Abstract
Microbiologically induced corrosion plays a key role in implanted materials survival, especially those exposed to the oral environment. Despite considerable progress in this field, a consensus is still missing due to contradictory findings regarding the role of oral biofilms in the electrochemical behavior of titanium (Ti) implant surfaces. This scoping review comprehensively reviews and discusses the current evidence and new perspectives on microbial corrosion. The main focus is understanding oral biofilm formation and its synergistic effect under the corrosion/tribocorrosion phenomenon. We critically revisited the literature to refine key concepts and mechanisms involved in polymicrobial biofilm formation on implant devices, microbial corrosion phenomenon, and its consequence for surrounding tissues. To summarize what is currently known about this topic, we have conducted a scoping review. Data of eligible in vitro studies suggest that oral biofilm and bacterial metabolites products can affect negatively the electrochemical behavior of Ti material and promote implant surface deterioration. Relevant experimental strategies to practically approach the field of microbial corrosion mechanisms are outlined. Finally, new approaches to enhance biomaterial development should consider improved corrosion resistance to promote higher implant survival.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
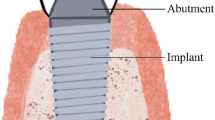
Dental implants are some of the most successful implantable devices with long-term predictability and clinical performance [1]. Titanium (Ti) has been a commonly employed material used for dental implants with high success rates (90.9% to 97.7%) after 15 years of post-implantation [2, 3]. The success of these Ti-based implants is mainly due to a combination of suitable biomaterial properties and the ability to spontaneously form a passive titanium oxide layer when in contact with atmosphere O2 (named as TiO2) [4, 5]. However, albeit TiO2 film protects the metal surface against oxidative degradation processes from biological fluids [6], dental implants are inserted in a challenging and humid environment in which they are constantly exposed to corrosion and microbial colonization starting from the moment of the implantation and lasting for the entire implant lifetime [7]. Consequently, implant failures can be induced by several individuals or synergistic events related to the mechanical, chemical, biological, and microbiologically induced degradation processes [8].
Polymicrobial biofilm formation on the Ti surface is the primary etiologic factor in the etiopathogenesis of implant-related infections [9, 10]. Since the implantation, dental implants, like all oral surfaces, are a substrate for microbial adhesion and accumulation [11]. Therefore, polymicrobial infection induced by biofilms is the main reason for dental implant failures [10], as oral biofilms can mitigate the electrochemical stability of implanted material, leading to faster corrosion processes and deterioration [12]. Some studies have hypothesized that biofilm-covered implant surfaces undergo accelerated corrosion due to an acidic environment generated by bacterial cell metabolism and products released [12,13,14,15]. The microbiologically induced corrosion—as this deleterious phenomenon is called—promotes surface deterioration, including discoloration, pitting, cracking, scratches, and an increase of surface roughness [2]. Microbial corrosion results in the release of metallic ions or even particles (when associated with the fretting process) into the surrounding tissues that can stimulate an exacerbated inflammatory response, peri-implant bone reabsorption [16], and microbiological dysbiosis [17]. Ex vivo studies [18, 19] proved that the dissemination of Ti wear debris in the peri-implant tissues is strongly associated with implant device failure. Therefore, microbial corrosion has been considered a key issue on whether the implant will survive or fail.
Facing the boost growth in the implant market and patients seeking Ti-based implants for oral rehabilitation (https://www.grandviewresearch.com/industry-analysis/dental-implants-market), microbial corrosion concerns might increase. Here, we attempt to summarize what is currently known on this topic, identify gaps, refine key concepts, mechanisms involved, and report the types of evidence that guide practice in the field. For this, we conducted a scoping review to evaluate the main experimental findings in terms of the corrosion/tribocorrosion process, considering the synergistic interactions of oral biofilms with the Ti surface. This review gathers knowledge from materials sciences, microbiology, and dentistry, contributing to a better understanding of microbial corrosion phenomenon and points the way forward towards the rational design of safer and enhanced dental implant surfaces.
2 Oral Biofilms: A Powerful Microbiologically Influenced Corrosion Force
In the oral environment, indigenous microorganisms from the oral microbiome live in a symbiotic state with the host by adhering to any biotic [20] or abiotic surfaces [21] present in this environment. Microbial accumulation and biofilm formation on implanted materials can trigger different biological and chemical processes, such as polymicrobial infections [22] and material deterioration [14, 15]. Microbiologically induced corrosion has been defined and widely accepted as corrosion damage initiated or aggravated due to the direct or indirect activities of microorganisms colonizing materials surfaces [23]. The impact of biofilms on the TiO2 layer breakdown depends on the synergic effect of microenvironmental conditions and microbial activity [8]. Previously, research investigating the failed dental implants caused by Ti corrosion raises the possibility of oral bacteria having a relative contribution to this purpose [24]. Thus, it has to be emphasized that the role of oral microorganisms in the corrosion process is complex in that they can either accelerate corrosion or induce corrosion alone (i.e., microbiologically induced corrosion), and the latter is the central topic of this review and will be discussed in detail.
2.1 Biofilm Development on Implant Surfaces
It is essential to know the biofilm formation process to understand the unique effect of surface-attached biofilms in terms of the corrosion phenomenon. Theoretically, the main stages of oral biofilm formation may include the following: protein adsorption, microbial adhesion, followed by co-aggregation processes, biofilm formation, maturation, and dispersal [11, 25]. The temporal sequence of in vitro polymicrobial biofilm development on the Ti surface can be visualized in Fig. 1.
The temporal sequence of in vitro polymicrobial biofilm development on titanium surface using scanning electron microscopy images (15 kV, 1000 × magnification). To mimic the dental implant material, machined titanium samples were used as a substrate for biofilm formation from human saliva. After 2 h of in vitro bacterial incubation, it is possible to see bacteria (cocci species) attachment on the surface, representing the early-colonizer bacteria. After 24 h, polymicrobial biofilm with higher biovolume and complex 3D structure due to extracellular biofilm matrix can also be observed. These micrographs suggest that biofilm growth changes the microenvironment on the titanium surface and leads to biofilm maturation (48 h). Reprinted (adapted) from Costa et al. [5], Copyright (2020), with permission from Elsevier (license number 5078840308928)
Immediately after implant insertion in the oral cavity, Ti material is rapidly exposed to protein-rich fluids, such as saliva or blood plasma, forming a protein layer on the Ti surface [11]. In this way, protein adsorption represents the first biological response in the human body to implanted materials [26]. Typically, the serum protein layer formed by blood plasma comprises fibronectin, serum albumin, apolipoprotein, and fibrinogen, facilitating the biological interactions between the material and host cellular response [27, 28]. On the other hand, salivary pellicle composition mainly includes organic and inorganic components, such as aminoacids, proteins, glycoproteins, carbohydrates, lipids and sodium, chloride, calcium, phosphate, and bicarbonate, respectively, which could prevent corrosion of Ti material by a buffering mechanism [8]. However, the buffering mechanism can be limited considering the high density of bacterial cells or a low salivary flow rate [29]. Moreover, in the long term, several salivary proteins show a remarkable specificity in their ability to promote the adhesion of some prominent oral bacteria to these surfaces, which can favor bacterial colonization [30]. Another theory is that protein layers could protect surfaces against wear due to the viscoelastic and lubricating effect on the Ti and counterbody surfaces [31]. In fact, previous studies have shown lower friction and wear of Ti surfaces in the presence of whole human saliva [32], mucin [29], and albumin [33].
