Abstract
Video-thoracoscopic sympathectomy is an effective therapy for patients with severe primary palmar hyperhidrosis who are reaching the latter part of their teenage years. However, the best level, the extent of sympathectomy, and the optimal technique used to interrupt the sympathetic chain remain subjects of debate. Our review shows that single resection should be preferred to multiple levels of resection. In cases of isolated palmar hyperhidrosis, T3 is the level of choice, although T4 may be also reasonable. All procedures have similar outcomes, but sympathicotomy may be preferred because it is more simple and less extensive than others.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Palmar
- Hyperhidrosis
- Excessive sweating
- Surgery
- Thoracoscopy
- Sympathectomy
- Sympathicotomy
- Sympathotomy
- Clipping
- Ramicotomy
Introduction
Primary palmar hyperhidrosis (PH) is an excessive eccrine sweat production that often results in serious disruption of a patient’s social and occupational behavior. It is a condition of unknown origin that begins in childhood, occurs in adolescence, and without specific treatment persists throughout life. Medical management is not very effective, often leading many patients to try multiple unsuccessful treatment modalities. Advances in video-assisted thoracoscopic surgery have allowed video-thoracoscopic sympathectomy (VTS) to become a viable first-line therapy for PH, but at present significant controversy remains regarding the best operation as suggested by recent reviews [1, 2], a Cochrane protocol [3] and an Expert Consensus Report [4]. The best level for sympathectomy, the extent of surgery, and the optimal technique used to interrupt the sympathetic chain remain the subjects of debate in relation to the treatment efficacy and the limitation of unwanted side-effects, especially compensatory hyperhidrosis (CH), the most frequent and feared complication. The goal of the present chapter is to provide answers for such issues.
Search Strategy
In a patients with PH, what is the best level, the proper extent, and the optimal surgical technique to obtain resolution of symptoms and limit CH? To identify all scientific literature that addressed such issues, a search was done on PubMed, EMBASE and Cochrane databases using the following terms: palmar, palm, hand, hyperhidrosis, excessive sweating, surgery, thoracoscopy, sympathectomy, sympathicotomy, sympathotomy, clipping, ramicotomy, and clinical outcomes. The time frame was restricted to articles published in the last decade (from January 2003 to July 2013). Cited references of review articles on PH treatment were manually examined to find additional articles not found in the computerized databases. Additional articles were identified from reference lists of selected articles. Clinical end-points of interest were defined a priori and included both operative and longitudinal outcomes of procedural success, long-term recurrence of symptoms, patient satisfaction with the operation and perceived quality of life, and adverse events. Non-English language papers, case reports, abstracts only, letters, reviews, incomplete reports (studies that did not specify more than one outcomes of interest among sympathectomy for PH) and unpublished data were excluded. In addition, studies were excluded if (i) the population studied included patients with secondary PH in the setting of other medical conditions or (ii) if sympathectomy was performed for other reasons, such as refractory angina pectoris, Buerger’s disease, and Raynaud’s phenomenon. More than 350 English language abstracts were found using the search criteria above reported; of these, 62 papers were selected for the present review and divided in three groups as follows: papers reporting clinical outcomes after single or multiple levels of VTS (Table 57.1); papers comparing the results of different levels of VTS (Table 57.2); and papers evaluating the outcomes of different VTS procedures (Table 57.3).
Results
Overview
Only a small percentage of patients with PH should be considered for surgery. Careful patient selection and preoperative counseling are important to ensure a satisfactory outcome. When evaluating a candidable patient for VTS, it is important to determinate through clinical history, physical examination, and appropriate laboratory tests if hyperhidrosis is primary or secondary in origin, focal or generalized, the anatomic location (single or multiple sites), the severity, and any contraindications to surgery. Detailed quality of life assessment tests and/or tests quantifying sweat produce (Iodine test, Gravimetric test, etc.) are not routinely performed in clinical practice, yet they may helpful in making the diagnosis and/or in directing surgical treatment in selected cases. Finally, patients should also be told of the success and failure rates, and long-term results.
The bulk of the randomized trials and non-randomized comparisons identified the “ideal candidates” for VTS as those who have onset of hyperhidrosis at an early age (usually before 16 years of age), are reaching the latter part of their teenage years at the time of surgery (usually >18 years old), have an appropriate body mass index (<28), report no sweating during sleep, are relatively healthy (no other significant co-morbidities), and do not have bradycardia (resting heart rate <55 beats per minute) [4].
