Abstract
Childbirth-related trauma is a recurrent and widespread topic due to the disorders it can trigger, such as urinary and/or anal incontinence, and pelvic organ prolapse, affecting women at various levels. Pelvic floor dysfunction often results from weakening or direct damage to the pelvic floor muscles (PFM) or connective tissue, and vaginal delivery is considered the primary risk factor. Elucidating the normal labor mechanisms and the impact of vaginal delivery in PFM can lead to the development of preventive and therapeutic strategies to minimize the most common injuries. By providing some understanding of the function of the pelvic floor during childbirth, the existing biomechanical models attempt to respond to this problem. These models have been used to estimate the mechanical changes on PFM during delivery, to analyze fetal descent, the effect of the fetal head molding, and delivery techniques that potentially contribute to facilitating labor and reducing the risk of muscle injury.
Biomechanical models of childbirth should be sufficiently well-informed and functional for personalized planning of birth and obstetric interventions. Some challenges to be addressed with a focus on customization will be discussed including the in vivo acquisition of individual-specific pelvic floor mechanical properties.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Pregnancy and childbirth are very complex processes, and sometimes with harmful consequences for the woman and/or the newborn. During pregnancy, the pelvic floor function (sphincteric—regulating storage and evacuation of urine and stool; support and stability of the pelvic organs, and sexual) may be compromised due to the effect of hormonal changes and increased intra-abdominal pressure. In vaginal delivery, the deformations to which the pelvic floor muscles (PFM) are subjected, which may even exceed the physiological limits, can lead to muscle ruptures which in turn lead to pelvic floor disorders [1]. In fact, vaginal delivery is the most implicated epidemiological risk factor for the development of pelvic floor dysfunction (PFD). Dysfunction of the pelvic floor complex can result in a wide range of symptoms including urinary incontinence (UI), fecal incontinence (FI), and pelvic organ prolapse (POP). According to the International Urogynecological Association (IUGA)/International Continence Society (ICS) terminology, UI is the complaint of any involuntary leakage of urine, FI is the complaint of involuntary loss of feces, and POP is the descent of one or more of the anterior vaginal wall, posterior vaginal wall, the uterus (cervix) or the apex of the vagina [2].
Due to its high prevalence, PFD represents a major public health problem, considerably decreasing women’s quality of life [3, 4]. The number of women affected with PFD is forecast to widen to 43.8 million in 2050, representing an increase of more than 50% compared to 2010 (Fig. 1) [3]. Consequently, it is expected that the number of women undergoing surgery for PFD correction continues to increase, with a reoperation rate of 30%, and with an increasingly shorter time interval between repeated procedures [5].
According to De Souza et al. [6], about 54% of women have physiological or normal vaginal delivery, 21% undergo an instrumental delivery, and the remaining 25% give birth by cesarean section. Vaginal delivery is a perfect time to apply preventive strategies. Avoiding damage during vaginal delivery may prevent PFD from developing. Therefore, elucidating the pregnancy mechanisms and the impact of vaginal delivery on the PFM using pelvic floor biomechanics can lead to the development of preventive and therapeutic strategies to minimize the most common injuries.
2 Mechanism of Normal Labor
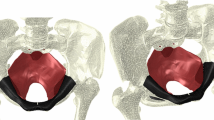
Labor is defined as regular uterine contractions that lead to progressive effacement and dilation of the cervix, resulting in delivery of the fetus, amniotic fluid, placenta, and membranes via expulsion through the vagina. The evolution of the vaginal delivery is dictated by the complex interaction between three essential factors, the uterine activity (the power—triple descending gradient), the maternal pelvis (the passage), and the fetus (the passenger). Computational models have become an interesting alternative to elucidate the labor mechanisms, allowing to evaluate the influence of individual features (Fig. 2). Uterine activity is characterized by the frequency, duration, and intensity of the contractions, and resting tone. The contractions start with an intensity of 1–2 kPa, increasing to 7 kPa as the cervix approaches full dilation, reaching 10–20 kPa with maternal pushing effort [7]. A successful vaginal delivery is dependent on an adequate pattern of uterine contractions.