Bacteria–surface interactions can occur in different ways, including electrostatic forces, hydrogen bonding, and Van der Waals forces [34]. After initial saliva or blood plasma coating, followed by bacterial adhesion, interactions among different species known as a co-aggregation drive towards a highly organized microbial accumulation and biofilm formation [35]. For instance, Streptococcus and Actinomyces spp. are considered primary colonizers, binding to salivary agglutinins and proline-rich proteins, and capable of providing additional sites for late colonizers adhesion, such as Aggregatibacter actinomycetemcomitans, Porphyromonas gingivalis, and Fusobacterium nucleatum, favoring biofilm development and increased pathogenicity over time [22, 36]. Conceptually, oral biofilms are complex and highly organized polymicrobial communities embedded in a self-produced extracellular matrix [37, 38]. Extracellular polymeric substances (EPS) in the biofilm matrix are responsible for the three-dimensional biofilm architecture [38]. They provide a unique environment, improve microbial adhesion, nutrient richness, and create an acidic microenvironment [38]. In addition, EPS diminishes the mechanical biofilm removal [25] and reduces biofilm susceptibility to antimicrobials drugs [39] on Ti surfaces. Figure 2 shows a schematic illustration of biofilm formation on dental implants and their effect under clinical progression of implant-related diseases.
Schematic representation for the steps of biofilm formation on titanium biomaterial. The schematic drawing depicts the five main steps for forming and spreading biofilms such as protein adsorption, microbial adhesion, biofilm formation, maturation, and dispersal. The clinical disease progression is dependent on biofilm accumulation (created with BioRender.com; License number: KL22UL22JY)
From a clinical standpoint, the microbial colonization of dental implants begins at supragingival area exposed to the oral environment, and initial biofilm formation depends on the surface properties, implant topography, oral microbiota, and environmental conditions, such as pH, oxygen level, fermentable carbohydrate exposed, and poor oral hygiene [40]. An area of particular interest is the implant–abutment connection region, in which microgaps (2.5–60 μm) can compromise the sealing performance, favoring the penetration of bacteria and microbial colonization of the inner threads of the implants [41, 42]. Interestingly, once inside the implant–abutment connections, biofilm can act as lubricants, decreasing friction between contacting prosthetic surfaces [43]. Such protection is attributed to the viscoelastic property of microbial cells provided by the presence of polysaccharides, proteins, phospholipids, and nucleic acids [44]. Notably, a loss of mechanical integrity of dental implant internal connections may occur due to the decrease in friction caused by biofilm formation, leading to screw loosening and other prosthetic complications [12]. Oppositely, biofilms can also detach from the surface as shear stress increases and no longer provide the protective lubricating effect on the surface [45]. Another relevant point is that corroded Ti surfaces may promote increased bacterial attachment and higher biofilm biovolume because of surface deterioration and increased roughness [46]. Thus, corroded implant surfaces can promote bacterial recolonization, impair regeneration procedures, and reduce the ability of host cells to reattach and proliferate [47].
2.2 Microbial Corrosion Mechanisms
Oral biofilms are assumed to change the implant's electrochemical environment, leading to disruption of the TiO2 layer [48]. This is hypothesized based on two main mechanisms: (1) bacteria can significantly reduce the peri-implant microenvironment pH by producing organic acids during fermentable carbohydrate catabolism [49]. This low pH creates a favorable environment for pitting attacks [13]. (2) Microbial accumulation on the dental implant can promote differential oxygen exposure on the Ti surface [23]. As a result, the less aerated zones act as the anode and undergo crevice corrosion, thereby mitigating the reformation of the oxide layer [14]. Both unfavorable conditions initiate metal dissolution and surface deterioration [15], as shown in Fig. 3.
In vitro microbial corrosion in titanium dental implants with sandblasted and acid-etched (SLA) surface after immersion in bacterial polyculture. In this panel it is possible to see the A–E whole-view of implant samples (× 20), B–F smooth collar (× 300), C–G collar–screw junction (× 500), and D–H implant screw (× 700). Black and red arrows indicate surface discoloration/pitting attack and crevice corrosion features, respectively. Apparently, the type of bacteria/growth conditions may modulate the surface damage. The black bars correspond to a length of 2000 μm and green bars to 100 μm. Reprinted from Siddiqui et al. [15], Copyright (2021), with permission from John Wiley and Sons (license number 5079500517450) (Color figure online)
As the biofilms develop, oral bacteria produce and release various corrosive agents such as lactic acid, methyl mercaptan, hydrogen sulfide, and dimethyl sulfide [50, 51]. In addition, it is well documented that several modulatory factors related to saliva can accelerate the metal electrochemical degradation by acidification around the implant, as follows: fluoride concentration [52], mouthwashes [53], teeth bleaching agents [54], chronic diseases, and medications [55]. Moreover, hydrogen peroxide (H2O2) synthesis during the peri-implant inflammation process negatively affects Ti corrosion resistance [51].
The biofilm composition is influenced by the local pH values and environmental conditions, considering the release and tolerance of bacteria to acids, nutritional factors, and how aerobic or anaerobic the microenvironment is [56, 57]. Among the several bacteria present in the oral cavity, Streptococcus mutans is a powerful corrosive microorganism because of its capacity to release lactic acid and grow in acidic environments [48]. Although S. mutans is not directly responsible for implant-related infections [58], this key pathogen promotes quick co-aggregation with periodontopathogens bacteria due to reduced oxygen content related to the biofilm accumulation and EPS formation [20]. Some studies have also appointed the role of bacterial components of periodontopathogens such as lipopolysaccharide (LPS) [59], dextrose [60], and sulfides [61] to change the Ti electrochemical behavior. Indeed, the biofilm structure can pick up external acidic substances from diet, caffeine, cotinine, or nicotine [62], as well as acidic substances produced from microbial metabolism [63]. Interestingly, although S. mutans has a high ability to produce acids, we have shown that S. mutans in vitro biofilms exposed to higher carbohydrate (sucrose) concentration did not affect the electrochemical behavior of Ti, which may be explained by the short time that the surface was exposed to the biofilm, knowing microbial corrosion is a chronic process a long-term acidic exposure might be needed for microbiologically induced corrosion [21].
The biofilm-covered implant surface is a cathodic area, and the exposed Ti is an anodic area, which forms galvanic corrosion [49]. In other words, these anodic and cathodic regions are produced by converting the biofilm-covered implant surface into an electrode, which increases the corrosion rate due to the high chemical reactivity of the Ti material [20]. Therefore, the Ti oxidation reaction can be summarized as follows:
-
(1)
TiO2 + H2O + H+ = Ti(OH)3+ (exposed surface)
-
(2)
4H+ + O2 + 4e = 2H2O (cathode region)
-
(3)
Ti + H2O = TiO2+ + 2H+ + 4e (anode region)
Consequently, this electrochemical reaction promotes pitting-like features, peaks, and valleys on the surface, releasing corrosion products into the surrounding tissues [63]. Interestingly, a previous ex vivo study [24] has suggested that aerobic bacteria could induce microbial corrosion primarily concentrated in the pits. In contrast, anaerobic bacteria are associated with crevicular corrosion due to decreased oxygen levels in the microenvironment. Furthermore, a unique pattern of surface discoloration also appears to be associated with the microbial profile [15]. However, the role of specific bacterial species in the microbial corrosion of Ti and how different factors affecting biofilm growth can also change this electrochemical behavior needs to be further evaluated. Overall, the microbial corrosion mechanisms are illustrated in Fig. 4.