Choice of Level
Once the decision is made for VTS, one main question is: at what level should we perform surgery? For many years, it was believed that the ideal treatment for PH would be sympathectomy at T2, because it was thought that the T2 ganglion was the only one responsible for sympathetic innervation of the upper limbs [5–14]. Subsequently, Lin and Telaranta [67] proposed that CH could be secondary to the interruption of the afferent fibers to the anterior part of the hypothalamus. Since the interruption of the interganglionic T3-T4 trunk did not abolish the sympathetic tone to the hypothalamus, and given that most of the fibers for the hand originate from T4, the best level of section to achieve good results in terms of efficiency and lower CH rate was exactly between T3-T4. Thus, various levels of the procedure from T2 to T4 were performed in recent years [15–34] and several papers showed a correlation between the severity of CH and higher resection levels.
Schmidt et al. [35] demonstrated that changing the sympathectomy level from T2-4 to T3-5 decreased CH from 19.1 to 4.9 % (p < 0.05). Dewey et al. [17] evaluated 222 patients, of whom 60 had PH. The level of sympathectomy depended upon clinical symptoms: T2 for face/scalp, T3 for palmar, and T4 for axillary hyperhidrosis, or a combination of levels for multiarea sweating. Compared with those with other levels, patients with a T2 lesion were significantly more likely to have severe CH (48.8 % versus 16.1 %; p < 0.001) and lower degree of satisfaction. Sugimura et al. [36] evaluated 727 patients with hyperhidrosis, of whom 538 suffered from PH. The level of sympathetic clipping was T2 in 399, T2-3 in 55, and T3-4 in 273 cases. When compared with T2 or T2–3 levels, clipping at the T3-4 levels was associated with a higher satisfaction rate (p < 0.01), and a lower rate of severe CH (p < 0.05). Similarly, Reisfled et al. [37] found that clamping at T3-T4 level had higher rate of success and a lower risk of severe CH compared to T2-T3 levels. Thus, if surgery is required at T2 or T3 levels, Chou et al. [38] strongly recommended the clipping method because of its potential reversibility. The main limit of these papers [17, 35–38] is that the level of sympathectomy depended upon clinical symptoms: T2 for face/scalp, T3 for palmar hyperhidrosis, and T4 for axillary hyperhidrosis, or a combination of levels for multiarea sweating. Thus, in theory the location of the primary sweating rather than the level of resection may affect the outcomes.
Other studies including patients having only PH confirmed that T2 resection resulted in a higher incidence and more degree of CH than lower levels. Yazbeck et al. [39] evaluated T2 (n = 30) versus T3 (n = 30) sympathectomy. The T3 group presented a lower degree of CH in the assessment 1 month (p < 0.001), 6 months (p = 0.033), and 20 months (p = 0.007) after the operation. Baumgartner et al. [40] in T2 sympathicotomy group (n = 61) found a higher incidence of CH than in T3 group (95 % versus 58 %, respectively). Similar results were reported by other authors [41–43]. Chang et al. [44] retrospectively compared the results of T2 (n = 86); T3 (n = 78), and T4 (n = 70) sympathectomy. All three levels of sympathectomy achieved comparable improvement of PH (p = 0.1). The T4 group had the lowest incidence of CS (p = 0.03), presented the least severity of CS (p = 0.002); and felt the least palmar over dryness (p < 0.001). However, the T3 and T4 group had a similar level of satisfaction. Mahdy et al. [45] compared T2; T3; and T4 sympathectomy (20 patients in each group). Treatment success was 90 % for T2; 95 % for T3; and 100 % for T4 groups. In the T2 (60 %) and T3 (45 %) groups a higher incidence of CH was observed than in T4 (10 %; p = 0.01). The CH was mild in T4 group, whereas moderate and/or severe CH was more common in the T2 and T3 groups. All patients in the T4 group were satisfied, while 40 % of T2 and 25 % of T3 were unsatisfied with their operation. Kim et al. [46] compared T3 (n = 56) versus T4 (n = 63) sympathectomy. Both procedures had similar success but T4 sympathectomy resulted in less CH than T3 (82.5 % versus 17.9 %; p < 0.01). Liu et al. [47] evaluated T3 (n = 68) versus T4 (n = 73) sympathicotomy. The success was 100 % in both groups but the incidence of CH and overly dry hands were both lower in the T4 than in the T3 group (56.5 % versus 77.4 %, p = 0.011 and 1.4 % versus 12.9 %, p = 0.013, respectively). The “very satisfied” rate was higher in T4 than in the T3 group (p < 0.0001) while the “partially satisfied” rate was similar between two groups. Ishy et al. [48] reported similar success for T3 versus T4 sympathectomy but the incidence of CH was higher in the T3 than in the T4 group (100 % versus 74 %; p = 0.047). These results were also corroborated by Wolosker et al. [49] and Yang et al. [50].
Single or Multiple Levels of Resection
The need for a combined approach towards the T2 and T3 ganglia has been based on the description of the Kuntz nerve (postganglionic fibers that would go from the T2 or T3 to the brachial plexus). For this reason, in the past some authors have advocated sympathectomy including T2-T3 levels while others proposed more extensive approach going from T2 to T4. Then, several studies reported on the relationship between the extent of thoracic sympathectomy and the severity of CH with a growing consensus that limiting the extent of sympathectomy maximized patient satisfaction and minimized the risk of severe CS [31, 51–58].
