Abstract
Background
Bilateral upper thoracic sympathectomy or sympathicolysis, currently the standard treatment for palmar or axillary hyperhidrosis, is regarded as a safe procedure. This study evaluates the quantitative and qualitative incidence of intraoperative and postoperative complications resulting from bilateral thoracic sympathicolysis.
Methods
From 1996 to 2004, 458 consecutive patients with primary hyperhidrosis underwent surgery. These patients comprised 143 men (31.2%) and 315 women (68.7%) with a mean age of 26 years (range, 14–52 years). In all but seven cases, the procedure was bilaterally synchronous.
Results
No mortality was recorded. The anhydrosis rate was 97.4%, with a hypohidrosis rate of 2.4% and a failure rate of 0.2%. The latter was resolved with reintervention. The mean hospital stay was 17 h. The rate of major perioperative complications with conversion to thoracotomy was 0.4%. The overall rate of postoperative complications was 3.6%. The complications and rates observed were as follows: pneumothorax (2.06%), subcutaneous emphysema (1.08%), pleural bleeding (0.2%), hemothorax (0.1%), and atelectasis (0.1%). Compensatory hyperhidrosis was observed in 48.4% of the patients, but the sensation of compensatory hyperhidrosis was reported in 85.6% of the cases. Excessive dryness of the hands was reported in 0.38%, Horner’s syndrome in 0.32%, and gustatory hyperhidrosis in 1.1% of the cases. The overall satisfaction rate was 88.5%.
Conclusions
The results suggest that endoscopic bilateral thoracic sympathicolysis is an effective method for managing primary hyperhidrosis, especially severe palmar hyperhidrosis, but it is necessary to inform patients fully concerning the undesirable effects.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Primary hyperhidrosis is a clinical condition of unknown etiology characterized by excessive sweating, typically on the palms of the hands, on the soles of the feet, and in the armpits. The condition affects up to 1% of the population. The glandular response is heightened by emotional stimuli, ambient temperature, or elevated anxiety levels.
Although the predominant symptom is excessive sweating, there may be associated symptoms suggestive of sympathetic hyperactivity such as reddening of the face, trembling, headache, and high levels of anxiety. It is difficult to determine whether these symptoms are a matter of cause or consequence. It is clear, however, that these symptoms produce general distress that can interfere with the everyday social and working lives of patients [25, 26]. The symptoms of primary hyperhidrosis usually begin in childhood or adolescence.
Bilateral upper thoracic sympathectomy or sympathicolysis currently is the standard treatment for primary hyperhidrosis [4, –21, 22, 31]. The aim of this study was to analyze the overall results obtained for 458 primary hyperhidrosis patients treated with bilateral upper thoracic sympathicolysis.
Patients and methods
From 1996 to 2004, 458 patients consecutively underwent surgery for upper limb primary hyperhidrosis or facial hyperhidrosis. Bilateral thoracic sympathicolysis was performed. The patients comprised 143 men (31.2%) and 315 women (68.7%) with a mean age of 26.8 years. In all but seven cases, the procedure was bilaterally synchronous. Written information about the technique along with the results and side effects was given to the patients during the first consultation. Individual consent was obtained before the surgery.
This study was approved by the ethics committee (equivalent in Spain to the institutional review board in the United States). All the patients underwent the same preoperative study, which consisted of clinical history, simple chest x-ray, electrocardiogram, complete hemogram, general biochemistry with coagulation parameters, determination of thyroid function, and simple spirometry. Patients with a history of asthma had their bronchial reactivity assessed by means of a metacholine provocation test that measured possible variations in their responsiveness. If the test yielded positive results, they were treated with inhaled corticoids 2 months before surgery.
