Abstract
Physical trauma in the central nervous system (CNS) is usually the result of a number of forces in different directions and dimensions. A large number of experimental models have been developed to improve the possibilities to understand the outcome of CNS trauma. In this chapter, we will describe the need for a variety of experimental models for research on traumatic brain injury (TBI) and spinal cord injury (SCI). Models can serve different needs, such as: to test new treatments for injuries, to reveal thresholds for injuries, to provide a better understanding of injury mechanisms, or to test tools and methods for translation between experiments and clinical data. In this chapter, we will discuss on the validation of models and translation between experimental and clinical studies.
Access provided by CONRICYT – Journals CONACYT. Download protocol PDF
Similar content being viewed by others
Key words
1 Introduction
The central nervous system (CNS) is the most delicate and complex part of the body. The definition for the CNS is based on the glial cells that surround and support neurons. Both the brain and the spinal cord are included in the CNS, since these parts of the nervous system comprise astrocytes and oligodendrocytes. Spinal nerve roots and peripheral nerves contain Schwann cells and are therefore regarded as parts of the peripheral nervous system (PNS).
Physical trauma in the central nervous system is often the result of a number of forces in different directions and dimensions. The timeline for the interaction between the acting forces and the nervous tissue is usually very narrow and it can therefore be very difficult to assess the influence of each contributing force. In addition, human patients, which come in different ages and sizes, may have a number of additional injuries or diseases as well a genetic background that may influence the outcome of the injury.
1.1 Spinal Cord Injury (SCI)
It has been known since ancient civilizations, such as the Pharaonic Egypt, that spinal cord injury (SCI) leads to chronic loss of functions, such as paralysis. The complex cellular response and lack of successful regenerative growth in CNS was described in great detail by Ramón y Cajal [1]. Although a substantial amount of research on SCI has been conducted, there has been only limited success in the identification of new strategies to improve the regenerative response after SCI. Models for SCI usually have a more regenerative focus than the models for brain injury.
1.2 Traumatic Brain Injury (TBI)
TBI is a leading cause for death and disability in both civilian life and at the battlefield. The signature TBI has evidently changed from penetrating TBI to blast-induced TBI in recent military conflicts. All types of TBI may occur in both the civilian and military setting. However, there are some important considerations for military TBI, mostly relating to the extreme energy transfer.
-
1.
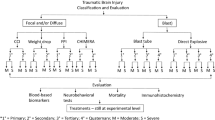
TBI can be graded from mild to severe and primary or secondary. TBI can be classified as diffuse or focal, and very often in a complex mixture.
-
(a)
Mild TBI: A TBI is often classified as mild (concussion or commotion) if loss of consciousness or confusion is shorter than 30 min. MRI (magnetic resonance imaging) and CT (computer tomography) scans are usually normal but the patient may have headache, cognitive problems (memory problems, mood disturbance, attention deficits), and the effect on the patient can be devastating. The majority of blast-induced TBI fall into this category, although the pathophysiology is largely unknown. Cerebral concussion is often associated with other types of brain injury.
-
(b)
Moderate and Severe TBI: These injuries can be divided into closed head injuries and penetrating injuries. Closed head injuries may be both diffuse and focal. The penetrating TBI will always induce a focal injury and often diffuse secondary injuries.
-
(c)
Diffuse TBI: The most common diffuse injury is the diffuse axonal injury (DAI), which is defined as the presence of diffuse damage to axons in the cerebral subcortical parasagittal white matter , corpus callosum, brain stem, and cerebellum. This is usually the result of an acceleration/deceleration trauma. Different parts of the brain move at different speeds because of their relative density. If this is a rotational trauma, the positions of the axis of rotation will be an important factor in the injury mechanism and areas at a greater distance from this axis will sustain larger forces. This can lead to shearing injury and DAI. Beta-amyloid precursor protein (APP) has been proven to be an excellent marker for axonal injury in histology. Modern imaging techniques, such as MRI with DTI (diffusion tensor imaging), have provided improved possibilities to detect DAI.
-
(d)
Focal TBI: Focal brain injuries include contusions and penetrating TBI. Focal TBI is usually the result of bullet and shrapnel entrance in the skull cavity or a contact between the head and a sharp or semi-blunt object that results in skull fracture. Also acceleration/deceleration trauma can cause focal injuries to the brain.
-
(e)
Secondary traumatic brain damage occurs as a complication of the different types of primary TBI and includes ischemic and hypoxic damage, swelling, raised intracranial pressure, and infection. The onset of these complications varies from minutes to hours. The secondary TBI is potentially reversible with adequate treatment. Axonal damage in both DAI and focal injuries interferes with axoplasmic transport. Severe traumatic injury results in primary axonal disruption or transection termed “primary axotomy” or sets in train a series of ill-understood events culminating in secondary axonal degeneration or secondary axotomy. Thus, adequate treatment could probably limit the axonal damage.
-
(a)
-
2.
Experimental models for studies of CNS injuries
Experimental research is a strategy to take control over confounding factors that may obscure data from real life clinical CNS injuries.
-
3.
Experimental models may serve many different purposes, such as
-
(a)
To test new treatments for injuries.
-
(b)
To provide a better understanding of injury mechanisms .
-
(c)
To reveal thresholds for injuries.
-
(d)
To develop test tools and methods for clinical settings. For example to develop protocols for MRI, new biomarkers, protocols for EEG.
-
(a)
1.3 Model requirements
It is difficult to provide a complete list of all different models that are employed in neuroscience. We will limit the description to examples of models for traumatic injuries and therefore exclude models for stroke, neurodegenerative diseases, infections, etc. It is usually important to test if the data from the employed model can be translated and provide any conclusions for the condition that is supposed to mimic. It is also important to enable verification of any data that can be harvested from the model. Thus, a good monitoring and documentation of physical data should be provided from all new models. The model needs to be both validated and verified. Thus, to show that the model can replicate exactly what it is suggested to replicate and that the experiments can be repeated by both the scientists that have developed the model and by any other scientist that has the proper tools. This is a highly complex process, since the methods for measurement also need to be validated and verified. It can be supposed that many of the failures in translating new treatments from experimental setups to clinical practice may be due to mistakes in verification and validation of the model or the experimental setup. It has also been said that a lot of published experimental data cannot be repeated, possibly due to improper validation and description of the experimental setup.
1.4 Obstacles for Translation
-
1.
There are a number of more or less obvious factors that may impede translation between an experimental model and the clinical situation—even if the model has been properly characterized:
-
(a)
Trauma in the clinical situation is the result of many complex forces, delivered during a short time. It is therefore extremely difficult to produce a model that can in all details simulate a clinical situation.