Neumayer et al. [51] found that the degree of satisfaction was greater in patients treated at single level than in those treated at multiple levels (100 % versus 80 %), but especially in the first group the incidence of CH was much lower (8 % vs. 52 %). Gossot et al. [31] reported CH rates of 72.2 % in the T2-T4 group and 70.9 % in the T4 group, but severe CH able to influence normal daily activities was described in 27 % of patients in the first group and in 13 % in the second group. Weksler et al. [52] showed that patients with more than one ganglion transected demonstrated a trend toward a higher incidence of CH, a significantly higher CH score, and were more dissatisfied with VTS. Age, surgery on T2, and high CH score were independent predictors of patient’s dissatisfaction. A trial comparing T2-T3 (n = 24) versus T3 (n = 30) sympathicotomy was reported by Yoon et al. [53] The success rate was 100 % in both group. CH was higher in the T2-T3 group than the T3 group (45 % versus 16 %; p = 0.034). 86.7 % of the T3 group and 66.7 % of the T2-T3 group were satisfied with their operation (p = 0.03). Yano et al. [54] compared T2-T3 (n = 39) versus T2 sympathectomy. All patients experienced early relief of their symptoms. The recurrence rates at 2 years were 3 and 19 % in the T2-3 group and the T2 groups, respectively. CH was observed in 100 % (T2-3 group) and 90 % (T2 group); the incidence of severe CH was 76 and 49 % in the T2-T3 and in the T2 groups, respectively. Li et al. [55] compared T3 (n = 117) versus T2-4 (n = 115) sympathectomy. The incidence of severe CH was significantly lower in the T3 versus the T2-4 group (3 % versus 10 %; p < 0.05). As for satisfaction rate, group T3 was superior to group T2-4 (96.6 % versus 89.6 %, p < 0.05). Aoki et al. [56] confirmed that VTS at a single level compared to two levels reduced the incidence and the severity of CH. Katara et al. [57] and Turhan et al. [58] reported no difference in terms of outcome, recurrence, CH, and satisfaction between single and multiple levels, validating that preserving the T2 ganglion was safe and did not compromise the effectiveness of the procedure.
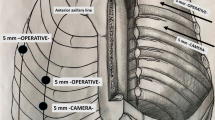
Type of Denervation
The technique of sympathetic denervation has been modified during the last decade, with a trend towards minimizing the extent of surgery from open to minimally invasive approaches, and from resection of ganglion to ablation (sympathectomy), transection (sympathicotomy), differential dissection (ramicotomy), and clipping. The rationale of ramicotomy is to achieve a selective division of the sympathetic postganglionic fibers that supply the eccrine glands of the upper extremity. Lee et al. [43] compared patients undergoing T2 sympathicotomy vs T3 ramicotomy. CH was approximately two-thirds lower in ramicotomy group but a lower rate of success was reported in ramicotomy than in sympathicotomy group (93 % versus 68 %, respectively). Cho et al. [59] found that the incidence of severe CH was lower in ramicotomy than sympathicotomy group (54 % versus 92 %, respectively) but the first group presented a higher recurrence rates (21 % versus 6 %, respectively). Recently, Hwang et al. [60] compared T3 sympathicotomy (n = 43) versus T2-3 ramicotomy (n = 43) showing that sympathicotomy had better outcomes than ramicotomy in terms of success (82 % versus 25 %, respectively); CH (80 % versus 95 %); and satisfaction (91 % versus 79 %, respectively).
The less than optimal results may be due to poor visualization of the anatomy of the sympathetic chain and the communicating fibers with conventional videothoracoscopy. Thus, Coveliers et al. [32] proposed the use of robotic technology to magnify visualization of the surgical field and facilitate complex maneuvers. Thirty-six patients underwent robotic T2-4 ramicotomy. The success rate was 100 %; the incidence of CH was 8.3 %. However, the main limit of robotic procedure is the high cost.
