, reduce the release of pro-inflammatory cytokines, increase the number and activity of NK cells, and promote the maturation of lymphocytes [359,360,361,362,363].
In addition, a mechanism underlying antitumor effect of Lf is regulation of NK cell activity [328, 364] and inhibition of vascular endothelial growth factor (VEGF)-mediated angiogenesis [365]. It was reported that Lf has a significant effect on NK cell cytotoxicity and target cell sensitivity to lysis in hematopoietic and breast epithelial cell [328]. Other studies reported inhibition of tumor growth and lung colonization by B16-F10 melanoma experimental metastasis in mice treated with human Lf through increased NK cell activity [351].
Rodent cancer models have shown enhancement of intestinal immune homeostasis following oral administration of Lf. In particular, increased activation of NK cells, CD4+ T-cells, and CD8+ T-cells was demonstrated after Lf administration [348, 349].
In vivo oral administration of bLf enhanced NK cell activity and CD4+ and CD8+ T-cells in tumor-bearing mice [349, 350, 362] and also increased CD3+ and CD4+ T-cells in immunocompromised mice [366]. Activation of CD4+ T-cells induces the generation of plasma B-cells, memory B-cells, and antibodies [367, 368]. Moreover, CD4+ activation improves macrophage function, by inducing the release of cytokines [346]. Further activation of CD4+ T-cells induces the generation of cytotoxic CD8+ T-cells, which would destroy virus-invaded cells, cancer cells, and intracellular bacteria, as indicated in experimentally induced cancers [369].
Inhibition of Angiogenesis
Administration of bLf was reported to inhibit angiogenesis in rats [365] and mice [370]. In contrast, human Lf promotes angiogenesis [371]. BLf may inhibit angiogenesis through inhibition of IL-18 production [372]. Moreover, increased levels of IL-18 raise mucosal and systemic immune responses via cytokine secretion and NK cell activation [373]. In addition, Lf can reduce the levels of pro-inflammatory cytokines such as IL-6 and IL-1β as potent angiogenic inducers [374].
Clinical Trials
Few studies investigated the effect of lactoferrin on the immune system. In one study, 2 g bLf/day for 4 weeks increased phagocytic activity of PMNs in three participants and increased CD16+ T-cell counts in two of them. There was an augmentation in the percentage of NK cells, the percentage of CD11b+ and CD56+ T-cells, and the CD16+ cell counts [375]. The oral administration of 40 mg bLf equivalent/day for 10 days in healthy participants resulted in an increased percentage of lymphocytes and immature cell forms, concurrent with a reduced percentage of neutrophils, eosinophils, and monocytes. Additionally, TNF-α levels were reduced, while changes in IL-6 were not significant [376]. The oral administration of placebo, 2, 10, or 50 mg of Lf daily, for 7 days in healthy subjects exhibited a significant, though transient, increase in the number of immature neutrophils and a significant reduction in the release of IL-6 and TNF-α by peripheral blood cells [377]. It has been suggested that a function of Lf could be to modify inflammatory reactions through the regulation of cytokine generation [378, 379].
Antitumor Immunity and Dietary Components
About ten plant-derived anticancer drugs are currently approved. They can be classified into four main classes of compounds: Vinca (or Catharanthus) alkaloids, epipodophyllotoxins, taxanes, and camptothecins. There are also a large number of phytochemicals subject to various phases of clinical trials, such as curcumin, epigallocatechin gallate (EGCG), soy isoflavones, etc. These compounds have shown anticancer effects both in vitro and in vivo. Some of them are discussed in the following section.
Resveratrol
Resveratrol is a polyphenol belonging to the stilbene class of phytochemicals. It is found in several plant species including grapes, peanuts, mulberries, cranberries, and other fruits [380, 381]. Resveratrol was found to be most abundant in the skin of grapes. It has been reported to block various cancer-related proliferative pathways making it a hopeful anticancer therapeutic candidate [382, 383]. A plant with considerably high content of resveratrol, Polygonum cuspidatum , is highly used in traditional Chinese medicine (TCM) to treat inflammation and cancer [384]. In 1997, resveratrol was first demonstrated to delay cancer initiation, promotion, and progression [385]. It is already used in clinical settings because of its antitumor cancer and chemopreventive activities [386]. Ongoing trials are investigating the possible effect of resveratrol on human cancers. Most clinical trials are testing the anticancer effects of resveratrol in CRC including NCT00256334, NCT00578396, NCT00920803, and NCT00433576. Two trials in GI cancers (NCT01476592) and thyroid cancers are assessing the effect of resveratrol on notch-1 signaling. The anticancer effect of resveratrol has also been investigated in leukemia, lymphoma, multiple myeloma, and prostate, breast, brain, and other nervous system cancers. In a bone cancer pain model, resveratrol was recently proposed to have palliative effects by blocking spinal glial activation and downregulating CX3CR1 [387].
Nuclear Factor-κB Pathway
Resveratrol has been shown to have anti-inflammatory and antitumor effects [388]. Resveratrol blocks cell proliferation and induces apoptosis in various cancer cell lines, such as breast, prostate, colon, and ovarian cancer cells [389]. The inhibitory effects of resveratrol on tumor growth have been attributed to its anti-inflammatory activity [389]. Aberrant regulation of NF-κB has been associated with cancer and autoimmune diseases. NF-κB is used by cells as a regulator of genes that control cell proliferation and cell survival. Many different types of human malignancies showed dysregulation of NF-κB. Resveratrol suppresses NF-κB activity mainly through blocking NF-κB inhibitor kinase (IKK) in murine and human macrophage cells along with downregulation of AP-1 [390, 391]. Resveratrol can downregulate NF-κB-induced gene products involved in inflammation, such as iNOS and COX-2, matrix metalloproteinase (MMP)-3, MMP-9, and vascular endothelial growth factor (VEGF) in macrophages and various cancer cells [392, 393]. NF-κB-mediated transcriptional activity stimulated by EGF and TNF-α was effectively blocked by resveratrol in prostate cancer cell lines [394]. Resveratrol treatment in human multiple myeloma cell line inhibited proliferation by decreasing proliferative and antiapoptotic factors. The effect, which was mediated through suppression of NF-κB, potentiated the effects of bortezomib and thalidomide [395].
MAPK phosphatase 5 (MAPK5) is a potent inhibitor of cellular inflammatory responses because it can inhibit the enzymatic activation of MAPK, one of the upstream kinases that control the activation of NF-κB [396]. It has been reported that resveratrol could upregulate MAPK5 and block p38 pathway in prostate cancer cell lines [397]. Furthermore, resveratrol can inhibit NF-κB by blocking the upstream activator PKCδ and by activating the inhibitor SIRT1 [398].
Anti-inflammatory Implications: Focus on COX-2
Resveratrol is a potent COX suppressor, which has been confirmed in different in vivo and in vitro studies. Resveratrol can inhibit COX-2 activity through direct binding or suppression of transcription factors [399]. Resveratrol counteracts the proliferation of CRC and MCF-7 breast cancer cell line through affecting p53-COX-2 pathway. In vivo studies confirmed that resveratrol in dietary levels leads to a reduction in the formation of DMBA-induced mammary tumors through inhibition of COX-2-, MMP-9-, and NF-κB-mediated tumor cell proliferation [400].
In an interesting study, resveratrol was shown to prevent apoptosis induced in human leukemia K562 cells by H202. In fact, resveratrol reversed the elevation of leukotriene B4 and prostaglandin E2 induced by H202 challenge through inhibition of 5-lipoxygenase, COX, and peroxidase activity of prostaglandin H synthase [401].
Other Inflammatory Pathways
Resveratrol is also able to suppress the expression of hypoxia-inducible factor-1α (HIF-1α) through inhibition of MAPK and increased degradation of HIF-1α protein via the proteasome pathway. Resveratrol also suppressed VEGF through inhibition of HIF-1α [402, 403].
Recent studies have discussed the role of microRNAs (miRNAs) in mediating the anti-inflammatory effects of resveratrol. Resveratrol can decrease the secretion of pro-inflammatory cytokines (e.g., IL-1, IL-6, IL-8, and TNF-α), the expression of adhesion proteins including intercellular adhesion molecule (ICAM)-1, and the expression of leukocyte chemoattractants, such as MCP-1 [404]. Resveratrol suppressed TNF-α-induced signaling pathways both via NF-κB activation and by increasing transcriptional activity of p65 [405]. In addition, resveratrol induced the expression of Egr-1 from its chromosomal locus. Egr-1 has demonstrated antitumor effects upon experimental increase in TNF-α [406]. The control of transgenic expression via activation of Egr-1 promoter by resveratrol may sensitize cancer cells, expanding the use of adenovector Ad.Egr-TNF in patients resistant to radiation or chemotherapy, suggesting a new means for development of inducible gene treatments [406]. In prostate cancer cell line, resveratrol increased the production of ROS and expression of pro-apoptotic factors including TRAIL [383]. In a mouse model with prostate cancer, resveratrol significantly reduced cell proliferation and the expression of growth factors and their receptors [383].
In human colon cancer cells resistant to the cytotoxic effect of resveratrol, resveratrol was able to sensitize tumor cells to TNF, anti-CD95 antibody, and TRAIL-mediated apoptosis and led to activation of a caspase-dependent death pathway [407]. Indeed, resveratrol sensitized lung cell lines to TNF-induced apoptosis by modifying sirtuin effect, and this activity is consistent with its ability to induce activity of Sirt1, a known NF-κB transcription repressor. Polyphenols can augment TRAIL expression in gastric cancer cell lines and are able to increase TRAIL-mediated apoptosis in various cancer types such as human melanoma, prostate carcinoma, pancreatic cancer, malignant glioma, prostate carcinoma, hepatocellular carcinoma, gastric carcinoma, neuroblastoma cells, Burkitt’s lymphoma, ovarian cancer cells, renal cancer cells, and colon cancer cells [408].
Resveratrol inhibited epithelial-mesenchymal transition (EMT) of pancreatic cancer cells by downregulating both the PI3K/AKT/NF-κB pathway and the EMT-related gene expression (E-cadherin, N-cadherin, vimentin, MMP-2, and MMP-9), which are essential for cancer cell motility and metastasis [409, 410]. In human pancreatic cancer cell, resveratrol treatment induced transcriptional upregulation of macrophage inhibitory cytokine-1 (MIC-1), which has antitumor activity [411]. Resveratrol is capable of blocking mediators of metastasis including lysophosphatidic acid (LPA), transforming growth factor (TGF), and focal adhesion kinase (FAK) in cancer cells like ovarian carcinoma cell. LPA induces the expression of HIF-1α and VEGF and thereby promotes cell migration [403]. Additionally, resveratrol can inhibit TGF-β1 and so cause inhibition of cell adhesion, migration, and invasion of lung cancer cells in A549 lung cancer cells [412, 413]. Resveratrol could diminish cell proliferation by influencing autocrine growth modulator pathways in breast cancer cells. For instance, it can increase the expression of the growth inhibitor TGF-ß2 without affecting the expression of TGF-ß1 and TGF-ß3 [414, 415]. Resveratrol may be used to modify the immunological reaction in tumor microenvironment, including inhibition of T-cell proliferation, reduction of IFN-γ and IL-4 secretion, downregulation of B-cell proliferation and therefore production of IgG1 and IgG2a isotypes, and suppression of CD28 expression on CD4+ T-cells and CD80 on macrophages [416].
Other possible antitumor effects from an immunological viewpoint include downregulation of MHC class I and II molecules; induction of tolerogenic DC phenotype; downregulation of the ability of bone marrow (BM)-derived DC to produce IL-12 p70 [417]; increasing the production of TNF-α, IL-12, and IL-1β in response to LPS stimulation; enhancing the secretion of IL-10; suppression of mucosal and systemic CXCR3−-expressing effector T-cells and inflammatory cytokines in the colon [418]; and inhibition of the suppressive activity of FoxP3-expressing TREG cells among CD4+CD25+ cells [416, 419,420,421,422,423].
Low-dose resveratrol was able to enhance cell-mediated immune responses by promoting TH1 cytokine production, macrophage function, and also APC-induced IL-12 and IFN-γ production [424]. Resveratrol treatment downregulated the frequency of TREG cells in EG7-bearing C57BL/6 mice. In addition, both CD4+CD25+FoxP3+ to CD4+CD25+ cell ratio and CD4+CD25+ to CD4+ cell ratio were reduced concurrently by resveratrol in a dose-dependent manner [425]. Resveratrol has been mostly investigated as an adjuvant agent combined with conventional chemotherapeutics to prevent or reduce the risk of multidrug resistance. Resveratrol strengthened the antitumor effect of 5-fluorouracil (5-FU) on CRC cells, thereby enhancing chemosensitization and reducing drug resistance [426]. For example, resveratrol sensitized various human cancer cell lines to chemotherapeutic agents such as doxorubicin, cytarabine, actinomycin D, Taxol, and methotrexate by suppressing the expression of survivin and enhancing apoptosis. The mechanism by which resveratrol chemosensitizes cancer cells includes inhibition of tumor cell proliferation, metastasis, and angiogenesis and induction of tumor cell apoptosis through inhibition of related signaling pathways, such as SIRT1, signal transducers and activators of transcription 3 (STAT3), Hh, AMPK/YAP, PTEN/PI3K/AKT, and NF-κB [427,428,429,430]. Moreover, NF-κB activation could upregulate the levels of some antiapoptotic genes, including TNF receptor-associated factor 1 (TRAF1) and TRAF2 [431]. Administration of resveratrol in IL-10−/− mice induced immunosuppressive CD11b+Gr−1+ MDSCs in the colon. The stimulation of immunosuppressive CD11b+Gr−1+ cells by resveratrol during colitis is distinctive and offers a novel mode of anti-inflammatory action of resveratrol [418].
AhR and Nrf2 as Inflammation-Environment-Diet Molecular Crossroads
AhR functions as a modulator of immunity (inflammation) and reaction to xenobiotics on one hand and acts as a mediator of effect of resveratrol on the other hand. Moreover, it is interesting to mention that the effect of resveratrol is frequently associated with upregulation or activation of Nrf2 [432, 433]. Resveratrol also augments the activation of nuclear factor E2-related factor-2 (Nrf2), which is followed by activation of antioxidant response element (ARE). Resveratrol has been reported to increase the expression of heme oxygenase-1 (HO-1) via Nrf2 activation in PC12 cells. In leukemia K562 cells, resveratrol increased NQO1 expression and stimulated Nrf2/Keap1/ARE binding to NQO1 promoter [434]. It also restored glutathione levels in human lung cancer A549 cells treated with cigarette smoke extracts by increasing the Nrf2-induced GCL expression [435]. There are some dietary AhR antagonists such as genistein, kaempferol, and EGCG. One recent agonist of AhR causes a number of anti-inflammatory responses in vitro and in vivo [436, 437]. Resveratrol assists Nrf2 and AhR in maintaining homeostasis against inflammatory insults, which may be involved in tumorigenesis. For instance, resveratrol caused inhibition of TCDD-induced recruitment of AhR and ARNT to the CYP1A1/CYP1A2 and CYP1A1/CYP1B1 promoter in hepatic cancer (HepG2) and breast cancer cell (MCF-7), respectively [438]. Therefore, resveratrol could modulate the activity of some cytochrome P450 enzymes and so act as chemopreventive compound by limiting activation of pro-carcinogens.
Immune Surveillance
Downregulation of tumor immunosurveillance involves resistance to apoptosis, production of immunosuppressive cytokines, and reduced expression of MHC class I antigens. Particularly, macrophages inhibit or increase the growth and spread of cancer based on their activation state. Synthetic resveratrol analog, HS-1793, significantly increased IFN-γ-secreting cells in splenocytes and also decreased CD206+ macrophage infiltration [439]. The local augmentation of IFN-γ modified the status of tumor-associated macrophages (TAMs) associated with the cancer microenvironment that occurred coincident with increased levels of pro-inflammatory and immunostimulatory cytokines (CD206, CD204, IL-10, TGF-β, EGF, and MMP-9) and decreased levels of IL-6 and immunosuppressive and tumor progressive mediators [439]. However, further studies are necessary to clarify the mechanism of action of resveratrol. Oral resveratrol significantly improved survival of lymphocytic leukemia L1210 cell-bearing mice through normalization of CD4/CD8 ratios and enhancement of NK cell activities and antisheep RBC titers. Furthermore, resveratrol suppressed cellular content, release, and mRNA expression of IL-6 [440].
CD95 Signaling Pathway
The Fas receptor (FasR), also known as CD95, Apo-1, and tumor necrosis factor receptor superfamily member 6 (TNFRSf6), leads to apoptosis. Resveratrol induces tumor cell death by modifying the levels of Fas and its ligand, FasL [441,442,443]. Earlier studies have reported this effect in leukemia cell lines [441] and colon [442] and breast carcinoma cells [443]. A study in multiple myeloma and T-cell leukemia cells emphasized the role of Fas/CD95 signaling in lipid rafts in anti-myeloma and anti-leukemia chemotherapy [444]. Using leukemia lines derived from patients with malignancies pro-B t(4;l1), pre-B, and T-cell ALL, it has been demonstrated that resveratrol could induce extensive apoptotic cell death not only in CD95-sensitive leukemia lines but also in B-lineage leukemic cells that are resistant to CD95 signaling [445]. Altogether, the CD95-CD95L system and its chemotherapeutic and chemopreventive potential are interesting enough to be considered in anticancer drugs [446].
Resveratrol and Its Interplay with NK Cells
Direct influence of resveratrol on NK cells and their killing ability on different levels has been reported in previous studies. Resveratrol exerts concurrent effects on NK cells and other immune cells like CD8+ and CD4+ T-cells [447]. The killing ability of NK cells against human immortalized myelogenous leukemia K562 cells was increased after resveratrol treatment. Furthermore, a dose-related inhibition of lytic activity was reported at high concentrations of resveratrol. Another study reported blocking of viability and enhanced apoptosis of NK cells upon incubation with high concentrations of resveratrol, whereas low concentrations of resveratrol resulted in upregulation of NKG2D and IFN-γ and increased killing of leukemia K562 target cells by NK cells [448]. Higher vulnerability of human lymphoblastoid T-cells (Jurkat cells) to cytotoxic effect of resveratrol also has been reported [449, 450]. Resveratrol in NK-92 cells increased the expression of perforin and phosphorylation of ERK-1/ ERK-2 and JNK, which are known to contribute NKG2D-mediated cytotoxicity [450]. Intragastric administration of resveratrol enhanced the killing ability of isolated spleen NK cells against mouse 51Cr-labeled lymphoma [451].
Furthermore, resveratrol increased the expression of NKG2D ligands on human promyeloblastic leukemia KG-1a cells, thus offering two mechanisms to potentiate cytokine-induced killer cells (CIK, a mixed phenotype between T-cells and NK cells) [452]. Stimulation of KG-1a cells susceptible to CIK-mediated cytolysis occurs via an increase in cell surface expression of NKG2D ligands and receptor DR4 and also via suppression of DcR1 along with activation of the TRAIL pathway [452]. Resveratrol may modify this axis, thereby promoting tumor surveillance by the innate immune system. Resveratrol is further capable of sensitizing cells of various cancer types, including neuroblastoma, medulloblastoma, glioblastoma, melanoma, T-cell leukemia, and pancreatic, breast, and colon cancer, to TRAIL-induced apoptotic cell death [453, 454]. In essence, resveratrol can upregulate the expression of receptors DR4 and DR5 in human prostate cells [455], thus enhancing TRAIL sensitivity and possibly facilitating NK cell-mediated killing activity. Resveratrol also considerably increased CD95L expression on HL-60 human leukemia cells and on T47D breast carcinoma cells [446], which would further help in NK cell-mediated apoptosis. Resveratrol has another therapeutic potential in defeating aggressive NK cell leukemias and lymphomas through inhibition of constitutively active signal transducers and activators of transcription 3 (STAT3) signaling [456].
Possible Interaction with TREG
Resveratrol is also able to decrease the cell number and function of immune TREG cells. High-dose IL-2 (HDIL-2) led to TREG expansion, but it was inhibited by resveratrol which could abrogate the toxic effects of HDIL-2 on endothelial cells [457]. Resveratrol was also involved in suppression of TGF-β secretion from the spleen of tumor-bearing mice and concurrent increase in IFN-γ expression in CD8+ T-cells, together resulting in immune stimulation [423]. Despite its immunostimulatory activity, IFN-γ is also reported to induce T-cell inhibitory molecule IDO in many cell types, including APCs [458]. Resveratrol can inhibit IFN-γ-induced IDO expression in bone marrow-derived dendritic cells (BMDCs) [459]. Resveratrol-mediated inhibition of EG7 thymoma tumor growth was dependent on IDO through inhibition of the Jak/Stat pathway and protein kinase C-δ (PKCδ), which both need IFN-γ-mediated IDO expression [460]. Resveratrol combined with thymoquinone was reported to decrease tumor size and increase serum levels of INF-γ in breast cancer tumor-bearing mice [461].
Regulatory B-Cells
The most fascinating antitumor immune mechanism of action of resveratrol is through inhibition of tumor-induced regulatory B-cells (tBregs), which inhibit breast cancer metastasis [462, 463]. Low concentrations of resveratrol significantly decreased tBregs (defined as CD25+ CD81high cells within the CD19+ population) and Treg populations in mice. It must be emphasized that resveratrol had no effect on MDSCs in the tumor models [462, 463].
Modulation of Mucosal Integrity: Implication of MUC2 and MUC1
Oral administration of resveratrol activated the expression of MUC2 and inhibited the expression of MUC1 through modification of the enzymes that initiate o-glycosylation of mucin in 1,2-dimethylhydrazine (DMH)-treated rats. Therefore, resveratrol assists in maintaining integrity of the colon [464] through modification of enzymes that initiate o-glycosylation of mucin [465].
Curcumin
Curcumin is the active polyphenol derived from the Curcuma longa plant, which is also known as turmeric. Two curcuminoids, demethoxycurcumin and bisdemethoxycurcumin, exhibit antiproliferative activity on various cancer cells [466,467,468]. Curcumin has been reported to be effective as a therapeutic and preventive agent for cancer of the colorectum, liver, lung, pancreas, breast, ovary, uterine, bladder, prostate, kidney, and brain, non-Hodgkin lymphoma, and leukemia [469,470,471]. It can exert effective immune responses and cytotoxic activity on different cancer cell lines, such as YAC-1 murine lymphoma, human HL-60 leukemia, and MDAMB breast carcinomas [472]. In vivo studies have shown immunostimulatory effects of curcumin [472, 473].
Mechanisms of Action of Curcumin: A Role for NF-ĸB
Inflammation has been implicated in the different steps of tumorigenesis, including induction, survival, proliferation, invasion, and metastasis. Primary studies described curcumin as an effective modulator of inflammation [474]. The direct effect of curcumin on inflammation has been attributed to inhibition of NF-κB signaling. NF-ĸB is a transcription factor that controls the expression of several genes involved in growth, inflammation, carcinogenesis, and apoptosis [475]. Curcumin can inhibit this pathway through downregulation of the activation of IκBα kinase (IKK), phosphorylation and degradation of IκBα, and phosphorylation and nuclear translocation of the p65 subunit [476, 477] in several cancer and premalignant cell types [478, 479]. The results were confirmed in cells isolated from patients with multiple myeloma [480] and advanced pancreatic cancer [481]. As NF-κB regulates several pathways like MMP, inhibition of NF-κB leads to downregulation of molecular events implicated in other signaling pathways and thus offers different opportunities for prevention and treatment [482] as indicated in several studies [483,484,485]. For instance, curcumin suppresses the production of CXC chemokines through inhibition of the NF-κB pathway [486]. In addition, the expression of multiple NF-κB-regulated gene products, including IL-6, IL-8, MMP-9, COX-2, and CCL2, was reduced with curcumin. Furthermore, curcumin also affects other inflammatory markers and subsequent tumor promotion [474], such as inflammatory cytokines (TNFα, IL-1, IL-6, and IL-8) [487, 488], inflammatory transcription factors (STATs), and inflammatory enzymes (COX-2, 5-lipoxygenase (LOX)) [489]. Curcumin can inhibit different invasion, cell adhesion, and extracellular matrix molecules, such as matrix metalloproteinase, CCRX4, COX-2, ELAM1, and ECAM1 [490].
Curcumin can inhibit iNOS induction and scavenge NO radicals in breast cancer cells in the promotion phase of carcinogenesis [491, 492]. TNF-α is a direct stimulator of aerobic glycolysis in malignant breast epithelial cell lines, and interestingly curcumin could reverse this effect of TNF-α [493].
Curcumin strongly prevents the generation of hematogenous metastases through suppression of the expression of NF-κB/activator protein-1 (AP-1)-dependent MMP, Egr-1, [494], and other genes involved in cell adhesion (chemokines, TNF, and Cox-2) [495, 496]. On the other hand, inhibition of NF-κB reduced the expression of prometastatic chemokine (C-X-C motif) ligand (CXCL) 1 and 2, which, in turn, decreased the expression of chemotactic receptor CXCR4 along with other prometastatic genes [486]. Decreased expression of matrix metalloproteinases, ICAM-1, and CXCR4 along with suppressed cell migration and invasion has been reported in breast cancer cell line [497].
Effect of Curcumin on Matrix Metalloproteinase-9 (MMP-9)
MMPs have been considered as one of the important molecules assisting tumor cells during metastasis [498, 499]. MMP-9 shows a major role in the breakdown of extracellular matrix in disease processes such as tumor metastasis [500]. However, curcumin shows a vital role in the inhibition of MMP-9 activities and cell invasion through downregulating NF-κB [501].
Restoration of CD4+ and CD8+ T-Cell Populations and Increased TH1-Type Response
Curcumin could efficiently restore CD4+ and CD8+ T-cell populations in the tumor microenvironment and prevent depletion of central memory and effector memory T-cells in peripheral circulating blood and lymph nodes and at the tumor site. In this manner, curcumin can drive TH2 cytokine response toward a TH1-type response [502, 503]. However, results regarding this point are not consistent. These contradicting reports suggest that curcumin may be implicated in complex signaling pathways, leading to an enhanced antitumor immunity. Curcumin is able to reverse the decrease in the levels of TH1 cytokines such as IFN-γ and the increase in TH2 cytokines such as IL-4 during cancer progression. Although some studies suggest different outcomes in which curcumin favors a TH2-type response, there are studies reporting that curcumin supports cancer regression by restoring TH1 immune responses [504, 505]. The elevated population of tumor-infiltrating lymphocytes leads to increased tumor cell killing. A delayed NK cell cytotoxic response and a simultaneous increase in IL-12 secretion in the serum of treated mice were reported after curcumin treatment [472]. Curcumin might prevent T-cell depletion by inhibiting secretion of suppressive molecule PGE-2 by tumor cells [506]. PGE-2 inhibits expression of the cytokine receptor gamma chain (γc) in T-cells, which causes deactivation of the Jak/Stat pathway and reduces expression of pro-survival protein Bcl-2 in T-cells. Curcumin through inhibition of PGE-2 would restore γc and Bcl-2 expression in T-cells and so support T-cell survival and differentiation [507].
It has been reported that curcumin arrests maturation of DCs and stimulates a tolerogenic phenotype that next promotes functional FoxP3+ TREG cells. It has been shown that DCs generated in the presence of curcumin had minimal CD83 expression, suppressed levels of CD80 and CD86, and reduced expression of both MHC class II and CD40 in comparison with those DCs that were differentiated in the absence of curcumin. Curcumin enabled arrested maturation of DCs and induced a tolerogenic phenotype [473, 503, 508, 509]. An increase in the generation of CD4+CD25highCD127low FoxP3+ TREG cells that exert suppressive functions on naïve syngeneic T-cells has also been observed with curcumin treatment [508]. Curcumin prevented loss of effector and memory T-cells, extended central memory T-cell (TCM)/effector memory T-cell (TEM) populations, reversed TH2 immune response, and attenuated tumor-induced inhibition of T-cell proliferation in tumor-bearing hosts [510].
Reduction of TREG Cell Population
CD4+CD25+FOXP3+ TREG cells play an important part in the tumor immune evasion process. Progression of tumor coincides with an elevation in TREG cells, which secrete immunosuppressive cytokines like TGF-β and IL-10 and express the high-affinity IL-2 receptor CD25, which sequesters IL-2 from the tumor milieu. It must be noted that IL-2 is necessary for proliferation of other T-cells, and so its reduction leads to effector T-cell apoptosis [511, 512].
Curcumin is able to block IL-2 signaling by decreasing accessible IL-2 and high-affinity IL-2R, as well as interfering with IL-2R signaling. Curcumin has also been demonstrated to block IL-2-induced phosphorylation of STAT5A and Janus kinase (JAK), but not JAK1, suggesting inhibition of critical proximal events in IL-2R signaling [513].
Curcumin can efficiently decrease TREG cell number and the levels of IL-10 and TGF-β [514]. Other studies also reported similar results, suggesting that treatment of CD4+CD25+ TREG cells with curcumin decreased their immunosuppressive activity [472, 515]. FOXP3 and CTLA-4 are essential for TREG function [516]. It has been shown that curcumin can reduce the expression of CTLA-4 and FOXP3, two key transcription factors that are involved in regulating transcriptional program of TREG cells and are necessary for development and function of TREG [516]. Curcumin inhibited TREG function by blocking cell-cell contact [514].
Increased oxidative stress in tumor inhibits NF-κB activity in thymic T-cells, which makes T-cells vulnerable to apoptosis by TNF-α secreted from tumor cells [517, 518]. Curcumin through inhibition of oxidative stress and reduction of surface expression of TNF-α receptor (TNFR1) on thymic T-cells of tumor-bearing mice [517] prevents reduction of NF-κB activity in thymic T-cells.
Curcumin treatment can inhibit the tumor suppressor indoleamine-2,3-dioxygenase (IDO) as well as the immunosuppressive cytokine TGF-β, thereby promoting T-cell cytotoxic activity [519]. IDO exerts its immune suppressive effect by catalyzing tryptophan, which is necessary for T-cell proliferation [520].
Reduced T-Cell Apoptosis
Prolonged injections of curcumin maintained levels of TH1 cytokines, NK cell cytotoxic activity, and production of ROS and NO by macrophages [472]. Tumor-bearing mice treated with curcumin showed improvement in immune cell numbers and tumor regression, consistent with inhibition of apoptosis in thymocytes and splenocytes [502]. Curcumin reduced T-cell apoptosis in tumor-bearing mice through activation of the JAK3-STAT5a pathway in T-cells and subsequent restoration of BCL-2 levels [506]. Inhibition of tumor-induced thymic atrophy by restoring the activity of NF-κB pathway also has been reported after curcumin treatment [517]. Eventually, although low dose of curcumin stimulated effective antitumor response by escalating CD8+ cytotoxic T-cells and IFN-γ production, higher dose of curcumin was harmful for T-cells [473].
STAT Pathway
STATs modify tumor-promoting inflammation via collaboration of other transcription factors [474, 521]. Curcumin inhibits the expression of STATs, especially nuclear STAT3, STAT5a, and STAT5b in human chronic K562 leukemia cells. When used as a pretreatment, curcumin inhibited IFN-γ-induced phosphorylation of nuclear STAT1 and STAT3 [522, 523] in human K562 leukemia cells and STAT1 in human lung A549 carcinoma and melanoma cells [524]. Following treatment with curcumin and its analogs such as GO-Y030 [525], FLLL1, and FLLL12 [526], similar downregulation of STAT3 activation was also observed in Hodgkin’s lymphoma [483], T-cell leukemia [527], head and neck squamous cell carcinoma [528], multiple myeloma cells [529], and CD138+ cells derived from multiple myeloma patients [480].
Curcumin alone or in combination with epigallocatechin gallate (EGCG) blocked STAT3 phosphorylation and undermined the interaction between STAT3 and NF-κB through suppression of CD44 expression, together diminishing breast cancer stem cells (bCSCs) population [530, 531].
COX-2
Curcumin is an effective inhibitor of COX-2 in several cancer types [532,533,534,535]. Moreover, curcumin can inhibit COX-2 expression in PBMCs of patients with pancreatic cancer [481] and on oral premalignant cells [476]. Furthermore, fluorocurcumin, a curcumin analog, has been reported to suppress NF-κB and PGE-2, and so it was suggested to be a potential agent against COX-2-overexpressing tumors [536]. Curcumin downregulates the expression of EGFR in pancreatic and lung adenocarcinoma expressing COX-2 [537] through inhibition of ligand-induced activation of EGFR [538] or through decreasing the transcriptional activity of Egr-1.
Synergy with Drugs
Several studies investigated the potential synergistic activity of curcumin in combination with conventional chemotherapeutic agents. Curcumin combined with omega-3 fatty acid could suppress the expression and activity of iNOS, COX-2, and 5-LOX and upregulation of p21 [534] and therefore prevent or even treat pancreatic tumor xenografts [534]. Curcumin would potentiate the effect of paclitaxel-mediated chemotherapy in advanced breast cancer in vitro and in vivo. This effect has been attributed to suppression of NF-κB and serine/threonine Akt pathways, COX-2, and MMP-9 [539, 540]. Reduction of COX-2 is also reported in human colon cancer HT-29 cell lines treated with curcumin combined with 5-FU [541]. Although prostate and breast cancer cells (DU145, PC-3, and LNCaP) are typically resistant to TRAIL-induced apoptosis, they can be sensitized with curcumin. This mixture stimulates inhibition of active NF-κB and other pathways that also were confirmed by preclinical studies performed in PC-3- and TRAIL-resistant LNCaP xenografts [542,543,544,545].
Interleukins
M2 macrophages and TREG cells are two main leukocytes that secrete the anti-inflammatory cytokine IL-10 [546]. M2 macrophages play a critical role in tumor progression and development consistent with increased IL-10 concentrations in various solid tumors. M1 macrophages produce IL-12, an antitumor chemokine. So, the IL-10/IL-12 ratio might predict tumor progression [547]. IL-10 could inhibit several components of immunity, including co-stimulatory and adhesion molecules (CD86 and CD54) that induce an inflammatory response in macrophages [548] and cytokines such as IL-12, IL-23, IL-1β, and TNF-α that are involved in inflammatory immune response [548,549,550]. IL-10 enhances the activation and proliferation of B-cells and antibody production. Maintaining the TH1/TH2 balance is one of the important facets of immunomodulatory action of IL-10. IL-10 has potential anticancer effects which may be mediated through reductions in the production of pro-inflammatory cytokines such as IL-1β, TNF-α, and IL-6 that play important roles in neovascularization as well [551, 552].
