Abstract
Background
Titanium and its alloys are the gold standard for dental implants because of their unique combination of chemical, physical, and biological properties, and in particular thanks to their biocompatibility, resistance to corrosion, and mechanical properties. However, despite advanced technologies to avoid corrosion of dental implants, the mechanisms toward the release of metals and their role in the onset of peri-implant diseases are still under-investigated. The combination of stress, corrosion, and bacteria contributes to implant failure. Recent studies suggest the existence of wear/corrosion products may correlate with peri-implantitis progress by triggering microbial dysbiosis, the release of pro-inflammatory cytokines, and animal bone resorption.
Aim
The aim of the present article is to highlight the various features of corrosion of titanium alloys used in dental titanium implants, to review the evidence toward biocorrosion in the oral environment and to discuss the methodological and electrochemical aspects of surface treatments and titanium-based alloys.
Methods
The present review was conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines. The research question was about the corrosion of titanium alloys used in dental implants and their consequent biological side effects on peri-implant tissue.
Results
After screening the duplicates and following the application of exclusion criteria, the full texts of 23 articles were included in the review.
Conclusions
The development of improved strategies toward the reduction of corrosion and degradation of titanium alloys used for dental implants is crucial, also to prevent metal release in the tissue surrounding them to prolong their lifetime. As chemical and physical properties are crucial for the electrochemical behavior of the implant material, the development of appropriate alloys or coatings/layers for corrosion inhibition is mandatory.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cobalt-based alloys, magnesium (Mg), and its alloys have proven their applicability as bone implants. However, titanium (Ti) is the most popular material used for dental implants, and its alloys have been widely applied clinically. An ideal implant should be biocompatible, possess high strength, fatigue and fracture toughness behavior and should be able to withstand the reactive environment it is exposed to inside the human body [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96].
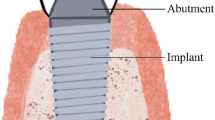
Ti-based dental implants have become a predictable standard of care for replacing missing teeth, thanks to the good mechanical properties, the resistance to corrosion, and the excellent biological performance of Ti, that is able to produce a spontaneous Ti oxide layer after exposure to oxygen atmosphere (mainly TiO2) [2, 4, 7, 10,11,12,13,14,15]. However, corrosion of dental implants may jeopardize the mechanical stability of the device, as well as the integrity of the surrounding tissue. Pure titanium, in spite of its corrosion-resistant characteristics within controlled environments and in the absence of load, it can corrode under oral conditions and in association with cyclic loads, thus influencing the mechanical stability of dental implants. In fact, exposure to acidic substances and microbial metabolites can lead to a reduction in pH, potentially causing the rupture of the passive film. Moreover, the TiO2 barrier might have a poor tribological efficacy and it might be removed/disrupted under loading [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30]. Metallic debris may induce an inflammatory response. In fact, the products yielded by corrosion may have cytotoxic effects on the tissue surrounding the implant [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37].
Types of corrosion associated with metallic implants may be galvanic, fretting, pitting, and crevice corrosion. As for galvanic corrosion, theoretically, titanium screw would represent the anode, the metallic fill the cathode, and saliva would be the electrolyte. Fretting corrosion would occur because of disruption of the protective layer on titanium screws, while pitting corrosion would be the consequence of the spontaneous breakdown of the passivating film on a flat or overexposed area. Finally, crevice corrosion is associated with uneven surfaces.
These corrosive factors, together with wear induced by implantation procedures (e.g., friction, micro-motion), may determine an undesired release of metallic ions and particles from the implant to the surrounding tissues, thus eventually leading to severe biological complications such as peri-implant diseases [1,2,3,4,5,6,7,8, 13,14,15,16, 25, 36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63]. Furthermore, the rate of a corrosion process depends on the oxide layer formed, pH, the concentration and composition of the electrolyte, and the transport of oxygen vacancy across the film.
Therefore, in consideration of corrosion as a potential risk factor for peri-implantitis, the knowledge of the influence of corrosion-induced release of ions and particles as a driving factor for peri-implant diseases and early/late failure of dental implants is fundamental and clinically relevant.
The aim of the present article is to review the currently available information about the corrosion of titanium alloys used in dental implants and their consequent biological side effects on peri-implant tissue.
Materials and Methods
The present review was conducted according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines. The research question was about the corrosion of titanium alloys used in dental implants and their consequent biological side effects on peri-implant tissue. A literature search was conducted in four electronic databases (Medline/PubMed, Scopus, Embase, and Web of Science) using the combination of the terms “dental implants” OR “surface treatments” OR “alloys” AND “corrosion” OR “electrochemical” OR “degradation.
Articles not in English language were excluded.
The following types of articles were excluded: duplicated/overlapping articles, animal studies, conference proceedings, expert statements, editorials, case reports, and nonoriginal papers.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Results
The initial search resulted in 543 articles. After screening the duplicates and following the application of exclusion criteria, the full texts of 23 articles were included in the review (Fig. 1).