Regarding the passage, the pelvis has three important diameters: the pelvic inlet, diagonal conjugate, and pelvic outlet (Fig. 3). The pelvic inlet has a wide transverse diameter of approximately 13 cm. It is the distance from the sacral promontory to the upper border of the pubic symphysis. The diagonal conjugate is the most easily and commonly assessed. It is measured from the lower border of the pubic symphysis to sacral promontory (around 11.5 cm). The pelvic outlet has a wide anterior–posterior diameter and is defined by the distance between the inferior aspect of the pubic symphysis to the coccyx. Laterally, the pelvic outlet is defined by the interspinous diameter which is the most limiting transverse diameter.
The pelvic inlet and outlet define the distance and the series of important maneuvers through which the fetus must pass while descending through the pelvis. Different pelvic shapes can restrain the position and the cardinal movements of the fetus [8]. Cardinal movements are described sequentially, although labor and delivery occur continuously. Moreover, not all fetuses follow the same pattern, as it is dependent on the presenting part. At the onset of labor, the position of the fetus in relation to the birth canal is critical to the route of delivery. The most common situation is with the fetus in a longitudinal lie with a cephalic presentation and a well-flexed attitude, described as a vertex presentation (smallest diameter presented—the suboccipitobregmatic diameter). A computational finite element model used to analyze the influence of fetal head flexion during vaginal delivery (represented by θ in the Fig. 4) suggested that a well-flexed attitude may facilitate birth, make uterine contractions more effective, and protect the pelvic floor [9]. The seven cardinal movements are then engagement, descent, flexion, internal rotation, extension, restitution and external rotation, and expulsion, and can be reproduced using computational simulation.
The fetal head is the hardest part to deliver. However, since the fetal skull is composed of sutures and fontanelles (Fig. 5), which has material properties softer than the surrounding skull bones, changes in shape are possible as the head passes through the pelvis and is subjected to constriction by external compressive forces (molding). The skull sutures and fontanelles allow the parietal and occipital bones to be pressed and displaced, resulting in a shortened suboccipitobregmatic diameter and an elongated mentovertical diameter, already reproduced by computational simulations [10]. The degree to which the head is capable of molding may make the difference between spontaneous delivery versus operative delivery. A malposition of the head can also lead to labor and delivery complications by obstructing fetal passage through the birth canal. A presentation with a mentovertical diameter (brow presentation) can be difficult or impossible to be delivered vaginally, because the diameter of the presenting part may be too large to safely fit through the pelvis [11].
3 Biomechanical Childbirth Simulation
Computational simulations of childbirth aim to illustrate the whole progression of labor, and to act as an adjuvant tool in the clinical setting for specific cases that may result in complicated labor, predicted by the computational model. Modeling takes into account the geometry of the structures and their mechanical properties. In biomechanics, engineering simulation tools based on the finite element method (FEM) are regularly used. However, the results of the simulations are strongly dependent on the material model chosen and the material parameters defined. Inaccurate choices lead to imprecise simulation results.
3.1 Constitutive Models
Constitutive laws are applied to reproduce the biomechanical behavior of the pelvic structures, taking into account the fundamentals of their inner structure. Most of the pelvic soft structures are assumed to be hyperelastic (describing nonlinear material behavior and large shape changes) and often incompressible materials (maintaining volume constant under pressure). Also, as some structures, for example, the pelvic striated skeletal muscles, are embedded in a connective tissue matrix, their features have to be set, as, for instance, their anisotropic and isotropic behavior, respectively. Isotropy is the property of being directionally independent, as opposed to anisotropy, which means heterogeneity in all directions.
3.1.1 Isotropic Constitutive Models: Simulating the Passive Behavior
The hyperelastic models (Neo-Hookean, Mooney–Rivlin, and Yeoh) are mainly used to simulate the passive mechanical behavior for two main reasons. Firstly, because they are simple models (with few parameters to optimize) that employ a nonlinear relationship between stress and strain to describe incompressible hyperelastic materials, and also because they seem to be able to describe the biomechanical behavior of the PFM during simulation of Valsalva maneuver and defecation and vaginal delivery [12,13,14].
The Neo-Hookean (Eq. 1), Mooney–Rivlin (Eq. 2), and Yeoh (Eq. 3) constitutive models are characterized by:
where W is the strain energy function and c 1, c 2, and c 3 are the material parameters to be determined and have dimensions of stress; and I 1, I 2, and I 3 are the principal strain invariants (Eq. 4) of the right Cauchy-Green tensor [12]. For the case uniaxial stretching, the principal strain invariants are represented as follows:
where λ is the maximum principal stretch.
