Abstract
Lenalidomide and dexamethasone (Rd) treatment is common for patients with newly diagnosed multiple myeloma (NDMM) ineligible for autologous stem-cell transplantation. Daratumumab plus Rd (D-Rd) is effective and well tolerated for treating relapsed or refractory multiple myeloma. In this ongoing phase 1b trial, transplant-ineligible Japanese patients with NDMM received daratumumab (16 mg/kg intravenously every week for 8 weeks, every 2 weeks for 16 weeks, then every 4 weeks until disease progression) plus Rd (R 25 mg on Days 1‒21 of 28-day cycle; d 40 mg weekly). The primary objective was to evaluate D-Rd tolerability and safety in Japanese patients with NDMM. Secondary objectives included daratumumab pharmacokinetics and response rate. During the dose-limiting toxicity (DLT) evaluation period, two DLTs occurred in seven (28.6%) patients, indicating D-Rd tolerability. At an 11.0-month median follow-up (interim analysis), grade 3/4 treatment-emergent adverse events occurred in six (85.7%) patients, including lymphopenia (71.4%), leukopenia (57.1%), and neutropenia (42.9%). Three (42.9%) patients experienced infusion-related reactions (IRRs). All IRRs were grade 2, occurred during the first daratumumab infusion, and resolved within 24 h. Pharmacokinetic findings were comparable to those in previous studies. A 100% overall response rate was achieved. These findings suggest D-Rd is tolerable in Japanese patients with transplant-ineligible NDMM. ClinicalTrials.gov identifier NCT02918331.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The risk of multiple myeloma (MM) increases with age, and patients who are ≥ 65 years of age represent more than half of all new cases each year in Japan [1]. The introduction of novel therapeutic agents and autologous stem-cell transplantation (ASCT) has improved overall survival of Japanese and non-Japanese patients with MM in the past 20 years, but alternative treatment options are still needed to improve clinical outcomes for elderly and frail patients who are often not suitable for these therapies [2, 3].
Lenalidomide and low-dose dexamethasone (Rd) is an approved regimen for newly diagnosed MM (NDMM) [4,5,6,7,8]. In the global FIRST phase 3 clinical trial, continuous Rd treatment prolonged survival and improved response rates versus fixed-duration treatment with melphalan, prednisone, and thalidomide in transplant-ineligible MM patients [5]. A similar clinical benefit of Rd in Japanese patients with transplant-ineligible MM was later demonstrated in a single-arm, phase 2 follow-up study [4]. Importantly, patients treated with Rd generally reported fewer grade 3 or 4 adverse events (AEs) and lower incidence of hematologic and neurologic toxicity [5].
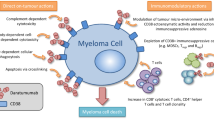
Daratumumab is a CD38-targeted human IgGκ monoclonal antibody that induces MM cell death through a direct on-tumor and immunomodulatory mechanism of action [9,10,11,12,13,14,15]. Daratumumab has demonstrated deep and durable responses as a monotherapy and superior clinical benefit across lines of therapy when combined with standard-of-care regimens for the treatment of MM [16,17,18,19,20]. Daratumumab in combination with Rd (D-Rd; POLLUX trial, NCT02076009) or bortezomib/dexamethasone (D-Vd; CASTOR trial, NCT02136134) prolonged progression-free survival and induced higher response rates versus Rd or bortezomib/dexamethasone (Vd) alone in relapsed or refractory MM (RRMM) patients with ≥ 1 prior line of therapy [18, 19, 21]. In addition, no new safety concerns were observed with the addition of daratumumab to standard-of-care regimens in these patients with RRMM [19, 21, 22]. Among Japanese patients with RRMM, phase 1 studies of daratumumab monotherapy or D-Vd also showed acceptable safety and favorable efficacy, consistent with non-Japanese patients [23, 24].
The clinical benefit of daratumumab was recently extended to patients with NDMM who were not eligible for high-dose chemotherapy and ASCT (ALCYONE trial, NCT02195479). Daratumumab plus bortezomib, melphalan, and prednisone (D-VMP) improved response rates and lowered the risk of disease progression or death in transplant-ineligible patients with NDMM [20]. A global, ongoing phase 3 clinical trial is comparing the clinical benefit of D-Rd versus Rd in patients outside of Japan with NDMM who are not candidates for high-dose chemotherapy and ASCT (MAIA trial, NCT02252172). In MAIA, D-Rd treatment significantly reduced the risk of disease progression or death by 44% at a median follow-up of 28.0 (range, 0.0–41.4) months [25]. Here, we report results from the first clinical trial of the D-Rd regimen in Japanese patients with NDMM who are not eligible for transplant. This ongoing, open-label, multicenter, phase 1b study of Japanese patients parallels the MAIA study and provides clinical data to support D-Rd approval for NDMM in Japan. This interim analysis evaluated the tolerability and safety of D-Rd, pharmacokinetics and immunogenicity of daratumumab, and efficacy in Japanese patients with transplant-ineligible NDMM.