Discussion
After dental implants are inserted in the jaws, the integrity of the protective TiO2 passive layer, as well as the maintenance of their physicochemical properties, depends on the hostile electrolytic oral environment. In fact, oral fluids (saliva, blood plasma) are characterized by organic and inorganic substances in combination with a pH between 6 and 7, that may be reduced by some factors such as microbial metabolites and corrosive substances, thus making the environment acidic and highly reactive to chemically attack the metallic surfaces [20,21,22,23,24,25, 36, 42, 62, 70,71,72,73,74, 82].
Cl− , F− , H+ , and other corrosive substances, may be found not only in saliva, but also in prophylactic commercial formulations, such as toothpaste and mouth rinses, and foods.
In particular, in literature, the F− ion concentration adversely affects the corrosion resistance of titanium-based materials because of the formation of hydrofluoric acid (HF) from fluoride ions when the aqueous environment is acidified by some food or microbial metabolites. HF is strongly reactive to metals because of its chemical characteristics prone to induce the breakdown of the TiO2 protective layer (TiO2 + 4HF → TiF4 + 2H2O). Therefore, HF not only promotes the degradation but also the discoloration of the metal surface because of the generated fluoride-titanium compounds [53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69].
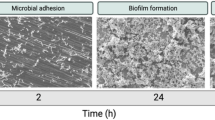
One of the significant factors contributing to the reduction in the corrosion resistance of titanium is the action of oral bacteria. When dental implants are inserted in the oral cavity, the outer implant surface and the micro gaps between the implant and abutments are covered by protein-rich fluid pellicle (saliva, blood), thus promoting the adhesion of bacteria to these surfaces. Bacterial acidic metabolites and oxygen level deficiency may determine oxidation reactions between the biofilm-covered Ti surface and the exposed Ti, increasing the corrosion rate of the implant material [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41].
Therefore, bacterial cells and physical, chemical, microbiological, and inflammatory corrosion processes promote the surface damage of dental implants and contribute to the implant surface degradation. This may adversely alter the microenvironment conditions of peri-implant tissues, leading to cytotoxic and inflammatory reactions. Finally, such events compromise the success of dental implant rehabilitations [10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32].
The processes involved in the corrosion of titanium alloys of dental implants may be mechanical (wear particles/debris), electrochemical (corrosion-related free metal ions, organometallic complexes, and salts), and/or a combination of both mechanical and electrochemical processes (tribocorrosion).
Tribocorrosion occurs under the dual action of wear and corrosion under a variety of conditions such as sliding, fretting, rolling, impingement in a corrosive medium.
The most common types of electrochemical corrosion found in titanium alloys used for implant applications are galvanic, fretting, and pitting/crevice corrosion, as well as environmentally induced cracking (EIC) [20,21,22,23,24,25, 36, 42, 62, 70,71,72,73,74, 82].
Galvanic corrosion is associated with a direct contact of two dissimilar metals in an electrolytic solution. The difference in electrochemical potential of the two metals promotes oxidation of the more reactive metal. This becomes the anode, which generates a flow of electrons and ions to the cathode. Galvanic corrosion is not frequent in dental implant applications because of the presence of only one component, the dental screw, and the insulating nature of the protective passive layer that forms on the surface. Anyway, in some cases, the surrounding tissue might behave as a medium for electrical flow between metallic implants and other types of alloys used in dentistry for amalgams or orthodontic devices [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15].
Fretting corrosion is due to the repeated micro-motion or friction of a metal component against another material that causes mechanical wear and breaks up the passivating layer on the contact surface of the metallic device. Fretting between dental implants and bone during implantation and due to cyclic loads imparted from chewing has been suggested as a cause of Ti corrosion and metal ion release. The release of metal debris and ions has been linked to inhibition of cell differentiation, phagocytosis of Ti particles by macrophages and other cells, and inflammation. Abnormal electrical signals may affect the stability of the adjacent tissue, and fretting corrosion may amplify other types of corrosion by rupturing the passivating film and exposing bare Ti [10,11,12,13,14,15,16,17,18,19,20,21,22,23].
Pitting corrosion (i.e. the result of the spontaneous breakdown of the passive film on a flat and evenly exposed area) is not likely to occur on Ti surfaces.
Instead, crevice corrosion has been observed on Ti and Ti alloys, and it consists of a localized corrosion due to a geometric confinement in the design of the device or from a previously corroded region on the surface [26,27,28,29,30,31].
Finally, EIC is the most common cause of corrosion in implants for bone applications, and because of its localized nature, may go unnoticed until failure of the implant. It consists of the brittle mechanical failure of metallic devices under stress levels significantly lower than their ultimate tensile strength. The magnitudes of the forces that can cause EIC vary over a wide range and include forces that, under non-corrosive conditions, would be considered negligible [10,11,12,13,14,15,16,17,18,19,20,21,22,23].