In the case of uniaxial stretching, the Cauchy stress σ, a function of the invariants (Eq. 5), can be described by the following equation [12]:
3.1.2 Anisotropic Constitutive Models: Simulating the Passive and Active Behavior of the Muscle
Additionally, a quasi-incompressible transversely isotropic hyperelastic model is used to characterize more realistically the PFM behavior—composed by a solid extracellular matrix, collagen, and muscle fibers with a preferred orientation, proposed by Martins et al. [15]. This hyperelastic model was used by other authors to simulate the PFM contraction, comparing the numerical displacements with data from dynamic sagittal MR images [16, 17], and to study the biomechanical behavior of the PFM during vaginal delivery [18, 19].
For the constitutive model used, the strain energy per unit volume of the reference configuration can be written using the following equation:
where U I is the strain energy related with deformation of the isotropic matrix embedding the muscle fibers, defined as:
and U f is the strain energy related with each muscle fiber, considering a passive elastic part, U PE, and an active part, U SE, due to contraction. The function f SE(λ M, α) ensures that the muscle produces no energy for values of 0.5 ≥ λ M ≥ 1.5, and allows to control the level of activation by the internal variable α ∈ [0, 1].
U J is the term of the strain energy associated with the volume change,
In these definitions, c, b, A, a, D, and \( {T}_0^M \) are constants, \( {\overline{I}}_1^C \) is the first invariant of the right Cauchy-Green strain tensor, C, with the volume change eliminated, i.e.,
It represents the fiber stretch ratio in the direction N of the undeformed fiber and ⊗ denotes the tensor product. In Eq. (10), \( \overline{\mathbf{F}} \) is the deformation gradient with the volume change eliminated and J the volume change.
Based on the constitutive equations governing the material response at a continuum level the stress tensor and the associated material tangent, H, must be provided for numerical calculations. However, to implement the constitutive model in the software Abaqus it is mandatory to define the spatial tangent tensor, h. In particular, the Cauchy stress tensor and the tangent stiffness matrix using the Jaumann rate of Cauchy stress are given by [20]
In Eq. (12), S is the second Piola-Kirchhoff stress tensor given by
where E is the Green-Lagrange strain tensor.
3.2 In Vivo Characterization
The female pelvic floor is a soft tissue support structure associated with different disorders. These affect the quality of life of many women and can be related with changes in the biomechanical properties of muscles, ligaments, and fascia [21]. In this sense, the biomechanical analysis of the pelvic floor tissues is important to understand different PFD. Decreased tissue elasticity often causes inability to maintain the normal position of the pelvic organs and levator hiatus closure, so such analysis will also improve clinical outcomes by better understanding the effect of changes in tissue elasticity. PFD may result from changes in the biomechanical properties of the supportive structures that occur from weakness or impairment of muscles or ligaments, or alterations in the stiffness of the pelvic fascia associated with the risk factors—age, hormonal changes, childbirth, among others [21].
Previous experimental in vitro studies have been addressed to evaluate biomechanical properties of the pelvic ligaments, vaginal tissue, and levator ani (LA) muscle [22,23,24,25,26]. To obtain these biomechanical properties, the tissue collected during surgeries or from female cadavers has been tested using different techniques: uniaxial [24] and biaxial tensile tests [27]. However, these collected tissues are frequently afflicted in clinical environment, and consequently, the comparison to in vivo healthy tissues is difficult [28], mainly due to their location. Hence, the computational models are a powerful tool to understand the behavior of the PFM, being used by several authors [1, 16, 18, 29].
Numerical simulations of the mechanical behavior of the PFM based on the FEM use in vitro biomechanical properties obtained from experimental studies with both normal and pathological specimens [30, 31]. Nonetheless, to achieve realistic simulation of the PFM, Silva etal. implemented an inverse finite element analysis (FEA) to obtain in vivo biomechanical properties of the PFM for a specific subject [32]. The methodology consisted in comparing dynamic MR images during Valsalva maneuver and contraction with the PFM behavior described by different constitutive models in order to define the material parameters that best mimicked the in vivo muscle behavior shown in those dynamic images [13, 32]. Silva et al. found lower elasticity for the PFM of incontinent women when compared to asymptomatic women [14]. Demographic or morphological characteristics did not explain the difference obtained, and may be associated with histological changes, due to the fact that women with incontinence usually present a significant reduction of type III collagen [33]. Lower elasticity in the PFM of incontinent women means greater displacements during Valsalva maneuver. Additionally, the mean values of the material properties related with stiffness were higher for the muscles of women with prolapse. This increase in stiffness is in line with other experimental works involving vaginal tissue, which showed that the elasticity module is significantly higher in the prolapsed tissue when compared with the normal tissue [24, 34]. The higher values of the material parameters for women with prolapse can be associated with differences in muscle morphology, regarding to the fact that women with POP presented thinner muscles. The thinner muscles in women with POP can have a histological response, decreasing the total collagen content and increasing the concentration of collagen type III [35].