-
(b)
Severe trauma to the head or spine is usually combined with other injuries, thus a multitrauma situation that can modify the outcome of the TBI or spinal cord injury by for example a systemic inflammation, infection, and hypoxia. The importance of such contributing factors can be tested in the experimental situation, but will still provide an obstacle in translation between experiments and the clinical populations.
-
(c)
The time scale for biological response in experimental animals, such as rodents, is probably very different than that in humans.
-
(d)
The genetic variation in rodent strains is usually very limited compared to clinical populations. It is therefore possible that some results are over-amplified in the experimental situation and may not at all be relevant in a clinical situation.
-
(a)
2 Experimental Models of Brain Neurotrauma
Below are a set of different experimental models of brain trauma. For each model, we will try to describe the rationale (why the model was developed), the development, results obtained, and limitations with the model. We will also describe the work with validation, verification, and translation. In each section, we also give examples of alternative useful and validated models.
2.1 Spinal Injury, with Focus on Motor Axons
The pioneering studies of Ramón y Cajal demonstrated that injured neurons in the central nervous system (CNS) have a strong capacity to extend new axons into the peripheral nervous system (PNS) [1], he showed that motor axons that had been severed due to spinal cord injury had the capacity to regrow to neighboring ventral roots. The observation that neurons in the CNS could extend axons into PNS tissue was reinvestigated by Richardson and colleagues [2].
2.1.1 A Lesion in the Ventral Funiculus of the Spinal Cord
With background from the observations that motoneurons in adult cats survived after peripheral nerve injuries to a much better degree than sensory neurons, it was decided to analyze if motoneurons would survive also after very proximal injuries. The most proximal location would then be to cut the axons inside the spinal cord, but outside the motor nuclei in the grey matter. The selected site was the ventral funiculus, i.e. the white matter between the ventral horn and the transition to the spinal ventral nerve root. The experiments were performed in adult cats that were subjected to a lumbar laminectomy. The denticulte ligament at the side of the lumbosacral enlargement was divided and used to gently twist the spinal cord so that the junction between the spinal cord and the ventral root was visible. A thin fragment of a razor blade (or a specialized knife for micro-surgery) was pushed into the lateral aspect of the spinal cord segment L7 and moved longitudinally to produce a selective lesion in the ventral funiculus. The aim was to cut the motor axons at this location, without damage to the grey matter (where the cell bodies reside) or the connection between the spinal cord and the nerve root. It was observed that, although the animals were deeply anesthetized, the muscles in the hindlimb corresponding to the L7 segment (the L7 myotome) responded with contractions during this procedure. The erector spinae muscle, fascia, and skin were closed with sutures in separate layers. The animals were sacrificed after survival times from 1 to around 300 days and fixed by intravascular fixation with glutaraldehyde. Using electron microscopy, it was revealed that the lesion was located in the white matter and had spared both the grey matter and the nerve root exit zone. A large proportion of the motoneurons actually had survived the lesion (Fig. 1).
A schematic representation of the ventral funiculus lesion model. The lesion area in the ventral funiculus of the spinal cord is penetrated by regrowing motor axons, surrounded by a thin sheet or glial tissue. The extracellular room is expanded and contains large amounts of matrix molecules such as laminin and collagen, the blood–brain barrier has a more or less permanent defect
It was shown with electron microscopy and intracellular labeling with horseradish peroxidase that axons from such surviving motoneurons penetrated the scar tissue in the ventral funiculus of the spinal cord and entered the ventral roots [3–5]. The regrowing axons penetrate through a highly unusual CNS environment which lacks a blood–brain barrier (BBB) function [6] but possesses a high content of cells bearing neurotrophin receptors [7–9] and matrix molecules [10, 11].
2.1.2 Avulsion Injuries: The Clinical Use of the Observed Regenerative Response
A clinical counterpart to this injury is a ventral root avulsion at the border between the CNS and PNS, typically caused by a high-energy trauma such as a motorbike accident causing excessive trauma to the shoulder and head resulting in stretching and rupturing of ventral roots. Ventral root avulsion is not followed by spontaneous regrowth, since the avulsed roots are widely separated from the spinal cord inside the subarachnoid space or even pulled to a position outside the vertebral channel. Replantation of avulsed spinal ventral roots into the spinal cord (Fig. 2) has been shown to enable significant and useful regrowth of motor axons in both experimental animals and human clinical cases [12–15]. Gene expression array studies show that replantation of the ventral root can initiate a rapid upregulation in the expression of genes associated with neurite growth, in contrast to neurons subjected to avulsion only [16]. Thus, the replantation can influence gene programs in the spinal cord.
A schematic representation of replantation of avulsed ventral roots. The ventral roots are avulsed at the border between CNS and PNS (spinal cord surface). The rootlets are then replanted into the ventro-lateral surface of the spinal cord. Regrowth into the ventral root can occur both directly within the spinal cord and by growth in the pia mater. After reaching the ventral root, motor axons can continue and reinnervate denervated muscle
The results from such treatment in humans are less successful in older patients and good reinnervation in distal muscles like in the hand is seldom possible. In a recent case report, Carlstedt et al. [14] described a preadolescent boy with complete brachial plexus avulsion injury that was treated by replantation of five ventral roots. Shoulder muscle recovery started 8–10 months after the spinal cord operation. At 12–15 months, elbow function began to recover, followed 2 years postoperatively by forearm, wrist, and intrinsic hand muscle activity. This led to recovery of hand motor function without restoration of sensation. Bilateral motor cortex activity and activation of the sensory cortex on use of the affected hand was demonstrated by fMRI . The findings of that case study suggested that the restored hand function might rely on cortical sensory programs established before the injury. Although the time needed for recovery seems very long, it cannot be excluded that the final result is dependent on several biological programs that are elicited in the early acute stage.
The method for producing nerve root injuries has a significant role for the outcome of the injury. Rhizotomy (division of the root) leads to a milder representation of the spinal cord trauma that occurs after “true” avulsion injury [17]. Shortland and colleagues employ a model for extra-vertebral avulsion (without need for laminectomy) [18]. However, for replantation surgery laminectomy is necessary. One limitation with most animal studies for replantation is that the injury and the replantation surgery are performed at the same time, whereas delayed surgery is the typical clinical situation.
This is to our knowledge, the only example of an experimental model that has been translated into practical clinical use for treatment of a traumatic injury that involves axonal growth in the spinal cord. Many models for SCI seem to simplifications of the usual clinical type of SCI. Maybe it would be of benefit to develop models for spinal cord contusion that could represent a better representation of actual clinical situations, with high-energy transfer, rapid deformation of vertebra and incomplete injury to the spinal cord.