Curcumin can increase the frequency of M1 macrophages while decreasing the frequency of M2 macrophages, resulting in a decrease in the expression of STAT3, IL-10, and arginase-1 in mice with metastatic breast cancer. Through reduction in IL-10 levels, curcumin can also block Janus kinase-STAT signaling and increase tumor cell apoptosis [547].
Curcumin can act as an antitumor agent through prevention of tumor-induced T-cell depletion by increasing the production of IFN-γ, an important TH1 cytokine for the production and function of peripheral T-cells, and IL-2, which is crucial for differentiation of cytotoxic T-lymphocytes. Antitumor activity of curcumin could also be due to the restoration of activated/effector CD4+ and CD8+ T-cells, induction of tumor-infiltrating lymphocytes (TILs), and upregulation of IFN-γ expression. Curcumin also reduces the levels of TGF-β and IL-10 in TREG cells and decreases the number of TREG cells in the tumor microenvironment [503].
IL-8 was overexpressed in ER-negative cancer cells and showed a potential correlation with tumor progression and invasiveness. Overexpression of IL-8 is linked to progression and metastasis of cancer cells in the colon [553]. Treatment of colon cancer cells with curcumin inhibited neurotensin-induced gene expression and protein secretion of IL-8, thereby preventing migration of cancer cells [554]. Curcumin also reduced the expression of IL-8 in human pancreatic cancer cell line [555].
Exosomes and Immune Suppression in Cancer
Exosomes are small particles that are released from normal and neoplastic cells and are present in serum and other bodily fluids. Exosomes have various molecules including signal peptides, mRNA, and microRNA. Tumors also secrete exosomes which are immune suppressive bodies containing a distinct set of proteins that can affect the immune system. In cancer, signaling via exosomes affects the immune system through inhibition of T-cell and NK cell functions and an increase in the number and/or activity of immune suppressor cells, including myeloid-derived suppressor cells (MDSCs), TREG cells, and CD116+ HLA-DR−/low cells [556]. Curcumin reduces the inhibitory effects of exosomes on NK cytotoxicity [557]. Of note, curcumin can reverse the tumor exosome-mediated inhibition of NK cell function via the ubiquitin-proteasome pathway [558].
Green Tea and Catechins
Several epidemiological and experimental studies have reported a negative correlation between green tea and development of cancers of the bladder, cervix, breast, esophagus, colorectum, stomach, lung, liver, ovaries, oropharynx, pancreas, prostate, and skin [559]. The health benefits of green tea could be mostly attributed to catechins, including catechin (C), epicatechin (EC), epigallocatechin (EGC), and epicatechin gallate (EGCG).
Transcription Factors
EGCG has been found to suppress the expression and/or activity of many transcription factors, such as HIF-1α, nuclear STAT1 and STAT3, NF-κB, and AP-1. In addition, different MMPs, including MMP-2, MMP-9, and MMP-14/MT1-MMP, have been downregulated by EGCG [559]. EGCG has been reported to block angiogenesis and decrease xenograft tumor growth via inhibition of IGF-1 through downregulating the protein expression of HIF-1α and VEGF in A549 lung cancer cells [560, 561] and via inhibition of HIF-1α-dependent expression of VEGF, IL-8, and CD31 in other lung NCI-H460 cell lines [562]. EGCG blocked xenograft angiogenesis and tumor growth in gastric cancer cell line BGC-823 [563]. EGCG is also able to inhibit IL-6-induced angiogenesis via inhibition of VEGF expression through downregulating Stat3 activity in human gastric carcinoma AGS cells and SGC-7901 cancer cells [564, 565]. In HeLa cervical cancer cell line, EGCG inhibited cell proliferation and invasion through suppression of MMP-9 gene expression and upregulation of TIMP-1 gene expression [566]. In SW837 CRC cell line, EGCG inhibited tumor growth by downregulating HIF-1α and several major growth factors [567]. In T-24 bladder cancer cell line and SW620 cell line, EGCG inhibited cell adhesion, migration, and invasion through suppression of MMP-9 expression via inhibition of NF-κB signaling pathway [568]. In esophageal TE-8 and SKGT-4 cancer cells, EGCG reduced cell invasion through lessening p-ERK1/p-ERK2, c-Jun, and COX-2 [569].
Overexpression of the human epidermal growth factor receptor-2 (HER2/neu) is linked to poor prognosis in various types of cancer. EGCG blocks activation of these receptors by inhibiting STAT3 and NF-κB activation. EGCG and Polyphenon E (PolyE) have been shown to decrease transcriptional activity of AP-1 and NF-κB promoters and inhibit COX-2 transcription and PGE-2 production in CRC cell lines [570].
Effect of Green Tea on Nuclear Transcription Factor NF-κB
EGCG has been reported to inhibit the activation of NF-κB in H891 human HNSCC cells, MDA-MB-231 human breast cancer cells, PC-9 human lung cancer cells, human colon cancer cells, A431 epidermoid carcinoma cells, and H891 head and neck cancer cells. EGCG decreased lipopolysaccharide (LPS)-induced TNF production in the RAW 264.7 macrophage cell line [571]. Treatment with EGCG and PolyE reduced the levels of inflammatory cytokines, such as TNF-α, in the colon epithelium and also inhibited inflammation-related colon carcinogenesis induced by AOM and DSS injection in a mouse colon cancer model [572].
Regulation of the NF-κB pathway may play a critical role in mediating chemopreventive properties of catechin in prostate cancer cells. Catechin treatment regulates NF-κB gene expression through accumulation of IκBα, repression of NF-κB phosphorylation [573], reduction in IKKα expression, inhibition of IKK activity [574] and proteasome and caspase cleavage of the p65 subunit [575], and reduction in other signaling factors, including RANK and NIK [573]. NF-κB target genes involved in carcinogenesis, including Bcl-2, Bcl-xL, survivin, MMPs, VEGF, uPA, and iNOS [576,577,578], are also decreased by catechin treatment. Thus, one of the probable mechanisms by which EGCG can exert antitumor effects is through suppression of the NF-κB signaling pathway.
EGCG treatment resulted in decreased COX-2 promoter activity through inhibition of NF-κB activation [579]. AP-1 serves as another potential target for anticancer effects of EGCG [580]. EGCG has been demonstrated to interfere with AP-1-induced transcriptional activity through inhibition of a JNK-dependent pathway [581].
Effect of Green Tea Catechins on Cyclooxygenase and Lipoxygenase
EGCG has been reported to inhibit mitogen-induced COX-2 expression in androgen-sensitive LNCaP and androgen-insensitive PC-3 human prostate carcinoma cells [582]. Pretreatment with green tea catechins inhibited COX-2 expression induced by 12-O-tetradecanoylphorbol-13-acetate (TPA) in mouse skin and reduced COX-2 expression in the SW837 human CRC cell line, colon epithelium, and LPS-induced macrophages. It has been shown that EGCG decreases the activity of COX-2 after IL-1A stimulation of human chondrocytes [583]. Recent cancer research suggests that development of compounds, which can inhibit COX-2 expression preferably without affecting COX-1, is a hopeful approach for cancer chemoprevention. The inhibition of NF-κB is suggested as a possible mechanism for inhibition of COX-2 expression. EGCG, EGC, and ECG from green tea and theaflavins from black tea have been reported to inhibit lipoxygenase (LOX)-dependent activity by 30–75% [584]. Consumption of green tea and dietary fat modulates 5-lipoxygenase-dependent pathway of arachidonic acid metabolism throughout AOM-induced colon carcinogenesis [585].
Effect of Green Tea on AP-1 Transcription Factor
AP- 1 is another transcription factor including Jun and Fos protein families that regulates expression of gene associated with apoptosis and proliferation. AP-1 has been implicated in cancer development and progression. AP-1 is induced by TNF and IL-1 as well as by a variety of environmental stimulators like UV radiation. Theaflavins and EGCG inhibited ultraviolet B (UVB)-induced AP-1 activation [586] and AP-1-dependent transcriptional activity and DNA binding activity [587, 588]. A previous study in JB6 mouse epidermal cell line demonstrated that EGCG treatment inhibits AP-1 activation and cell transformation and Ras-activated AP-1 activity in the H-ras-transformed cells. EGCG inhibits AP-1 activity through inhibition of JNK but not ERK activation [586]. EGCG or PolyE treatment causes inhibition of AP-1 and NF-κB luciferase reporter activity in the HT29 human colon cancer cell line. These findings indicate that inhibition of the NF-κB and/or AP-1 pathways is a possible mechanism underlying anticancer effects of green tea catechins [589, 590].
Effect of Green Tea on STAT3
EGCG inhibited phosphorylation of EGFR, Stat3, and ERK proteins in human HNSCC cell lines such as YCU-N861 and YCU-H891 [591]. Inhibition of activation of the EGFR, Stat3, and Akt by EGCG treatment has been shown in YCU-H891 HNSCC and MDA-MB-231 breast carcinoma cell lines [592].
EGCG-induced increase in IFN-γ secretion in a previous study has been attributed to an increase in NK and NK T-cell numbers that could be due to induced STAT1 activity. A previous clinical trial on 20 patients with stage IV cancer with a special regime containing soy extract reported increased cytotoxic activity of NK cells and TNF-α secretion [593]. An aggressive combination of immunoactive nutraceuticals was efficient in significantly increasing NK function [593].
Inflammatory Factors
Different studies reported that EGCG is able to inhibit the expression of various inflammatory factors in tumor cells including inflammatory cytokines (IL-8), inflammatory growth factors (insulin-like growth factor 1 (IGF-1) and VEGF), and inflammatory mediators (COX-2 and iNOS). In addition, it can inhibit the expression of chemokines, such as the colony-stimulating factor 1 (CSF-1) and C-C motif chemokine ligand 2 (CCL2). Therefore, targeting different inflammatory factors might play an important role in EGCG-mediated cancer inhibition [559, 594,595,596,597].
Modulation of Antitumor Immunity
Green tea has been reported to enhance humoral and cell-mediated immunity, resulting in reduced risk of certain cancers [579]. IDO, an immune regulatory enzyme, is associated with tumor immune escape. EGCG has been reported to downregulate the expression of IDO in human oral and colorectal cancer cells by inhibition of STAT1 function [579], concurrent with increased antitumor immunity. This indicates that EGCG can be a potential regulator of tumor immunity [598, 599].
Myeloid-Derived Suppressor Cells
MDSCs contribute to the negative regulation of immune responses. MDSCs downregulate T-cell function through generation of arginase, NO, ROS, and peroxynitrate. However, in the tumor microenvironment, MDSCs are able to differentiate into tumor-associated macrophages (TAMs) and express arginase and iNOS and suppress generation of ROS [600, 601]. Besides antigens and co-stimulation, cytokines are required for T-cell activation, proliferation, and maintenance. Recent studies have shown that cytokines (IL-12 or IFN-γ) released by DCs or other APCs can act as the third signal that is responsible for activation, expansion, and appropriate production of effector and memory T-cells [602]. However, the tumor microenvironment cannot supply such inflammatory signals, leading to inappropriate activation of DCs. Furthermore, tumors produce immunosuppressive cytokines such as IL-10 and TGF-β and also increase TREG cell number, which both further dampen proper DC activation [600].
Myeloid cells hamper the function of T- and NK cells. It is well known that tumor-induced TREG cells blunt NK and CD4+/CD8+ T-cell-mediated immune responses. PolyE is able to promote the differentiation of MDSCs into more mature neutrophil-like cells with hypersegmented nuclei [603]. These cells are unable to inhibit the secretion of IFN-γ from CD3+ splenocytes in vitro. MDSCs were less infiltrated into the neuroblastomas of mice drinking PolyE in comparison with control group. This confirms the hypothesis that catechins hinder the migration of myeloid cells to the tumor site. MDSCs interfere with the antitumor activity of CD8+ T-cells. Intriguingly, another study has reported that EGCG enhances CD8+ T-cell-mediated antitumor immunity as obtained by DNA vaccination. Depletion of immunosuppressive TREG cells by means of a CD4-specific antibody decreases the growth of neuroblastomas in A/J mice [604]. In another report, depletion of CD4+ cells failed to modify tumor growth in neuroblastoma cells of A/J mice, which received PolyE-pretreated MDSCs. These findings possibly show that MDSCs fail to stimulate CD4+ TREG cells when they have been exposed to PolyE. PolyE could be potentially beneficial in cancer patients by antagonizing cells that interfere with antitumor immune responses elicited by immunotherapy [604, 605].
Other investigators suggest the role of immunoregulatory cytokine IL-12 in DNA repairs and induction of cytotoxic T-cells in the tumor microenvironment in skin cancer models [606]. In fact, EGCG inhibits UVB-induced immunosuppression and induces repair in mice through stimulation of IL-12. Mechanisms of green tea for chemoprevention in lung cancer include antioxidant activity, phase II enzyme induction, and inhibition of TNF-α expression. EGCG also inhibits UVB-induced infiltration of leukocytes and APC depletion [603, 606, 607]. In addition, topical application of EGCG has been shown to inhibit UVB-induced angiogenesis while inducing cytotoxic T-lymphocytes (CD8+ T-cells) in skin tumors on SKH-1 mice [608].
Synergistic Effect of EGCG Combined with Other Bioactive Compounds and Chemotherapeutics
Recent studies have found synergistic antitumor effect of EGCG in combination with other dietary bioactive compounds like ascorbic acid, curcumin, 6-gingerol, N-acetylcysteine, panaxadiol, pterostilbene, quercetin, sulforaphane, vitexin-2-o-xyloside, raphasatin, EPA-FFA, and proanthocyanidins. Combination of EGCG with these small molecules can synergistically inhibit cancer growth through enhanced bioavailability of EGCG.
Several studies reported that EGCG could sensitize cancer cells to X-irradiation and ionizing radiation in different cell lines like glioblastomas and promyelocytic leukemia HL-60 cells. In addition, EGCG can also improve the chemotherapeutic effect of various drugs such as paclitaxel, capecitabine, cisplatin, docetaxel, and doxorubicin (DOX). Therefore, considering EGCG as an adjuvant therapy can be a practical and efficient approach for cancer treatment [559].
Ginseng
Ginseng (the root of Panax ginseng) is a well-known herbal medicine for the treatment of various disorders. The main active components of ginseng include a series of tetracyclic triterpenoid saponins (ginsenosides), polyacetylenes, polyphenolic compounds, and acidic polysaccharides [609]. Until now, 38 ginsenosides have been purified from ginseng roots, with seven major ones, namely, Rg1, Re, Rf, Rb1, Rc, Rb2, and Rd, comprising more than 80% of the total available ginseng [610]. Ginsenosides can be classified into three groups: the protopanaxadiol group (e.g., Rb1, Rb2, Rb3, Rc, and Rd), the protopanaxatriol group (e.g., Re, Rf, Rg1, and Rg2), and the oleanane group (e.g., Ro) [611, 612]. The acidic polysaccharides are found to be more biologically active. Preliminary studies showed that the neutral polysaccharides contain antitumor activity [613]. A case-control study in Korean population reported that long-term ginseng intake was associated with a decreased risk of different types of cancers [614]. The main active components of red ginseng for cancer prevention are ginsenosides Rg3, Rh2, Rg5, and PPD, which work synergistically [615, 616].
Acidic polysaccharides of ginseng (ginsan) isolated from the ethanol-insoluble fraction of the P. ginseng root have also demonstrated anticancer immune modulatory function [617, 618]. Treatment with ginsan (acidic polysaccharide fraction of ginseng) makes splenocytes isolated from unprimed normal mice to be converted into activated killer (AK) cells, which can induce cytotoxic activity on numerous tumor cells comprising NK-resistant murine mastocytoma cell line P815 and NK-sensitive murine lymphoma cell line YAC-1 [619, 620]. Ginsan can be combined with other immunotherapeutics like IL-2 to enhance antitumor effect. Ginsan can stimulate the production of cytokines IFN-γ, IL-2, IL-1, TNF-α, IL-12, GMCSF, and IL-4 to modify the function of AK cells. Macrophages are also necessary as accessory cells for the production of AK cells by ginsan [619]. The immune phenotype of these cells was described to be Thy1+ (thymocyte and peripheral T-cell marker), AsGM+ (NK cell and basophil marker), CD4+, and CD8+ [619].
Ginsan is able to convert macrophages into an M1 tumor inhibitory phenotype [617] as reported in peritoneal macrophages on murine B16 melanoma and fibroblast L929 cells. Generation of NO and ROS by macrophages is modified by inflammatory cytokines; and ginsan-treated peritoneal macrophages significantly enhance secretion of IFN-γ, TNF-α, IL-1β, and IL-6 [617].
Red ginseng acidic polysaccharide (RGAP) increased cytokine secretion by macrophages but did not stimulate their tumoricidal activity on its own [618]. RGAP combined with recombinant IFN-γ possesses an increased synergistic effect on the cytokine production and phagocytic and cytotoxic capacity of macrophages against murine B16 melanoma cells. Activation of the NF-κB pathway has been postulated to be responsible for this synergistic effect [618].
The red ginseng ginsenoside Rg3 also showed stimulatory effects on macrophages and increased the phagocytic index of peripheral blood macrophages resulting in an improved antitumor effect in a mice model of lung carcinoma [621]. Korean red ginseng (KRG) possesses no effect on the accumulation of MDSCs. However, it might inhibit suppressive function of these cells leading to immune activation mediated by T-cell proliferation and cytokines IFN-γ and IL-2 [622]. Altogether, it must be mentioned that the bioactive constituents of ginseng demonstrated favorable anticancer immunotherapeutic effects, which are mainly modified via production of tumoricidal macrophages and AK cells.
Anti-inflammatory Effects
Several ginsenosides have been shown to affect inflammatory signaling pathways, thereby inhibiting cancer development [623]. In a chemically induced mouse model of skin carcinogenesis, topical administration of ginsenoside Rg3 suppressed TPA-induced activation of NF-κB and AP-1 and COX-2 expression, accounting for its antitumor effects [624]. 20(S)-Rg3 can inhibit the production of ROS, but not that of NO, and decrease the production of cytokines, such as TNF-α, IL-1β, IL-6, and PGE-2 in LPS-stimulated Raw 264.7 murine macrophages and human keratinocyte (HaCaT) cells [625]. In MCF-7 cells, ginsenoside Rg1 inhibited MMP-9 activity through NF-κB-mediated suppression of breast cell migration and invasion [626].
Ginsenoside Rg5 is also able to suppress NF-κB activity in a lung inflammation model. Rg5 reduced the expression of COX-2, iNOS, IL-1β, and TNF-α in LPS-stimulated alveolar macrophages through inhibition of IL-1 receptor-associated kinases (IRAKs) and IκB kinase-β (IKKβ), subsequently blocking the phosphorylation and nuclear accumulation of NF-κB [627]. Inhibition of NF-κB and subsequent reduction in IL-8 and PGE-2 also have been demonstrated in human embryonic kidney (HEK)-293 cells and HaCaT keratinocytes [628].
Treatment of human esophageal carcinoma cells with ginsenoside Rg3 reduced expression of VEGF, which was associated with the reduced expression of HIF-1α and COX-2 and diminished NF-κB activity [629]. Rg3 combined with gemcitabine significantly reduced the growth rate of Lewis lung carcinoma cells transplanted in C57BL/6 mice by reducing the expression of VEGF [630].
P. ginseng can inhibit chemically induced aberrant crypt foci in mice maybe through anti-inflammatory activities like inhibition of COX-2. Ginseng can also inhibit MMPs and kinase pathways. In addition, it was demonstrated that ginseng activates PPAR-γ and TGF-β1, which are capable to interfere with the inflammation-to-cancer process. The following anti-inflammatory effects of ginsenosides have been reported in cancer models: inhibition of COX-2 and NF-κB in gastric cancer; inhibition of MAPK, NF-κB, and AP-1 in liver, lung, and breast cancer; and inhibition of iNOS, COX-2, and NF-κB in mammary and liver cancer [631].
Compound K (CK) significantly inhibited the secretion and protein expression of MMP-9. The inhibitory effect of compound K on MMP-9 expression was correlated with decreased MMP-9 mRNA levels and reduced MMP-9 promoter activity [632].
Red ginseng inhibited tumor growth by influencing neovascularization and angiogenesis. The angiosuppressive effect of Rg3 could be due to the differential regulation of MMP-2 and MMP-9 activities [633]. Dose-dependent downregulation of MMP-2 and MMP-9 production by Rg3 is thought to be responsible for the inhibition of endothelial cell invasiveness and angiogenesis [633]. Rg3 effectively abrogated the VEGF-dependent neovessel formation, leading to delayed tumor angiogenesis [634]. In a model for gastritis and gastric cancer, treatment of endothelial cells with KRG significantly reduced the expression of inflammatory mediators, including iNOS, COX-2, IL-8, and IL-1β, and angiogenic factors including IL-6, VEGF, platelet-derived growth factor, and MMPs [618].
Role of microRNA in Inflammation-Related Angiogenesis
Recent researches have highlighted a role for microRNAs (miRNAs) – noncoding short RNA molecules (18 to 23 nucleotides) – in controlling gene expression by directing mRNA degradation or repressing post-transcriptional translation, thereby silencing gene expression [635].
A recent study showed that ginsenoside Rh2 caused upregulation of 44 miRNAs and downregulation of 24 miRNAs in human non-small cell lung cancer cells. Interestingly, affected miRNAs were mostly involved in angiogenesis, inflammation, and cell proliferation [636]. Furthermore, Rh2 suppressed miR-21, miR-27b, and miR-31, all of which exhibit pro-angiogenic effects consistent with the reported anti-angiogenic activities of Rh2 [637]. Ginsenoside Rg3 has been shown to regulate VEGF-induced angiogenic response via miRNA modulation [635]. Red ginseng caused a synergistic effect with drug 5-FU for antiproliferative impact on a human CRC model [638]. Red ginseng significantly potentiated the anticancer activities of epirubicin and paclitaxel; thus, their dose and adverse events could be decreased [639]. Rg3 has been demonstrated to block NF-κB signaling and improve the vulnerability of prostate cancer cells to docetaxel and other chemotherapeutics. Also, protective effect of red ginseng in anticancer drug-induced toxicity was reported to be mediated via the regulation of NF-κB activities [640].
Carotenoids
β-Carotene is the main carotenoid isolated from orange and yellow fruits and vegetables. Lycopene is the main carotenoid found in red fruits and vegetables. The correlation between the high dietary consumption of carotenoids and low risk of prostate cancer has been frequently investigated. The inhibitory effect of β-carotene on the proliferation of human cancer cell lines (PC-3, DU 145, and LNCaP) has been previously demonstrated [641]. Carotenoids have been investigated for their immune-enhancing effects mostly via induction of NK cell activities and increasing leukocyte cell number, CD4/CD8 ratio, and MHC I expression [642]. The antitumor effect of dietary lutein has been investigated in a mammary tumor-bearing mice model. Lutein showed a stimulatory effect on IFN-γ expression while suppressing the expression of IL-10 in splenocytes [643, 644].
Lycopene is a potent antioxidant that can be used as a protective anticancer agent [645]. The antiproliferative and apoptotic effects of lycopene have been shown in prostate cancer cell line (LNCaP) [646], colon cells (HT-29 and T84), and breast cancer cell lines [647]. Both lycopene and β-carotene have been shown to inhibit metastasis in experimental settings, for example, lung metastasis in B16F-10 melanoma cells in C57BL/6 mice and in human hepatoma SK-Hep1-1 cells. Lycopene also decreases the level of VEGF and MMP [648].
In vitro administration of lycopene effectively reduced inflammatory signaling. Lycopene was able to inhibit the mRNA and protein expression of the pro-inflammatory cytokine IL-8 via inactivation of the NF-κB transcription factor through inhibition of the phosphorylation of IKK and IKB and by decreasing the translocation of the NF-Bp65 subunit from the cytosol to the nucleus. Lycopene also decreased the production of TNF, COX-2, iNOS, and IL-6 [649, 650]. The effects of lycopene were correlated with reduced phosphorylation of COX-2, PGE-2, and ERK1/ERK2 [651]. Lycopene also decreased MMP-7 expression in colon cancer cells. The decrease of MMP-7 expression by lycopene was associated with diminished stability and increased E-cadherin expression, showing that MMP-7 may hydrolyze this adhesion molecule. Furthermore, lycopene decreased MMP-7 and c-myc expression by blocking AKT, GSK3, and ERK1/ERK2 phosphorylation [652].
β-Cryptoxanthin was shown to reduce the gene expression of IL-1α in mouse macrophage RAW 264 cells [653]. Both astaxanthin and canthaxanthin exhibited inhibitory activity in relation to cancer development in the urinary bladder, tongue, and colorectum through downregulation of cell proliferation. Another study demonstrated the anti-inflammatory and antitumor effects of astaxanthin in inflamed colon due to modification of the expression of inflammatory cytokines that are involved in inflammation-associated carcinogenesis [654]. Indeed, astaxanthin may aid COX-2 suppression [655]. Other studies reported that in 1,2-dimethylhydrazine (DMH)-induced colon carcinogenesis, daily administration of astaxanthin significantly blocked colon carcinogenesis by modifying the expression of NF-κB, COX-2, MMP-2, MMP-9, ERK2, and protein kinase B (Akt) [656]. Lycopene decreased the invasive ability of hepatoma cells by downregulating the activity of NF-κB [657], maybe through suppression of IGF-1 receptor. Lycopene could be efficient in treatment of benign prostate hyperplasia (BPH) via inhibition of NF-κB. On the contrary of the inhibitory effect of lycopene on NF-κB activity, β-carotene stimulated NF-κB in human leukemic (HL-60) and colon adenocarcinoma (LS-174 and WiDr) cells [658]. Astaxanthin attenuated the production of inflammatory markers and cytokines by LPS in vitro (LPS-treated RAW 264.7 cells and primary macrophages) and in vivo (LPS-treated mice) through NF-κB inhibition. Furthermore, astaxanthin thoroughly inhibited all the main signaling molecules involved in NF-κB activation, like IkB kinase phosphorylating activity, IkBa degradation, and the nuclear translocation of the NF-κB p65 subunit [659]. Anti-angiogenic effect of β-carotene was investigated by an in vivo model of B16F-10 melanoma in mice and by in vitro studies [660]. β-Carotene treatment significantly decreased the number of tumor-directed vessels concurrent with reduction of serum VEGF and pro-inflammatory cytokines, e.g., IL-1β, TNF-α, and IL-6. In addition, similar decrease of these cytokines was detected after β-carotene treatment in melanoma cells and found to result from inhibition of c-Rel subunit of NF-κB and AP-1. AP-1 transcription system has been shown to be blocked by lycopene in MCF-7 mammary cancer cells [661]. The AP-1 complex comprises proteins from the Jun (c-Jun, JunB, and JunD) and Fos (c-Fos, FosB, Fra-1, and Fra-2) families, which are connected as homo- (Jun/Jun) or heterodimers (Jun/Fos). It is probable that lycopene and retinoic acid decrease growth factor-induced induction of AP-1 transcriptional activity by changing the composition of AP-1 complexes that bind to DNA [662, 663]. There was a three- to fourfold increase in the expression of c-Jun and c-Fos genes in the lungs of ferrets, supplemented with high-dose β-carotene and exposed to tobacco smoke. This study suggested a possible explanation for the enhancing effect of β-carotene on lung carcinogenesis in smokers, as demonstrated in large intervention studies [664].
Under basal conditions, Nrf1 and Nrf2 are present in the cytoplasm bound to the inhibitory protein Keap1. After challenge with stimulating agents, they are released from Keap1 and translocated to the nucleus [665, 666]. Studies have shown that dietary antioxidants (terpenoids [667]), flavonoids (epigallocatechin gallate (EGCG) [668, 669]), and isothiocyanates may function as anticancer agents by activating this transcription system. However, hydrophobic carotenoids such as lycopene lack any electrophilic group and, therefore, are unable to interact with Keap1. Thus, it seems that oxidative products actively play a role in the induction of the EpRE/ARE (electrophile/antioxidant response element) transcription system by carotenoids. It has been demonstrated that oxidized derivatives, isolated by ethanol from partially oxidized lycopene, transactivated EpRE/ARE in HepG2 human hepatocellular carcinoma cells [670] with a strength resembling to that observed with unextracted lycopene mixture. In contrast, the intact carotenoid exhibited a small insignificant effect [671].
Isoflavones
Isoflavones, such as daidzein and genistein, are mostly found in soybeans. Previous experimental and epidemiological studies suggest cancer protective effects of isoflavones and their metabolites. Genistein was described to downregulate direct cellular cytotoxicity and ADCC. Genistein is able to inhibit tyrosine kinase activity, which is crucially involved in NK cell activation in epidermoid carcinoma A431 cells [672]. Both genistein and daidzein are extensively metabolized in humans and found as conjugated metabolites, mainly glucuronides [673, 674]. Genistein and daidzein glucuronides could increase NK cell-mediated cytotoxicity in human PBMCs at nutritionally achievable concentrations, which were tenfold lower than concentrations of isoflavones used to inhibit tumor cell (MCF-7 and MDA-468 human breast cancer cells) growth in vitro [673, 675]. At higher concentrations, however, genistein decreased NK cell-mediated killing of K562 target cells. In the presence of IL-2, genistein increased NK cell activation at even lower concentrations. The existence of IL-2 may be essential for genistein to increase NK cell activity, and this may be correct for other flavonoids too. Factors determining the effects of genistein on NK cell activity in mice include the duration of exposure, sex, and even generation. The described effects may be of nutritional relevance as isoflavone concentrations after soy consumption are within the range (<2 μmol/L) for which NK cell activation is anticipated. The glucuronides were generally less potent than genistein and daidzein [673]. Genistein administration by oral gavage for 1–4 weeks increased NK cell-mediated cytolysis and cytotoxic T-cell activity in B6C3F1 mice [676].
Moreover, increased host resistance was shown in adult B6C3F1 mice (intravenous injection of B16F10 melanoma cells) treated with genistein, as reflected in lung tumor weight and NK cell modulatory effects [676]. Increased intake of dietary soy has been reported to reduce the severity of macroscopic lung metastasis [677]. In a study in bladder cancer, isoflavone-rich soy phytochemical concentrate (SPC) was shown to have greater anti-metastatic effect in comparison with genistein. Particularly, SPC but not genistein significantly blocked lung metastases through suppression of NF-κB expression in tumor tissues and reduction of circulating IGF-1 levels [678]. Besides decreasing the metastasis of breast cancer cell to lung [679], genistein has been shown to be a useful chemotherapeutic agent to inhibit the development and metastasis of sex gland cancers such as prostate cancer [680]. Inhibition of MMP-9 by genistein also has been suggested as a possible mechanism for prevention of prostate cancer to bone metastasis [681, 682]. Other genes targeted by genistein in primary stages of breast cancer include MMP-2, MMP-7, and CXCL12, which support invasion and metastasis [683, 684]. Genistein also inhibited the activation of focal adhesion kinase [685] and HSP27 pathway [685], which regulate cancer cell detachment and invasion, respectively. Genistein has been reported for its cytotoxic effect in prostate cancer cell lines LNCaP and PC3 [686], hepatoma cancer cell lines (HepG2, Hep3B) [687], and A431 and Colo205 xenograft tumors, [688, 689]. Genistein can be used combined with conventional therapy such as 5-FU, all-trans retinoic acid (ATRA), and trichostatin A to improve their cytotoxicity and apoptotic activity in human pancreatic cancer cell line (MIA PaCa-2) [690] and human lung cancer cell line (A549) [691, 692]. Genistein at very low concentrations stimulated the proteinase inhibitor 9 (PI-9), which is a granzyme B inhibitor and inhibits the capability of NK cells to lyse breast cancer cells [693] with an opposite activity in high concentrations [676]. Moreover, it seems that polyphenol-stimulated NK cytotoxicity depends on the cell type. Genistein has also shown to decrease in vitro cytotoxic activity of NK cells in melanoma and breast cancer cells [524, 693] and, in contrast, was found to increase NK-mediated cytotoxicity in in vitro and in vivo tumor models [676, 694, 695].
Quercetin
Quercetin is a well-known flavanol, which has been shown to inhibit NK cell killing activity in peripheral blood lymphocytes from human donors. However, high doses of quercetin could cause pro-apoptotic or cytotoxic effects through the inhibition of Ca2+ channels and Na+/K+ ATPase activity [122, 696]. More clearly, indirect NK cell stimulation by quercetin resulting in augmented IFN secretion has been reported in low doses of quercetin. Quercetin improved NK cell activity in BALB/c mice treated with WEHI-3 leukemia cells and oral quercetin [697].
Quercetin stimulated NK cell activity through inhibition of protein kinase C (PKC), PI3K, and HSP70 in target cells while increasing the expression of NKG2D ligands [698, 699]. Some chemotherapeutics were reported to increase the expression of NKG2D and HSPs, thereby decreasing cell vulnerability to NK cell-mediated cytolysis. It has been reported that quercetin can induce the expression of NKG2D ligands, MHC class I-related chain B (MICB), UL16-binding protein 1 (ULBP1), and UL16-binding protein 2 (ULBP2) while downregulating the expression of HSP70 in K562 (erythroleukemia), SNU-1 (gastric carcinoma), SNU-C4 (colon cancer), and human Raji (Burkitt’s lymphoma) target cells, together reflected in increasing cell susceptibility to NK-92-mediated lysis [698]. It has been suggested that increased NKG2D ligand expression was mostly responsible for the inhibitory effect of quercetin on NF-κB and PI3K [698]. Quercetin demonstrated an antiproliferative effect through the induction of apoptosis by disturbing the MMP system [700, 701]. In addition, quercetin can be administrated combined with other chemotherapeutic agents such as doxorubicin to enhance their cytotoxic effects on liver cancer cells (SMMC7721 and QGY7701) as well as to provide protection for non-tumoral liver cells from toxic effects of free radicals [702].
Quercetin is able to reduce the number and size of polyp in the Apc (Min/+) mouse through reduction in macrophage infiltration [703]. In addition, treatment with quercetin prior to intraperitoneal injection of EAT tumor cells stimulated macrophage spreading, suggesting that this compound affects the tumoricidal activity of macrophages [704]. In vivo, tumor-bearing mice treated with quercetin showed an improvement in the phagocytic activity of peritoneal macrophages [697].
