Abstract
The International Federation for the Surgery of Obesity and Metabolic Disorders has endorsed one anastomosis gastric bypass (OAGB) as a mainstream bariatric procedure. Several studies have shown excellent results with OAGB or mini-gastric bypass (MGB) in terms of metabolic outcomes. OAGB has seen a journey of 20 years but still there is no consensus on the ideal biliopancreatic limb (BPL) length to be bypassed. Some authors prefer using fixed limb lengths while some prefer using a tailored limb length according to the patient’s weight. There is a reasonable body of evidence suggesting that longer BPL length may lead to higher rate of nutritional deficiencies without any significant increase in weight loss and comorbidity improvement/resolution. Increased nutritional deficiencies may require admissions and even revisional surgery. This may lead to poor quality of life along with additional financial burden on the patient.
Recently, several authors have published data about the nutritional deficiencies that occur after OAGB/MGB. There has been increased interest in using a limb length of 150 cm and to measure the complete small bowel length if longer BPL length is used. Small bowel length varies greatly between 2.5 and 10 meters. Also, interoperative variability and difficulty in measuring the small bowel during laparoscopic surgery, in a morbidly obese patient, add to the complexity of the procedure. Thus, it is important for the bariatric surgeon community to standardize the procedure with respect to lengths of BPL to be used and techniques of measurement.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
Introduction
One anastomosis gastric bypass (OAGB) has been accepted as a mainstream bariatric procedure by the International Federation for the Surgery of Obesity and Metabolic Disorders in a recent consensus statement [1]. The procedure was first performed by Dr. Rutledge in 1997 [2] and has been adopted widely in Asian and European countries because of its technical simplicity, good results in terms of weight loss and comorbidity resolution, and ease of reconversion in case of an adverse event [3]. It has also become an attractive option for revisional bariatric procedure [4, 5]. OAGB involves the creation of a long gastric pouch with a loop gastrojejunostomy at the end of the pouch. In a randomized control trial (RCT) by Lee et al. [6], they compared OAGB with Roux-en-Y gastric bypass (RYGB) at 2 years and reported better weight loss outcome and improved short-term safety profile with OAGB. In another study from the same authors, they showed that the weight loss advantage is maintained at 5 years with OAGB over RYGB but they also observed lower hemoglobin levels with OAGB [7]. This has been reflected in the Indian Bariatric Surgery Outcome Reporting (IBSOR) multicenter study, in 9417 patients, where authors reported a similar trend of higher weight loss and lower mean hemoglobin and albumin levels [8].
These recurrent observations suggest that OAGB is a malabsorptive procedure that shows superior weight loss but with higher incidence of nutritional deficiencies. This has led surgeons to search for an ideal biliopancreatic limb (BPL) length that can achieve a reasonable weight loss but with acceptable rates of malnutrition.
So far, there is no consensus among surgeons on the ideal length of the BPL. BPL lengths ranging up to 350 cm have been described by some authors, while others have described tailoring the limb length depending on the weight and comorbidity of the patient [9]. Predictably, severe malnutrition has been reported after long limb OAGB [10, 11] and, therefore, suggestions have been made to reduce the limb length to 150 cm [12].
In this chapter, we will delve into the literature on the small bowel anatomy and physiology and the results of its bypass, the limb lengths used in duodenal switch (DS) and RYGB and its extrapolation in OAGB, and finally the published outcomes based on the BPL length in OAGB.
Small Intestine Anatomy and Physiology
The small intestine, especially the duodenum and jejunum are the most important locations for digestion and absorption of most of the macronutrients as well as micronutrients. Although protein is absorbed over the whole length of the small bowel, the proximal part is the main area for protein absorption. Minerals such as iron, calcium, copper, and zinc are also absorbed actively from the duodenum and the proximal intestine. (Fig. 1 shows the absorption of important nutrients along the length of the entire bowel). These micronutrients can also be absorbed from the distal intestine but the absorption is less effective since it relies on passive absorption. Most of the water-soluble vitamins (most of the vitamin B complex except cobalamin (B12)) are absorbed from the proximal intestine. Therefore, the bypass of proximal intestine leads to the malabsorption of these important nutrients.
The clinical data on the short gut syndrome shows that when the small gut resection is increased and the common channel is decreased, the malabsorption and the incidence of malnutrition is increased [13]. Also, the data on gastrectomy with Billroth-II reconstruction shows that the duodenal bypass affects the protein, iron, and calcium metabolism [14]. Therefore, the proximal small gut has immense importance in maintaining the nutrition of individuals. Since gastric bypass involves the exclusion of proximal gut, the limb lengths become a topic of immense importance.
