Abstract
Intravenous daratumumab (DARZALEX®) is a human CD38 monoclonal antibody approved as combination therapy (with bortezomib, melphalan and prednisone) for patients with newly diagnosed multiple myeloma (NDMM) who are ineligible for autologous stem cell transplantation (ASCT). The approval was based on results of the phase 3 ALCYONE trial in which the addition of daratumumab to bortezomib, melphalan and prednisone significantly prolonged median progression-free survival (PFS) relative to bortezomib, melphalan and prednisone alone (primary endpoint). Daratumumab addition was also associated with deeper and durable responses relative to the comparator. The addition of daratumumab did not increase overall toxicity, with the exception of infusion-related reactions and increased rates of infections. The incidences of the most common grade 3 or 4 adverse events in the daratumumab group (neutropenia, thrombocytopenia and anaemia) were largely similar to those in the comparator group. Thus, daratumumab in combination with bortezomib, melphalan and prednisone represents a promising treatment option for patients with NDMM who are ineligible for ASCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
First-in-class CD38 monoclonal antibody |
Prolongs PFS, and induces deeper and durable responses, when combined with bortezomib, melphalan and prednisone |
Acceptable tolerability profile; does not increase overall toxicity of the combination, apart from infections and infusion-related reactions |
1 Introduction
Multiple myeloma (MM) is a malignant neoplasm of plasma cells [1]. Although MM remains incurable, survival rates are steadily increasing due to the availability of new classes of drugs, such as proteasome inhibitors (bortezomib, carfilzomib, ixazomib), immunomodulatory drugs (thalidomide, lenalidomide, pomalidomide), histone deacetylase inhibitors (panobinostat) and monoclonal antibodies (daratumumab, elotuzumab), which are used with corticosteroids and chemotherapy in doublet, triplet or quadruplet combinations [1,2,3].
ASCT is an important component of the treatment plan for NDMM [1, 3, 4] and is associated with high response rates and improved PFS and overall survival (OS) [1, 5, 6]. However, ASCT is reserved for fit patients, typically up to 65 (Europe) or 75 (USA) years of age or in good clinical condition; thus, elderly patients and those with comorbidities or poor performance status are ineligible for ASCT [4, 6]. Ironically, the risk of MM increases with age and the majority of those diagnosed are > 65 years old [7]. The majority of ASCT-ineligible patients also do not receive subsequent lines of therapy, with attrition rates ranging from 46 to 51% per line of therapy [8]. Therefore, an effective first-line treatment is required for these patients [4, 8]. One strategy to deepen responses and improve efficacy in ASCT-ineligible patients with NDMM is to add an immunotherapy (i.e. anti-myeloma antibodies) to the first-line treatment [4].
CD38 is a transmembrane glycoprotein expressed on the surface of haematopoietic cells and is overexpressed on MM cells [9, 10]. Acting as a receptor and as an ectoenzyme, CD38 has multiple functions, including receptor-mediated adhesion, signalling and modulation of cyclase and hydrolase activity [11]. Thus, monoclonal antibodies targeting CD38 are being developed for the treatment of MM [11].
Daratumumab (DARZALEX®) is a first-in-class human IgG1κ monoclonal antibody targeting CD38. Intravenous daratumumab, as monotherapy and combination therapy, has been previously approved in patients with relapsed and/or refractory MM [12]. Recently, daratumumab has also been approved in the EU [13] and USA [10] for use in combination with bortezomib, melphalan and prednisone for the treatment of patients with NDMM who are ineligible for ASCT. This article reviews the clinical efficacy, safety and tolerability of daratumumab in this population, with a brief overview of its pharmacological properties.
2 Pharmacological Properties of Daratumumab
2.1 Pharmacodynamics
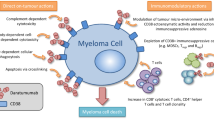
Daratumumab binds to CD38 with high affinity and inhibits the growth of CD38-expressing tumour cells through multiple mechanisms of actions (Fig. 1) [14, 15]. Daratumumab induces myeloma cell lysis by complement-dependent cytotoxicity (CDC), antibody-dependent cell-mediated cytotoxicity (ADCC) and antibody-dependent cellular phagocytosis [16, 17]. It also eliminates CD38-expressing immunosuppressive cells, such as myeloid-derived suppressor cells and regulatory T cells and B cells, resulting in clonal expansion of cytotoxic T cells [18]. In addition, daratumumab directly induces apoptosis via Fcγ receptor-mediated crosslinking [19]. Daratumumab may also modulate enzymatic activity, such as inhibiting the production of immunosuppressive adenosine and boosting intracellular nicotinamide adenine dinucleotide levels, resulting in cytotoxicity [14]. While the direct on-tumour actions of daratumumab may produce rapid anti-myeloma responses, its immunomodulatory actions may contribute to durable responses and improved survival seen with this drug [14, 18, 19].