β-Glucan
β-Glucan is a polymer made of D-glucose molecules that are connected by linear β-glycosidic bond with side branches that are different based on their sources [705]. β-Glucans, including zymosan, laminarin, lentinan, and pleuran, are found in mushroom, barley, cereals, and seaweeds as well as bacterial and fungal cell wall. The anticancer effect of β-glucan is chiefly because of its immunomodulatory effect rather than its direct cytotoxic activity. A range of β-glucans have been described as immunomodulators [706]. β-Glucans are able to induce the immune system effector cells, mostly macrophages, monocytes, neutrophils, NK cells, and DCs via their interaction with glucan-specific receptors, such as dectin-1, TLR, and CR3 (complement receptor 3 or CD11b/CD18), expressed by these cells [707]. In addition, they can increase the phagocytic effects of neutrophils, NK cells, and cytotoxic T-lymphocytes. β-D-Glucans have been demonstrated to stimulate the secretion of pro-inflammatory cytokines (IL-1α/IL-1β, TNF-α, IL-2, IFN-γ, and IL-12) that stimulate antitumor immune response as well as NO and H2O2 by activated macrophages that demonstrated antitumor effect [708]. The effect of natural β-glucan, schizophyllan, combined with chemotherapy was investigated on the survival rate of patients with ovarian cancer [709]. Furthermore, Maitake D-fraction found in Grifola frondosa (Maitake mushroom) has been reported to decrease the size of tumors, primarily in the lung, liver, and breast, in more than 60% of treated patients [710]. Moreover, supplementation with 5.4 grams Ganoderma polysaccharides per day for 12 weeks boosted immune responses in patients with lung and colorectal cancer [711, 712]. β-Glucans combined with mAbs RMA-S-MUC1 subcutaneously implanted in C57Bl/6 mice improved complement receptor 3 (CR3)-mediated phagocytosis of ic3b (inactivated C3b)-opsonized tumor cells by effector granulocytes and enhanced tumor recession in treated animals [713]. Lentinan, derived from Lentinus edodes, was shown to induce apoptosis in hepatoma H22-bearing mice [714], cervical carcinoma HeLa cells, and hepatocellular carcinoma (HepG2 and SMMC-7721 cell). Furthermore, lentinan induced antitumor immune responses through enrollment of immune cells, mostly macrophages and T-lymphocytes, into TME to attack tumor cells and release inflammatory chemokines (TNF-α, IL-2, IL-1β, TGF-β, IP-10, M-CSF, and TREM-1). The immunomodulating effects of arabinogalactan (AG) and fucoidan (FU) in vitro have been investigated in mouse spleen lymphocytes, which turned cytotoxic after treatment with AG and FU. Novel maloyl glucans have been isolated from aloe vera gel (Aloe barbadensis) – veracylglucan B possesses both anti-inflammatory and antiproliferative effects, while veracylglucan C has merely shown anti-inflammatory effects and appears to complement the actions of veracylglucan B [715].
Withania somnifera
Withania somnifera (WS), also known as Ashwagandha, has been a part of Ayurvedic medicine for many centuries. WS has been reported to be efficient in arthritis, cancer, and mental disorders [716, 717]. Steroidal lactones, including withanolides and withaferins, are the most biologically active components [716]. Among them, withaferin A (WA) and withanolide A have been investigated for anticancer and immunomodulatory effects, respectively [718, 719].
Along with its antitumor effect, treatment of tumor-bearing mice with withanolide A led to the polarization of TH1 cells and subsequent increase in the production of pro-inflammatory cytokines (IFN-γ and IL-2) while reducing the polarization of TH2 cells [720]. Moreover, there was a significant increase in the proliferative activity of CD4+ and CD8+ T-cells present in the serum of WS-treated mice. In response to stimulation with concanavalin A (Con A) and LPS, proliferation of T-cells and B-cells was also significantly increased with WS treatment. Treatment with WA not only increased NK cell population in one study but also increased its cytotoxic activity. In addition, APCs purified from blood samples of tumor-bearing mice showed an enhanced maturation and expression of co-stimulation markers (CD80, CD40, and CD40L) on T-cells [720], suggesting the effective role of WS in DC-mediated activation of T-cells – all of which may be involved in antitumor function of WS. WA treatment induced tumor rejection and protection from rechallenge. This indicates that WA can build immunological memory in Ehrlich ascites carcinoma model. A possible mechanism of tumor rejection could be attributed to macrophages because WA increased the frequency of peritoneal macrophages, and transfer of these macrophages from cured mice caused tumor rejection. In a breast cancer model, WA induced immunogenic cell death (ICD) in cancer cells through expression of HSPs such as HSP70, HSP90, and calreticulin on the membrane of tumoral cells. All of these ICD mediators bind to receptors on DCs, leading to activation and maturation of DCs and the production of inflammatory cytokine IL-12 [721]. Of note, WA could diminish the function of the tumor inhibitory immune cell type, i.e., myeloid-derived suppressor cells (MDSCs), to generate ROS known to mediate the suppressive effect of MDSCs on T-cells [722].
Flavone Acetic Acid (a Synthetic Flavonoid)
Synthetic flavone acetic acid (FAA) has been frequently investigated for its antitumor activities. In particular, it has the ability to induce NK cell activity [723]. FAA increased NK cell-mediated killing activity in both healthy and tumor-bearing mice [723] as well as cancer patients [724]. It has been postulated that an indirect mechanism (e.g., induction of cytokines), rather than a direct interaction of FAA with NK cells [725], is responsible for the discovered effect. In mouse renal cancer, intravenous or intraperitoneal administration of FAA increased NK cell activity in the spleen, liver, lungs, and peritoneum and was synergistically enhanced by co-administration of IL-2 [725]. The first report on the enhancing effect of FAA on NK cell function in humans came from a study with six cancer patients undergoing a weekly treatment with FAA. Three out of the six patients showed a considerably enhanced NK cell activity after treatment [724]. In another trial, NK cell activity not only remained unchanged after treatment with FAA in cancer patients but even significantly reduced 24 h after treatment [726]. The synergistic activity of FAA and IL-2 [725] was subsequently studied in 26 melanoma patients. In 23 of 26 patients, NK activity was significantly enhanced (2–20-fold higher cytotoxicity) during combined treatment with FAA and IL-2. However, large variations in NK cell activity were observed in patients over the duration of the trial [727]. Of nine cancer patients receiving 1–6 courses of FAA infusions, enhanced NK cell activity was reported in only three patients, while six others were unresponsive to treatment [728].
However, intravenous FAA in the abovementioned trials differed completely from the oral intake of flavonoids through diet or supplements. After intravenous injection, compounds are 100% bioavailable, which surpass the usual maximum plasma concentrations of dietary flavonoids. A possible mechanism of action by which FAA induces NK cell activity is through induction of cytokines, including IFN-α, thereby improving NK cell function.
Phenoxodiol (a Synthetic Flavonoid)
Phenoxodiol is a synthetic analog of genistein [729]. Phenoxodiol could induce NK cell function and their perforin content in human PBMCs from healthy donors, thereby increasing cytotoxicity of NK-sensitive K562 cells. The increased cytotoxicity of phenoxodiol-treated cells was more prominent in PBMCs from cancer patients than in those from healthy volunteers. On the contrary, genistein and daidzein only marginally stimulated PBMC cytotoxicity [675]. In a previous experimental in vivo study, the effects of phenoxodiol genistein and daidzein were investigated in tumor-bearing mice. Only phenoxodiol and only at high-dose of 20 mg/kg body weight was able to enhance the cytolytic activity of splenocytes against NK-sensitive target cells (CT-26 and YAC-1) [675].
Polymethoxylated Flavones
Treatment with a mixture of polymethoxylated flavones derived from orange peel oil in high doses mildly downregulated NK cell activity with no effect on humoral immunity [730]. These findings suggest that consumption of high-dose citrus fruit during certain conditions like tamoxifen therapy of mammary tumors must be avoided. Polymethoxylated flavones, such as nobiletin, tangeretin, and sinensetin, from the peel of citrus fruits, have been reported to potentiate the cytotoxicity of KHYG-1 (NK leukemia cells that exhibit high cytolytic activity against K562 target cells [731]) by enhancing the expression of granzyme B [731]. Among them, nobiletin was also able to increase the levels of IFN-γ, perforin, granzyme A, and granzyme B in KHYG-1 cells [731]. The important role of granzyme B in nobiletin-mediated cytolysis has been confirmed in that study. It must be noted that nobiletin increased phosphorylation of cAMP response element-binding protein (CREB) while controlling the phosphorylation of ERK1/ERK2 and p38 MAPK [731].
Apigenin and Amentoflavone
Apigenin is found in common fruits and vegetables, such as parsley, onions, oranges, tea, chamomile, wheat sprouts, apple, guava, tomato, and broccoli, and in some seasonings. Studies have reported its antitumor effects. Topical application of apigenin prior to UV irradiation prevents UV-induced tumorigenesis in mice. In addition, it exhibited antiproliferative effects on breast cancer cell lines that expressed different levels of HER2/neu. It induced apoptosis in HER2/neu-overexpressing breast cancer cells. Apigenin has been shown to inhibit cancer cell proliferation and transcriptional activation of VEGF in A549 lung cancer cells [732,733,734,735,736,737]. Amentoflavone is a biflavonoid formed out of two apigenin units [738]. It is present in Ginkgo biloba, Saint John’s wort [739], and Nandina domestica [740]. Treatment with amentoflavone increased NK cell activity in splenocytes in control and tumor-bearing BALB/c mice [741]. Tumor-bearing controls showed weaker and delayed NK cell activity in comparison with amentoflavone-treated mice [741]. NK cell activity was investigated in splenocytes isolated from tumor-bearing mice incubated with K562 target cells. Furthermore, antibody-dependent cellular cytotoxicity (ADCC) was significantly improved in amentoflavone-treated mice [741]. Taken together, amentoflavone effectively increased lymphoid cell proliferation and effector cell functions by inducing the production of IL-2 and IFN-γ in tumor-bearing mice [741].
Proanthocyanidins
Proanthocyanidins derived from grape seeds have different strong immunomodulatory properties. Ultraviolet B (UVB), as a part of UV irradiation, causes immunosuppression which can be inhibited by proanthocyanidins through the induction of IL-12 in mice [742]. In addition, proanthocyanidins can inhibit UVB-induced immunosuppression by inducing CD8+ effector T-cells and reducing regulatory CD4+ T-cells. Proanthocyanidins make UVB-exposed mice to secrete higher levels (five- to eightfold) of TH1 cytokines from CD8+ T-cells and lower levels (80–100%) of TH2 cytokines from CD4+ T-cells [743]. Of note, proanthocyanidins increase the frequency of CD4+CD25+FoxP3+ regulatory T-cells while decreasing the frequency of CD4+IL-17+ pathogenic T-cells. Downregulation of IL-17 secretion and enhancement of Foxp3 expression because of proanthocyanidin treatment have been reported in vivo.
Organosulfur Compounds
Garlic is a rich source of organosulfur compounds (OSCs), including allicin, diallyl sulfide, and diallyl disulfide, which contain, respectively, mono-, di-, and polysulfide functional groups [744]. Garlic and its compounds are capable to facilitate stimulation of immune effector cells to promote antitumor immunity [745]. Aged garlic extract (AGE) has been reported to stimulate phagocytosis by macrophages and cytotoxic activities of T-lymphocytes [746] in sarcoma-180-bearing mice. In addition, it can increase the secretion of pro-inflammatory cytokines (IL-2, IL-12, TNF-α, and IFN-γ) and the frequency of NK cells. However, diallyl disulfide, diallyl sulfide, and allyl methyl sulfide exhibited an inhibitory effect on the release of TNF-α, IL-10, and NO generation in LPS-stimulated RAW 264.7 macrophages [747]. Some dietary phytochemicals like sulforaphane are powerful stimulators of phase II/detoxifying genes, and this effect is dependent on nuclear factor erythroid 2-related factor 2 (Nrf2) [748]. In fact, sulforaphane is able to stabilize Nrf2 [749].
Capsaicin
Capsaicin is the dominant pungent component present in red chili pepper [750, 751]. The antiproliferative effects of capsaicin through several mechanisms including production of ROS and disruption of mitochondrial membrane and release of cytochrome c have been reported in some cancer cell lines, such as leukemic cells (NB4 and Kasumi-1 cells) [752], prostate cancer cell line PC-3 [753], and human colon adenocarcinoma Colo205 cells [754]. The anti-angiogenic effects of capsaicin have been shown via its suppressive effects on VEGF. Capsaicin is able to inhibit NF-кB and STAT3 transcriptional pathway that play a vital role in inflammation and tumor growth [755, 756].
Bromelain
Bromelain is a mixture of proteolytic enzymes purified from pineapple (Ananas comosus). It has been approved as an anti-inflammatory agent for post-surgical conditions and infection. Immunomodulatory effects of bromelain include (1) induction of CD2-mediated T-cell activation [757], (2) increasing T-lymphocyte proliferation in splenocytes without significant effect on purified CD4+ and CD8+ T-cells [758], and (3) decreasing the production of pro-inflammatory cytokines, such as IL-2, IL-6, IL-4, IFN-γ, and G-CSF, from inflamed tissues [759]. The immunostimulatory effect of bromelain was only demonstrated on the healthy immune system when combating foreign antigens [760, 761]. Also, bromelain is able to stimulate the oxidative explosion in neutrophils by increasing intracellular ROS that induce DNA destruction, thereby enhancing the cytotoxic effect of neutrophils on tumor cells [762]. The antitumor and cytotoxic effect of bromelain has been shown in mouse skin papilloma through inhibition of NF-кB and COX-2 expression [763]. Its cytotoxic effect has been shown on melanoma B16F10-Nex2 cells [764] and human cholangiocarcinoma cell lines (TFK-1, SZ-1) as well [765]. Bromelain has the ability to decrease the expression of CD44 surface marker, which is involved in tumor proliferation [766]. Of note, bromelain treatment led to a significant reduction in invasion, migration, and adhesion of glioma cells without any adverse effect on marginal cells [767].
Betulinic Acid
Betulinic acid (Bet A) is a naturally occurring triterpenoid present in several plant species such as the white birch (Betula pubescens). Bet A has been investigated for its cytotoxic effects on melanoma cells [768], neuroblastoma tumor cells [769], glioma cells [770], human leukemia HL-60 cells [771], malignant head and neck squamous cell carcinoma SCC25 and SCC9 cell lines [772], and colon cancer cells [773]. Of note, Bet A is able to inhibit the secretion of IL-6, COX-2, and PGE-2 in LPS-induced PBMCs via downregulation of NF-кB signaling [774, 775].
Zerumbone
Zerumbone is a sesquiterpene in the rhizomes of shampoo ginger. Zerumbone has immunomodulatory activity via modulation of MAPK and NF-кB pathways [776] and cytokine secretion [777]. It has been demonstrated to downregulate production of different inflammatory mediators, mainly NO, COX-2, PGE-2, and iNOS in macrophages [778]. Moreover, this potent immunomodulator has been investigated for its anticancer effects and suggested to be helpful in cancers of the breast, bone marrow, liver, lung, cervix, colon, prostate, pancreas, and skin [778,779,780,781,782,783,784].
Noni Fruit
Morinda citrifolia (noni) is a Hawaiian plant used for cancer. Its polysaccharide-rich substance has been shown to possess antitumor effect in the Lewis lung tumor model, resulting in improvement of the host immune system through affecting the production of cytokines (TNF-α and IFN-γ) and nitric oxide. Two glycosides, 6-O-(β-d-glucopyranosyl)-1-O-octanosyl-β-d-glucopyranose and asperulosidic acid, were purified as active compounds from noni juice. Both compounds were efficient in downregulating TPA- or EGF-induced cell transformation and associated AP-1 activity [785].
Flavanols
Other flavanols like myricetin have been investigated in the context of antitumor immunology. Myricetin potentiated the ability of NK-92 cells to lyse K562 erythroleukemia target cells [786].
Naringenin
Naringenin is the major flavanone in grapefruit. It was reported to increase the expression of NKG2D ligands in human Raji (Burkitt’s lymphoma) cells [787]. MICA, MICB, ULBP1, and ULBP2 protein expressions were also increased compared with untreated control cells [787]. Although quercetin exhibited weaker but similar effect on NKG2D ligand expression, luteolin (flavone), kaempferol (flavonol), taxifolin (flavanonol), apigenin (flavone), and hesperetin (flavanone) did not show modulation of NKG2D ligand expression [787].
Chrysin
Chrysin is the main flavanone of Passiflora incarnata (also known as passion flower) [788]. It can be found in natural products like propolis and honey [789]. Chrysin has been reported to have anti-inflammatory, antioxidative, and chemopreventive activities [789]. Oral administration of chrysin in a murine leukemia mouse model increased populations of T- and B-lymphocytes and enhanced phagocytosis by macrophages as well as NK cell-mediated cytotoxicity. After chrysin treatment, the viability of WEHI-3 cells (murine leukemia cells) was reduced. Splenocytes isolated from WEHI-3-injected leukemic BALB/c mice after chrysin treatment exhibited an enhanced NK cell toxicity toward YAC-1 target cells [789].
Tangeretin
The flavone tangeretin is found in citrus fruit peel [790]. Tangeretin treatment in female C3H mice reduced lymphocyte counts, suggesting an inhibitory effect of tangeretin on cell proliferation and differentiation of NK cells [791]. Tangeretin also antagonized the tumor-suppressive effects of tamoxifen in MCF-7/MCF-6 tumor-bearing mice by reducing the number of NK cells and NK cell activation through lymphokines [790]. The in vivo antitumor effect of tangeretin has been shown in DMBA (7,12-dimethylbenz(a)anthracene)-induced breast cancer-bearing animals [792]. The antiproliferative and anti-angiogenic effects of tangeretin in A549 human lung cancer cell line have been attributed to downregulation of IL-1β-induced COX-2 expression. Moreover, it has the capability to enhance the levels of non-enzymatic antioxidants (ascorbic acid, vitamin E, and GSH) and reduce the serum levels of tumor markers [793, 794].
Silymarin
Silymarin has shown both antitumoral and cytoprotective effects. It has been reported that silymarin can inhibit NF-κB activation [795]. Another study has shown the biphasic effect of silymarin on Jurkat cells, a human peripheral blood leukemia T-cell line [796]. Low dose of silymarin increased cell proliferation, while high doses caused inhibition of DNA synthesis and significant cell death [797].
Alkaloids
Caffeine is a major phytochemical, which belongs to the alkaloid class. Using the B16F-10 melanoma cell-induced experimental metastasis model, oral and intraperitoneal caffeine administration significantly decreased tumor size [798]. Investigation using a spontaneous transgene-induced mammary tumor model provided further evidence of inhibition of metastasis by caffeine [799].
6-Gingerol
6-Gingerol is the pungent phenolic compound derived from ginger (Zingiber officinale). 6-Gingerol demonstrated antiproliferative effect by stimulation of apoptosis against several tumor cell lines such as OSCC and cervical HeLa [800]. Moreover, 6-gingerol showed an anti-metastasis effect on lung B16F10 melanoma in vivo. Inhibition of angiogenesis occurred through downregulation of VEGF. Also, it exhibited its inhibitory effect on COX-2 expression by downregulation of p38 MAPK and NF-кB in vivo [801].
Kaempferitrin
The antitumor and immunostimulatory effects of bioactive flavonoid kaempferitrin from Justicia spicigera have been reported in human cervical carcinoma cells (HeLa) [802]. More precisely, kaempferitrin is able to stimulate antitumor immune responses by inducing phagocytic activity of human macrophage in vitro, enhancing the levels of NO and generation of H2O2, and stimulating NK activity.
References
Reddy BS, Rao CV. Chemoprophylaxis of colon cancer. Curr Gastroenterol Rep. 2005;7(5):389–95.
Paterson J, Baxter G, Lawrence J, Duthie G. Is there a role for dietary salicylates in health? Proc Nutr Soc. 2006;65(1):93–6.
Newsholme P. Why is L-glutamine metabolism important to cells of the immune system in health, postinjury, surgery or infection? J Nutr. 2001;131(9):2515S–22S.
Grimble RF. The effects of sulfur amino acid intake on immune function in humans. J Nutr. 2006;136(6):1660S–5S.
Opitz CA, Litzenburger UM, Sahm F, Ott M, Tritschler I, Trump S, et al. An endogenous tumour-promoting ligand of the human aryl hydrocarbon receptor. Nature. 2011;478(7368):197.
Kiss EA, Vonarbourg C, Kopfmann S, Hobeika E, Finke D, Esser C, et al. Natural aryl hydrocarbon receptor ligands control organogenesis of intestinal lymphoid follicles. Science. 2011;334(6062):1561–5.
Calder P, Grimble R. Polyunsaturated fatty acids, inflammation and immunity. Eur J Clin Nutr. 2002;56(S3):S14.
Babcock TA, Helton WS, Hong D, Espat NJ. Omega-3 fatty acid lipid emulsion reduces LPS-stimulated macrophage TNF-α production. Surg Infect. 2002;3(2):145–9.
Fan Y-Y, Ly LH, Barhoumi R, McMurray DN, Chapkin RS. Dietary docosahexaenoic acid suppresses T cell protein kinase Cθ lipid raft recruitment and IL-2 production. J Immunol. 2004;173(10):6151–60.
Calder PC. Polyunsaturated fatty acids, inflammation, and immunity. Lipids. 2001;36(9):1007–24.
Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly-y M, et al. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science. 2013;341(6145):569–73.
Philpott M, Ferguson LR. Immunonutrition and cancer. Mutat Res/Fundam Mol Mech Mutagen. 2004;551(1):29–42.
Kocdor H, Ates H, Aydin S, Cehreli R, Soyarat F, Kemanli P, et al. Zinc supplementation induces apoptosis and enhances antitumor efficacy of docetaxel in non-small-cell lung cancer. Drug Des Devel Ther. 2015;9:3899.
Rosenkranz E, Prasad A, Rink L. Immunobiology and hematology of zinc. In: Rink L, editor. Zinc in human health. Amsterdam: IOS Press; 2011. p. 195–233.
Taylor PR, Greenwald P. Nutritional interventions in cancer prevention. J Clin Oncol. 2005;23(2):333–45.
Arthur JR, McKenzie RC, Beckett GJ. Selenium in the immune system. J Nutr. 2003;133(5):1457S–9S.
Padayatty SJ, Katz A, Wang Y, Eck P, Kwon O, Lee J-H, et al. Vitamin C as an antioxidant: evaluation of its role in disease prevention. J Am Coll Nutr. 2003;22(1):18–35.
Yanaka N, Koyama T-A, Komatsu S-I, Nakamura E, Kanda M, Kato N. Vitamin B6 suppresses NF-κB activation in LPS-stimulated mouse macrophages. Int J Mol Med. 2005;16(6):1071–5.
Go EK, Jung KJ, Kim JY, Yu BP, Chung HY. Betaine suppresses proinflammatory signaling during aging: the involvement of nuclear factor-κB via nuclear factor-inducing kinase/IκB kinase and mitogen-activated protein kinases. J Gerontol Ser A Biol Med Sci. 2005;60(10):1252–64.
Pandolfi F, Franza L, Mandolini C, Conti P. Immune modulation by vitamin D: special emphasis on its role in prevention and treatment of cancer. Clin Ther. 2017;39(5):884–93.
Duffy MJ, Murray A, Synnott NC, O’Donovan N, Crown J. Vitamin D analogues: potential use in cancer treatment. Crit Rev Oncol Hematol. 2017;112:190–7.
Ng K, Venook AP, Sato K, Yuan C, Hollis BW, Niedzwiecki D, et al. Vitamin D status and survival of metastatic colorectal cancer patients: results from CALGB/SWOG 80405 (Alliance). J Clin Oncol. 2015;33(15_suppl):3503.
Oh B, Figtree G, Costa D, Eade T, Hruby G, Lim S, et al. Oxidative stress in prostate cancer patients: a systematic review of case control studies. Prostate Int. 2016;4(3):71–87.
Wu D, Nikbin MS. Age-associated changes in immune function: impact of vitamin E intervention and the underlying mechanisms. Endocr, Metab Immune Disord Drug Targets (Formerly Current Drug Targets-Immune, Endocrine & Metabolic Disorders). 2014;14(4):283–9.
Galli F, Azzi A, Birringer M, Cook-Mills JM, Eggersdorfer M, Frank J, et al. Vitamin E: emerging aspects and new directions. Free Radic Biol Med. 2017;102:16–36.
Hemilä H. Vitamin C and infections. Nutrients. 2017;9(4):339.
Percival SS, Bukowski JF, Milner J. Bioactive food components that enhance gammadelta T cell function may play a role in cancer prevention. J Nutr. 2008;138(1):1–4.
García-Closas R, García-Closas M, Kogevinas M, Malats N, Silverman D, Serra C, et al. Food, nutrient and heterocyclic amine intake and the risk of bladder cancer. Eur J Cancer. 2007;43(11):1731–40.
Sacerdote C, Matullo G, Polidoro S, Gamberini S, Piazza A, Karagas MR, et al. Intake of fruits and vegetables and polymorphisms in DNA repair genes in bladder cancer. Mutagenesis. 2007;22(4):281–5.
Lunet N, Valbuena C, Vieira AL, Lopes C, Lopes C, David L, et al. Fruit and vegetable consumption and gastric cancer by location and histological type: case–control and meta-analysis. Eur J Cancer Prev. 2007;16(4):312–27.
Pavia M, Pileggi C, Nobile CG, Angelillo IF. Association between fruit and vegetable consumption and oral cancer: a meta-analysis of observational studies. Am J Clin Nutr. 2006;83(5):1126–34.
Kirsh VA, Peters U, Mayne ST, Subar AF, Chatterjee N, Johnson CC, et al. Prospective study of fruit and vegetable intake and risk of prostate cancer. J Natl Cancer Inst. 2007;99(15):1200–9.
Ambrosini GL, de Klerk NH, Fritschi L, Mackerras D, Musk B. Fruit, vegetable, vitamin A intakes, and prostate cancer risk. Prostate Cancer Prostatic Dis. 2008;11(1):61.
McClain KL. Immunodeficiency states and related malignancies. Cancer Treat Res. 1997;92:39–61.
Tanaka Y, Morita CT, Tanaka Y, Nieves E, Brenner MB, Bloom BR. Natural and synthetic non-peptide antigens recognized by human gamma delta T cells. Nature. 1995;375(6527):155–8.
Zhao Y, Niu C, Cui J. Gamma-delta (gammadelta) T cells: friend or foe in cancer development? J Transl Med. 2018;16(1):3.
Knies D, Klobuch S, Xue SA, Birtel M, Echchannaoui H, Yildiz O, et al. An optimized single chain TCR scaffold relying on the assembly with the native CD3-complex prevents residual mispairing with endogenous TCRs in human T-cells. Oncotarget. 2016;7(16):21199–221.
Blaeschke F, Thiel U, Kirschner A, Thiede M, Rubio RA, Schirmer D, et al. Human HLA-A∗02:01/CHM1+ allo-restricted T cell receptor transgenic CD8+ T cells specifically inhibit Ewing sarcoma growth in vitro and in vivo. Oncotarget. 2016;7(28):43267–80.
Hedges JF, Lubick KJ, Jutila MA. Gamma delta T cells respond directly to pathogen-associated molecular patterns. J Immunol. 2005;174(10):6045–53.
Lubick K, Jutila MA. LTA recognition by bovine gammadelta T cells involves CD36. J Leukoc Biol. 2006;79(6):1268–70.
Chen Y, Chou K, Fuchs E, Havran WL, Boismenu R. Protection of the intestinal mucosa by intraepithelial gamma delta T cells. Proc Natl Acad Sci U S A. 2002;99(22):14338–43.
Sharp LL, Jameson JM, Cauvi G, Havran WL. Dendritic epidermal T cells regulate skin homeostasis through local production of insulin-like growth factor 1. Nat Immunol. 2005;6(1):73–9.
Rincon-Orozco B, Kunzmann V, Wrobel P, Kabelitz D, Steinle A, Herrmann T. Activation of V gamma 9V delta 2 T cells by NKG2D. J Immunol. 2005;175(4):2144–51.
Hayday A, Tigelaar R. Immunoregulation in the tissues by gammadelta T cells. Nat Rev Immunol. 2003;3(3):233–42.
Ferrarini M, Ferrero E, Dagna L, Poggi A, Zocchi MR. Human gammadelta T cells: a nonredundant system in the immune-surveillance against cancer. Trends Immunol. 2002;23(1):14–8.
Kabelitz D, Glatzel A, Wesch D. Antigen recognition by human gammadelta T lymphocytes. Int Arch Allergy Immunol. 2000;122(1):1–7.
Kato Y, Tanaka Y, Hayashi M, Okawa K, Minato N. Involvement of CD166 in the activation of human gamma delta T cells by tumor cells sensitized with nonpeptide antigens. J Immunol. 2006;177(2):877–84.
Das H, Wang L, Kamath A, Bukowski JF. Vgamma2Vdelta2 T-cell receptor-mediated recognition of aminobisphosphonates. Blood. 2001;98(5):1616–8.
Wang L, Kamath A, Das H, Li L, Bukowski JF. Antibacterial effect of human V gamma 2V delta 2 T cells in vivo. J Clin Invest. 2001;108(9):1349–57.
Kamath AB, Wang L, Das H, Li L, Reinhold VN, Bukowski JF. Antigens in tea-beverage prime human Vγ2Vδ2 T cells in vitro and in vivo for memory and nonmemory antibacterial cytokine responses. Proc Natl Acad Sci. 2003;100(10):6009–14.
Hirsh MI, Junger WG. Roles of heat shock proteins and γδT cells in inflammation. Am J Respir Cell Mol Biol. 2008;39(5):509–13.
Gober H-J, Kistowska M, Angman L, Jenö P, Mori L, De Libero G. Human T cell receptor γδ cells recognize endogenous mevalonate metabolites in tumor cells. J Exp Med. 2003;197(2):163–8.
Duncan RE, El-Sohemy A, Archer MC. Dietary factors and the regulation of 3-hydroxy-3-methylglutaryl coenzyme A reductase: implications for breast cancer and development. Mol Nutr Food Res. 2005;49(2):93–100.
Hayday AC. [gamma][delta] cells: a right time and a right place for a conserved third way of protection. Annu Rev Immunol. 2000;18:975–1026.
Ebert LM, Meuter S, Moser B. Homing and function of human skin gammadelta T cells and NK cells: relevance for tumor surveillance. J Immunol. 2006;176(7):4331–6.
Inagaki-Ohara K, Chinen T, Matsuzaki G, Sasaki A, Sakamoto Y, Hiromatsu K, et al. Mucosal T cells bearing TCRgammadelta play a protective role in intestinal inflammation. J Immunol. 2004;173(2):1390–8.
Jameson J, Havran WL. Skin gammadelta T-cell functions in homeostasis and wound healing. Immunol Rev. 2007;215:114–22.
Komori HK, Meehan TF, Havran WL. Epithelial and mucosal gamma delta T cells. Curr Opin Immunol. 2006;18(5):534–8.
Brandes M, Willimann K, Moser B. Professional antigen-presentation function by human gammadelta T cells. Science. 2005;309(5732):264–8.
Vantourout P, Hayday A. Six-of-the-best: unique contributions of gammadelta T cells to immunology. Nat Rev Immunol. 2013;13(2):88–100.
Wu YL, Ding YP, Tanaka Y, Shen LW, Wei CH, Minato N, et al. gammadelta T cells and their potential for immunotherapy. Int J Biol Sci. 2014;10(2):119–35.
Bonneville M, Chen ZW, Dechanet-Merville J, Eberl M, Fournie JJ, Jameson JM, et al. Chicago 2014--30 years of gammadelta T cells. Cell Immunol. 2015;296(1):3–9.
Todaro M, Meraviglia S, Caccamo N, Stassi G, Dieli F. Combining conventional chemotherapy and gammadelta T cell-based immunotherapy to target cancer-initiating cells. Oncoimmunology. 2013;2(9):e25821.
Beetz S, Wesch D, Marischen L, Welte S, Oberg HH, Kabelitz D. Innate immune functions of human gammadelta T cells. Immunobiology. 2008;213(3–4):173–82.
Bouet-Toussaint F, Cabillic F, Toutirais O, Le Gallo M, Thomas de la Pintiere C, Daniel P, et al. Vgamma9Vdelta2 T cell-mediated recognition of human solid tumors. Potential for immunotherapy of hepatocellular and colorectal carcinomas. Cancer Immunol Immunother: CII. 2008;57(4):531–9.
Zheng BJ, Ng SP, Chua DT, Sham JS, Kwong DL, Lam CK, et al. Peripheral gamma delta T-cell deficit in nasopharyngeal carcinoma. Int J Cancer. 2002;99(2):213–7.
Sakamoto M, Nakajima J, Murakawa T, Fukami T, Yoshida Y, Murayama T, et al. Adoptive immunotherapy for advanced non-small cell lung cancer using zoledronate-expanded gammadeltaTcells: a phase I clinical study. J Immunother (Hagerstown, Md: 1997). 2011;34(2):202–11.
Cordova A, Toia F, La Mendola C, Orlando V, Meraviglia S, Rinaldi G, et al. Characterization of human gammadelta T lymphocytes infiltrating primary malignant melanomas. PLoS One. 2012;7(11):e49878.
Zgani I, Menut C, Seman M, Gallois V, Laffont V, Liautard J, et al. Synthesis of prenyl pyrophosphonates as new potent phosphoantigens inducing selective activation of human Vgamma9Vdelta2 T lymphocytes. J Med Chem. 2004;47(18):4600–12.
Egan PJ, Carding SR. Downmodulation of the inflammatory response to bacterial infection by γδ T cells cytotoxic for activated macrophages. J Exp Med. 2000;191(12):2145–58.
Carding SR, Egan PJ. The importance of gd T cells in the resolution of pathogen-induced inflammatory immune responses. Immunol Rev. 2000;173(1):98–108.
Gombart AF, Luong QT, Koeffler HP. Vitamin D compounds: activity against microbes and cancer. Anticancer Res. 2006;26(4A):2531–42.
Beetz S, Marischen L, Kabelitz D, Wesch D. Human gamma delta T cells: candidates for the development of immunotherapeutic strategies. Immunol Res. 2007;37(2):97–111.
Bukowski JF, Morita CT, Brenner MB. Human γδ T cells recognize alkylamines derived from microbes, edible plants, and tea: implications for innate immunity. Immunity. 1999;11(1):57–65.
Mitchell S, Zhang A, Smith R. Ethylamine in human urine. Clin Chim Acta. 2000;302(1–2):69–78.
Unno T, Suzuki Y, Kakuda T, Hayakawa T, Tsuge H. Metabolism of theanine, γ-glutamylethylamide, in rats. J Agric Food Chem. 1999;47(4):1593–6.
Morita CT, Jin C, Sarikonda G, Wang H. Nonpeptide antigens, presentation mechanisms, and immunological memory of human Vgamma2Vdelta2 T cells: discriminating friend from foe through the recognition of prenyl pyrophosphate antigens. Immunol Rev. 2007;215:59–76.