Because of these processes, a series of biochemical reactions might be triggered at the biointerface microenvironment.
As a consequence of the corrosion processes of dental implants and the Ti particle/ion release, signaling factors promoting the differentiation and recruitment of osteoclast cells responsible for peri-implant bone resorption determine an induction of inflammatory process in the peri-implant soft tissue cells and bone cells [10,11,12,13,14,15,16,17,18,19,20,21,22,23, 41,42,43,44,45,46,47,48,49,50,51,52].
Once metallic particles/ions are released, the peri-implant inflammatory process may be caused by the activation of the function of phagocytic cells such as neutrophils and macrophages, by the stimulation of communication pathways of osteoblastic cells, or by the promotion of microbial accumulation in the degraded rougher surface region. In particular, the phagocytosis of Ti ions may determine a higher expression level of pro-inflammatory cytokines (e.g., Interleukin 1β, Interleukin 6, and Tumor necrosis factorβ). Finally, the induction of receptor activator of nuclear factor kappa-Β ligand (RANKL) expression within osteogenic cells is promoted, thus indirectly promoting RANKL-induced osteoclast differentiation and consequent tissue inflammation and bone resorption [41,42,43,44,45,46,47,48,49,50,51,52].
The cytotoxic effect of Ti products on the inflammatory response of human cells has been demonstrated for particles and Ti ions.
In the literature, evidence for Ti degradation in diseased peri-implant tissues has been detected by inductively coupled plasma mass spectrometry in submucosal plaque, soft-tissue biopsies, and exfoliative cytologic samples in greater amount in diseased peri-implant mucosa than in healthy sites. Nevertheless, for both healthy and inflamed tissue biopsies, the Ti concentration found (7.3 to 38.9 μM) was within the levels needed to activate the IL-1β secretion from human macrophage in vitro, that is a phenomenon closely related to stimulating an in vivo proinflammatory reaction.
Therefore, there seems to be poor specificity between the biological impact of Ti concentration and the pathological process of peri-implant diseases [62,63,64,65,66,67,68,69,70,71,72,73,74].
To resume, it is likely a multidirectional pathway loop for the degradation of Ti surface in the oral environment: (1) first of all, wear, acidic substances, and metabolites released from oral bacteria promote the degradation of the peri-implant microenvironment, thus provoking the passive oxide layer breakdown and consequent pitting and galvanic attacks; (2) then, the corroded Ti surface with an increased roughness provides additional niches for bacterial recolonization; (3) the microbial accumulation promotes oxygen level deficiency that prevents the re-formation of the passive oxide layer; (4) finally, corrosion products induce microbial dysbiosis, the occurrence of inflammatory reaction, and the consequent generation of acid products (hydrogen peroxide and H+) that in the end also negatively affect the corrosion resistance of Ti [62,63,64,65,66,67,68,69,70,71,72,73,74].
An interdisciplinary engineering and biomedical approach is needed to improve the strategies to reduce the corrosion of dental implants and the consequent undesired effects.
Exploring Titanium Alloy Compositions for Dental Implants
Altering the composition of titanium alloys for dental implants to resist corrosion is the most straightforward option with the aim of creating a material that can achieve passivity, regulate the hydrogen evolution reaction, and reduce the anodic/cathodic activity directly. In fact, several elements are acknowledged to inhibit the degradation process by leading the growth of highly stable passive oxide films and microstructures [62,63,64,65,66,67,68,69,70,71,72,73,74, 76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96].
The main elements proposed for titanium alloys and their role in improving their electrochemical properties are resumed in Table 1. When an alloying element is added to Ti, the alloy may undergo phase transformation reactions, that may result in three microstructure phases (β, β + β, and β) with intermetallic variants. Anyway, there is no consensus regarding the best crystalline phase to prevent corrosion: β crystalline phase is expected to be more resistant to dissolution and stabler than the β-phase, but the single β-phase in Ti alloys has proven a better electrochemical behavior than β + β and β alloys.
Zirconium (Zr), tantalum (Ta), niobium (Nb), chromium (Cr), and molybdenum (Mo) are normally added to Ti to form a stable and resistant oxide film when in contact with the environment.
Ta incorporation forms a stable Ta2O5 passive film and a β phase in the Ti matrix, which reduces pitting initiations, the corrosion rate, and icorr while enhancing the corrosion potential (Ecorr) parameter of Ti–Ta alloys [76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96].
Instead, adding Mo to pure Ti improves the stability of the anodic oxides, increasing Rp and decreasing icorr and ipass as the content of Mo enhances in Ti–Mo alloys.
As for intermetallic compounds, they will dissolve preferentially on the surface by developing a galvanic cell with the matrix, which impairs the alloy’s electrochemical stability. Single-phase alloys exhibit better electrochemical properties. When more than one phase and/or diverse crystallographic orientations are present, it is necessary to achieve grain refinement and an even distribution of the elements.