adapted from McKeage and Lyseng-Williamson [15] with permission
Mechanism of action of daratumumab
In preclinical studies, daratumumab showed synergistic and additive anti-myeloma activity in combination with other drugs [11, 14]. Daratumumab may sensitize myeloma cells to other drugs by decreasing CD38 expression levels and/or by restoring exhausted T cell responses [14]. The addition of daratumumab to bortezomib and dexamethasone prolonged PFS and improved rates of response and minimal residual disease (MRD) negativity versus bortezomib and dexamethasone alone in previously treated patients with MM [20].
There is a marked heterogeneity of clinical response to daratumumab in patients with MM, which can be partly explained by the expression levels of CD38 and complement-inhibitory proteins on myeloma cells [21, 22]. A higher level of CD38 expression in patient-derived myeloma cells was associated with a greater degree of daratumumab-mediated ADCC and CDC [21]. Consistently, in daratumumab recipients, baseline CD38 expression levels were higher in those who achieved at least partial response than in those with less than partial response [22]. On the other hand, an increased expression of complement-inhibitory proteins such as CD55 and CD59 was associated with resistance to daratumumab therapy [22]. CD38 expression and daratumumab-mediated ADCC and CDC did not differ markedly between newly diagnosed and relapsed or refractory patients [21].
CD38 is also expressed in natural killer (NK) cells and daratumumab therapy is associated with a decrease in total and activated NK cells in peripheral whole blood and bone marrow; this reduction, however, did not affect the efficacy or safety of daratumumab [23]. Furthermore, baseline level of NK cells was not associated with a clinical response to daratumumab [13].
Daratumumab binds to CD38 on red blood cells (RBCs), which may result in a positive indirect antiglobulin test (indirect Coombs test) for up to 6 months after the last daratumumab infusion [10, 13]. Daratumumab bound to RBCs may also mask detection of antibodies to minor antigens in the patient’s serum [10]. Therefore, blood typing and screening should be performed prior to starting daratumumab therapy [10]. A number of strategies can be used to negate the daratumumab interference with blood compatibility testing [11, 13], including removal of CD38 by incubating with dithiothreitol [24]. Daratumumab does not interfere with ABO and Rh typing [10]. For emergency, non-cross-matched ABO/RhD-compatible RBCs can be transfused, according to local blood bank practices [25].
Daratumumab may be detected on serum protein electrophoresis and immunofixation assays used for monitoring endogenous monoclonal protein [10, 13]. This can result in false positive test results, affecting the assessment of complete response and disease progression in some patients with the IgG1κ myeloma protein [10, 13]. In patients with a persistent very good partial response, where daratumumab interference is suspected, a validated daratumumab-specific immunofixation electrophoresis reflex assay [26] may be considered for the assessment of a complete response [13].
2.2 Pharmacokinetics
Pharmacokinetics data for intravenous daratumumab over a dose range of 1–24 mg/kg (monotherapy) or 1–16 mg/kg (combination therapy) are available from patients with relapsed or refractory MM [10, 13, 27,28,29]. Daratumumab concentration-time profiles were largely similar following the monotherapy and combination therapies [13].
Daratumumab exhibited complex, time- and concentration-dependent nonlinear pharmacokinetics, consistent with target-mediated drug disposition [27, 28]. Following weekly administrations, peak daratumumab serum concentrations increased in approximately dose-proportional manner after the first dose and in a greater than dose-proportional manner after multiple doses [13, 27]. The area under the concentration-time curve of daratumumab increased in a greater than dose-proportional manner after the first and subsequent doses [13, 27]. Daratumumab is primarily distributed in the vascular system, with limited extravascular tissue distribution [27]. Following a 16 mg/kg dose as combination therapy, the mean central volume of distribution of daratumumab was 4.4 L [10]. Daratumumab clearance decreased and its mean terminal half-life (t1/2) increased with increasing doses and with multiple doses [13, 27]. With 16 mg/kg monotherapy, the estimated mean linear clearance of daratumumab was 171.4 mL/day [10]. The estimated mean t1/2 based on linear clearance was 22–23 days for combination therapy [10].
