Abstract
Background
Due to the failure of the “old Mason loop,” the mini-gastric bypass (MGB) has been viewed with skepticism. During the past 12 years, a growing number of authors from around the world have continued to report excellent short- and long-term results with MGB.
Methods
One university center, three regional hospitals, and two private hospitals participated in this study. From July 2006 to December 2012, 475 men (48.8 %) and 499 women (51.2 %) underwent 974 laparoscopic MGBs. The mean age of these patients was 39.4, and their preoperative body mass index was 48 ± 4.58 kg/m2. Type 2 diabetes mellitus (T2DM) affected 224 (22.9 %) of the 974 patients, whereas 291 of the 974 patients (29.8 %) presented with hypertension. The preoperative gastrointestinal status was explored in all the patients through esophagogastroduodenoscopia. The major end points of the study were definitions of both MGB safety and efficacy in the long term as well as the endoscopic changes in symptomatic patients eventually produced by surgery.
Results
The rate of conversion to open surgery was 1.2 % (12/974), and the mortality rate was 0.2 % (2/974). The perioperative morbidity rate was 5.5 % (54/974), with 20 (2 %) of the 974 patients requiring an early surgical revision. The mean hospital length of stay was 4.0 ± 1.7 days. At this writing, 818 patients are being followed up. Late complications have affected 74 (9 %) of the 818 patients. The majority of these complications (66/74, 89.1 %) have occurred within 1 year after surgery. Bile reflux gastritis was symptomatic, with endoscopic findings reported for 8 (0.9 %) and acid peptic ulcers for 14 (1.7 %) of the 818 patients. A late revision surgery was required for 7 (0.8 %) of the 818 patients. No patient required revision surgery due to biliary gastritis. At 60 months, the percentage of excess weight loss was 77 ± 5.1 %, the T2DM remission was 84.4 %, and the resolution of hypertension was 87.5 %.
Conclusions
Despite initial skepticism, this study, together with many other large-scale, long-term similar studies from around the world (e.g., Taiwan, United States, France, Spain, India, Lebanon) demonstrated the MGB to be a short, simple, low-risk, effective, and durable bariatric procedure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The mini-gastric bypass (MGB) was introduced by Rutledge [1] in 1997 and reported some years later. Since then, thousands of patients have been treated with this approach by several authors in different countries [2–8].
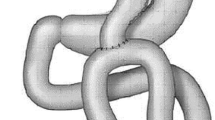
The technique, previously described in detail [1], consists of a laterolateral anastomosis between a sleeved gastric pouch 10–12 cm long and a jejunal loop ~200 cm distal to the duodenal ligament of Treitz. Although some modifications to the original description have been proposed in the execution of the anastomosis or in the length of the jejunal loop, the rationale of this intervention remains unchanged [4, 9]. However, it must be highlighted that although some bariatric surgeons confuse the two techniques, MGB, from a technical point of view, is not the old loop gastric bypass proposed by Mason and Ito [10] in 1967. In this early configuration, the gastric pouch was very high, short, and horizontally shaped, exposing the esophageal mucosa to caustic alkaline bile reflux coming from the jejunal loop. Figure 1A, B show the differences between the two techniques.
When presented, MGB raised harsh criticism [11], but despite that skeptical position, reprised in more recent papers [12, 13], different authors have reported interesting results in terms of weight loss and resolution of obesity-related comorbidities, describing a low rate of mid- and long-term postoperative complications [2–8, 14–17]. Furthermore, MGB efficacy has been tested with success in women with obesity-related infertility [18].
According to the Italian Society for Metabolic and Bariatric Surgery (SICOB), the standard surgical procedures are considered to be laparoscopic adjustable gastric banding (LAGB), vertical banded gastroplasty (VBG), sleeve gastrectomy (SG), Roux-en-Y gastric bypass (RYGBP), and standard biliopancreatic diversion (BPD) with or without a duodenal switch (BPD–DS).