The theoretical possibility of procedural reversibility with clamping or clipping the nerve instead of other procedures in the event of severe CH has led some authors to advocate leaving the nerve in continuity. Neumayer et al. [51] found a significantly decreased incidence of CH (86 % versus 100 %) and higher rate of satisfaction (80 % versus 100 %, respectively) in clipping compared to sympathicotomy group. Lin et al. [14] reported a success of 98 % after T2 block. In two cases with severe CH a full reversibility was obtained after unclipping. Conversely, other authors did not show any advantage of clipping versus sympathectomy or sympathicotomy. Findikcioglu et al. [61] compared T3 sympathectomy (n = 28) versus T3 clipping (n = 32). Both clipping and cauterization were highly effective for the treatment of PH with success rates of 93 % and 100 %, respectively. The methods were comparable in terms of effectiveness and side effects despite the fact that the recurrence rate was higher in the cauterization than clipping group (19 % versus 6 %, respectively, p = 0.01). Inan et al. [62] evaluated four different VTS procedures at the T2-4 level including: resection (n = 20), transection (n = 20), ablation (n = 20), and clipping (n = 20). No significant differences were seen between the four groups with regard to success or complication rates. The overall success rate of the operation was 95 %; no recurrence was observed; and more than 20 % of patients complained of CH irrespective of the surgical technique adopted. Yanagihara et al. [63] compared T3 sympathectomy versus T3 clamping. Among two groups, there were no differences in any outcome, including CH and quality of life. Similar results were reported by Scognamillo et al. [64].
Despite the initial enthusiasm, the presumption that the patient can return for “surgical reversal” by removing the clip appears dubious. Chou et al. [38] and Sugimura et al. [36] reported a resolution of CH in 76 and 47 %, respectively, of patients undergoing the reversal procedure. The clip reversal procedures are imperfect with only a limited window in which the opportunity for reversal exists. If the clip has produced cell body death or reorganization within the spinal cord, then the abnormal modulation of sympathetic output causing CH will likely not resolve. The findings of a recent animal study [68] showed that after unclipping, although the nerve appeared to recover normal morphology, and although local inflammatory cells disappear, there was a striking and almost complete absence of amyelinate fibers suggesting that there was no nerve regeneration.
Sympathicotomy intentionally does not remove or injure ganglia of the chain or axons from spinal cord neurons innervating the ganglia. Thus, some authors [13, 15, 27] supported that such procedure had a potential lower risk of CH than sympathectomy due to the less extensive areas of skin anhydrosis. However, Inan et al. [62] showed no clear differences among two procedures. Assalia et al. [65] found that sympathectomy may achieve slightly better long term results than sympathicomy. Because both techniques were used in the same patient, the differences between techniques as to the occurrence of CH could not be assessed in this study [65]. The authors [66] found no significant difference between two procedures in terms of success, recurrence and CH but sympathectomy compared to sympathicotomy resulted in a sub-clinical disturbance of bronchomotor tone and cardiac function theoretically correlated with the extent of denervation.
Recommendations
From the analysis of the literature, surgery is indicated in patients with severe primary hyperhidrosis who are reaching the latter part of their teenage years (usually >18 years old) and in whom all secondary causes of hyperhidrosis have been ruled out. CH is significantly more likely to be severe in those patient who had the T2 ganglia excised [17, 35–43]. Seven studies compared the T3 versus the T4 level [44–50]. Resolution of symptoms was favored in the T3 groups in three studies [44, 46, 49] and the T4 group in one study [45]. Three studies were similar in outcomes [47, 48, 50]. However, all seven studies [44–50] reported a reduction of CH in the T4 groups. Nine papers compared the occurrence of CH after sympathetic chain resection at a single levels versus multiple levels [31, 51–58]. All papers but two [57, 58] showed a strong correlation between the number of levels excised and the degree of CH. Eleven papers compared different techniques of sympathetic chain resection [38, 43, 51, 59–66]. In one paper [51] clipping was superior to sympathicotomy and in another [43] ramicotomy was superior to sympathicotomy. However in both studies, the procedures were attended at different anatomical level that may affected the results. Nine papers [38, 59–66] found no significant differences among the various procedures. In the light of these results, single resection is preferred to multiple levels of resection. In case of isolated PH, T3 is the level of choice although T4 interruption may be also reasonable. Sympathicotomy may be preferred to sympathectomy because it is more simple and less extensive and has similar outcomes.
A Personal View of the Data
The literature on VTS must be carefully interpreted. Most of the current evidences comes from observational studies. Some papers comparing different level of resection present a lack of uniformity in patient populations. Not all studies assess and/or quantify the degree of CH similarly or at the same point postoperatively. Because the incidence of recurrence and/or of CH may increase with time regardless of the level resected, the differences in the follow-up period among different papers may interfere in the analysis of the outcomes. In theory, the shortest duration of follow-up may account for the lowest incidence of recurrence and/or of CH after surgery. Objective specific tests and/or questionnaires to quantify the sweating and the clinical improvement after surgery are rarely used, and most papers simply rely on subjective reporting by the patient. Some authors do not use the term sympathectomy with extreme precision; sometimes a sympathicotomy is done, leaving the ganglion intact. Thus the true level of sympathectomy/sympathicotomy is also something that should not always be presumed accurate in various reports. Especially in novices, confusion may arise as to the true ganglion or rib level, and published errors or questions of level exist. Although the differentiation may seem subtle, the clinical implications are huge and may well impact on the mishmash of conflicting conclusions regarding the level and the extent of resection.
