Abstract
Introduction and hypothesis
Pelvic organ prolapse (POP) affects one third of women of all ages and is a major concern for gynecological surgeons. In pelvic reconstructive surgery, native ligaments are widely used as a corrective support, while their biomechanical properties are unknown. We hypothesized differences in the strength of various pelvic ligaments and therefore, aimed to evaluate and compare their biomechanical properties.
Materials and methods
Samples from the left and right broad, round, and uterosacral ligaments from 13 fresh female cadavers without pelvic organ prolapse were collected. Uniaxial tension tests at a constant rate of deformation were performed and stress–strain curves were obtained.
Results
We observed a non-linear stress–strain relationship and a hyperelastic mechanical behavior of the tissues. The uterosacral ligaments were the most rigid whether at low or high deformation, while the round ligament was more rigid than the broad ligament.
Conclusion
Pelvic ligaments differ in their biomechanical properties and there is fairly good evidence that the uterosacral ligaments play an important role in the maintenance of pelvic support from a biomechanical point of view.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
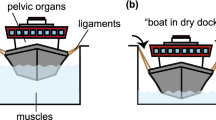
Pelvic organ prolapse (POP) is a major health issue among aging women and one of the most common indications for surgical treatment. It is estimated that 50% of parous women have at least some minor degree of POP [1, 2]. It has been recognized that, apart from birth trauma and other biographical factors, abnormalities of the connective tissue composition may specifically contribute to the genesis of POP [3]. These abnormalities can have a direct impact on the biomechanical properties of pelvic floor supportive structures and thus contribute to the development of a clinically relevant POP [4].
The pelvic ligaments are thought to be key structures in the maintenance of pelvic support. Specifically, those which suspend the uterus, such as the uterosacral ligaments (USL), are thought to play a major role in maintaining pelvic statics. [5–7]. According to DeLancey, the USL provide the level 1 support to the cervix and the upper vagina [8]. In recent years, our understanding of pelvic floor disorders has advanced, leading to the development of new surgical techniques such as the implantation of prosthetic material aimed at reinforcing the native vaginal tissue or replacing defective, weakened ligaments [9]. However, the biomechanical properties of pelvic ligaments from a comparative standpoint have been poorly evaluated, leading to a paucity of data in the literature [10–15]. Specifically, the biomechanical characterization of pelvic ligaments could improve our understanding of the events contributing to the occurrence and recurrence of POP. Furthermore, a better understanding of tissue biomechanics could enhance the development of more functional prosthetic material for use in pelvic reconstructive surgery.
We hypothesized that there are biomechanical differences among various pelvic ligaments. Therefore, the purpose of this study was to evaluate and compare the biomechanical properties of various pelvic ligaments obtained from 13 fresh female cadavers without POP.
Materials and methods
Tissues were obtained from 13 fresh female cadavers without a clinically relevant, i.e., grade 2 or greater POP, according to the Baden–Walker half-way classification system, which was excluded by gynecological examination and using a Pozzi clamp to pull gently on the cervix. The cadavers were frozen (not formolized) for conservation and unfrozen just prior to the dissection. Each patient had consented prior to their death to their cadaver being used for scientific and/or educational purposes, according to local legislation. The institutional review board approved the experimental protocol (Cos2009/05; CCPRB no. 03/81; DRC 0315). We had previously established and validated an experimental protocol for the biomechanical characterization of human tissue, which we employed in this study [16]. All specimens were collected in the same manner according to the following protocol: a transverse laparotomy was performed and the uterus was placed under traction in order to better delineate those ligaments to be removed. The pelvic ligaments (USL, round, and broad) were removed completely, as far as possible, starting at their insertion point at the uterus to the parietal pelvic wall or sacrum respectively. The broad ligament of the uterus was defined as the parauterine tissue consisting of the wide fold of peritoneum that connects the sides of the uterus to the walls and floor of the pelvis.