Representative proposed mechanisms of microbial corrosion in titanium-based dental implants. 1 Titanium material in contact with biological fluids leads to passive TiO2 layer formation and, subsequently, bacterial adhesion on the surface. 2 Biofilm formation promotes a drop in the pH (acidification) of the microenvironment around the implant due to bacterial metabolism. 3 The exposed titanium surface is susceptible to material corrosion trigger by human saliva (biological electrolyte). 4 The biofilm-covered implant surface is a cathodic area, and the exposed titanium is an anodic area. 5 Several modulator factors may also accelerate the corrosion process. 6 Finally, the TiO2 breakdown reactions with the environment induce titanium particles/ions release and corrosion products accumulation (created with BioRender.com; License number: YE22UL1A3B)
3 Titanium Corrosion Products and Peri-implant Diseases: An Overview
Microbial corrosion may induce accelerated, and localized Ti dissolution, contributing to the burden of particles released surrounding the implant site [15, 48]. In addition, these particles can be dissolved in contact with biological fluids, generating Ti ions [64]. However, emerging researches have demonstrated that Ti corrosion products are not entirely bioinert materials [65, 66]. To further support this claim, multiple systematic reviews have confirmed that Ti corrosion products can induce peri-implant inflammation and decrease the long-term success rate of dental implants [16, 67, 68].
Although the cause–effect relationship between Ti dissolution and peri-implant diseases is not fully comprehended, higher Ti particles/ions concentrations have been found in peri-implantitis sites [16]. These Ti particles released may have different sizes and morphologies (0.5–54 μm) and direct contact with bone tissue, as demonstrated in post-mortem human jawbone (HE et al. 2016) in Fig. 5A, B. Animal models have also been shown that Ti particles enhance pro-inflammatory cytokines release, infiltration of immune-inflammatory cells, and activation of osteoclast activity, resulting in unfavorable healing and osseointegration outcomes [69, 70]. From a microbiological point of view, our group recently demonstrated that Ti particle/ions interaction with bacterial cells, as visualized in Fig. 5C, D. This interaction can potentially change the microbiological composition of biofilms formed on Ti surfaces in the oral cavity leading to a composition similar to polymicrobial infections with higher pathogenicity [17]. Therefore, the presence of Ti products around dental implants may contribute to peri-implant bone resorption, microbial dysbiosis and, consequently, enhance the risk of peri-implantitis development [65].
Effect of titanium corrosion products on peri-implant tissues and oral biofilms. A and B Histological images of bone slices with a dental implant (300 μm thick, Giemsa-Eosin stained; light microscopy analysis) show that the primary location of Ti particles is in the bone marrow tissue at a distance of 60–700 μm from the implant, with particle sizes < 40 μm, confirming the corrosion products release in post-mortem human jawbone. C and D Transmission electron microscopy (80 kV, 5 and 1 μm magnification) showed biofilms formed in situ (oral cavity) on Ti surface and exposed to the treatment of Ti particles. Red arrows indicate Ti particles agglomerated and precipitated Ti ions on extracellular sites around microorganism cells. EX extracellular environment, MI microorganism. Reprinted (adapted) from He et al. [18] and Souza et al. [11], Copyright (2021), with permission from Elsevier and John Wiley and Sons (license numbers 5079491368023, 5074931356473) (Color figure online)
4 The Current Weight of Evidence of the Microbial Corrosion in Dental Implants
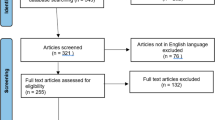
In this section, we strive to offer an overview of the scientific evidence on microbial corrosion in dental implants, regardless of the methodological quality of the studies. For this, we followed the guidelines of Preferred Reporting Items for Systematic reviews or Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) [71]. The orientated research question was: “What is the current state of knowledge regarding microbial corrosion in titanium-based dental implants?” In this review, only studies with electrochemical data related to biofilm-covered Ti surfaces were considered. For full methodological details, see Supplementary Methods (available online). To explore differences among each study design, data from biofilm models (Table 1), electrochemical assays (Table 2), and corrosion/tribocorrosion outcomes (Table 3) were outlined.
cpTi
4.1 State-of-Art in Microbial Corrosion Science
The initial search identified a total of 1643 records from all electronic databases and manual searches. Following the scoping review strategy, 15 eligible studies were included in the quantitative synthesis (please see Supplemental Results; Fig. S1). Six pre-eligible studies [61, 72,73,74,75,76] were excluded during the studies selection because they only performed surface characterization tests after biofilm exposure without referring to electrochemical assays. Furthermore, two studies [77, 78] that evaluated the microbiological effect and corrosion behavior independently and two studies [79, 80] that did not use titanium material as a substrate for biofilm growth were also excluded.
All eligible studies (n = 15) were published between 2003 [49] and 2021 [81] in nine different countries (United States of America, Taiwan, Brazil, Mexico, Spain, Portugal, Japan, China, and Chile), showing a progressive increase in the rate of publication in this field. Medical-grade pure titanium, titanium–aluminum–vanadium (Ti–6Al–4V), and titanium–zirconia (Ti–Zr) alloys were used among the implant materials. In terms of surface treatment, only five studies considered SLA [7, 15, 20, 75], modified SLA (modSLA) [15], anodized [7] or porous [82] surfaces, while the others used machined surfaces. The surface feature before electrochemical tests was impossible to summarize due to the lack of information in most studies. Considering that roughness and surface area have an essential role in Ti material's electrochemical behavior [4], this lack of data represents a significant scientific barrier to overcome in future studies to ensure better interpreting of microbial corrosion results and comparison among different studies.
4.2 Oral Biofilm Models to Test Microbial Corrosion
Regarding the biofilm model used on the selected studies (Table 1), mono-species [7, 13, 20, 21, 48, 49, 63, 82,83,84,85], dual-species [12, 85], and polymicrobial [15, 81, 86] were used. S. mutans is the preferred pathogen used to test microbial corrosion in aerobic conditions (37 °C, 5% CO2), possibly due to its high acidogenic ability [7, 12, 13, 15, 21, 48, 49, 81, 86]. Despite the well-known ability of S. mutans to adversely lower the electrochemical behavior of Ti surfaces [48, 74], this oral pathogen is not directly associated with the pathogenesis of the peri-implant diseases [58]. Similarly, Staphylococcus aureus, the main bacterium related to a bone infection in orthopedic implants [86], was investigated in one study for dental purposes [82]. To date, only one study [81] provided experimental results of microbial corrosion using a polymicrobial biofilm model with key periodontopathogens, such as P. gingivalis, A. actinomycetemcomitans, and F. nucleatum in anaerobic condition (37 °C, 85% N2, 5% H2, 10% CO2). Thus, biofilm models considering the wide microbial diversity of oral cavity and environmental conditions (i.e., anaerobiosis, pH, temperature, carbohydrate exposure), which mimics the in vivo implant site, should be considered further in vitro and in vivo tests for better translating these findings into clinical situations and generate more clinically significant results.
Another relevant point is related to in vitro bacteria supplementation. Several solutions have been used to stimulate bacterial growth (e.g., glucose, sucrose, mucin, peptone, urea, hydrochloric acid, yeast extract, hemin, and vitamin K). However, some solutions may change the pH of the medium, as hydrochloric acid with a pH ~ 6.7 [83]. Additionally, carbohydrate supplementation, as the combination of sucrose and S. mutans, may drastically decrease the pH due to the acid production in the bacteria inoculum even before the biofilm formation, which does not mimic an in vivo process. Moreover, we found a broad range of bacterium inoculum concentrations (103–109 CFU/mL) with incubation time from 90 min up to 30 days for biofilm formation. Considering that deterioration of the oxide layer by acids produced by bacteria might be a slow and chronic process and dependent on the presence of viable bacteria, the electrochemical analysis can be performed during biofilm development [7, 12, 13, 15, 48, 49, 63, 81,82,83,84,85] or after biofilm removal of the surface [20, 21, 86]. When electrochemical tests are performed after the biofilm removal, it is possible to eliminate the acids' direct effect produced in the biofilm present in the medium. Meanwhile, biofilm elimination in the electrochemical test allows an estimation of the actual surface conditions and the direct effect of microbial accumulation in the electrochemical behavior of the surface after biofilm formation, being a better model alternative overall [21]. The currently published microbiological methodologies used are illustrated in Fig. 6.