Materials and methods
2.1 Patients
Eligible patients were ≥ 20 years of age, had documented NDMM, and were not eligible for high-dose chemotherapy and ASCT due to comorbid condition(s) or an age of ≥ 65 years. These patients had hemoglobin levels ≥ 8.0 g/dL, an absolute neutrophil count ≥ 1.0 × 109/L, a platelet count ≥ 75 × 109/L (if < 50% of bone marrow nucleated cells were plasma cells; otherwise platelet count ≥ 50 × 109/L), aspartate and alanine aminotransferase levels ≤ 2.5 times the upper limit of normal (ULN), alkaline phosphatase levels ≤ 2.5 times ULN, total bilirubin ≤ 1.5 times ULN, a creatinine clearance ≥ 30 mL/min, and corrected serum calcium levels ≤ 14 mg/dL or free ionized calcium < 6.5 mg/dL. In addition, an Eastern Cooperative Oncology Group (ECOG) performance status score of 0 or 1 was required for study inclusion [26].
The patients with primary amyloidosis, monoclonal gammopathy of undetermined significance, smoldering MM, plasma cell leukemia, Waldenström’s macroglobulinemia, and POEMS syndrome (polyneuropathy, organomegaly, endocrinopathy, monoclonal protein, and skin changes) were excluded. Other concurrent medical conditions that could interfere with study procedures or results, or that could constitute a hazard during study participation, also warranted study exclusion. Additional exclusion criteria included prior or current systemic therapy or ASCT for MM, history of malignancy within the prior 5 years other than defined exceptions, radiation therapy within 14 days of the first dose, plasmapheresis within 28 days of the first dose, and known meningeal involvement of MM.
The protocol and amendments for this study were reviewed and approved by affiliated local Independent Ethics Committees and Internal Review Boards. The study was conducted in accordance with ethical principles that have their origin in the Declaration of Helsinki and that are consistent with Good Clinical Practices and applicable regulatory requirements. All patients provided written consent to participate in the study.
2.2 Study design
This phase 1b, open-label, single-arm study of daratumumab in combination with lenalidomide and dexamethasone (MMY1006, NCT02918331) was conducted at 4 sites in Japan starting on October 7, 2016, with an interim analysis conducted up to a clinical cutoff date of January 30, 2018. The study included a screening phase (up to 21 days before treatment initiation on Cycle 1, Day 1), a treatment phase (Cycle 1, Day 1 until discontinuation due to documented disease progression, unacceptable toxicity, or any other reason), and a follow-up phase (immediately following the end of treatment until 8 weeks after the last daratumumab dose, loss to follow-up, withdrawal of consent, death, or study end).
Demographic information and baseline disease characteristics were recorded during the screening phase. Cytogenetic assessment occurred before the clinical cutoff date of January 30, 2018, with the exception of 1 patient. Testing of this patient was performed using fluorescent in situ hybridization (FISH) on December 22, 2018 to validate an earlier assessment.
2.2.1 Dosing and administration schedule
Daratumumab (16 mg/kg) was administered intravenously (IV) weekly for the first 8 weeks of treatment (Cycles 1–2), every 2 weeks for 16 weeks (Cycles 3–6), and then every 4 weeks in 28-day cycles until discontinuation. Dexamethasone, acetaminophen, and an antihistamine were given before each daratumumab infusion to prevent infusion-related reactions (IRRs). Lenalidomide was administered orally as capsules at a dose of 25 mg each day on Day 1 through 21 of each cycle (or given as a 10 mg dose if creatinine clearance was 30–60 mL/min). Dexamethasone was administered IV as single-use vials and/or orally as tablets at a dose of 40 mg weekly (patients aged ≥ 75 years or with body mass index < 18.5 kg/m2 were given 20 mg weekly). On daratumumab infusion days, dexamethasone was administered IV as the treatment dose of steroid for that day and the required premedication prior to daratumumab infusion.
2.3 Objectives and assessments
The primary objective was to evaluate the tolerability and safety of D-Rd as determined by the frequency of dose-limiting toxicity (DLT; primary endpoint). Secondary objectives included assessment of daratumumab pharmacokinetics (PK) and immunogenicity, and response rate.
2.3.1 Tolerability and safety
DLT was used to evaluate the tolerability of the 16 mg/kg dose of daratumumab when combined with Rd. DLT evaluation began immediately with the first administration of daratumumab and ended following the end of Cycle 1 with a safety evaluation before Day 1 of Cycle 2. DLTs included IRRs (grade ≥ 3), hematologic toxicities (mainly grade ≥ 4), and non-hematologic toxicities (grade ≥ 3) that occurred during the DLT evaluation period. Only daratumumab-related AEs as judged by the study evaluation team (SET) were regarded as a DLT.