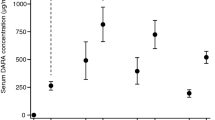
Due to its target-mediated disposition, a tapered administration schedule was established for daratumumab: 16 mg/kg weekly for 8 weeks, every 2 weeks for 16 weeks and every 4 weeks thereafter [27, 28]. This schedule rapidly saturated target-mediated clearance during weekly administration and the saturation was maintained during the every 2- and 4-week administration periods [27]. Following monotherapy, daratumumab steady-state concentrations were attained after ≈ 5 months of 4-weekly administration (by the 21st infusion) [13]. Daratumumab exposure strongly correlated with efficacy but not with safety, although the overall incidence of infection increased slightly with increased exposure [28]. The 16 mg/kg schedule provided an optimal benefit-risk profile; ≈ 80% of patients treated with this schedule could achieve the effective target serum trough concentration (274 µg/mL), with acceptable safety outcomes [28].
Daratumumab exposure (predicted mean maximal trough concentration) was not significantly affected by age, sex, race, renal or hepatic function, number of prior lines of therapy, refractory status or ECOG performance status at baseline [29]. The linear clearance of daratumumab was 110% (p < 0.0001) higher in patients with IgG MM than in those with non-IgG MM, resulting in a ≈ 70% greater daratumumab exposure in the latter. Baseline albumin levels also had a significant (p < 0.0001) effect on daratumumab linear clearance, resulting in a 26% lower daratumumab exposure in patients with an abnormal level (< 35 g/L) than in those with normal levels (≥ 35 g/L). The central volume of distribution and clearance of daratumumab increased with increasing bodyweight, supporting the bodyweight-based dosage schedule. However, daratumumab exposure-response analyses indicated that none of the patient or disease characteristics had a significant effect on the overall response rate [29]. Daratumumab pharmacokinetics were generally similar when administered as monotherapy and with various combination therapies, including bortezomib, melphalan and prednisone [30]. When coadministered, daratumumab did not affect the pharmacokinetics of bortezomib [10, 13].
3 Therapeutic Efficacy of Daratumumab
The efficacy of daratumumab in combination with bortezomib, melphalan and prednisone in patients with documented NDMM [International Myeloma Working Group (IMWG) updated criteria] who were ineligible for ASCT because of comorbid conditions or old age (≥ 65 years) was demonstrated in the randomized, open-label, multicentre phase 3 ALCYONE trial [31]. Combination bortezomib, melphalan and prednisone (a standard-of-care in this setting [32]) was used as the comparator in ALYCONE, although a reduced bortezomib dosage was used to reduce neuropathy.
In ALCYONE, eligible patients had a haemoglobin level of ≥ 7.5 g/dL, an absolute neutrophil count of ≥ 1.0 × 109/L, a platelet count of > 50 × 109/L (> 70 × 109/L if < 50% of bone marrow nucleated cells were plasma cells), AST and ALT levels of ≤ 2.5 × upper limit of the normal (ULN), a total bilirubin level of ≤ 1.5 × ULN, a creatinine clearance of ≥ 40 mL/min, a corrected serum calcium level of ≤ 3.5 mmol/L and an ECOG performance status of 0–2. Patients with other typical plasma cell disorders were excluded, as were those with cancer within 3 years before randomization (with a few exceptions), peripheral neuropathy or grade ≥ 2 neuropathic pain [31].
Patients were stratified according to the International Staging System (ISS) disease stage (I, II or III), geographic region (Europe vs. other) and age (< 75 vs. ≥ 75 years) [31]. Patients received up to nine 42-day cycles of subcutaneous bortezomib (1.3 mg/m2 twice weekly on weeks 1, 2, 4, and 5 of cycle 1 and once weekly on weeks 1, 2, 4 and 5 of cycles 2 through 9), oral melphalan (9 mg/m2 once daily on days 1 through 4 of each cycle) and oral prednisone (60 mg/m2 once daily on days 1 through 4 of each cycle), with or without intravenous daratumumab (16 mg/kg once weekly in cycle 1 and every 3 weeks in cycles 2 through 9). After nine cycles, all patients in the comparator group discontinued treatment and those in the daratumumab group received daratumumab monotherapy (16 mg/kg every 4 weeks) until disease progression or unacceptable toxicity. The median treatment duration of treatment was 14.7 and 12.0 months in the daratumumab and comparator groups. Pre-infusion medications (paracetamol, antihistamines, dexamethasone and leukotriene inhibitors) were administered in daratumumab recipients to mitigate infusion-related reactions. Post-infusion respiratory medications were permitted for patients with a higher risk of respiratory complications. The primary endpoint was median PFS in the intent-to-treat (ITT) population in a planned interim analysis, when 231 PFS events had occurred. If the primary endpoint was significant, secondary endpoints were tested in a hierarchical order [31].