Holderness J, Jackiw L, Kimmel E, Kerns H, Radke M, Hedges JF, et al. Select plant tannins induce IL-2Ralpha up-regulation and augment cell division in gammadelta T cells. J Immunol. 2007;179(10):6468–78.
Jutila MA, Holderness J, Graff JC, Hedges JF. Antigen-independent priming: a transitional response of bovine γδ T-cells to infection. Anim Health Res Rev. 2008;9(1):47–57.
Percival SS. Nutrition and immunity: balancing diet and immune function. Nutr Today. 2011;46(1):12–7.
Nantz MP, Rowe CA, Nieves C, Percival SS. Immunity and antioxidant capacity in humans is enhanced by consumption of a dried, encapsulated fruit and vegetable juice concentrate. J Nutr. 2006;136(10):2606–10.
Nantz MP, Rowe CA, Bukowski JF, Percival SS. Standardized capsule of Camellia sinensis lowers cardiovascular risk factors in a randomized, double-blind, placebo-controlled study. Nutrition. 2009;25(2):147–54.
Rowe CA, Nantz MP, Bukowski JF, Percival SS. Specific formulation of Camellia sinensis prevents cold and flu symptoms and enhances γδ T cell function: a randomized, double-blind, placebo-controlled study. J Am Coll Nutr. 2007;26(5):445–52.
Heinzerling L, von Baehr V, Liebenthal C, von Baehr R, Volk HD. Immunologic effector mechanisms of a standardized mistletoe extract on the function of human monocytes and lymphocytes in vitro, ex vivo, and in vivo. J Clin Immunol. 2006;26(4):347–59.
Lopez RD, Xu S, Guo B, Negrin RS, Waller EK. CD2-mediated IL-12-dependent signals render human gamma delta-T cells resistant to mitogen-induced apoptosis, permitting the large-scale ex vivo expansion of functionally distinct lymphocytes: implications for the development of adoptive immunotherapy strategies. Blood. 2000;96(12):3827–37.
Fischer S, Scheffler A, Kabelitz D. Activation of human gamma delta T-cells by heat-treated mistletoe plant extracts. Immunol Lett. 1996;52(2–3):69–72.
Akiyama H, Sato Y, Watanabe T, Nagaoka MH, Yoshioka Y, Shoji T, et al. Dietary unripe apple polyphenol inhibits the development of food allergies in murine models. FEBS Lett. 2005;579(20):4485–91.
Graff JC, Jutila MA. Differential regulation of CD11b on γδ T cells and monocytes in response to unripe apple polyphenols. J Leukoc Biol. 2007;82(3):603–7.
Nagafuchi S, Totsuka M, Hachimura S, Goto M, Takahashi T, Yajima T, et al. Dietary nucleotides increase the proportion of a TCR gammadelta+ subset of intraepithelial lymphocytes (IEL) and IL-7 production by intestinal epithelial cells (IEC); implications for modification of cellular and molecular cross-talk between IEL and IEC by dietary nucleotides. Biosci Biotechnol Biochem. 2000;64(7):1459–65.
Berger A, German JB, Chiang BL, Ansari AA, Keen CL, Fletcher MP, et al. Influence of feeding unsaturated fats on growth and immune status of mice. J Nutr. 1993;123(2):225–33.
Bassaganya-Riera J, Hontecillas R, Zimmerman DR, Wannemuehler MJ. Dietary conjugated linoleic acid modulates phenotype and effector functions of porcine CD8(+) lymphocytes. J Nutr. 2001;131(9):2370–7.
Bukowski JF, Morita CT, Brenner MB. Human gamma delta T cells recognize alkylamines derived from microbes, edible plants, and tea: implications for innate immunity. Immunity. 1999;11(1):57–65.
Atawodi SE, Mende P, Pfundstein B, Preussmann R, Spiegelhalder B. Nitrosatable amines and nitrosamide formation in natural stimulants: Cola acuminata, C. nitida and Garcinia cola. Food Chem Toxicol: Int J Publi Br Indust Biol Res Assoc. 1995;33(8):625–30.
Rowe CA, Nantz MP, Nieves C Jr, West RL, Percival SS. Regular consumption of concord grape juice benefits human immunity. J Med Food. 2011;14(1–2):69–78.
Dai X, Stanilka JM, Rowe CA, Esteves EA, Nieves C Jr, Spaiser SJ, et al. Consuming Lentinula edodes (Shiitake) mushrooms daily improves human immunity: a randomized dietary intervention in healthy young adults. J Am Coll Nutr. 2015;34(6):478–87.
Nantz MP, Rowe CA, Muller CE, Creasy RA, Stanilka JM, Percival SS. Supplementation with aged garlic extract improves both NK and γδ-T cell function and reduces the severity of cold and flu symptoms: a randomized, double-blind, placebo-controlled nutrition intervention. Clin Nutr. 2012;31(3):337–44.
Ishikawa H, Saeki T, Otani T, Suzuki T, Shimozuma K, Nishino H, et al. Aged garlic extract prevents a decline of NK cell number and activity in patients with advanced cancer. J Nutr. 2006;136(3):816S–20S.
Nantz MP, Rowe CA, Muller C, Creasy R, Colee J, Khoo C, et al. Consumption of cranberry polyphenols enhances human γδ-T cell proliferation and reduces the number of symptoms associated with colds and influenza: a randomized, placebo-controlled intervention study. Nutr J. 2013;12(1):161.
Holderness J, Hedges JF, Daughenbaugh K, Kimmel E, Graff J, Freedman B, et al. Response of γδ T cells to plant-derived tannins. Crit Rev Immunol. 2008;28(5):377–402.
Holderness J, Jackiw L, Kimmel E, Kerns H, Radke M, Hedges JF, et al. Select plant tannins induce IL-2Rα up-regulation and augment cell division in γδ T cells. J Immunol. 2007;179(10):6468–78.
Ramiro-Puig E, Pérez-Cano FJ, Ramos-Romero S, Pérez-Berezo T, Castellote C, Permanyer J, et al. Intestinal immune system of young rats influenced by cocoa-enriched diet. J Nutr Biochem. 2008;19(8):555–65.
Percival SS, Bukowski JF, Milner J. Bioactive food components that enhance γδ T cell function may play a role in cancer prevention. J Nutr. 2008;138(1):1–4.
Lee Y-C, Kim S-H, Roh S-S, Choi H-Y, Seo Y-B. Suppressive effects of Chelidonium majus methanol extract in knee joint, regional lymph nodes, and spleen on collagen-induced arthritis in mice. J Ethnopharmacol. 2007;112(1):40–8.
Hu Y-M, Yeh C-L, Pai M-H, Lee W-Y, Yeh S-L. Glutamine administration modulates lung γδ T lymphocyte expression in mice with polymicrobial sepsis. Shock. 2014;41(2):115–22.
Pai M-H, Liu J-J, Yeh S-L, Chen W-J, Yeh C-L. Glutamine modulates acute dextran sulphate sodium-induced changes in small-intestinal intraepithelial γδ-T-lymphocyte expression in mice. Br J Nutr. 2014;111(6):1032–9.
Brandes M, Willimann K, Lang AB, Nam K-H, Jin C, Brenner MB, et al. Flexible migration program regulates γδ T-cell involvement in humoral immunity. Blood. 2003;102(10):3693–701.
Kawaguchi-Miyashita M, Shimada S, Kurosu H, Kato-Nagaoka N, Matsuoka Y, Ohwaki M, et al. An accessory role of TCRgammadelta (+) cells in the exacerbation of inflammatory bowel disease in TCRalpha mutant mice. Eur J Immunol. 2001;31(4):980–8.
Falk MC, Ng G, Zhang GY, Fanning GC, Kamath KR, Knight JF. Predominance of T cell receptor V delta 3 in small bowel biopsies from coeliac disease patients. Clin Exp Immunol. 1994;98(1):78–82.
Rusconi M, Conti A. Theobroma cacao L., the food of the gods: a scientific approach beyond myths and claims. Pharmacol Res. 2010;61(1):5–13.
Hurst WJ, Tarka SM Jr, Powis TG, Valdez F Jr, Hester TR. Archaeology: cacao usage by the earliest Maya civilization. Nature. 2002;418(6895):289.
Vinson JA, Proch J, Zubik L. Phenol antioxidant quantity and quality in foods: cocoa, dark chocolate, and milk chocolate. J Agric Food Chem. 1999;47(12):4821–4.
Tomas-Barberán FA, Cienfuegos-Jovellanos E, Marín A, Muguerza B, Gil-Izquierdo A, Cerdá B, et al. A new process to develop a cocoa powder with higher flavonoid monomer content and enhanced bioavailability in healthy humans. J Agric Food Chem. 2007;55(10):3926–35.
Sánchez-Rabaneda F, Jáuregui O, Casals I, Andrés-Lacueva C, Izquierdo-Pulido M, Lamuela-Raventós RM. Liquid chromatographic/electrospray ionization tandem mass spectrometric study of the phenolic composition of cocoa (Theobroma cacao). J Mass Spectrom. 2003;38(1):35–42.
Pan MH, Lai CS, Wu JC, Ho CT. Molecular mechanisms for chemoprevention of colorectal cancer by natural dietary compounds. Mol Nutr Food Res. 2011;55(1):32–45.
Ramos S. Cancer chemoprevention and chemotherapy: dietary polyphenols and signalling pathways. Mol Nutr Food Res. 2008;52(5):507–26.
Natsume M, Osakabe N, Yamagishi M, Takizawa T, Nakamura T, Miyatake H, et al. Analyses of polyphenols in cacao liquor, cocoa, and chocolate by normal-phase and reversed-phase HPLC. Biosci Biotechnol Biochem. 2000;64(12):2581–7.
Hammerstone JF, Lazarus SA, Schmitz HH. Procyanidin content and variation in some commonly consumed foods. J Nutr. 2000;130(8):2086S–92S.
Gu L, House SE, Wu X, Ou B, Prior RL. Procyanidin and catechin contents and antioxidant capacity of cocoa and chocolate products. J Agric Food Chem. 2006;54(11):4057–61.
Prior RL, Gu L. Occurrence and biological significance of proanthocyanidins in the American diet. Phytochemistry. 2005;66(18):2264–80.
Manach C, Williamson G, Morand C, Scalbert A, Rémésy C. Bioavailability and bioefficacy of polyphenols in humans. I. Review of 97 bioavailability studies. Am J Clin Nutr. 2005;81(1):230S–42S.
Urpi-Sarda M, Monagas M, Khan N, Lamuela-Raventos RM, Santos-Buelga C, Sacanella E, et al. Epicatechin, procyanidins, and phenolic microbial metabolites after cocoa intake in humans and rats. Anal Bioanal Chem. 2009;394(6):1545–56.
Middleton E, Kandaswami C, Theoharides TC. The effects of plant flavonoids on mammalian cells: implications for inflammation, heart disease, and cancer. Pharmacol Rev. 2000;52(4):673–751.
Steinberg FM, Bearden MM, Keen CL. Cocoa and chocolate flavonoids: implications for cardiovascular health. J Am Diet Assoc. 2003;103(2):215–23.
Weisburger JH. Chemopreventive effects of cocoa polyphenols on chronic diseases. Exp Biol Med (Maywood). 2001;226(10):891–7.
Andújar IRM, Giner RM, Ríos JL. Cocoa polyphenols and their potential benefits for human health. Oxidative Med Cell Longev. 2012;2012:906252.
Coussens LM, Werb Z. Inflammation and cancer. Nature. 2002;420(6917):860.
Tsilidis KK, Branchini C, Guallar E, Helzlsouer KJ, Erlinger TP, Platz EA. C-reactive protein and colorectal cancer risk: a systematic review of prospective studies. Int J Cancer. 2008;123(5):1133–40.
Il’yasova D, Colbert LH, Harris TB, Newman AB, Bauer DC, Satterfield S, et al. Circulating levels of inflammatory markers and cancer risk in the health aging and body composition cohort. Cancer Epidemiol Prevent Biomark. 2005;14(10):2413–8.
Milner JA. Diet and cancer: facts and controversies. Nutr Cancer. 2006;56(2):216–24.
Arts IC, Hollman PC. Polyphenols and disease risk in epidemiologic studies. Am J Clin Nutr. 2005;81(1):317S–25S.
Bayard V, Chamorro F, Motta J, Hollenberg NK. Does flavanol intake influence mortality from nitric oxide-dependent processes? Ischemic heart disease, stroke, diabetes mellitus, and cancer in Panama. Int J Med Sci. 2007;4(1):53.
Garcia-Closas R, Gonzalez CA, Agudo A, Riboli E. Intake of specific carotenoids and flavonoids and the risk of gastric cancer in Spain. Cancer Causes Control. 1999;10(1):71–5.
Arts IC, Jacobs DR, Gross M, Harnack LJ, Folsom AR. Dietary catechins and cancer incidence among postmenopausal women: the Iowa Womens Health Study (United States). Cancer Causes Control. 2002;13(4):373–82.
Frankenfeld CL, Cerhan JR, Cozen W, Davis S, Schenk M, Morton LM, et al. Dietary flavonoid intake and non-Hodgkin lymphoma risk. Am J Clin Nutr. 2008;87(5):1439–45.
Arts IC. A review of the epidemiological evidence on tea, flavonoids, and lung cancer. J Nutr. 2008;138(8):1561S–6S.
Rouillier P, Senesse P, Cottet V, Valléau A, Faivre J, Boutron-Ruault M-C. Dietary patterns and the adenomacarcinoma sequence of colorectal cancer. Eur J Nutr. 2005;44(5):311–8.
Rossi M, Bosetti C, Negri E, Lagiou P, Vecchia CL. Flavonoids, proanthocyanidins, and cancer risk: a network of case-control studies from Italy. Nutr Cancer. 2010;62(7):871–7.
Arts IC, Hollman PC, Bueno de Mesquita HB, Feskens EJ, Kromhout D. Dietary catechins and epithelial cancer incidence: the Zutphen elderly study. Int J Cancer. 2001;92(2):298–302.
Lee I-M, Paffenbarger RS Jr. Life is sweet: candy consumption and longevity. BMJ. 1998;317(7174):1683–4.
Paganini-Hill A, Kawas CH, Corrada MM. Non-alcoholic beverage and caffeine consumption and mortality: the Leisure World Cohort Study. Prev Med. 2007;44(4):305–10.
Thompson CA, Habermann TM, Wang AH, Vierkant RA, Folsom AR, Ross JA, et al. Antioxidant intake from fruits, vegetables and other sources and risk of non-Hodgkin’s lymphoma: the Iowa Women’'s Health Study. Int J Cancer. 2010;126(4):992–1003.
Mathur S, Devaraj S, Grundy SM, Jialal I. Cocoa products decrease low density lipoprotein oxidative susceptibility but do not affect biomarkers of inflammation in humans. J Nutr. 2002;132(12):3663–7.
Rein D, Lotito S, Holt RR, Keen CL, Schmitz HH, Fraga CG. Epicatechin in human plasma: in vivo determination and effect of chocolate consumption on plasma oxidation status. J Nutr. 2000;130(8):2109S–14S.
Murphy KJ, Chronopoulos AK, Singh I, Francis MA, Moriarty H, Pike MJ, et al. Dietary flavanols and procyanidin oligomers from cocoa (Theobroma cacao) inhibit platelet function. Am J Clin Nutr. 2003;77(6):1466–73.
Engler MB, Engler MM, Chen CY, Malloy MJ, Browne A, Chiu EY, et al. Flavonoid-rich dark chocolate improves endothelial function and increases plasma epicatechin concentrations in healthy adults. J Am Coll Nutr. 2004;23(3):197–204.
Monagas M, Khan N, Andres-Lacueva C, Casas R, Urpí-Sardà M, Llorach R, et al. Effect of cocoa powder on the modulation of inflammatory biomarkers in patients at high risk of cardiovascular disease. Am J Clin Nutr. 2009;90(5):1144–50.
Vázquez-Agell M, Urpi-Sarda M, Sacanella E, Camino-López S, Chiva-Blanch G, Llorente-Cortés V, et al. Cocoa consumption reduces NF-κB activation in peripheral blood mononuclear cells in humans. Nutr Metab Cardiovasc Dis. 2013;23(3):257–63.
Ramos S. Effects of dietary flavonoids on apoptotic pathways related to cancer chemoprevention. J Nutr Biochem. 2007;18(7):427–42.
Ramiro-Puig E, Castell M. Cocoa: antioxidant and immunomodulator. Br J Nutr. 2009;101(7):931–40.
Belščak A, Komes D, Horžić D, Ganić KK, Karlović D. Comparative study of commercially available cocoa products in terms of their bioactive composition. Food Res Int. 2009;42(5–6):707–16.
Miller KB, Stuart DA, Smith NL, Lee CY, McHale NL, Flanagan JA, et al. Antioxidant activity and polyphenol and procyanidin contents of selected commercially available cocoa-containing and chocolate products in the United States. J Agric Food Chem. 2006;54(11):4062–8.
Noé V, Peñuelas S, Lamuela-Raventós RM, Permanyer J, Izquierdo-Pulido M. Epicatechin and a cocoa polyphenolic extract modulate gene expression in human Caco-2 cells. J Nutr. 2004;134(10):2509–16.
Oleaga C, García M, Solé A, Ciudad CJ, Izquierdo-Pulido M, Noé V. CYP1A1 is overexpressed upon incubation of breast cancer cells with a polyphenolic cocoa extract. Eur J Nutr. 2012;51:465–76.
Lee KW, Kundu JK, Kim SO, Chun K-S, Lee HJ, Surh Y-J. Cocoa polyphenols inhibit phorbol ester-induced superoxide anion formation in cultured HL-60 cells and expression of cyclooxygenase-2 and activation of NF-κB and MAPKs in mouse skin in vivo. J Nutr. 2006;136(5):1150–5.
Weyant MJ, Carothers AM, Dannenberg AJ, Bertagnolli MM. (+)-Catechin inhibits intestinal tumor formation and suppresses focal adhesion kinase activation in the min/+ mouse. Cancer Res. 2001;61(1):118–25.
Gu Q, Hu C, Chen Q, Xia Y, Feng J, Yang H. Development of a rat model by 3, 4-benzopyrene intra-pulmonary injection and evaluation of the effect of green tea drinking on p53 and bcl-2 expression in lung carcinoma. Cancer Detect Prev. 2009;32(5–6):444–51.
Preza AM, Jaramillo ME, Puebla AM, Mateos JC, Hernández R, Lugo E. Antitumor activity against murine lymphoma L5178Y model of proteins from cacao (Theobroma cacao L.) seeds in relation with in vitro antioxidant activity. BMC Complement Alternat Med. 2010;10(1):61.
Granado-Serrano AB, Martín MA, Haegeman G, Goya L, Bravo L, Ramos S. Epicatechin induces NF-κB, activator protein-1 (AP-1) and nuclear transcription factor erythroid 2p45-related factor-2 (Nrf2) via phosphatidylinositol-3-kinase/protein kinase B (PI3K/AKT) and extracellular regulated kinase (ERK) signalling in HepG2 cells. Br J Nutr. 2010;103(2):168–79.
Bahia PK, Rattray M, Williams RJ. Dietary flavonoid (−) epicatechin stimulates phosphatidylinositol 3-kinase-dependent anti-oxidant response element activity and up-regulates glutathione in cortical astrocytes. J Neurochem. 2008;106(5):2194–204.
Wang JF, Schramm DD, Holt RR, Ensunsa JL, Fraga CG, Schmitz HH, et al. A dose-response effect from chocolate consumption on plasma epicatechin and oxidative damage. J Nutr. 2000;130(8):2115S–9S.
Di Giuseppe R, Di Castelnuovo A, Centritto F, Zito F, De Curtis A, Costanzo S, et al. Regular consumption of dark chocolate is associated with low serum concentrations of C-reactive protein in a healthy Italian population. J Nutr. 2008;138(10):1939–45.
Crusz SM, Balkwill FR. Inflammation and cancer: advances and new agents. Nat Rev Clin Oncol. 2015;12(10):584.
Grivennikov SI, Karin M. Inflammatory cytokines in cancer: tumour necrosis factor and interleukin 6 take the stage. Ann Rheum Dis. 2011;70(Suppl 1):i104–8.
Grivennikov SI, Greten FR, Karin M. Immunity, inflammation, and cancer. Cell. 2010;140(6):883–99.
Munn LL. Cancer and inflammation. Wiley Interdiscip Rev Syst Biol Med. 2017;9(2) https://doi.org/10.1002/wsbm.1370.
Kashfi K. Anti-inflammatory agents as cancer therapeutics. Adv Pharmacol (San Diego, Calif). 2009;57:31–89.
Maeda S, Omata M. Inflammation and cancer: role of nuclear factor-kappaB activation. Cancer Sci. 2008;99(5):836–42.
Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15(11):e493–503.
Kim J-E, Son JE, Jung SK, Kang NJ, Lee CY, Lee KW, et al. Cocoa polyphenols suppress TNF-α-induced vascular endothelial growth factor expression by inhibiting phosphoinositide 3-kinase (PI3K) and mitogen-activated protein kinase kinase-1 (MEK1) activities in mouse epidermal cells. Br J Nutr. 2010;104(7):957–64.
Rodriguez-Ramiro I, Ramos S, Lopez-Oliva E, Agis-Torres A, Bravo L, Goya L, et al. Cocoa polyphenols prevent inflammation in the colon of azoxymethane-treated rats and in TNF-alpha-stimulated Caco-2 cells. Br J Nutr. 2013;110(2):206–15.
Bitzer ZT, Glisan SL, Dorenkott MR, Goodrich KM, Ye L, O’Keefe SF, et al. Cocoa procyanidins with different degrees of polymerization possess distinct activities in models of colonic inflammation. J Nutr Biochem. 2015;26(8):827–31.
Martín MA, Goya L, Ramos S. Preventive effects of cocoa and cocoa antioxidants in colon cancer. Diseases. 2016;4(1):6.
Hong MY, Nulton E, Shelechi M, Hernandez LM, Nemoseck T. Effects of dark chocolate on azoxymethane-induced colonic aberrant crypt foci. Nutr Cancer. 2013;65(5):677–85.
Marincola FM, Jaffee EM, Hicklin DJ, Ferrone S. Escape of human solid tumors from T–cell recognition: molecular mechanisms and functional significance. Adv Immunol Elsevier. 2000;74:181–273.
Liu Y, Zeng G. Cancer and innate immune system interactions: translational potentials for cancer immunotherapy. J Immunother (Hagerstown, Md: 1997). 2012;35(4):299.
Chen DS, Mellman I. Oncology meets immunology: the cancer-immunity cycle. Immunity. 2013;39(1):1–10.
Balkwill F. Tumour necrosis factor and cancer. Nat Rev Cancer. 2009;9(5):361.
Corrales L, Matson V, Flood B, Spranger S, Gajewski TF. Innate immune signaling and regulation in cancer immunotherapy. Cell Res. 2017;27(1):96.
Tanaka A, Sakaguchi S. Regulatory T cells in cancer immunotherapy. Cell Res. 2017;27(1):109.
Fridman WH, Pagès F, Sautès-Fridman C, Galon J. The immune contexture in human tumours: impact on clinical outcome. Nat Rev Cancer. 2012;12(4):nrc3245.
Farashi-Bonab S, Khansari N. Regulatory T cells in cancer patients and their roles in cancer development/progression. MOJ Immunol. 2014;1(4):00024.
Erdman SE, Poutahidis T. Cancer inflammation and regulatory T cells. Int J Cancer. 2010;127(4):768–79.
Sakaguchi S, Yamaguchi T, Nomura T, Ono M. Regulatory T cells and immune tolerance. Cell. 2008;133(5):775–87.
De Rosa V, Di Rella F, Di Giacomo A, Matarese G. Regulatory T cells as suppressors of anti-tumor immunity: role of metabolism. Cytokine Growth Factor Rev. 2017;35:15–25.
Mougiakakos D, Choudhury A, Lladser A, Kiessling R, Johansson CC. Regulatory T cells in cancer. Adv Cancer Res Elsevier. 2010;107:57–117.
Colombo MP, Piconese S. Regulatory T-cell inhibition versus depletion: the right choice in cancer immunotherapy. Nat Rev Cancer. 2007;7(11):880.
Nishikawa H, Sakaguchi S. Regulatory T cells in cancer immunotherapy. Curr Opin Immunol. 2014;27:1–7.
Whiteside TL, editor. What are regulatory T cells (Treg) regulating in cancer and why? Semin Cancer Biol. 2012;22(4):327–34.
Liakou CI, Kamat A, Tang DN, Chen H, Sun J, Troncoso P, et al. CTLA-4 blockade increases IFNγ-producing CD4+ ICOShi cells to shift the ratio of effector to regulatory T cells in cancer patients. Proc Natl Acad Sci. 2008;105(39):14987–92.
Eckburg PB, Bik EM, Bernstein CN, Purdom E, Dethlefsen L, Sargent M, et al. Diversity of the human intestinal microbial flora. Science. 2005;308(5728):1635–8.
Qin J, Li R, Raes J, Arumugam M, Burgdorf KS, Manichanh C, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010;464(7285):59.
Maynard CL, Elson CO, Hatton RD, Weaver CT. Reciprocal interactions of the intestinal microbiota and immune system. Nature. 2012;489(7415):231.
de Vos WM, de Vos EA. Role of the intestinal microbiome in health and disease: from correlation to causation. Nutr Rev. 2012;70(suppl_1):S45–56.
Nyangale EP, Mottram DS, Gibson GR. Gut microbial activity, implications for health and disease: the potential role of metabolite analysis. J Proteome Res. 2012;11(12):5573–85.
Cho I, Blaser MJ. The human microbiome: at the interface of health and disease. Nat Rev Genet. 2012;13(4):260.
Lee YK, Mazmanian SK. Has the microbiota played a critical role in the evolution of the adaptive immune system? Science. 2010;330(6012):1768–73.
Peterson C, Sharma V, Elmén L, Peterson S. Immune homeostasis, dysbiosis and therapeutic modulation of the gut microbiota. Clin Exp Immunol. 2015;179(3):363–77.
Klaenhammer TR, Kleerebezem M, Kopp MV, Rescigno M. The impact of probiotics and prebiotics on the immune system. Nat Rev Immunol. 2012;12(10):728.
Cerf-Bensussan N, Gaboriau-Routhiau V. The immune system and the gut microbiota: friends or foes? Nat Rev Immunol. 2010;10(10):735.
Guarner F, Bourdet-Sicard R, Brandtzaeg P, Gill HS, McGuirk P, Van Eden W, et al. Mechanisms of disease: the hygiene hypothesis revisited. Nat Rev Gastroenterol Hepatol. 2006;3(5):275.
Strober W, Fuss IJ, Blumberg RS. The immunology of mucosal models of inflammation. Annu Rev Immunol. 2002;20(1):495–549.
Gewirtz AT, Navas TA, Lyons S, Godowski PJ, Madara JL. Cutting edge: bacterial flagellin activates basolaterally expressed TLR5 to induce epithelial proinflammatory gene expression. J Immunol. 2001;167(4):1882–5.
Macpherson AJ, Uhr T. Induction of protective IgA by intestinal dendritic cells carrying commensal bacteria. Science. 2004;303(5664):1662–5.
Hooper LV, Macpherson AJ. Immune adaptations that maintain homeostasis with the intestinal microbiota. Nat Rev Immunol. 2010;10(3):159.
Salzman NH, Underwood MA, Bevins CL. Paneth cells, defensins, and the commensal microbiota: a hypothesis on intimate interplay at the intestinal mucosa. Semin Immunol. 2007;19(2):70–83.
Bevins CL, Salzman NH. Paneth cells, antimicrobial peptides and maintenance of intestinal homeostasis. Nat Rev Microbiol. 2011;9(5):356.
Lathrop SK, Bloom SM, Rao SM, Nutsch K, Lio C-W, Santacruz N, et al. Peripheral education of the immune system by colonic commensal microbiota. Nature. 2011;478(7368):250.
Di Giacinto C, Marinaro M, Sanchez M, Strober W, Boirivant M. Probiotics ameliorate recurrent Th1-mediated murine colitis by inducing IL-10 and IL-10-dependent TGF-β-bearing regulatory cells. J Immunol. 2005;174(6):3237–46.
Honda K, Littman DR. The microbiota in adaptive immune homeostasis and disease. Nature. 2016;535(7610):75.
Park S-G, Mathur R, Long M, Hosh N, Hao L, Hayden MS, et al. T regulatory cells maintain intestinal homeostasis by suppressing γδ T cells. Immunity. 2010;33(5):791–803.
Le MG, Moulton LH, Hill C, Kramar A. Consumption of dairy produce and alcohol in a case-control study of breast cancer. JNCI: J Nat Cancer Inst. 1986;77(3):633–6.
Peters RK, Pike MC, Garabrant D, Mack TM. Diet and colon cancer in Los Angeles county, California. Cancer Causes Control. 1992;3(5):457–73.
van’t Veer P, Dekker JM, Lamers JW, Kok FJ, Schouten EG, Brants HA, et al. Consumption of fermented milk products and breast cancer: a case-control study in the Netherlands. Cancer Res. 1989;49(14):4020–3.
Aso Y, Akazan H. Prophylactic effect of a Lactobacillus casei preparation on the recurrence of superficial bladder cancer. Urol Int. 1992;49(3):125–9.
Pala V, Sieri S, Berrino F, Vineis P, Sacerdote C, Palli D, et al. Yogurt consumption and risk of colorectal cancer in the Italian European prospective investigation into cancer and nutrition cohort. Int J Cancer. 2011;129(11):2712–9.
Rafter J, Bennett M, Caderni G, Clune Y, Hughes R, Karlsson PC, et al. Dietary synbiotics reduce cancer risk factors in polypectomized and colon cancer patients. Am J Clin Nutr. 2007;85(2):488–96.
Ishikawa H, Akedo I, Otani T, Suzuki T, Nakamura T, Takeyama I, et al. Randomized trial of dietary fiber and Lactobacillus casei administration for prevention of colorectal tumors. Int J Cancer. 2005;116(5):762–7.
Toi M, Hirota S, Tomotaki A, Sato N, Hozumi Y, Anan K, et al. Probiotic beverage with soy isoflavone consumption for breast cancer prevention: a case-control study. Curr Nutr Food Sci. 2013;9(3):194–200.
Campbell CG, Chew BP, Luedecke LO, Shultz TD. Yogurt consumption does not enhance immune function in healthy premenopausal women. Nutr Cancer. 2000;37(1):27–35.
Capurso G, Marignani M, Delle FG. Probiotics and the incidence of colorectal cancer: when evidence is not evident. Dig Liver Dis: Off J Ital Soc Gastroenterol Ital Assoc Study Liver. 2006;38(Suppl 2):S277–82.
Rossini A, Rumio C, Sfondrini L, Tagliabue E, Morelli D, Miceli R, et al. Influence of antibiotic treatment on breast carcinoma development in proto-neu transgenic mice. Cancer Res. 2006;66(12):6219–24.
Yoshimoto S, Loo TM, Atarashi K, Kanda H, Sato S, Oyadomari S, et al. Obesity-induced gut microbial metabolite promotes liver cancer through senescence secretome. Nature. 2013;499(7456):97.
Dapito DH, Mencin A, Gwak G-Y, Pradere J-P, Jang M-K, Mederacke I, et al. Promotion of hepatocellular carcinoma by the intestinal microbiota and TLR4. Cancer Cell. 2012;21(4):504–16.
Galdeano CM, De Leblanc ADM, Vinderola G, Bonet MB, Perdigon G. Proposed model: mechanisms of immunomodulation induced by probiotic bacteria. Clin Vaccine Immunol. 2007;14(5):485–92.
Corthésy B, Gaskins HR, Mercenier A. Cross-talk between probiotic bacteria and the host immune system. J Nutr. 2007;137(3):781S–90S.
Sheng YH, Hasnain SZ, Florin TH, McGuckin MA. Mucins in inflammatory bowel diseases and colorectal cancer. J Gastroenterol Hepatol. 2012;27(1):28–38.
Amit-Romach E, Uni Z, Reifen R. Multistep mechanism of probiotic bacterium, the effect on innate immune system. Mol Nutr Food Res. 2010;54(2):277–84.
Anderson RC, Cookson AL, McNabb WC, Park Z, McCann MJ, Kelly WJ, et al. Lactobacillus plantarum MB452 enhances the function of the intestinal barrier by increasing the expression levels of genes involved in tight junction formation. BMC Microbiol. 2010;10(1):316.
Yan F, Polk DB. Characterization of a probiotic-derived soluble protein which reveals a mechanism of preventive and treatment effects of probiotics on intestinal inflammatory diseases. Gut Microbes. 2012;3(1):25–8.
Khailova L, Mount Patrick SK, Arganbright KM, Halpern MD, Kinouchi T, Dvorak B. Bifidobacterium bifidum reduces apoptosis in the intestinal epithelium in necrotizing enterocolitis. Am J Physiol Gastrointest Liver Physiol. 2010;299(5):G1118–G27.
Stetinova V, Smetanova L, Kholova D, Kvetina J, Svoboda Z, Zidek Z, et al. Effect of probiotic Escherichia coli Nissle 1917 components on transepithelial transport of 5-aminosalicylic acid across Caco-2 monolayers. Toxicol Lett. 2011;205:S190.
Karczewski J, Troost FJ, Konings I, Dekker J, Kleerebezem M, Brummer R-JM, et al. Regulation of human epithelial tight junction proteins by Lactobacillus plantarum in vivo and protective effects on the epithelial barrier. Am J Physiol Gastrointest Liver Physiol. 2010;298(6):G851–G9.
Kaji R, Kiyoshima-Shibata J, Nagaoka M, Nanno M, Shida K. Bacterial teichoic acids reverse predominant IL-12 production induced by certain lactobacillus strains into predominant IL-10 production via TLR2-dependent ERK activation in macrophages. J Immunol. 2010;184(7):3505–13.
Sivieri K, Bedani R, Cavallini DCU, Rossi EA. Probiotics and intestinal microbiota: implications in colon cancer prevention. In: Kongo M, editor. Lactic acid bacteria-R & D for food, health and livestock purposes: Janeza Trdine 9, 51000 Rijeka. Croatia: InTech; 2013. p. 217–42.
Shida K, Kiyoshima-Shibata J, Kaji R, Nagaoka M, Nanno M. Peptidoglycan from lactobacilli inhibits interleukin-12 production by macrophages induced by Lactobacillus casei through toll-like receptor 2-dependent and independent mechanisms. Immunology. 2009;128(1 Suppl):e858–69.
Forsythe P, Bienenstock J. Immunomodulation by commensal and probiotic bacteria. Immunol Investig. 2010;39(4–5):429–48.