In Italy, following a similar trend in the United States [16], MGB surgery has raised doubt concerning the risk of determining biliary gastritis and, in the long term, cancer of the gastric pouch. Only recently, in June 2012, SICOB [19] has allowed an “investigational” role for this procedure. The aim of this multicenter retrospective study was to assess both the efficacy and safety of MGB in the treatment of morbid obesity and to compare our result with that of previously published studies.
Patients and methods
The review was planned during the first MGB-one anastomosis gastric bypass (OAGB) consensus conference held at Paris in October 2012. One university center, three regional hospitals, and two private hospitals were involved. Center recruitment was done based on experience with more than 20 cases.
From July 2006 to December 2012, 475 men (48.8 %) and 499 women (51.2 %) underwent 974 laparoscopic MGB–OAGB procedures. The mean age of the patients was 39.4 years, and the mean preoperative body mass index (BMI) was 48 ± 4.58 kg/m2.
As previously suggested for obese patients scheduled to undergo bariatric surgery [20], all 974 patients underwent a preoperative esophagogastroduodenoscopia (EGDS). If Helicobacter pylori was present, it was treated by standard eradication therapy. All the patients received an antipulmonary thromboembolism (PE) prophylaxis according to SICOB guidelines. One of two patients younger than 18 years presented with Prader Willi syndrome (PWS).
Table 1 shows the mean preoperative parameters in terms of BMI, presence of type 2 diabetes mellitus (T2DM), and hypertension. In this study, T2DM was defined according to the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) guidelines [21].
The first end point of the study was the assessed safety of MGB. For this aim, all intra- and perioperative parameters were reported. Additionally, both early and late complications occurring during the follow-up were described.
The second end point was the gastrointestinal endoscopic status of the patients. From this perspective, 26 patients (3.1 %) presenting with prolonged dyspepsia, heartburn, vomiting, or gastric pain symptoms during the follow-up period underwent EGDS to evaluate the presence of histologic abnormalities. The endoscopic findings and the timing of their appearance also were reported.
A final end point was the assessed efficacy of this surgery in the long term. For this aim, percentage of excess weight loss (EWL %), BMI decrease, glycemic status, and blood arterial pressure (BP) were assessed 1, 3, and 5 years after the intervention. Remission of T2DM was defined as glycated hemoglobin (HbA1c) less than 6.5 % in the absence of hypoglycemic drugs. Remission of hypertension was defined as the discontinuation of antihypertensive therapy.
To define perioperative complications, all 974 operated patients were considered. To define long-term complications, all the patients currently being followed up were considered. To assess MGB efficacy in terms of both diabetes and hypertension resolution, all the patients presenting with at least 1 year of follow-up evaluation were considered. Data are reported as mean ± standard deviation.
Surgical technique
All 974 patients were approached by laparoscopy. In all cases, five to six ports were used. To create the gastric pouch, the caliber of the bougie used was 42 Fr in 380 cases, 40 Fr in 70 cases, and a smaller 36 Fr in 524 cases. With all the patients considered, the length of the jejunal loop was measured to be 224.6 ± 23.2 cm from the Treitz duodenal ligament according to Lee et al. [9].
In all cases, the gastrojejunal anastomosis was performed with a blue cartridge linear stapler. A 30-mm cartridge was used in 70 cases, whereas 45-mm cartridges were used in 451 patients and 60-mm cartridges in 453 patients.
In 573 patients, the stapler holes where closed by a double-layer running 2–0 suture, whereas a single layer running 2–0 suture was used in 21 patients. In 380 patients, interrupted 2–0 stitches were used. In 451 patients, an antibiliary reflux mechanism [4] was provided. A reinforcement of the suture line was obtained by a fibrin sealant in 52 patients and by oversewing in 45 patients. All 974 patients were checked by an intraoperative methylene blue test at the end of the procedure. A drain tube was placed in all the patients.