ALYCONE enrolled 706 patients and the baseline demographic and clinical characteristics in the ITT population were generally well balanced between the treatment groups [31]. Across the groups, the median patient age was 71 years (≈ 30% were aged ≥ 75 years) and the median time since MM diagnosis was 0.8 months. The majority of patients in the daratumumab and comparator groups had an ECOG performance status of 1 (52.0 vs. 48.6%) or 2 (25.7 vs. 23.6%), ISS disease stage II (39.7 vs. 44.9%) or III (40.6 vs. 36.2%) and a standard cytogenetic risk profile (83.1 vs. 85.1%) [31].
At the time of planned interim analysis (median follow-up 16.5 months; data cutoff date 12 June 2017), the addition of daratumumab to bortezomib, melphalan and prednisone significantly prolonged median PFS relative to bortezomib, melphalan and prednisone alone, reducing the risk of progression or death by 50% (Table 1) [31]. The PFS benefit with daratumumab was seen across a number of prespecified subgroups of the ITT population, such as sex, age, race, geographic region, creatinine clearance, hepatic function, ISS disease stage, IgG MM, cytogenetic profile and ECOG performance status [hazard ratios (HR) ranged from 0.22 to 0.81]. PFS benefit did not reach statistical significance in subgroups of patients with ISS stage I, non-IgG MM and those with a high-risk cytogenetic profile, although the sample sizes of these subgroups were small. Furthermore, a post hoc analysis of PFS by revised ISS criteria found that HR for the stage III disease subgroup (also based on a small sample size) did not reach statistical significance [31].
In addition to prolonged median PFS, 18-month PFS rate was significantly higher in the daratumumab than in the comparator group (Table 1) [31]. The median overall survival was not reached in either treatment group [31].
The addition of daratumumab to bortezomib, melphalan and prednisone was also associated with deep and durable responses [31]. The rates of overall response, complete response or better, very good partial response or better and negative status for MRD (key secondary endpoints) were significantly higher in the daratumumab than in the comparator group (Table 1). Of note, the rate of stringent complete response (i.e. complete response plus a normal free light-chain ratio and absence of clonal plasma cells) was 2.6 times as high in the daratumumab as in the comparator group (18.0 vs. 7.0%). The median time to response and best response was 0.79 and 4.9 months in the daratumumab group, compared with 0.82 and 4.1 months in the comparator group. While the median duration of response was not reached in the daratumumab group, it was 21.3 months (95% CI 18.4 to not estimable) in the comparator group, with 77.2 and 60.4% of patients in the respective groups continuing to have a response after 18 months [31].
After an additional 1 year of follow-up (updated analysis), significant PFS and response benefits were maintained in the daratumumab group relative to the comparator group (Table 1) [33]. Of note, the addition of daratumumab was associated with maintenance of PFS benefit during subsequent line of therapy (PFS2 in Table 1) [33].
In ALCYONE, the addition of daratumumab to bortezomib, melphalan and prednisone was associated with improvements in health-related quality of life, as assessed by the European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire-Core 30 Global health status and the EuroQol Questionnaire 5-dimension 5-level visual analogue scale [34].
4 Tolerability and Safety of Daratumumab
Daratumumab added to bortezomib, melphalan and prednisone had an acceptable tolerability profile in ASCT-ineligible patients with NDMM in ALCYONE [31]. With the exception of infections and infusion-related reactions (IRRs), the addition of daratumumab did not increase the overall toxicity [31].
In both daratumumab and comparator groups, haematological adverse events (AEs), such as neutropenia, thrombocytopenia and anaemia occurred frequently, with the majority of neutropenia and thrombocytopenia (and approximately half of anaemia) events being grade 3 or 4 severity in both groups (Fig. 2) [31]. The addition of daratumumab did not increase the incidence of any grade and grade 3 or 4 haematological AEs (Fig. 2) [31].
The most common adverse events of any grade (incidence ≥ 20% in either group) and grade 3 or 4 in ALCYONE [31]. B bortezomib, D daratumumab, M melphalan, P prednisone, PSN peripheral sensory neuropathy
The most common non-haematological AEs in both treatment groups included peripheral sensory neuropathy, diarrhoea, pyrexia and nausea, with individual grade 3 or 4 of these events occurring in < 5% of patients in both groups (Fig. 2) [31]. Of note, grade 3 or 4 peripheral sensory neuropathy occurred in 1.4 and 4% of patients in the daratumumab and comparator groups [31].