Kwon H-K, Lee C-G, So J-S, Chae C-S, Hwang J-S, Sahoo A, et al. Generation of regulatory dendritic cells and CD4+ Foxp3+ T cells by probiotics administration suppresses immune disorders. Proc Natl Acad Sci. 2010;107(5):2159–64.
Smits HH, Engering A, van der Kleij D, de Jong EC, Schipper K, van Capel TM, et al. Selective probiotic bacteria induce IL-10–producing regulatory T cells in vitro by modulating dendritic cell function through dendritic cell–specific intercellular adhesion molecule 3–grabbing nonintegrin. J Allergy Clin Immunol. 2005;115(6):1260–7.
Roller M, Clune Y, Collins K, Rechkemmer G, Watzl B. Consumption of prebiotic inulin enriched with oligofructose in combination with the probiotics Lactobacillus rhamnosus and Bifidobacterium lactis has minor effects on selected immune parameters in polypectomised and colon cancer patients. Br J Nutr. 2007;97(4):676–84.
Elmadfa I, Klein P, Meyer AL. Immune-stimulating effects of lactic acid bacteria in vivo and in vitro. Proc Nutr Soc. 2010;69(3):416–20.
Ewaschuk JB, Walker JW, Diaz H, Madsen KL. Bioproduction of conjugated linoleic acid by probiotic bacteria occurs in vitro and in vivo in mice. J Nutr. 2006;136(6):1483–7.
Nagao F, Nakayama M, Muto T, Okumura K. Effects of a fermented milk drink containing Lactobacillus casei strain Shirota on the immune system in healthy human subjects. Biosci Biotechnol Biochem. 2000;64(12):2706–8.
Zeuthen LH, Christensen HR, Frøkiær H. Lactic acid bacteria inducing a weak interleukin-12 and tumor necrosis factor alpha response in human dendritic cells inhibit strongly stimulating lactic acid bacteria but act synergistically with gram-negative bacteria. Clin Vaccine Immunol. 2006;13(3):365–75.
Raman M, Ambalam P, Kondepudi KK, Pithva S, Kothari C, Patel AT, et al. Potential of probiotics, prebiotics and synbiotics for management of colorectal cancer. Gut Microbes. 2013;4(3):181–92.
Feyisetan O, Tracey C, Hellawell GO. Probiotics, dendritic cells and bladder cancer. BJU Int. 2012;109(11):1594–7.
Stagg AJ, Hart AL, Knight SC, Kamm MA. Interactions between dendritic cells and bacteria in the regulation of intestinal immunity. Best Pract Res Clin Gastroenterol. 2004;18(2):255–70.
Christensen HR, Frøkiær H, Pestka JJ. Lactobacilli differentially modulate expression of cytokines and maturation surface markers in murine dendritic cells. J Immunol. 2002;168(1):171–8.
Rizzello V, Bonaccorsi I, Dongarra ML, Fink LN, Ferlazzo G. Role of natural killer and dendritic cell crosstalk in immunomodulation by commensal bacteria probiotics. J Biomed Biotechnol. 2011;2011:473097. https://doi.org/10.1155/2011/473097.
Takagi A, Ikemura H, Matsuzaki T, Sato M, Nomoto K, Morotomi M, et al. Relationship between the in vitro response of dendritic cells to Lactobacillus and prevention of tumorigenesis in the mouse. J Gastroenterol. 2008;43(9):661–9.
Matsumoto S, Hara T, Nagaoka M, Mike A, Mitsuyama K, Sako T, et al. A component of polysaccharide peptidoglycan complex on Lactobacillus induced an improvement of murine model of inflammatory bowel disease and colitis-associated cancer. Immunology. 2009;128(1 Suppl):e170–80.
Foligne B, Zoumpopoulou G, Dewulf J, Younes AB, Chareyre F, Sirard J-C, et al. A key role of dendritic cells in probiotic functionality. PLoS One. 2007;2(3):e313.
Shida K, Kiyoshima-Shibata J, Nagaoka M, Watanabe K, Nanno M. Induction of interleukin-12 by Lactobacillus strains having a rigid cell wall resistant to intracellular digestion. J Dairy Sci. 2006;89(9):3306–17.
Fink LN, Zeuthen LH, Christensen HR, Morandi B, Frøkiær H, Ferlazzo G. Distinct gut-derived lactic acid bacteria elicit divergent dendritic cell-mediated NK cell responses. Int Immunol. 2007;19(12):1319–27.
Miettinen M, Matikainen S, Vuopio-Varkila J, Pirhonen J, Varkila K, Kurimoto M, et al. Lactobacilli and streptococci induce interleukin-12 (IL-12), IL-18, and gamma interferon production in human peripheral blood mononuclear cells. Infect Immun. 1998;66(12):6058–62.
Haller D, Serrant P, Granato D, Schiffrin E, Blum S. Activation of human NK cells by staphylococci and lactobacilli requires cell contact-dependent costimulation by autologous monocytes. Clin Diagn Lab Immunol. 2002;9(3):649–57.
Takeda K, Suzuki T, Shimada SI, Shida K, Nanno M, Okumura K. Interleukin-12 is involved in the enhancement of human natural killer cell activity by Lactobacillus casei Shirota. Clin Exp Immunol. 2006;146(1):109–15.
Kang H-J, Im S-H. Probiotics as an immune modulator. J Nutr Sci Vitaminol. 2015;61(Supplement):S103–S5.
Santaolalla R, Sussman DA, Abreu MT. TLR signaling: a link between gut microflora, colorectal inflammation and tumorigenesis. Drug Discov Today: Dis Mech. 2011;8(3–4):e57–62.
Lee J-H, Lee B, Lee H-S, Bae E-A, Lee H, Ahn Y-T, et al. Lactobacillus suntoryeus inhibits pro-inflammatory cytokine expression and TLR-4-linked NF-κB activation in experimental colitis. Int J Color Dis. 2009;24(2):231–7.
Baricault L, Denariaz G, Houri J-J, Bouley C, Sapin C, Trugnan G. Use of HT-29, a cultured human colon cancer cell line, to study the effect of fermented milks on colon cancer cell growth and differentiation. Carcinogenesis. 1995;16(2):245–52.
Grimoud J, Durand H, De Souza S, Monsan P, Ouarné F, Theodorou V, et al. In vitro screening of probiotics and synbiotics according to anti-inflammatory and anti-proliferative effects. Int J Food Microbiol. 2010;144(1):42–50.
Biragyn A, Ruffini PA, Leifer CA, Klyushnenkova E, Shakhov A, Chertov O, et al. Toll-like receptor 4-dependent activation of dendritic cells by β-defensin 2. Science. 2002;298(5595):1025–9.
Paolillo R, Carratelli CR, Sorrentino S, Mazzola N, Rizzo A. Immunomodulatory effects of Lactobacillus plantarum on human colon cancer cells. Int Immunopharmacol. 2009;9(11):1265–71.
Möndel M, Schroeder B, Zimmermann K, Huber H, Nuding S, Beisner J, et al. Probiotic E. coli treatment mediates antimicrobial human β-defensin synthesis and fecal excretion in humans. Mucosal Immunol. 2009;2(2):166.
Foo N-P, Ou Yang H, Chiu H-H, Chan H-Y, Liao C-C, Yu C-K, et al. Probiotics prevent the development of 1, 2-dimethylhydrazine (DMH)-induced colonic tumorigenesis through suppressed colonic mucosa cellular proliferation and increased stimulation of macrophages. J Agric Food Chem. 2011;59(24):13337–45.
Schwartz-Albiez R, Monteiro R, Rodriguez M, Binder C, Shoenfeld Y. Natural antibodies, intravenous immunoglobulin and their role in autoimmunity, cancer and inflammation. Clin Exp Immunol. 2009;158(s1):43–50.
Galdeano CM, Perdigon G. The probiotic bacterium Lactobacillus casei induces activation of the gut mucosal immune system through innate immunity. Clin Vaccine Immunol. 2006;13(2):219–26.
Yasui H, Shida K, Matsuzaki T, Yokokura T. Immunomodulatory function of lactic acid bacteria. In: Konings W, Kuipers OP, Huis in’t Veld JHJ, editors. Lactic acid bacteria: genetics, metabolism and applications. New York: Springer; 1999. p. 383–9.
Lee JW, Kim EH, Yim IB, Joo HG. Immunomodulatory and antitumor effects in vivo by the cytoplasmic fraction of Lactobacillus casei and Bifidobacterium longum. J Vet Sci. 2004;5(1):41–8.
Lim BK, Mahendran R, Lee YK, Bay BH. Chemopreventive effect of lactobacttlus rhamnosus on growth of a subcutaneously implanted bladder cancer cell line in the mouse. Cancer Sci. 2002;93(1):36–41.
Chen C-C, Lin W-C, Kong M-S, Shi HN, Walker WA, Lin C-Y, et al. Oral inoculation of probiotics Lactobacillus acidophilus NCFM suppresses tumour growth both in segmental orthotopic colon cancer and extra-intestinal tissue. Br J Nutr. 2012;107(11):1623–34.
Bassaganya-Riera J, Viladomiu M, Pedragosa M, De Simone C, Carbo A, Shaykhutdinov R, et al. Probiotic bacteria produce conjugated linoleic acid locally in the gut that targets macrophage PPAR γ to suppress colitis. PLoS One. 2012;7(2):e31238.
Hu J, Wang C, Ye L, Yang W, Huang H, Meng F, et al. Anti-tumour immune effect of oral administration of Lactobacillus plantarum to CT26 tumour-bearing mice. J Biosci. 2015;40(2):269–79.
Aragón F, Carino S, Perdigón G. de LeBlanc AdM. The administration of milk fermented by the probiotic Lactobacillus casei CRL 431 exerts an immunomodulatory effect against a breast tumour in a mouse model. Immunobiology. 2014;219(6):457–64.
Lakritz JR, Poutahidis T, Levkovich T, Varian BJ, Ibrahim YM, Chatzigiagkos A, et al. Beneficial bacteria stimulate host immune cells to counteract dietary and genetic predisposition to mammary cancer in mice. Int J Cancer. 2014;135(3):529–40.
Seow SW, Cai S, Rahmat JN, Bay BH, Lee YK, Chan YH, et al. Lactobacillus rhamnosus GG induces tumor regression in mice bearing orthotopic bladder tumors. Cancer Sci. 2010;101(3):751–8.
Delcenserie V, Martel D, Lamoureux M, Amiot J, Boutin Y, Roy D. Immunomodulatory effects of probiotics in the intestinal tract. Curr Issues Mol Biol. 2008;10(1/2):37.
PERDIGÓN G, VALDEZ JC, RACHID M. Antitumour activity of yogurt: study of possible immune mechanisms. J Dairy Res. 1998;65(1):129–38.
Urbanska AM, Bhathena J, Martoni C, Prakash S. Estimation of the potential antitumor activity of microencapsulated Lactobacillus acidophilus yogurt formulation in the attenuation of tumorigenesis in Apc (Min/+) mice. Dig Dis Sci. 2009;54(2):264–73.
Matsuzaki T, Yokokura T, Mutai M. Antitumor effect of intrapleural administration of Lactobacillus casei in mice. Cancer Immunol Immunother. 1988;26(3):209–14.
Matsuzaki T. Immunomodulation by treatment with Lactobacillus casei strain Shirota. Int J Food Microbiol. 1998;41(2):133–40.
de LeBlanc AM, Perdigón G. Yogurt feeding inhibits promotion and progression of experimental colorectal cancer. Med Sci Monit. 2004;10(4):BR96–BR104.
Meydani SN, Ha W-K. Immunologic effects of yogurt. Am J Clin Nutr. 2000;71(4):861–72.
Grivennikov SI, editor. Inflammation and colorectal cancer: colitis-associated neoplasia. Semin Immunopathol. 2013;35:299. Springer
Femia AP, Luceri C, Dolara P, Giannini A, Biggeri A, Salvadori M, et al. Antitumorigenic activity of the prebiotic inulin enriched with oligofructose in combination with the probiotics Lactobacillus rhamnosus and Bifidobacterium lactis on azoxymethane-induced colon carcinogenesis in rats. Carcinogenesis. 2002;23(11):1953–60.
Rafter J, Bennett M, Caderni G, Clune Y, Hughes R, Karlsson PC, et al. Dietary synbiotics reduce cancer risk factors in polypectomized and colon cancer patients. Am J Clin Nutr. 2007;85(2):488–96.
Fotiadis CI, Stoidis CN, Spyropoulos BG, Zografos ED. Role of probiotics, prebiotics and synbiotics in chemoprevention for colorectal cancer. World J Gastroenterol: WJG. 2008;14(42):6453.
Grivennikov SI, Wang K, Mucida D, Stewart CA, Schnabl B, Jauch D, et al. Adenoma-linked barrier defects and microbial products drive IL-23/IL-17-mediated tumour growth. Nature. 2012;491(7423):254.
Tosolini M, Kirilovsky A, Mlecnik B, Fredriksen T, Mauger S, Bindea G, et al. Clinical impact of different classes of infiltrating T cytotoxic and helper cells (Th1, th2, treg, th17) in patients with colorectal cancer. Cancer Res. 2011;71(4):1263–71.
Li J, Sung CYJ, Lee N, Ni Y, Pihlajamäki J, Panagiotou G, et al. Probiotics modulated gut microbiota suppresses hepatocellular carcinoma growth in mice. Proc Natl Acad Sci. 2016;113(9):E1306–E15.
Lee N-K, Son S-H, Jeon EB, Jung GH, Lee J-Y, Paik H-D. The prophylactic effect of probiotic Bacillus polyfermenticus KU3 against cancer cells. J Funct Foods. 2015;14:513–8.
Han KJ, Lee N-K, Park H, Paik H-D. Anticancer and anti-inflammatory activity of probiotic Lactococcus lactis NK34. J Microbiol Biotechnol. 2015;25:1697–701.
Blasingame CA, Billups LH, Graham T, Henry J, Carter B, Threadgill DW, et al. Modulation of colorectal cancer by the probiotic organism Lactobacillus reuteri. Prof Agric Workers J. 2016;3(2):3.
Lenoir M, Del Carmen S, Cortes-Perez NG, Lozano-Ojalvo D, Muñoz-Provencio D, Chain F, et al. Lactobacillus casei BL23 regulates Treg and Th17 T-cell populations and reduces DMH-associated colorectal cancer. J Gastroenterol. 2016;51(9):862–73.
Murugaiyan G, Saha B. Protumor vs antitumor functions of IL-17. J Immunol. 2009;183(7):4169–75.
Bailey SR, Nelson MH, Himes RA, Li Z, Mehrotra S, Paulos CM. Th17 cells in cancer: the ultimate identity crisis. Front Immunol. 2014;5:276.
Zaidi MR, Merlino G. The two faces of interferon-γ in cancer. Clin Cancer Res. 2011;17(19):6118–24.
Beatty GL, Paterson Y. Regulation of tumor growth by IFN-γ in cancer immunotherapy. Immunol Res. 2001;24(2):201–10.
Fooladi AAI, Yazdi MH, Pourmand MR, Mirshafiey A, Hassan ZM, Azizi T, et al. Th1 cytokine production induced by Lactobacillus acidophilus in BALB/c mice bearing transplanted breast tumor. Jundishapur J Microbiol. 2015;8(4):e17354. https://doi.org/10.5812/jjm.8(4)2015.17354.
Gui Q, Lu H, Zhang C, Xu Z, Yang Y. Well-balanced commensal microbiota contributes to anti-cancer response in a lung cancer mouse model. Genet Mol Res. 2015;14(2):5642–51.
Sharma M, Shukla G. Metabiotics: one step ahead of probiotics; an insight into mechanisms involved in anticancerous effect in colorectal cancer. Front Microbiol. 2016;7:1940.
Vipperla K, O’Keefe SJ. The microbiota and its metabolites in colonic mucosal health and cancer risk. Nutr Clin Pract. 2012;27(5):624–35.
Kumar M, Nagpal R, Verma V, Kumar A, Kaur N, Hemalatha R, et al. Probiotic metabolites as epigenetic targets in the prevention of colon cancer. Nutr Rev. 2013;71(1):23–34.
Tedelind S, Westberg F, Kjerrulf M, Vidal A. Anti-inflammatory properties of the short-chain fatty acids acetate and propionate: a study with relevance to inflammatory bowel disease. World J Gastroenterol: WJG. 2007;13(20):2826.
Hosseini E, Grootaert C, Verstraete W, Van de Wiele T. Propionate as a health-promoting microbial metabolite in the human gut. Nutr Rev. 2011;69(5):245–58.
Bassaganya-Riera J, Viladomiu M, Pedragosa M, De Simone C, Hontecillas R. Immunoregulatory mechanisms underlying prevention of colitis-associated colorectal cancer by probiotic bacteria. PLoS One. 2012;7(4):e34676.
Iida N, Dzutsev A, Stewart CA, Smith L, Bouladoux N, Weingarten RA, et al. Commensal bacteria control cancer response to therapy by modulating the tumor microenvironment. Science. 2013;342(6161):967–70.
Vicari AP, Chiodoni C, Vaure C, Aït-Yahia S, Dercamp C, Matsos F, et al. Reversal of tumor-induced dendritic cell paralysis by CpG immunostimulatory oligonucleotide and anti–interleukin 10 receptor antibody. J Exp Med. 2002;196(4):541–9.
Viaud S, Saccheri F, Mignot G, Yamazaki T, Daillère R, Hannani D, et al. The intestinal microbiota modulates the anticancer immune effects of cyclophosphamide. Science. 2013;342(6161):971–6.
Daillère R, Vétizou M, Waldschmitt N, Yamazaki T, Isnard C, Poirier-Colame V, et al. Enterococcus hirae and Barnesiella intestinihominis facilitate cyclophosphamide-induced therapeutic immunomodulatory effects. Immunity. 2016;45(4):931–43.
Vétizou M, Pitt JM, Daillère R, Lepage P, Waldschmitt N, Flament C, et al. Anticancer immunotherapy by CTLA-4 blockade relies on the gut microbiota. Science. 2015;350(6264):1079–84.
Sivan A, Corrales L, Hubert N, Williams JB, Aquino-Michaels K, Earley ZM, et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti–PD-L1 efficacy. Science. 2015;350(6264):1084–9.
Dubin K, Callahan MK, Ren B, Khanin R, Viale A, Ling L, et al. Intestinal microbiome analyses identify melanoma patients at risk for checkpoint-blockade-induced colitis. Nat Commun. 2016;7:10391.
Rupnik M. Toward a true bacteriotherapy for Clostridium difficile infection. N Engl J Med. 2015;372(16):1566–8.
Van Nood E, Vrieze A, Nieuwdorp M, Fuentes S, Zoetendal EG, de Vos WM, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407–15.
Swidsinski A, Khilkin M, Kerjaschki D, Schreiber S, Ortner M, Weber J, et al. Association between intraepithelial Escherichia coli and colorectal cancer. Gastroenterology. 1998;115(2):281–6.
Wu S, Rhee K-J, Albesiano E, Rabizadeh S, Wu X, Yen H-R, et al. A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses. Nat Med. 2009;15(9):1016.
Uronis JM, Mühlbauer M, Herfarth HH, Rubinas TC, Jones GS, Jobin C. Modulation of the intestinal microbiota alters colitis-associated colorectal cancer susceptibility. PLoS One. 2009;4(6):e6026.
Chen GY, Shaw MH, Redondo G, Núñez G. The innate immune receptor Nod1 protects the intestine from inflammation-induced tumorigenesis. Cancer Res. 2008;68(24):10060–7.
Poutahidis T, Kleinewietfeld M, Erdman S. Gut microbiota and the paradox of cancer immunotherapy. Front Immunol. 2014;5:157.
Erdman SE, Poutahidis T, Tomczak M, Rogers AB, Cormier K, Plank B, et al. CD4+ CD25+ regulatory T lymphocytes inhibit microbially induced colon cancer in Rag2-deficient mice. Am J Pathol. 2003;162(2):691–702.
Poutahidis T, Kleinewietfeld M, Smillie C, Levkovich T, Perrotta A, Bhela S, et al. Microbial reprogramming inhibits Western diet-associated obesity. PLoS One. 2013;8(7):e68596.
Hassoun LA, Sivamani RK. A systematic review of lactoferrin use in dermatology. Crit Rev Food Sci Nutr. 2017;57(17):3632–9.
Legrand D, Pierce A, Elass E, Carpentier M, Mariller C, Mazurier J. Lactoferrin structure and functions. In: Bosze Z, editor. Bioactive components of Milk. New York: Springer; 2008. p. 163–94.
Caccavo D, Pellegrino NM, Altamura M, Rigon A, Amati L, Amoroso A, et al. Antimicrobial and immunoregulatory functions of lactoferrin and its potential therapeutic application. J Endotoxin Res. 2002;8(6):403–17.
Kennedy RS, Konok GP, Bounous G, Baruchel S, Lee TD. The use of a whey protein concentrate in the treatment of patients with metastatic carcinoma: a phase I-II clinical study. Anticancer Res. 1995;15(6):2643–50.
Damiens E, El Yazidi I, Mazurier J, Elass-Rochard E, Duthille I, Spik G, et al. Role of heparan sulphate proteoglycans in the regulation of human lactoferrin binding and activity in the MDA-MB-231 breast cancer cell line. Eur J Cell Biol. 1998;77(4):344–51.
Damiens E, Mazurier J, El Yazidi I, Masson M, Duthille I, Spik G, et al. Effects of human lactoferrin on NK cell cytotoxicity against haematopoietic and epithelial tumour cells. Biochimica et Biophysica Acta (BBA)-molecular. Cell Res. 1998;1402(3):277–87.
Sakamoto N. Antitumor effect of human lactoferrin against newly established human pancreatic cancer cell line SPA. Gan to kagaku ryoho Cancer Chemother. 1998;25(10):1557–63.
McKeown ST, Lundy FT, Nelson J, Lockhart D, Irwin CR, Cowan CG, et al. The cytotoxic effects of human neutrophil peptide-1 (HNP1) and lactoferrin on oral squamous cell carcinoma (OSCC) in vitro. Oral Oncol. 2006;42(7):685–90.
Ishii K, Takamura N, Shinohara M, Wakui N, Shin H, Sumino Y, et al. Long-term follow-up of chronic hepatitis C patients treated with oral lactoferrin for 12 months. Hepatol Res. 2003;25(3):226–33.
Wolf JS, Li D, Taylor RJ, O’Malley BW Jr. Lactoferrin inhibits growth of malignant tumors of the head and neck. ORL. 2003;65(5):245–9.
Sekine K, Watanabe E, Nakamura J, Takasuka N, Kim DJ, Asamoto M, et al. Inhibition of azoxymethane-initiated colon tumor by bovine lactoferrin administration in f344 rats. Cancer Sci. 1997;88(6):523–6.
Ushida Y, Sekine K, Kuhara T, Takasuka N, Iigo M, Maeda M, et al. Possible chemopreventive effects of bovine lactoferrin on esophagus and lung carcinogenesis in the rat. Cancer Sci. 1999;90(3):262–7.
Wolf JS, Li G, Varadhachary A, Petrak K, Schneyer M, Li D, et al. Oral lactoferrin results in T cell–dependent tumor inhibition of head and neck squamous cell carcinoma in vivo. Clin Cancer Res. 2007;13(5):1601–10.
Kanwar JR, Palmano KP, Sun X, Kanwar RK, Gupta R, Haggarty N, et al. ‘Iron-saturated’lactoferrin is a potent natural adjuvant for augmenting cancer chemotherapy. Immunol Cell Biol. 2008;86(3):277–88.
Rodrigues L, Teixeira J, Schmitt F, Paulsson M, Månsson HL. Lactoferrin and cancer disease prevention. Crit Rev Food Sci Nutr. 2008;49(3):203–17.
Hartog A, Leenders I, van der Kraan PM, Garssen J. Anti-inflammatory effects of orally ingested lactoferrin and glycine in different zymosan-induced inflammation models: evidence for synergistic activity. Int Immunopharmacol. 2007;7(13):1784–92.
Spagnuolo PA, Bird RP, Hoffman-Goetz L. Effect of short-term dietary intake of bovine lactoferrin on intestinal lymphocyte apoptosis in healthy mice. Nutrition. 2007;23(11):812–7.
Lee H-Y, Park J-H, Seok S-H, Baek M-W, Kim D-J, Lee B-H, et al. Potential antimicrobial effects of human lactoferrin against oral infection with Listeria monocytogenes in mice. J Med Microbiol. 2005;54(11):1049–54.
Zimecki M, Artym J, Chodaczek G, Kocieba M, Kruzel M. Protective effects of lactoferrin in Escherichia coli-induced bacteremia in mice: relationship to reduced serum TNF alpha level and increased turnover of neutrophils. Inflamm Res. 2004;53(7):292–2296.
Lupetti A, Brouwer CP, Bogaards SJ, Welling MM, de Heer E, Campa M, et al. Human lactoferrin-derived peptide’s antifungal activities against disseminated Candida albicans infection. J Infect Dis. 2007;196(9):1416–24.
Takakura N, Wakabayashi H, Yamauchi K, Takase M. Influences of orally administered lactoferrin on IFN-γ and IL-10 production by intestinal intraepithelial lymphocytes and mesenteric lymph-node cells. Biochem Cell Biol. 2006;84(3):363–8.
Guillén C, McInnes IB, Vaughan DM, Kommajosyula S, Van Berkel PH, Leung BP, et al. Enhanced Th1 response to Staphylococcus aureus infection in human lactoferrin-transgenic mice. J Immunol. 2002;168(8):3950–7.
Zuccotti GV, Vigano A, Borelli M, Saresella M, Giacomet V, Clerici M. Modulation of innate and adaptive immunity by lactoferrin in human immunodeficiency virus (HIV)-infected, antiretroviral therapy-naïve children. Int J Antimicrob Agents. 2007;29(3):353–5.
Fischer R, Debbabi H, Dubarry M, Boyaka P, Tome D. Regulation of physiological and pathological Th1 and Th2 responses by lactoferrin. Biochem Cell Biol. 2006;84(3):303–11.
Zimecki M, Właszczyk A, Zagulski T, Kübler A. Lactoferrin lowers serum interleukin 6 and tumor necrosis factor alpha levels in mice subjected to surgery. Arch Immunol Ther Exp. 1998;46(2):97–104.
Kuhara T, Iigo M, Itoh T, Ushida Y, Sekine K, Terada N, et al. Orally administered lactoferrin exerts an antimetastatic effect and enhances production of IL-18 in the intestinal epithelium. Nutr Cancer. 2000;38(2):192–9.
Wang WP, Iigo M, Sato J, Sekine K, Adachi I, Tsuda H. Activation of intestinal mucosal immunity in tumor-bearing mice by lactoferrin. Cancer Sci. 2000;91(10):1022–7.
Iigo M, Kuhara T, Ushida Y, Sekine K, Moore MA, Tsuda H. Inhibitory effects of bovine lactoferrin on colon carcinoma 26 lung metastasis in mice. Clin Exp Metastasis. 1999;17(1):43–9.
Bezault J, Bhimani R, Wiprovnick J, Furmanski P. Human lactoferrin inhibits growth of solid tumors and development of experimental metastases in mice. Cancer Res. 1994;54(9):2310–2.
Sekine K, Ushida Y, Kuhara T, Iigo M, Baba-Toriyama H, Moore MA, et al. Inhibition of initiation and early stage development of aberrant crypt foci and enhanced natural killer activity in male rats administered bovine lactoferrin concomitantly with azoxymethane. Cancer Lett. 1997;121(2):211–6.
Mulder AM, Connellan PA, Oliver CJ, Morris CA, Stevenson LM. Bovine lactoferrin supplementation supports immune and antioxidant status in healthy human males. Nutr Res. 2008;28(9):583–9.
Legrand D, Elass E, Carpentier M, Mazurier J. Lactoferrin: a modulator of immune and inflammatory responses. Cell Mole Life Sci: CMLS. 2005;62(22):2549–59.
Yamauchi K, Wakabayashi H, Shin K, Takase M. Bovine lactoferrin: benefits and mechanism of action against infections. Biochem Cell Biol. 2006;84(3):291–6.
Ward P, Paz E, Conneely O. Multifunctional roles of lactoferrin: a critical overview. Cell Mol Life Sci. 2005;62(22):2540–8.
Suzuki YA, Lopez V, Lonnerdal B. Mammalian lactoferrin receptors: structure and function. Cell Mole Life Sci: CMLS. 2005;62(22):2560–75.
Na YJ, Han SB, Kang JS, Yoon YD, Park S-K, Kim HM, et al. Lactoferrin works as a new LPS-binding protein in inflammatory activation of macrophages. Int Immunopharmacol. 2004;4(9):1187–99.
Szuster-Ciesielska A, Kaminska T, Kandefer-Szerszeń M. Phagocytosis-enhancing effect of lactoferrin on bovine peripheral. Arch Vet Pol. 1995;35:1–2.
Kai K, Ki K, Komine Y, Kuroishi T, Kozutsumi T, Kobayashi J, et al. Lactoferrin stimulates a Staphylococcus aureus killing activity of bovine phagocytes in the mammary gland. Microbiol Immunol. 2002;46(3):187–94.
Damiens E, El Yazidi I, Mazurier J, Duthille I, Spik G, Boilly-Marer Y. Lactoferrin inhibits G1 cyclin-dependent kinases during growth arrest of human breast carcinoma cells. J Cell Biochem. 1999;74(3):486–98.
Kuhara T, Yamauchi K, Tamura Y, Okamura H. Oral administration of lactoferrin increases NK cell activity in mice via increased production of IL-18 and type I IFN in the small intestine. J Interf Cytokine Res. 2006;26(7):489–99.
Zimecki M, Mazurier J, Machnicki M, Wieczorek Z, Montreuil J, Spik G. Immunostimulatory activity of lactotransferrin and maturation of CD4− CD8− murine thymocytes. Immunol Lett. 1991;30(1):119–23.
Matsuda Y, Saoo K, Hosokawa K, Yamakawa K, Yokohira M, Zeng Y, et al. Post-initiation chemopreventive effects of dietary bovine lactoferrin on 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone-induced lung tumorigenesis in female A/J mice. Cancer Lett. 2007;246(1):41–6.
Norrby K, Mattsby-Baltzer I, Innocenti M, Tuneberg S. Orally administered bovine lactoferrin systemically inhibits VEGF165-mediated angiogenesis in the rat. Int J Cancer. 2001;91(2):236–40.
Artym J, Zimecki M, Paprocka M, Kruzel ML. Orally administered lactoferrin restores humoral immune response in immunocompromised mice. Immunol Lett. 2003;89(1):9–15.
Lee WJ, Farmer JL, Hilty M, Kim YB. The protective effects of lactoferrin feeding against endotoxin lethal shock in germfree piglets. Infect Immun. 1998;66(4):1421–6.
Wada T, Aiba Y, Shimizu K, Takagi A, Miwa T, Koga Y. The therapeutic effect of bovine lactoferrin in the host infected with Helicobacter pylori. Scand J Gastroenterol. 1999;34(3):238–43.
Tsuda H, Ohshima Y, Nomoto H, Fujita K-I, Matsuda E, Iigo M, et al. Cancer prevention by natural compounds. Drug Metab Pharmacokinet. 2004;19(4):245–63.
Shimamura M, Yamamoto Y, Ashino H, Oikawa T, Hazato T, Tsuda H, et al. Bovine lactoferrin inhibits tumor-induced angiogenesis. Int J Cancer. 2004;111(1):111–6.
Norrby K. Human apo-lactoferrin enhances angiogenesis mediated by vascular endothelial growth factor A in vivo. J Vasc Res. 2004;41(4):293–304.
Iigo M, Shimamura M, Matsuda E, Fujita K-i, Nomoto H, Satoh J, et al. Orally administered bovine lactoferrin induces caspase-1 and interleukin-18 in the mouse intestinal mucosa: a possible explanation for inhibition of carcinogenesis and metastasis. Cytokine. 2004;25(1):36–44.
Pinchuk G. Theory and problems of immunology (Schaum’s outlines series). New York: McGraw-Hill; 2002.
Håversen L, Ohlsson BG, Hahn-Zoric M, Hanson LÅ, Mattsby-Baltzer I. Lactoferrin down-regulates the LPS-induced cytokine production in monocytic cells via NF-κB. Cell Immunol. 2002;220(2):83–95.
Yamauchi K, Wakabayashi H, Hashimoto S, Teraguchi S, Hayasawa H, Tomita M. Effects of orally administered bovine lactoferrin on the immune system of healthy volunteers. Adv Exp Med Biol. 1998;443:261–5.
Zimecki M, Właszczyk A, Cheneau P, Brunel A-S, Mazurier J, Spik G, et al. Immunoregulatory effects of a nutritional preparation containing bovine lactoferrin taken orally by healthy individuals. Arch Immunol Ther Exp. 1998;46(4):231–40.
Zimecki M, Spiegel K, Właszczyk A, Kübler A, Kruzel ML. Lactoferrin increases the output of neutrophil precursors and attenuates the spontaneous production of TNF-alpha and IL-6 by peripheral blood cells. Arch Immunol Ther Exp. 1999;47(2):113–8.
Kimber I, Cumberbatch M, Dearman R, Headon D, Bhushan M, Griffiths CE. Lactoferrin: influences on Langerhans cells, epidermal cytokines, and cutaneous inflammation. Biochem Cell Biol. 2002;80(1):103–7.
Ishikado A, Imanaka H, Kotani M, Fujita A, Mitsuishi Y, Kanemitsu T, et al. Liposomal lactoferrin induced significant increase of the interferon-alpha (IFN-α) producibility in healthy volunteers. Biofactors. 2004;21(1–4):69–72.
Burns J, Yokota T, Ashihara H, Lean ME, Crozier A. Plant foods and herbal sources of resveratrol. J Agric Food Chem. 2002;50(11):3337–40.
Lyons MM, Yu C, Toma R, Cho SY, Reiboldt W, Lee J, et al. Resveratrol in raw and baked blueberries and bilberries. J Agric Food Chem. 2003;51(20):5867–70.
Carrizzo A, Forte M, Damato A, Trimarco V, Salzano F, Bartolo M, et al. Antioxidant effects of resveratrol in cardiovascular, cerebral and metabolic diseases. Food Chem Toxicol. 2013;61:215–26.
Udenigwe CC, Ramprasath VR, Aluko RE, Jones PJ. Potential of resveratrol in anticancer and anti-inflammatory therapy. Nutr Rev. 2008;66(8):445–54.
Peng W, Qin R, Li X, Zhou H. Botany, phytochemistry, pharmacology, and potential application of Polygonum cuspidatum Sieb. et Zucc.: a review. J Ethnopharmacol. 2013;148(3):729–45.