We currently limit the extent of our resection for isolated PH to a single level, generally T3 at the top of the third rib. In the event that patient has multisite sweating (i.e. palmar associated with facial or axillar hyperhidrosis) and requires multilevel resections, we advise the patient regarding the increased risk of CH. We have not tested clip blocking in our unit, because we are unsure of its reversibility. Sympathectomy is the procedure of choice; however, in selected cases sympathicotomy may be preferred for the lower incidence of adverse effects, especially on cardio-respiratory function. We believe that in the future a standardized nomenclature (i.e. for the level of resection and/or the procedures adopted) and follow-up algorithms or surveys should be adopted in order to allow surgeons from all over the world to better communicate with one another and compare their results.
Recommendations
-
Surgery is indicated in patients with severe primary palmar hyperhidrosis who are reaching the latter part of their teenage years (Evidence quality moderate; strong recommendation)
-
Single resection is preferred over multiple levels of resection. (Evidence quality low; weak recommendation)
-
T3 is the level of choice, althoughT4 interruption may be also reasonable. (Evidence quality moderate; weak recommendation)
-
Sympathicotomy is preferred over sympathectomy because it is more simple, is less extensive, and has similar outcomes. (Evidence quality low; weak recommendation)
References
Deng B, Tan QY, Jiang YG, Zhao YP, Zhou JH, Ma Z, Wang RW. Optimization of sympathectomy to treat palmar hyperhidrosis: the systematic review and meta-analysis of studies published during the past decade. Surg Endosc. 2011;25(6):1893–901.
Moreno Balsalobre R, Moreno Mata N, Ramos Izquierdo R, Aragón Valverde FJ, Molins López-Rodo L, de Andrés Rivas JJ, García Fernández JL, Cañizares Carretero MÁ, Congregado Loscertales M, Carbajo Carbajo M, SEPAR. Guidelines on surgery of the thoracic sympathetic nervous system. Arch Bronconeumol. 2011;47(2):94–102.
Rzany BBR, Spinner D. Interventions for localised excessive sweating. Cochrane Database Syst Rev. 2001; (1): CD002953. doi: 10.1002/14651858.CD002953.
Cerfolio RJ, De Campos JR, Bryant AS, Connery CP, Miller DL, DeCamp MM, McKenna RJ, Krasna MJ. The Society of Thoracic Surgeons expert consensus for the surgical treatment of hyperhidrosis. Ann Thorac Surg. 2011;91(5):1642–8.
Neumayer C, Zacherl J, Holak G, Jakesz R, Bischof G. Experience with limited endoscopic thoracic sympathetic block for hyperhidrosis and facial blushing. Clin Auton Res. 2003;13 Suppl 1:I52–7.
Schick CH, Fronek K, Held A, Birklein F, Hohenberger W, Schmelz M. Differential effects of surgical sympathetic block on sudomotor and vasoconstrinctor function. Neurology. 2003;60(11):1770–6.
Atkinson JL, Fealey RD. Sympathotomy instead of sympathectomy for palmar hyperhidrosis: minimizing postoperative compensatory hyperhidrosis. Mayo Clin Proc. 2003;78:167–72.
Lladó A, León L, Valls-Solé J, Mena P, Callejas MA, Peri JM. Changes in the sympathetic skin response after thoracoscopic sympathectomy in patients with primary palmar hyperhidrosis. Clin Neurophysiol. 2005;116(6):1348–54.
Ting H, Lee SD, Chung AH, Chuang ML, Chen GD, Liao JM, Chang CL, Chiou TS, Lin TB. Effects of bilateral T2-sympathectomy on static and dynamic heart rate responses to exercise in hyperhidrosis patients. Auton Neurosci. 2005;121(1–2):74–80.
Eisenach JH, Pike TL, Wick DE, Dietz NM, Fealey RD, Atkinson JL, Charkoudian N. A comparison of peripheral skin blood flow and temperature during endoscopic thoracic sympathectomy. Anesth Analg. 2005;100(1):269–76.
Miller DL, Force SD. Outpatient microthoracoscopic sympathectomy for palmar hyperhidrosis. Ann Thorac Surg. 2007;83(5):1850–3.
Leis S, Meyer N, Bickel A, Schick CH, Kruger S, Schmelz M, Birklein F. Thoracoscopic sympathectomy at the T2 or T3 level facilitates bradykinin-induced protein extravasation in human forearm skin. Pain Med. 2010;11(5):774–80.
Atkinson JL, Fode-Thomas NC, Fealey RD, Eisenach JH, Goerss SJ. Endoscopic transthoracic limited sympathotomy for palmar-plantar hyperhidrosis: outcomes and complications during a 10-year period. Mayo Clin Proc. 2011;86(8):721–9.
Lin TS, Chou MC. Treatment of palmar hyperhidrosis using needlescopic T2 sympathetic block by clipping: analysis of 102 cases. Int Surg. 2004;89(4):198–201.