However, it is important to consider some limitations and simplifications involved: (1) this sample is small; (2) the numerical models did not include the connective tissues (fascia and ligaments) and pelvic organs, which would be more realistic.
In this context, the determination of the in vivo biomechanical properties is essential to obtain customized computational models to simulate the vaginal delivery.
3.3 Vaginal Delivery Simulation
The biomechanical principles of childbirth are still unknown but it is recognized that the physiological changes that occur during pregnancy and childbirth have a detrimental effect on the structure and function of the muscles, nerves, and connective tissue that make up the pelvic floor complex. As such, the computational models arise with the intention of improving current knowledge, studying mechanical aspects during vaginal delivery (stress, tension, forces, and contact pressures), having the capability to isolate and evaluate the mechanical significance of a single feature. Hence, biomechanical studies are mainly focused on pelvic floor muscles, in order to predict obstetric trauma that will result in an increased risk of developing pelvic floor muscle dysfunction [36,37,38]. The computational models are meant to represent, from a mechanical point of view, the effects that the passage of a fetal head can induce on the muscles of the pelvic floor. Parente et al. found that during a vaginal delivery with the fetus in vertex position and occipito-anterior presentation, the maximal rate of stretching of the pelvic floor muscles exceeded by approximately 10% the largest noninjurious stretch ratio (Fig. 6) [37, 39]. They concluded that if the injury is caused by stretching of fibers that exceeds a maximum permissible value, during vaginal delivery there is a high risk for injury to the pelvic floor muscles [37]. It was also verified that if there is a malposition of the fetus during childbirth, namely an occipito-posterior presentation, the maximum rate of stretching of the pelvic floor muscles exceeds the limit of muscle resistance in more than 15% (Fig. 6) [40]. Yan et al. noticed that the region of the pelvic floor muscles most subjected to stresses are independent of the fetal head geometry, suggesting that the locations of potential avulsion injuries could be entirely dependent on the morphology of the maternal pelvis [8].
Oliveira et al. quantified the muscle damage during vaginal delivery with the fetus in vertex position and occipito-anterior presentation and concluded that, particularly during fetus head extension, the pelvic floor muscles are injured and that the puborectalis component of the levator ani muscle is the most prone to damage (Fig. 7) [41]. Immediately after delivery, the tissues are swollen and deformed, making it difficult to diagnose the degree of tear, leading to errors in determining the prevalence of obstetric lesions. These models thus become valuable tools in assisting the diagnosis of injuries. However, since the problem studied is quite complex, it is necessary to consider the limitations involved in order to properly interpret the research findings. Moreover, the impact of the computational model simplifications in the expected results should be taken into account. Yan et al. verified that the inclusion of a full pelvis provides a more complete anterior constraint to the childbirth model, resulting in noticeably variations in the fetal head motion and in higher forces required for delivery compared to a simplified model [42].
In most computational models, the viscous effects present in all biological soft tissues were disregarded, which may hinder the evaluation of the tissue behavior during labor. Vila Pouca et al. used a visco-hyperelastic constitutive model to characterize the mechanical behavior of the pelvic floor muscles to assess how the childbirth duration affects the efforts sustained by the pelvic floor [43]. They concluded that viscoelasticity increases the stiffness of the tissue, increasing strength compared to the elastic response, which justifies the higher efforts associated with precipitous labors. By including a continuum mechanics damage model, Vila Pouca et al. also found that tissue relaxation properties contribute to decrease damage levels, supporting the theory of delayed pushing applied in the second stage of labor [44].
There is a growing interest in improving computational models, taking into account, for example, the influence of the birthing positions on physiological outcomes [45]. Such computational models take pelvic joint motion into account and are able to determine pelvic kinematics under loading conditions, allowing to determine the loads applied to the female pelvis during dynamic movements that may occur during labor [46].