The right and left sides were harvested from each cadaver and a total of 66 ligaments were obtained. Only clearly identifiable (i.e., delimitable and thus definable) and qualitatively satisfactory (i.e., accurately tailored and cut, filling the size of the punch [i.e., not too short] for adequate length, and according to the requirements of the measuring system) ligaments were used for the study. All samples were orientated and marked before being frozen in 0.9% sodium chloride solution at minus 18°C. The excised tissues were used to perform uniaxial tension tests at a constant rate of deformation up to the point of rupture, according to a previously described and validated experimental protocol, established by Rubod et al [16]. In our previous study we have exhaustively studied and determined the experimental conditions such as temperature, hygrometry, and rate of deformation in order to allow reproducible tests. We were also able to prove that freezing had no effect on the mechanical properties of the tissues, so that there was no difference when comparing the mechanical response of fresh and frozen tissues [16]. Depending on the size of the sample for each ligament, several tests (range, 1–3) were performed. Briefly, the tissue samples were unfrozen at an ambient temperature (20°C) for 9 h and were then stored in sodium chloride solution to avoid tissue deterioration. The specimens were of varying size; therefore, in order to determine an area of uniform stress in the center of the test samples during the tension test, standardized test samples were excised from the tissues using a punch. The mean thickness of each standardized sample [16] was measured with a caliper rule to further determine the nominal stress (F/S 0, where F is the load and S 0 is the size of the initial cross section). Each sample was clamped in a tightening grip and strained at a constant strain rate (2 × 10-2 s−1) at an ambient temperature (20°C) within 24 h of unfreezing. The grips fixture has been designed in such a way as to prevent tissue slippage during the test [16]. Samples were directly loaded, without a preloading phase. The results presented in this study take into account the complete response from zero force to rupture. The rupture tests were performed using a conventional tension machine (Instron 4302™). A low capacity load cell (1 kN) was used to measure the nominal stress (force per unit of surface) during the test, knowing the forces and the initial cross-section of the samples. The load cell sensitivity was 0.01 N (0.001 class), which is in agreement with the quantity measured. Strains (l-l 0 /l 0 where l is the length and l 0 the initial length) were measured with a contactless video extensometer. Subsequently, the stress–strain curves were obtained and analyzed to characterize the biomechanical behavior of the specimens. The mechanical response of the specimens before rupture was then studied.
For a comparative statistical analysis of all the experimental data, a behavior model had to be incorporated, taking into account nonlinear elasticity phenomena during major deformation. The Mooney–Rivlin-type model was used [17, 18]. Two parameters, C0 and C1, characterizing the biomechanical behavior with low and high deformation respectively were identified on the curves using a least squared roots method:\( \sigma = 2\left( {\lambda - {{1} \left/ {{{\lambda^2}}} \right.}} \right)\left[ {{\text{C}}0 + 2{\text{C}}1\left( {{\lambda^2} + {{2} \left/ {\lambda } \right.} - 3} \right)} \right] \) where σ is the nominal stress and λ is the stretch.
Each ligament removed was used to provide several samples. Each sample was then tested and thus, two parameters per sample, C0 and C1, were obtained. SAS v9.1 software was used for statistical analyses. The comparison was performed using the mixed linear model, as well as a nonparametric test according to Conover, studying the influence of each factor and all their interactions. A p value of < 0.05 was considered to be statistically significant.
Results
Tissue samples from the left and right USL, broad and round ligaments were collected from 13 fresh female cadavers without POP. The mean age was 83.5 ± 12.3 (range, 61–100) years. Overall, 66 ligaments of appropriate quality and according to the requirements of the experimental protocol (see Materials and methods) were harvested and studied. These included 22 USL, 23 round ligaments, and 21 broad ligaments.
Uniaxial tension tests were performed up to the rupture point of the specimens. We were able to demonstrate a nonlinear stress-deformation response and a hyperelastic behavior (i.e., with high deformation) for the pelvic ligaments examined (Fig. 1). This mechanical behavior was identified with the help of a Mooney–Rivlin-type law. The individual C0 and C1 parameters, characterizing the mechanical behavior at low and high deformation of the uterine ligaments respectively, are given in Table 1.
