Abstract
The aim of this study was to explore the relationship between biomechanical properties and the occurrence of pelvic organ prolapse (POP) through analysis on biomechanical properties of vaginal tissue. The biopsy specimens were obtained from 43 patients undergoing transvaginal hysterectomy, who were assigned into premenopausal POP, postmenopausal POP, premenopausal control and postmenopausal control groups. Tissue specimens were biomechanically assessed by a purpose-built tissue puller system, and stress–strain curves were digitally recorded. The Young’s modulus, Poisson’s ratio, maximum elongation, maximum fracture of vaginal tissue were 9.45 ± 0.70, 0.43 ± 0.01, 1.50 ± 0.02, 0.60 ± 0.02 in premenopausal POP group; 12.10 ± 1.10, 0.39 ± 0.01, 1.14 ± 0.05, 0.27 ± 0.03 in postmenopausal POP group; 6.65 ± 1.48, 0.46 ± 0.01, 1.68 ± 0.11, 0.79 ± 0.05 in premenopausal control group and 10.26 ± 1.10, 0.42 ± 0.01, 1.37 ± 0.04, 0.42 ± 0.03 in postmenopausal control group. There was significant difference in biomechanical properties between premenopausal POP group and premenopausal control group (p < 0.01). There was significant difference in biomechanical properties between postmenopausal POP group and postmenopausal control group (p < 0.01). Biomechanical properties in POP group were significantly lower than that in control group, suggesting that degeneration of biomechanical properties in pelvic support construction might lead to the occurrence of POP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pelvic organ prolapse (POP) constitutes a very common medical problem especially among the elderly, which is commonly associated with financial, social and psychological problem [1–5]. The proportion of the Chinese population over age 65 was almost a hundred million in the year 2001 and is expected to grow substantially during the coming decades. POP affects older women disproportionately. Among women more than 60 years old, the prevalence of POP was approximately 25% [6]. Prevalence of POP appears to gradually increase in the elderly. The causes of POP are multifactorial. There is still debate regarding the exact underlying pathophysiology of genital tract prolapse.
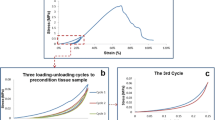
The aim of this study was to measure elastic properties of non-linear, visco-elastic and plastic connective tissue that are sensitive to small stiffness changes of the tissue over a wide range of mechanical loading. This method is based on the application of the tissue [7, 8]. In mechanical testing, a material is elastic when it returns completely to its original shape after the force or load is removed without the application of any compressive force. Various investigators have already demonstrated decreased collagen content and altered morphologic features in the POP [9–13]. Although abnormalities in connective tissue have been implicated in vaginal prolapse, few studies have been performed to examine its biomechanical properties. Biomechanical assessment of supports of the pelvic organs may provide the clinician with further insight into the etiology of this complex condition.
Methods
In 1998, a new method for testing skin (or vaginal tissue) under more physiological stress and strain was developed [14]. The method for testing was able to examine the elastic properties of non-linear, visco-elastic and plastic connective tissue that was sensitive to small stiffness changes in tissue over a wide range of mechanical loading.
Forty-three women participated in the study, and they were divided in four groups as follows: 9 premenopausal patients who had POP without accompanying urinary incontinence served as group 1; 12 postmenopausal patients who had POP without accompanying urinary incontinence served as group 2. Women with previous prolapse surgical procedures were excluded. Women with POP were staged by the pelvic organ prolapse quantitative (POP-Q) system [15]. This was the standard classification used by the clinicians at the gynecology outpatient clinic. Fourteen premenopausal patients who had enlarged uteri with benign diseases served as group 3; eight postmenopausal patients who had enlarged uteri with benign disease served as group 4. Groups 3 and 4 were observed without POP or stress urinary incontinence by history and medical examination; therefore, they served as control groups. None of the study subjects was receiving hormone replacement therapy, and none of them smoked. All patients gave their informed consent to the study, which was also approved by the Ethics Committee of the hospital.
Tissue from the vaginal wall was collected at the time of transvaginal hysterectomy. An incision was made in the horizontal axis of anterior vaginal fornix of the anterior lower uterine segment. The resultant horizontal strips of vaginal tissue were tested. The vaginal strip was wrapped in a saline-soaked gauze, placed in a clean labeled container and frozen at −70°C. The frozen tissue was thawed for approximately 1 h to room temperature and trimmed to a rectangular shape about 5 × 25 mm in size.
The machine was calibrated before each test. The ends of the tissue were carefully secured to two metal hooks by sutures and tissue glue (prevention of tissue slippage was confirmed by careful visual examination of the specimens after testing). The tissue was then connected to a purpose-built tissue puller system with force accuracy within 0.05 N and length accuracy within 0.01 mm [7]. One of the metal hooks with vaginal tissue attached was held securely and fixed to a metal device clamped to the bench. The other was connected to the computerized puller system. Force was applied to the latter end of the specimen by pulling on the second hook. During biomechanical testing, the tissues were kept under a layer of paraffin oil to prevent dehydration, and the ambient temperature of the tissue was kept at a constant 37°C.