Jang M, Cai L, Udeani GO, Slowing KV, Thomas CF, Beecher CW, et al. Cancer chemopreventive activity of resveratrol, a natural product derived from grapes. Science. 1997;275(5297):218–20.
Hosseini A, Ghorbani A. Cancer therapy with phytochemicals: evidence from clinical studies. Avicenna J Phytomed. 2015;5(2):84.
Cheng W, Zhao Y, Liu H, Fan Q, Lu FF, Li J, et al. Resveratrol attenuates bone cancer pain through the inhibition of spinal glial activation and CX3CR1 upregulation. Fundam Clin Pharmacol. 2014;28(6):661–70.
Surh Y-J. Cancer chemoprevention with dietary phytochemicals. Nat Rev Cancer. 2003;3(10):768.
Aggarwal BB, Bhardwaj A, Aggarwal RS, Seeram NP, Shishodia S, Takada Y. Role of resveratrol in prevention and therapy of cancer: preclinical and clinical studies. Anticancer Res. 2004;24(5A):2783–840.
Holmes-McNary M, Baldwin AS. Chemopreventive properties of trans-resveratrol are associated with inhibition of activation of the IκB kinase. Cancer Res. 2000;60(13):3477–83.
Manna SK, Mukhopadhyay A, Aggarwal BB. Resveratrol suppresses TNF-induced activation of nuclear transcription factors NF-κB, activator protein-1, and apoptosis: potential role of reactive oxygen intermediates and lipid peroxidation. J Immunol. 2000;164(12):6509–19.
Leiro J, Alvarez E, Arranz JA, Laguna R, Uriarte E, Orallo F. Effects of cis-resveratrol on inflammatory murine macrophages: antioxidant activity and down-regulation of inflammatory genes. J Leukoc Biol. 2004;75(6):1156–65.
Mutoh M, Takahashi M, Fukuda K, Matsushima-Hibiya Y, Mutoh H, Sugimura T, et al. Suppression of cyclooxygenase-2 promoter-dependent transcriptional activity in colon cancer cells by chemopreventive agents with a resorcin-type structure. Carcinogenesis. 2000;21(5):959–63.
Benitez DA, Hermoso MA, Pozo-Guisado E, Fernández-Salguero PM, Castellón EA. Regulation of cell survival by resveratrol involves inhibition of NFκB-regulated gene expression in prostate cancer cells. Prostate. 2009;69(10):1045–54.
Bhardwaj A, Sethi G, Vadhan-Raj S, Bueso-Ramos C, Takada Y, Gaur U, et al. Resveratrol inhibits proliferation, induces apoptosis, and overcomes chemoresistance through down-regulation of STAT3 and nuclear factor-kappaB-regulated antiapoptotic and cell survival gene products in human multiple myeloma cells. Blood. 2007;109(6):2293–302.
Suh DH, Kim M-K, Kim HS, Chung HH, Song YS. Cancer-specific therapeutic potential of resveratrol: metabolic approach against hallmarks of cancer. Funct Foods Health Dis. 2013;3(8):332–43.
Nonn L, Duong D, Peehl DM. Chemopreventive anti-inflammatory activities of curcumin and other phytochemicals mediated by MAP kinase phosphatase-5 in prostate cells. Carcinogenesis. 2006;28(6):1188–96.
Yeung F, Hoberg JE, Ramsey CS, Keller MD, Jones DR, Frye RA, et al. Modulation of NF-κB-dependent transcription and cell survival by the SIRT1 deacetylase. EMBO J. 2004;23(12):2369–80.
Kundu JK, Surh Y-J. Cancer chemopreventive and therapeutic potential of resveratrol: mechanistic perspectives. Cancer Lett. 2008;269(2):243–61.
Banerjee S, Bueso-Ramos C, Aggarwal BB. Suppression of 7,12-dimethylbenz(a)anthracene-induced mammary carcinogenesis in rats by resveratrol: role of nuclear factor-kappaB, cyclooxygenase 2, and matrix metalloprotease 9. Cancer Res. 2002;62(17):4945–54.
Maccarrone M, Lorenzon T, Guerrieri P, Agrò AF. Resveratrol prevents apoptosis in K562 cells by inhibiting lipoxygenase and cyclooxygenase activity. FEBS J. 1999;265(1):27–34.
Cao Z, Fang J, Xia C, Shi X, Jiang B-H. Trans-3, 4, 5′-Trihydroxystibene inhibits hypoxia-inducible factor 1α and vascular endothelial growth factor expression in human ovarian cancer cells. Clin Cancer Res. 2004;10(15):5253–63.
Park SY, Jeong KJ, Lee J, Yoon DS, Choi WS, Kim YK, et al. Hypoxia enhances LPA-induced HIF-1α and VEGF expression: their inhibition by resveratrol. Cancer Lett. 2007;258(1):63–9.
Latruffe N, Lançon A, Frazzi R, Aires V, Delmas D, Michaille JJ, et al. Exploring new ways of regulation by resveratrol involving miRNAs, with emphasis on inflammation. Ann N Y Acad Sci. 2015;1348(1):97–106.
Ren Z, Wang L, Cui J, Huoc Z, Xue J, Cui H, et al. Resveratrol inhibits NF-κB signaling through suppression of p65 and IB kinase activities. Die Pharmazie- Int J Pharm Sci. 2013;68(8):689–94.
Bickenbach K, Veerapong J, Shao M, Mauceri H, Posner M, Kron S, et al. Resveratrol is an effective inducer of CArG-driven TNF-α gene therapy. Cancer Gene Ther. 2008;15(3):133.
Delmas D, Rebe C, Micheau O, Athias A, Gambert P, Grazide S, et al. Redistribution of CD95, DR4 and DR5 in rafts accounts for the synergistic toxicity of resveratrol and death receptor ligands in colon carcinoma cells. Oncogene. 2004;23(55):8979.
Ghiringhelli F, Rebe C, Hichami A, Delmas D. Immunomodulation and anti-inflammatory roles of polyphenols as anticancer agents. Anti-Cancer Agents Med Chem (Formerly Current Medicinal Chemistry-Anti-Cancer Agents). 2012;12(8):852–73.
Li W, Ma J, Ma Q, Li B, Han L, Liu J, et al. Resveratrol inhibits the epithelial-mesenchymal transition of pancreatic cancer cells via suppression of the PI-3K/Akt/NF-κB pathway. Curr Med Chem. 2013;20(33):4185–94.
Zhong L-X, Li H, Wu M-L, Liu X-Y, Zhong M-J, Chen X-Y, et al. Inhibition of STAT3 signaling as critical molecular event in resveratrol-suppressed ovarian cancer cells. J Ovarian Res. 2015;8(1):25.
Golkar L, Ding X-Z, Ujiki MB, Salabat MR, Kelly DL, Scholtens D, et al. Resveratrol inhibits pancreatic cancer cell proliferation through transcriptional induction of macrophage inhibitory cytokine-1. J Surg Res. 2007;138(2):163–9.
Wang H, Zhang H, Tang L, Chen H, Wu C, Zhao M, et al. Resveratrol inhibits TGF-β1-induced epithelial-to-mesenchymal transition and suppresses lung cancer invasion and metastasis. Toxicology. 2013;303:139–46.
Schaafsma E, Hsieh T-C, Doonan BB, Pinto JT, Wu JM. Anticancer activities of resveratrol in colorectal cancer. Biol Med. 2016;8(5):1.
Basly J-P, Marre-Fournier F, Le Bail J-C, Habrioux G, Chulia AJ. Estrogenic/antiestrogenic and scavenging properties of (E)-and (Z)-resveratrol. Life Sci. 2000;66(9):769–77.
Serrero G, Lu R. Effect of resveratrol on the expression of autocrine growth modulators in human breast cancer cells. Antioxid Redox Signal. 2001;3(6):969–79.
Sharma S, Chopra K, Kulkarni S, Agrewala J. Resveratrol and curcumin suppress immune response through CD28/CTLA-4 and CD80 co-stimulatory pathway. Clin Exp Immunol. 2007;147(1):155–63.
Kim GY, Cho H, Ahn SC, Oh YH, Lee CM, Park YM. Resveratrol inhibits phenotypic and functional maturation of murine bone marrow-derived dendritic cells. Int Immunopharmacol. 2004;4(2):245–53.
Singh UP, Singh NP, Singh B, Hofseth LJ, Taub DD, Price RL, et al. Role of resveratrol-induced CD11b(+) Gr-1(+) myeloid derived suppressor cells (MDSCs) in the reduction of CXCR3(+) T cells and amelioration of chronic colitis in IL-10(-/-) mice. Brain Behav Immun. 2012;26(1):72–82.
Švajger U, Obermajer N, Jeras M. Dendritic cells treated with resveratrol during differentiation from monocytes gain substantial tolerogenic properties upon activation. Immunology. 2010;129(4):525–35.
Petro TM. Regulatory role of resveratrol on Th17 in autoimmune disease. Int Immunopharmacol. 2011;11(3):310–8.
Feng Y-H, Zou J-P, Li X-Y. Effects of resveratrol and ethanol on production of proinflammtory factors from endotoxin activated murine macrophages. Acta Pharmacol Sin. 2002;23(11):1002–6.
Singh UP, Singh NP, Singh B, Hofseth LJ, Taub DD, Price RL, et al. Role of resveratrol-induced CD11b+ Gr-1+ myeloid derived suppressor cells (MDSCs) in the reduction of CXCR3+ T cells and amelioration of chronic colitis in IL-10−/− mice. Brain Behav Immun. 2012;26(1):72–82.
Yang Y, Paik JH, Cho D, Cho J-A, Kim C-W. Resveratrol induces the suppression of tumor-derived CD4+ CD25+ regulatory T cells. Int Immunopharmacol. 2008;8(4):542–7.
Feng Y-H, Zhou W-L, Wu Q-L, Li X-Y, Zhao W-M, Zou J-P. Low dose of resveratrol enhanced immune response of mice. Acta Pharmacol Sin. 2002;23(10):893–7.
Yang Y, Paik JH, Cho D, Cho JA, Kim CW. Resveratrol induces the suppression of tumor-derived CD4+CD25+ regulatory T cells. Int Immunopharmacol. 2008;8(4):542–7.
Buhrmann C, Shayan P, Kraehe P, Popper B, Goel A, Shakibaei M. Resveratrol induces chemosensitization to 5-fluorouracil through up-regulation of intercellular junctions, epithelial-to-mesenchymal transition and apoptosis in colorectal cancer. Biochem Pharmacol. 2015;98(1):51–68.
Jiang Z, Chen X, Chen K, Sun L, Gao L, Zhou C, et al. YAP inhibition by resveratrol via activation of AMPK enhances the sensitivity of pancreatic cancer cells to gemcitabine. Nutrients. 2016;8(10):546.
Kala R, Shah HN, Martin SL, Tollefsbol TO. Epigenetic-based combinatorial resveratrol and pterostilbene alters DNA damage response by affecting SIRT1 and DNMT enzyme expression, including SIRT1-dependent γ-H2AX and telomerase regulation in triple-negative breast cancer. BMC Cancer. 2015;15(1):672.
Huang H, Lin H, Zhang X, Li J. Resveratrol reverses temozolomide resistance by downregulation of MGMT in T98G glioblastoma cells by the NF-κB-dependent pathway. Oncol Rep. 2012;27(6):2050–6.
Xu J, Liu D, Niu H, Zhu G, Xu Y, Ye D, et al. Resveratrol reverses Doxorubicin resistance by inhibiting epithelial-mesenchymal transition (EMT) through modulating PTEN/Akt signaling pathway in gastric cancer. J Exp Clin Cancer Res. 2017;36(1):19.
Ben-Neriah Y, Karin M. Inflammation meets cancer, with NF-κB as the matchmaker. Nat Immunol. 2011;12(8):715.
Cheng A-S, Cheng Y-H, Chiou C-H, Chang T-L. Resveratrol upregulates Nrf2 expression to attenuate methylglyoxal-induced insulin resistance in Hep G2 cells. J Agric Food Chem. 2012;60(36):9180–7.
Ungvari Z, Bagi Z, Feher A, Recchia FA, Sonntag WE, Pearson K, et al. Resveratrol confers endothelial protection via activation of the antioxidant transcription factor Nrf2. Am J Phys Heart Circ Phys. 2010;299(1):H18–24.
Hsieh TC, Lu X, Wang Z, Wu JM. Induction of quinone reductase NQO1 by resveratrol in human K562 cells involves the antioxidant response element ARE and is accompanied by nuclear translocation of transcription factor Nrf2. Med Chem (Shariqah (United Arab Emirates)). 2006;2(3):275–85.
Kode A, Rajendrasozhan S, Caito S, Yang SR, Megson IL, Rahman I. Resveratrol induces glutathione synthesis by activation of Nrf2 and protects against cigarette smoke-mediated oxidative stress in human lung epithelial cells. Am J Physiol Lung Cell Mol Physiol. 2008;294(3):L478–88.
Baba N, Rubio M, Kenins L, Regairaz C, Woisetschlager M, Carballido JM, et al. The aryl hydrocarbon receptor (AhR) ligand VAF347 selectively acts on monocytes and naïve CD4+ Th cells to promote the development of IL-22-secreting Th cells. Hum Immunol. 2012;73(8):795–800.
Platzer B, Richter S, Kneidinger D, Waltenberger D, Woisetschläger M, Strobl H. Aryl hydrocarbon receptor activation inhibits in vitro differentiation of human monocytes and Langerhans dendritic cells. J Immunol. 2009;183(1):66–74.
Beedanagari SR, Bebenek I, Bui P, Hankinson O. Resveratrol inhibits dioxin-induced expression of human CYP1A1 and CYP1B1 by inhibiting recruitment of the aryl hydrocarbon receptor complex and RNA polymerase II to the regulatory regions of the corresponding genes. Toxicol Sci: Off J Soc Toxicol. 2009;110(1):61–7.
Jeong SK, Yang K, Park YS, Choi YJ, Oh SJ, Lee CW, et al. Interferon gamma induced by resveratrol analog, HS-1793, reverses the properties of tumor associated macrophages. Int Immunopharmacol. 2014;22(2):303–10.
Li T, Fan GX, Wang W, Li T, Yuan YK. Resveratrol induces apoptosis, influences IL-6 and exerts immunomodulatory effect on mouse lymphocytic leukemia both in vitro and in vivo. Int Immunopharmacol. 2007;7(9):1221–31.
Boocock DJ, Faust GE, Patel KR, Schinas AM, Brown VA, Ducharme MP, et al. Phase I dose escalation pharmacokinetic study in healthy volunteers of resveratrol, a potential cancer chemopreventive agent. Cancer Epidemiol Prevent Biomark. 2007;16(6):1246–52.
Wenzel E, Soldo T, Erbersdobler H, Somoza V. Bioactivity and metabolism of trans-resveratrol orally administered to Wistar rats. Mol Nutr Food Res. 2005;49(5):482–94.
Pervaiz S. Resveratrol-from the bottle to the bedside? Leuk Lymphoma. 2001;40(5–6):491–8.
Athar M, Back JH, Tang X, Kim KH, Kopelovich L, Bickers DR, et al. Resveratrol: a review of preclinical studies for human cancer prevention. Toxicol Appl Pharmacol. 2007;224(3):274–83.
Dörrie J, Gerauer H, Wachter Y, Zunino SJ. Resveratrol induces extensive apoptosis by depolarizing mitochondrial membranes and activating caspase-9 in acute lymphoblastic leukemia cells. Cancer Res. 2001;61(12):4731–9.
Clément M-V, Hirpara JL, Chawdhury S-H, Pervaiz S. Chemopreventive agent resveratrol, a natural product derived from grapes, triggers CD95 signaling-dependent apoptosis in human tumor cells. Blood. 1998;92(3):996–1002.
Falchetti R, Fuggetta MP, Lanzilli G, Tricarico M, Ravagnan G. Effects of resveratrol on human immune cell function. Life Sci. 2001;70(1):81–96.
Li Q, Huyan T, Ye L-J, Li J, Shi J-L, Huang Q-S. Concentration-dependent biphasic effects of resveratrol on human natural killer cells in vitro. J Agric Food Chem. 2014;62(45):10928–35.
Lu CC, Chen JK. Resveratrol enhances perforin expression and NK cell cytotoxicity through NKG2D-dependent pathways. J Cell Physiol. 2010;223(2):343–51.
Chen X, Trivedi PP, Ge B, Krzewski K, Strominger JL. Many NK cell receptors activate ERK2 and JNK1 to trigger microtubule organizing center and granule polarization and cytotoxicity. Proc Natl Acad Sci. 2007;104(15):6329–34.
Lu CC, Lai HC, Hsieh SC, Chen JK. Resveratrol ameliorates Serratia marcescens-induced acute pneumonia in rats. J Leukoc Biol. 2008;83(4):1028–37.
Hu L, Cao D, Li Y, He Y, Guo K. Resveratrol sensitized leukemia stem cell-like KG-1a cells to cytokine-induced killer cells-mediated cytolysis through NKG2D ligands and TRAIL receptors. Cancer Biol Ther. 2012;13(7):516–26.
Fulda S, Debatin K-M. Sensitization for tumor necrosis factor-related apoptosis-inducing ligand-induced apoptosis by the chemopreventive agent resveratrol. Cancer Res. 2004;64(1):337–46.
Fulda S, Debatin K-M. Resveratrol-mediated sensitisation to TRAIL-induced apoptosis depends on death receptor and mitochondrial signalling. Eur J Cancer. 2005;41(5):786–98.
Shankar S, Chen Q, Siddiqui I, Sarva K, Srivastava RK. Sensitization of TRAIL-resistant LNCaP cells by resveratrol (3, 4′, 5 tri-hydroxystilbene): molecular mechanisms and therapeutic potential. J Mol Signal. 2007;2(1):7.
Trung LQ, Espinoza JL, Takami A, Nakao S. Resveratrol induces cell cycle arrest and apoptosis in malignant NK cells via JAK2/STAT3 pathway inhibition. PLoS One. 2013;8(1):e55183.
Guan H, Singh NP, Singh UP, Nagarkatti PS, Nagarkatti M. Resveratrol prevents endothelial cells injury in high-dose interleukin-2 therapy against melanoma. PLoS One. 2012;7(4):e35650.
Takikawa O, Habara-Ohkubo A, Yoshida R. IFN-gamma is the inducer of indoleamine 2, 3-dioxygenase in allografted tumor cells undergoing rejection. J Immunol. 1990;145(4):1246–50.
Noh KT, Chae SH, Chun SH, Jung ID, Kang HK, Park Y-M. Resveratrol suppresses tumor progression via the regulation of indoleamine 2, 3-dioxygenase. Biochem Biophys Res Commun. 2013;431(2):348–53.
Jeong Y-I, Kim SW, Jung ID, Lee JS, Chang JH, Lee C-M, et al. Curcumin suppresses the induction of indoleamine 2, 3-dioxygenase by blocking the Janus-activated kinase-protein kinase Cδ-STAT1 signaling pathway in interferon-γ-stimulated murine dendritic cells. J Biol Chem. 2009;284(6):3700–8.
Alobaedi OH, Talib WH, Basheti IA. Antitumor effect of thymoquinone combined with resveratrol on mice transplanted with breast cancer. Asian Pac J Trop Med. 2017;10(4):400–8.
Lee-Chang C, Bodogai M, Martin-Montalvo A, Wejksza K, Sanghvi M, Moaddel R, et al. Inhibition of breast cancer metastasis by resveratrol-mediated inactivation of tumor-evoked regulatory B cells. J Immunol. 2013;191(8):4141–51.
Olkhanud PB, Damdinsuren B, Bodogai M, Gress RE, Sen R, Wejksza K, et al. Tumor-evoked regulatory B cells promote breast cancer metastasis by converting resting CD4+ T cells to T-regulatory cells. Cancer Res. 2011;71(10):3505–15.
Sengottuvelan M, Deeptha K, Nalini N. Influence of dietary resveratrol on early and late molecular markers of 1, 2-dimethylhydrazine–induced colon carcinogenesis. Nutrition. 2009;25(11):1169–76.
Araújo JR, Gonçalves P, Martel F. Chemopreventive effect of dietary polyphenols in colorectal cancer cell lines. Nutr Res. 2011;31(2):77–87.
Huang T-Y, Hsu C-W, Chang W-C, Wang M-Y, Wu J-F, Hsu Y-C. Demethoxycurcumin retards cell growth and induces apoptosis in human brain malignant glioma GBM 8401 cells. Evid Based Complement Alternat Med. 2012;2012:396573. https://doi.org/10.1155/2012/396573.
Li Y-B, Gao J-L, Zhong Z-F, Hoi P-M, Lee SM-Y, Wang Y-T. Bisdemethoxycurcumin suppresses MCF-7 cells proliferation by inducing ROS accumulation and modulating senescence-related pathways. Pharmacol Rep. 2013;65(3):700–9.
Basile V, Ferrari E, Lazzari S, Belluti S, Pignedoli F, Imbriano C. Curcumin derivatives: molecular basis of their anti-cancer activity. Biochem Pharmacol. 2009;78(10):1305–15.
Shehzad A, Lee J, Lee YS. Curcumin in various cancers. Biofactors. 2013;39(1):56–68.
Bemis DL, Katz AE, Buttyan R. Clinical trials of natural products as chemopreventive agents for prostate cancer. Expert Opin Investig Drugs. 2006;15(10):1191–200.
Goel A, Kunnumakkara AB, Aggarwal BB. Curcumin as “Curecumin”: from kitchen to clinic. Biochem Pharmacol. 2008;75(4):787–809.
Varalakshmi C, Ali AM, Pardhasaradhi B, Srivastava RM, Singh S, Khar A. Immunomodulatory effects of curcumin: in-vivo. Int Immunopharmacol. 2008;8(5):688–700.
Luo F, Song X, Zhang Y, Chu Y. Low-dose curcumin leads to the inhibition of tumor growth via enhancing CTL-mediated antitumor immunity. Int Immunopharmacol. 2011;11(9):1234–40.
Aggarwal BB, Gehlot P. Inflammation and cancer: how friendly is the relationship for cancer patients? Curr Opin Pharmacol. 2009;9(4):351–69.
Vallianou NG, Evangelopoulos A, Schizas N, Kazazis C. Potential anticancer properties and mechanisms of action of curcumin. Anticancer Res. 2015;35(2):645–51.
Sharma C, Kaur J, Shishodia S, Aggarwal BB, Ralhan R. Curcumin down regulates smokeless tobacco-induced NF-κB activation and COX-2 expression in human oral premalignant and cancer cells. Toxicology. 2006;228(1):1–15.
Dhandapani KM, Mahesh VB, Brann DW. Curcumin suppresses growth and chemoresistance of human glioblastoma cells via AP-1 and NFκB transcription factors. J Neurochem. 2007;102(2):522–38.
Milacic V, Banerjee S, Landis-Piwowar KR, Sarkar FH, Majumdar AP, Dou QP. Curcumin inhibits the proteasome activity in human colon cancer cells in vitro and in vivo. Cancer Res. 2008;68(18):7283–92.
Yang H, Landis-Piwowar K, Chen D, Milacic V, Dou Q. Natural compounds with proteasome inhibitory activity for cancer prevention and treatment. Curr Protein Peptide Sci. 2008;9(3):227–39.
Bharti AC, Shishodia S, Reuben JM, Weber D, Alexanian R, Raj-Vadhan S, et al. Nuclear factor–κB and STAT3 are constitutively active in CD138+ cells derived from multiple myeloma patients, and suppression of these transcription factors leads to apoptosis. Blood. 2004;103(8):3175–84.
Dhillon N, Wolff R, Abbruzzese J, Hong D, Camacho L, Li L, et al. Phase II clinical trial of curcumin in patients with advanced pancreatic cancer. J Clin Oncol. 2006;24(18_suppl):14151.
Aggarwal BB, Vijayalekshmi R, Sung B. Targeting inflammatory pathways for prevention and therapy of cancer: short-term friend, long-term foe. Clin Cancer Res. 2009;15(2):425–30.
Mackenzie GG, Queisser N, Wolfson ML, Fraga CG, Adamo AM, Oteiza PI. Curcumin induces cell-arrest and apoptosis in association with the inhibition of constitutively active NF-κB and STAT3 pathways in Hodgkin’s lymphoma cells. Int J Cancer. 2008;123(1):56–65.
Sandur SK, Deorukhkar A, Pandey MK, Pabón AM, Shentu S, Guha S, et al. Curcumin modulates the radiosensitivity of colorectal cancer cells by suppressing constitutive and inducible NF-κB activity. Int J Radiat Oncol Biol Phys. 2009;75(2):534–42.
Mukhopadhyay A, Bueso-Ramos C, Chatterjee D, Pantazis P, Aggarwal BB. Curcumin downregulates cell survival mechanisms in human prostate cancer cell lines. Oncogene. 2001;20(52):7597.
Bachmeier BE, Mohrenz IV, Mirisola V, Schleicher E, Romeo F, Höhneke C, et al. Curcumin downregulates the inflammatory cytokines CXCL1 and-2 in breast cancer cells via NFκB. Carcinogenesis. 2007;29(4):779–89.
Shao-Ling W, Ying L, Ying W, Yan-Feng C, Li-Xin N, Song-Tao L, et al. Curcumin, a potential inhibitor of up-regulation of TNF-alpha and IL-6 induced by palmitate in 3T3-L1 adipocytes through NF-kappaB and JNK pathway. Biomed Environ Sci. 2009;22(1):32–9.
Moon D-O, Jin C-Y, Lee J-D, Choi YH, Ahn S-C, Lee C-M, et al. Curcumin decreases binding of Shiga-like toxin-1B on human intestinal epithelial cell line HT29 stimulated with TNF-α and IL-1β: suppression of p38, JNK and NF-κB p65 as potential targets. Biol Pharm Bull. 2006;29(7):1470–5.
Menon VP, Sudheer AR. Antioxidant and anti-inflammatory properties of curcumin. In: Aggarwal BB, Surh Y-J, Shishodia S, editors. The molecular targets and therapeutic uses of curcumin in health and disease. New York: Springer; 2007. p. 105–25.
Shehzad A, Lee YS. Molecular mechanisms of curcumin action: signal transduction. Biofactors. 2013;39(1):27–36.
Onoda M, Inano H. Effect of curcumin on the production of nitric oxide by cultured rat mammary gland. Nitric Oxide. 2000;4(5):505–15.
Inano H, Onoda M, Inafuku N, Kubota M, Kamada Y, Osawa T, et al. Potent preventive action of curcumin on radiation-induced initiation of mammary tumorigenesis in rats. Carcinogenesis. 2000;21(10):1835–41.
Vaughan RA, Garcia-Smith R, Dorsey J, Griffith JK, Bisoffi M, Trujillo KA. Tumor necrosis factor alpha induces Warburg-like metabolism and is reversed by anti-inflammatory curcumin in breast epithelial cells. Int J Cancer. 2013;133(10):2504–10.
Han SS, Keum YS, Seo HJ, Surh YJ. Curcumin suppresses activation of NF-kappaB and AP-1 induced by phorbol ester in cultured human promyelocytic leukemia cells. J Biochem Mol Biol. 2002;35(3):337–42.
Jobin C, Bradham CA, Russo MP, Juma B, Narula AS, Brenner DA, et al. Curcumin blocks cytokine-mediated NF-kappa B activation and proinflammatory gene expression by inhibiting inhibitory factor I-kappa B kinase activity. J Immunol. 1999;163(6):3474–83.
Singh S, Aggarwal BB. Activation of transcription factor NF-kappa B is suppressed by curcumin (diferuloylmethane) [corrected]. J Biol Chem. 1995;270(42):24995–5000.
Yodkeeree S, Ampasavate C, Sung B, Aggarwal BB, Limtrakul P. Demethoxycurcumin suppresses migration and invasion of MDA-MB-231 human breast cancer cell line. Eur J Pharmacol. 2010;627(1–3):8–15.
Lynch CC, Matrisian LM. Matrix metalloproteinases in tumor–host cell communication. Differentiation. 2002;70(9–10):561–73.
Fingleton B. Matrix metalloproteinases: roles in cancer and metastasis. Front Biosci. 2006;11:479–91.
Fridman R, Toth M, Peña D, Mobashery S. Activation of progelatinase B (MMP-9) by gelatinase A (MMP-2). Cancer Res. 1995;55(12):2548–55.
Kim S, Kim Y, Youn H, Jung S. Abstract P1-10-01: curcumin suppresses MMP-9 expression via inhibition of PKCα/MAPKs and NF-κB/AP-1 activation in MCF-7 cells: AACR. Cancer Res. 2012;72(24 Supplement):P1-10-01. https://doi.org/10.1158/0008-5472.SABCS12-P1-10-01.
Pal S, Bhattacharyya S, Choudhuri T, Datta GK, Das T, Sa G. Amelioration of immune cell number depletion and potentiation of depressed detoxification system of tumor-bearing mice by curcumin. Cancer Detect Prev. 2005;29(5):470–8.
Bhattacharyya S, Hossain DMS, Mohanty S, Sen GS, Chattopadhyay S, Banerjee S, et al. Curcumin reverses T cell-mediated adaptive immune dysfunctions in tumor-bearing hosts. Cell Mol Immunol. 2010;7(4):306.
Churchill M, Chadburn A, Bilinski RT, Bertagnolli MM. Inhibition of intestinal tumors by curcumin is associated with changes in the intestinal immune cell profile. J Surg Res. 2000;89(2):169–75.
Gertsch J, Güttinger M, Heilmann J, Sticher O. Curcumin differentially modulates mRNA profiles in Jurkat T and human peripheral blood mononuclear cells. Bioorg Med Chem. 2003;11(6):1057–63.
Bhattacharyya S, Mandal D, Saha B, Sen GS, Das T, Sa G. Curcumin prevents tumor-induced T cell apoptosis through Stat-5a-mediated Bcl-2 induction. J Biol Chem. 2007;282(22):15954–64.
Liu C, Yu S, Zinn K, Wang J, Zhang L, Jia Y, et al. Murine mammary carcinoma exosomes promote tumor growth by suppression of NK cell function. J Immunol. 2006;176(3):1375–85.
Cong Y, Wang L, Konrad A, Schoeb T, Elson CO. Curcumin induces the tolerogenic dendritic cell that promotes differentiation of intestine-protective regulatory T cells. Eur J Immunol. 2009;39(11):3134–46.
Rogers J, Perkins I, Olphen AV, Burdash N, Klein TW, Friedman H. Epigallocatechin gallate modulates cytokine production by bone marrow-derived dendritic cells stimulated with lipopolysaccharide or muramyldipeptide, or infected with Legionella pneumophila. Exp Biol Med. 2005;230(9):645–51.
Bhattacharyya S, Md Sakib Hossain D, Mohanty S, Sankar Sen G, Chattopadhyay S, Banerjee S, et al. Curcumin reverses T cell-mediated adaptive immune dysfunctions in tumor-bearing hosts. Cell Mol Immunol. 2010;7(4):306–15.
Sakaguchi S, Miyara M, Costantino CM, Hafler DA. FOXP3+ regulatory T cells in the human immune system. Nat Rev Immunol. 2010;10(7):490.
Pandiyan P, Zheng L, Ishihara S, Reed J, Lenardo MJ. CD4+ CD25+ Foxp3+ regulatory T cells induce cytokine deprivation–mediated apoptosis of effector CD4+ T cells. Nat Immunol. 2007;8(12):1353.
Forward NA, Conrad DM, Power Coombs MR, Doucette CD, Furlong SJ, Lin TJ, et al. Curcumin blocks interleukin (IL)-2 signaling in T-lymphocytes by inhibiting IL-2 synthesis, CD25 expression, and IL-2 receptor signaling. Biochem Biophys Res Commun. 2011;407(4):801–6.
G-j Z, Lu Z-q, L-m T, Wu Z-s, Wang D-w, Zheng J-y, et al. Curcumin inhibits suppressive capacity of naturally occurring CD4+ CD25+ regulatory T cells in mice in vitro. Int Immunopharmacol. 2012;14(1):99–106.
Hossain D, Panda AK, Chakrabarty S, Bhattacharjee P, Kajal K, Mohanty S, et al. MEK inhibition prevents tumour-shed transforming growth factor-β-induced T-regulatory cell augmentation in tumour milieu. Immunology. 2015;144(4):561–73.
Hossain DMS, Panda AK, Manna A, Mohanty S, Bhattacharjee P, Bhattacharyya S, et al. FoxP3 acts as a cotranscription factor with STAT3 in tumor-induced regulatory T cells. Immunity. 2013;39(6):1057–69.
Bhattacharyya S, Mandal D, Sen GS, Pal S, Banerjee S, Lahiry L, et al. Tumor-induced oxidative stress perturbs nuclear factor-κB activity-augmenting tumor necrosis factor-α–mediated T-cell death: protection by curcumin. Cancer Res. 2007;67(1):362–70.
Stuelten CH, Byfield SD, Arany PR, Karpova TS, Stetler-Stevenson WG, Roberts AB. Breast cancer cells induce stromal fibroblasts to express MMP-9 via secretion of TNF-α and TGF-β. J Cell Sci. 2005;118(10):2143–53.
Chang Y-F, Chuang H-Y, Hsu C-H, Liu R-S, Gambhir SS, Hwang J-J. Immunomodulation of curcumin on adoptive therapy with T cell functional imaging in mice. Cancer Prevent Res (Phila). 2012;5(3):444–52.
Fallarino F, Grohmann U, Puccetti P. Indoleamine 2, 3-dioxygenase: from catalyst to signaling function. Eur J Immunol. 2012;42(8):1932–7.
Yu H, Pardoll D, Jove R. STATs in cancer inflammation and immunity: a leading role for STAT3. Nat Rev Cancer. 2009;9(11):798.
Blasius R, Reuter S, Henry E, Dicato M, Diederich M. Curcumin regulates signal transducer and activator of transcription (STAT) expression in K562 cells. Biochem Pharmacol. 2006;72(11):1547–54.
Teiten MH, Eifes S, Reuter S, Duvoix A, Dicato M, Diederich M. Gene expression profiling related to anti-inflammatory properties of curcumin in K562 leukemia cells. Ann N Y Acad Sci. 2009;1171(1):391–8.
Bill MA, Bakan C, Benson DM, Fuchs J, Young G, Lesinski GB. Curcumin induces proapoptotic effects against human melanoma cells and modulates the cellular response to immunotherapeutic cytokines. Mol Cancer Ther. 2009;8(9):2726–35.