The surgical protocol consisted of the following. General anesthesia was administered with double-lumen endotracheal intubation. The patient was placed in a 25° semisitting position with abduction of the upper extremities and semi-extension of the forearms. The table was lateralized about 10° toward the opposite side of the hemithorax under surgery, and a single entry port was created for the 5-mm Wolf endoscope (5.5/3.5 mm 0°; Richard Ellis Wolf, University of Leipzig, Leipzig, Germany) at the level of the third intercostal space and axillary midline. The rib spaces and corresponding segment of the upper thoracic sympathetic chain then were visualized in their locations 0.5 to 1 cm laterally from the head of the rib. Sympathicolysis was applied to the T2–T3 ganglia in cases of palmar hyperhidrosis and to the T2–T3–T4 in axillary patients by means of electrocoagulation with monopolar forceps at 25 W in series of 5 to 10 applications cutting the chain at the level of the ribs. Collateral nerve trunks were coagulated (nerve of Kuntz). Hemostasia and evacuation of the pneumothorax were accomplished by means of air aspiration through the endoscope working channel. No drain was left in place. The patients were discharged 17 h after the intervention if x-rays were favorable.
Data collection
All the patients completed a preoperative questionnaire 8 weeks before surgery. The independent study variables were family history of primary hyperhidrosis, location of the hyperhidrosis, associated symptoms, and negative repercussions of the primary hyperhidrosis on family, friends, spouse/partner, and work.
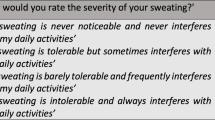
The patients completed another questionnaire 12 weeks after surgery to record data about postoperative pain, partial drooping of the eyelid, gustatory hyperhidrosis, degree of hand dryness, and degree of palmar or axillary hypohidrosis.
Evaluation of the results included another self-administered specific questionnaire or a telephone contact annually for 5 years. The patients with a minimal follow-up period of 18 months were selected to register compensatory hyperhidrosis, and those with a minimal follow-up period of 24 months were selected to register satisfaction or dissatisfaction with the surgery.
Results
Epidemiologic results
A family history of primary hyperhidrosis was reported by 49% of the patients. Concerning the distribution of primary hyperhidrosis, 131 patients had palmar hyperhidrosis (28.6%), 66 had palmar-axillary hyperhidrosis (14.4%), 144 had palmar-axillary-plantar hyperhidrosis (31.4%), 95 had palmar-plantar hyperhidrosis (20.7%), 11 had axillary hyperhidrosis (2.4%), 2 had palmar-facial hyperhidrosis (0.4%), 5 had facial hyperhidrosis (1.1%), and 4 had palmar-axillary-facial-plantar hyperhidrosis (0.9%). In terms of accompanying symptoms, facial reddening was reported by 298 patients (65.1%), palpitations by 262 patients (57.2%), trembling of the hands by 159 patients (34.7%), and headaches by 152 patients (33.2%).
Relationships with friends and with associates in the work environment are the two areas most affected by primary hyperhidrosis. These were reported, respectively, in 74.3% and 89% of the cases.
Efficacy of the procedure
Anhydrosis of the target area was achieved by 97.4% of the procedures. Hypohidrosis (visible improvement but not complete dryness) was achieved for 2.4% of the patients, and two procedures (0.2%) failed. Complete anhydrosis was achieved in the latter cases through reintervention. The mean postoperative hospital stay was 17 h.
Perioperative complications
No mortality was recorded for either group. There was an intraoperative morbidity rate of 0.4% (4/918). Conversion to thoracotomy was required in four cases. One conversion was needed to manage hemopericardium 4 h after surgery. Another procedure presented hemothorax with hemodynamic instability that required thoracotomy 24 h after surgery, and two patients presented with a prolonged air leak, which was treated using axillary thoracotomy and pleurodesis.
Postoperative complications
The overall rate of complications was 3.6% (33/918 procedures). The complications included pneumothorax (2.06%, 19/918), which required drainage with 0.5% (5/918) of the procedures; pleural bleeding (0.2%, 2/918); pleural effusion (hemothorax) (0.1%, 1/918) 2 weeks after the surgery secondary to pseudoaneurysm of the intercostal artery, which was resolved via embolization and respiratory physiotherapy without the need for thoracic drainage; isolated radiologic subcutaneous emphysema (1.08%, 10/918); and atelectasis (0.1%, 1/918).