Yoon DH, Ha Y, Park YG, Chang JW. Thoracoscopic limited T-3 sympathicotomy for primary hyperhidrosis: prevention for compensatory hyperhidrosis. J Neurosurg. 2003;99(1 Suppl):39–43.
Doolabh N, Horswell S, Williams M, Huber L, Prince S, Meyer DM, Mack MJ. Thoracoscopic sympathectomy for hyperhidrosis: indications and results. Ann Thorac Surg. 2004;77(2):410–4.
Dewey TM, Herbert MA, Hill SL, Prince SL, Mack MJ. One-year follow-up after thoracoscopic sympathectomy for hyperhidrosis: outcomes and consequences. Ann Thorac Surg. 2006;81(4):1227–32.
Weksler B, Luketich JD, Shende MR. Endoscopic thoracic sympathectomy: at what level should you perform surgery? Thorac Surg Clin. 2008;18(2):183–91.
Lima AG, Marcondes GA, Teixeira AB, Toro IF, Campos JR, Jatene FB. The incidence of residual pneumothorax after video-assisted sympathectomy with and without pleural drainage and its effect on postoperative pain. J Bras Pneumol. 2008;34(3):136–42.
Fiorelli A, Vicidomini G, Laperuta P, Busiello L, Perrone A, Napolitano F, Messina G, Santini M. Pre-emptive local analgesia in video-assisted thoracic surgery sympathectomy. Eur J Cardiothorac Surg. 2010;37(3):588–93.
Zhu LH, Wang W, Yang S, Li D, Zhang Z, Chen S, Cheng X, Chen L, Chen W. Transumbilical thoracic sympathectomy with an ultrathin flexible endoscope in a series of 38 patients. Surg Endosc. 2013;27(6):2149–55.
Chou SH, Kao EL, Li HP, Lin CC, Huang MF. T4 sympathectomy for palmar hyperhidrosis: an effective approach that simultaneously minimizes compensatory hyperhidrosis. Kaohsiung J Med Sci. 2005;21(7):310–3.
Baumgartner FJ, Toh Y. Severe hyperhidrosis: clinical features and current thoracoscopic surgical management. Ann Thorac Surg. 2003;76(6):1878–83.
Loscertales J, Arroyo Tristán A, Congregado Loscertales M, Jiménez Merchán R, Girón Arjona JC, Arenas Linares C, Ayarra Jarné J. Thoracoscopic sympathectomy for palmar hyperhidrosis. Immediate results and postoperative quality of life. Arch Bronconeumol. 2004;40(2):67–71.
De Campos de Campos JR, Wolosker N, Takeda FR, Kauffman P, Kuzniec S, Jatene FB, de Oliveira SA. The body mass index and level of resection: predictive factors for compensatory sweating after sympathectomy. Clin Auton Res. 2005;15(2):116–20.
Sihoe AD, Manlulu AV, Lee TW, Thung KH, Yim AP. Pre-emptive local anesthesia for needlescopic video-assisted thoracic surgery: a randomized controlled trial. Eur J Cardiothorac Surg. 2007;31(1):103–8.
Jeganathan R, Jordan S, Jones M, Grant S, Diamond O, McManus K, Graham A, McGuigan J. Bilateral thoracoscopic sympathectomy: results and long-term follow-up. Interact Cardiovasc Thorac Surg. 2008;7(1):67–70.
Little AG. Video-assisted thoracic surgery sympathectomy for hyperhidrosis. Arch Surg. 2004;139(6):586–9.
Georghiou GP, Berman M, Bobovnikov V, Vidne BA, Saute M. Minimally invasive thoracoscopic sympathectomy for palmar hyperhidrosis via a transaxillary single-port approach. Interact Cardiovasc Thorac Surg. 2004;3(3):437–41.
Moya J, Ramos R, Morera R, Villalonga R, Perna V, Macia I, Ferrer G. Thoracic sympathicolysis for primary hyperhidrosis: a review of 918 procedures. Surg Endosc. 2006;20(4):598–602.
Gossot D, Galetta D, Pascal A, Debrosse D, Caliandro R, Girard P, Stern JB, Grunenwald D. Long-term results of endoscopic thoracic sympathectomy for upper limb hyperhidrosis. Ann Thorac Surg. 2003;75(4):1075–9.
Coveliers H, Meyer M, Gharagozloo F, Wisselink W, Rauwerda J, Margolis M, Tempesta B, Strother E. Robotic selective postganglionic thoracic sympathectomy for the treatment of hyperhidrosis. Ann Thorac Surg. 2013;95(1):269–74.
Apiliogullari B, Esme H, Yoldas B, Duran M, Duzgun N, Calik M. Early and midterm results of single-port video-assisted thoracoscopic sympathectomy. Thorac Cardiovasc Surg. 2012;60(4):285–9.