Safety evaluations were performed throughout the treatment phase of the study, including AE monitoring, periodic physical examinations, electrocardiogram monitoring, measurement of vital signs, determination of ECOG performance status, and clinical laboratory parameter assessment (serum chemistry and hematology). Serum chemistry assessments included phosphate and alanine aminotransferase (ALT) levels; hematology assessments included white blood cell, red blood cell, platelet, neutrophil, and lymphocyte counts, and measurement of hemoglobin levels. The patients were monitored throughout the study for AEs, serious AEs (SAEs), other significant AEs, and AEs of special interest until 30 days after the last dose of daratumumab at the end of treatment. ECOG performance status was used to evaluate the effect of disease status on the activity of daily living at the beginning of each cycle and at the end of treatment visit.
2.3.2 Pharmacokinetics and immunogenicity
Blood samples to assess PK of daratumumab were collected on Day 1 of Cycles 1, 3, 6, and 12, and at the end of treatment and follow-up visit. Blood was drawn before and immediately after daratumumab IV infusion. Immunogenicity was assessed by measuring anti-daratumumab antibodies in serum samples collected at pre-dose on Day 1 of Cycles 1, 3, and 12, and at the end of treatment and follow-up visit. Serum samples were screened for antibodies binding to daratumumab and the titer of confirmed positive samples reported.
2.3.3 Response rates
There was no primary efficacy endpoint in this study. Key secondary endpoints were the rate of complete response (CR) or better (CR + stringent CR [sCR]), very good partial response (VGPR) or better (VGPR + CR + sCR), partial response (PR), stable disease, and progressive disease (PD). Overall response rate (ORR; PR + VGPR + CR + sCR) was also quantified. Response to treatment was evaluated in accordance with the International Myeloma Working Group (IMWG) criteria [27]. Other efficacy endpoints included the duration of response (DOR; first response to PD), time to response (first dose to ≥ PR), time to disease progression (TTP; first dose to PD), and serum and urine M-protein response.
2.4 Statistical analyses
At least six patients were to be enrolled and examined for the tolerability and safety of D-Rd. The analysis set included all patients who received ≥ 1 dose of daratumumab. If a daratumumab dose reduction was needed, ≥ 3 patients would be enrolled in subsequent cohorts. The next dose level was guided by the Bayesian logistic regression model (BLRM) using the escalation with overdose control (EWOC) principle. Dose escalation to levels with a probability of excessive dose > 0.25 was prohibited. Safety analyses included descriptive statistics and frequency tabulations of all reported treatment-emergent AEs (TEAEs), deaths, SAEs, other significant AEs, and AEs of special interest. AEs were graded for severity according to National Cancer Institute Common Terminology Criteria for Adverse Events, version 4.03 [28]. Serum daratumumab concentrations and the incidence of anti-daratumumab antibody concentrations for PK and immunogenicity analyses, respectively, were summarized, and descriptive statistics are presented. For response data, the number and percentage of patients with each response rate and PD are presented. The median DOR, time to response, and TTP with 95% confidence intervals (CI) were estimated using the Kaplan–Meier method. Descriptive statistics were also provided to summarize time to response. M-protein levels for each M-component were summarized, listed, and plotted.
Results
3.1 Patient demographics and disposition
This study was initiated on October 7, 2016 and was ongoing at the time of this report. Of 13 patients screened, 7 were enrolled in the study and received ≥ 1 dose of daratumumab. At the clinical cutoff date (January 30, 2018), 6 (85.7%) patients remained on treatment and 1 (14.3%) discontinued treatment due to an AE. The patient demographics and baseline characteristics are shown in Table 1. All patients were > 65 years of age (median, 70.0; range, 66–81) with four men (57.1%) and three women (42.9%). Most (n = 4, 57.1%) patients had International Staging System disease stage II MM, and the median time since diagnosis was 0.59 months (range, 0.5–2.1). Two (28.6%) patients had high-risk cytogenetics with t(4;14) abnormalities (five patients were assessed by both FISH and karyotyping, and two by FISH alone).
3.2 Duration of treatment and exposure
At the clinical cutoff date, the median duration of D-Rd treatment was 10.9 months (range, 4.2–15.4) and patients received a median of 12 (range, 5–17) treatment cycles. Six (85.7%) patients received at least 9 cycles of study treatment. One patient discontinued treatment due to a TEAE (grade 3 rash generalized). The median relative dose intensities for daratumumab, lenalidomide, and dexamethasone were 99.5%, 79.4%, and 100.0%, respectively. The median duration of follow-up was 11.0 months (range, 4.9–15.6; Table 2).