Pain during the first month after intervention was reported in 370 cases (80.7%), after 1 to 2 months in 56 cases (12.2 %), and after more than 2 months in 32 cases (7%). Because of pain, 10 patients (2.2%) had to be signed off work for 2 weeks after the intervention. After 3 months, only one patient (0.2%) had invalid pain (sympathetic neuralgia).
Undesirable effects
Compensatory hyperhidrosis
This condition was evaluated by selecting 325 patients for a minimum follow-up evaluation of 18 months. The patients were contacted by telephone, and a specific questionnaire was given during another consultation in January 2004. Complete follow-up evaluation was achieved for 285 patients (87.7%). A sensation of compensatory hyperhidrosis was reported in 244 cases (85.6%). However, when the degree of sweating in different body regions was compared according to the preoperative and postoperative questionnaires, only 138 cases (48.4%) showed changes in the degree of sweating. The body regions with significant changes in sweating were the trunk (increased sweating) and the feet (reduced sweating).
Hypohidrosis
Hypohidrosis of the denervated area was recorded 12 weeks after 22 of the interventions (2.4%): 14 (1.5%) involving palmar hypohidrosis and 8 (0.87%) involving axillary hypohidrosis.
Excessive dryness of the hands
This condition was reported in two cases (0.43%), involving both extremities.
Unilateral partial Horner syndrome
This condition was recorded for three procedures (0.3%), with all three patients recovering within 12 months after the intervention.
Gustatory hyperhidrosis
This condition was reported by only five patients (1.1%). Hyperhidrosis developed on the thorax, neck, and back associated with eating foods. This gustatory hyperhidrosis is activated by chocolate.
Level of satisfaction
To study the level of satisfaction, 350 patients were evaluated over a minimum follow-up period of 24 months. All the patients were contacted by telephone, with 310 (88.5%) describing themselves as very satisfied, 32 (9.1%) reporting that they were dissatisfied, and 8 (2.3%) saying that they were very dissatisfied after the intervention, even regretting that they had undergone the operation.
Discussion
In the absence of specific and effective medical treatment for primary hyperhidrosis, the interventions most widely accepted by authors working in the field are sympathectomy and sympathicolysis [4, 5, 7, 21, 22, 37].
Although no mortality was recorded in our surgical series of 918 procedures, the literature does contain reports of deaths secondary to cerebral edema [2], possibly in relation to carbon dioxide insufflation in the pleural cavity. Carbon dioxide insufflation is routinely performed during laparoscopic surgery to achieve and maintain the pneumoperitoneum during the intervention. In our clinical practice, we induce pneumothorax by means of selective bronchial intubation and the passive entry of air through the working port.
In terms of the epidemiologic results in our series, 49% of the patients reported a family history of primary hyperhidrosis. The reports indicated a predominantly palmar-axillary-plantar location (31.4%), followed by palmar (28.6%) and palmar-axillary (14.4%) locations rather than other locations. These results are consistent with those from other series [6, 9]. In terms of accompanying symptoms, there was ratio of 1.9 symptoms per patient including facial reddening (65.1%), palpitations (57.2%), trembling hands (34.7%), and headache (33.2%). These results are similar to those reported for other series [9, 12].
From the psychological point of view, our study shows that primary hyperhidrosis has negative repercussions for the work environment (89%) and friendships (74.3%), and it is precisely these negative repercussions that motivate patients to undergo surgery. There is a lack of specific reports on this issue in the literature.
The efficacy of surgery in our series was high, with systematic elimination of T2–T3. Anhydrosis of the target area was achieved with 97.4% of procedures. The hypohidrosis rate was 2.4%, and the failure rate was 0.2%. However, complete anhydrosis was obtained in the latter cases through reintervention. These results are in keeping with those obtained by other authors [6, 9, 12], including those with series [1, 1, 10, 20, 24, 34] in which T1–T4 or only T2 was eliminated [11].