2.2 TBI in the Military Setting: Modeling Primary Blast TBI
The use of Improvised Explosive Devices (IED) in contemporary warfare has changed the scene and spectrum of TBI at the battlefield. At the same time, new equipment for body protection has increased the survival rate after TBI at the battlefield. It may be assumed that several mechanisms contribute to the injury. TBI has been identified as major health problem in military personnel returning from service. The injuries range from severe multitrauma to a number of mild TBI that still has to be settled. Propagation of blast waves is very complex. It could involve both direct propagation through the skull and indirect propagation via blood vessels and it is obvious that a systemic response comes along with the blast TBI. It is difficult to identify a reliable borderline between mild blast TBI and posttraumatic stress syndrome (PTSD). Many of the symptoms are similar and many patients might suffer from both TBI and PTSD. The energy transfer during an explosion is extremely complex and it is difficult to predict how energy is propagated into the body and absorbed. Exposure data from clinical situations at the battlefield are usually lacking. One way to generate a better understanding of the mechanisms of TBI after a blast exposure is to perform controlled experiments in animals. Many clinical TBI cases have a complex mixture of diffuse and focal injuries, which are complicated by secondary injury events. Individuals exposed to a blast often suffer from multiple injuries, i.e., pulmonary lesions or amputations. Severe blast-related TBI with brain edema and vascular spasm [19] can be assumed to be the result of a combination of more than one injury mechanism (see Fig. 3).
A schematic representation of different mechanisms for blast-induced neurotrauma. Previously published in [94]
-
1.
One way to understand the effects of a blast wave is to divide the mechanism into
-
(a)
Primary blast: Effects of the primary blast wave, thus the propagation of a supersonic pressure transient with short duration. The threshold for injuries is determined by factors such as peak pressure, duration, and shape of the wave.
-
(b)
Secondary effects of blast, i.e., due to the impact of flying objects, such as shrapnel fragments, which can generate penetrating injuries. The proportion of such injuries was larger in previous conflicts and seems to have been reduced by improvements in helmet construction.
-
(c)
Tertiary effects of blast, i.e., the result of acceleration movements, which may result in tissue shearing and diffuse injuries, such as diffuse axonal injuries (DAI).
-
(d)
Quaternary effects of blast, the result of heat, smoke, or emission of electromagnetic pulses (EMP).
-
(a)
-
2.
Open field exposure
Large-scale experiments during the 1950s in desert areas and ponds generated fundamental data for effects of blast with simple wave forms. Large numbers of animals of different species were subjected to open field exposure to blast. These experiments determined thresholds for mortality and injuries such as bleeding in air-filled organs such as the lungs and intestines. The potential effects on the central nervous system were generally not assessed. These experiments provided the Friedländer type of wave and dose–response curves (the Bowen curves) were determined [20–22]. Large amounts of explosives are needed and dosimetry can be difficult. Good control of the physiology of the experimental animals and proper tissue collection is usually not possible in outdoor conditions in combination with a large number of animals in a single experiment. However, open field experiments may allow for more realistic experiments with large animals that are more similar in size to humans. It also makes it possible to use waveforms relevant for simulation of IED, for example reflection from the ground or vehicles. Examples of new models with open field exposures aimed to produce mild TBI include the Combat Zone-like blast scenery for mice [23] and a primate model [24].
-
3.
Shock tubes with compressed air or gas
Shock tubes employ compressed air or gas, rather than explosives. Systems with compressed air were used already in the 1950s [25]. Most systems comprise two chambers, separated by a membrane (Fig. 4). Compressed gas is loaded into one of these chambers (the overpressure chamber or the driver section), which is separated from the other chamber, referred to as the main section or the driven section, by a diaphragm. The main section is usually several meters long. The object, i.e., the experimental animal, is positioned somewhere in the main section and the operator can rupture the diaphragm. The compressed gas enters the main section and simulates a propagating blast wave. One advantage associated with this type of shock tube is the absence of quaternary blast effects as well as other disadvantages of explosives. There are a number of modifications of the shock tube design and there seems to be a need to calibrate the different systems. Well-documented modern shock tubes can for instance be found at the Walter Reed institute [26], Wayne State University [27], and the US Naval Medical Research Center (Maryland, Silver Spring, USA) [28, 29]. One sophisticated shock tube system has been installed at the Applied Physics Laboratory at Johns Hopkins University [30]. This is a modular, multi-chamber shock tube capable of reproducing complex shock wave signatures. The instrumentation should allow direct measurement and calculation of the various shock loading characteristics, including static pressure , total pressure, and overpressure impulse.
Fig. 4 A schematic representation of a typical over pressure shock tube composed of two chambers separated by a membrane. Compressed air/gas in the driver section is released as a pressure wave to the other (driven) compartment by the controlled puncture of the membrane. Previously published in [94]
-
4.
A Swedish Blast tube for studies on primary blast
In 1949, Carl-Johan Clemedson published a thesis titled “An experimental study on air blast injuries” in 1949 at the university in Uppsala [31]. He continued his research at FOA (Swedish Defence Research Establishment) using compressed air [25] and finally a newly constructed blast tube [32] in which a charge of plastic explosive (pentaerythritol tetranitrate PETN) was used. The system was composed of a cylindrical 400 mm wide and 565 mm long cast iron tube, with a cone shaped tip where the charge is placed. The wall thickness at the tip is 100 mm. At the other end, the iron tube is elongated to a total length by an extension tube of steel (wall thickness 10 mm). The open end of the extension tube was by a steel disc connected to a pendulum in Clemedson’s initial experiments. At the conical end of the tube, there is a threaded screw plug for the insertion of the charge that is mounted on the detonator. The charge is fixed at a distance of 100 mm from the inner tip. Clemedson and his coworkers published a number of studies on muscle tissue [33] as well as vascular and respiratory effects of blast in the rabbit [34]. After some time, this work was extended to include the central nervous system [35] and the cerebral vasculature [36]. The blast tube (without the pendulum door—which results in a more complex waveform) was modified for work with rodents by Anders Suneson. Annette Säljö used this system in her thesis work [37–39]. The ignition system was later changed to a non-electric ignition (NONEL from Nobel). The anesthetized rat is mounted in the blast tube at a distance of 1 m from the charge. The PETN generates a pulse with rapid raise time and very short duration (<0.3 ms). An increase in the charge has a direct and proportional effect on the peak pressure, but only a small effect on the duration. Secondary reflections are limited. By moving the object to the orifice of the tube (1.5 m from the charge) the peak pressure drops to about half, whereas the duration is increased somewhat. All rat experiments have been performed at the 1 m distance from the charge (Fig. 5), which has been varied from 0.5 to 5 g PETN (Spherical charges of Swedish army plastic explosive m/46, containing 86 % pentaerythritol tetranitrate PETN and mineral oil, where used. In the following text, the weights of the plastic explosive charges are given in gram). We have previously reported that the peak pressure during detonation of 2.5 g PETN would be 260 kPa and nearly 600 kPa with a 5 g charge. To get representative recordings of the peak pressure during a detonation of explosives is connected to substantial methodological difficulties due to the extreme requirement for good dynamics. Recent recordings with a set of open silicon piezoresistive sub-miniature pressure transducers (Entran Sensors & Electronics) indicate a peak pressure exceeding 10 bar during detonation of 5 g PETN, as recorded in front of a rat dummy at the 1 m position in the tube. A charge of 2.5 g in an unprotected animal (side-on at 1 m from the charge) results in about 50 % lethality and at 3 g the majority of the exposed animals die from pulmonary bleedings. On the other hand, the lethality is less than 10 % at 2 g PETN. In recent experiments we have used a full protection (rigid steel tube) of the body, except for the head and had no lethality with 5 g charges.