3.3 Tolerability and safety
DLTs were reported in two (28.6%) patients during Cycle 1 among seven eligible and DLT-evaluable patients. The DLTs included grade 3 abnormal hepatic function and grade 3 pneumonia observed in two separate patients that resolved within 30 days of onset. No patient discontinued study treatment due to a DLT. The risk of excessive dose according to the EWOC principle of DLT at the daratumumab 16 mg/kg dose level was 19.8% (< 25%). The estimated median DLT rate was 20.4% (95% credible interval, 3.8–52.8%). Based on the DLT evaluation, it was concluded by the SET that the 16 mg/kg dose of daratumumab with Rd was tolerable in Japanese patients with NDMM.
All 7 patients reported at least 1 TEAE, and 6 (85.7%) patients had a TEAE related to ≥ 1 component of D-Rd treatment. The most frequently reported all-grade TEAEs (≥ 2 patients) were leukopenia and lymphopenia (5 [71.4%] patients each), neutropenia (4 [57.1%] patients), and rash and constipation (3 [42.9%] patients each) (Table 3). Other all-grade TEAEs reported in 2 (28.6%) patients each included thrombocytopenia, cough, hiccups, rash generalized, back pain, deep vein thrombosis, and viral upper respiratory tract infection. Lymphopenia, leukopenia, and neutropenia were grade 3 or 4 TEAEs in 5 (71.4%), 4 (57.1%), and 3 (42.9%) patients, respectively. Three SAEs were reported in two patients, comprising grade 3 pneumonia and grade 3 back pain in one patient, and grade 3 pulmonary embolism in one patient (Table 3). No grade 5 TEAEs were reported in this study, and no deaths were reported by the clinical cutoff date. One patient (14.3%) discontinued study treatment due to grade 3 rash generalized reported on Day 121.
Three (42.9%) patients reported 6 IRRs, all of which were grade 2 toxicity, occurred during the first infusion, and were resolved within 24 h of onset (Table 3). No IRRs occurred during the second or subsequent infusions. All patients received acetaminophen, diphenhydramine, and dexamethasone (also part of the study treatment) as premedication for IRRs.
3.4 Pharmacokinetics and immunogenicity
All seven patients were included in pharmacokinetic analysis. Following the weekly daratumumab (16 mg/kg) dosing period, daratumumab accumulation in serum was observed for at least the first nine doses through Day 1 of Cycle 3, leading to a 3.1-fold increase in daratumumab peak concentration (Fig. 1). Serum daratumumab concentrations decreased during subsequent every 2-week and every 4-week dosing periods. No patient tested positive for anti-daratumumab antibodies.
Serum daratumumab concentrations during D-Rd treatment. Daratumumab concentration in serum was measured at the time points indicated and plotted as mean (SD) peak and trough concentrations. DARA daratumumab, C cycle, D day, PK pharmacokinetics, D-Rd daratumumab plus lenalidomide and dexamethasone, SD standard deviation
3.5 Response rates
The ORR was 100.0%. Two (28.6%) patients had a response of CR or better, one of whom (14.3%) achieved an sCR. Six (85.7%) patients achieved a VGPR or better. Although 1 patient discontinued study treatment due to an AE, no patients had disease progression at the time of the clinical cutoff date (Fig. 2). The median time to first response (PR rate or better) was 1.0 month (95% CI, 0.9–1.9 months). Parallel decreases in serum M-protein (≥ 50.0% reduction) were observed in 6 evaluable patients with measurable heavy chain at baseline (Fig. 3a). The M-protein response in urine was observed in 2 (28.6%) patients with measurable light chain at baseline (both 100% reduction; Fig. 3b).
Overall response rate of NDMM patients treated with D-Rd. Response rates are shown for patients at a median follow-up time of 11.0 months. ORR overall response rate, CR complete response, VGPR very good partial response, D-Rd daratumumab plus lenalidomide and dexamethasone, PR partial response, sCR stringent complete response, NDMM newly diagnosed multiple myeloma
Percent change from baseline in serum M-proteins and urine M-proteins with D-Rd treatment in individual patients. Individual plot of a serum M-protein levels of six patients with measurable heavy chain at baseline and b urine M-protein levels of two patients with measurable light chain at baseline. D-Rd daratumumab plus lenalidomide and dexamethasone, M monoclonal
Discussion
This open-label, multicenter, phase 1b study is the first to evaluate D-Rd in Japanese patients with NDMM who are not candidates for high-dose chemotherapy and ASCT. The data suggest that D-Rd had an acceptable tolerability and safety profile. Based on the evaluation according to the EWOC principle, this study confirmed daratumumab 16 mg/kg plus Rd was tolerable in Japanese patients with NDMM.