Prasad A, Ali M, Kaul S. Endoscopic thoracic sympathectomy for primary palmar hyperidrosis. Surg Endosc. 2010;24(8):1952–7.
Schmidt J, Bechara FG, Altmeyer P, Zirngibl H. Endoscopic thoracic sympathectomy for severe hyperhidrosis: impact of restrictive denervation on compensatory sweating. Ann Thorac Surg. 2006;81(3):1048–55.
Sugimura H, Spratt EH, Compeau CG, Kattail D, Shargall Y. Thoracoscopic sympathetic clipping for hyperhidrosis: long-term results and reversibility. J Thorac Cardiovasc Surg. 2009;137(6):1370–6; discussion 1376–7.
Reisfeld R. Sympathectomy for hyperhidrosis: should we place the clamps at T2-T3 or T3-T4? Clin Auton Res. 2006;16(6):384–9.
Chou SH, Kao EL, Lin CC, Chang YT, Huang MF. The importance of classification in sympathetic surgery and a proposed mechanism for compensatory hyperhidrosis: experience with 464 cases. Surg Endosc. 2006;20(11):1749–53.
Yazbek G, Wolosker N, Kauffman P, Campos JR, Puech-Leão P, Jatene FB. Twenty months of evolution following sympathectomy on patients with palmar hyperhidrosis: sympathectomy at the T3 level is better than at the T2 level. Clinics. 2009;64(8):743–9.
Baumgartner FJ, Reyes M, Sarkisyan GG, Iglesias A, Reyes E. Thoracoscopic sympathicotomy for disabling palmar hyperhidrosis: a prospective randomized comparison between two levels. Ann Thorac Surg. 2011;92(6):2015–9.
Lin M, Tu YR, Li X, Lai FC, Chen JF, Dai ZJ. Comparison of curative effects of sympathectomy at different segments on palmar hyperhidrosis. Zhonghua Yi Xue Za Zhi. 2006;86(33):2315–7.
Miller DL, Bryant AS, Force SD, Miller Jr JI. Effect of sympathectomy level on the incidence of compensatory hyperhidrosis after sympathectomy for palmar hyperhidrosis. J Thorac Cardiovasc Surg. 2009;138(3):581–5.
Lee DY, Kim DH, Paik HC. Selective division of T3 rami communicantes (T3 ramicotomy) in the treatment of palmar hyperhidrosis. Ann Thorac Surg. 2004;78(3):1052–5.
Chang YT, Li HP, Lee JY, Lin PJ, Lin CC, Kao EL, Chou SH, Huang MF. Treatment of palmar hyperhidrosis: T(4) level compared with T(3) and T(2). Ann Surg. 2007;246(2):330–6.
Mahdy T, Youssef T, Elmonem HA, Omar W, Elateef AA. T4 sympathectomy for palmar hyperhidrosis: looking for the right operation. Surgery. 2008;143(6):784–9.
Kim WO, Kil HK, Yoon KB, Yoon DM, Lee JS. Influence of T3 or T4 sympathicotomy for palmar hyperhidrosis. Am J Surg. 2010;199(2):166–9.
Liu Y, Yang J, Liu J, Yang F, Jiang G, Li J, Huang Y, Wang J. Surgical treatment of primary palmar hyperhidrosis: a prospective randomized study comparing T3 and T4 sympathicotomy. Eur J Cardiothorac Surg. 2009;35(3):398–402.
Ishy A, de Campos JR, Wolosker N, Kauffman P, Tedde ML, Chiavoni CR, Jatene FB. Objective evaluation of patients with palmar hyperhidrosis submitted to two levels of sympathectomy: T3 and T4. Interact Cardiovasc Thorac Surg. 2011;12(4):545–8.
Wolosker N, Yazbek G, Ishy A, de Campos JR, Kauffman P, Puech-Leão P. Is sympathectomy at T4 level better than at T3 level for treating palmar hyperhidrosis? J Laparoendosc Adv Surg Tech A. 2008;18(1):102–6.
Yang J, Tan JJ, Ye GL, Gu WQ, Wang J, Liu YG. T3/T4 thoracic sympathictomy and compensatory sweating in treatment of palmar hyperhidrosis. Chin Med J. 2007;120(18):1574–7.
Neumayer C, Zacherl J, Holak G, Függer R, Jakesz R, Herbst F, Bischof G. Limited endoscopic thoracic sympathetic block for hyperhidrosis of the upper limb: reduction of compensatory sweating by clipping T4. Surg Endosc. 2004;18(1):152–6.
Weksler B, Blaine G, Souza ZB, Gavina R. Transection of more than one sympathetic chain ganglion for hyperhidrosis increases the severity of compensatory hyperhidrosis and decreases patient satisfaction. J Surg Res. 2009;156(1):110–5.