The length of the small intestine is variable since it is a dynamic organ. The total small bowel length (TSBL) varies between 2 and 8.5 m with an approximate average length of five meters [15]. In a large study, the mean length of the small intestine was 6.9 m with a maximum length of 13 m and a minimum length of only 2.5 m [16].
The TSBL may be associated with the height, male gender, and body mass index (BMI) [17]. The body weight in a morbidly obese patient may be related to the jejunal length [17]. It seems that longer jejunal length is directly related to a higher degree of obesity [17]. Also, height is consistently associated with the TSBL [18]. However, a study by Bekheit et al. [16], including 606 patients, reported that there is no clinically significant correlation between TSBL and weight and height of an individual.
This knowledge is important in the field of bariatric surgery since the length of the bypass which is generally practiced is fixed rather than tailored.
Limb Lengths in Bariatric Surgery: What Have We Learnt?
There are many difficulties in choosing the limb length for gastric bypass. It is not clear whether the proportion of the bypass (bypassed limb/TSBL) is more important than the absolute length of the alimentary limb (AL), BPL, and common limb (CL).
Surgeons performing different bariatric procedures have used different limb lengths, and that knowledge can guide us in choosing the ideal limb length. Surgeons performing DS have used a CL of 200 cm and showed superior efficacy for weight loss and metabolic control but with high rates of malnutrition [19]. This configuration indicates that longer BPL may be responsible for superior efficacy and increasing nutritional deficiencies. Most of the RYGB surgeons have used a BPL of 50 cm and AL of 100–200 cm with reasonable efficacy and acceptable malnutrition rates [20, 21]. To improve weight loss outcomes and reduce the numbers of primary and secondary nonresponders, there has been a recent interest among surgeons to use greater BPL length [22]. It reflects the thought process of surgeons performing OAGB/MGB. Here is a review of relevant literature that has guided bariatric surgeons on choosing the optimum BPL.
A systemic review by Mahawar et al. [23] reported that the distal RYGB with longer AL was associated with higher risk of malnutrition but without any significant improvement in weight loss or comorbidity resolution. Several studies showed that BPL is more important in gastric bypass and is responsible for the weight loss and comorbidity resolution [24]. A study on RYGB observed that most of these benefits happen in the proximal bypass with a combined bypass length (BPL + AL) of 150 cm [23]. The distal gastric bypass may not provide a gross advantage in terms of weight loss [23]. ARCT showed no difference in weight loss and comorbidity resolution when a constant AL of 150 cm was used either with a BPL of 120 cm or 70 cm [25]. However, the group with 120 cm BPL was associated with higher risk of micronutrient deficiencies [25]. This was confirmed in the Ducati trial [26], where 444 patients were randomized into two groups who either underwent a very long roux limb RYGB (VL-RYGB) (variable AL, BPL 60 cm, and CL100 cm) or a standard RYGB (AL 150 cm, BPL 60 cm, and variable CL length). The excess weight loss percentage (EWL%) and total weight loss percentage was comparable between the two groups with no significant difference. However, 1.4% of the patients who underwent VL-RYGB and 0.9% of those who underwent standard RYGB required surgical bowel length correction due to severe malabsorption. Moreover, the significant lengthening of the AL, at the cost of the CL, did not affect the weight loss at one year, which also supported the theory that absorption of nutrients also occurs in the AL [26]. At one year postoperatively, patients who underwent VL-RYGB had significantly lower levels of calcium, iron, and vitamin D compared to patients who underwent standard RYGB [27]. The AL in RYGB starts breaking and absorbing the carbohydrates present in the food and the absorptive capacity increases with time as the small gut starts to adapt. However, a systematic review by Mahawar et al. [28] noted that malabsorption contributes only 11% to a calorie deficit particularly in the early period, and possibly it contributes even lower on long-term follow-up [28]. The percentage of CL length had no effect on weight loss in patients who underwent RYGB; however, lower CL% was related to higher nutritional deficiencies [29].