No new safety concerns were observed during the median D-Rd treatment period of 10.9 months at the time of the clinical cutoff date. Three SAEs were reported in two patients, including one patient with grade 3 pneumonia and grade 3 back pain, and one patient with grade 3 pulmonary embolism. All SAEs resolved and did not lead to treatment discontinuation. The event of pneumonia was considered possibly related to D-Rd treatment, whereas back pain was considered doubtfully related to D-Rd. Pneumonia was the most common SAE reported in the recently published interim analysis of the phase 3 MAIA study, occurring in 13.2% of patients treated with D-Rd [25]. In addition, it is known that MM patients who receive daratumumab combined with other chemotherapeutics (ie, D-VMP, D-Rd, D-Vd) are at increased risk for infection, including pneumonia [18,19,20]. The pulmonary embolism reported in 1 patient occurred on study Day 26, resolved within 14 days, and was considered not related to daratumumab but probably and doubtfully related to lenalidomide and dexamethasone, respectively. Lenalidomide has previously been associated with increased incidence of thrombosis, which can lead to pulmonary embolism [29]. In MAIA, no differences were observed between D-Rd and Rd in incidence rates of grade 3 or 4 deep vein thrombosis, pulmonary embolism, or both (both groups, 23 (6%) patients) [30].
D-Rd induced manageable AEs that were consistent with the toxicity profile of Rd and daratumumab monotherapy [5, 16]. The safety profile of D-Rd in Japanese NDMM patients was also generally comparable to non-Japanese patients with NDMM in the phase 3 MAIA clinical study [25]. The most common grade 3 or 4 adverse events in Japanese patients in the current study included lymphopenia, leukopenia, and neutropenia, similar to non-Japanese patients in the MAIA study. Although the frequency of these cytopenias was higher in this study compared with MAIA, these AEs were manageable and did not lead to study treatment discontinuation. Baseline counts of white blood cells, neutrophils, and lymphocytes in Japanese patients were lower than those in the MAIA study, but reduction from baseline to the lowest value for these blood cells did not differ substantially between Japanese and non-Japanese patients (unpublished data). One patient discontinued treatment due to an AE of grade 3 rash generalized that was possibly or probably related to daratumumab and lenalidomide, respectively. Skin rash is a frequent symptom of toxicity caused by lenalidomide, sometimes resulting in treatment discontinuation [31]. We acknowledge that the sample size in this study was small, and further studies with a larger Japanese population are required to confirm these findings.
In the phase 1/2 GEN503 study and phase 3 POLLUX study, daratumumab given with Rd was associated with IRRs and a high rate of any-grade neutropenia in RRMM patients with ≥ 1 prior line of therapy [19, 22]. Subanalyses of POLLUX data demonstrated that the rate of IRRs and any-grade neutropenia were generally similar between a subgroup of Japanese patients treated with D-Rd [21] and findings from the current study. IRRs are common during the first IV infusion of daratumumab and can be controlled with pre-infusion medications; neutropenia is a known lenalidomide-associated toxicity that can be attributed to extended exposure to lenalidomide, the introduction of daratumumab, or both, with D-Rd treatment [19, 21, 32].
In the current study, low-grade IRRs were reported by 42.9% of patients and occurred during the first infusion, similar to GEN503, POLLUX, and MAIA [19, 22, 25]. The rates of any-grade neutropenia (57.1%) and grade 3/4 neutropenia (42.9%) in this study were similar to MAIA, but lower than the overall ITT population and in Japanese patients from POLLUX. However, the incidences of any-grade leukopenia and lymphopenia (71.4% each) in the current study were higher than those reported in these other clinical studies, but did not lead to treatment discontinuation or daratumumab dose modifications, and were clinically manageable. Cross-study comparisons should be interpreted with caution, particularly considering differences among studies in the phase of drug testing, inclusion criteria, and specifically sample size (only seven Japanese patients participated in the current study).
The favorable tolerability and safety profile of D-Rd in Japanese patients with NDMM in this study were supported by PK findings, immunogenicity, and response rates that were consistent with previous daratumumab studies [16, 17, 20, 22, 25]. D-Rd recipients demonstrated robust increases in serum daratumumab concentrations during the first nine doses of daratumumab given weekly, while no anti-daratumumab antibodies were detected. The weekly daratumumab dosing regimen allowed all patients to rapidly achieve responses (within 1 month of therapy). Despite a short follow-up of 11 months, six of seven patients achieved a VGPR rate or better that was paralleled by decreases in serum and urine M-protein levels.
Daratumumab has been shown to be safe and effective in combination with standard-of-care regimens in patients with RRMM, including Japanese patients in the phase 3 POLLUX study of daratumumab plus Rd and the phase 1b MMY1005 study of daratumumab plus Vd [16,17,18,19, 23, 33]. Based on these results, daratumumab in combination with Rd or Vd was approved for treatment of adults with RRMM in Japan [34]. Recently, a similar clinical benefit of daratumumab was demonstrated in patients with NDMM who are not eligible for ASCT [20, 25]; daratumumab plus bortezomib, melphalan, and prednisone was approved for transplant-ineligible NDMM patients in the United States, European Union, and Brazil, and daratumumab plus Rd was approved for such patients in the United States.