The addition of daratumumab was associated with an increase in infections (Fig. 2), the most common of which were upper respiratory tract infection [26.3 vs. 13.8% in the daratumumab and comparator groups (any grade); 2.0 vs. 1.4% (grade 3 or 4)] and pneumonia [15.3 vs. 4.8% (any grade); 11.3 vs. 4.0% (grade 3 or 4)] [31]. Most infections, including pneumonia, resolved in both groups (87.9% vs. 86.5% of patients). Moreover, the incidences of infections leading to treatment discontinuation (0.9 vs. 1.4%) or death (1.4 vs. 1.1%) were generally similar between the daratumumab and comparator groups. Infections that lead to death were pneumonia (2 patients), peritonitis (1), septic shock (1) and upper respiratory tract infection (1) in the daratumumab group, and septic shock (1), candida-related sepsis (1), bacterial pneumonia (1) and sepsis (1) in the comparator group [31].
Any grade IRRs occurred in 27.7% of daratumumab recipients, the majority of which were of grade 1 or 2 severity and occurred during the first infusion [31]. The most common IRRs (incidence ≥ 2%, any grade) included dyspnoea, chills, hypertension, pyrexia, bronchospasm, cough, hypotension, nausea and decreased oxygen saturation. Grade 3 or 4 IRRs occurred in 4.9% of daratumumab recipients, with dyspnoea (2.3%) and hypertension (1.7%) being the most common [31]
The incidence of secondary primary cancer (a prespecified AE) was 2.3 and 2.5% in the daratumumab and comparator groups, with two patients in each group experiencing tumour lysis syndrome [31]. Serious AEs occurred in 41.6 and 32.5% of patients the respective groups, most common of which was pneumonia (10.1 and 3.1%). The incidence of treatment discontinuation due to AEs was 4.9 and 9.0% in the daratumumab and comparator groups. The incidence of death from AEs within 30 days after the last dose of study medications was 4.0 and 4.5% in the respective groups [31].
Daratumumab has low potential for immunogenicity [10]. In clinical trials, none of the 111 patients receiving daratumumab as monotherapy and 2 of the 411 patients receiving it as combination therapy developed anti-daratumumab antibodies. One daratumumab combination therapy recipient developed transient neutralizing antibodies against daratumumab. These incidences might not have been reliably determined because the assay used is known to have limitations in detecting anti-daratumumab antibodies in the presence of high concentrations of daratumumab [10].
5 Dosage and Administration of Daratumumab
In the EU [13] and USA [10], the recommended dosage of daratumumab (in combination with bortezomib, melphalan and prednisone) for ASCT-ineligible patients with NDMM is 16 mg/kg, administered as an intravenous infusion weekly from weeks 1 to 6 (six doses), every 3 weeks from weeks 7 to 54 (16 doses) and every 4 weeks from week 55 until disease progression. To facilitate administration, the first daratumumab dose may be split into two 8 mg/kg doses over two consecutive days (i.e. day 1 and 2). The efficacy and safety of daratumumab has not been established in paediatric patients (aged < 18 years) [10, 13]. Consult local prescribing information for detailed information regarding preparation and administration procedures, dosing schedule, pre- and post-infusion medications, management of infusion reactions, warnings and precautions, and use in special populations.
6 Place of Daratumumab in the Management of NDMM in the Non-Transplant Setting
Treatment should be started in all patients with symptomatic NDMM as defined by the updated IMWG criteria [1, 3]. The ESMO clinical practice guidelines (published prior to daratumumab approval) recommend bortezomib (subcutaneous) plus melphalan plus prednisone or lenalidomide plus low-dose dexamethasone for the treatment of NDMM in transplant-ineligible elderly patients (level I evidence, grade A recommendation) [3]. According to the NCCN, the preferred regimens for this population are bortezomib plus lenalidomide plus dexamethasone, lenalidomide plus low-dose dexamethasone or daratumumab plus bortezomib plus melphalan plus prednisone (all category 1); bortezomib plus cyclophosphamide plus dexamethasone is the preferred initial treatment for patients with acute renal insufficiency [1]. Other NCCN recommended regimens for NDMM in transplant-ineligible patients are carfilzomib or ixazomib with lenalidomide plus dexamethasone or carfilzomib plus cyclophosphamide plus dexamethasone [1]. In the USA, while triplet regimens are recommended as the standard therapy, a doublet regimen containing bortezomib and dexamethasone can be used in elderly or frail patients [1].