When the tissue was initially connected to the puller system, the specimen was set at its slack length, that was, the length at which resistance against elongation was just measurable to the device. The tissue was stretched at a constant rate of 0.8 mm/s to an elongation of 8 mm. Superimposed on this linear elongation was a sinewave with its vibration frequency at 50 Hz. The measurement was repeated at increasing lengths every minute. The initial elongated length was 10% of the original slack length. All experimental tracings were recorded digitally. A detailed description of the experimental protocol was given elsewhere [13].
Statistical analyses were conducted using SPSS version 10.0 software. Results were expressed as mean±SEM. Statistical comparisons between two groups were conducted by a Student’s t test for normally distributed data. Comparisons among multiple groups were conducted with a one way analysis of variance, followed by post-hoc Student Neuman–Keuls test. A p value of <0.05 was considered significant.
Results
The samples were collected over a period of 10 months from June 2004 to May 2005. The average time between collecting the sample and the measurement was 24 h. The clinical characteristics of women from whom vaginal samples were obtained are listed in Tables 1 and 2. All the results are reported in Tables 3 and 4. Because of the small numbers in POP group, we took stages I and II as mild type, stage III as moderate type and stage IV as severe type. Some details of the POP-Q values of the prolapsed patients are in Tables 3 and 4. The biomechanical properties of all types POP are reported in Tables 7, 8, and 9.
From Tables 1 and 2, we can see that the pre- and postmenopausal groups did not show any significant differences in age, BMI, parity, vaginal parity and time since menopause. Biomechanical analysis of vaginal tissue in pre- and postmenopausal women in this study demonstrated that there are marked significant differences in biomechanical properties (Tables 5 and 6). We affirmed that connective tissue is less elastic, and stiffness increased in POP group. There are significant differences in biomechanical properties between mild type and moderate type and between mild type and severe type. There are no significant differences between moderate type and severe type (Table 7, 8, and 9).
Discussion
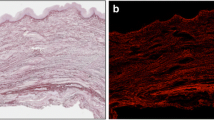
Supports for pelvic organs include the bony pelvis, pelvic floor muscles and fascial supports. The endopelvic fascia is composed of collagen, elastin and smooth muscle. This pelvic supportive tissue contains blood vessels, nerves and fibrous connective tissue and, therefore, functions as a combined neurovascular and supportive structure. POP is said to be due to mechanical, neurological and connective tissue factors. The possible relationship between POP and connective tissue factors has been indirectly implied by the repeated association of clinically significant prolapse and joint hypermobility in women [16]. It is believed that most of the biomechanical properties determined from testing connective tissue are due to collagen. Collagen, as the main component of the pelvic supportive tissue, is responsible for its resisting tensile force. Biomechanical study is based on ultrastructure study. Previous biomechanical studies on premenopausal women demonstrated lowered collagen content in upper vaginal epithelium of women with POP compared with those without [17, 18].
The elastic modulus is the relationship between stress and strain when the relationship is linear. Stress is load or force per unit cross-sectional area, and strain is the change in original length. As a mathematical equation, the elastic modulus is stress divided by strain. Thus, with a higher elastic modulus, the strain–stress curve is steeper. There is a paucity of published literature [19–22] on the “time- or rate-dependent” biomechanical studies of the human vagina. In a study comparing pre- and postmenopausal women with prolapse, Goh demonstrated only age-related changes in full thickness of the anterior vaginal wall tissue strips (5 × 1 cm) collected at the time of vaginal prolapse surgery. This study demonstrated that the only significant difference in biomechanical parameters among the groups was a higher elastic modulus in postmenopausal women, indicating that postmenopausal vaginal tissue was stiffer. At the same time, Cosson adopted a different method to measure the tensile and bending strength of sample of vaginal tissue collected during corrective surgery of prolapse. The study demonstrated that the maximum strength at rupture of the vaginal samples and the elongation before rupture of the samples are greatly variable. The study also demonstrated that there was no relation between the values observed and the patient age. Our study confirmed that the elastic modulus of POP group is higher than of control group; the anterior vaginal wall has reduced elasticity in patients with uterovaginal prolapse. The maximum elongation and maximum fracture are decreased in POP. I think that the difference between our study and Goh’s and Cosson’s might be due to the different race and the small numbers in both groups. Because we are not too sure that if age is related to the biomechanical properties, we eliminate the influence such as age, BMI, parity and time since menopause. So the difference of biomechanical properties between POP group and control group is related to the POP disease, simply. Therefore, the alteration of the biomechanical properties in POP might prove that the function of supports for pelvic organs decreases in pelvic floor dysfunction, and POP might be a functional disease that the biomechanical properties of supports for pelvic organs progressively decrease.
The study also confirmed that there are significant differences between slight type and secondary, gravis type, but no significant differences between secondary type and gravis type. This might be because the pelvic supportive tissue has been destroyed conspicuously when POP comes into secondary or gravis stage. That is, just as when a rubber band is dragged constantly, it eventually breaks, and any mechanical properties’ changes cannot be detected. Hence, when POP is in stages I or II, the expectant treatment such as pelvic floor muscle exercise might be valid.