Results
Perioperative outcome
The mean duration of the procedure was 95 ± 51.6 min. The conversion rate to open surgery was 1.23 % (12/974). In 8 (66.6 %) of 12 cases, the cause for conversion was abdominal adhesions. A jejunal loop tear, Veress needle vascular damage, and two spleen injuries were responsible for the remaining conversions. A postoperative intensive care unit stay of 57.6 ± 50.4 h was needed by 56 patients (5.7 %).
The overall mortality rate was 0.2 % (2/974). One of the two deaths was related to MGB procedure complications (0.1 %), whereas the other followed a PE occurrence. The perioperative morbidity rate was 5.5 % (54/974).
Table 2 presents in detail the postoperative complications that occurred within the first 30 days. An early surgical revision was required for 20 (2 %) of the 974 patients. A liquid diet was started for all the patients at 2.5 ± 1.1 postoperative days. The mean hospital length of stay (LOS) was 4.0 ± 1.7 days.
Follow-up outcome
At this writing, 795 (94.8 %) of 838 eligible patients have been followed up for 1 year, 510 (89.4 %) of 570 eligible patients for 3 years, and 201 (79.1 %) of 254 eligible patients for 5 years. The total number of dropouts has been 156 (16 %) of the 974 patients, although 136 patients who underwent surgery later than December 2011 have had a follow-up period shorter than 12 months. Globally, 818 patients under follow-up evaluation from July 2006 to December 2012 have therefore been considered.
The complications that occurred during the follow-up period are reported in Table 3. The majority of these complications (66/74, 89.1 %) occurred within the first postoperative year. A late revision surgery was required for 7 (0.8 %) of the 818 patients, with 2 patients (0.2 %) undergoing redo surgery for both EWL higher than 100 % and weight regain.
Among 26 (3.1 %) of the 818 patients requiring EGDS for the aforementioned clinical symptoms, biliary gastritis was an endoscopic finding for 8 patients (0.9 %, 8/818), peptic anastomotic ulcers for 14 patients (1.7 % (14/818), and gastric pouch enlargement causing dyspepsia and gastric pain for the remaining 4 patients (0.4 %, 4/818). Conservative treatment was effective in all cases except for 4 of 14 patients needing a surgical revision. No dysplasia of any grade was encountered.
Table 4 presents the time at which the endoscopic findings were presented and the year of surgery. At this writing, all these patients remain under careful follow-up evaluation. If all 224 diabetic patients who underwent surgery are considered, at this writing, the follow-up period has been shorter than 1 year for 9 patients and has been 1 year for 201 (93.4 %) of 215 eligible patients, 3 years for 186 (97.3 %) of 191 eligible patients, and 5 years for 103 (85.8 %) of 120 eligible patients.
If all 291 hypertensive patients who underwent surgery are considered, at this writing, the follow-up period has been shorter than 1 year for 67 patients and has been 1 year for 190 (84.8 %) of 224 eligible patients, 3 years for 155 of 181 eligible patients (85.6 %), and 5 years for 96 (77.4 %) of 124 eligible patients. Table 5 presents the outcomes of the current study in terms of weight loss, diabetes, and hypertension resolution at 1, 3, and 5 years of follow-up evaluation, respectively.
Discussion
In the last decade, some articles have reported an appealing outcome for the MGB. It has been described as a reasonable laparoscopic operation meeting many of the criteria of an ideal weight loss surgery [1]. The results presented regarding the perioperative period have been encouraging in terms of safety. A short operative time corresponding with very low rates of mortality, morbidity, and LOS have been reported [1–8], with a favorable outcome for MGB even compared with RYGBP [3].
Our current series appears to be in agreement with published results. As shown in Table 6; our mortality rate was 0.2 %, with a perioperative complication rate of 5.5 % and an LOS of 4.0 ± 1.7 days. A very acceptable morbidity rate during the follow-up period (9 %) also was confirmed in our study.