Approval of daratumumab as combination therapy in ASCT-ineligible patients with NDMM was based on ALCYONE trial data (Sect. 3). In this trial, the addition of daratumumab to bortezomib, melphalan and prednisone significantly prolonged median PFS in ASCT-ineligible patients with NDMM, reducing the risk of progression or death by 50% (Sect. 3). Results of an updated analysis were generally consistent with that of the primary analysis (Table 1). In ALCYONE, patients in the comparator arm received only nine cycles of treatment whereas those in the daratumumab arm continued to receive daratumumab monotherapy beyond nine cycles (Sect. 3), with no re-randomization performed at the start of daratumumab monotherapy. Thus, beyond nine cycles, the effect of daratumumab monotherapy was evaluated compared with no treatment (i.e. observation only).
The goal of upfront treatment in the non-transplant setting is to achieve the deepest response possible, as the depth of response correlates with long-term outcomes [4]. Stringent complete response is generally considered as the deepest response measured by conventional criteria, with MRD negativity regarded as an even deeper response [35]. Stringent complete response and MRD negativity (using a threshold of 1 tumour cell per 105 white cells) rates were 2.6 and 3.6 times higher in patients receiving the daratumumab-containing regimen versus the comparator group (Sect. 3).
A Bayesian network meta-analysis of 20 randomized clinical trials has predicted favourable efficacy outcomes for daratumumab added to bortezomib, melphalan and prednisone in ASCT-ineligible patients with NDMM [36]. This quadruplet regimen ranked first among 19 and 20 treatment regimens with respect to PFS and overall response rate, respectively. It was significantly (based on 95% CI) more effective than 10 of 19 regimens for PFS and 12 of 20 regimens for overall response rate [36].
Combining daratumumab with bortezomib, melphalan and prednisone did not increase haematological or non-haematological toxicities, although infections and IRRs were common with daratumumab addition (Sect. 4). Most infections resolved and did not lead to treatment discontinuation or death. The majority of IRRs were of mild or moderate severity and occurred during the first infusion of daratumumab. The incidence of grade 3 or 4 peripheral sensory neuropathy (an AE associated with bortezomib) was 1.4 and 4.0% in the daratumumab and comparator groups.
Some additional data for daratumumab as combination therapy in transplant-ineligible patients with NDMM are awaited with interest. Although the clinical use of daratumumab in combination with bortezomib, melphalan and prednisone was demonstrated in ALYCYONE, final OS results are yet to be determined. Also of interest are clinical trials to evaluate the addition of daratumumab to other standard-of-care combinations in this indication, with promising preliminary findings recently reported (abstract [37]). Furthermore, adding a targeted therapy such as daratumumab to a doublet or triplet therapy can substantially increase the treatment cost [38]. Thus, robust cost effectiveness analyses are required.
In conclusion, the addition of daratumumab to bortezomib, melphalan and prednisone (a standard-of-care) was more effective than bortezomib, melphalan and prednisone alone in ASCT-ineligible patients with NDMM. The quadruplet regimen had an acceptable tolerability profile in this population. Although additional data are warranted to definitively establish the place of daratumumab in the management of NDMM in transplant ineligible patients, given the need for balancing the efficacy, tolerability and treatment burden in this frail population, daratumumab in combination with bortezomib, melphalan and prednisone represents a promising treatment option for these patients.
Data Selection Daratumumab: 227 records identified
Duplicates removed | 24 |
Excluded during initial screening (e.g. press releases; news reports; not relevant drug/indication; preclinical study; reviews; case reports; not randomized trial) | 139 |
Excluded during writing (e.g. reviews; duplicate data; small patient number; nonrandomized/phase I/II trials) | 26 |
Cited efficacy/tolerability articles | 3 |
Cited articles not efficacy/tolerability | 35 |
Search Strategy: EMBASE, MEDLINE and PubMed from 1946 to present. Clinical trial registries/databases and websites were also searched for relevant data. Key words were: daratumumab; Darzalex; HuMax-CD38; humanised anti-CD38 monoclonal antibody; monoclonal antibody humax-CD38; JNJ-54767414. Records were limited to those in English language. Searches last updated 18 February 2019. | |
References
National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®): multiple myeloma (version 2.2019). 2018. http://www.nccn.org. Accessed 7 Feb 2019.
Fonseca R, Abouzaid S, Bonafede M, et al. Trends in overall survival and costs of multiple myeloma, 2000–2014. Leukemia. 2017;31(9):1915–21.