Fig. 5 Pictures showing the blast tube that was constructed by the Swedish scientist Clemedson in the 1950s. This system may be one of the oldest systems that still are in use. Previously published in [94]
In spite of the substantial lethality with this system (in unprotected animals), structural changes in the brain seem very limited or absent. The cell death in the brain that was reported by Säljö and coworkers [39], employing a similar protocol, has not been possible to verify. Instead, there is a significant cell death and gene expression changes [40, 41] in the inner ear. The hippocampus of the brain of rats exposed to a 2 g charge has been subjected to examination of the gene expression by use of Affymetrix Rat Gene Arrays. In such experiments, the expression of all known genes can be evaluated at the same time. It was found that about 100 genes had a significant expression change 24 h survival after the blast. The majority (76 genes) had a decrease in their expression whereas an increased expression was found in 39 genes [42]. Affected systems include synaptic transmission and neurogenesis. Both unprotected rats exposed to detonation of 2 g PETN and rats with the torso protected by a rigid steel tube during exposure to a 5 g blast have been examined. Taken together, the lack of structural damage combined with some functional changes indicates that the primary blast in this model generates a mild TBI. Future work with the blast tube will include repeated exposures and variations in body position. The blast tube in the current setting creates a very simple and short pulse that may imitate the situation at short distance with an open field charge. This pulse form is probably not at all similar to the situation in a protected vehicle that is hit by a road bomb. It should therefore be of interest to modify the length of the blast tube and introduce reflecting objects that could create a more complex pulse form. One aspect with this type of blast tube is the heat and gas emission that is a result of the use of explosives instead of compressed air. Thus, quaternary blast is added to the primary blast. Acceleration movements are however limited, by the montage of the animal, and impacts of flying objects do not occur. Secondary and tertiary blast is instead imitated and better controlled in other models.
-
5.
Breacher studies
“Breachers” are military or law enforcement personnel that are routinely exposed to low-level blast during training. Such repeated exposure has been associated with symptoms similar to that of sports concussion. The physical parameters of the blast exposure can be monitored during training in a much better way than in battle-field situations. This creates a situation that is similar to an experimental model and collection of samples, such as biomarkers [43], can therefore be compared to animal experiments for primary blast.
3 Models for Acceleration TBI
Although TBI can be associated with skull fractures, it commonly occurs without fractures [44]. About 40 % of all TBI patients admitted to hospitals are non-focal injuries [45] and are usually referred to as distributed brain injuries (DBI).
At least four categories of DBI can be identified: diffuse axonal injury (DAI) ; diffuse hypoxic, anoxic, or ischemic injury; diffuse swelling; and diffuse vascular injury. DAI is the most common type of DBI and commonly results in unconsciousness or death [44, 46]. The DAI pathology, which is characterized by perturbations to the axoplasmic transport along the length of axons [47], is likely to cause axonal swelling or degeneration which can reduce the functionality or disconnect the axons from their existing networks [48]. It has been reported that DAI commonly are localized in the subcortical white matter, grey–white matter interface and corpus callosum [44, 49], and at points of attachment, such as cranial nerves [50].
DBI is commonly a result of inertial induced loads; intracranial motions arise when the skull is accelerated and the brain mass, due to its inertia, lags behind or continues its motion relative to the skull. These inertia-induced loads are most common in rapid head rotations [51] which often occur in fall accidents, traffic accidents, and military assaults. Mechanical and mathematical models have been used to show that these inertia-induced loads produce strains in the brain tissue and that these strains cause the following neurological deficiencies [48, 52–58].
An attractive approach to study DBI pathology and its associated injury mechanism and threshold would be to reconstruct well-documented accident cases in which the patient is slightly injured. The real life accidents are however commonly rather complex, the injuries are regularly sever, and the patient suffers from a multitude of injuries. Therefore, anesthetized animals have been used in the past, and are in use, to study DBI and DAI .
The rotational weight drop model that [59] was developed by Marmarou and coworkers [60, 61] has generated very important data on development of diffuse brain injuries, including an improved understanding of diffuse axonal injury [47]. One of the advantages/disadvantages with this model is that it combines DAI with a contusion injury. Andersen [62] developed a model in which a stunner was used to accelerate the head. Both sever local brain damage and axonal injury was produced by this model. Both the forth-mentioned models have been found to be less useful for threshold studies on DAI and when DAI is to be studied separately.
Several models were developed in the past to study DAI using primates [44, 63], miniature swine [59], and rabbits [64, 65]. Few of these are in use today due to ethical considerations, or a lack of appropriate methods to assess the effects of the trauma, or due to excessive meningeal bleedings.
Models developed for rats provide several advantages over models using large animals. Ellingson et al. [66] and Fijalkowski et al. [67] exposed rats at low to medium severity rotational accelerations in the coronal plane. Despite the higher accelerations, the rats suffered from classical concussion injuries with minimal histological abnormalities.
3.1 A Rotational Acceleration Model
A rotational acceleration model aimed for studies into diffuse brain injuries and mTBI is described in detail by Davidsson [68]. It is designed to produce brain injuries by sagittal plane rearward rotational acceleration. This model allows for the production of graded injury and studies into injury thresholds.
In brief, the skull of an anesthetized adult Sprague–Dawley rat, weighing from 280 to 450 g, is tightly secured to a rotating bar. The bar is impacted by a striker that causes the bar and the animal head to rotate rearward; the acceleration phase lasts 0.4 ms and is followed by a rotation at constant speed and a gentle deceleration when the bar makes contact with a padded stop (Fig. 6). By adjusting the air pressure in the rifle used to accelerate the striker, rotational acceleration between 0.3 and 2.1 Mrad/s2 can be produced.