Nevertheless, when presented in 2001, MGB raised several doubts due to the predictable high rate of both biliary reflux in the short term and gastric pouch cancer in the long term [11, 12]. These worrisome complications were attributed to the proposed technique, which involved a single-loop anastomosis, thus resembling the Billroth II (BII) reconstruction after subtotal gastrectomy.
Conversely, according to authors performing MGB–OAGB, biliary reflux rarely has been found, and if present, has been symptomatic only in a small number of patients. This was described by Carbajo et al. [4], who reported the lack of symptomatic biliary reflux in a series of 209 patients at 2 years, and by Noun et al. [8], who reported the same results for 923 primary MGBs. Finally, Chevallier et al. [22], in a series of 451 patients enrolled in a postoperative screening program, found 57 (75 %) of 76 EGDS normal at 2 years, 5 peptic ulcers (11.9 %), and 2 follicular hyperplasias (4.6 %) but no dysplasia in 43 endoscopic biopsies 4 years after MGB surgery in asymptomatic patients. Our data seem to confirm this trend, showing biliary gastritis at 0.9 %, anastomotic ulcers at 1.7 %, and no dysplasia after EGDS in 26 symptomatic subjects during the follow-up period, with no patient requiring any redo surgery related to biliary reflux.
Authoritative warnings against the cancer risk coming from BII reconstruction were published starting from the mid-1980s [23–25]. In those papers, the passage of bile reflux into the stomach was supposed to strongly empower carginogenesis, leading to a significantly higher rate of gastric stump cancer observed during the long term in patients who underwent a BII surgery for benign peptic disease compared with those who had a BI reconstruction. However, it must be remarked that during the same period, although some papers claimed a nonsignificant difference in the gastric stump cancer rate between BI and BII [26, 27], the potential carcinogenetic role of Helicobacter pylori was not yet completely understood [28].
From this perspective, an interesting metaanalysis published in 1990 [29] evaluating 827 gastric stump cancers in patients who underwent a subtotal gastrectomy for benign disease showed that the difference in cancer rate was not significant after BII reconstruction compared with BI reconstruction, leading those same authors to affirm the endoscopic surveillance of postgastrectomy patients to be justified only for selected cases [30]. Similar concepts were later reprised by Bassily et al. [31], and this is what led us to consider a screening postoperative EGDS to be unjustified for our patients, in whom Helicobacter was indeed negative or eradicated before surgery.
These observations, representing the scientific background driving us to consider MGB as safe surgery to be proposed, have been confirmed in a recent metaanalysis published by Scozzari et al. [32]. In their paper, 33 esophagogastric cancers after bariatric procedures are reported. Although four cancers appeared after a loop bypass (12.1 %), three were detected in the excluded stomach, and thus were unrelated to the surgical reconstruction. One of them was found in the gastric pouch 26 years later during a 1980 surgery that certainly was not a mini-gastric bypass first described in 2001.
On the other hand, a worrisome finding of this paper is that 15 esophagogastric cancers (45.4 %) followed restrictive bariatric procedures including LAGB, VBG, and SG, 14 (42.4 %) of which were detected after RYGBP including five located in the excluded stomach. Finally, although studies of a potential gastric carcinogenesis induced by BII consider a follow-up period longer than 15 years [23–29], which we cannot have for any MGB series, it must be remembered that the pathogenetic basis for these gastric resections was a Helicobacter pylori infection, responsible for a peptic ulcer and unknown at that time. To confirm such a hypothesis, only a long-term EGDS screening study after MGB, although debatable [30, 31], could give an accurate answer. To date, the endoscopic findings from our MGB series and others do not raise any significant alarm.
If we consider the long-term results of the changes in body weight and resolution of obesity-related comorbidities at 1, 3, and 5 years, our series shows a satisfactory comparison with published papers (Fig. 2; Table 6). The concept of a logarithmic decline in weight loss [2] appears to be confirmed at 5 years in our series, whereas both T2DM and hypertension remission is maintained at 5 years (84.4 and 87.5 %, respectively; Table 5).