Few studies have compared OAGB with RYGB. In YOMEGA trial, patients who underwent OAGB with BPL length of 200 cm, compared to RYGB with an AL of 150 cm and BPL of 50 cm, had a significantly higher incidence of steatorrhea and diarrhea along with nutritional deficiencies leading to adverse outcomes [30]. Similarly, Bhandari et al. [31] reported better efficacy with OAGB (BPL of 250 cm), compared to RYGB (BPL of 80 cm and Roux limb of 120 cm), but with higher rates of nutritional deficiencies than RYGB at 5 years. A meta-analysis by Jia D et al. [32] compared OAGB with RYGB and concluded that OAGB is possibly associated with more weight loss in obese patients even though the quality of evidence was low with inconsistent BPL length in OAGB group. Probably, the weight loss benefit appears to be confined to OAGB using the extended length of BPL but not to OAGB using the standard length of BPL, when compared with RYGB [32].
This finding reinforces the fact that OAGB is primarily a malabsorptive procedure while RYGB is primarily a restrictive procedure. The difference in malabsorption even when similar lengths of the small bowel are bypassed in the two procedures may be due to the anatomical variation between the procedures. The presence of the AL allows initial digestion and absorption of nutrients by the small bowel mucosa even before the food reaches the CL. In OAGB, since AL is absent, the food is directly delivered to the distal jejunum where it gets mixed with biliopancreatic juices for breakdown and absorption and thus completely bypasses the proximal jejunum.
Fixed Versus Tailored Limb Length Model in OAGB/MGB
Some surgeons hypothesized that since the TSBL is variable, the proportion of proximal small bowel bypass may be more important than the fixed limb model. A study evaluated how the proportion of bypass will affect the outcomes and reported that tailoring the BPL by bypassing 40% of short bowel length was safe and effective [33]. The authors noted that tailoring the BPL length was better than using a fixed BPL of 200 cm because of the equivalent weight loss but with decreased nutritional deficiencies [33]. However, there are technical challenges in implementing this model. Measuring the entire small bowel is fraught with the dangers of bowel injury mostly due to handling and instrumentation issues. The surgeon needs to measure from both the ligament of Trietz and the ileocecal junction which can be cumbersome. It also increases the operative time. These measurements are technically more difficult in obese patients because of the fatty mesentery. It is also difficult to differentiate between the capacious and vascular jejunum from a narrower and less vascular ileum [15].
Moreover, there is a high degree of interoperator variability in measuring the TSBL [34] probably due to the lack of standardization in the technique of measurement. This variation is more significant in laparoscopic surgery when compared to open surgery [33]. Factors that lead to variability are: small bowel condition (its tone or flaccidity at the time of measurement), effect of anesthetic drugs, position of the patient, and gravity being used at the time of surgery [35]. The magnitude of the error is correlated to the total length of small bowel measured and the surgeons usually tend to underestimate the length [33].
Using a fixed limb length without measuring the TSBL can have potential clinical implications. When TSBL is not measured and only the length of BPL is measured, it can lead to harmful effects in patients with short TSBL. For instance, a 200 cm bypass of the small bowel in a patient with TSBL of 800 cm is definitely not the same when compared to a patient with TSBL of 300 cm. The latter is definitely a high-risk factor for severe malnutrition.
Currently, apart from preoperative computerized tomography scan and three-dimensional reconstruction for the measurement of TSBL [36], artificial intelligence and information technology navigated intraoperative measurements of the bowel length that are being developed [37]. This may help the surgeon to plan the limb lengths to be bypassed well in advance.
Effects of Limb Length on Efficacy and Malnutrition in OAGB/MGB: Review of Literature
Presently, there is no consensus on the adequate limb length to be used for bypassing in OAGB. Earlier, studies have described the use of longer limb lengths of up to 350 cm in OAGB. The CL length mostly used in various studies was around 200 cm [38]. In a survey of 208 surgeons, 35% of surgeons preferred a constant BPL length while the remaining 65% preferred a tailored limb length [38]. Out of 208 surgeons, 62.1% used 200 cm as fixed limb length [38]. In a consensus statement, there was no agreement on the use of 150 cm BPL as a standard length while there was agreement on the use of 200 cm as routinely used limb length [39]. In a consensus statement on OAGB which included 52 international experts, it was agreed that BPL length ≥ 200 cm increases the risk of malabsorption and protein-calorie malnutrition [40]. There was also consensus among the experts that when the BPL length is >200 cm, TSBL should be measured [40]. Several studies have reported an increased rate of nutritional deficiencies leading to complications after OAGB [41]. These complications increase the morbidity of the patients and in some cases have not only required readmissions and revision surgeries but also have led to mortality [37]. A systematic review reported that the incidence of malnutrition after OAGB ranged from 0–3.8% with a mean incidence of 0.71% [41]. Severe malabsorption and protein-calorie malnutrition following OAGB can lead to liver failure [41]. This is more significant in patients who follow a vegetarian diet that is deficient in proteins or who are noncompliant to regular protein supplementation [10].