Hutzen B, Friedman L, Sobo M, Lin L, Cen L, De Angelis S, et al. Curcumin analogue GO-Y030 inhibits STAT3 activity and cell growth in breast and pancreatic carcinomas. Int J Oncol. 2009;35(4):867–72.
Lin L, Hutzen B, Ball S, Foust E, Sobo M, Deangelis S, et al. New curcumin analogues exhibit enhanced growth-suppressive activity and inhibit AKT and signal transducer and activator of transcription 3 phosphorylation in breast and prostate cancer cells. Cancer Sci. 2009;100(9):1719–27.
Rajasingh J, Raikwar HP, Muthian G, Johnson C, Bright JJ. Curcumin induces growth-arrest and apoptosis in association with the inhibition of constitutively active JAK–STAT pathway in T cell leukemia. Biochem Biophys Res Commun. 2006;340(2):359–68.
Chakravarti N, Myers JN, Aggarwal BB. Targeting constitutive and interleukin-6-inducible signal transducers and activators of transcription 3 pathway in head and neck squamous cell carcinoma cells by curcumin (diferuloylmethane). Int J Cancer. 2006;119(6):1268–75.
Sandur SK, Ichikawa H, Pandey MK, Kunnumakkara AB, Sung B, Sethi G, et al. Role of pro-oxidants and antioxidants in the anti-inflammatory and apoptotic effects of curcumin (diferuloylmethane). Free Radic Biol Med. 2007;43(4):568–80.
Chung SS, Vadgama JV. Curcumin and epigallocatechin gallate inhibit the cancer stem cell phenotype via down-regulation of STAT3–NFκB signaling. Anticancer Res. 2015;35(1):39–46.
Charpentier MS, Whipple RA, Vitolo MI, Boggs AE, Slovic J, Thompson KN, et al. Curcumin targets breast cancer stem–like cells with microtentacles that persist in mammospheres and promote reattachment. Cancer Res. 2014;74(4):1250–60.
Shishodia S, Potdar P, Gairola CG, Aggarwal BB. Curcumin (diferuloylmethane) down-regulates cigarette smoke-induced NF-κB activation through inhibition of IκBα kinase in human lung epithelial cells: correlation with suppression of COX-2, MMP-9 and cyclin D1. Carcinogenesis. 2003;24(7):1269–79.
Rao CV. Regulation of COX and LOX by curcumin. In: Aggarwal BB, Surh Y-J, Shishodia S, editors. The molecular targets and therapeutic uses of curcumin in health and disease. New York: Springer; 2007. p. 213–26.
Swamy MV, Citineni B, Patlolla JM, Mohammed A, Zhang Y, Rao CV. Prevention and treatment of pancreatic cancer by curcumin in combination with omega-3 fatty acids. Nutr Cancer. 2008;60(S1):81–9.
Goel A, Boland CR, Chauhan DP. Specific inhibition of cyclooxygenase-2 (COX-2) expression by dietary curcumin in HT-29 human colon cancer cells. Cancer Lett. 2001;172(2):111–8.
Padhye S, Banerjee S, Chavan D, Pandye S, Swamy KV, Ali S, et al. Fluorocurcumins as cyclooxygenase-2 inhibitor: molecular docking, pharmacokinetics and tissue distribution in mice. Pharm Res. 2009;26(11):2438–45.
Lev-Ari S, Starr A, Vexler A, Karaush V, Loew V, Greif J, et al. Inhibition of pancreatic and lung adenocarcinoma cell survival by curcumin is associated with increased apoptosis, down-regulation of COX-2 and EGFR and inhibition of Erk1/2 activity. Anticancer Res. 2006;26(6B):4423–30.
Korutla L, Cheung JY, Medelsohn J, Kumar R. Inhibition of ligand-induced activation of epidermal growth factor receptor tyrosine phosphorylation by curcumin. Carcinogenesis. 1995;16(8):1741–5.
Bava SV, Puliappadamba VT, Deepti A, Nair A, Karunagaran D, Anto RJ. Sensitization of taxol-induced apoptosis by curcumin involves down-regulation of nuclear factor-κB and the serine/threonine kinase Akt and is independent of tubulin polymerization. J Biol Chem. 2005;280(8):6301–8.
Kang HJ, Lee SH, Price JE, Kim LS. Curcumin suppresses the paclitaxel-induced nuclear factor-κB in breast cancer cells and potentiates the growth inhibitory effect of paclitaxel in a breast cancer nude mice model. Breast J. 2009;15(3):223–9.
Du B, Jiang L, Xia Q, Zhong L. Synergistic inhibitory effects of curcumin and 5-fluorouracil on the growth of the human colon cancer cell line HT-29. Chemotherapy. 2006;52(1):23–8.
Deeb D, Jiang H, Gao X, Hafner MS, Wong H, Divine G, et al. Curcumin sensitizes prostate cancer cells to tumor necrosis factor–related apoptosis-inducing ligand/Apo2L by inhibiting nuclear factor-κB through suppression of IκBα phosphorylation. Mol Cancer Ther. 2004;3(7):803–12.
Deeb D, Xu YX, Jiang H, Gao X, Janakiraman N, Chapman RA, et al. Curcumin (diferuloyl-methane) enhances tumor necrosis factor-related apoptosis-inducing ligand-induced apoptosis in lncap prostate cancer cells1. Mol Cancer Ther. 2003;2(1):95–103.
Andrzejewski T, Deeb D, Gao X, Danyluk A, Arbab AS, Dulchavsky SA, et al. Therapeutic efficacy of curcumin/TRAIL combination regimen for hormone-refractory prostate cancer. Oncol Res Featuring Preclini Clin Cancer Therap. 2008;17(6):257–67.
Shankar S, Ganapathy S, Chen Q, Srivastava RK. Curcumin sensitizes TRAIL-resistant xenografts: molecular mechanisms of apoptosis, metastasis and angiogenesis. Mol Cancer. 2008;7(1):16.
Gabryšová L, Nicolson KS, Streeter HB, Verhagen J, Sabatos-Peyton CA, Morgan DJ, et al. Negative feedback control of the autoimmune response through antigen-induced differentiation of IL-10–secreting Th1 cells. J Exp Med. 2009;206(8):1755–67.
Shiri S, Alizadeh AM, Baradaran B, Farhanghi B, Shanehbandi D, Khodayari S, et al. Dendrosomal curcumin suppresses metastatic breast cancer in mice by changing m1/m2 macrophage balance in the tumor microenvironment. Asian Pac J Cancer Prev. 2014;16(9):3917–22.
McKinstry KK, Strutt TM, Buck A, Curtis JD, Dibble JP, Huston G, et al. IL-10 deficiency unleashes an influenza-specific Th17 response and enhances survival against high-dose challenge. J Immunol. 2009;182(12):7353–63.
Kwilasz A, Grace P, Serbedzija P, Maier S, Watkins L. The therapeutic potential of interleukin-10 in neuroimmune diseases. Neuropharmacology. 2015;96:55–69.
Sabat R, Grütz G, Warszawska K, Kirsch S, Witte E, Wolk K, et al. Biology of interleukin-10. Cytokine Growth Factor Rev. 2010;21(5):331–44.
Huang S, Ullrich SE, Bar-Eli M. Regulation of tumor growth and metastasis by interleukin-10: the melanoma experience. J Interf Cytokine Res. 1999;19(7):697–703.
Ng T, Britton GJ, Hill EV, Verhagen J, Burton BR, Wraith DC. Regulation of adaptive immunity; the role of interleukin-10. Front Immunol. 2013;4:129.
Deng Y, Verron E, Rohanizadeh R. Molecular mechanisms of anti-metastatic activity of curcumin. Anticancer Res. 2016;36(11):5639–47.
Wang X, Wang Q, Ives KL, Evers BM. Curcumin inhibits neurotensin-mediated interleukin-8 production and migration of HCT116 human colon cancer cells. Clin Cancer Res. 2006;12(18):5346–55.
Li L, Braiteh FS, Kurzrock R. Liposome-encapsulated curcumin. Cancer. 2005;104(6):1322–31.
Zhang H-G, Grizzle WE. Exosomes and cancer: a newly described pathway of immune suppression. Clin Cancer Res. 2011;17(5):959–64.
Zhang H-G, Kim H, Liu C, Yu S, Wang J, Grizzle WE, et al. Curcumin reverses breast tumor exosomes mediated immune suppression of NK cell tumor cytotoxicity. Biochimica et Biophysica Acta (BBA)-Mol Cell Res. 2007;1773(7):1116–23.
Zhang H-G, Kim H, Liu C, Yu S, Wang J, Grizzle WE, et al. Curcumin reverses breast tumor exosomes mediated immune suppression of NK cell tumor cytotoxicity. Biochimica et Biophysica Acta (BBA) – Mol Cell Res. 2007;1773(7):1116–23.
Gan R-Y, Li H-B, Sui Z-Q, Corke H. Absorption, metabolism, anti-cancer effect and molecular targets of epigallocatechin gallate (EGCG): An updated review. Crit Rev Food Sci Nutr. 2018;58(6):924–41.
Relat J, Blancafort A, Oliveras G, Cufí S, Haro D, Marrero PF, et al. Different fatty acid metabolism effects of (−)-epigallocatechin-3-gallate and C75 in adenocarcinoma lung cancer. BMC Cancer. 2012;12(1):280.
Sakamoto Y, Terashita N, Muraguchi T, Fukusato T, Kubota S. Effects of epigallocatechin-3-gallate (EGCG) on A549 lung cancer tumor growth and angiogenesis. Biosci Biotechnol Biochem. 2013;77(9):1799–803.
He L, Zhang E, Shi J, Li X, Zhou K, Zhang Q, et al. (−)-Epigallocatechin-3-gallate inhibits human papillomavirus (HPV)-16 oncoprotein-induced angiogenesis in non-small cell lung cancer cells by targeting HIF-1α. Cancer Chemother Pharmacol. 2013;71(3):713–25.
Wu H, Xin Y, Xiao Y, Zhao J. Low-dose docetaxel combined with (−)-epigallocatechin-3-gallate inhibits angiogenesis and tumor growth in nude mice with gastric cancer xenografts. Cancer Biother Radiopharm. 2012;27(3):204–9.
Zhu B-H, Chen H-Y, Zhan W-H, Wang C-Y, Cai S-R, Wang Z, et al. (-)-Epigallocatechin-3-gallate inhibits VEGF expression induced by IL-6 via Stat3 in gastric cancer. World J Gastroenterol: WJG. 2011;17(18):2315.
Zhu B-H, Zhan W-H, Li Z-R, Wang Z, He Y-L, Peng J-S, et al. (-)-Epigallocatechin-3-gallate inhibits growth of gastric cancer by reducing VEGF production and angiogenesis. World J Gastroenterol: WJG. 2007;13(8):1162.
Sharma C, Nusri QE-A, Begum S, Javed E, Rizvi TA, Hussain A. (-)-Epigallocatechin-3-gallate induces apoptosis and inhibits invasion and migration of human cervical cancer cells. Asian Pac J Cancer Prev. 2012;13(9):4815–22.
Shimizu M, Shirakami Y, Sakai H, Yasuda Y, Kubota M, Adachi S, et al. (−)-Epigallocatechin gallate inhibits growth and activation of the VEGF/VEGFR axis in human colorectal cancer cells. Chem Biol Interact. 2010;185(3):247–52.
Qin J, Wang Y, Bai Y, Yang K, Mao Q, Lin Y, et al. Epigallocatechin-3-gallate inhibits bladder cancer cell invasion via suppression of NF-κB-mediated matrix metalloproteinase-9 expression. Mol Med Rep. 2012;6(5):1040–4.
Ye F, Zhang G-H, Guan B-X, Xu X-C. Suppression of esophageal cancer cell growth using curcumin,(-)-epigallocatechin-3-gallate and lovastatin. World J Gastroenterol: WJG. 2012;18(2):126.
Shimizu M, Shirakami Y, Moriwaki H. Targeting receptor tyrosine kinases for chemoprevention by green tea catechin, EGCG. Int J Mol Sci. 2008;9(6):1034–49.
Yang F, De Villiers WJ, McClain CJ, Varilek GW. Green tea polyphenols block endotoxin-induced tumor necrosis factor-production and lethality in a murine model. J Nutr. 1998;128(12):2334–40.
Shirakami Y, Shimizu M, Tsurumi H, Hara Y, Tanaka T, Moriwaki H. EGCG and Polyphenon E attenuate inflammation-related mouse colon carcinogenesis induced by AOM plus DDS. Mol Med Rep. 2008;1(3):355–61.
Siddiqui IA, Shukla Y, Adhami VM, Sarfaraz S, Asim M, Hafeez BB, et al. Suppression of NFκB and its regulated gene products by oral administration of green tea polyphenols in an autochthonous mouse prostate cancer model. Pharm Res. 2008;25(9):2135–42.
Zhang L, Altuwaijri S, Deng F, Chen L, Lal P, Bhanot UK, et al. NF-κB regulates androgen receptor expression and prostate cancer growth. Am J Pathol. 2009;175(2):489–99.
Gupta S, Hastak K, Afaq F, Ahmad N, Mukhtar H. Essential role of caspases in epigallocatechin-3-gallate-mediated inhibition of nuclear factor kappaB and induction of apoptosis. Oncogene. 2004;23(14):2507.
Baud V, Karin M. Is NF-κB a good target for cancer therapy? Hopes and pitfalls. Nat Rev Drug Discov. 2009;8(1):33.
Dutta J, Fan Y, Gupta N, Fan G, Gelinas C. Current insights into the regulation of programmed cell death by NF-κB. Oncogene. 2006;25(51):6800.
Lee CH, Jeon Y-T, Kim S-H, Song Y-S. NF-κB as a potential molecular target for cancer therapy. Biofactors. 2007;29(1):19–35.
Butt MS, Sultan MT. Green tea: nature’s defense against malignancies. Crit Rev Food Sci Nutr. 2009;49(5):463–73.
Chen L, Zhang H-Y. Cancer preventive mechanismsof the green tea polyphenol (-)-epigallocatechin-3-gallate. Molecules. 2007;12(5):946–57.
Huang C, Ma W-Y, Hanenberger D, Cleary MP, Bowden GT, Dong Z. Inhibition of ultraviolet B-induced activator protein-1 (AP-1) activity by aspirin in AP-1-luciferase transgenic mice. J Biol Chem. 1997;272(42):26325–31.
Hussain T, Gupta S, Adhami VM, Mukhtar H. Green tea constituent epigallocatechin-3-gallate selectively inhibits COX-2 without affecting COX-1 expression in human prostate carcinoma cells. Int J Cancer. 2005;113(4):660–9.
Ahmad N, Adhami VM, Gupta S, Cheng P, Mukhtar H. Role of the retinoblastoma (PRB)–E2F/DP pathway in cancer chemopreventive effects of green tea polyphenol epigallocatechin-3-gallate. Arch Biochem Biophys. 2002;398(1):125–31.
Hong J, Smith TJ, Ho CT, August DA, Yang CS. Effects of purified green and black tea polyphenols on cyclooxygenase- and lipoxygenase-dependent metabolism of arachidonic acid in human colon mucosa and colon tumor tissues. Biochem Pharmacol. 2001;62(9):1175–83.
Ju J, Liu Y, Hong J, Huang MT, Conney AH, Yang CS. Effects of green tea and high-fat diet on arachidonic acid metabolism and aberrant crypt foci formation in an azoxymethane-induced colon carcinogenesis mouse model. Nutr Cancer. 2003;46(2):172–8.
Nomura M, Ma WY, Huang C, Yang CS, Bowden GT, Miyamoto K, et al. Inhibition of ultraviolet B-induced AP-1 activation by theaflavins from black tea. Mol Carcinog. 2000;28(3):148–55.
Chung JY, Huang C, Meng X, Dong Z, Yang CS. Inhibition of activator protein 1 activity and cell growth by purified green tea and black tea polyphenols in H-ras-transformed cells: structure-activity relationship and mechanisms involved. Cancer Res. 1999;59(18):4610–7.
Dong Z, Ma W, Huang C, Yang CS. Inhibition of tumor promoter-induced activator protein 1 activation and cell transformation by tea polyphenols, (-)-epigallocatechin gallate, and theaflavins. Cancer Res. 1997;57(19):4414–9.
Shimizu M, Deguchi A, Joe AK, McKoy JF, Moriwaki H, Weinstein IB. EGCG inhibits activation of HER3 and expression of cyclooxygenase-2 in human colon cancer cells. J Exp Ther Oncol. 2005;5(1):69–78.
Shimizu M, Deguchi A, Lim JT, Moriwaki H, Kopelovich L, Weinstein IB. (-)-Epigallocatechin gallate and polyphenon E inhibit growth and activation of the epidermal growth factor receptor and human epidermal growth factor receptor-2 signaling pathways in human colon cancer cells. Clin Cancer Res: Off J Am Assoc Cancer Res. 2005;11(7):2735–46.
Masuda M, Suzui M, Weinstein IB. Effects of epigallocatechin-3-gallate on growth, epidermal growth factor receptor signaling pathways, gene expression, and chemosensitivity in human head and neck squamous cell carcinoma cell lines. Clin Cancer Res. 2001;7(12):4220–9.
Masuda M, Suzui M, Lim JT, Deguchi A, Soh JW, Weinstein IB. Epigallocatechin-3-gallate decreases VEGF production in head and neck and breast carcinoma cells by inhibiting EGFR-related pathways of signal transduction. J Exp Ther Oncol. 2002;2(6):350–9.
See D, Mason S, Roshan R. Increased tumor necrosis factor alpha (TNF-α) and natural killer cell (NK) function using an integrative approach in late stage cancers. Immunol Investig. 2002;31(2):137–53.
Sen T, Dutta A, Chatterjee A. Epigallocatechin-3-gallate (EGCG) downregulates gelatinase-B (MMP-9) by involvement of FAK/ERK/NFκB and AP-1 in the human breast cancer cell line MDA-MB-231. Anti-Cancer Drugs. 2010;21(6):632–44.
Jang J-Y, Lee J-K, Jeon Y-K, Kim C-W. Exosome derived from epigallocatechin gallate treated breast cancer cells suppresses tumor growth by inhibiting tumor-associated macrophage infiltration and M2 polarization. BMC Cancer. 2013;13(1):421.
Shi J, Liu F, Zhang W, Liu X, Lin B, Tang X. Epigallocatechin-3-gallate inhibits nicotine-induced migration and invasion by the suppression of angiogenesis and epithelial-mesenchymal transition in non-small cell lung cancer cells. Oncol Rep. 2015;33(6):2972–80.
Singh T, Katiyar SK. Green tea polyphenol,(−)-epigallocatechin-3-gallate, induces toxicity in human skin cancer cells by targeting β-catenin signaling. Toxicol Appl Pharmacol. 2013;273(2):418–24.
Cheng C-W, Shieh P-C, Lin Y-C, Chen Y-J, Lin Y-H, Kuo D-H, et al. Indoleamine 2, 3-dioxygenase, an immunomodulatory protein, is suppressed by (−)-epigallocatechin-3-gallate via blocking of γ-interferon-induced JAK-PKC-δ-STAT1 signaling in human oral cancer cells. J Agric Food Chem. 2009;58(2):887–94.
Ogawa K, Hara T, Shimizu M, Nagano J, Ohno T, Hoshi M, et al. (-)-Epigallocatechin gallate inhibits the expression of indoleamine 2, 3-dioxygenase in human colorectal cancer cells. Oncol Lett. 2012;4(3):546–50.
Lindau D, Gielen P, Kroesen M, Wesseling P, Adema GJ. The immunosuppressive tumour network: myeloid-derived suppressor cells, regulatory T cells and natural killer T cells. Immunology. 2013;138(2):105–15.
Kusmartsev S, Gabrilovich DI. STAT1 signaling regulates tumor-associated macrophage-mediated T cell deletion. J Immunol. 2005;174(8):4880–91.
Curtsinger JM, Lins DC, Mescher MF. Signal 3 determines tolerance versus full activation of naive CD8 T cells: dissociating proliferation and development of effector function. J Exp Med. 2003;197(9):1141–51.
Kang TH, Lee JH, Song CK, Han HD, Shin BC, Pai SI, et al. Epigallocatechin-3-gallate enhances CD8+ T cell–mediated antitumor immunity induced by DNA vaccination. Cancer Res. 2007;67(2):802–11.
Croce M, Corrias MV, Orengo AM, Brizzolara A, Carlini B, Borghi M, et al. Transient depletion of CD4+ T cells augments IL-21-based immunotherapy of disseminated neuroblastoma in syngeneic mice. Int J Cancer. 2010;127(5):1141–50.
Kowalczyk A, Wierzbicki A, Gil M, Bambach B, Kaneko Y, Rokita H, et al. Induction of protective immune responses against NXS2 neuroblastoma challenge in mice by immunotherapy with GD2 mimotope vaccine and IL-15 and IL-21 gene delivery. Cancer Immunol Immunother. 2007;56(9):1443–58.
Meeran SM, Mantena SK, Katiyar SK. Prevention of ultraviolet radiation-induced immunosuppression by (−)-epigallocatechin-3-gallate in mice is mediated through interleukin 12-dependent DNA repair. Clin Cancer Res: Off J Am Assoc Cancer Res. 2006;12(7 Pt 1):2272–80.
Yoneyama S, Kawai K, Tsuno NH, Okaji Y, Asakage M, Tsuchiya T, et al. Epigallocatechin gallate affects human dendritic cell differentiation and maturation. J Allergy Clin Immunol. 2008;121(1):209–14.
Mantena SK, Roy AM, Katiyar SK. Epigallocatechin-3-gallate inhibits photocarcinogenesis through inhibition of angiogenic factors and activation of CD8+ T cells in tumors. Photochem Photobiol. 2005;81(5):1174–9.
Kim MK, Lee JW, Lee KY, Yang DC. Microbial conversion of major ginsenoside rb(1) to pharmaceutically active minor ginsenoside rd. J Microbiol (Seoul, Korea). 2005;43(5):456–62.
Lee J-J, Kwon H-K, Jung I-H, Cho Y-B, Kim K-J, Kim J-L. Anti-cancer activities of ginseng extract fermented with Phellinus linteus. Mycobiology. 2009;37(1):21–7.
Baek SH, Bae ON, Park JH. Recent methodology in ginseng analysis. J Ginseng Res. 2012;36(2):119–34.
Cui J, Garle M, Eneroth P, Bjorkhem I. What do commercial ginseng preparations contain? Lancet (London, England). 1994;344(8915):134.
Kim YS, Kang KS, Kim SI. Study on antitumor and immunomodulating activities of polysaccharide fractions fromPanax ginseng: comparison of effects of neutral and acidic polysaccharide fraction. Arch Pharm Res. 1990;13(4):330–7.
Yun T-K, Choi S-Y. Preventive effect of ginseng intake against various human cancers: a case-control study on 1987 pairs. Cancer Epidemiol Prevent Biomark. 1995;4(4):401–8.
Yun TK, Lee YS, Lee YH, Kim SI, Yun HY. Anticarcinogenic effect of Panax ginseng CA Meyer and identification of active compounds. J Korean Med Sci. 2001;16(Suppl):S6.
Wang C-Z, Zhang Z, Anderson S, Yuan C-S. Natural products and chemotherapeutic agents on cancer: prevention vs. treatment. Am J Chin Med. 2014;42(06):1555–8.
Shin J-Y, Song J-Y, Yun Y-S, Yang H-O, Rhee D-K, Pyo S. Immunostimulating effects of acidic polysaccharides extract of Panax ginseng on macrophage function. Immunopharmacol Immunotoxicol. 2002;24(3):469–82.
Choi H-S, Kim K-H, Sohn E, Park J-D, Kim B-O, Moon E-Y, et al. Red ginseng acidic polysaccharide (RGAP) in combination with IFN-γ results in enhanced macrophage function through activation of the NF-κB pathway. Biosci Biotechnol Biochem. 2008;72(7):1817–25.
Lee Y, Chung I, Lee I, Kim K, Hong W, Yun Y. Activation of multiple effector pathways of immune system by the antineoplastic immunostimulator acidic polysaccharide ginsan isolated from Panax ginseng. Anticancer Res. 1997;17(1A):323–31.
Kim K-H, Lee Y-S, Jung I-S, Park S-Y, Chung H-Y, Lee I-R, et al. Acidic polysaccharide from Panax ginseng, ginsan, induces Th1 cell and macrophage cytokines and generates LAK cells in synergy with rIL-2. Planta Med. 1998;64(02):110–5.
Park D, Bae D-K, Jeon JH, Lee J, Oh N, Yang G, et al. Immunopotentiation and antitumor effects of a ginsenoside Rg3-fortified red ginseng preparation in mice bearing H460 lung cancer cells. Environ Toxicol Pharmacol. 2011;31(3):397–405.
Jeon C, Kang S, Park S, Lim K, Hwang KW, Min H. T cell stimulatory effects of Korean Red Ginseng through modulation of myeloid-derived suppressor cells. J Ginseng Res. 2011;35(4):462.
Qi L-W, Wang C-Z, Yuan C-S. Ginsenosides from American ginseng: chemical and pharmacological diversity. Phytochemistry. 2011;72(8):689–99.
Keum Y-S, Han SS, Chun K-S, Park K-K, Park J-H, Lee SK, et al. Inhibitory effects of the ginsenoside Rg 3 on phorbol ester-induced cyclooxygenase-2 expression, NF-κB activation and tumor promotion. Mutat Res/Fundam Mol Mech Mutagen. 2003;523:75–85.
Shin Y-M, Jung H-J, Choi W-Y, Lim C-J. Antioxidative, anti-inflammatory, and matrix metalloproteinase inhibitory activities of 20 (S)-ginsenoside Rg3 in cultured mammalian cell lines. Mol Biol Rep. 2013;40(1):269–79.
Li L, Wang Y, Qi B, Yuan D, Dong S, Guo D, et al. Suppression of PMA-induced tumor cell invasion and migration by ginsenoside Rg1 via the inhibition of NF-κB-dependent MMP-9 expression. Oncol Rep. 2014;32(5):1779–86.
Kim T-W, Joh E-H, Kim B, Kim D-H. Ginsenoside Rg5 ameliorates lung inflammation in mice by inhibiting the binding of LPS to toll-like receptor-4 on macrophages. Int Immunopharmacol. 2012;12(1):110–6.
Huang J, Ding L, Shi D, Hu J, Qg Z, Gao S, et al. Transient receptor potential vanilloid-1 participates in the inhibitory effect of ginsenoside Rg1 on capsaicin-induced interleukin-8 and prostaglandin E2 production in HaCaT cells. J Pharm Pharmacol. 2012;64(2):252–8.
He B-C, Gao J-L, Luo X, Luo J, Shen J, Wang L, et al. Ginsenoside Rg3 inhibits colorectal tumor growth through the down-regulation of Wnt/ss-catenin signaling. Int J Oncol. 2011;38(2):437–45.
Liu T-G, Huang Y, Cui D-D, Huang X-B, Mao S-H, Ji L-L, et al. Inhibitory effect of ginsenoside Rg3 combined with gemcitabine on angiogenesis and growth of lung cancer in mice. BMC Cancer. 2009;9(1):250.
Ahuja A, Kim JH, Kim J-H, Yi Y-S, Cho JY. Functional role of ginseng-derived compounds in cancer. J Ginseng Res. 2018;42(3):248–54.
Wang C-Z, Cai Y, Anderson S, Yuan C-S. Ginseng metabolites on cancer chemoprevention: an angiogenesis link? Diseases. 2015;3(3):193–204.
Yue PY, Wong DY, Wu P, Leung P, Mak N, Yeung H, et al. The angiosuppressive effects of 20 (R)-ginsenoside Rg3. Biochem Pharmacol. 2006;72(4):437–45.
Zhou B, Wang J, Yan Z. Ginsenoside Rg3 attenuates hepatoma VEGF overexpression after hepatic artery embolization in an orthotopic transplantation hepatocellular carcinoma rat model. Onco Targets Ther. 2014;7:1945.
Wong AS, Che C-M, Leung K-W. Recent advances in ginseng as cancer therapeutics: a functional and mechanistic overview. Nat Prod Rep. 2015;32(2):256–72.
An I-S, An S, Kwon KJ, Kim YJ, Bae S. Ginsenoside Rh2 mediates changes in the microRNA expression profile of human non-small cell lung cancer A549 cells. Oncol Rep. 2013;29(2):523–8.
Szade A, Grochot-Przeczek A, Florczyk U, Jozkowicz A, Dulak J. Cellular and molecular mechanisms of inflammation-induced angiogenesis. IUBMB Life. 2015;67(3):145–59.
Fishbein AB, Wang C-Z, Li X-L, Mehendale SR, Sun S, Aung HH, et al. Asian ginseng enhances the anti-proliferative effect of 5-fluorouracil on human colorectal cancer: comparison between white and red ginseng. Arch Pharm Res. 2009;32(4):505–13.
Lin Y, Jiang D, Li Y, Han X, Yu D, Park JH, et al. Effect of sun ginseng potentiation on epirubicin and paclitaxel-induced apoptosis in human cervical cancer cells. J Ginseng Res. 2015;39(1):22–8.
Kim SJ, Kwak HJ, Kim DS, Choi HM, Sim JE, Kim SH, et al. Protective mechanism of Korean Red Ginseng in cisplatin-induced ototoxicity through attenuation of nuclear factor-κB and caspase-1 activation. Mol Med Rep. 2015;12(1):315–22.
Williams AW, Boileau TW-M, Zhou JR, Clinton SK, Erdman JW. β-Carotene modulates human prostate cancer cell growth and may undergo intracellular metabolism to retinol. J Nutr. 2000;130(4):728–32.
Namin MH, Ebrahimzadeh H, Ghareyazie B, Radjabian T, Gharavi S, Tafreshi N. In vitro expression of apocarotenoid genes in Crocus sativus L. Afr J Biotechnol. 2009;8(20):5378–82.
Chew BP, Park JS. Carotenoid action on the immune response. J Nutr. 2004;134(1):257S–61S.
Bolhassani A, Khavari A, Bathaie SZ. Saffron and natural carotenoids: biochemical activities and anti-tumor effects. Biochimica et Biophysica Acta (BBA) – Rev Cancer. 2014;1845(1):20–30.
Rao AV. Processed tomato products as a source of dietary lycopene: bioavailability and antioxidant properties. Can J Diet Pract Res. 2004;65(4):161–5.
Ivanov NI, Cowell SP, Brown P, Rennie PS, Guns ES, Cox ME. Lycopene differentially induces quiescence and apoptosis in androgen-responsive and -independent prostate cancer cell lines. Clin Nutr. 2007;26(2):252–63.
Prakash P, Russell RM, Krinsky NI. In vitro inhibition of proliferation of estrogen-dependent and estrogen-independent human breast cancer cells treated with carotenoids or retinoids. J Nutr. 2001;131(5):1574–80.
Huang C-S, Liao J-W, Hu M-L. Lycopene inhibits experimental metastasis of human hepatoma SK-Hep-1 cells in athymic nude mice. J Nutr. 2008;138(3):538–43.
Feng D, Ling W-H, Duan R-D. Lycopene suppresses LPS-induced NO and IL-6 production by inhibiting the activation of ERK, p38MAPK, and NF-κB in macrophages. Inflamm Res. 2010;59(2):115–21.
Rafi MM, Yadav PN, Reyes M. Lycopene inhibits LPS-induced proinflammatory mediator inducible nitric oxide synthase in mouse macrophage cells. J Food Sci. 2007;72(1):S069–74.
Tang F-Y, Pai M-H, Wang X-D. Consumption of lycopene inhibits the growth and progression of colon cancer in a mouse xenograft model. J Agric Food Chem. 2011;59(16):9011–21.
Lin M-C, Wang F-Y, Kuo Y-H, Tang F-Y. Cancer chemopreventive effects of lycopene: suppression of MMP-7 expression and cell invasion in human colon cancer cells. J Agric Food Chem. 2011;59(20):11304–18.
Katsuura S, Imamura T, Bando N, Yamanishi R. β-Carotene and β-cryptoxanthin but not lutein evoke redox and immune changes in RAW264 murine macrophages. Mol Nutr Food Res. 2009;53(11):1396–405.
Yasui Y, Hosokawa M, Mikami N, Miyashita K, Tanaka T. Dietary astaxanthin inhibits colitis and colitis-associated colon carcinogenesis in mice via modulation of the inflammatory cytokines. Chem Biol Interact. 2011;193(1):79–87.
McCarty MF. Minimizing the cancer-promotional activity of cox-2 as a central strategy in cancer prevention. Med Hypotheses. 2012;78(1):45–57.
Nagendraprabhu P, Sudhandiran G. Astaxanthin inhibits tumor invasion by decreasing extracellular matrix production and induces apoptosis in experimental rat colon carcinogenesis by modulating the expressions of ERK-2, NFkB and COX-2. Investig New Drugs. 2011;29(2):207–24.
Huang CS, Fan YE, Lin CY, Hu ML. Lycopene inhibits matrix metalloproteinase-9 expression and down-regulates the binding activity of nuclear factor-kappa B and stimulatory protein-1. J Nutr Biochem. 2007;18(7):449–56.
Palozza P, Serini S, Torsello A, Di Nicuolo F, Piccioni E, Ubaldi V, et al. Beta-carotene regulates NF-kappaB DNA-binding activity by a redox mechanism in human leukemia and colon adenocarcinoma cells. J Nutr. 2003;133(2):381–8.
Lee SJ, Bai SK, Lee KS, Namkoong S, Na HJ, Ha KS, et al. Astaxanthin inhibits nitric oxide production and inflammatory gene expression by suppressing I(kappa)B kinase-dependent NF-kappaB activation. Mol Cells. 2003;16(1):97–105.
Guruvayoorappan C, Kuttan G. Beta-carotene inhibits tumor-specific angiogenesis by altering the cytokine profile and inhibits the nuclear translocation of transcription factors in B16F-10 melanoma cells. Integr Cancer Ther. 2007;6(3):258–70.
Karas M, Amir H, Fishman D, Danilenko M, Segal S, Nahum A, et al. Lycopene interferes with cell cycle progression and insulin-like growth factor I signaling in mammary cancer cells. Nutr Cancer. 2000;36(1):101–11.
Palozza P, Parrone N, Catalano A, Simone R. Tomato lycopene and inflammatory cascade: basic interactions and clinical implications. Curr Med Chem. 2010;17(23):2547–63.
Huang C-S, Fan Y-E, Lin C-Y, Hu M-L. Lycopene inhibits matrix metalloproteinase-9 expression and down-regulates the binding activity of nuclear factor-kappa B and stimulatory protein-1. J Nutr Biochem. 2007;18(7):449–56.