To date, only Lee et al. [16] have reported a follow-up assessment for MGB patients at 10 years. In their study, MGB proved to be effective in the long term, significantly outperforming even RYGB in several parameters including BMI reduction, resolution of metabolic syndrome, and the need for revision surgery due to both bowel obstruction and internal hernia.
Frequently, MGB is reported as an easier technique [1–9], to be preferred to other bariatric approaches, including both RYGB and SG, for the results in both the short and long terms [3, 16]. Although technical simplicity and shorter operative time are unquestionable issues in the choice of an intervention, we do however support the use of MGB, especially for the positive results reported in terms of safety, efficacy in the treatment of morbid obesity, and resolution of comorbidities.
To define safety, a very comprehensive issue has been raised by the American College of Surgeons (ACS) [33]. In the ACS study, 28.616 patients were reviewed. The results, while addressing a rising trend for laparoscopic SG, showed a 30-day mortality rate of 0.1 %, a 30-day morbidity rate of 5.61 %, and an early reintervention rate of 2.97 %.
Conversely, LAGB and laparoscopic RYGBP presented respective 30-day mortality rates of 0.05 and 0.1 %, 30-day morbidity rates of 1.44 and 5.91 %, and finally, early reintervention rates of 0.9 and 5.02 %. Our series seems to conform in terms of safety relative to SG and RYGBP, with a 30-day mortality rate of 0.2 % (although only one death (0.1 %) was effectively related to surgical technique) and a 30-day morbidity rate of 5.5 %, but with an early reintervention rate of 2 %, lower than for either SG or RYGBP.
With regard to efficacy of bariatric procedures, Padwal et al. [34], in an interesting metaanalysis of 31 randomized controlled trials, reported the good performance of MGB in producing significant BMI reduction. In that study, MGB exceeded other bariatric procedures such as RYGB, SG, VBG, LAGB, and even BPD by producing a decrease in BMI levels from baseline of −11.3 kg/m2 at 1 year. O’Brien et al. [35], in a systematic review of bariatric literature limited to studies with a follow-up period longer than 10 years, reported, by pooling data, an EWL ranging from 28 to 68 % for RYGBP and from 33 to 64 % for LAGB. These data appear to show significantly less effectiveness than the EWL of 72 ± 19.3 % reported in the only study available for MGB at 10 years [16]. Our results, showing an EWL of 77 ± 5.14 %, although limited to 5 years, seems to confirm this trend.
Gastric sleeve and RYGBP both have shown good results in terms of diabetes resolution. However, Gill et al. [36] described a T2DM resolution rate of 66.2 % after SG in a metaanalysis involving 673 patients with a follow-up period limited to 36 months, whereas Higa et al. [37], in a long-term evaluation of 242 patients who underwent RYGBP, showed a T2DM resolution of 67 % at 10 years. In the same study, 86 % of the patients experienced hypertension resolution. From this perspective, although limited to a follow-up period of 5 years, our T2DM and hypertension resolution rates of 84.4 and 87.5 %, respectively, appear encouraging.
Our series presents several limitations. It was a retrospective study in which the predictable loss of some data, in addition to the dropout of patients at follow-up assessment, must be taken into account. The MGB outcome for 16 % of all the patients in fact remain unknown in terms of weight loss, endoscopic abnormalities, diabetes, and hypertension.
In conclusion, in our opinion, the most important criteria in the selection of a bariatric procedure remain safety and efficacy in the resolution of both weight loss and comorbidities during the long term rather than a faster or easier approach. Despite the intrinsic limitation imposed by a retrospective study, our results seem to confirm that to date, the MGB surgery is both safe and effective for the treatment of morbidly obese patients.