In this study, we extend upon these findings and demonstrate that D-Rd is tolerable and safe in Japanese patients with previously untreated MM who are ineligible for high-dose chemotherapy and ASCT. In addition, preliminary data suggest that D-Rd is efficacious in these patients, with an ORR of 100% and 85.7% of patients achieving a VGPR or better. Although the sample size in the study was small (seven Japanese patients), it was controlled according to a prespecified tolerability confirmation scheme guided by a BLRM using the EWOC principle. The study objective was accomplished in these seven Japanese patients, and therefore, the sample size was appropriate when considering the primary objective of the study.
This study parallels the global, ongoing MAIA phase 3 clinical trial evaluating the safety and efficacy of D-Rd versus Rd in transplant-ineligible patients with NDMM [25]. The findings of the current study in Japanese patients are important, as the tolerability and safety of targeted anticancer therapies may vary in clinical trials depending on the ethnicity and geographical backgrounds of study participants [21, 35, 36]. Moreover, this is the first clinical study to evaluate the tolerability and safety of the D-Rd regimen in Japanese patients with NDMM.
We also evaluated the probability of achieving consistency in terms of ORR between the MAIA study and the current study (MMY1006), although this analysis was exploratory (not prespecified). For the seven Japanese patients in the current study, the target ORR was 92.9% based on the MAIA D-Rd group, and the probability of exceeding the threshold ORR of the MAIA Rd control group (81.3%) was approximately 90%. With an ORR of 100% in the current study, these results support a clinical benefit of D-Rd treatment in Japanese patients with NDMM, which was confirmed in the MAIA study that enrolled an overseas population. For these reasons, MMY1006 is a key study providing clinical data in Japanese individuals, along with the global MAIA study, to support D-Rd approval for NDMM in Japan.
In conclusion, daratumumab in combination with Rd demonstrated a favorable tolerability and safety profile in Japanese patients with NDMM who are ineligible for transplantation. PK findings were consistent with previous daratumumab studies, and preliminary data suggest that this daratumumab-based combination regimen is efficacious in these patients. Further study is needed to confirm the long-term efficacy and safety of D-Rd in Japanese patients with transplant-ineligible NDMM.
Data availability
The data sharing policy of Janssen Pharmaceutical Companies of Johnson & Johnson is available at https://www.janssen.com/clinical-trials/transparency. As noted on this site, requests for access to the study data can be submitted through Yale Open Data Access (YODA) Project site at https://yoda.yale.edu.
References
Kim K, Lee JH, Kim JS, Min CK, Yoon SS, Shimizu K, et al. Clinical profiles of multiple myeloma in Asia—an Asian myeloma network study. Am J Hematol. 2014;89(7):751–6.
Ozaki S, Handa H, Saitoh T, Murakami H, Itagaki M, Asaoku H, et al. Trends of survival in patients with multiple myeloma in Japan: a multicenter retrospective collaborative study of the Japanese Society of Myeloma. Blood Cancer J. 2015;5:e349.
Tamura H. Immunopathogenesis and immunotherapy of multiple myeloma. Int J Hematol. 2018;107(3):278–85.
Suzuki K, Shinagawa A, Uchida T, Taniwaki M, Hirata H, Ishizawa K, et al. Lenalidomide and low-dose dexamethasone in Japanese patients with newly diagnosed multiple myeloma: a phase II study. Cancer Sci. 2016;107(5):653–8.
Benboubker L, Dimopoulos MA, Dispenzieri A, Catalano J, Belch AR, Cavo M, et al. Lenalidomide and dexamethasone in transplant-ineligible patients with myeloma. N Engl J Med. 2014;371(10):906–17.
Moreau P, San Miguel J, Sonneveld P, Mateos MV, Zamagni E, Avet-Loiseau H, et al. Multiple myeloma: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017;28(suppl_4):52–61.
Suzuki K. Current therapeutic strategy for multiple myeloma. Jpn J Clin Oncol. 2013;43(2):116–24.
Iida S, Ishida T, Murakami H, Ozaki S, Abe M, Hata H, et al. JSH practical guidelines for hematological malignancies, 2018: III. Myeloma-1. Multiple myeloma (MM). Int J Hematol. 2019;109(5):509–38.
de Weers M, Tai YT, van der Veer MS, Bakker JM, Vink T, Jacobs DC, et al. Daratumumab, a novel therapeutic human CD38 monoclonal antibody, induces killing of multiple myeloma and other hematological tumors. J Immunol. 2011;186(3):1840–8.
Overdijk MB, Verploegen S, Bogels M, van Egmond M, van Bueren JJL, Mutis T, et al. Antibody-mediated phagocytosis contributes to the anti-tumor activity of the therapeutic antibody daratumumab in lymphoma and multiple myeloma. MAbs. 2015;7(2):311–21.
van Bueren JL, Jakobs D, Kaldenhoven N, Roza M, Hiddingh S, Meesters J, et al. Direct in vitro comparison of daratumumab with surrogate analogs of CD38 antibodies MOR03087, SAR650984 and Ab79. Blood. 2014;124(21):3474.