The intraoperative morbidity rate was 0.4%. In every case, the morbidity was completely resolved without sequela. It should be noted that there was one case of hemopericardium. Although most published series report similar complication rates [1, 8, 10, 13, 20, 24, 34], we found no examples of chylothorax [3, 8], nervous lesions [15, 16], or pulmonary edema [14]. Table 1 compares the rates of complication, recurrence, undesirable effects, and level of satisfaction reported in several series.
The rate of postoperative complications in our study was 3.6%. Pneumothorax was the most common complication, although only 0.5% of the cases required pleural drainage. Compensatory hyperhidrosis, the most widely reported (48.4%) undesirable effect in our study, did not depend on the number of ganglia eliminated. The body regions that experienced significant changes in sweating were the trunk (increased sweating) and the feet (reduced sweating). Some series report similar percentages of compensatory hyperhidrosis, with a gradual fall in its intensity observed over 5-year follow-up period [1, 10, 20, 24, 34].
Although the etiology of compensatory hyperhidrosis is unknown, it generally is believed to have no relation to anxiety or stressful situations, unlike primary hyperhidrosis [25, 26]. Some authors directly relate compensatory hyperhidrosis to the number of sympathetic ganglia eliminated or the extent of sympathicolysis [11, 28, 29, 29, 33], although other studies report no such relationship [18]. With the aim of reducing compensatory hyperhidrosis, and even reversing the effect of sympathicolysis, some authors apply pressure to the sympathetic chain by means of a clip [27], a procedure with which we disagree [23]. Other authors only eliminate T3 and do not report compensatory hyperhidrosis at the 3½-year follow-up assessment [28].
We found that 2.4% of the well-tolerated hypohidroses did not require reintervention. In contrast, we found an excessive hand dryness rate of 0.38%. We believe that these contrasting responses to the same procedure are related to personal characteristics of individual patients rather than to the procedure in itself.
The rate of gustatory hyperhidrosis in our study was 1.1%, consistent with the findings of some authors [7, 8] and in contrast with the high rate of 30% to 50% reported from other series [19–23]. This undesirable effect causes a great deal of anxiety among patients, and they often require psychotherapy. Currently, we can offer no coherent explanation for this genuinely unpleasant consequence.
In our clinical practice, the rate of Horner’s syndrome has been 0.3%, whereas other current series show an incidence of 0% to 3.8% [1, 4, 8, 10, 20, 24, 34]. Several causes have been proposed for this syndrome, including the diffusion of the electric current from monopolar cautery, excessive traction of the sympathetic chain [15], and an erroneous localization of the second rib or anatomic distribution of the sympathetic chain [27, 30, 32]. Whatever the case, if sympathicolysis of T2 alone is performed, the incidence of this complication approaches zero, yet is sufficient to obtain anhydrosis in the event of palmar or facial hyperhidrosis [11].
Despite the 48.4% incidence of compensatory hyperhidrosis, we obtained high levels of satisfaction (88.5%). An understanding of this should take into account that, unlike what happens with primary hyperhidrosis, which is characterized by sweating in anticipation of stressful situations, compensatory hyperhidrosis appears in the context of ambient temperature changes.
Taken together, the results obtained lend support to the idea that the surgical technique of bilateral upper thoracic sympathicolysis offers a favorable treatment for primary hyperhidrosis. This is exemplified by the high level of patient satisfaction, the very low morbidity rate, and the acceptable levels of postoperative comfort. Despite the notable incidence of compensatory hyperhidrosis, the procedure remains valid because the natural trend of the process is toward less intense sweating, which is progressively accepted by the patient. Indeed, the high level of satisfaction outweighs this undesirable effect. In this regard, we believe it would be interesting to study baseline sympathetic activity among patients affected by primary hyperhidrosis to discriminate nosological subgroups within the clinical context [17].