Diagrams. Top row: skull cap and attachments plate and oblique view of test device (crossbeam removed for visibility). Bottom row: oblique view of test device and side view of the head with central nervous system schematically depicted (screws and accelerometer not depicted) (Previously published in [94])
Numerous combinations of trauma levels, posttrauma survival times, brain and serum retrieval, and tissue preparation techniques were adopted to characterize this model. The trauma cause subdural bleedings in animals exposed to severe trauma although such hematoma can occasionally be found at rather low acceleration levels [69]. Staining brain tissue with amyloid precursor protein (APP) antibodies, which expose axons with reduced axioplasmic transport, revealed widespread axonal injuries (AI) in the frontal region of the corpus callosum, the upper and lower borders of the corpus callosum, and sometimes stretched into the caudate putamen. In the mid brain region APP-stained axons were found in the same regions as well as in the thalamus and hippocampus regions. Further, APP-stained axons were found in some of the tracts in the brain stem. Staining brain tissue with FD Neurosilver that detects degenerating axons confirmed the injury pattern [69]. For older subjects, those weighing on average 700 g, fewer positive axons appeared in the corpus callosum in animals while injured axons were found in clusters elsewhere: in the internal capsules, inside and in the vicinity of the anterior commissure, and in the structures between the lateral ventricles [70]. In addition to these areas, positive axons were spread out and frequent in structures close to the centerlines and the skull bases. The observed AI was apparent only when the rotational acceleration level was moderate (1.1 Mrad/s2) and above [71]. Older animals required higher accelerations to exhibit similar injury levels as younger animals [70]. Only limited signs of contusion injury were observed following trauma. Macrophage invasions, glial fibrillary acidic protein redistribution or hypertrophy, and blood–brain barrier (BBB) changes were unusual. S100B serum analyses indicate that blood vessel, axonal, and glial cell injuries occur following moderate level of trauma despite absence of obvious BBB injuries [72]. Affymetrix gene arrays showed changes in the expression in a large number of gene families including cell death, inflammation, and neurotransmitters in the hippocampus 24 h after moderate to severe trauma [42].
In conclusion, the signature injury with this rotational model is diffuse axonal injuries in the corpus callosum, subcortical white matter , and the brain stem. The absence of cell death and excessive bleedings indicate that this is a mild TBI and effects on behavior are indeed limited [72]. Thus, this model can add knowledge about mechanisms and thresholds for acceleration-induced mild TBI and such data can be relevant for the understanding of consequences of tertiary blast.
4 Models for Penetrating Ballistic TBI
A penetrating ballistic TBI occurs when objects impact the head and penetrate skin, skull and meninges and cause injury directly to the brain tissue . In contrast to closed head injury, penetrating ballistic TBI involves direct laceration of brain tissue, often complicated by secondary effects such as hemorrhage, edema, inflammation, and higher risk of coagulopathy [73]. The Vietnam head injury study has generated a lot of extremely valuable data on the long-term effects of penetrating TBI [74–76]. The Vietnam head injury study included baseline (pre-injury) data and a fairly homogenous group of patients (in terms of age and type of injury). Thus, interesting possibilities for translation emerge if this type of injury can be properly represented in experimental models.
A number of models have been developed to study penetrating ballistic TBI using cat [77], dog [78], monkey [79], and sheep [80]. None of these models are currently in routine use. To date, there are only two models in use and these both use rodents. In one of these a designed probe is inserted in the brain at the desired location and rapid inflation of an attached balloon is used to mimic the temporary cavity caused by energy dissipation from the bullet [81]. In the other model, a probe penetrates the brain at high velocity [82]. When shooting this probe into gel samples large temporary cavities are formed that are correlated to both speed of penetration and the shape of the penetrating object. The latter model will be presented in greater detail below.
4.1 Penetration TBI at High Velocity
A midline incision was made through the skin and periosteum of the anesthetized rat head, and a burr hole of 2.75 mm in diameter was drilled with its center slightly lateral and posterior to bregma. The rat was thereafter placed in a stereotactic frame and positioned so that a probe, commonly 2 mm in diameter with a spherical tip, was positioned directly above the dura exposed by the burr hole. This probe was fitted into a holder and guided by a narrow tube (Fig. 7). A lead pellet was accelerated by air pressure from a specially designed air rifle and impacted the probe. The probe penetrates 5–6 mm into the brain at high speed; 90 m/s at the time it starts to enter the brain.
The penetration rig (Previously published in [94])
The injury caused severe damage to the lateral and medial parietal cortecies, corpus callosum, hippocampus, and several parts of the posterior thalamus [82]. After a few days after trauma, a large cavity was formed in the brain. The penetration trauma also causes hemorrhages, blood–brain barrier breakdown, neurodegenerations , gliosis, transient changes in several behavior tests, and persistent deficiency of reference memory. There are significant changes in gene expression, both in the cerebral cortex that surrounds the penetration and in the hippocampus [42] and leakage of S-100B into serum [83]. The inflammatory response in the cortex includes an activation of the terminal pathway of the complement system [84]. This model has also been used to characterize changes in BDNF and neurotrophin receptors after penetrating injury [85] in order to provide a correlate to data on the importance of BDNF gene polymorphism for the outcome of penetrating TBI in the Vietnam Head Injury study [86].
5 Concluding Remarks
Far to many experimental studies end up with data that cannot be translated into clinical work. Translation can fail if the models are not properly validated and provide a good representation of the clinical injury they are supposed to model. Translation can also be impeded by large differences in the methods for outcome measure [87]. In order to facilitate the translation of experimental data, it may be important to include outcome recordings that could be used also in clinical work, such as serological biomarkers and MRI [88]. One additional strategy is to develop and use Finite Element Models of the animal and the model that is used to load the animal during the experiment. One model for the rat head has recently been employed to model rotational acceleration injury [89]. Such work can enable scaling and comparison with human clinical cases of TBI [56, 90, 91]. The choice of the animal species or strain can obviously have a significant impact on the outcome of the injury. Differences in body size and the geometry of the skull can be assumed to represent critical factors in experimental design. For example, experiments with rotational acceleration are very dependent on the distance to the axis of rotation, thus a larger brain may be far less resistant to rotational injury. Different rat strains may exhibit different inflammatory responses and reactions to TBI.
Validated and verified experimental models are necessary for successful identification of new drug candidates for treatment of TBI or SCI [92]. Differences in time scales between experimental animals, such as rodents, and humans are difficult to represent and compensate for in experimental work [93].