The summarized sequence of in vitro biofilm model to test microbial corrosion on titanium material. Titanium discs can be exposed to different electrolyte solutions [human/artificial saliva, simulated body fluid (SBF) solution, and bacteria media] to spontaneously form a TiO2 layer on the surface. Next, mono or multispecies bacterial inoculum can promote biofilm-covered surface in a specific time. Then, the electrochemical assay can be performed during biofilm growth or after biofilm removal to check the microbial corrosion process. Finally, simultaneous corrosion, tribocorrosion, and wear characterizations can be obtained (created with BioRender.com; License number: DV22UL3LDQ)
4.3 Unraveling the Role of Oral Biofilm in Corrosion and Tribocorrosion Properties
Corrosion is an electrochemical process; therefore, electrochemical techniques have been frequently employed to determine and measure the Ti corrosion rate in static or dynamic conditions [55]. The vast majority of studies have used a standardized method of three-electrode cells coupled in a potentiostat system (Table 2), following the standard ANSI/AAMI/ISO 10993-15:2000 applicable for implantable devices or ASTM International (American Society for Testing and Materials, G61-86 and G31-72). A saturated calomel electrode was commonly used as the reference electrode, a platinum rod as the counter electrode, and the exposed surface of the sample as the working electrode. The working parameters employed to test the electrochemical stability of Ti material during or after biofilm exposure differ across the studies.
Regarding the electrolyte solution, inert solutions such as phosphate-buffered saline (PBS), NaCl 0.9%, Hank's, and Ringer's solutions were the most considered in corrosion tests. Nevertheless, six studies [12, 21, 48, 63, 83, 84] choose artificial saliva with different compositions and bacterial medium solution as the electrolyte to mimic the oral situation. Additionally, we observed that the pH range of solutions used in all studies varied from 5 (acidic) [84] to 7.4 (neutral/physiologic) [86]. This key information is not reported by some authors [15, 20, 48, 49, 63, 81, 82, 85]. The choice of electrolyte is a relevant factor because the effect of oral biofilm can overlap with solution characteristics, as pH level [4] and ionic exchange trigger by electrolyte composition [21].
Among the 15 eligible studies, only 2 research groups [12, 63] used a linear reciprocating tribometer to investigate the synergic interaction between wear and corrosion in the presence of oral biofilms. The main difference between corrosion and tribocorrosion systems can be seen in Fig. 7. Nowadays, electrochemical and tribological synergic analyses have been suggested to translate the tribocorrosion phenomenon in the oral environment to the bench [8, 29, 55]. However, considering that these studies focused on the specific effect of Streptococcus salivarius [63] or S. mutans + Candida albicans [12] on the Ti corrosion/wear, in-depth analysis of the tribocorrosion kinetics using a polymicrobial biofilm model lack in the literature. Moreover, similar to corrosion assays, different working parameters (e.g., load, time, frequency) were employed in tribocorrosion systems. Therefore, guidelines and standardized protocols are also needed to improve the quality of electrochemical data obtained and allow direct comparison between the studies outcomes in the future.
Schematic diagram of corrosion and tribocorrosion testing systems. Static (corrosion) and dynamic (tribocorrosion) conditions can be considered to evaluate the microbial corrosion in Ti material. In addition to electrical and electrochemical outcomes, the tricorrosion systems can provide the samples' wear features and weight loss. Specific working parameters are recommended for each system. OCP open circuit potential, EIS electrochemical impedance spectroscopy, PP potentiodynamic polarization (created by Biorender®; License number AA22UL1R54)
Regardless of the type of electrochemical assay, the oral biofilm developed on the Ti surface negatively affected the material’s corrosion resistance (Table 3). In terms of electrical parameters, higher polarization resistance (Rp) and lower capacitance/constant phase element (Cdl, Q) values indicate higher corrosion resistance [87]. The available corrosion results revealed that the polarization resistance (Rp) and capacitance (Q) values shifted to lower and higher levels in biofilm-covered surfaces, respectively. Even studies that not considered groups without biofilms [7, 12, 15, 20, 21, 63, 81, 83, 85, 86], this trend was confirmed along the time points evaluated for the group with biofilms [7, 13, 15, 20, 21, 48, 49, 81,82,83,84, 86]. This fact supports the disadvantageous electrochemical properties of Ti material when it is exposed to different oral microorganisms (Streptococcus spp., Actinomyces spp., P. gingivalis, F. nucleatum, and C. albicans) since higher capacitance values indicate an increase in the ionic exchange between the material and the electrolyte/biofilm structure [53]. Moreover, a lower Rp suggests higher corrosion rates since this parameter is considered a measure of the barrier effect of the passive film against charge transfer [4]. Consequently, biofilm-covered surface may be more susceptible to Ti deterioration and material loss over time.
The electrochemical parameters, including corrosion potential (Ecorr), corrosion current density (icorr), and passive current density (ipass), also were negatively influenced by biofilm presence. Conceptually, nobler Ecorr values are associated with more remarkable passivity and lower corrosion tendency, while icorr indicates the current flow at an open circuit potential as a result of oxidation or reduction reactions, and ipass corresponds to the current value in the transition from the active region to the passive state of Ti [4, 53]. In other words, higher Ecorr and lower icorr and ipass values reflect low electrochemical activity and high corrosion resistance properties. Most studies found lower Ecorr [20, 49, 81, 83, 85], with higher icorr [13, 83, 85] and ipass [49, 85] values, demonstrating unfavorable electrochemical properties of Ti in the presence of biofilm.
Although it is difficult to estimate how much changes in the electrical and electrochemical parameters would have clinical relevance, it is known that reduced electrochemical properties of Ti have a direct relationship with surface deterioration. Microscopy analysis investigated this correlation in 12 studies [12, 15, 20, 21, 48, 63, 81,82,83,84,85,86]. To understand the whole kinetics of corrosion, inductively coupled plasma mass spectrometry should also be used to investigate Ti ions' content in the electrolyte solution after microbial corrosion tests, as conducted in two studies [7, 13]. Surprisingly, one study [21] showed the absence of pitting corrosion and no clear evidence of changes in the Ti surface after biofilm removal. Therefore, one may assume a threshold between the time/condition of biofilm growth and the risk of pitting corrosion, which needs further investigation. Additionally, only five studies [7, 20, 82, 86] evaluated the microbial corrosion on commercial surface treatment (i.e., SLA, anodized, or porous), representing one condition closer to clinical settings. Finally, preclinical and clinical studies investigating the influence of microbial corrosion on the longevity of Ti-based dental implants are lacking.
5 Preventing Microbial Corrosion in Implant Dentistry
Microbial corrosion is rarely linked to a single mechanism but is considered a complex reaction in which bacterial metabolites trigger or enhance the corrosion process [8, 29]. Therefore, there is an outstanding effort to prevent microbial corrosion using methods to inhibit biofilm formation or antimicrobial approaches or improve surface mechanical and chemical properties [88]. For this purpose, surface modification development to enhance the electrochemical behavior of Ti material for long-term dental implant clinical applications has been widely investigated [5]. Newly developed strategies have been focused mainly on surface properties dedicated to non-fouling abilities to prevent bacteria attachment and improve corrosion resistance [11, 89]. Nowadays, it is known that topographic patterns with different shapes and sizes have been shown to inhibit biofilm formation compared to flat surfaces [90]. In addition to the early-mentioned surfaces, antibacterial, anti-corrosive, and biocompatible coatings have also been indicated as strategies to improved implant survival and, consequently, decrease the harmful effect of microbial corrosion [39, 53]. Thus, since microorganisms can adhere directly to surfaces and lead to corrosion, inhibiting bacterial attachment or biofilm formation is a promising strategy to reduce microbial corrosion in the long term.