Rutledge et al. [42] reported an excessive weight loss with malnutrition in 31 patients (1.28%) leading to revisional surgery. Similarly, Taha et al. [43] reported >100% EWL in three patients (0.2%) and Noun et al. [44] in four patients (0.4%) leading to revisional surgery in those patients. In a large series by Lee et al. [7], 10 patients (0.9%) needed conversion to sleeve gastrectomy due to severe malnutrition. Kular et al. [45] reversed the OAGB procedure in two patients due to protein deficiency in one patient and excessive weight loss in another patient. It is important to note that in both of these patients BPL of 300 cm was used [45].
In the review by Parmar et al. [40], the incidence of anemia was reported to be 0.64–15% with a mean of 7%. Carbajo et al. [46] reported severe anemia requiring parenteral supplementation in 1.25% of patients and mild anemia requiring oral supplementation in 30% of patients. Taha et al. [43] and Jammu et al. [47] observed anemia in 3.1% and 4.9% patients, respectively. Kular et al. [45] reported anemia in 7.6% of patients and all were managed conservatively with oral or injectable iron, while Rutledge et al. [42] reported anemia in 5% of patients [42].
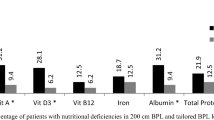
The study by the UK MGB/OAGB group reported that 2.3% (23/923) of patients required revisional surgery after OAGB [48]. Out of these, one patient required revision each for excessive weight loss and severe protein malnutrition while two patients required revision for liver decompensation. All these patients were managed by either reversal to normal anatomy or shortening of BPL. The authors concluded that BPL ≥200 cm was associated with more severe complications but 150 cm limb length was safe to use [48]. Ahuja et al. [10] compared the outcomes after OAGB in three groups of patients using either 150 cm, 180 cm, or 250 cm of BPL length. BPL of 250 cm was associated with significantly higher deficiencies of iron, ferritin, Vitamin B12, Vitamin D3, total protein, and albumin when compared to BPL of 150 cm. However, when compared to 180 cm BPL, 250 cm BPL was associated with significantly higher deficiencies of total protein, Vitamin D3, and Vitamin B12. EWL% and comorbidity resolution (type 2 diabetes and hypertension) were comparable between the three groups with no statistically significant difference. The authors concluded that 150 cm BPL is an adequate limb length with good results but with minimum morbidity [10]. In super obese patients requiring more weight loss, 180 cm BPL may be used [10]. In this study, two patients with 250 cm BPL required readmission and treatment for severe anemia and severe protein deficiency while one mortality was reported with 250 cm BPL due to severe malnutrition leading to liver failure and ascites [10, 11]. Similarly, severe malnutrition and mortality after OAGB with ≥200 cm BPL were reported by two case reports [49, 50]. Pizza et al. [51] compared the outcomes between 150 cm, 180 cm, and 200 cm BPL in OAGB and found that BPL of 150–180 cm was the safest with good EWL% and comorbidity resolution along with minimal morbidity in terms of malnutrition. They noted that iron and ferritin deficiencies were significantly higher in the 200 cm BPL group [51]. Boyle et al. [52] compared the most popular limb length of 200 cm with 150 cm in OAGB and reported that there was no significant difference in terms of weight loss outcomes between the two groups. Results of OAGB/MGB from large series are summarized in Table 1.
Trovar et al. [53] recommended that the most accurate method to achieve optimal weight loss was the CL/TSBL ratio followed by the measurement of CL length, while measurement of BPL length only was the parameter with the lowest accuracy to predict long-term weight loss [53].
Considering the above points, it may seem that there is little consensus regarding the optimum limb length; however, there are pointers to use lower BPL for safe clinical practice. In a systematic review of OAGB in patients with BMI ≤35 kg/m2, the median length of BPL used was 120 cm [54]. All these evidences suggest that we can at least begin to perform OAGB with smaller BPL in patients with comparatively lower BMI, till more data is available.
Summary
With the increasing popularity of OAGB, globally, it becomes imperative to have a better understanding of its mechanism of action along with standardization of the length of the small bowel to be used as BPL. For the past several years, studies have suggested that a BPL of 150 cm, compared to longer BPL (>200 cm), is adequate and provides good and comparable results in terms of weight loss and comorbidity resolution. This avoids the unnecessary risk of severe nutritional deficiencies and its related complications. It is important to confirm these findings by comparing the results of different limb lengths in a randomized control trial. It may also be reasonable to study the results of OAGB with a BPL length between 100 and 150 cm because this may suggest whether OAGB can be utilized for the amelioration of comorbidities in patients with lower BMI.