Omenn GS, Goodman GE, Thornquist MD, Balmes J, Cullen MR, Glass A, et al. Effects of a combination of beta carotene and vitamin A on lung cancer and cardiovascular disease. N Engl J Med. 1996;334(18):1150–5.
Dhakshinamoorthy S, Jaiswal AK. Functional characterization and role of INrf2 in antioxidant response element-mediated expression and antioxidant induction of NAD (P) H: quinone oxidoreductase1 gene. Oncogene. 2001;20(29):3906.
Hayes JD, McMahon M. Molecular basis for the contribution of the antioxidant responsive element to cancer chemoprevention. Cancer Lett. 2001;174(2):103–13.
Kwak M-K, Egner PA, Dolan PM, Ramos-Gomez M, Groopman JD, Itoh K, et al. Role of phase 2 enzyme induction in chemoprotection by dithiolethiones. Mut Res/Fundam Mol Mech Mutagen. 2001;480:305–15.
Kong A-NT, Owuor E, Yu R, Hebbar V, Chen C, Hu R, et al. Induction of xenobiotic enzymes by the MAP kinase pathway and the antioxidant or electrophile response element (ARE/EpRE). Drug Metab Rev. 2001;33(3–4):255–71.
Xu C, Li CY-T, Kong A-NT. Induction of phase I, II and III drug metabolism/transport by xenobiotics. Arch Pharm Res. 2005;28(3):249.
Ben-Dor A, Steiner M, Gheber L, Danilenko M, Dubi N, Linnewiel K, et al. Carotenoids activate the antioxidant response element transcription system. Mol Cancer Ther. 2005;4(1):177–86.
Linnewiel K, Ernst H, Caris-Veyrat C, Ben-Dor A, Kampf A, Salman H, et al. Structure activity relationship of carotenoid derivatives in activation of the electrophile/antioxidant response element transcription system. Free Radic Biol Med. 2009;47(5):659–67.
Akiyama T, Ishida J, Nakagawa S, Ogawara H, Watanabe S-i, Itoh N, et al. Genistein, a specific inhibitor of tyrosine-specific protein kinases. J Biol Chem. 1987;262(12):5592–5.
Zhang Y, Song TT, Cunnick JE, Murphy PA, Hendrich S. Daidzein and genistein glucuronides in vitro are weakly estrogenic and activate human natural killer cells at nutritionally relevant concentrations. J Nutr. 1999;129(2):399–405.
Smit S, Szymańska E, Kunz I, Roldan VG, Tilborg MW, Weber P, et al. Nutrikinetic modeling reveals order of genistein phase II metabolites appearance in human plasma. Mol Nutr Food Res. 2014;58(11):2111–21.
Georgaki S, Skopeliti M, Tsiatas M, Nicolaou KA, Ioannou K, Husband A, et al. Phenoxodiol, an anticancer isoflavene, induces immunomodulatory effects in vitro and in vivo. J Cell Mol Med. 2009;13(9b):3929–38.
Guo TL, Chi RP, Hernandez DM, Auttachoat W, Zheng JF. Decreased 7, 12-dimethylbenz [a] anthracene-induced carcinogenesis coincides with the induction of antitumor immunities in adult female B6C3F1 mice pretreated with genistein. Carcinogenesis. 2007;28(12):2560–6.
Connolly JM, Liu XH, Rose DP. Effects of dietary menhaden oil, soy, and a cyclooxygenase inhibitor on human breast cancer cell growth and metastasis in nude mice. Nutr Cancer. 1997;29(1):48–54.
Singh AV, Franke AA, Blackburn GL, Zhou J-R. Soy phytochemicals prevent orthotopic growth and metastasis of bladder cancer in mice by alterations of cancer cell proliferation and apoptosis and tumor angiogenesis. Cancer Res. 2006;66(3):1851–8.
Vantyghem SA, Wilson SM, Postenka CO, Al-Katib W, Tuck AB, Chambers AF. Dietary genistein reduces metastasis in a postsurgical orthotopic breast cancer model. Cancer Res. 2005;65(8):3396–403.
Schleicher R, Lamartiniere C, Zheng M, Zhang M. The inhibitory effect of genistein on the growth and metastasis of a transplantable rat accessory sex gland carcinoma. Cancer Lett. 1999;136(2):195–201.
Iishi H, Tatsuta M, Baba M, Yano H, Sakai N, Akedo H. Genistein attenuates peritoneal metastasis of azoxymethane-induced intestinal adenocarcinomas in Wistar rats. Int J Cancer. 2000;86(3):416–20.
Li Y, Che M, Bhagat S, Ellis K-L, Kucuk O, Doerge DR, et al. Regulation of gene expression and inhibition of experimental prostate cancer bone metastasis by dietary genistein. Neoplasia. 2004;6(4):354–63.
Lee W-Y, Huang S-C, Tzeng C-C, Chang T-L, Hsu K-F. Alterations of metastasis-related genes identified using an oligonucleotide microarray of genistein-treated HCC1395 breast cancer cells. HNUC. 2007;58(2):239–46.
El Touny LH, Banerjee PP. Genistein induces the metastasis suppressor kangai-1 which mediates its anti-invasive effects in TRAMP cancer cells. Biochem Biophys Res Commun. 2007;361(1):169–75.
Lakshman M, Xu L, Ananthanarayanan V, Cooper J, Takimoto CH, Helenowski I, et al. Dietary genistein inhibits metastasis of human prostate cancer in mice. Cancer Res. 2008;68(6):2024–32.
Zhao R, Xiang N, Domann FE, Zhong W. Effects of selenite and genistein on G2/M cell cycle arrest and apoptosis in human prostate cancer cells. Nutr Cancer. 2009;61(3):397–407.
Su S-J, Chow N-H, Kung M-L, Hung T-C, Chang K-L. Effects of soy isoflavones on apoptosis induction and G2-M arrest in human hepatoma cells involvement of caspase-3 activation, Bcl-2 and Bcl-XL downregulation, and Cdc2 kinase activity. Nutr Cancer. 2003;45(1):113–23.
Myoung H, Hong SP, Yun PY, Lee JH, Kim MJ. Anti-cancer effect of genistein in oral squamous cell carcinoma with respect to angiogenesis and in vitro invasion. Cancer Sci. 2003;94(2):215–20.
Honndorf VS, Wiehr S, Rolle A-M, Schmitt J, Kreft L, Quintanilla-Martinez L, et al. Preclinical evaluation of the anti-tumor effects of the natural isoflavone genistein in two xenograft mouse models monitored by [18F] FDG,[18F] FLT, and [64Cu] NODAGA-cetuximab small animal PET. Oncotarget. 2016;7(19):28247.
Suzuki R, Kang Y, Li X, Roife D, Zhang R, Fleming JB. Genistein potentiates the antitumor effect of 5-fluorouracil by inducing apoptosis and autophagy in human pancreatic cancer cells. Anticancer Res. 2014;34(9):4685–92.
Zhou R-J, Yang X-Q, Wang D, Zhou Q, Xia L, Li M-X, et al. Anti-tumor effects of all-trans retinoic acid are enhanced by genistein. Cell Biochem Biophys. 2012;62(1):177–84.
Wu T-C, Lin Y-C, Chen H-L, Huang P-R, Liu S-Y, Yeh S-L. The enhancing effect of genistein on apoptosis induced by trichostatin A in lung cancer cells with wild type p53 genes is associated with upregulation of histone acetyltransferase. Toxicol Appl Pharmacol. 2016;292:94–102.
Jiang X, Patterson NM, Ling Y, Xie J, Helferich WG, Shapiro DJ. Low concentrations of the soy phytoestrogen genistein induce proteinase inhibitor 9 and block killing of breast cancer cells by immune cells. Endocrinology. 2008;149(11):5366–73.
Guo TL, McCay JA, Zhang LX, Brown RD, You L, Karrow NA, et al. Genistein modulates immune responses and increases host resistance to B16F10 tumor in adult female B6C3F1 mice. J Nutr. 2001;131(12):3251–8.
Bhaumik S, Jyothi MD, Khar A. Differential modulation of nitric oxide production by curcumin in host macrophages and NK cells. FEBS Lett. 2000;483(1):78–82.
Ferriola PC, Cody V, Middleton E Jr. Protein kinase C inhibition by plant flavonoids: kinetic mechanisms and structure-activity relationships. Biochem Pharmacol. 1989;38(10):1617–24.
Yu CS, Lai KC, Yang JS, Chiang JH, Lu CC, Wu CL, et al. Quercetin inhibited murine leukemia WEHI-3 cells in vivo and promoted immune response. Phytother Res. 2010;24(2):163–8.
Bae J-H, Kim J-Y, Kim M-J, Chang S-H, Park Y-S, Son C-H, et al. Quercetin enhances susceptibility to NK cell-mediated lysis of tumor cells through induction of NKG2D ligands and suppression of HSP70. J Immunother. 2010;33(4):391–401.
Russo M, Spagnuolo C, Tedesco I, Bilotto S, Russo GL. The flavonoid quercetin in disease prevention and therapy: facts and fancies. Biochem Pharmacol. 2012;83(1):6–15.
Gibellini L, Pinti M, Nasi M, Montagna JP, De Biasi S, Roat E, et al. Quercetin and cancer chemoprevention. Evid Based Complement Alternat Med: eCAM. 2011;2011:591356.
Chen X, Dong XS, Gao HY, Jiang YF, Jin YL, Chang YY, et al. Suppression of HSP27 increases the anti-tumor effects of quercetin in human leukemia U937 cells. Mol Med Rep. 2016;13(1):689–96.
Wang G, Zhang J, Liu L, Sharma S, Dong Q. Quercetin potentiates doxorubicin mediated antitumor effects against liver cancer through p53/Bcl-xl. PLoS One. 2012;7(12):e51764.
Murphy EA, Davis JM, McClellan JL, Carmichael MD. Quercetin’s effects on intestinal polyp multiplicity and macrophage number in the Apc min/+ mouse. Nutr Cancer. 2011;63(3):421–6.
Oršolić N, Bašić I. Water-soluble derivative of propolis and its polyphenolic compounds enhance tumoricidal activity of macrophages. J Ethnopharmacol. 2005;102(1):37–45.
BeMiller J, Bohn J. β-D-glucans as biological response modifiers: a review of structure-functional activity. Carbohydr Polym. 1995;28:3–14.
Yan J, Allendorf DJ, Brandley B. Yeast whole glucan particle (WGP) β-glucan in conjunction with antitumour monoclonal antibodies to treat cancer. Expert Opin Biol Ther. 2005;5(5):691–702.
Vetvicka V, Thornton BP, Ross GD. Soluble beta-glucan polysaccharide binding to the lectin site of neutrophil or natural killer cell complement receptor type 3 (CD11b/CD18) generates a primed state of the receptor capable of mediating cytotoxicity of iC3b-opsonized target cells. J Clin Invest. 1996;98(1):50–61.
Volman JJ, Ramakers JD, Plat J. Dietary modulation of immune function by β-glucans. Physiol Behav. 2008;94(2):276–84.
Inoue M, Tanaka Y, Sugita N, Yamasaki M, Yamanaka T, Minagawa J, et al. Improvement of long-term prognosis in patients with ovarian cancers by adjuvant sizofiran immunotherapy: a prospective randomized controlled study. Biotherapy. 1993;6(1):13–8.
Kodama N, Komuta K, Nanba H. Can maitake MD-fraction aid cancer patients? Altern Med Rev. 2002;7(3):236–9.
Gao Y, Tang W, Dai X, Gao H, Chen G, Ye J, et al. Effects of water-soluble Ganoderma lucidum polysaccharides on the immune functions of patients with advanced lung cancer. J Med Food. 2005;8(2):159–68.
Chen X, Hu Z-P, Yang X-X, Huang M, Gao Y, Tang W, et al. Monitoring of immune responses to a herbal immuno-modulator in patients with advanced colorectal cancer. Int Immunopharmacol. 2006;6(3):499–508.
Hong F, Hansen RD, Yan J, Allendorf DJ, Baran JT, Ostroff GR, et al. β-Glucan functions as an adjuvant for monoclonal antibody immunotherapy by recruiting tumoricidal granulocytes as killer cells. Cancer Res. 2003;63(24):9023–31.
Wang K-p, Q-l Z, Liu Y, Wang J, Cheng Y, Zhang Y. Structure and inducing tumor cell apoptosis activity of polysaccharides isolated from Lentinus edodes. J Agric Food Chem. 2013;61(41):9849–58.
Esua MF, Rauwald J-W. Novel bioactive maloyl glucans from Aloe vera gel: isolation, structure elucidation and in vitro bioassays. Carbohydr Res. 2006;341(3):355–64.
Mishra L-C, Singh BB, Dagenais S. Scientific basis for the therapeutic use of Withania somnifera (ashwagandha): a review. Altern Med Rev. 2000;5(4):334–46.
Agnihotri AP, Sontakke SD, Thawani VR, Saoji A, Goswami VS. Effects of Withania somnifera in patients of schizophrenia: a randomized, double blind, placebo controlled pilot trial study. Indian J Pharmacol. 2013;45(4):417–8.
Kour K, Pandey A, Suri K, Satti N, Gupta K, Bani S. Restoration of stress-induced altered T cell function and corresponding cytokines patterns by Withanolide A. Int Immunopharmacol. 2009;9(10):1137–44.
Malik F, Singh J, Khajuria A, Suri KA, Satti NK, Singh S, et al. A standardized root extract of Withania somnifera and its major constituent withanolide-A elicit humoral and cell-mediated immune responses by up regulation of Th1-dominant polarization in BALB/c mice. Life Sci. 2007;80(16):1525–38.
Malik F, Kumar A, Bhushan S, Mondhe DM, Pal HC, Sharma R, et al. Immune modulation and apoptosis induction: two sides of antitumoural activity of a standardised herbal formulation of Withania somnifera. Eur J Cancer. 2009;45(8):1494–509.
Inoue H, Tani K. Multimodal immunogenic cancer cell death as a consequence of anticancer cytotoxic treatments. Cell Death Differ. 2014;21(1):39.
Sinha P, Ostrand-Rosenberg S. Myeloid-derived suppressor cell function is reduced by Withaferin A, a potent and abundant component of Withania somnifera root extract. Cancer Immunol Immunother. 2013;62(11):1663–73.
Ching L-M, Baguley BC. Induction of natural killer cell activity by the antitumour compound flavone acetic acid (NSC 347 512). Eur J Cancer Clin Oncol. 1987;23(7):1047–50.
Urba WJ, Longo DL, Lombardo FA, Weiss RB. Enhancement of natural killer activity in human peripheral blood by flavone acetic acid. JNCI: J Nat Cancer Inst. 1988;80(7):521–5.
Wiltrout RH, Boyd MR, Back TC, Salup RR, Arthur JA, Hornung RL. Flavone-8-acetic acid augments systemic natural killer cell activity and synergizes with IL-2 for treatment of murine renal cancer. J Immunol. 1988;140(9):3261–5.
Triozzi PL, Rinehart JJ, Malspeis L, Young DC, Grever MR. Immunological effects of flavone acetic acid. Cancer Res. 1990;50(20):6483–5.
Ghosh AK, Mellor M, Prendiville J, Thatcher N. Recombinant interleukin-2 (rIL-2) with flavone acetic acid (FAA) in advanced malignant melanoma: immunological studies. Br J Cancer. 1990;61(3):471.
Galligioni E, Quaia M, Spada A, Crivellari D, Favar D, Sorio R, et al. Natural killer (NK) and lymphokine activated killer (LAK) cell activity in patients (PTS) treated with favone acetic acid (FAA). Ann Oncol. 1991;2(2):145–50.
Morré DJ, Chueh P-J, Yagiz K, Balicki A, Kim C, Morré DM. ECTO-NOX target for the anticancer isoflavene phenoxodiol. Oncol Res Featuring Preclin Clin Cancer Ther. 2006;16(7):299–312.
Delaney B, Phillips K, Buswell D, Mowry B, Nickels D, Cox D, et al. Immunotoxicity of a standardized citrus polymethoxylated flavone extract. Food Chem Toxicol. 2001;39(11):1087–94.
Saito T, Abe D, Nogata Y. Polymethoxylated flavones potentiate the cytolytic activity of NK leukemia cell line KHYG-1 via enhanced expression of granzyme B. Biochem Biophys Res Commun. 2015;456(3):799–803.
Birt D, Mitchell D, Gold B, Pour P, Pinch H. Inhibition of ultraviolet light induced skin carcinogenesis in SKH-1 mice by apigenin, a plant flavonoid. Anticancer Res. 1997;17(1A):85–91.
Gupta S, Afaq F, Mukhtar H. Involvement of nuclear factor-kappa B, Bax and Bcl-2 in induction of cell cycle arrest and apoptosis by apigenin in human prostate carcinoma cells. Oncogene. 2002;21(23):3727.
Liu L-Z, Fang J, Zhou Q, Hu X, Shi X, Jiang B-H. Apigenin inhibits expression of vascular endothelial growth factor and angiogenesis in human lung cancer cells: implication of chemoprevention of lung cancer. Mol Pharmacol. 2005;68(3):635–43.
Patel D, Shukla S, Gupta S. Apigenin and cancer chemoprevention: progress, potential and promise. Int J Oncol. 2007;30(1):233–45.
Shukla S, Gupta S. Apigenin and cancer chemoprevention. In: Watson R, Preedy V, editors. Bioactive foods in promoting health: fruits and vegetables. Massachusetts: Elsevier; 2010. p. 663–89.
Way T-D, Kao M-C, Lin J-K. Apigenin induces apoptosis through proteasomal degradation of HER2/neu in HER2/neu-overexpressing breast cancer cells via the phosphatidylinositol 3-kinase/Akt-dependent pathway. J Biol Chem. 2004;279(6):4479–89.
Coulerie P, Nour M, Maciuk A, Eydoux C, Guillemot J-C, Lebouvier N, et al. Structure-activity relationship study of biflavonoids on the Dengue virus polymerase DENV-NS5 RdRp. Planta Med. 2013;79(14):1313–8.
Hammer KD, Birt DF. Evidence for contributions of interactions of constituents to the anti-inflammatory activity of Hypericum perforatum. Crit Rev Food Sci Nutr. 2014;54(6):781–9.
Suzuki A, Matsunaga K, Mimaki Y, Sashida Y, Ohizumi Y. Properties of amentoflavone, a potent caffeine-like Ca2+ releaser in skeletal muscle sarcoplasmic reticulum. Eur J Pharmacol. 1999;372(1):97–102.
Guruvayoorappan C, Kuttan G. Amentoflavone, a biflavonoid from Biophytum sensitivum augments lymphocyte proliferation, natural killer cell and antibody dependent cellular cytotoxicity through enhanced production of IL-2 and IFN-γ and restrains serum sialic acid and gamma glutamyl transpeptidase production in tumor--bearing animals. J Exp Ther Oncol. 2007;6(4):285–95.
Vaid M, Singh T, Li A, Katiyar N, Sharma S, Elmets CA, et al. Proanthocyanidins inhibit UV-induced immunosuppression through IL-12–dependent stimulation of CD8+ effector T cells and inactivation of CD4+ T cells. Cancer Prev Res. 2011;4(2):238–47.
Park M-K, Park J-S, Cho M-L, Oh H-J, Heo Y-J, Woo Y-J, et al. Grape seed proanthocyanidin extract (GSPE) differentially regulates Foxp3+ regulatory and IL-17+ pathogenic T cell in autoimmune arthritis. Immunol Lett. 2011;135(1–2):50–8.
Naganawa R, Iwata N, Ishikawa K, Fukuda H, Fujino T, Suzuki A. Inhibition of microbial growth by ajoene, a sulfur-containing compound derived from garlic. Appl Environ Microbiol. 1996;62(11):4238–42.
Schafer GH, Kaschula C. The immunomodulation and anti-inflammatory effects of garlic organosulfur compounds in cancer chemoprevention. Anti-Cancer Agents Med Chem (Formerly Current Medicinal Chemistry-Anti-Cancer Agents). 2014;14(2):233–40.
Kyo E, Uda N, Kasuga S, Itakura Y. Immunomodulatory effects of aged garlic extract. J Nutr. 2001;131(3):1075S–9S.
Chang H-P, Huang S-Y, Chen Y-H. Modulation of cytokine secretion by garlic oil derivatives is associated with suppressed nitric oxide production in stimulated macrophages. J Agric Food Chem. 2005;53(7):2530–4.
Cheung KL, Khor TO, Kong A-N. Synergistic effect of combination of phenethyl isothiocyanate and sulforaphane or curcumin and sulforaphane in the inhibition of inflammation. Pharm Res. 2009;26(1):224–31.
Hong F, Freeman ML, Liebler DC. Identification of sensor cysteines in human Keap1 modified by the cancer chemopreventive agent sulforaphane. Chem Res Toxicol. 2005;18(12):1917–26.
Kang J, Teng C, Wee A, Chen F. Effect of capsaicin and chilli on ethanol induced gastric mucosal injury in the rat. Gut. 1995;36(5):664–9.
Cao S, Chen H, Xiang S, Hong J, Weng L, Zhu H, et al. Anti-cancer effects and mechanisms of capsaicin in chili peppers. Am J Plant Sci. 2015;6(19):3075.
Ito K, Nakazato T, Yamato K, Miyakawa Y, Yamada T, Hozumi N, et al. Induction of apoptosis in leukemic cells by homovanillic acid derivative, capsaicin, through oxidative stress: implication of phosphorylation of p53 at Ser-15 residue by reactive oxygen species. Cancer Res. 2004;64(3):1071–8.
Sánchez AM, Malagarie-Cazenave S, Olea N, Vara D, Chiloeches A, Díaz-Laviada I. Apoptosis induced by capsaicin in prostate PC-3 cells involves ceramide accumulation, neutral sphingomyelinase, and JNK activation. Apoptosis. 2007;12(11):2013–24.
Lu H-F, Chen Y-L, Yang J-S, Yang Y-Y, Liu J-Y, Hsu S-C, et al. Antitumor activity of capsaicin on human colon cancer cells in vitro and colo 205 tumor xenografts in vivo. J Agric Food Chem. 2010;58(24):12999–3005.
Min J-K, Han K-Y, Kim E-C, Kim Y-M, Lee S-W, Kim O-H, et al. Capsaicin inhibits in vitro and in vivo angiogenesis. Cancer Res. 2004;64(2):644–51.
Oyagbemi A, Saba A, Azeez O. Capsaicin: a novel chemopreventive molecule and its underlying molecular mechanisms of action. Indian J Cancer. 2010;47(1):53.
Hale L, Haynes B. Bromelain treatment of human T cells removes CD44, CD45RA, E2/MIC2, CD6, CD7, CD8, and Leu 8/LAM1 surface molecules and markedly enhances CD2-mediated T cell activation. J Immunol. 1992;149(12):3809–16.
Engwerda CR, Andrew D, Ladhams A, Mynott TL. Bromelain modulates T cell and B cell immune responses in vitro and in vivo. Cell Immunol. 2001;210(1):66–75.
Onken JE, Greer PK, Calingaert B, Hale LP. Bromelain treatment decreases secretion of pro-inflammatory cytokines and chemokines by colon biopsies in vitro. Clin Immunol. 2008;126(3):345–52.
Desser L, Rehberger A, Paukovits W. Proteolytic enzymes and amylase induce cytokine production in human peripheral blood mononuclear cells in vitro. Cancer Biother Radiopharm. 1994;9(3):253–63.
Engwerda CR, Andrew D, Murphy M, Mynott TL. Bromelain activates murine macrophages and natural killer cells in vitro. Cell Immunol. 2001;210(1):5–10.
Zavadova E, Desser L, Mohr T. Stimulation of reactive oxygen species production and cytotoxicity in human neutrophils in vitro and after oral administration of a polyenzyme preparation. Cancer Biother Radiopharm. 1995;10(2):147–52.
Kalra N, Bhui K, Roy P, Srivastava S, George J, Prasad S, et al. Regulation of p53, nuclear factor κB and cyclooxygenase-2 expression by bromelain through targeting mitogen-activated protein kinase pathway in mouse skin. Toxicol Appl Pharmacol. 2008;226(1):30–7.
Guimarães-Ferreira CA, Rodrigues EG, Mortara RA, Cabral H, Serrano FA, Ribeiro-dos-Santos R, et al. Antitumor effects in vitro and in vivo and mechanisms of protection against melanoma B16F10-Nex2 cells by fastuosain, a cysteine proteinase from Bromelia fastuosa. Neoplasia. 2007;9(9):723–33.
MüLLER A, Barat S, Chen X, Bui KC, Bozko P, Malek NP, et al. Comparative study of antitumor effects of bromelain and papain in human cholangiocarcinoma cell lines. Int J Oncol. 2016;48(5):2025–34.
Mayer S, Zur Hausen A, Watermann DO, Stamm S, Jäger M, Gitsch G, et al. Increased soluble CD44 concentrations are associated with larger tumor size and lymph node metastasis in breast cancer patients. J Cancer Res Clin Oncol. 2008;134(11):1229.
Tysnes BB, Maurert HR, Porwol T, Probst B, Bjerkvig R, Hoover F. Bromelain reversibly inhibits invasive properties of glioma cells. Neoplasia. 2001;3(6):469–79.
Pisha E, Chai H, Lee I-S, Chagwedera TE, Farnsworth NR, Cordell GA, et al. Discovery of betulinic acid as a selective inhibitor of human melanoma that functions by induction of apoptosis. Nat Med. 1995;1(10):1046.
Fulda S, Friesen C, Los M, Scaffidi C, Mier W, Benedict M, et al. Betulinic acid triggers CD95 (APO-1/Fas)-and p53-independent apoptosis via activation of caspases in neuroectodermal tumors. Cancer Res. 1997;57(21):4956–64.
Wick W, Grimmel C, Wagenknecht B, Dichgans J, Weller M. Betulinic acid-induced apoptosis in glioma cells: a sequential requirement for new protein synthesis, formation of reactive oxygen species, and caspase processing. J Pharmacol Exp Ther. 1999;289(3):1306–12.
Ji Z-N, Ye W-C, Liu G-G, Hsiao WLW. 23-Hydroxybetulinic acid-mediated apoptosis is accompanied by decreases in bcl-2 expression and telomerase activity in HL-60 cells. Life Sci. 2002;72(1):1–9.
Thurnher D, Turhani D, Pelzmann M, Wannemacher B, Knerer B, Formanek M, et al. Betulinic acid: a new cytotoxic compound against malignant head and neck cancer cells. Head Neck. 2003;25(9):732–40.
Jung GR, Kim KJ, Choi CH, Lee TB, Han SI, Han HK, et al. Effect of Betulinic acid on anticancer drug-resistant colon cancer cells. Basic Clin Pharmacol Toxicol. 2007;101(4):277–85.
Zdzisiñska B, Rzeski W, Paduch R, Szuster-Ciesielska A, Kaczor J, Wejksza K, et al. Differential effect of betulin and betulinic acid on cytokine production in human whole blood cell cultures. Pol J Pharmacol. 2003;55(2):235–8.
Viji V, Shobha B, Kavitha SK, Ratheesh M, Kripa K, Helen A. Betulinic acid isolated from Bacopa monniera (L.) Wettst suppresses lipopolysaccharide stimulated interleukin-6 production through modulation of nuclear factor-κB in peripheral blood mononuclear cells. Int Immunopharmacol. 2010;10(8):843–9.
Liu WY, Tzeng T-F, Liu I-M. Zerumbone, a bioactive sesquiterpene, ameliorates diabetes-induced retinal microvascular damage through inhibition of Phospho-p38 mitogen-activated protein kinase and nuclear factor-κB pathways. Molecules. 2016;21(12):1708.
Shieh Y-H, Huang H-M, Wang C-C, Lee C-C, Fan C-K, Lee Y-L. Zerumbone enhances the Th1 response and ameliorates ovalbumin-induced Th2 responses and airway inflammation in mice. Int Immunopharmacol. 2015;24(2):383–91.
Murakami A, Takahashi M, Jiwajinda S, Koshimizu K, Ohigashi H. Identification of zerumbone in Zingiber zerumbet Smith as a potent inhibitor of 12-O-tetradecanoylphorbol-13-acetate-induced Epstein-Barr virus activation. Biosci Biotechnol Biochem. 1999;63(10):1811–2.
Abdelwahab SI, Abdul AB, Mohan S, Taha MME, Syam S, Ibrahim MY, et al. Zerumbone induces apoptosis in T-acute lymphoblastic leukemia cells. Leuk Res. 2011;35(2):268–71.
Abdelwahab SI, Abdul AB, Devi N, Ehassan Taha MM, Al-zubairi AS, Mohan S, et al. Regression of cervical intraepithelial neoplasia by zerumbone in female Balb/c mice prenatally exposed to diethylstilboestrol: involvement of mitochondria-regulated apoptosis. Exp Toxicol Pathol. 2010;62(5):461–9.
Shamoto T, Matsuo Y, Shibata T, Tsuboi K, Nagasaki T, Takahashi H, et al. Zerumbone inhibits angiogenesis by blocking NF-κB activity in pancreatic cancer. Pancreas. 2014;43(3):396–404.
Murakami A, Tanaka T, Lee JY, Surh YJ, Kim HW, Kawabata K, et al. Zerumbone, a sesquiterpene in subtropical ginger, suppresses skin tumor initiation and promotion stages in ICR mice. Int J Cancer. 2004;110(4):481–90.
Kim M, Miyamoto S, Yasui Y, Oyama T, Murakami A, Tanaka T. Zerumbone, a tropical ginger sesquiterpene, inhibits colon and lung carcinogenesis in mice. Int J Cancer. 2009;124(2):264–71.
Alwi S, Sakinah S, Nallappan M, Pihie L, Hawariah A. Zerumbone exerts antiproliferative activity via apoptosis on HepG2 cells. Malaysian J Biochem Mol Biol. 2007;15(1):19–23.
Park EJ, Pezzuto JM. Botanicals in cancer chemoprevention. Cancer Metastasis Rev. 2002;21(3–4):231–55.
Lindqvist C, Bobrowska-Hägerstrand M, Mrówczyńska L, Engblom C, Hägerstrand H. Potentiation of natural killer cell activity with myricetin. Anticancer Res. 2014;34(8):3975–9.
Kim JH, Lee JK. Naringenin enhances NK cell lysis activity by increasing the expression of NKG2D ligands on Burkitt’s lymphoma cells. Arch Pharm Res. 2015;38(11):2042–8.
Dixon P, Veit B. The effects of chrysin, a Passiflora incarnata extract, on natural killer cell activity in male Sprague-Dawley rats undergoing abdominal surgery. AANA J. 2008;76(2):113.
Lin C-C, Yu C-S, Yang J-S, Lu C-C, Chiang J-H, Lin J-P, et al. Chrysin, a natural and biologically active flavonoid, influences a murine leukemia model in vivo through enhancing populations of T-and B-cells, and promoting macrophage phagocytosis and NK cell cytotoxicity. In Vivo. 2012;26(4):665–70.
Depypere H, Bracke M, Boterberg T, Mareel M, Nuytinck M, Vennekens K, et al. Inhibition of tamoxifen’s therapeutic benefit by tangeretin in mammary cancer. Eur J Cancer. 2000;36:73.
Vanhoecke BW, Delporte F, Van Braeckel E, Heyerick A, Depypere HT, Nuytinck M, et al. A safety study of oral tangeretin and xanthohumol administration to laboratory mice. In Vivo. 2005;19(1):103–7.
Lakshmi A, Subramanian S. Chemotherapeutic effect of tangeretin, a polymethoxylated flavone studied in 7, 12-dimethylbenz(a)anthracene induced mammary carcinoma in experimental rats. Biochimie. 2014;99:96–109.
Morley KL, Ferguson PJ, Koropatnick J. Tangeretin and nobiletin induce G1 cell cycle arrest but not apoptosis in human breast and colon cancer cells. Cancer Lett. 2007;251(1):168–78.
Pan M-H, Chen W-J, Lin-Shiau S-Y, Ho C-T, Lin J-K. Tangeretin induces cell-cycle G1 arrest through inhibiting cyclin-dependent kinases 2 and 4 activities as well as elevating Cdk inhibitors p21 and p27 in human colorectal carcinoma cells. Carcinogenesis. 2002;23(10):1677–84.
Gharagozloo M, Velardi E, Bruscoli S, Agostini M, Di Sante M, Donato V, et al. Silymarin suppress CD4+ T cell activation and proliferation: effects on NF-κB activity and IL-2 production. Pharmacol Res. 2010;61(5):405–9.
Gharagozloo M, Amirghofran Z. Effects of silymarin on the spontaneous proliferation and cell cycle of human peripheral blood leukemia T cells. J Cancer Res Clin Oncol. 2007;133(8):525–32.
Johnson VJ, He Q, Osuchowski MF, Sharma RP. Physiological responses of a natural antioxidant flavonoid mixture, silymarin, in BALB/c mice. Planta Med. 2003;69(01):44–9.
Gude R, Menon L, Rao S. Effect of Caffeine, a xanthine derivative, in the inhibition of experimental lung metastasis induced by B16F10 melanoma cells. J Exp Clin Cancer Res: CR. 2001;20(2):287–92.
Yang H, Rouse J, Lukes L, Lancaster M, Veenstra T, Zhou M, et al. Caffeine suppresses metastasis in a transgenic mouse model: a prototype molecule for prophylaxis of metastasis. Clin Exp Metastasis. 2005;21(8):719–35.
Kapoor V, Aggarwal S, Das SN. 6-Gingerol mediates its anti tumor activities in human oral and cervical cancer cell lines through apoptosis and cell cycle arrest. Phytother Res. 2016;30(4):588–95.
Kim E-C, Min J-K, Kim T-Y, Lee S-J, Yang H-O, Han S, et al. [6]-Gingerol, a pungent ingredient of ginger, inhibits angiogenesis in vitro and in vivo. Biochem Biophys Res Commun. 2005;335(2):300–8.
Alonso-Castro AJ, Ortiz-Sánchez E, Domínguez F, Arana-Argáez V, Juárez-Vázquez MC, Chávez M, et al. Antitumor and immunomodulatory effects of Justicia spicigera Schltdl (Acanthaceae). J Ethnopharmacol. 2012;141(3):888–94.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ghaedi, E., Rezaei, N., Mahmoudi, M. (2019). Nutrition, Immunity, and Cancer. In: Mahmoudi, M., Rezaei, N. (eds) Nutrition and Immunity. Springer, Cham. https://doi.org/10.1007/978-3-030-16073-9_12
Download citation
DOI: https://doi.org/10.1007/978-3-030-16073-9_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-16072-2
Online ISBN: 978-3-030-16073-9
eBook Packages: MedicineMedicine (R0)