References
Ramón y Cajal S (1928) Degeneration and regeneration of the nervous system. In: DeFelipe J, Jones EG (eds) History of neuroscience, vol 5. Oxford University Press, New York, Reprinted 1991 ed
Richardson PM, McGuinness UM, Aguayo AJ (1980) Axons from CNS neurons regenerate into PNS grafts. Nature 284:264–265
Risling M, Cullheim S, Hildebrand C (1983) Reinnervation of the ventral root L7 from ventral horn neurons following intramedullary axotomy in adult cats. Brain Res 280(1):15–23
Lindå H, Risling M, Cullheim S (1985) ‘Dendraxons’ in regenerating motoneurons in the cat: do dendrites generate new axons after central axotomy? Brain Res 358(1-2):329–333
Lindå H, Cullheim S, Risling M (1992) A light and electron microscopic study of intracellularly HRP-labeled lumbar motoneurons after intramedullary axotomy in the adult cat. J Comp Neurol 318(2):188–208
Risling M, Linda H, Cullheim S, Franson P (1989) A persistent defect in the blood-brain barrier after ventral funiculus lesion in adult cats: implications for CNS regeneration? Brain Res 494(1):13–21
Risling M, Fried K, Lindå H, Cullheim S, Meier M (1992) Changes in nerve growth factor receptor-like immunoreactivity in the spinal cord after ventral funiculus lesion in adult cats. J Neurocytol 21(2):79–93
Frisén J, Verge VM, Cullheim S, Persson H, Fried K, Middlemas DS, Hunter T, Hokfelt T, Risling M (1992) Increased levels of trkB mRNA and trkB protein-like immunoreactivity in the injured rat and cat spinal cord. Proc Natl Acad Sci U S A 89(23):11282–11286
Frisén J, Risling M, Korhonen L, Zirrgiebel U, Johansson CB, Cullheim S, Lindholm D (1998) Nerve growth factor induces process formation in meningeal cells: implications for scar formation in the injured CNS. J Neurosci 18(15):5714–5722
Risling M, Fried K, Lindå H, Carlstedt T, Cullheim S (1993) Regrowth of motor axons following spinal cord lesions: distribution of laminin and collagen in the CNS scar tissue. Brain Res Bull 30(3-4):405–414
Deckner M, Lindholm T, Cullheim S, Risling M (2000) Differential expression of tenascin-C, tenascin-R, tenascin/J1, and tenascin-X in spinal cord scar tissue and in the olfactory system. Exp Neurol 166(2):350–362
Carlstedt T, Linda H, Cullheim S, Risling M (1986) Reinnervation of hind limb muscles after ventral root avulsion and implantation in the lumbar spinal cord of the adult rat. Acta Physiol Scand 128(4):645–646
Carlstedt T, Grane P, Hallin RG, Noren G (1995) Return of function after spinal cord implantation of avulsed spinal nerve roots. Lancet 346(8986):1323–1325
Carlstedt T, Hultgren T, Nyman T, Hansson T (2009) Cortical activity and hand function restoration in a patient after spinal cord surgery. Nat Rev Neurol 5(10):571–574
Cullheim S, Carlstedt T, Linda H, Risling M, Ulfhake B (1989) Motoneurons reinnervate skeletal muscle after ventral root implantation into the spinal cord of the cat. Neuroscience 29(3):725–733
Risling M, Ochsman T, Carlstedt T, Linda H, Plantman S, Rostami E, Angeria M, Skold MK (2011) On acute gene expression changes after ventral root replantation. Front Neurol 1:159
Chew DJ, Carlstedt T, Shortland PJ (2011) A comparative histological analysis of two models of nerve root avulsion injury in the adult rat. Neuropathol Appl Neurobiol 37(6):613–632
Chew DJ, Murrell K, Carlstedt T, Shortland PJ (2013) Segmental spinal root avulsion in the adult rat: a model to study avulsion injury pain. J Neurotrauma 30(3):160–172
Armonda RA, Bell RS, Vo AH, Ling G, DeGraba TJ, Crandall B, Ecklund J, Campbell WW (2006) Wartime traumatic cerebral vasospasm: recent review of combat casualties. Neurosurgery 59(6):1215–1225, discussion 1225
White CS, IG Bowen, Richmond DR (1965) Biological tolerance to air blast and related biomedical criteria. CEX-65.4. CEX [reports]; civil effects exercise. U.S. Atomic Energy Commission, 1–239
Richmond DR, Damon EG, Bowen IG, Fletcher ER, White CS (1967) Air-blast studies with eight species of mammals. Techn Progr Rep DASA 1854. Fission product inhalation project [technical progress report]. Lovelace Foundation for Medical Education and Research, 1–44
Richmond DR, Damon EG, Fletcher ER, Bowen IG, White CS (1967) The relationship between selected blast-wave parameters and the response of mammals exposed to air blast. Techn Progr Rep DASA 1860. Fission product inhalation project [technical progress report]. Lovelace Foundation for Medical Education and Research, 1–36
Rubovitch V, Ten-Bosch M, Zohar O, Harrison CR, Tempel-Brami C, Stein E, Hoffer BJ, Balaban CD, Schreiber S, Chiu WT, Pick CG (2011) A mouse model of blast-induced mild traumatic brain injury. Exp Neurol 232(2):280–289
Lu J, Ng KC, Ling GS, Wu J, Poon JF, Kan EM, Tan MH, Wu YJ, Li P, Moochhala S, Yap E, Lee LK, Teo AL, Yeh IB, Sergio DM, Chua F, Kumar SD, Ling EA (2012) Effect of blast exposure on the brain structure and cognition in the Macaca fascicularis. J Neurotrauma 29:1434
Celander H, Clemedson CJ, Ericsson UA, Hultman HI (1955) The use of a compressed air operated shock tube for physiological blast research. Acta Physiol Scand 33(1):6–13
Long JB, Bentley TL, Wessner KA, Cerone C, Sweeney S, Bauman RA (2009) Blast overpressure in rats: recreating a battlefield injury in the laboratory. J Neurotrauma 26(6):827–840
Bolander R, Mathie B, Bir C, Ritzel D, VandeVord P (2011) Skull flexure as a contributing factor in the mechanism of injury in the rat when exposed to a shock wave. Ann Biomed Eng 39(10):2550–2559
Chavko M, Koller WA, Prusaczyk WK, McCarron RM (2007) Measurement of blast wave by a miniature fiber optic pressure transducer in the rat brain. J Neurosci Methods 159(2):277–281
Chavko M, Watanabe T, Adeeb S, Lankasky J, Ahlers ST, McCarron RM (2011) Relationship between orientation to a blast and pressure wave propagation inside the rat brain. J Neurosci Methods 195(1):61–66