Such biomechanical models also allow to address the influence of common obstetric procedures, such as episiotomy. The latest Cochrane reviews do not recommend the routine use of episiotomy for vaginal delivery, irrespective of the fetal position, ensuring that the reduction in perineal/vaginal trauma is not justified by current evidence [47]. However, there is a particular group, when instrumental delivery is intended, where further research is needed. Oliveira et al. simulated vaginal deliveries with the fetus in vertex presentation and occipito-anterior position with different mediolateral episiotomies approaches, varying the length and angle of the incision [48]. According to the obtained results, they concluded that a mediolateral episiotomy has a protective effect, reducing stress on the muscles and the force necessary to delivery successfully up to 52.2% (Fig. 8). The influence of performing mediolateral episiotomies during a malposition childbirth was also addressed by Oliveira et al. [49]. They concluded that episiotomy can reduce muscle damage to values obtained during labor in normal position, making the fetal position almost irrelevant [49]. Although the results look promising for protection of PFM trauma, the model does not include the perineal body, which is the primary structure that is implicated. Therefore, further work which includes the perineal body is needed.
4 Personalized Childbirth Models
Most of the current biomechanical models of the maternal pelvic floor and fetus system remain generic and do not provide individualized information. However, an accurate estimation of the effects of childbirth on the pelvic soft tissues implies using subject-specific biomechanical models, which will certainly improve delivery approaches. Particularly if one considers that there are significant individual differences in the anatomy of the maternal bony pelvis (size and shape), fetal head size, the mechanical properties of the pelvic floor structures, and boundary conditions. The inverse FEA will be adjusted to the ultrasound technique, replacing the magnetic resonance imaging (MRI), to obtain the in vivo biomechanical properties during vaginal delivery. Additionally, the boundary conditions will be included, according to subject-specific ultrasound technique. Patient-specific modeling has caught the attention of many relevant research groups around the world because of its potential to improve diagnosis, and optimize clinical treatment by predicting outcomes of therapies and surgical interventions. Most current medical diagnostic practices lead to rough estimates of outcomes for a particular treatment plan, and treatments and their outcomes usually find their basis in the results of clinical trials. Nonetheless, these results might not apply directly to individual patients because they are based on averages. As an alternative, patient-specific modeling can be used as a diagnostic tool to adapt treatment and optimize an individual’s therapy. The patient-specific modeling workflow should involve the collection and processing of data from an individual patient and their integration into a mathematical model. The model should incorporate the mathematical representations of the patient’s geometry, boundary and initial conditions, and the governing equations and parameters, with leeway for the optimization of the mechanical properties of the tissues. Regarding boundary conditions, a formulation requiring observation of tissue displacements, compliance boundary conditions, will ensure that these are individual-specific [50]. Data collected from the patient can be used for model validation; however, it should be distinct to data used for model development.
Biomechanical models in general, and of childbirth in particular, will become sufficiently well-informed and functional to enable personalized planning of surgical interventions, mainly due to the advent of clinical imaging modalities, coupled with the biostatistics, data analytics, and physics-based computational models.
5 Conclusions
As has been brought to mind throughout this chapter, the simulation of vaginal deliveries is a huge challenge. Mainly because it focuses on a region whose biomechanical research is in its infancy. There are still many issues to investigate, and many unanswered questions. Due to the advances in the field of medical imaging and in the physics-based computational models, it is expected that great advances will be made in the field of pelvic floor biomechanics. In the future, therefore, biomechanical models of childbirth will be sufficiently well-informed and functional for the personalized planning of childbirth, still serving as educational tools for physicians. The evaluation of the risk for childbirth-related pelvic floor trauma is one of the main objectives of simulating vaginal childbirth, by identifying the relevant processes that are involved in structural failure, such as the stress–strain values in the insertion points of the rectal area of the levator ani, and in the pubic symphysis. Obstetric techniques could be improved if they are informed by biomechanical models and simulations demonstrating the effect of certain approaches on pelvic floor biomechanics. Computational models have already shown that rupture of muscle fibers leading to macroscopic trauma of the levator ani can be overcome by mediolateral episiotomy, which seems to reduce the amount of stress in the PFM.