Overdijk MB, Jansen JH, Nederend M, van Bueren JJL, Groen RW, Parren PW, et al. The therapeutic CD38 monoclonal antibody daratumumab induces programmed cell death via Fcgamma receptor-mediated cross-linking. J Immunol. 2016;197(3):807–13.
Krejcik J, Casneuf T, Nijhof IS, Verbist B, Bald J, Plesner T, et al. Daratumumab depletes CD38+ immune-regulatory cells, promotes T-cell expansion, and skews T-cell repertoire in multiple myeloma. Blood. 2016;128(3):384–94.
Adams HC 3rd, Stevenaert F, Krejcik J, Van der Borght K, Smets T, Bald J, et al. High-parameter mass cytometry evaluation of relapsed/refractory multiple myeloma patients treated with daratumumab demonstrates immune modulation as a novel mechanism of action. Cytometry A. 2019;95(3):279–89.
Chiu C, Casneuf T, Axel A, Lysaght A, Bald J, Khokhar NZ, et al. Daratumumab in combination with lenalidomide plus dexamethasone induces clonality increase and T-cell expansion: results from a phase 3 randomized study (POLLUX). Blood. 2016;128:4531.
Lonial S, Weiss BM, Usmani S, Singhal S, Chari A, Bahlis N, et al. Daratumumab monotherapy in patients with treatment-refractory multiple myeloma (SIRIUS): an open-label, randomised, phase 2 trial. Lancet. 2016;387(10027):1551–60.
Lokhorst HM, Plesner T, Laubach JP, Nahi H, Gimsing P, Hansson M, et al. Targeting CD38 with daratumumab monotherapy in multiple myeloma. N Engl J Med. 2015;373(13):1207–19.
Palumbo A, Chanan-Khan A, Weisel K, Nooka AK, Masszi T, Beksac M, et al. Daratumumab, bortezomib, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375(8):754–66.
Dimopoulos MA, Oriol A, Nahi H, San-Miguel J, Bahlis N, Usmani S, et al. Daratumumab, lenalidomide, and dexamethasone for multiple myeloma. N Engl J Med. 2016;375(14):1319–31.
Mateos MV, Dimopoulos MA, Cavo M, Suzuki K, Jakubowiak A, Knop S, et al. Daratumumab plus bortezomib, melphalan, and prednisone for untreated myeloma. N Engl J Med. 2018;378(6):518–28.
Suzuki K, Dimopoulos M, Takezako N, Okamoto S, Shinagawa A, Matsumoto M, et al. Daratumumab, lenalidomide, and dexamethasone in East Asian patients with relapsed or refractory multiple myeloma: subgroup analyses of the phase 3 POLLUX study (in press). Blood Cancer J. 2018;8(4):41.
Plesner T, Arkenau HT, Gimsing P, Krejcik J, Lemech C, Minnema MC, et al. Phase 1/2 study of daratumumab, lenalidomide, and dexamethasone for relapsed multiple myeloma. Blood. 2016;128:1821–8.
Iida S, Ichinohe T, Shinagawa A, Suzuki K, Takezako N, Aoki M. Safety and efficacy of daratumumab in combination with bortezomib and dexamethasone in Japanese patients with relapsed or refractory multiple myeloma. Int J Hematol. 2018;107(4):460–7.
Iida S, Suzuki K, Kusumoto S, Ri M, Tsukada N, Abe Y, et al. Safety and efficacy of daratumumab in Japanese patients with relapsed or refractory multiple myeloma: a multicenter, phase 1, dose-escalation study. Int J Hematol. 2017;106:541–51.
Facon T, Kumar S, Plesner T, Orlowski RZ, Moreau P, Bahlis N, et al. Daratumumab plus lenalidomide and dexamethasone for untreated myeloma. N Engl J Med. 2019;380(22):2104–15.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–55.
Kumar S, Paiva B, Anderson KC, Durie B, Landgren O, Moreau P, et al. International Myeloma Working Group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol. 2016;17(8):e328–e46.
US Department of Health and Human Services, National Institutes of Health, National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE). Version 4.03. 2010.
Palumbo A, Rajkumar SV, Dimopoulos MA, Richardson PG, San Miguel J, Barlogie B, et al. Prevention of thalidomide- and lenalidomide-associated thrombosis in myeloma. Leukemia. 2008;22(2):414–23.