In fact, a fine microstructure determines an “enveloping effect” by modifying the cathode/anode area ratio between the intermetallic and the matrix to minimize the galvanic effects and provide corrosion protection of the less noble phase, while homogeneous microstructures and greater elemental distributions may cause an increased corrosion resistance because of the improved stability and durability of the passivation films formed on the matrices.
Table 1 only resumes binary Ti alloys, but several other elements have been used to develop corrosion resistant ternary, high entropy alloys (HEAs), or compositionally complex alloys (CCAs). For this reason, researchers should first model combinations of elements by computational tools that consider first-principles calculations to predict material properties and electrochemical mechanisms before testing it by in vitro studies.
Surface Treatment Options for Dental Implants
Surface treatments are applied to the implant substrate to minimize the corrosion damages by avoiding the penetration of corrodents on metal underneath and preventing the electrochemical reactions [16,17,18,19,20,21,22,23, 45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96]. The outcomes of the most frequent technologies proposed to protect against corrosion of dental implants surfaces are resumed in Table 2.
The electrochemical stability of coatings is influenced by their elemental and crystalline composition. Moreover, the reinforcement of the oxide layer with homogeneously distributed functional and stable compounds and crystal phases by coating/film deposition techniques has demonstrated to enhance the corrosion performance of the implant material.
To this aim, a series of mechanism and ideal criteria that coatings and films need to meet for corrosion inhibition have been proposed: the formation of stabler oxide films (for example containing TiO2, ZrO2, Nb2O5, Ta2O5) contribute to prevent the internal dissolution of the coating due to corrosive attacks; dense, compact, and defect-free layers should fill the substrate porosities in order to prevent the corrosive fluid to reach the surface of the implant; thick layers may decrease the dissolution of the coatings in the immersion medium; an improved ability of substrates to form passive layers after coating/film deposition determines a better protective behavior; a strong bond strength between the coating and the substrate might prevent the coating cracking and peeling off in the body fluid, thus avoiding local corrosion [16,17,18,19,20,21,22,23, 45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96].
Conclusions
The development of improved strategies toward the reduction of corrosion and degradation of titanium alloys used for dental implants is crucial, also to prevent metal release in the tissue surrounding them to prolong their lifetime.
As chemical and physical properties are crucial for the electrochemical behavior of the implant material, the development of appropriate alloys or coatings/layers for corrosion inhibition is mandatory.
A thorough knowledge of corrosion mechanisms and the development of better methods to improve the corrosion resistance of dental implants may contribute to control peri-implant diseases and achieve safe and long-term dental implant rehabilitation treatment.
References
Howe M-S, Keys W, Richards D (2019) Long-term (10-year) dental implant survival: a systematic review and sensitivity meta-analysis. J Dent 84:9–21
Nagay BE, Cordeiro JM, Barao VAR (2022) Insight into corrosion of dental implants: from biochemical mechanisms to designing corrosion-resistant materials. Curr Oral Health Rep 9(2):7–21
Dini C, Costa RC, Sukotjo C, Takoudis CG, Mathew MT, Barão VAR (2020) Progression of bio-tribocorrosion in implant dentistry. Front Mech Eng 6:1
Revathi A, Borrás AD, Muñoz AI, Richard C, Manivasagam G (2017) Degradation mechanisms and future challenges of titanium and its alloys for dental implant applications in oral environment. Mater Sci Eng C 76:1354–1368
Souza JGS, Costa Oliveira BE, Bertolini M, Lima CV, Retamal-Valdes B, Faveri M et al (2020) Titanium particles and ions favor dysbiosis in oral biofilms. J Periodontal Res 55:258–266
Barão VAR, Mathew MT, Assunção WG, Yuan JC-C, Wimmer MA, Sukotjo C (2012) Stability of cp-Ti and Ti-6Al-4V alloy for dental implants as a function of saliva pH-an electrochemical study. Clin Oral Implants Res 23:1055–1062