References
Rutledge R (2001) The mini-gastric bypass: experience with the first 1,274 cases. Obes Surg 11:276–280
Rutledge R, Walsh W (2005) Continued excellent results with the mini-gastric bypass: six-year study in 2,410 patients. Obes Surg 15:1304–1308
Lee WJ, Yu PJ, Wang W et al (2005) Laparoscopic Roux-en-Y versus mini-gastric bypass for the treatment of morbid obesity. Ann Surg 242:20–28
Carbajo MA, Garcia-Caballero M, Toledano M et al (2005) One anastomosis gastric bypass by laparoscopy: results of the first 209 patients. Obes Surg 15:398–404
Chakhtoura G, Zinzindohoué F, Ghanem Y, Ruseykin I, Dutranoy JC, Chevallier JM (2008) Primary results of laparoscopic mini-gastric bypass in a French obesity-surgery specialized university hospital. Obes Surg 18:1130–1133
Peraglie C (2008) Laparoscopic mini-gastric bypass (LMGB) in the super–super obese: outcomes in 16 patients. Obes Surg 18:1126–1129
Piazza L, Ferrara F, Leanza S, Coco D, Sarvà S, Bellia A, Di Stefano C, Basile F, Biondi A (2011) Laparoscopic mini-gastric bypass: short-term single-institute experience. Updates Surg 63:239–242
Noun R, Skaff J, Riachi E, Daher R, Antoun NA, Nasr M (2012) One thousand consecutive mini-gastric bypass: short- and long-term outcome. Obes Surg 22:697–703
Lee WJ, Wang W, Lee YC, Huang MT, Ser KH, Chen JC (2008) Laparoscopic mini-gastric bypass: experience with tailored bypass limb according to body weight. Obes Surg 18:294–299
Mason EE, Ito C (1967) Gastric bypass in obesity. Surg Clin North Am 47:1345–1351
Fisher BL, Buchwald H, Clark W, Champion JK, Fox SR, MacDonald KG, Mason EE, Terry BE, Schauer PR, Sugerman HJ (2001) Mini-gastric bypass controversy. Obes Surg 11:773–777
Johnson WH, Fernanadez AZ, Farrell TM, Macdonald KG, Grant JP, McMahon RL, Pryor AD, Wolfe LG, DeMaria EJ (2007) Surgical revision of loop (“mini”) gastric bypass procedure: multicenter review of complications and conversions to Roux-en-Y gastric bypass. Surg Obes Relat Dis 3:37–41
Collins BJ, Miyashita T, Schweitzer M, Magnuson T, Harmon JW (2007) Gastric bypass: why Roux-en-Y? A review of experimental data. Arch Surg 142:1000–1003
Chevallier JM, Chakhtoura G, Zinzindohoué F (2009) Laparoscopic mini-gastric bypass. J Chir Paris 146:60–64
Kim Z, Hur KY (2011) Laparoscopic mini-gastric bypass for type 2 diabetes: the preliminary report. World J Surg 35:631–636
Lee WJ, Ser KH, Lee YC, Tsou JJ, Chen SC, Chen JC (2012) Laparoscopic Roux-en-Y vs mini-gastric bypass for the treatment of morbid obesity: a 10-year experience. Obes Surg 22:1827–1834
Lee WJ, Chong K, Ser KH, Lee YC, Chen SC, Chen JC, Tsai MH, Chuang LM (2011) Gastric bypass vs sleeve gastrectomy for type 2 diabetes mellitus: a randomized controlled trial. Arch Surg 146:143–148
Musella M, Milone M, Bellini M et al (2012) Effect of bariatric surgery on obesity-related infertility. Surg Obes Relat Dis 8:445–449
www.sicob.org. Accessed 24 Sept 2012
Muñoz R, Ibáñez L, Salinas J, Escalona A, Pérez G, Pimentel F, Guzmán S, Boza C (2009) Importance of routine preoperative upper GI endoscopy: why all patients should be evaluated? Obes Surg 19:427–431
Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR (2012) Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 55:1577–1596
Chevallier JM, Trelles N, Arienzo R, Jamal W, Chakhtoura G, Zinzindohoué F (2011) Endoscopic findings after laparoscopic omega loop gastric bypass. Obes Surg 21:956