Yoon SH, Rim DC. The selective T3 sympathicotomy in patients with essential palmar hyperhidrosis. Acta Neurochir (Wien). 2003;145(6):467–71.
Yano M, Kiriyama M, Fukai I, Sasaki H, Kobayashi Y, Mizuno K, Haneda H, Suzuki E, Endo K, Fujii Y. Endoscopic thoracic sympathectomy for palmar hyperhidrosis: efficacy of T2 and T3 ganglion resection. Surgery. 2005;138(1):40–5.
Li X, Tu YR, Lin M, Lai FC, Chen JF, Dai ZJ. Endoscopic thoracic sympathectomy for palmar hyperhidrosis: a randomized control trial comparing T3 and T2-4 ablation. Ann Thorac Surg. 2008;85(5):1747–51.
Aoki H, Sakai T, Murata H, Sumikawa K. Extent of sympathectomy affects postoperative compensatory sweating and satisfaction in patients with palmar hyperhidrosis. J Anesth. 2014;28(2):210–3.
Katara AN, Domino JP, Cheah WK, So JB, Ning C, Lomanto D. Comparing T2 and T2–T3 ablation in thoracoscopic sympathectomy for palmar hyperhidrosis: a randomized control trial. Surg Endosc. 2007;21(10):1768–71.
Turhan K, Cakan A, Cagirici U. Preserving T2 in thoracic sympathicotomy for palmar hyperhidrosis: less tissue trauma, same effectiveness. Thorac Cardiovasc Surg. 2011;59(6):353–6.
Cho HM, Chung KY, Kim DJ, Lee KJ, Kim KD. The comparison of VATS ramicotomy and VATS sympathicotomy for treating essential hyperhidrosis. Yonsei Med J. 2003;44(6):1008–13.
Hwang JJ, Kim do H, Hong YJ, Lee DY. A comparison between two types of limited sympathetic surgery for palmar hyperhidrosis. Surg Today. 2013;43(4):397–402.
Findikcioglu A, Kilic D, Hatipoglu A. Is clipping superior to cauterization in the treatment of palmar hyperhidrosis? Thorac Cardiovasc Surg. 2013: (in press). PubMed PMID: 23839873.
Inan K, Goksel OS, Uçak A, Temizkan V, Karaca K, Ugur M, Arslan G, Us M, Yilmaz AT. Thoracic endoscopic surgery for hyperhidrosis: comparison of different techniques. Thorac Cardiovasc Surg. 2008;56(4):210–3.
Yanagihara TK, Ibrahimiye A, Harris C, Hirsch J, Gorenstein LA. Analysis of clamping versus cutting of T3 sympathetic nerve for severe palmar hyperhidrosis. J Thorac Cardiovasc Surg. 2010;140(5):984–9.
Scognamillo F, Serventi F, Attene F, Torre C, Paliogiannis P, Pala C, Trignano E, Trignano M. T2-T4 sympathectomy versus T3-T4 sympathicotomy for palmar and axillary hyperhidrosis. Clin Auton Res. 2011;21(2):97–102.
Assalia A, Bahouth H, Ilivitzki A, Assi Z, Hashmonai M, Krausz MM. Thoracoscopic sympathectomy for primary palmar hyperhidrosis: resection versus transection – a prospective trial. World J Surg. 2007;31(10):1976–9.
Fiorelli A, D’Aponte A, Canonico R, Palladino A, Vicidomini G, Limongelli F, Santini M. T2-T3 sympathectomy versus sympathicotomy for essential palmar hyperhidrosis: comparison of effects on cardio-respiratory function. Eur J Cardiothorac Surg. 2012;42(3):454–61.
Lin CC, Telaranta T. Lin-Telaranta classification: the importance of different procedures for different indications in sympathetic surgery. Ann Chir Gynaecol. 2001;90(3):161–6.
Loscertales J, Congregado M, Jimenez-Merchan R, Gallardo G, Trivino A, Moreno S, Loscertales B, Galera-Ruiz H. Sympathetic chain clipping for hyperhidrosis is not a reversible procedure. Surg Endosc. 2012;26(5):1258–63.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag London
About this chapter
Cite this chapter
Santini, M., Fiorelli, A. (2014). Surgery for Palmar Hyperhidrosis: Patient Selection and Extent of Surgery. In: Ferguson, M. (eds) Difficult Decisions in Thoracic Surgery. Difficult Decisions in Surgery: An Evidence-Based Approach, vol 1. Springer, London. https://doi.org/10.1007/978-1-4471-6404-3_57
Download citation
DOI: https://doi.org/10.1007/978-1-4471-6404-3_57
Published:
Publisher Name: Springer, London
Print ISBN: 978-1-4471-6403-6
Online ISBN: 978-1-4471-6404-3
eBook Packages: MedicineMedicine (R0)