Another relevant strategy consists of dual-targeting therapies to disrupt the extracellular biofilm matrix without promoting implant surface damages. In mature biofilms with high bacterial cell density, the EPS-matrix forms a transport barrier, which may maintain the bacteria metabolites in contact with the surface and impeded saliva penetration to lixiviate these acidic [83]. Consequently, a higher deterioration of the TiO2 layer with increasing the time of biofilm development is expected. Recently, our group has shown that the iodopovidone (pre-treatment) may enhance the antibiofilm efficacy of antibiotics (second treatment) by dismantling the EPS matrix, amplifying the killing of pathogenic bacteria on Ti surfaces [39]. However, further studies are needed to check the effect of iodopovidone on Ti surface as a possible way to control peri-implant diseases and synergically microbial corrosion.
In a nutshell, these alternatives strategies mentioned above are promising approaches to control microbial corrosion. However, future preclinical and clinical studies need to consider some challenges, such as prolong effectiveness, enhanced surface properties, and effect on comprehensive microbial composition. Furthermore, this scoping review focused only on titanium-based dental implants, but other biomaterials (such as zirconium and its alloys) should also be considered in others research. Additionally, with greater reliability, the well-documented tribocorrosion assay can provide answers regarding titanium degradation against corrosive environments, including polymicrobial biofilms. Lastly, this review is a guide for researchers and materials scientists in developing new investigations and clinicians to understand the mechanisms involved in microbiologically induced corrosion in dental implants.
6 Conclusion and Outlook
In this scoping review, we reinforced that the microbial corrosion phenomenon can be considered one of the emerging areas of interest and research in implant dentistry and biomaterial fields. Considering the loss of passivity potential on titanium material and the corrosion of implant devices due to acidic metabolites produced from oral biofilms, this research topic is a concerning issue. To predict the microbial corrosion effects in in vitro conditions, corrosion/tribocorrosion tests can be used as suitable tools during biofilm formation or after biofilm removal from the titanium surface. Notably, the polymicrobial biofilm model represents a more clinical reliable condition to evaluate the changes in the electrochemical behavior of titanium but still is under-investigated. Additionally, the cause–effect relationship between biofilm formation and titanium deterioration is not fully understood due to its chronic long-term effect. The direct effect of microbial accumulation on the specific chemical, physical, and mechanical properties of the implant surface and its mechanism needs to be further investigated. Moreover, a feedback loop is expected in this process since biofilm leads to surface deterioration, and particles and ions released promote microbial accumulation and microbiological shift. Therefore, in the future, it is necessary for preclinical and clinical studies to investigate the influence of microbiologically induced corrosion on the survival of Ti-based dental implants. Additionally, to prevent this deleterious phenomenal, anti-fouling, antibacterial, and anti-corrosive coatings from preventing bacterial attachment or biofilm formation are encouraged to reduce microbial load and consequently corrosion. For instance, surface coatings—even without antimicrobial ability—may act as a protective film improving the material's corrosion resistance and can be a promising approach for implant device manufacturing.
Data Availability
Data sources are PubMed (MEDLINE), Scopus, Web of Science, EMBASE, Google Scholar, and the System for Information on Grey Literature in Europe (SIGLE) through the OpenGrey.
Change history
30 September 2021
A Correction to this paper has been published: https://doi.org/10.1007/s40735-021-00590-9
References
Albrektsson T, Dahl E, Enbom L, Engevall S, Engquist B, Eriksson AR, Feldmann G, Freiberg N, Glantz PO, Kjellman O (1988) Osseointegrated oral implants. A Swedish multicenter study of 8139 consecutively inserted Nobelpharma implants. J Periodontol 5:287–296. https://doi.org/10.1902/jop.1988.59.5.287
Moraschini V, Poubel LA, Ferreira VF, Barboza E (2015) Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: a systematic review. Int J Oral Maxillofac Surg 3:377–388. https://doi.org/10.1016/j.ijom.2014.10.023
Adell R, Lekholm U, Rockler B, Brånemark PI (1981) A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 6:387–416. https://doi.org/10.1016/s0300-9785(81)80077-4
Barão VA, Mathew MT, Assunção WG, Yuan JC, Wimmer MA, Sukotjo C (2012) Stability of cp-Ti and Ti–6Al–4V alloy for dental implants as a function of saliva pH—an electrochemical study. Clin Oral Implants Res. https://doi.org/10.1111/j.1600-0501.2011.02265.x
Costa RC, Souza J, Cordeiro JM, Bertolini M, de Avila ED, Landers R, Rangel EC, Fortulan CA, Retamal-Valdes B, da Cruz NC, Feres M, Barão V (2020) Synthesis of bioactive glass-based coating by plasma electrolytic oxidation: untangling a new deposition pathway toward titanium implant surfaces. J Colloid Interface Sci. https://doi.org/10.1016/j.jcis.2020.06.102
Villanueva J, Trino L, Thomas J, Bijukumar D, Royhman D, Stack M, Mathew M (2017) Corrosion, tribology, and tribocorrosion research in biomedical implants: progressive trend in the published literature. J Bio Tribo Corros 1:1–8. https://doi.org/10.1007/s40735-016-0060-1
Díaz I, Pacha-Olivenza MÁ, Tejero R, Anitua E, González-Martín ML, Escudero ML, García-Alonso MC (2018) Corrosion behavior of surface modifications on titanium dental implant. In situ bacteria monitoring by electrochemical techniques. J Biomed Mater Res B 3:997–1009. https://doi.org/10.1002/jbm.b.33906
Dini C, Costa RC, Sukotjo C, Takoudis CG, Mathew MT, Barão VAR (2020) Progression of bio–tribocorrosion in implant dentistry. Front Mech Eng. https://doi.org/10.3389/fmech.2020.00001
Berglundh T, Armitage G, Araujo MG, Avila-Ortiz G, Blanco J, Camargo PM, Chen S, Cochran D, Derks J, Figuero E, Hämmerle C, Heitz-Mayfield L, Huynh-Ba G, Iacono V, Koo KT, Lambert F, McCauley L, Quirynen M, Renvert S, Salvi GE, Zitzmann N (2018) Peri-implant diseases and conditions: Consensus Report of Workgroup 4 of the 2017 World Workshop on the Classification of Periodontal and Peri-implant Diseases and Conditions. J Clin Periodontol 20:286-S291. https://doi.org/10.1111/jcpe.12957