References
Adar R (1994) Surgical treatment of palmar hyperhidrosis before thoracoscopy: experience with 475 patients. Eur J Surg 572(Suppl): 9–11
Cameron AE (1998) Complications of endoscopic sympathectomy. Eur J Surg 164: 33–35
Cheng W, Chang C, Lin T (1994) Chylothorax after endoscopic sympathectomy: case report. Neurosurgery 35: 330–331
Doolabh N, Horswell S, Williams M, Huber L, Prince S, Meyer DM, Mack MJ (2004) Thoracoscopic sympathectomy for hyperhidrosis: indications and results. Ann Thorac Surg 77: 410–414
Drott C, Göthberg G, Claes G (1995) Endoscopic transthoracic sympathectomy: an efficient and safe method for the treatment of hyperhidrosis. J Am Acad Dermatol; 33: 78–81
Dumont P, Denoyer A, Robin P (2004) Long-term results of thoracoscopic sympathectomy for hyperhidrosis. Ann Thorac Surg 78: 1801–1807
Gossot D, Galetta D, Pascal A, Debrosse D, Caliandro R, Girard P, Stern JB, Grunenwald D (2003) Long-term results of endoscopic thoracic sympathectomy for upper limb hyperhidrosis. Ann Thorac Surg 75: 1075–1079
Gossot D, Kabiri H, Caliandro R, Debrosse D, Girard P, Grunenwald D (2001) Early complications of thoracic endoscopic sympathectomy: a prospective study of 940 procedures. Ann Thorac Surg 71: 1116–1119
Hederman WP (1994) Present and future trends in thoracoscopic sympathectomy. Eur J Surg 572(Suppl): 17–19
Herbst F, Plas EG, Fugger R, Fritsch A (1994) Endoscopic thoracic sympathectomy for primary hyperhidrosis of the upper limbs: a critical analysis and long-term results of 480 operations. Ann Surg 220: 86–90
Hyndman OR, Wolkin J (1942) Sympathectomy of the upper extremity: evidence that only the second dorsal ganglion need be removed for complete sympathectomy. Arch Surg 45: 145–155
Kopelman D, Hashmonai M, Ehrenreich M, Assalia A (1998) Thoracoscopic sympathectomy for hyperhidrosis: is there a learning curve? Surg Laparosc Endosc 8: 370–375
Lai YT, Yang LH, Chio CC, Chen HH (1997) Complications in patients with palmar hyperhidrosis treated with transthoracic endoscopic sympathectomy. Neurosurgery 41: 110–113
Lan CJ, Luk HN, Wu CT, Chang WK, Tsou MY, Lui PW, Lee TY (2001) Bilateral pulmonary edema after endoscopic sympathectomy in a patient with glucose-6-phosphate dehydrogenase deficiency. Acta Anaesthesiol Scand 45: 123–126
Lange JF (1995) Inferior brachial plexus injury during thoracoscopic sympathectomy. Surg Endosc 9: 830
Lardinois D, Ris HB (2002) Minimally invasive video-endoscopic sympathectomy by use of a transaxillary single port approach. Eur J Cardiothorac Surg 21: 67–70
Lefaucheur JP, Fitoussi M, Becquemin JP (1996) Abolition of sympathetic skin responses following endoscopic thoracic sympathectomy. Muscle Nerve 19: 581–586
Lesèche G, Castier Y, Thabut G, Petit MD, Combes M, Cerceau O, Besnard M (2003) Endoscopic transthoracic sympathectomy for upper limb hyperhidrosis: limited sympathectomy does not reduce postoperative compensatory sweating. J Vasc Surg 37: 124–128
Lin CC, Mo LR, Lee SM, Ng SM, Hwang MH (1998) Thoracoscopic T2-sympathectomy block by clipping: a better and reversible operation for treatment of hyperhidrosis palmaris: experience in 326 cases. Eur J Surg 64: 13–16