References
Friedman S, Blomquist J, Nugent J et al (2012) Pelvic muscle strength after childbirth. Obstet Gynecol 120:1021–1028. https://doi.org/10.1097/AOG.0b013e318265de39
Haylen BT, de Ridder D, Freeman RM et al (2010) An international urogynecological association (IUGA)/international continence society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 29:4–20. https://doi.org/10.1002/nau.20798
Wu JM, Kawasaki A, Hundley AF et al (2011) Predicting the number of women who will undergo incontinence and prolapse surgery, 2010 to 2050. Am J Obstet Gynecol 205:1–5. https://doi.org/10.1016/j.ajog.2011.03.046
Kiyosaki K, Ackerman L, Histed S et al (2012) Patient understanding of pelvic floor disorders: what women want to know. Female Pelvic Med Reconstr Surg 18:137–142. https://doi.org/10.1097/SPV.0b013e318254f09c. Patient
Wu MP, Wu CJ, Weng SF (2015) The choice of reoperation after primary surgeries for uterine prolapse: a nationwide study. Gynecol Minim Invasive Ther 4:120–125. https://doi.org/10.1016/j.gmit.2015.02.002
De Souza A, Dwyer P, Charity M et al (2015) The effects of mode delivery on postpartum sexual function: a prospective study. BJOG Int J Obstet Gynaecol 122:1410–1418. https://doi.org/10.1111/1471-0528.13331
Rempen A, Kraus M (1991) Pressures on the fetal head during normal labor. J Perinat Med 19:199–206. https://doi.org/10.1515/jpme.1991.19.3.199
Yan X, Kruger J, Nielsen P, Nash M (2015) Effects of fetal head shape variation on the second stage of labour. J Biomech 48(9):1593–1599. https://doi.org/10.1016/j.jbiomech.2015.02.0629
Parente MP, Natal Jorge RM, Mascarenhas T et al (2010) Computational modeling approach to study the effects of fetal head flexion during vaginal delivery. Am J Obstet Gynecol 203:217.e1–217.e6. https://doi.org/10.1016/j.ajog.2010.03.038
Silva MET, Oliveira D, Roza TH et al (2015) Study on the influence of the fetus head molding on the biomechanical behavior of the pelvic floor muscles, during vaginal delivery. J Biomech 48(9):1600–1605. https://doi.org/10.1016/j.jbiomech.2015.02.032
Cunningham F, Leveno K, Bloom S et al (2018) Williams obstetrics, 25th edn. McGraw-Hill Education/Medical, Pennsylvania
Noakes KF, Pullan AJ, Bissett IP, Cheng LK (2008) Subject specific finite elasticity simulations of the pelvic floor. J Biomech 41:3060–3065. https://doi.org/10.1016/j.jbiomech.2008.06.037
Silva MET, Parente MPL, Brandão S et al (2018) Characterization of the passive and active material parameters of the pubovisceralis muscle using an inverse numerical method. J Biomech 71:100–110. https://doi.org/10.1016/j.jbiomech.2018.01.033
Silva MET, Brandão S, Parente MPL et al (2017) Biomechanical properties of the pelvic floor muscles of continent and incontinent women using an inverse finite element analysis. Comput Methods Biomech Biomed Engin 5842:1–11. https://doi.org/10.1080/10255842.2017.130454215
Martins JAC, Pires EB, Salvado R, Dinis PB (1998) A numerical model of passive and active behavior of skeletal muscles. Comput Methods Appl Mech Eng 151:419–433. https://doi.org/10.1016/S0045-7825(97)00162-X
Roza TH, Brandão S, Oliveira D et al (2015) Football practice and urinary incontinence: relation between morphology, function and biomechanics. J Biomech 48:1587–1592. https://doi.org/10.1016/j.jbiomech.2015.03.013
Saleme CS, Parente MPL, Natal Jorge RM et al (2011) An approach on determining the displacements of the pelvic floor during voluntary contraction using numerical simulation and MRI. Comput Methods Biomech Biomed Engin 14:365–370. https://doi.org/10.1080/10255842.2010.482045
Parente MP, Natal Jorge R, Mascarenhas T et al (2009) The influence of the material properties on the biomechanical behavior of the pelvic floor muscles during vaginal delivery. J Biomech 42:1301–1306. https://doi.org/10.1016/j.jbiomech.2009.03.011