We observed considerable differences in tissue rigidity among the cadavers for the same type of ligament, which was in line with the relatively high standard deviations (SD) for the C0 and C1 parameters (Table 1).
Our results showed that the USL was the most rigid ligament at both low and high deformation (p = 0.05 and 0.003 respectively), compared with the round and broad ligaments. Furthermore, the round ligament was more rigid than the broad ligament (Fig. 1).
Discussion
In the present study, we describe the biomechanical characteristics of the USL, round, and broad ligaments, which are thought to play a significant role in the maintenance of pelvic and uterine support. In our study of 13 fresh female cadavers without POP, it is important to note that the USL was by far the most rigid ligament, compared with the round and broad ligaments at both low and high deformation. To the best of our knowledge the nonlinear and hyperelastic mechanical behavior of the ligaments studied has been defined for the first time.
The USL appear to be quite relevant in maintaining pelvic support, and are widely used as a corrective support in pelvic reconstructive surgery [5–8]. In vitro studies have shown that the cervical portion of the USL is able to support more than 17 kg of weight before failing [6]. Interestingly, in patients with POP, the expression of the gene product responsible for the development of the USL is deficient [19]. On the basis of the first histology studies on USL, Blaisdell concluded that these ligaments consisted only of connective tissue [20]. However, this concept has largely evolved in the last few decades. A recent study by Ramanah et al. suggested that the USL represent a ligamentary complex, consisting of the inferior hypogastric plexus and hypogastric nerves, as well as vascular elements surrounded by a fine connective envelope [21]. Gabriel et al. histomorphologically investigated the cervical portion of the USL and found that, apart from the connective tissue, a considerable amount of smooth muscle cells was present, pointing to its functional role in pelvic support [22]. In the USL of women with POP, a higher expression of collagen III and matrix metalloproteinase (MMP)-2, but no change in collagen I, has been described [22, 23]. Collagen III plays a role in tissue elasticity and extensibility. Therefore, the increased amount of collagen III noted in patients with POP could be responsible for the increased tissue laxity in these patients, pointing to the interrelationship between connective tissue composition and biomechanical behavior. Active remodeling of the connective tissue in the USL of women with POP as a result of biomechanical stress has also been proposed by other authors [24, 25]. The regulation of smooth muscle contractility in key structures of the pelvic support could represent one potential bridge between biochemical and biomechanical pathways [26].
Our results suggest that the USL might be the least deformable and most rigid structures among the three pelvic ligaments studied, which can be explained by their histological composition and biomechanical characteristics. Thus, it seems appropriate to continue using the USL as a strong anchoring element in pelvic reconstructive surgery.
We recently studied the vaginal tissue of 11 fresh female cadavers without POP on the basis of the Rubod et al. protocol [27]. Hence, a comparison of the biomechanical properties between vaginal tissue and the three pelvic ligaments studied here was possible after superimposing the respective curves. Of note, the USL and the round ligaments were even more rigid and less extendible than vaginal tissue, indicating that the deformation of the ligaments at a prescribed stress was always smaller than the deformation of the vagina, and pointing to their important role in pelvic support. Serious consideration should be given to the fact that such a comparison is hampered by the use of different cadavers. However, as the experimental protocol and the methodology were identical [16], we feel that these observations should not be withheld.
Martins et al. [28] investigated prolapsed vaginal tissue taken intraoperatively and described maximum stress values of 3–8 MPa, which is considerably higher than our reported values of 0.58 MPa [27], as well as the data reported by Lei et al. (0.27–0.42 MPa) [29]. Interestingly, in two other studies we were able to show that prolapsed vaginal tissue was more rigid than healthy vaginal tissue [16, 30], which was initially somewhat striking, but could be in line with the described differences in the previously mentioned studies [27–29]. Such comparisons, however, are hampered by the various methodologies employed, using cadaveric tissue vs tissue derived intraoperatively, varying protocols, the presence or absence of prolapse, and different age cohorts, among other factors.