Chaturvedi TP (2016) Corrosive behaviour of implant biomaterials in oral environment. Mater Technol 31:689–695
Mombelli A, Hashim D, Cionca N (2018) What is the impact of titanium particles and biocorrosion on implant survival and complications? A critical review. Clin Oral Implants Res 29:37–53
Lugowski SJ, Smith DC, McHugh AD, Van Loon JC (1991) Release of metal ions from dental implant materialsin vivo: determination of Al Co, Cr, Mo, Ni, V, and Ti in organ tissue. J Biomed Mater Res 25:1443–1458
Asri RIM, Harun WSW, Samykano M, Lah NAC, Ghani SAC, Tarlochan F et al (2017) Corrosion and surface modification on biocompatible metals: a review. Mater Sci Eng C 77:1261–1274
Pettersson M, Pettersson J, Johansson A, Molin TM (2019) Titanium release in peri-implantitis. J Oral Rehabil 46:179–188
Schwarz F, Derks J, Monje A, Wang H-L (2018) Peri-implantitis. J Clin Periodontol 45:S246–S266
Costa RC, Abdo VL, Mendes PHC, Mota-Veloso I, Bertolini M, Mathew MT et al (2021) Microbial corrosion in titanium-based dental implants: how tiny bacteria can create a big problem? J Bio- Tribo-Corros 7:136
Souza JCM, Apaza-Bedoya K, Benfatti CAM, Silva FS, Henriques B (2020) A comprehensive review on the corrosion pathways of titanium dental implants and their biological adverse effects. Metals (Basel) 10:1272
Virtanen S, Milošev I, Gomez-Barrena E, Trebše R, Salo J, Konttinen YT (2008) Special modes of corrosion under physiological and simulated physiological conditions. Acta Biomater 4:468–476
Fraser BM (2018) Does fluoride cause corrosion of titanium dental implants? Int J Oral Implantol Clin Res 9:7–10
Mabilleau G, Bourdon S, Joly-Guillou ML, Filmon R, Baslé MF, Chappard D (2006) Influence of fluoride, hydrogen peroxide and lactic acid on the corrosion resistance of commercially pure titanium. Acta Biomater 2:121–129
Wang ZB, Hu HX, Zheng YG, Ke W, Qiao YX (2016) Comparison of the corrosion behavior of pure titanium and its alloys in fluoride containing sulfuric acid. Corros Sci 103:50–65
Noguti J, de Oliveira F, Peres RC, Renno ACM, Ribeiro DA (2012) The role of fluoride on the process of titanium corrosion in oral cavity. Biometals 25:859–862
Chen W-Q, Zhang S-M, Qiu J (2020) Surface analysis and corrosion behavior of pure titanium under fluoride exposure. J Prosthet Dent 124:239.e1-239.e8
Boere G (1995) Influence of fluoride on titanium in an acidic environment measured by polarization resistance technique. J Appl Biomater 6:283–288
Eger M, Sterer N, Liron T, Kohavi D, Gabet Y (2017) Scaling of titanium implants entrains inflammation-induced osteolysis. Sci Rep 7:39612
Cordeiro JM, Pires JM, Souza JGS, Lima CV, Bertolini MM, Rangel EC et al (2021) Optimizing citric acid protocol to control implant-related infections: an in vitro and in situ study. J Periodontal Res 56:558–568
Noronha Oliveira M, Schunemann WVH, Mathew MT, Henriques B, Magini RS, Teughels W et al (2018) Can degradation products released from dental implants affect peri-implant tissues? J Periodontal Res 53:1–11
Sousa CA, Cordeiro JM, Silva AO, Barão VAR, Faverani LP, Assunção WG (2021) Dynamic action of mouthwashes affects the electrochemical behavior of Ti6Al4V alloy. J Bio Tribo Corros 7:158
Kunrath MF, Muradás TC, Penha N, Campos MM (2021) Innovative surfaces and alloys for dental implants: what about biointerface safety concerns? Dent Mater 37:1447–1462
Prestat M, Thierry D (2021) Corrosion of titanium under simulated inflammation conditions: clinical context and in vitro investigations. Acta Biomater 136:72–87
Suárez-López del Amo F, Garaicoa-Pazmiño C, Fretwurst T, Castilho RM, Squarize CH (2018) Dental implants-associated release of titanium particles: a systematic review. Clin Oral Implants Res 29:1085–1100
Wachi T, Shuto T, Shinohara Y, Matono Y, Makihira S (2015) Release of titanium ions from an implant surface and their effect on cytokine production related to alveolar bone resorption. Toxicology 327:1–9
Safioti LM, Kotsakis GA, Pozhitkov AE, Chung WO, Daubert DM (2017) Increased levels of dissolved titanium are associated with peri-implantitis–a cross-sectional study. J Periodontol 88:436–442
Pettersson M, Kelk P, Belibasakis GN, Bylund D, Molin Thorén M, Johansson A (2017) Titanium ions form particles that activate and execute interleukin-1β release from lipopolysaccharide-primed macrophages. J Periodontal Res 52:21–32