Parente MP, Natal Jorge R, Mascarenhas T, Silva-Filho A (2010) The influence of pelvic muscle activation during vaginal delivery. Obstet Gynecol 115:804–808. https://doi.org/10.1097/AOG.0b013e3181d534cd
Crisfield M (2001) Non-linear finite element analysis of solids and structures, volume 2 - advanced topics. Wiley, London
Abramowitch SD, Feola A, Jallah Z, Moalli PA (2009) Tissue mechanics, animal models, and pelvic organ prolapse: a review. Eur J Obstet Gynecol Reprod Biol 144:S146–S158. https://doi.org/10.1016/j.ejogrb.2009.02.022
Cosson M, Lambaudie E, Boukerrou M et al (2004) A biomechanical study of the strength of vaginal tissues: results on 16 post-menopausal patients presenting with genital prolapse. Eur J Obstet Gynecol Reprod Biol 112:201–205. https://doi.org/10.1016/S0301-2115(03)00333-6
Cosson M, Boukerrou M, Lacaze S et al (2003) A study of pelvic ligament strength. Eur J Obstet Gynecol Reprod Biol 109:80–87. https://doi.org/10.1016/S0301-2115(02)00487-6
Lei L, Song Y, Chen R (2007) Biomechanical properties of prolapsed vaginal tissue in pre- and postmenopausal women. Int Urogynecol J Pelvic Floor Dysfunct 18:603–607. https://doi.org/10.1007/s00192-006-0214-7
Rubod C, Boukerrou M, Brieu M et al (2008) Biomechanical properties of vaginal tissue: preliminary results. Int Urogynecol J Pelvic Floor Dysfunct 19:811–816
Martins PAL (2010) Experimental and numerical studies of soft biological tissues. PhD. Thesis. Faculty of Engineering, University of Porto, Porto
Janda S (2006) Biomechanics of the pelvic floor musculature. PhD. Thesis. Technische Universiteit Delft, Delft
Baah-Dwomoh A, McGuire J, Tan T, De Vita R (2016) Mechanical properties of female reproductive organs and supporting connective tissues: a review of the current state of knowledge. Appl Mech Rev 68:060801. https://doi.org/10.1115/1.4034442
Brandão FS, Parente MP, Rocha PA et al (2016) Modeling the contraction of the pelvic floor muscles. Comput Methods Biomech Biomed Engin 19:347–356. https://doi.org/10.1080/10255842.2015.1028031
Rivaux G, Rubod C, Dedet B et al (2013) Comparative analysis of pelvic ligaments: a biomechanics study. Int Urogynecol J 24:135–139. https://doi.org/10.1007/s00192-012-1861-5
Martins P, Silva-Filho AL, Fonseca AMRM et al (2013) Strength of round and uterosacral ligaments: a biomechanical study. Arch Gynecol Obstet 287:313–318. https://doi.org/10.1007/s00404-012-2564-3
Silva MET, Brandao S, Parente MP et al (2016) Establishing the biomechanical properties of the pelvic soft tissues through an inverse finite element analysis using magnetic resonance imaging. Proc Inst Mech Eng Part H J Eng Med 230:298–309. https://doi.org/10.1177/0954411916630571
Patel PD, Amrute KV, Badlani GH (2007) Pelvic organ prolapse and stress urinary incontinence: a review of etiological factors. Indian J Urol 23:135–141. https://doi.org/10.4103/0970-1591.32064
Jean-Charles C, Rubod C, Brieu M et al (2010) Biomechanical properties of prolapsed or non-prolapsed vaginal tissue: impact on genital prolapse surgery. Int Urogynecol J 21:1535–1538. https://doi.org/10.1007/s00192-010-1208-z
Kerkhof MH, Hendriks L, Brölmann H a M (2009) Changes in connective tissue in patients with pelvic organ prolapse--a review of the current literature. Int Urogynecol J Pelvic Floor Dysfunct 20:461–474. https://doi.org/10.1007/s00192-008-0737-1
Ashton-Miller JA, Delancey JO (2009) On the biomechanics of vaginal birth and common sequelae. Annu Rev Biomed Eng 11:163–176. https://doi.org/10.1146/annurev-bioeng-061008-12482337
Parente MP, Natal Jorge RM, Mascarenhas T et al (2008) Deformation of the pelvic floor muscles during a vaginal delivery. Int Urogynecol J Pelvic Floor Dysfunct 19:65–71. https://doi.org/10.1007/s00192-007-0388-7
Li X, Kruger J, Chung J, Nash M, Nielsen P (2008) Modelling the pelvic floor for investigating difficulties in childbirth. In: SPIE (Medical Imaging), vol 6916, p 69160V