Moreau P, San Miguel J, Sonneveld P, et al. Multiple myeloma: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(Suppl 6):52–61.
Willenbacher E, Balog A, Willenbacher W. Short overview on the current standard of treatment in newly diagnosed multiple myeloma. Memo. 2018;11(1):59–64.
Chari A, Mehra M, Slavcev M, et al. Evaluation and comparison of characteristics and outcomes among frontline multiple myeloma (FLMM) patients with and without stem cell transplant treatment [abstract no. 4738]. In: 60th American Society of Hematology Annual Meeting and Exposition. 2018.
Mahajan S, Tandon N, Kumar S. The evolution of stem-cell transplantation in multiple myeloma. Ther Adv Hematol. 2018;9(5):123–33.
American Cancer Society. Multiple myeloma. 2018. https://www.cancer.org. Accessed 7 Feb 2019.
Fonseca R, Usmani SZ, Mehra M, et al. Characterization of frontline treatment patterns and attrition rates by lines of therapy in non-transplant patients with newly diagnosed multiple myeloma [abstract no. 3291]. In: 60th American Society of Hematology Annual Meeting and Exposition. 2018.
Lin P, Owens R, Tricot G, et al. Flow cytometric immunophenotypic analysis of 306 cases of multiple myeloma. Am J Clin Pathol. 2004;121(4):482–8.
Janssen Pharmaceutical. Darzalex (daratumumab): US prescribing information. 2015. https://www.janssenmd.com. Accessed 18 Feb 2019.
van de Donk N, Richardson PG, Malavasi F. CD38 antibodies in multiple myeloma: back to the future. Blood. 2018;131(1):13–29.
Blair HA. Daratumumab: a review in relapsed and/or refractory multiple myeloma. Drugs. 2017;77(18):2013–24.
European Medicines Agency. Darzalex: summary of product characteristics. 2018. http://www.ema.europa.eu. Accessed 18 Feb 2019.
Plesner T, Krejcik J. Daratumumab for the treatment of multiple myeloma. Front Immunol. 2018. https://doi.org/10.3389/fimmu.2018.01228.
McKeage K, Lyseng-Williamson KA. Daratumumab in multiple myeloma: a guide to its use as monotherapy in the EU. Drugs Ther Perspect. 2016;32:463–9.
de Weers M, Tai YT, van der Veer MS, et al. Daratumumab, a novel therapeutic human CD38 monoclonal antibody, induces killing of multiple myeloma and other hematological tumors. J Immunol. 2011;186(3):1840–8.
Overdijk MB, Verploegen S, Bogels M, et al. Antibody-mediated phagocytosis contributes to the anti-tumor activity of the therapeutic antibody daratumumab in lymphoma and multiple myeloma. mAbs. 2015;7(2):311–21.
Krejcik J, Casneuf T, Nijhof IS, et al. Daratumumab depletes CD38 + immune regulatory cells, promotes T-cell expansion, and skews T-cell repertoire in multiple myeloma. Blood. 2016;128(3):384–94.
Overdijk MB, Jansen JH, Nederend M, et al. The therapeutic CD38 monoclonal antibody daratumumab induces programmed cell death via Fcγ receptor-mediated cross-linking. J Immunol. 2016;197(3):807–13.
Palumbo A, Chanan-Khan A, Weisel K, et al. Daratumumab, bortezomib, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375(8):754–66.
Nijhof IS, Groen RW, Lokhorst HM, et al. Upregulation of CD38 expression on multiple myeloma cells by all-trans retinoic acid improves the efficacy of daratumumab. Leukemia. 2015;29(10):2039–49.
Nijhof IS, Casneuf T, van Velzen J, et al. CD38 expression and complement inhibitors affect response and resistance to daratumumab therapy in myeloma. Blood. 2016;128(7):959–70.
Casneuf T, Xu XS, Adams HC 3rd, et al. Effects of daratumumab on natural killer cells and impact on clinical outcomes in relapsed or refractory multiple myeloma. Blood Adv. 2017;1(23):2105–14.
Chapuy CI, Nicholson RT, Aguad MD, et al. Resolving the daratumumab interference with blood compatibility testing. Transfusion. 2015;55(6 Pt 2):1545–54.
Janssen Pharmaceutical. Darzalex® (daratumumab): product information. 2017. https://www.janssen.com. Accessed 7 Feb 2019.