One strength of our study was the use of the standardized Rubod protocol [16], which has been validated at each stage by exhaustive tests on sheep vaginal tissue. This protocol has been used in several studies concerning healthy and pathological vaginal tissue [16, 27, 30], skin, and aponeurosis [27]. It has also been tested in terms of measurement reproducibility. Our sample size was relatively small because the number of available cadavers was limited, both by legislation and by the need for educational use of the cadavers. Another limitation is that we studied a population of cadavers well advanced in years, and post-mortem changes must be taken into account. Studying cadaveric tissue does not allow extrapolation of our results to the in vivo situation. The analysis of nonprolapsed pelvic ligament specimens from live patients is hampered by ethical considerations. There was also a lack of certain clinical data, such as the parity, the use of hormonal replacement therapy, and the physical activity level during the person' s lifetime. The size of the error introduced by these limitations is unknown.
In summary, our findings demonstrate that pelvic ligaments differ in their biomechanical properties, and that the USL are suitable candidates for the maintenance of pelvic support. A well-designed comparative study on the biomechanical properties of pelvic ligaments in women with and without POP is warranted in the future.
References
Samuelsson E, Victor F, Tibblin G, Svardsudd K (1999) Signs of genital prolapse in a Swedish population of women 20 to 59 years of age and possible related factors. Am J Obstet Gynecol 180:299–305
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark A (1997) Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol 89:501–506
Dietz HP (2008) The aetiology of prolapse. Int Urogynecol J 19:1323–1329
Alperin M, Debes K, Abramowitch S, Meyn L, Moalli PA (2008) LOXL1 deficiency negatively impacts the biomechanical properties of the mouse vagina and supportive tissues. Int Urogynecol J 19:977–986
Amundsen CL, Flynn BJ, Webster GD (2003) Anatomical correction of vaginal vault prolapse by uterosacral ligament fixation in women who also require a pubovaginal sling. J Urol 169:1770–1774
Buller JL, Thompson JR, Cundiff GW, Krueger Sullivan L, Schon Ybarra MA, Bent AE (2001) Uterosacral ligament: description of anatomic relationships to optimize surgical safety. Obstet Gynecol 97:873–879
Shull BL, Bachofen C, Coates KW, Kuehl TJ (2000) A transvaginal approach to repair of apical and other associated sites of pelvic organ prolapse with uterosacral ligaments. Am J Obstet Gynecol 183(6):1365–1373
DeLancey JOL (1992) Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol 166:1717–1724
Fatton B, Amblard J, Debodinance P, Cosson M, Jacquetin B (2007) Transvaginal repair of genital prolapse: preliminary results of a new tension-free vaginal mesh (Prolift technique)-a case series multicentric study. Int Urogynecol J 18:743–752
Conza NE, Rixen DJ, Plomp S (2007) Vibration testing of a fresh-frozen human pelvis: the role of pelvic ligaments. J Biomech 40:1599–1605
Cosson M, Boukerrou M, Lacaze S et al (2003) A study of pelvic ligament strength. Eur J Obstet Gynecol Reprod Biol 109:80–87
Reay Jones NH, Healy JC, King LJ, Saini S, Shousha S, Allen-Mersh TG (2003) Pelvic connective tissue resilience decreases with vaginal delivery, menopause and uterine prolapse. Br J Surg 90:466–472
Boukerrou M, Lambaudie E, Collinet P et al (2004) Mechanical resistance of pelvic ligaments used for incontinence or prolapse surgery. Gynecol Obstet Fertil 32:601–606
Vardy MD, Gardner TR, Cosman F et al (2005) The effects of hormone replacement on the biomechanical properties of the uterosacral and round ligaments in the monkey model. Am J Obstet Gynecol 192(5):1741–1751