Olmedo DG, Nalli G, Verdú S, Paparella ML, Cabrini RL (2013) Exfoliative cytology and titanium dental implants: a pilot study. J Periodontol 84:78–83
Zhang M, Hector LG, Guo Y, Liu M, Qi L (2019) First-principles search for alloying elements that increase corrosion resistance of Mg with second-phase particles of transition metal impurities. Comput Mater Sci 165:154–166
Henderson JD, Ebrahimi N, Dehnavi V, Guo M, Shoesmith DW, Noël JJ (2018) The role of internal cathodic support during the crevice corrosion of Ni–Cr–Mo alloys. Electrochim Acta 283:1600–1608
Cordeiro JM, Beline T, Ribeiro ALR, Rangel EC, da Cruz NC, Landers R et al (2017) Development of binary and ternary titanium alloys for dental implants. Dent Mater 33:1244–1257
Cordeiro JM, Faverani LP, Grandini CR, Rangel EC, da Cruz NC, Nociti Junior FH et al (2018) Characterization of chemically treated Ti-Zr system alloys for dental implant application. Mater Sci Eng C 92:849–861
Zhao D, Han C, Li Y, Li J, Zhou K, Wei Q et al (2019) Improvement on mechanical properties and corrosion resistance of titanium tantalum alloys in-situ fabricated via selective laser melting. J Alloys Compd 804:288–298
Han M-K, Kim J-Y, Hwang M-J, Song H-J, Park Y-J (2015) Effect of Nb on the microstructure, mechanical properties, corrosion behavior, and cytotoxicity of Ti-Nb alloys. Materials (Basel) 8:5986–6003
Zhang E, Ren J, Li S, Yang L, Qin G (2016) Optimization of mechanical properties, biocorrosion properties and antibacterial properties of as-cast Ti–Cu alloys. Biomed Mater 11:065001
Takada Y, Nakajima H, Okuno O, Okabe T (2001) Microstructure and corrosion behavior of binary titanium alloys with betastabilizing elements. Dent Mater J 20:34–52
Chen M, Zhang E, Zhang L (2016) Microstructure, mechanical properties, bio-corrosion properties and antibacterial properties of Ti–Ag sintered alloys. Mater Sci Eng C 62:350–360
Romero-Resendiz L, Gómez-Sáez P, Vicente-Escuder A, Amigó-Borrás V (2021) Development of Ti–In alloys by powder metallurgy for application as dental biomaterial. J Mater Res Technol 11:1719–1729
Song H-J, Lee H, Lee J-Y, Moon W-J, Lee W-Y, Park Y-J (2020) Characteristics and oxidation mechanism of thermal oxide on Ti-xCr and Ti-xV (x = 5, 10, 15) alloys. J Alloys Compd 815:152390
Takemoto S, Hattori M, Yoshinari M, Kawada E, Asami K, Oda Y (2004) Corrosion behavior and surface characterization of Ti-20Cr alloy in a solution containing fluoride. Dent Mater J 23:379–386
Kim J-W, Hwang M-J, Han M-K, Kim Y-G, Song H-J, Park Y-J (2016) Effect of manganese on the microstructure, mechanical properties and corrosion behavior of titanium alloys. Mater Chem Phys 180:341–348
Qiu KJ, Liu Y, Zhou FY, Wang BL, Li L, Zheng YF et al (2015) Microstructure, mechanical properties, castability and in vitro biocompatibility of Ti–Bi alloys developed for dental applications. Acta Biomater 15:254–265
Oliveira NTC, Guastaldi AC (2008) Electrochemical behavior of Ti–Mo alloys applied as biomaterial. Corros Sci 50:938–945
Bolat G, Mareci D, Chelariu R, Izquierdo J, González S, Souto RM (2013) Investigation of the electrochemical behaviour of TiMo alloys in simulated physiological solutions. Electrochim Acta 113:470–480
Niu J, Guo Y, Li K, Liu W, Dan Z, Sun Z et al (2021) Improved mechanical, bio-corrosion properties and in vitro cell responses of Ti-Fe alloys as candidate dental implants. Mater Sci Eng C 122:111917
Cordeiro JM, Barão VAR (2017) Is there scientific evidence favoring the substitution of commercially pure titanium with titanium alloys for the manufacture of dental implants? Mater Sci Eng C 71:1201–1215
Liu X, Chen S, Tsoi JKH, Matinlinna JP (2017) Binary titanium alloys as dental implant materials-a review. Regen Biomater 4:315–323
Chen J-R, Tsai W-T (2011) In situ corrosion monitoring of Ti–6Al–4V alloy in H2SO4/HCl mixed solution using electrochemical AFM. Electrochim Acta 56:1746–1751
Dai N, Zhang L-C, Zhang J, Chen Q, Wu M (2016) Corrosion behavior of selective laser melted Ti-6Al-4 V alloy in NaCl solution. Corros Sci 102:484–489
Cordeiro JM, Nagay BE, Ribeiro ALR, da Cruz NC, Rangel EC, Fais LMG et al (2019) Functionalization of an experimental Ti–Nb–Zr–Ta alloy with a biomimetic coating produced by plasma electrolytic oxidation. J Alloys Compd 770:1038–1048
Atapour M, Pilchak AL, Frankel GS, Williams JC (2011) Corrosion behavior of β titanium alloys for biomedical applications. Mater Sci Eng C 31:885–891