Cernak I, Merkle AC, Koliatsos VE, Bilik JM, Luong QT, Mahota TM, Xu L, Slack N, Windle D, Ahmed FA (2011) The pathobiology of blast injuries and blast-induced neurotrauma as identified using a new experimental model of injury in mice. Neurobiol Dis 41(2):538–551
Clemedson CJ (1949) An experimental study on air blast injuries. Acta Physiol Scand 18(Suppl LXI):7
Clemedson CJ, Criborn CO (1955) A detonation chamber for physiological blast research. J Aviat Med 26(5):373–381
Clemedson CJ, Jonsson A, Pettersson H (1956) Propagation of an air-transmitted shock wave in muscular tissue. Nature 177(4504):380–381
Clemedson CJ, Hultman H (1958) Cardiac output in early phase of blast injury in rabbits. Am J Physiol 194(3):601–606
Clemedson CJ (1956) Shock wave transmission to the central nervous system. Acta Physiol Scand 37(2-3):204–214
Clemedson CJ, Hartelius H, Holmberg G (1957) The effect of high explosive blast on the cerebral vascular permeability. Acta Pathol Microbiol Scand 40(2):89–95
Säljo A, Bao F, Haglid KG, Hansson HA (2000) Blast exposure causes redistribution of phosphorylated neurofilament subunits in neurons of the adult rat brain. J Neurotrauma 17(8):719–726
Säljö A, Bao F, Hamberger A, Haglid KG, Hansson HA (2001) Exposure to short-lasting impulse noise causes microglial and astroglial cell activation in the adult rat brain. Pathophysiology 8(2):105–111
Säljö A, Bao F, Jingshan S, Hamberger A, Hansson HA, Haglid KG (2002) Exposure to short-lasting impulse noise causes neuronal c-Jun expression and induction of apoptosis in the adult rat brain. J Neurotrauma 19(8):985–991
Kirkegaard M, Murai N, Risling M, Suneson A, Jarlebark L, Ulfendahl M (2006) Differential gene expression in the rat cochlea after exposure to impulse noise. Neuroscience 142(2):425–435
Murai N, Kirkegaard M, Jarlebark L, Risling M, Suneson A, Ulfendahl M (2008) Activation of JNK in the inner ear following impulse noise exposure. J Neurotrauma 25(1):72–77
Risling M, Plantman S, Angeria M, Rostami E, Bellander BM, Kirkegaard M, Arborelius U, Davidsson J (2011) Mechanisms of blast induced brain injuries, experimental studies in rats. Neuroimage 54(Suppl 1):S89–S97
Tate CM, Wang KK, Eonta S, Zhang Y, Carr W, Tortella FC, Hayes RL, Kamimori GH (2013) Serum brain biomarker level, neurocognitive performance, and self-reported symptom changes in soldiers repeatedly exposed to low-level blast: a breacher pilot study. J Neurotrauma 30(19):1620–1630
Gennarelli TA, Thibault LE, Adams JH, Graham DI, Thompson CJ, Marcincin RP (1982) Diffuse axonal injury and traumatic coma in the primate. Ann Neurol 12(6):564–574
Wismans J, Janssen E, Beusenberg M, Bovendeerd P (2000) Injury bio-mechanics. Course book. Eindhoven Technical University
Melvin J, Lighthall WJ, Ueno K (1993) Accidental injury, biomechanics and prevention. Springer, New York, NY
Povlishock JT, Jenkins LW (1995) Are the pathobiological changes evoked by traumatic brain injury immediate and irreversible? Brain Pathol 5(4):415–426
Povlishock JT (1992) Traumatically induced axonal injury: pathogenesis and pathobiological implications. Brain Pathol 2(1):1–12
Smith DH, Meaney DF (2000) Axonal damage in traumatic brain injury. Neuroscientist 6(6):483–495
Viano DC (197) Brain injury biomechanics in closed-head impact: studies on injury epidemiology, tolerance criteria, biomechanics, and traffic injury prevention, Karolinska institutet
Holbourn AHS (1943) The mechanics of head injuries. Lancet ii:438–441
Adams JH, Doyle D, Ford I, Gennarelli TA, Graham DI, McLellan DR (1989) Diffuse axonal injury in head injury: definition, diagnosis and grading. Histopathology 15(1):49–59
Margulies SS, Thibault LE, Gennarelli TA (1990) Physical model simulations of brain injury in the primate. J Biomech 23(8):823–836
Margulies SS, Thibault LE (1992) A proposed tolerance criterion for diffuse axonal injury in man. J Biomech 25(8):917–923
Zhang L, Yang KH, King AI (2004) A proposed injury threshold for mild traumatic brain injury. J Biomech Eng 126(2):226–236
Kleiven S (2007) Predictors for traumatic brain injuries evaluated through accident reconstructions. Stapp Car Crash J 51:81–114
Antona-Makoshi J, Davidsson J, Ejima S, Ono K, Brolin K, Anata K (2013) Correlation of global head and brain tissue injury criteria to experimental concussion derived from monkey head trauma experiments. Proceeding of the 2013 International IRCOBI Conference on the Biomechanics of Impact
Strich SJ (1961) Shearing of nerve fibres as a cause of brain damage due to head injury. A pathological study of twenty cases. Lancet ii:443–448
Ross DT, Meaney DF, Sabol MK, Smith DH, Gennarelli TA (1994) Distribution of forebrain diffuse axonal injury following inertial closed head injury in miniature swine. Exp Neurol 126(2):291–299
Marmarou A, Foda MA, van den Brink W, Campbell J, Kita H, Demetriadou K (1994) A new model of diffuse brain injury in rats. Part I: Pathophysiology and biomechanics. J Neurosurg 80(2):291–300
Foda MA, Marmarou A (1994) A new model of diffuse brain injury in rats. Part II: Morphological characterization. J Neurosurg 80(2):301–313
Andersson RWG (2000) A study on the biomechanics of axonal injury, in University of Adelaide
Ono K, Kikuchi A, Nakamura M, Kobayashi H, Nakamura N (1980) Human head tolerance to sagittal impact reliable estimation deduced from experimental head injury using subhuman primates and human cadaver skulls. Proc. of the 24th Stapp Car Crash Conf., 101–160
Runnerstam M, Bao F, Huang Y, Shi J, Gutierrez E, Hamberger A, Hansson HA, Viano D, Haglid K (2001) A new model for diffuse brain injury by rotational acceleration: II. Effects on extracellular glutamate, intracranial pressure, and neuronal apoptosis. J Neurotrauma 18(3):259–273