Lin TS, Fang HY (2000) Transthoracic endoscopic sympathectomy in the treatment of palmar hyperhidrosis with emphasis on perioperative management (1,360 case analyses). Surg Neurol 52: 453–457
Moya J, Ferrer G, Morera R, Pujol R, Ramos R, Villalonga R, Bernat R (2001) Estudio comparativo entre gangliectomía y la simpaticolisis torácica superior para el tratamiento quirúrgico de la hiperhidrosis palmar primaria: a propósito de 185 procedimientos en 100 pacientes. Actas Dermosifiliogr 92: 369–375
Moya J, Ferrer G, Peyrí J, Pujol R, Morera R, Tarrado X, Villalonga R (2000) Simpatectomía torácica endoscópica en el tratamiento de la hiperhidrosis palmar primaria: a propósito de 28 casos. Actas Dermosifiliogr 91: 43–46
Moya J, Ramos R, Vives N, Perez J, Morera R, Perna V, Villalonga R, Ferrer G (2004) Compensatory sweating after thoracic sympathectomy: prospective study of 123 cases. Arch Bronconeumol 40: 360–363
Neumayer CH, Bischof G, Fugger R, Imhof M, Jakesz R, Plas EG, Herbst FR, Zacherl J (2001) Efficacy and safety of thoracoscopic sympathectomy for hyperhidrosis of the upper limb: results of 734 sympathectomies. Ann Chir Gynaecol 90: 195–199
Ramos R, Moya J, Pérez J, Villalonga R, Morera R, Pujol R,Ferrer G (2003) Primary hyperhidrosis: prospective study in 338 patients. Med Clin (Barc) 121: 201–203
Ramos R, Moya J, Turón V, Pérez J,Villalonga R,Morera R, Perna V, Ferrer G (2005) Primary hyperhidrosis and anxiety: a prospective preoperative survey of 158 patients. Arch Bronconeumol 41: 86–90
Ramsaroop L, Singh B, Moodley J, Partab P, Satyapal KS (2004) Anatomical basis for a successful upper limb sympathectomy in the thoracoscopic era. Clin Anat 17: 294–299
Riet M, Smet AA, Kuiken H, Kazemier G, Bonjer HJ (2001) Prevention of compensatory hyperhidrosis after thoracoscopic sympathectomy for hyperhidrosis. Surg Endosc 15: 1159–1162
Selley WB, Florence R (1960) Compensatory hyperhidrosis of sympathectomy. N Engl J Med 263: 1056–1058
Wang YC, Sun MH, Lin CW, Chen YJ (2002) Anatomical location of T2–T3 sympathetic trunk and Kuntz nerve determined by transthoracic endoscopy. J Neurosurg 96(1 Suppl): 68–72
Wittmoser R (1994) Sympathectomies et vagotomies par thoracoscopie. In: Gossot D (ed) Techniques de chirurgie endoscopique du thorax. Springer-Verlag, Paris pp 168–189
Yarzebski JL, Wilkinson HA (1987) T2 and T3 sympathetic ganglia in the adult human: a cadaver and clinical–radiographic study and its clinical application. Neurosurgery 21: 339–342
Yoon H, Ha Y, Park YG, Chang JW (2003) Thoracoscopic limited T3 sympathectomy for primary hyperhidrosis: prevention for compensatory hyperhidrosis. J Neurosurg 99(Suppl 1): 39–43
Zacherl J, Huber ER, Imhof M, Plas EG, Herbst F, Fugger R (1998) Long-term results of 630 thoracoscopic sympathectomies for primary hyperhidrosis: the Vienna experience. Eur J Surg Suppl 580: 43–46
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moya, J., Ramos, R., Morera, R. et al. Thoracic sympathicolysis for primary hyperhidrosis. Surg Endosc 20, 598–602 (2006). https://doi.org/10.1007/s00464-005-0557-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-005-0557-z