Facon T, Kumar SK, Plesner T, Orlowski RZ, Moreau P, Bahlis N, et al. Phase 3 randomized study of daratumumab plus lenalidomide and dexamethasone (D-Rd) versus lenalidomide and dexamethasone (Rd) in patients with newly diagnosed multiple myeloma (NDMM) ineligible for transplant (MAIA). Presented at the 60th American Society of Hematology (ASH) Annual Meeting & Exposition. December 1–4, 2018; San Diego, CA, USA. 2018. Abstract LBA-2.
Dote S, Ito K, Itakura S, Yasu T, Hira D, Noda S, et al. Impact of prior bortezomib therapy on the incidence of lenalidomide-induced skin rash in multiple myeloma: a propensity score-matched multi-institutional cohort study. Leuk Lymphoma. 2019;60(12):2975–81.
Chari A, Mark TM, Krishnan A, Stockerl-Goldstein K, Usmani SZ, Londhe A, et al. Use of montelukast to reduce infusion reactions in an early access treatment protocol of daratumumab in United States patients relapsed or refractory multiple myeloma. Presented at the 58th American Society of Hematology (ASH) Annual Meeting & Exposition; December 3–6, 2016; San Diego, CA, USA. Abstract 2142. 2016.
Ichinohe T, Suzuki K, Iida S, Takazako N, Shinagawa A, Aoki M. Daratumumab with bortezomib + dexamethasone in Japanese pts with relapsed/refractory multiple myeloma 2017. Presented at the 79th annual meeting of the Japanese Society of Hematology (JSH); October 20–22, 2017; Tokyo. Abstract OS3-12D-3. 2017.
Genmab. Genmab announces approval of DARZALEX® (daratumumab) for relapsed or refractory multiple myeloma in Japan. 2017. https://ir.genmab.com/news-releases/news-release-details/genmab-announces-approval-darzalexr-daratumumab-relapsed-or/. Accessed 20 Jan 2020.
Ohtsu A, Shah MA, Van Cutsem E, Rha SY, Sawaki A, Park SR, et al. Bevacizumab in combination with chemotherapy as first-line therapy in advanced gastric cancer: a randomized, double-blind, placebo-controlled phase III study. J Clin Oncol. 2011;29(30):3968–76.
Kiyota N, Schlumberger M, Muro K, Ando Y, Takahashi S, Kawai Y, et al. Subgroup analysis of Japanese patients in a phase 3 study of lenvatinib in radioiodine-refractory differentiated thyroid cancer. Cancer Sci. 2015;106(12):1714–21.
Acknowledgements
This study was sponsored by Janssen Pharmaceutical K.K. The authors would like to acknowledge Hidehisa Noguchi for contributions to statistical analyses, and Akiko Suzuki, Hiromi Koga, and Ryo Tamamura for critical review of the manuscript. Medical writing support was provided by J. Matthew Kuczmarski, PhD, and Jill E. Kolesar, PhD, of MedErgy, and was funded by Janssen Global Services, LLC.
Author information
Authors and Affiliations
Contributions
All authors made substantive contributions to experimental design, data acquisition and/or analysis, and critical revision of the manuscript. All authors read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Conflict of interest
Hiroyuki Takamatsu received honoraria from Janssen Pharmaceutical K.K., Celgene, Takeda, Ono Pharmaceutical, Bristol-Myers Squibb, Daiichi Sankyo Company, Fujimoto Pharmaceutical, and Sanofi; received research funds from Celgene, Ono Pharmaceutical, Bristol-Myers Squibb, and CSL Behring; and consulted for Janssen, Celgene, AbbVie, and Sanofi. Shinsuke Iida received honoraria and research funds from Janssen, Celgene, Ono, Takeda, Novartis, Daiichi Sankyo, and Bristol-Myers Squibb; and received research funds from Chugai, Sanofi, MSD, AbbVie, Gilead, Kyowa Hakko Kirin, Astellas, and Teijin Pharma. Hirohiko Shibayama received honoraria and research funds from Takeda, Ono, Eisai, Sumitomo Dainippon Pharma, Mundipharma, and Nippon Shinyaku; received honoraria from Janssen, Celgene, Novartis, Chugai, Kyowa Kirin, Otsuka, AstraZeneca, AbbVie, Daiichi Sankyo, Fujimoto, Sanofi, Bristol-Myers Squibb, and Pfizer; and received research funds from Astellas, Teijin, MSD, Shionogi, and Taiho. Kazuhiro Shibayama and Hiroshi Yamazaki are employees of Janssen Pharmaceutical K.K. Kenshi Suzuki received honoraria from Celgene, Takeda, Amgen, Novartis, Genesis Pharmaceuticals, and Janssen; and received honoraria and research funds from Bristol-Myers Squibb.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Takamatsu, H., Iida, S., Shibayama , H. et al. Daratumumab, lenalidomide, and dexamethasone in Japanese patients with transplant-ineligible newly diagnosed multiple myeloma: a phase 1b study. Int J Hematol 111, 692–701 (2020). https://doi.org/10.1007/s12185-020-02825-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-020-02825-w