Key Learning Points
-
Small bowel is a dynamic organ with great variability in its length.
-
The variation in the measurement of small bowel depends on several factors including position of the patient, tonicity of the small bowel muscle, and effect of anesthetic drug. The variability is greater in laparoscopic surgery and poses challenge in a morbidly obese patient.
-
Whether it is fixed limb length or a tailored approach, BPL >150 cm is associated with higher rates of protein-calorie malnutrition without any clinically significant proportionate gains in terms of weight loss and other metabolic outcomes.
-
Consensus needs to be developed to standardize the technique of limb length measurement.
-
Future studies are needed to evaluate how a BPL with <150 cm affects the results of OAGB.
References
De Luca M, Tie T, Ooi G, Higa K, Himpens J, Carbajo M-A, et al. Mini gastric bypass-one anastomosis gastric bypass (MGB-OAGB)-IFSO position statement. Obes Surg. 2018;28(5):1188–206. https://doi.org/10.1007/s11695-018-3182-3.
Rutledge R. The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg. 2001;11(3):276–80. https://doi.org/10.1381/096089201321336584.
Lee WJ, Almalki OM, Ser KH, Chen J-C, Lee Y-C. Randomized controlled trial of one anastomosis gastric bypass versus Roux-En-Y gastric bypass for obesity: comparison of the YOMEGA and Taiwan studies. Obes Surg. 2019;29(9):3047–53. https://doi.org/10.1007/s11695-019-04065-2.
Kermansaravi M, Shahmiri SS, DavarpanahJazi AH, Valizadeh R, Berardi G, Vitiello A, et al. One anastomosis/mini-gastric bypass (OAGB/MGB) as revisional surgery following primary restrictive bariatric procedures: a systematic review and meta-analysis. Obes Surg. 2021;31(1):370–83. https://doi.org/10.1007/s11695-020-05079-x.
Parmar CD, Gan J, Stier C, Dong Z, Chiappetta S, El-Kadre L, et al. One anastomosis/mini gastric bypass (OAGB-MGB) as revisional bariatric surgery after failed primary adjustable gastric band (LAGB) and sleeve gastrectomy (SG): a systematic review of 1075 patients. Int J Surg. 2020;81:32–8. https://doi.org/10.1016/j.ijsu.2020.07.007.
Lee W-J, Yu P-J, Wang W, Chen T-C, Wei P-L, Huang M-T. Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity: a prospective randomized controlled clinical trial. Ann Surg. 2005;242(1):20–8. https://doi.org/10.1097/01.sla.0000167762.46568.98.
Lee W-J, Ser K-H, Lee Y-C, Tsou J-J, Chen S-C, Chen J-C. Laparoscopic Roux-en-Y vs. mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg. 2012;22(12):1827–34. https://doi.org/10.1007/s11695-012-0726-9.
Baig SJ, Priya P, Mahawar KK, Shah S, Indian Bariatric Surgery Outcome Reporting (IBSOR) Group. Weight regain after bariatric surgery-a multicentre study of 9617 patients from Indian bariatric surgery outcome reporting group. Obes Surg. 2019;29(5):1583–92. https://doi.org/10.1007/s11695-019-03734-6.
Lee W-J, Wang W, Lee Y-C, Huang M-T, Ser K-H, Chen J-C. Laparoscopic mini-gastric bypass: experience with tailored bypass limb according to body weight. Obes Surg. 2008;18(3):294–9. https://doi.org/10.1007/s11695-007-9367-9.
Ahuja A, Tantia O, Goyal G, Chaudhuri T, Khanna S, Poddar A, et al. MGB-OAGB: effect of biliopancreatic limb length on nutritional deficiency, weight loss, and comorbidity resolution. Obes Surg. 2018;28(11):3439–45. https://doi.org/10.1007/s11695-018-3405-7.
Ahuja A, Tantia O, Goyal G, Chaudhuri T, Khanna S, Poddar A, et al. Reply to: yet another mortality with a bilio-pancreatic limb of > 200 cm with one anastomosis gastric bypass. Obes Surg. 2018;28(11):3636–7. https://doi.org/10.1007/s11695-018-3463-x.
Mahawar KK. A biliopancreatic limb of >150 cm with OAGB/MGB is ill-advised. Obes Surg. 2017;27(8):2164–5. https://doi.org/10.1007/s11695-017-2736-0.