Osório WR, Cremasco A, Andrade PN, Garcia A, Caram R (2010) Electrochemical behavior of centrifuged cast and heat treated Ti–Cu alloys for medical applications. Electrochim Acta 55:759–770
Sander G, Tan J, Balan P, Gharbi O, Feenstra DR, Singer L et al (2018) Corrosion of additively manufactured alloys: a review. Corrosion 74:1318–1350
Wang JC, Liu YJ, Qin P, Liang SX, Sercombe TB, Zhang LC (2019) Selective laser melting of Ti–35Nb composite from elemental powder mixture: microstructure, mechanical behavior and corrosion behavior. Mater Sci Eng A 760:214–224
Marattukalam JJ, Singh AK, Datta S, Das M, Balla VK, Bontha S et al (2015) Microstructure and corrosion behavior of laser processed NiTi alloy. Mater Sci Eng C Mater Biol Appl 57:309–313
Wu S, Wang S, Wang G, Yu X, Liu W, Chang Z et al (2019) Microstructure, mechanical and corrosion properties of magnesium alloy bone plate treated by high-energy shot peening. Trans Nonferrous Met Soc China 29:1641–1652
Salahshoor M, Li C, Liu ZY, Fang XY, Guo YB (2018) Surface integrity and corrosion performance of biomedical magnesium-calcium alloy processed by hybrid dry cutting-finish burnishing. J Mech Behav Biomed Mater 78:246–253
Vasilescu C, Drob SI, Calderon Moreno JM, Osiceanu P, Popa M, Vasilescu E et al (2015) Long-term corrosion resistance of new Ti–Ta–Zr alloy in simulated physiological fluids by electrochemical and surface analysis methods. Corros Sci 93:310–323
Panigrahi P, Liao Y, Mathew MT, Fischer A, Wimmer MA, Janbozorgi M, Karimi Taheri K, Karimi TA (2019) Microstructural evolution, mechanical properties, and corrosion resistance of a heat-treated Mg alloy for the bio-medical application. J Magnes Alloy 7:80–89
Ma H, Chen X-Q, Li R, Wang S, Dong J, Ke W (2017) First-principles modeling of anisotropic anodic dissolution of metals and alloys in corrosive environments. Acta Mater 130:137–146
Gutiérrez Moreno JJ, Bönisch M, Panagiotopoulos NT, Calin M, Papageorgiou DG, Gebert A et al (2017) Ab-initio and experimental study of phase stability of Ti–Nb alloys. J Alloys Compd 696:481–489
Feng Z, Dong H, Kang J, Li J, Zhang X, Ma M et al (2019) Study on the correlation between microstructures and corrosion properties of novel ZrTiAlV alloys. Mater Sci Eng C 101:92–102
Grimm M, Lohmüller A, Singer RF, Virtanen S (2019) Influence of the microstructure on the corrosion behaviour of cast Mg–Al alloys. Corros Sci 155:195–208
Guo S, Lu Y, Wu S, Liu L, He M, Zhao C et al (2017) Preliminary study on the corrosion resistance, antibacterial activity and cytotoxicity of selective-laser-melted Ti6Al4V-xCu alloys. Mater Sci Eng C Mater Biol Appl 72:631–640
Ogawa ES, Matos AO, Beline T, Marques ISV, Sukotjo C, Mathew MT et al (2016) Surface-treated commercially pure titanium for biomedical applications: electrochemical, structural, mechanical and chemical characterizations. Mater Sci Eng C 65:251–261
Barranco V, Escudero ML, García-Alonso MC (2007) 3D, chemical and electrochemical characterization of blasted TI6Al4V surfaces: its influence on the corrosion behaviour. Electrochim Acta 52:4374–4384
Cordeiro JM, Pantaroto HN, Paschoaleto EM, Rangel EC, da Cruz NC, Sukotjo C et al (2018) Synthesis of biofunctional coating for a TiZr alloy: surface, electrochemical, and biological characterizations. Appl Surf Sci 452:268–278
Mohammad NF, Ahmad RN, Mohd Rosli NL, Abdul Manan MS, Marzuki M, Wahi A (2021) Sol gel deposited hydroxyapatite-based coating technique on porous titanium niobium for biomedical applications: a mini review. Mater Today Proc 41:127–135
Ansari Z, Kalantar M, Kharaziha M, Ambrosio L, Raucci MG (2020) Polycaprolactone/fluoride substituted-hydroxyapatite (PCL/FHA) nanocomposite coatings prepared by in-situ sol-gel process for dental implant applications. Prog Org Coatings 147:105873
El Hadad AA, García-Galván FR, Mezour MA, Hickman GJ, Soliman IE, Jiménez-Morales A et al (2020) Organic-inorganic hybrid coatings containing phosphorus precursors prepared by sol–gel on Ti6Al4V alloy: electrochemical and in-vitro biocompatibility evaluation. Prog Org Coatings 148:105834
Chen S, Zhang C, Xiao D, Shi F, Liu K, Wan Y et al (2021) Magnesium- incorporated sol-gel Ta2O5 coating on Ti6Al4V and in vitro biocompatibility. Surf Coatings Technol 426:127769
da Marques ISV, Barão VAR, da Cruz NC, Yuan JC-C, Mesquita MF, Ricomini-Filho AP et al (2015) Electrochemical behavior of bioactive coatings on cp-Ti surface for dental application. Corros Sci 100:133–146