Brooks S, Zerba E, Faulkner J (1995) Injury to muscle fibres after single stretches of passive and maximally stimulated muscles in mice. J Physiol 488:459–469
Parente MP, Natal Jorge RM, Mascarenhas T et al (2009) The influence of an occipito-posterior malposition on the biomechanical behavior of the pelvic floor. Eur J Obstet Gynecol Reprod Biol 144S:S166–S169. https://doi.org/10.1016/j.ejogrb.2009.02.033
Oliveira D, Parente M, Calvo B, Mascarenhas T, Natal Jorge R (2016) Numerical simulation of the damage evolution in the pelvic floor muscles during childbirth. J Biomech 49(4):594–601. https://doi.org/10.1016/j.jbiomech.2016.01.014
Yan X, Kruger J, Li X, Nash M, Nielsen P (2013) Modelling effect of bony pelvis on childbirth mechanics. Neurourol Urodyn 32(6):531–532
Vila Pouca M, Ferreira J, Oliveira D, Parente M, Natal Jorge R (2018) Viscous effects in pelvic floor muscles during childbirth: a numerical study. Int J Numer Methods Biomed Eng 34(3):e2927. https://doi.org/10.1002/cnm.2927
Vila Pouca M, Ferreira J, Oliveira D, Parente M, Mascarenhas T, Natal Jorge R (2018) On the effect of labour durations using an anisotropic visco-hyperelastic-damage approach to simulate vaginal deliveries. J Mech Behav Biomed Mater 88:120–126. https://doi.org/10.1016/j.jmbbm.2018.08.011
Hemmerich A, Diesbourg T, Dumas G (2018) Development and validation of a computational model for understanding the effects of an upright birthing position on the female pelvis. J Biomech 77:99–106. https://doi.org/10.1016/j.jbiomech.2018.06.013
Hemmerich A, Diesbourg T, Dumas G (2018) Determining loads acting on the pelvis in upright and recumbent birthing positions: a case study. Clin Biomech 57:10–18. https://doi.org/10.1016/j.clinbiomech.2018.05.011
Jiang H, Qian X, Carroli G, Garner P (2017) Selective versus routine use of episiotomy for vaginal birth. Cochrane Database Syst Rev (2):CD000081. https://doi.org/10.1002/14651858.CD000081.pub3
Oliveira D, Parente M, Calvo B, Mascarenhas T, Natal Jorge R (2016) A biomechanical analysis on the impact of episiotomy during childbirth. Biomech Model Mechanobiol 15(6):1523–1534. https://doi.org/10.1007/s10237-016-0781-6
Oliveira D, Parente M, Calvo B, Mascarenhas T, Natal Jorge R (2017) The management of episiotomy technique and its effect on pelvic floor muscles during a malposition childbirth. Comput Methods Biomech Biomed Engin 20(11):1249–1259. https://doi.org/10.1080/10255842.2017.1349762
Ozkan E, Goksel O (2015) Compliance boundary conditions for simulating deformations in a limited target region. In: 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), pp 929–932. https://doi.org/10.1109/EMBC.2015.7318515
Acknowledgments
The authors gratefully acknowledge the support from the Portuguese Foundation of Science under grants IF/00159/2014, and the funding of project 030062 SIM4SafeBirth—A biomechanical approach to improve childbirth outcomes and NORTE-01-0145-FEDER-000022 SciTech—Science and Technology for Competitive and Sustainable Industries, cofinanced by Norte’s Regional Operational Programme (NORTE2020), through European Regional Development Fund (ERDF).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this paper
Cite this paper
Oliveira, D.A., Silva, M.E.T., Pouca, M.V., Parente, M.P.L., Mascarenhas, T., Natal Jorge, R.M. (2020). Biomechanical Simulation of Vaginal Childbirth: The Colors of the Pelvic Floor Muscles. In: Nash, M., Nielsen, P., Wittek, A., Miller, K., Joldes, G. (eds) Computational Biomechanics for Medicine. Springer, Cham. https://doi.org/10.1007/978-3-030-15923-8_1
Download citation
DOI: https://doi.org/10.1007/978-3-030-15923-8_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-15922-1
Online ISBN: 978-3-030-15923-8
eBook Packages: EngineeringEngineering (R0)