Nightingale J, Woodward JM, Small Bowel and Nutrition Committee of the British Society of Gastroenterology. Guidelines for management of patients with a short bowel. Gut. 2006;55(Suppl 4):iv1–iv12. https://doi.org/10.1136/gut.2006.091108.
Tovey FI, Hobsley M. Post-gastrectomy patients need to be followed up for 20–30 years. World J Gastroenterol. 2000;6(1):45–8.
Hounnou G, Destrieux C, Desmé J, Bertrand P, Velut S. Anatomical study of the length of the human intestine. Surg Radiol Anat. 2002;24(5):290–4. https://doi.org/10.1007/s00276-002-0057-y.
Bekheit M, Ibrahim MY, Tobar W, Galal I, Elward AS. Correlation between the total small bowel length and anthropometric measures in living humans: cross-sectional study. Obes Surg. 2020;30(2):681–6. https://doi.org/10.1007/s11695-019-04238-z.
Tacchino RM. Bowel length: measurement, predictors, and impact on bariatric and metabolic surgery. Surg Obes Relat Dis. 2015;11(2):328–34. https://doi.org/10.1016/j.soard.2014.09.016.
Teitelbaum EN, Vaziri K, Zettervall S, Amdur RL, Orkin BA. Intraoperative small bowel length measurements and analysis of demographic predictors of increased length. Clin Anat. 2013;26(7):827–32. https://doi.org/10.1002/ca.22238.
Hedberg J, Sundström J, Sundbom M. Duodenal switch versus Roux-en-Y gastric bypass for morbid obesity: systematic review and meta-analysis of weight results, diabetes resolution and early complications in single-centre comparisons. Obes Rev. 2014;15(7):555–63.
Berbiglia L, Zografakis JG, Dan AG. Laparoscopic Roux-en-Y gastric bypass: surgical technique and perioperative care. Surg Clin North Am. 2016;96(4):773–94. https://doi.org/10.1016/j.suc.2016.03.003.
Powell MS, Fernandez AZ. Surgical treatment for morbid obesity: the laparoscopic Roux-en-y gastric bypass. Surg Clin North Am. 2011;91(6):1203–24. https://doi.org/10.1016/j.suc.2011.08.013.
Shah K, Nergård BJ, Fagerland MW, Gislason H. Distal gastric bypass: 2-m biliopancreatic limb construction with varying lengths of common channel. Surg Obes Relat Dis. 2019;15(9):1520–6. https://doi.org/10.1016/j.soard.2019.05.003.
Mahawar KK, Kumar P, Parmar C, Graham Y, Carr WR, Jennings N, et al. Small bowel limb lengths and Roux-en-Y gastric bypass: a systematic review. Obes Surg. 2016;26(3):660–71. https://doi.org/10.1007/s11695-016-2050-2.
Zorrilla-Nunez LF, Campbell A, Giambartolomei G, Menzo EL, Szomstein S, Rosenthal RJ. The importance of the biliopancreatic limb length in gastric bypass: a systematic review. Surg Obes Relat Dis. 2019;15(1):43–9. https://doi.org/10.1016/j.soard.2018.10.013.
Ruiz-Tovar J, Vorwald P, Gonzalez-Ramirez G, Posada M, Salcedo G, Llavero C, et al. Impact of biliopancreatic limb length (70 cm vs 120 cm), with constant 150 cm alimentary limb, on long-term weight loss, remission of comorbidities and supplementation needs after Roux-En-Y gastric bypass: a prospective randomized clinical trial. Obes Surg. 2019;29(8):2367–72. https://doi.org/10.1007/s11695-019-03717-7.
Gadiot RPM, Leeman M, Biter LU, et al. Does the length of the common channel as part of the total alimentary tract matter? One year results from the multicenter Dutch Common Channel Trial (DUCATI) comparing standard versus distal Roux-en-Y gastric bypass with similar biliopancreatic bowel limb lengths. Obes Surg. 2020;30(12):4732–40. https://doi.org/10.1007/s11695-020-04982-7.
Leeman M, Gadiot RP, Wijnand JM, Birnie E, Apers JA, Biter LU, et al. Effects of standard v. very long Roux limb Roux-en-Y gastric bypass on nutrient status: a 1-year follow-up report from the Dutch Common Channel Trial (DUCATI) study. Br J Nutr. 2020;123(12):1434–40. https://doi.org/10.1017/S0007114520000616.