Beline T, da Marques ISV, Matos AO, Ogawa ES, Ricomini- Filho AP, Rangel EC et al (2016) Production of a biofunctional titanium surface using plasma electrolytic oxidation and glowdischarge plasma for biomedical applications. Biointerphases 11:011013
Kaluđerović MR, Schreckenbach JP, Graf H-L (2016) Titanium dental implant surfaces obtained by anodic spark depositionfrom the past to the future. Mater Sci Eng C Mater Biol Appl 69:1429–1441
Höhlinger M, Heise S, Wagener V, Boccaccini AR, Virtanen S (2017) Developing surface pre-treatments for electrophoretic deposition of biofunctional chitosan-bioactive glass coatings on a WE43 magnesium alloy. Appl Surf Sci 405:441–448
Tabesh E, Salimijazi HR, Kharaziha M, Mahmoudi M, Hejazi M (2019) Development of an in-situ chitosan-copper nanoparticle coating by electrophoretic deposition. Surf Coat Technol 364:239–247
Beline T, de Almeida AB, Azevedo Neto NF, Matos AO, Ricomini-Filho AP, Sukotjo C et al (2020) β-Ta2O5 thin film for implant surface modification triggers superior anti-corrosion performance and cytocompatibility of titanium. Appl Surf Sci 520:146326
Pantaroto HN, Cordeiro JM, Pereira LT, de Almeida AB, Nociti Junior FH, Rangel EC et al (2021) Sputtered crystalline TiO2 film drives improved surface properties of titanium-based biomedical implants. Mater Sci Eng C 119:111638
Gaur S, Agnihotri R, Albin S (2022) Bio-tribocorrosion of titanium dental implants and its toxicological implications: a scoping review. Sci World J 21(2022):4498613
Amine M, Merdma W, El Boussiri K (2022) Electrogalvanism in oral implantology: a systematic review. Int J Dent 5(2022):4575416
Bao Y, Wang W, Cui W, Qin G (2021) Corrosion resistance and antibacterial activity of Ti–N–O coatings deposited on dental titanium alloy. Surf Coat Technol 419:127296
Safavi MS, Surmeneva MA, Surmenev RA, Khalil-Allafi J (2021) RF magnetron sputter deposited hydroxyapatite-based composite & multilayer coatings: a systematic review from mechanical, corrosion, and biological points of view. Ceram Int 47:3031–3053
Souza JGS, Bertolini M, Costa RC, Cordeiro JM, Nagay BE, de Almeida AB et al (2020) Targeting pathogenic biofilms: newly developed superhydrophobic coating favors a host-compatible microbial profile on the titanium surface. ACS Appl Mater Interfaces 12:10118–10129
Tyczkowski J, Kierzkowska-Pawlak H, Kapica R, Balcerzak J, Sielski J (2019) Cold plasma−a promising tool for the production of thin-film nanocatalysts. Catal Today 337:44–54
Ting W-T, Chen K-S, Wang M-J (2021) Dense and anti-corrosion thin films prepared by plasma polymerization of hexamethyldisilazane for applications in metallic implants. Surf Coat Technol 410:126932
Přikrylová J, Procházková J, Podzimek Š (2019) Side effects of dental metal implants: impact on human health (metal as a risk factor of implantologic treatment). Biomed Res Int 10(2019):2519205
Gittens RA, Olivares-Navarrete R, Tannenbaum R, Boyan BD, Schwartz Z (2011) Electrical implications of corrosion for osseointegration of titanium implants. J Dent Res 90(12):1389–1397
Singh S, Pandey KK, Islam A, Keshri AK (2020) Corrosion behaviour of plasma sprayed graphene nanoplatelets reinforced hydroxyapatite composite coatings in simulated body fluid. Ceram Int 46:13539–13548
Bansal P, Singh G, Sidhu HS (2020) Investigation of corrosion behavior and surface properties of plasma sprayed HA/Sr reinforced coatings on CoCr alloys. Mater Chem Phys 253:123330
Ling L, Cai S, Li Q, Sun J, Bao X, Xu G (2021) Recent advances in hydrothermal modification of calcium phosphorus coating on magnesium alloy. J Magnes Alloys 10(1):62–80
Xi Z, Wu Y, Xiang S, Sun C, Wang Y, Yu H et al (2020) Corrosion resistance and biocompatibility assessment of a biodegradable hydrothermal-coated Mg–Zn–Ca alloy: an in vitro and in vivo study. ACS Omega 5:4548–4557
Wu H, Xi K, Xiao S, Qasim AM, Fu RKY, Shi K et al (2020) Formation of self-layered hydrothermal coating on magnesium aided by titanium ion implantation: synergistic control of corrosion resistance and cytocompatibility. Surf Coat Technol 401:126251
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Boffano, P., Brucoli, M. & Rocchetti, V. Corrosion Features of Titanium Alloys in Dental Implants: A Systematic Review. J. Maxillofac. Oral Surg. (2024). https://doi.org/10.1007/s12663-024-02169-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12663-024-02169-6