Daubert DM, Weinstein BF (2000) (2019) Biofilm as a risk factor in implant treatment. Periodontology 1:29–40. https://doi.org/10.1111/prd.12280
Souza J, Bertolini MM, Costa RC, Nagay BE, Dongari-Bagtzoglou A, Barão V (2021) Targeting implant-associated infections: titanium surface loaded with antimicrobial. iScience 1:102008. https://doi.org/10.1016/j.isci.2020.102008
Souza JCM, Henriques M, Oliveira R, Teughels W, Celis JP, Rocha LA (2010) Do oral biofilms influence the wear and corrosion behavior of titanium? Biofouling 4:471–478. https://doi.org/10.1080/08927011003767985
Fukushima A, Mayanagi G, Nakajo K, Sasaki K, Takahashi N (2014) Microbiologically induced corrosive properties of the titanium surface. J Dent Res 5:525–529. https://doi.org/10.1177/0022034514524782
Rodrigues DC, Sridhar S, Gindri IM, Siddiqui DA, Pilar V, Wilsom TG Jr, Chung K, Wadhwani C (2016) Spectroscopic and microscopic investigation of the effects of bacteria on dental implant surfaces. RSC Adv 54:48283–48293. https://doi.org/10.1039/c6ra07760a
Siddiqui DA, Guida L, Sridhar S, Valderrama P, Wilson TG Jr, Rodrigues DC (2019) Evaluation of oral microbial corrosion on the surface degradation of dental implant materials. J Periodontol 3:72–81. https://doi.org/10.1002/JPER.18-0110
Suárez-López Del Amo F, Garaicoa-Pazmiño C, Fretwurst T, Castilho RM, Squarize CH (2018) Dental implants-associated release of titanium particles: a systematic review. Clin Oral Implants Res 11:1085–1100. https://doi.org/10.1111/clr.13372
Souza J, Costa Oliveira BE, Bertolini M, Lima CV, Retamal-Valdes B, de Faveri M, Feres M, Barão V (2020) Titanium particles and ions favor dysbiosis in oral biofilms. J Periodontal Res 2:258–266. https://doi.org/10.1111/jre.12711
He J, Zhou W, Zhou X, Zhong X, Zhang X, Wan P, Zhu B, Chen W (2008) The anatase phase of nanotopography titania plays an important role on osteoblast cell morphology and proliferation. J Mater Sci Mater Med. https://doi.org/10.1007/s10856-008-3505-3
Pettersson M, Pettersson J, Molin Thorén M, Johansson A (2017) Release of titanium after insertion of dental implants with different surface characteristics—an ex vivo animal study. Acta biomater odontol Scand 1:63–73. https://doi.org/10.1080/23337931.2017.1399270
Xu L, Yu X, Chen W, Zhang S, Qiu J (2020) Biocorrosion of pure and SLA titanium surfaces in the presence of Porphyromonas gingivalis and its effects on osteoblast behavior. RSC Adv 14:8198–8206. https://doi.org/10.1039/d0ra00154f
Souza J, Beline T, Matos AO, Costa Oliveira BE, Ricomini-Filho AP, Barão V (2018) Electrochemical behavior of titanium exposed to a biofilm supplemented with different sucrose concentrations. J Prosthet Dent 2:290–298. https://doi.org/10.1016/j.prosdent.2017.10.012
Mombelli A, Décaillet F (2011) The characteristics of biofilms in peri-implant disease. J Clin Periodontol 11:203–213. https://doi.org/10.1111/j.1600-051X.2010.01666.x
Zuo R (2007) Biofilms: strategies for metal corrosion inhibition employing microorganisms. Appl Microbiol Biotechnol 6:1245–1253. https://doi.org/10.1007/s00253-007-1130-6
Rodrigues DC, Valderrama P, Wilson TG, Palmer K, Thomas A, Sridhar S, Adapalli A, Burbano M, Wadhwani C (2013) Titanium corrosion mechanisms in the oral environment: a retrieval study. Materials (Basel Switz) 11:5258–5274. https://doi.org/10.3390/ma6115258
Arciola CR, Campoccia D, Montanaro L (2018) Implant infections: adhesion, biofilm formation and immune evasion. Nat Rev Microbiol 7:397–409. https://doi.org/10.1038/s41579-018-0019-y
Rabe M, Verdes D, Seeger S (2011) Understanding protein adsorption phenomena at solid surfaces. Adv Colloid Interface Sci 1:87–106. https://doi.org/10.1016/j.cis.2010.12.007
Dodo CG, Senna PM, Custodio W, Paes Leme AF, Del Bel Cury AA (2013) Proteome analysis of the plasma protein layer adsorbed to a rough titanium surface. Biofouling. https://doi.org/10.1002/jbm.a.30754
An YH, Dickinson RB, Doyle RJ (2000) Mechanisms of bacterial adhesion and pathogenesis of implant and tissue infections. In: An YH, Friedman RJ (eds) Handbook of bacterial adhesion: principles, methods, and applications. Humana Press, Totowa, pp 1–27. https://doi.org/10.1385/1-59259-224-4:1
Souza J, Henriques M, Teughels W, Ponthiaux P, Celis J, Rocha LA (2015) Wear and corrosion interactions on titanium in oral environment: literature review. J Bio Tribo Corros 2:1–13. https://doi.org/10.1007/s40735-015-0013-0
Souza J, Bertolini M, Costa RC, Lima CV, Barão V (2020) Proteomic profile of the saliva and plasma protein layer adsorbed on Ti–Zr alloy: the effect of sandblasted and acid-etched surface treatment. Biofouling 4:428–441. https://doi.org/10.1080/08927014.2020.1769613
Celli J, Gregor B, Turner B, Afdhal NH, Bansil R, Erramilli S (2005) Viscoelastic properties and dynamics of porcine gastric mucin. Biomacromolecules 3:1329–1333. https://doi.org/10.1021/bm0493990
Branco AC, Moreira V, Reis JA, Colaço R, Figueiredo-Pina CG, Serro AP (2019) Influence of contact configuration and lubricating conditions on the microtriboactivity of the zirconia–Ti6Al4V pair used in dental applications. J Mech Behav Biomed Mater. https://doi.org/10.1016/j.jmbbm.2018.12.009
Serro AP, Gispert MP, Martins MC, Brogueira P, Colaço R, Saramago B (2006) Adsorption of albumin on prosthetic materials: implication for tribological behavior. J Biomed Mater Res A 78:581–589. https://doi.org/10.1002/jbm.a.30754
Nakanishi K, Sakiyama T, Imamura K (2001) On the adsorption of proteins on solid surfaces, a common but very complicated phenomenon. J Biosci Bioeng 3:233–244. https://doi.org/10.1263/jbb.91.233
Bowen WH, Burne RA, Wu H, Koo H (2018) Oral biofilms: pathogens, matrix, and polymicrobial interactions in microenvironments. Trends Microbiol 3:229–242. https://doi.org/10.1016/j.tim.2017.09.008
Belibasakis GN, Manoil D (2021) Microbial community-driven etiopathogenesis of peri-implantitis. J Dent Res 1:21–28. https://doi.org/10.1177/0022034520949851
Flemming HC, Wingender J, Szewzyk U, Steinberg P, Rice SA, Kjelleberg S (2016) Biofilms: an emergent form of bacterial life. Nat Rev Microbiol 9:563–575. https://doi.org/10.1038/nrmicro.2016.94
Karygianni L, Ren Z, Koo H, Thurnheer T (2020) Biofilm matrixome: extracellular components in structured microbial communities. Trends Microbiol. https://doi.org/10.1016/j.tim.2020.03.016
Costa RC, Souza J, Bertolini M, Retamal-Valdes B, Feres M, Barão V (2020) Extracellular biofilm matrix leads to microbial dysbiosis and reduces biofilm susceptibility to antimicrobials on titanium biomaterial: an in vitro and in situ study. Clin Oral Implants Res 12:1173–1186. https://doi.org/10.1111/clr.13663