Mahawar KK, Sharples AJ. Contribution of malabsorption to weight loss after Roux-en-Y gastric bypass: a systematic review. Obes Surg. 2017;27(8):2194–206. https://doi.org/10.1007/s11695-017-2762-y.
Abellan I, Luján J, Frutos MD, Abrisqueta J, Hernandez Q, Lopez V, et al. The influence of the percentage of the common limb in weight loss and nutritional alterations after laparoscopic gastric bypass. Surg Obes Relat Dis. 2014;10(5):829–33. https://doi.org/10.1016/j.soard.2014.06.009.
Robert M, Espalieu P, Pelascini E, Caiazzo R, Sterkers A, Khamphommala L, et al. Efficacy and safety of one anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity (YOMEGA): a multicentre, randomised, open-label, non-inferiority trial. Lancet. 2019;393(10178):1299–309. https://doi.org/10.1016/S0140-6736(19)30475-1.
Bhandari M, Nautiyal HK, Kosta S, Mathur W, Fobi M. Comparison of one-anastomosis gastric bypass and Roux-en-Y gastric bypass for treatment of obesity: a 5-year study. Surg Obes Relat Dis. 2019;15(12):2038–44. https://doi.org/10.1016/j.soard.2019.05.025.
Jia D, Tan H, Faramand A, Fang F. One anastomosis gastric bypass versus Roux-en-Y gastric bypass for obesity: a systematic review and meta-analysis of randomized clinical trials. Obes Surg. 2020;30(4):1211–8. https://doi.org/10.1007/s11695-019-04288-3.
Komaei I, Sarra F, Lazzara C, et al. One anastomosis gastric bypass-mini gastric bypass with tailored biliopancreatic limb length formula relative to Small bowel length: preliminary results. Obes Surg. 2019;29(9):3062–70. https://doi.org/10.1007/s11695-019-04019-8.
Gazer B, Rosin D, Bar-Zakai B, Willenz U, Doron O, Gutman M, et al. Accuracy and inter-operator variability of small bowel length measurement at laparoscopy. Surg Endosc. 2017;31(11):4697–704. https://doi.org/10.1007/s00464-017-5538-5.
Isreb S, Hildreth AJ, Mahawar K, Balupuri S, Small P. Laparoscopic instruments marking improve length measurement precision. World J Laparosc Surg. 2009;2(3):57–60.
Marie L, Nacache R, Scemama U, Chatta I, Gaborit B, Berdah SV, et al. Preoperative prediction of small bowel length using CT scan and tridimensional reconstructions: a new tool in bariatric surgery? Obes Surg. 2018;28(5):1217–24. https://doi.org/10.1007/s11695-017-3021-y.
Dray X, Iakovidis D, Houdeville C, et al. Artificial intelligence in small bowel capsule endoscopy – current status, challenges and future promise. J Gastroenterol Hepatol. 2021;36(1):12–9.
Mahawar KK, Kular KS, Parmar C, Van den Bossche M, Graham Y, Carr WR, et al. Perioperative practices concerning one anastomosis (mini) gastric bypass: a survey of 210 surgeons. Obes Surg. 2018;28(1):204–11. https://doi.org/10.1007/s11695-017-2831-2.
Mahawar KK, Himpens J, Shikora SA, Chevallier J-M, Lakdawala M, De Luca M, et al. The first consensus statement on one anastomosis/mini gastric bypass (OAGB/MGB) using a modified Delphi approach. Obes Surg. 2018;28(2):303–12. https://doi.org/10.1007/s11695-017-3070-2.
Ramos AC, Chevallier JM, Mahawar K, Brown W, Kow L, White KP, et al. IFSO (International Federation for Surgery of Obesity and metabolic disorders) consensus conference statement on one-anastomosis gastric bypass (OAGB-MGB): results of a modified Delphi study. Obes Surg. 2020;30(5):1625–34. https://doi.org/10.1007/s11695-020-04519-y.
Parmar CD, Mahawar KK. One anastomosis (mini) gastric bypass is now an established bariatric procedure: a systematic review of 12,807 patients. Obes Surg. 2018;28(9):2956–67. https://doi.org/10.1007/s11695-018-3382-x.
Rutledge R, Walsh TR. Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg. 2005;15(9):1304–8. https://doi.org/10.1381/096089205774512663.
Taha O, Abdelaal M, Abozeid M, Askalany A, Alaa M. Outcomes of omega loop gastric bypass, 6-years’ experience of 1520 cases. Obes Surg. 2017;27(8):1952–60. https://doi.org/10.1007/s11695-017-2623-8.