Chen L, Ashton-Miller JA, Hsu Y, DeLancey JO (2006) Interaction among apical support, levator ani impairment, and anterior vaginal wall prolapse. Obstet Gynecol 108:324–332
Rubod C, Boukerrou M, Brieu M, Dubois P, Cosson M (2007) Biomechanical properties of vaginal tissue-Part 1: new experimental protocol. J Urol 178:320–5
Mooney M (1947) A theory of large elastic deformation. J Appl Phys 1940(11):582–592
Rivlin RS (1948) Large elastic deformations of isotropic materials. I. Fundamental concepts, II. Some uniqueness theorems for pure homogenous deformations. Philos Trans R Soc Lond Ser A:Math Phys Sci A240:459–490
Connell KA, Guess MK, Chen H, Andikyan V, Bercik R, Taylor HS (2008) HOXA11 is critical for development and maintenance of uterosacral ligaments and deficient in pelvic prolapse. J Clin Invest 118:1050–1055
Blaisdell FE (1917) The anatomy of sacro-uterine ligaments. Anat Record 12:1–42
Ramanah R, Parratte B, Hubert N, Arbez-Gindre F, Maillet R, Riethmuller D (2009) Anatomical and histological study of the uterosacral ligament: practical surgical consequences. J Gynecol Obstet Biol Reprod 38(4):304–311
Gabriel B, Denschlag D, Göbel H et al (2005) Uterosacral ligament in postmenopausal women with or without pelvic organ prolapse. Int Urogynecol J 16:475–479
Gabriel B, Watermann D, Hancke K et al (2006) Increased expression of matrix metalloproteinase 2 in uterosacral ligaments is associated with pelvicorgan prolapse. Int Urogynecol J 17:478–482
Goepel C (2008) Differential elastin and tenascin immunolabeling in the uterosacral ligaments in postmenopausal women with and without pelvic organ prolapse. Acta Histochem 110:204–209
Moalli PA (2005) Remodeling of vaginal connective tissue in patients with prolapse. Obstet Gynecol 106:953–963
Boreham MK, Miller RT, Schaffer JI, Word RA (2001) Smooth muscle myosin heavy chain and caldesmon expression in the anterior vaginal wall of women with and without pelvic organ prolapse. Am J Obstet Gynecol 185:944–952
Gabriel B, Rubod C, Brieu M, Dedet B, De Landsheere L, Cosson M (2011) Vagina, abdominal skin and aponeurosis: do they have similar biomechanical properties ? Int Urogynecol J 22:23–27
Martins P, Pena E, Calvo B, Doblaré M, Mascarenhas T, Natal Jorge R, Ferreira A (2010) Prediction of nonlinear elastic behaviour of vaginal tissue: experimental results and model formulation. Comp Meth Biomech Biomed Eng 13:327–337
Lei L, Song Y, Chen RQ (2007) Biomechanical properties of prolapsed vaginal tissue in pre- and postmenopausal women. Int Urogynecol J 18:603–607
Jean-Charles C, Rubod C, Boukerrou M, Brieu M, Dubois P, Cosson M (2010) Biomechanical properties of prolapsed or non prolapsed vaginal tissue: impact on genital prolapsed surgery. Int Urogynecol J 21:1535–1538
Acknowledgements
The authors announce unconditional financial support of the basic research by Ethicon Women’s Health & Urology. MS is a consultant of Ethicon Women’s Health & Urology. BG was awarded an International Fellowship grant by the International Urogynecological Association (IUGA) in 2009, which partly funded this research project. We thank Patrick Devos for his help with the statistical analyses.
Conflicts of interest
Géraldine Rivaux, Chrystèle Rubot, Bruno Dedet, Mathias Brieu declare that they have no conflict of interest to declare. Boris Gabriel: Serag-Wiessner (acceptance of paid travel expenses and honoraria). Michel Cosson: consultant for Ethicon and AMS, acceptance of paid travel expenses and honoraria, acceptance of payment for research; teaching sessions for Ethicon and Ipsen.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Rivaux, G., Rubod, C., Dedet, B. et al. Comparative analysis of pelvic ligaments: a biomechanics study. Int Urogynecol J 24, 135–139 (2013). https://doi.org/10.1007/s00192-012-1861-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-012-1861-5