Apaza-Bedoya K, Tarce M, Benfatti CAM, Henriques B, Mathew MT, Teughels W (2017) Synergistic interactions between corrosion and wear at titanium-based dental implant connections: a scoping review. J Periodontal Res 52:946–954. https://doi.org/10.1111/jre.12469
Filho AP, Fernandes FS, Straioto FG, Silva WD, Cury AA (2010) Preload loss and bacterial penetration on different implant-abutment connection systems. Braz Dent J 2:123–129. https://doi.org/10.1590/S0103-64402010000200006
Piattelli A, Scarano A, Paolantonio M, Assenza B, Leghissa GC, Di Bonaventura G, Catamo G, Piccolomini R (2001) Fluids and microbial penetration in the internal part of cement-retained versus screw-retained implant-abutment connections. J Periodontol 9:1146–1150. https://doi.org/10.1902/jop.2000.72.9.1146
Bordin D, Cavalcanti IM, Jardim Pimentel M, Fortulan CA, Sotto-Maior BS, Del Bel Cury AA, da Silva WJ (2015) Biofilm and saliva affect the biomechanical behavior of dental implants. J Biomech 6:997–1002. https://doi.org/10.1016/j.jbiomech.2015.02.004
Cense AW, Peeters EA, Gottenbos B, Baaijens FP, Nuijs AM, van Dongen ME (2006) Mechanical properties and failure of Streptococcus mutans biofilms, studied using a microindentation device. J Microbiol Methods 3:463–472. https://doi.org/10.1016/j.mimet.2006.04.023
Hwang G, Klein MI, Koo H (2014) Analysis of the mechanical stability and surface detachment of mature Streptococcus mutans biofilms by applying a range of external shear forces. Biofouling. https://doi.org/10.1080/08927014.2014.969249
Barão VAR, Yoon CJ, Mathew MT, Yuan JCC, Wu CD, Sukotjo C (2014) Attachment of Porphyromonas gingivalis to corroded commercially pure titanium and titanium–aluminum–vanadium alloy. J Periodontol 9:1275–1282. https://doi.org/10.1902/jop.2014.130595
Ramesh D, Sridhar S, Siddiqui DA, Valderrama P, Rodrigues D (2017) Detoxification of titanium implant surfaces: evaluation of surface morphology and bone-forming cell compatibility. J Bio Tribo Corros 4:1–13. https://doi.org/10.1007/s40735-017-0111-2
Souza JC, Ponthiaux P, Henriques M, Oliveira R, Teughels W, Celis JP, Rocha LA (2013) Corrosion behaviour of titanium in the presence of Streptococcus mutans. J Dent 6:528–534. https://doi.org/10.1016/j.jdent.2013.03.008
Chang JC, Oshida Y, Gregory RL, Andres CJ, Barco TM, Brown DT (2003) Electrochemical study on microbiology-related corrosion of metallic dental materials. Biomed Mater Eng 3:281–295
Koike M, Fujii H (2001) The corrosion resistance of pure titanium in organic acids. Biomaterials 21:2931–2936. https://doi.org/10.1016/s0142-9612(01)00040-0
Mabilleau G, Bourdon S, Joly-Guillou M, Filmon R, Baslé M, Chappard D (2006) Influence of fluoride, hydrogen peroxide and lactic acid on the corrosion resistance of commercially pure titanium. Acta biomater 2:121–129. https://doi.org/10.1016/j.actbio.2005.09.004
Souza J, Barbosa SL, Ariza E, Celis J, Rocha LA (2012) Simultaneous degradation by corrosion and wear of titanium in artificial saliva containing fluorides. Wear. https://doi.org/10.1016/J.WEAR.2012.05.030
Beline T, Garcia CS, Ogawa ES, Marques ISV, Matos AO, Sukotjo C, Barão VAR (2016) Surface treatment influences electrochemical stability of cpTi exposed to mouthwashes. Mater Sci Eng C. https://doi.org/10.1016/j.msec.2015.11.045
Peñarrieta-Juanito G, Sordi MB, Henriques B, Dotto M, Teughels W, Silva FS, Magini RS, Souza J (2019) Surface damage of dental implant systems and ions release after exposure to fluoride and hydrogen peroxide. J Periodontal Res 1:46–52. https://doi.org/10.1111/jre.12603
Mathew MT, Abbey S, Hallab NJ, Hall DJ, Sukotjo C, Wimmer MA (2012) Influence of pH on the tribocorrosion behavior of cp-Ti in the oral environment: synergistic interactions of wear and corrosion. J Biomed Mater Res B 6:1662–1671. https://doi.org/10.1002/jbm.b.32735
Costerton JW, Lewandowski Z, Caldwell DE, Korber DR, Lappin-Scott HM (1995) Microbial biofilms. Annu Rev Microbiol. https://doi.org/10.1146/annurev.mi.49.100195.003431
Marsh PD, Moter A (2000) Devine DA (2011) Dental plaque biofilms: communities, conflict and control. Periodontology 1:16–35. https://doi.org/10.1111/j.1600-0757.2009.00339.x
Lafaurie GI, Sabogal MA, Castillo DM, Rincón MV, Gómez LA, Lesmes YA, Chambrone L (2017) Microbiome and microbial biofilm profiles of peri-implantitis: a systematic review. J Periodontol 10:1066–1089. https://doi.org/10.1902/jop.2017.170123
Barão VA, Mathew MT, Assunção WG, Yuan JC, Wimmer MA, Sukotjo C (2011) The role of lipopolysaccharide on the electrochemical behavior of titanium. J Dent Res 5:613–618. https://doi.org/10.1177/0022034510396880
Faverani LP, Assunção WG, de Carvalho PS, Yuan JC, Sukotjo C, Mathew MT, Barao VA (2014) Effects of dextrose and lipopolysaccharide on the corrosion behavior of a Ti–6Al–4V alloy with a smooth surface or treated with double-acid-etching. PLoS ONE 3:e93377. https://doi.org/10.1371/journal.pone.0093377
Harada R, Kokubu E, Kinoshita H, Yoshinari M, Ishihara K, Kawada E, Takemoto S (2018) Corrosion behavior of titanium in response to sulfides produced by Porphyromonas gingivalis. Dent Mater Off Publ Acad Dent Mater 2:183–191. https://doi.org/10.1016/j.dental.2017.10.004
Barão VA, Ricomini-Filho AP, Faverani LP, Del Bel Cury AA, Sukotjo C, Monteiro DR, Yuan JC, Mathew MT, do Amaral RC, Mesquita MF, da Silva WJ, Assunção WG (2015) The role of nicotine, cotinine and caffeine on the electrochemical behavior and bacterial colonization to cp-Ti. Mater Sci Eng C. https://doi.org/10.1016/j.msec.2015.06.026
Figueiredo-Pina CG, Guedes M, Sequeira J, Pinto D, Bernardo N, Carneiro C (2019) On the influence of Streptococcus salivarius on the wear response of dental implants: an in vitro study. J Biomed Mater Res B 5:1393–1399. https://doi.org/10.1002/jbm.b.34231
Soto-Alvaredo J, Blanco E, Bettmer J, Hevia D, Sainz RM, López Cháves C, Sánchez C, Llopis J, Sanz-Medel A, Montes-Bayón M (2014) Evaluation of the biological effect of Ti generated debris from metal implants: ions and nanoparticles. Metallomics Integr Biomet Sci 9:1702–1708. https://doi.org/10.1039/c4mt00133h
Fretwurst T, Nelson K, Tarnow DP, Wang HL, Giannobile WV (2018) Is metal particle release associated with peri-implant bone destruction? An emerging concept. J Dent Res 3:259–265. https://doi.org/10.1177/0022034517740560
Pettersson M, Kelk P, Belibasakis GN, Bylund D, Molin Thorén M, Johansson A (2017) Titanium ions form particles that activate and execute interleukin-1β release from lipopolysaccharide-primed macrophages. J Periodontal Res 1:21–32. https://doi.org/10.1111/jre.12364
Delgado-Ruiz R, Romanos G (2018) Potential causes of titanium particle and ion release in implant dentistry: a systematic review. Int J Mol Sci 11:3585. https://doi.org/10.3390/ijms19113585