In a word, pelvic floor support is multifactorial. This study examined biomechanical property of connective tissue of pelvic floor support. As there are few previous reports on biomechanical properties on human vaginal tissue to compare with, the clinical relevance of this study requires further investigation.
References
Jelovsek JE, Barber MD, Paraiso MF, Walters MD (2005) Functional bowel and anorectal disorders in patients with pelvic organ prolapse and incontinence. Am J Obstet Gynecol 193(6):2105–2111
Woodman PJ, Swift SE, O’boyle AL, Valley MT, Bland DR, Kahn MA, Schaffer JI (2006) Prevalence of severe pelvic organ prolapse in relation to job description and socioeconomic status: a multicenter cross-sectional study. Int Urogynecol J Pelvic Floor Dysfunct 17(4):340–345
Auwad W, Bombieri L, Adekanmi O, Waterfield M, Freeman R (2006) The development of pelvic organ prolapse after colposuspension: a prospective, long-term follow-up study on the prevalence and predisposing factors. Int Urogynecol J Pelvic Floor Dysfunct 17(4):389–394
Weber AM, Richter HE (2005) Pelvic organ prolapse. Obstet Gynecol 106(3):615–634
Tegerstedt G, Maehle-Schmidt M, Nyren O, Hammarstrom M (2005) Prevalence of symptomatic pelvic organ prolapse in a Swedish population. Int Urogynecol J Pelvic Floor Dysfunct 16(6):497–503
Lang JH (2005) Urogynecology and reconstructive pelvic surgery: past, present and future 2. Zhonghua Fu Chan Ke Za Zhi 40(3):145–147
Ettema GJC (1997) Mechanical behaviour of rat skeletal muscle during latiguing stretch-shorten cycle. Exp Physiol 82:107–119
Ettema GJC, Goh JTW, Forwood MR (1998) A new method to measure elastic properties of plastic-viscoelastic connective tissue. Med Eng Phys 20:308–314
Wong MY, Harmanli OH, Agar M, Dandolu V, Grody MH (2003) Collagen content of nonsupport tissue in pelvic organ prolapse and stress urinary incontinence. Am J Obstet Gynecol 189(6):1579–1597
FitzGerald MP, Mollenhauer J, Hale DS, Benson JT, Brubaker L (2000) Urethral collagen morphologic characteristics among women with genuine stress incontinence. Am J Obstet Gynecol 182:1565–1574
Norton P, Boyd C, Ekman G, Malmstrom A, Ulmsten U (1994) Decreased collagen synthesis in stress incontinent women. Obstet Gynecol 84:583–586
Falconer C, Ekman G, Malmstrom A, Ulmsten U (1994) Decreased collagen synthesis in stress incontinent women. Obstet Gynecol 84:583–586
Rechberger T, Postawski K, Jakowicki JA, Gunja-Smith Z, Woessner JF (1998) Role of fascial collagen in stress urinary incontinence. Am J Obstet Gynecol 179:1511–1514
Ettema GJC, Goh JTW, Forwood MR (1998) A new method to measure elastic properties of plastic-viscoelastic connective tissue. Med Eng Phys 20:308–314
Bump RC, Mattiasson A, Bo K, Brubaker LT, Delancey JOL, Klarksor P et al (1996) The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol 175:10–17
Bai SW, Choe BH, Kim JY, Park KH (2002) Pelvic organ prolapse and connective tissue abnormalities in Korean women. J Reprod Med 47:231–234
Norton P, Boyd C, Deak S (1992) Collagen synthesis in women with genital prolapse or stress urinary incontinence. Neurourol Urodyn 11:300
Jackson SR, Avery CH, Tarlton JF et al (1996) Changes in metabolism of collagen in genitourinary prolapse. Lancet 347:1658–1661
Landon CR et al (1990) Mechanical properties of fascia during pregnancy: a possible factor in the development of stress incontinence of urine. Contemp Rev Obstet Gynecol 2:40–46
Adekanmi O et al (2005) Cystocele: Does anterior repair fail because of weak vaginal wall tissue? Int Urogynecol J 16(Suppl 2):S72 (Abstract)
Goh JT (2002) Biomechanic properties of prolapse vaginal tissue in pre and post menopausal women. Int Urogynecol J 13(2):76–79
Cosson M, Lambaudie E, Boukerrou M et al (2004) A biomechanical study of the strength of vaginal tissue. Results on 16 post menopausal patients presenting with genital prolpase. Eur J Obstet Gynecol Reprod Biol 112(2):201–205
Author information
Authors and Affiliations
Corresponding author
Additional information
Grant Fujian Science & Technology Bureau Foundation No. 2000I1003.
Rights and permissions
About this article
Cite this article
Lei, L., Song, Y. & Chen, R. Biomechanical properties of prolapsed vaginal tissue in pre- and postmenopausal women. Int Urogynecol J 18, 603–607 (2007). https://doi.org/10.1007/s00192-006-0214-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-006-0214-7