Gutierrez E, Huang Y, Haglid K, Bao F, Hansson HA, Hamberger A, Viano D (2001) A new model for diffuse brain injury by rotational acceleration: I model, gross appearance, and astrocytosis. J Neurotrauma 18(3):247–257
Ellingson BM, Fijalkowski RJ, Pintar FA, Yoganandan N, Gennarelli TA (2005) New mechanism for inducing closed head injury in the rat. Biomed Sci Instrum 41:86–91
Fijalkowski RJ, Stemper BD, Pintar FA, Yoganandan N, Crowe MJ, Gennarelli TA (2007) New rat model for diffuse brain injury using coronal plane angular acceleration. J Neurotrauma 24(8):1387–1398
Davidsson J (2008) A new model, experiments and injury threshold for sagittal plane rotational induced diffuse brain injuries in 6th Frame work EU-project APROSYS2008
Davidsson J, Risling M (2011) A new model to produce sagittal plane rotational induced diffuse axonal injuries. Front Neurol 2(41):1–11
Davidsson J, Angeria M, Risling M (2013) Effect of age on amount and distribution of diffuse axonal injury after rotational trauma. Proceeding of JSAE Annual Congress, Yokohama, Japan, May 22–24, 2013
Davidsson J, Angeria M, Risling M (2009) Injury threshold for sagittal plane rotational induced diffuse axonal injuries. International IRCOBI conference on the biomechanics of injury. York, UK: IRCOBI Conference
Rostami E, Davidsson J, Ng KC, Lu J, Gyorgy A, Walker J, Wingo D, Plantman S, Bellander BM, Agoston DV, Risling M (2012) A model for mild traumatic brain injury that induces limited transient memory impairment and increased levels of axon related serum biomarkers. Front Neurol 3:115
Talving P, Benfield R, Hadjizacharia P, Inaba K, Chan LS, Demetriades D (2009) Coagulopathy in severe traumatic brain injury: a prospective study. J Trauma 66(1):55–61, discussion 61-2
Raymont V, Salazar AM, Krueger F, Grafman J (2011) “Studying injured minds” - the Vietnam head injury study and 40 years of brain injury research. Front Neurol 2:15
Grafman J, Schwab K, Warden D, Pridgen A, Brown HR, Salazar AM (1996) Frontal lobe injuries, violence, and aggression: a report of the Vietnam Head Injury Study. Neurology 46(5):1231–1238
Salazar AM, Schwab K, Grafman JH (1995) Penetrating injuries in the Vietnam war. Traumatic unconsciousness, epilepsy, and psychosocial outcome. Neurosurg Clin N Am 6(4):715–726
Carey ME, Sarna GS, Farrell JB, Happel LT (1989) Experimental missile wound to the brain. J Neurosurg 71(5 Pt 1):754–764
Tan Y, Zhou S, Liu Y, Li Z (1998) A gross and microscopic study of cerebral injuries accompanying maxillofacial high-velocity projectile wounding in dogs. J Oral Maxillofac Surg 56(3):345–348
Crockard HA, Brown FD, Johns LM, Mullan S (1977) An experimental cerebral missile injury model in primates. J Neurosurg 46(6):776–783
Finnie JW (1993) Pathology of experimental traumatic craniocerebral missile injury. J Comp Pathol 108(1):93–101
Williams AJ, Hartings JA, Lu XC, Rolli ML, Dave JR, Tortella FC (2005) Characterization of a new rat model of penetrating ballistic brain injury. J Neurotrauma 22(2):313–331
Plantman S, Ng KC, Lu J, Davidsson J, Risling M (2012) Characterization of a novel rat model of penetrating traumatic brain injury. J Neurotrauma 29(6):1219–1232
Risling M, Sköld M, Larsson IL, Angeria M, Davidsson J (2004) Leakage of S-100 protein after high velocity penetration injury to the brain. 7th international neurotrauma symposium. Adelaide: Medimond
Rostami E, Davidsson J, Gyorgy A, Agoston DV, Risling M, Bellander BM (2013) The terminal pathway of the complement system is activated in focal penetrating but not in mild diffuse traumatic brain injury. J Neurotrauma 30(23):1954–1965
Rostami E, Krueger F, Plantman S, Davidsson J, Agoston D, Grafman J, Risling M (2014) Alteration in BDNF and its receptors, full-length and truncated TrkB and p75(NTR) following penetrating traumatic brain injury. Brain Res 1542:195–205
Rostami E, Krueger F, Zoubak S, Dal Monte O, Raymont V, Pardini M, Hodgkinson CA, Goldman D, Risling M, Grafman J (2011) BDNF polymorphism predicts general intelligence after penetrating traumatic brain injury. PLoS One 6(11):e27389
Agoston DV, Risling M, Bellander BM (2012) Bench-to-bedside and bedside back to the bench; coordinating clinical and experimental traumatic brain injury studies. Front Neurol 3:3
Kamnaksh A, Budde MD, Kovesdi E, Long JB, Frank JA, Agoston DV (2014) Diffusion tensor imaging reveals acute subcortical changes after mild blast-induced traumatic brain injury. Sci Rep 4:4809
Antona-Makoshi J, Davidsson J, Risling M, Ejima S, Ono K (2014) Validation of local brain kinematics of a novel rat brain finite element model under rotational acceleration. Int J Automot Eng 5:31–37
Kleiven S, Hardy WN (2002) Correlation of an FE model of the human head with local brain motion--consequences for injury prediction. Stapp Car Crash J 46:123–144
Kleiven S (2013) Why most traumatic brain injuries are not caused by linear acceleration but skull fractures are. Front Bioeng Biotechnol 1:15
Agoston DV, Risling M (2012) Where will the (new) drugs for traumatic brain injury treatment be coming from? Front Neurol 3:27
Agoston DV (2013) Of timescales, animal models, and human disease: the 50th anniversary of C. elegans as a biological model. Front Neurol 4:129
Risling M, Davidsson J (2012) Experimental animal models for studies on the mechanisms of blast induced neurotrauma. Front Neurol 3(30):1–9
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this protocol
Cite this protocol
Davidsson, J., Risling, M. (2016). Experimental Models for Neurotrauma Research. In: Kobeissy, F., Dixon, C., Hayes, R., Mondello, S. (eds) Injury Models of the Central Nervous System. Methods in Molecular Biology, vol 1462. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-3816-2_16
Download citation
DOI: https://doi.org/10.1007/978-1-4939-3816-2_16
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-3814-8
Online ISBN: 978-1-4939-3816-2
eBook Packages: Springer Protocols