Noronha Oliveira M, Schunemann W, Mathew MT, Henriques B, Magini RS, Teughels W, Souza J (2018) Can degradation products released from dental implants affect peri-implant tissues? J Periodontal Res 1:1–11. https://doi.org/10.1111/jre.12479
Biguetti C, Cavalla F, Fonseca AC, Tabanez AP, Siddiqui DA, Wheelis S, Taga R, Fakhouri W, Silva RM, Rodrigues D, Garlet G (2021) Effects of titanium corrosion products on in vivo biological response: a basis for the understanding of osseointegration failures mechanisms. Front Mater. https://doi.org/10.3389/fmats.2021.651970
Olmedo DG, Duffó G, Cabrini RL, Guglielmotti MB (2008) Local effect of titanium implant corrosion: an experimental study in rats. Int J Oral Maxillofac Surg 11:1032–1038. https://doi.org/10.1016/j.ijom.2008.05.013
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters M, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Straus SE (2018) PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 7:467–473. https://doi.org/10.7326/M18-0850
Gil FJ, Rodriguez A, Espinar E, Llamas JM, Padullés E, Juárez A (2012) Effect of oral bacteria on the mechanical behavior of titanium dental implants. Int J Oral Maxillofac Implants 1:64–68
Camargo S, Roy T, Xia X, Fares C, Hsu SM, Ren F, Clark AE, Neal D, Esquivel-Upshaw JF (2021) Novel coatings to minimize corrosion of titanium in oral biofilm. Materials (Basel Switz) 2:342. https://doi.org/10.3390/ma14020342
Rocha SS, Bernardi ACA, Pizzolito AC, Adabo GL, Pizzolito EL (2009) Streptococcus mutans attachment on a cast titanium surface. Mater Res 1:41–44. https://doi.org/10.1590/S1516-14392009000100003
Sridhar S, Wilson TG Jr, Palmer KL, Valderrama P, Mathew MT, Prasad S, Jacobs M, Gindri IM, Rodrigues DC (2015) In vitro investigation of the effect of oral bacteria in the surface oxidation of dental implants. Clin Implant Dent Relat Res 2:e562–e575. https://doi.org/10.1111/cid.12285
Sridhar S, Abidi Z, Wilson TG Jr, Valderrama P, Wadhwani C, Palmer K, Rodrigues DC (2016) In vitro evaluation of the effects of multiple oral factors on dental implants surfaces. J Oral Implantol 3:248–257. https://doi.org/10.1563/aaid-joi-D-15-00165
Lin N, Huang X, Zhang X, Fan A, Qin L, Tang B (2012) In vitro assessments on bacterial adhesion and corrosion performance of TiN coating on Ti6Al4V titanium alloy synthesized by multi-arc ion plating. Appl Surf Sci. https://doi.org/10.1016/J.APSUSC.2012.03.163
Liu R, Tang Y, Zeng L, Zhao Y, Ma Z, Sun Z, Xiang L, Ren L, Yang K (2018) In vitro and in vivo studies of anti-bacterial copper-bearing titanium alloy for dental application. Dent Mater Off Publ Acad Dent Mater 8:1112–1126. https://doi.org/10.1016/j.dental.2018.04.007
Laurent F, Grosgogeat B, Reclaru L, Dalard F, Lissac M (2001) Comparison of corrosion behaviour in presence of oral bacteria. Biomaterials 16:2273–2282. https://doi.org/10.1016/s0142-9612(00)00416-6
Koh I, Oshida Y, Andres CJ, Gregory RL (2008) Effect of surface area ratios and bacteria on electrochemical behavior of galvanically coupled titanium. Int J Prosthodont 5:433–436
Chandrashekar BL, Siddiqui BA, Palmer KL, Rodrigues DC (2021) Titanium surfaces and detoxification procedures: effects of bacterial biofilm and citric acid exposure on oxide layer behavior. J Bio Tribo Corros. https://doi.org/10.1007/s40735-021-00484-w
Silva D, Guerra C, Muñoz H, Aguilar C, Walter M, Azócar M, Muñoz L, Gürbüz E, Ringuedé A, Cassir M, Sancy M (2020) The effect of Staphylococcus aureus on the electrochemical behavior of porous Ti–6Al–4V alloy. Bioelectrochemistry. https://doi.org/10.1016/j.bioelechem.2020.107622
Li L, Li S, Qu Q, Zuo L, He Y, Zhu B, Li C (2017) Streptococcus sanguinis biofilm architecture and its influence on titanium corrosion in enriched artificial saliva. Materials (Basel Switz) 3:255. https://doi.org/10.3390/ma10030255
Zhang SM, Qiu J, Tian F, Guo XK, Zhang FQ, Huang QF (2013) Corrosion behavior of pure titanium in the presence of Actinomyces naeslundii. J Mater Sci Mater Med 5:1229–1237. https://doi.org/10.1007/s10856-013-4888-3
De la Garza-Ramos MA, Estupiñan-Lopez FH, Gaona-Tiburcio C, Beltrán-Novelo LG, Zambrano-Robledo P, Cabral-Miramontes J, Almeraya-Calderón F (2020) Electrochemical behavior of Ti6Al4V alloy used in dental implants immersed in Streptococcus gordonii and Fusobacterium nucleatum solutions. Materials (Basel Switz) 18:4185. https://doi.org/10.3390/ma13184185
Sridhar S, Wang F, Wilson TG, Palmer K, Valderrama P, Rodrigues DC (2019) The role of bacterial biofilm and mechanical forces in modulating dental implant failures. J Mech Behav Biomed Mater. https://doi.org/10.1016/j.jmbbm.2019.01.012
Ogawa ES, Matos AO, Beline T, Marques ISV, Sukotjo C, Mathew MT, Rangel EC, Cruz NC, Mesquita MF, Consani RX (2016) Surface-treated commercially pure titanium for biomedical applications: electrochemical, structural, mechanical and chemical characterizations. Mater Sci Eng 65:251–261. https://doi.org/10.1016/j.msec.2016.04.036
Spriano S, Yamaguchi S, Baino F, Ferraris S (2018) A critical review of multifunctional titanium surfaces: new frontiers for improving osseointegration and host response, avoiding bacteria contamination. Acta biomater. https://doi.org/10.1016/j.actbio.2018.08.013
Linklater DP, Baulin VA, Juodkazis S, Crawford RJ, Stoodley P, Ivanova EP (2021) Mechano-bactericidal actions of nanostructured surfaces. Nat Rev Microbiol 1:8–22. https://doi.org/10.1038/s41579-020-0414-z
Ferraris S, Venturello A, Miola M, Cochis A, Rimondini L, Spriano S (2014) Antibacterial and bioactive nanostructured titanium surfaces for bone integration. Appl Surf Sci. https://doi.org/10.1016/j.apsusc.2014.05.056
Acknowledgements
The authors express their gratitude to the São Paulo Research Foundation (FAPESP; Grant Number #2020/10436-4) for the scholarship provided to the first author), the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior: Brazil (CAPES, Finance Code 001) for the scholarship provided to the first and second authors, the Conselho Nacional de Desenvolvimento Científico e Tecnológico-Brazil (CNPq, Grant Number 304853/2018-6) provided to VARB.
Author information
Authors and Affiliations
Contributions
RCC, VLA, PHCM, and IMV collected the data and led the writing. MB, MTM, VAR, and JGSS made the critical review of article content and writing. All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Valentim A. R. Barão’s and João Gabriel S. Souza’s names were corrected.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Costa, R.C., Abdo, V.L., Mendes, P.H.C. et al. Microbial Corrosion in Titanium-Based Dental Implants: How Tiny Bacteria Can Create a Big Problem?. J Bio Tribo Corros 7, 136 (2021). https://doi.org/10.1007/s40735-021-00575-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40735-021-00575-8