Caygill CP, Hill MJ, Kirkham JS, Northfield TC (1986) Mortality from gastric cancer following gastric surgery for peptic ulcer. Lancet 1:929–931
Viste A, Bjørnestad E, Opheim P, Skarstein A, Thunold J, Hartveit F, Eide GE, Eide TJ, Søreide O (1986) Risk of carcinoma following gastric operations for benign disease: a historical cohort study of 3,470 patients. Lancet 2:502–505
Lundegårdh G, Adami HO, Helmick C, Zack M, Meirik O (1988) Stomach cancer after partial gastrectomy for benign ulcer disease. N Engl J Med 319:195–200
Fischer AB, Graem N, Jensen OM (1983) Risk of gastric cancer after Billroth II resection for duodenal ulcer. Br J Surg 70:552–554
Tokudome S, Kono S, Ikeda M, Kuratsune M, Sano C, Inokuchi K, Kodama Y, Ichimiya H, Nakayama F, Kaibara N et al (1984) A prospective study on primary gastric stump cancer following partial gastrectomy for benign gastroduodenal diseases. Cancer Res 44:2208–2212
Ito M, Takata S, Tatsugami M et al (2009) Clinical prevention of gastric cancer by Helicobacter pylori eradication therapy: a systematic review. J Gastroenterol 44:365–371
Tersmette AC, Offerhaus GJ, Tersmette KW, Giardiello FM, Moore GW, Tytgat GN, Vandenbroucke JP (1990) Meta-analysis of the risk of gastric stump cancer: detection of high-risk patient subsets for stomach cancer after remote partial gastrectomy for benign conditions. Cancer Res 50:6486–6489
Offerhaus GJ, Tersmette AC, Giardiello FM, Huibregtse K, Vandenbroucke JP, Tytgat GN (1992) Evaluation of endoscopy for early detection of gastric-stump cancer. Lancet 340:33–35
Bassily R, Smallwood RA, Crotty B (2000) Risk of gastric cancer is not increased after partial gastrectomy. J Gastroenterol Hepatol 15:762–765
Scozzari G, Trapani R, Toppino M, Morino M (2013) Esophagogastric cancer after bariatric surgery: systematic review of the literature. Surg Obes Relat Dis 9:133–142
Hutter MM, Schirmer BD, Jones DB, Ko CY, Cohen ME, Merkow RP, Nguyen NT (2011) First report from the American College of Surgeons Bariatric Surgery Center Network: laparoscopic sleeve gastrectomy has morbidity and effectiveness positioned between the band and the bypass. Ann Surg 254:410–422
Padwal R, Klarenbach S, Wiebe N, Birch D, Karmali S, Manns B, Hazel M, Sharma AM, Tonelli M (2011) Bariatric surgery: a systematic review and network meta-analysis of randomized trials. Obes Rev 12:602–621
O’Brien PE, MacDonald L, Anderson M, Brennan L, Brown WA (2013) Long-term outcomes after bariatric surgery: fifteen-year follow-up of adjustable gastric banding and a systematic review of the bariatric surgical literature. Ann Surg 257:87–94
Gill RS, Birch DW, Shi X, Sharma AM, Karmali S (2010) Sleeve gastrectomy and type 2 diabetes mellitus: a systematic review. Surg Obes Relat Dis 6:707–713
Higa K, Ho T, Tercero F, Yunus T, Boone KB (2011) Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis 7:516–525
Acknowledgments
Authors would like to thank Prof. M. Taglialatela and Dr. P. Bianco for their precious support.
Disclosure
M. Musella, A. Susa, F. Greco, M. De Luca, E. Manno, C. Di Stefano, M. Milone, R. Bonfanti, G. Segato, A. Antonino, and L. Piazza have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Musella, M., Susa, A., Greco, F. et al. The laparoscopic mini-gastric bypass: the Italian experience: outcomes from 974 consecutive cases in a multicenter review. Surg Endosc 28, 156–163 (2014). https://doi.org/10.1007/s00464-013-3141-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-013-3141-y