Noun R, Skaff J, Riachi E, Daher R, Antoun NA, Nasr M. One thousand consecutive mini-gastric bypass: short- and long-term outcome. Obes Surg. 2012;22(5):697–703. https://doi.org/10.1007/s11695-012-0618-z.
Kular KS, Manchanda N, Rutledge R. A 6-year experience with 1,054 mini-gastric bypasses-first study from Indian subcontinent. Obes Surg. 2014;24(9):1430–5. https://doi.org/10.1007/s11695-014-1220-3.
Carbajo MA, Luque-de-León E, Jiménez JM, Ortiz-de-Solórzano J, Pérez-Miranda M, Castro-Alija MJ. Laparoscopic one-anastomosis gastric bypass: technique, results, and long-term follow-up in 1200 patients. Obes Surg. 2017;27(5):1153–67. https://doi.org/10.1007/s11695-016-2428-1.
Jammu GS, Sharma R. A 7-year clinical audit of 1107 cases comparing sleeve gastrectomy, Roux-en-Y gastric bypass, and mini-gastric bypass, to determine an effective and safe bariatric and metabolic procedure. Obes Surg. 2016;26(5):926–32. https://doi.org/10.1007/s11695-015-1869-2.
Hussain A, Van den Bossche M, Kerrigan DD, Alhamdani A, Parmar C, Javed S, et al. Retrospective cohort study of 925 OAGB procedures. The UK MGB/OAGB collaborative group. Int J Surg. 2019;69:13–8. https://doi.org/10.1016/j.ijsu.2019.07.003.
Kermansaravi M, Abdolhosseini MR, Kabir A, Pazouki A. Severe hypoalbuminemia and steatohepatitis leading to death in a young vegetarian female, 8 months after mini gastric bypass: a case report. Int J Surg Case Rep. 2017;31:17–9. https://doi.org/10.1016/j.ijscr.2016.12.004.
Motamedi MA, Barzin M, Ebrahimi M, Ebrahimi R, Khalaj A. Severe fatal protein malnutrition and liver failure in a morbidly obese patient after mini-gastric bypass surgery: case report. Int J Surg Case Rep. 2017;33:71–4. https://doi.org/10.1016/j.ijscr.2017.02.033.
Pizza F, Lucido FS, D'Antonio D, Tolone S, Gambardella C, Dell’Isola C, et al. Biliopancreatic limb length in one anastomosis gastric bypass: which is the best? Obes Surg. 2020;30(10):3685–94. https://doi.org/10.1007/s11695-020-04687-x.
Boyle M, Mahawar K. One anastomosis gastric bypass performed with a 150-cm biliopancreatic limb delivers weight loss outcomes similar to those with a 200-cm biliopancreatic limb at 18–24 months. Obes Surg. 2020;30(4):1258–64. https://doi.org/10.1007/s11695-019-04359-5.
Ruiz-Tovar J, Carbajo MA, Jimenez JM, Luque-de-Leon E, Ortiz-de-Solorzano J, Castro MJ. Are there ideal small bowel limb lengths for One-Anastomosis Gastric Bypass (OAGB) to obtain optimal weight loss and remission of comorbidities with minimal nutritional deficiencies? World J Surg. 2020;44(3):855–62. https://doi.org/10.1007/s00268-019-05243-0.
Parmar CD, Zakeri R, Mahawar K. A systematic review of one anastomosis/mini gastric bypass as a metabolic operation for patients with body mass index ≤35 kg/m2. Obes Surg. 2020;30(2):725–35. https://doi.org/10.1007/s11695-019-04293-6.
Musella M, Susa A, Greco F, et al. The laparoscopic mini-gastric bypass: the Italian experience: outcomes from 974 consecutive cases in a multicenter review. Surg Endosc. 2014;28(1):156–63.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Section Editor information
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this entry
Cite this entry
Ahuja, A., Baig, S.J., Tantia, O. (2021). Laparoscopic One Anastomosis Gastric Bypass/Mini Gastric Bypass: Limb Length and Nutritional Issues. In: Agrawal, S. (eds) Obesity, Bariatric and Metabolic Surgery. Springer, Cham. https://doi.org/10.1007/978-3-030-54064-7_95-1
Download citation
DOI: https://doi.org/10.1007/978-3-030-54064-7_95-1
Received:
Accepted:
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-54064-7
Online ISBN: 978-3-030-54064-7
eBook Packages: Springer Reference MedicineReference Module Medicine