McCudden C, Axel AE, Slaets D, et al. Monitoring multiple myeloma patients treated with daratumumab: teasing out monoclonal antibody interference. Clin Chem Lab Med. 2016;54(6):1095–104.
Clemens PL, Yan X, Lokhorst HM, et al. Pharmacokinetics of daratumumab following intravenous infusion in relapsed or refractory multiple myeloma after prior proteasome inhibitor and immunomodulatory drug treatment. Clin Pharmacokinet. 2016;56(8):915–24.
Xu XS, Yan X, Puchalski T, et al. Clinical implications of complex pharmacokinetics for daratumumab dose regimen in patients with relapsed/refractory multiple myeloma. Clin Pharmacol Ther. 2017;101(6):721–4.
Yan X, Clemens PL, Puchalski T, et al. Influence of disease and patient characteristics on daratumumab exposure and clinical outcomes in relapsed or refractory multiple myeloma. Clin Pharmacokinet. 2018;57(4):529–38.
Xu XS, Dimopoulos MA, Sonneveld P, et al. Pharmacokinetics and exposure-response analyses of daratumumab in combination therapy regimens for patients with multiple myeloma. Adv Ther. 2018;35(11):1859–72.
Mateos MV, Dimopoulos MA, Cavo M, et al. Daratumumab plus bortezomib, melphalan, and prednisone for untreated myeloma. N Engl J Med. 2018;378(6):518–28.
San Miguel JF, Schlag R, Khuageva NK, et al. Bortezomib plus melphalan and prednisone for initial treatment of multiple myeloma. N Engl J Med. 2008;359(9):906–17.
Dimopoulos MA, Mateos MV, Cavo M, et al. One-year update of a phase 3 randomized study of daratumumab plus bortezomib, melphalan, and prednisone (D-VMP) versus bortezomib, melphalan, and prednisone (VMP) in patients (pts) with transplant-ineligible newly diagnosed multiple myeloma (NDMM): ALCYONE [abstract no. 156]. In: 60th American Society of Hematology Annual Meeting and Exposition. 2018.
Gries K, Fastenau J, Chen Y, et al. Health-related quality of life in patients with newly diagnosed multiple myeloma who are ineligible for stem cell transplantation: results from the ALCYONE trial [abstract no. 8042]. J Clin Oncol. 2018;36(15 Suppl).
Kumar S, Paiva B, Anderson KC, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17(8):e328–46.
San-Miguel JF, Facon T, Dimopoulos MA, et al. Treatment regimens for patients with newly diagnosed multiple myeloma who are ineligible for stem cell transplantation: a systematic literature review and network meta-analysis [abstract no. 4741]. In: 60th American Society of Hematology Annual Meeting and Exposition. 2018.
Kumar SK, Plesner T, Orlowski RZ, et al. Phase 3 randomized study of daratumumab plus lenalidomide and dexamethasone (D-Rd) versus lenalidomide and dexamethasone (Rd) in patients with newly diagnosed multiple myeloma (NDMM) ineligible for transplant (MAIA) [abstract no. LBA-2]. In: 60th Annual Meeting & Exposition Of The American Society Of Hematology. 2018.
Rajkumar SV, Harousseau JL. Next-generation multiple myeloma treatment: a pharmacoeconomic perspective. Blood. 2016;128(24):2757–64.
Acknowledgements
During the peer review process the manufacturer of daratumumab was also offered an opportunity to review this article. Changes resulting from comments received were made on the basis of scientific and editorial merit.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The preparation of this review was not supported by any external funding.
Conflicts of interest
Yahiya Y Syed is a salaried employee of Adis/Springer, is responsible for the article content and declares no relevant conflicts of interest.
Additional information
The manuscript was reviewed by: N. Callander, University of Wisconsin Carbone Cancer Center, Madison, WI, USA; C. Cerchione, Istituto Scientifico Romagnolo per lo Studio e la Cura dei Tumori (IRST) IRCCS, Meldola, Italy; S. A. Holstein, Internal Medicine, University of Nebraska Medical Center, Omaha, NE, USA; T. Ichinohe, Department of Haematology and Oncology, Hiroshima University, Hiroshima, Japan; S. Knop, Medizinische Klinik und Poliklinik II, Universitätsklinikum Würzburg, Würzburg, Germany.
Rights and permissions
About this article
Cite this article
Syed, Y.Y. Daratumumab: A Review in Combination Therapy for Transplant-Ineligible Newly Diagnosed Multiple Myeloma. Drugs 79, 447–454 (2019). https://doi.org/10.1007/s40265-019-01080-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40265-019-01080-6