Abstract
Background
There is little consensus regarding the prevalence and distribution of underlying systemic diseases among patients with pyoderma gangrenosum.
Objective
The objective of this study was to synthesize existing data on the prevalence of associated systemic diseases in patients with pyoderma gangrenosum.
Methods
We performed a systematic review and meta-analysis of observational studies in MEDLINE, EMBASE, and Scopus (1823–2017). The quality of evidence was assessed using a modified Newcastle–Ottawa Scale. A meta-analysis was performed using random-effects models to estimate pooled prevalence rates with 95% confidence intervals.
Results
Twenty-one eligible studies comprising 2611 patients with pyoderma gangrenosum were included in the quantitative synthesis. The overall random-effects pooled prevalence of associated systemic diseases was 56.8% (95% confidence interval 45.5–67.4). The leading underlying disease was inflammatory bowel disease (17.6%; 95% confidence interval 13.0–22.7), followed by arthritis (12.8%; 95% confidence interval 9.2–16.9), hematological malignancies (8.9%; 95% confidence interval 6.5–11.6), and solid malignancies (7.4%; 95% confidence interval 5.8–9.1). In 16.3% (95% confidence interval 7.7–27.1) of cases, the onset of pyoderma gangrenosum was attributed to the pathergy phenomenon.
Conclusions
More than half of patients with pyoderma gangrenosum present with a relevant underlying disease. Inflammatory bowel disease and arthritis are the most frequently associated diseases. Relative to the reported literature, the pooled prevalence of arthritis and hematological malignancies is lower, while the pooled prevalence of solid malignancies is higher. Owing to the high level of heterogeneity among most of the comparisons, results should be interpreted with caution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The pooled prevalence of arthritis and hematological malignancies is lower than previously reported, while the pooled prevalence of solid malignancies is higher than believed. |
The pooled prevalence of underlying solid malignancies was surprisingly high (7.4%). |
The onset of pyoderma gangrenosum was attributed to the pathergy phenomenon in 16.3% of cases. |
1 Introduction
Pyoderma gangrenosum (PG) is a rare inflammatory neutrophilic dermatosis usually affecting the skin, with rare extracutaneous involvement. PG is classically characterized by a sudden onset of erythematous nodules or sterile pustules that rapidly develop into very painful ulcerations with violaceous undermined borders on the lower legs. Less frequently, PG can present as tender nodules or pustules on other sites of the body. The pathophysiological mechanisms underlying this chronic skin disorder are not fully established, but the predominance of other immune-mediated comorbidities, the over-expression of cytokines/chemokines and molecules amplifying the inflammatory network, and the typically good response to immunomodulatory drugs such as corticosteroids, antitumor necrosis factor-α modalities, and calcineurin inhibitors support an immune-mediated mechanism for PG, rather than an infectious one as was initially presumed [1,2,3,4,5].
PG may occur alone, in syndromic forms, or associated with systemic diseases [2, 6]. Current knowledge about associated comorbidities in PG is insufficient and based chiefly on small-scale case series and a few retrospective cohort studies. Based on this information, associations with systemic diseases were reported in up to 86% of patients, with inflammatory bowel disease (IBD), inflammatory arthritis, monoclonal gammopathy, and other hematological disorders being the most frequently associated diseases [1, 7]. The existence of one of these conditions was proposed as a minor criterion suggesting the diagnosis of PG [1, 8]. However, there is little consensus regarding the true prevalence and the distribution of these underlying diseases among patients with PG.
Given the gap in knowledge and the inconsistency of studies evaluating underlying diseases in patients with PG, there is a need to synthesize data across studies. A better characterization of underlying diseases is highly important because the type and the severity of these comorbidities are of prognostic significance for PG [9, 10]. A recalcitrant associated disease usually results in poorer prognosis and unfavorable outcomes, whereas a successful treatment of the associated disease may lead to improvement in PG [9]. A meta-analysis aimed at determining the prevalence of underlying conditions in PG has not been previously performed. The aim of the current study is to perform a systematic review and meta-analysis summarizing the prevalence of underlying systemic comorbidities among patients with PG.
2 Methods
2.1 Literature Search
The literature for this review was searched using MEDLINE (1946 to present), EMBASE (1947 to present), and Scopus (1823 to present) to identify eligible studies. Publications up to 10 September, 2017 were searched independently and cross-checked by two researchers (K.K. and A.D.C.). The search strategies were designed with assistance from a medical librarian and are detailed in the Table 1 of the Electronic Supplementary Material (ESM). Reference lists of included studies were further screened for additional eligible publications.
Studies published online, in print, and in press from all years were considered. All search results with titles and abstracts written in English were eligible for inclusion. Studies were excluded based on the title, abstract, or both if there was no clear indication they were investigating comorbidities in patients with PG. If data were duplicated in more than one study, the most recent and complete study was included in the meta-analysis.
2.2 Data Extraction
The three researchers independently performed data extraction from these studies. Any disagreements regarding the suitability of individual studies were resolved by discussion. Each paper was critically reviewed and the following data extracted: study design and settings; country of origin; the period over which study was conducted; the midpoint of follow-up period; number of patients in the study; mean age of patients; percentage of female individuals; source of information; crude prevalence estimates of each comorbidity (number of cases divided by the sample size). Regarding the prevalence of overall associated comorbidities, the figure was explicitly provided by most authors. When this figure was missing, it was extracted by the addition of the prevalence rates of the well-established associated diseases: IBD, arthritis, and hematological and solid malignancies. Renal failure and endocrine and metabolic conditions were not considered as relevant associated diseases [10,11,12] because there is not enough evidence and biological plausibility to suggest that these conditions are implicated in the pathogenesis of PG. Prevalence figures and 95% confidence intervals (CIs) were extracted or calculated from the available data using Wilson’s method [13].
2.3 Methodological Quality Assessment
The quality of the studies was peer reviewed by K.K. and A.D.C. using a modified version of the Newcastle–Ottawa Scale (NOS) for observational studies [14]. The original NOS was developed for case-control and cohort studies; however, some authors have adapted it for cross-sectional studies [15, 16], using the applicable items for this type of investigation. Because all eligible studies were cross-sectional, the scoring system summarized five aspects of each one of the included studies: case definition adequacy, representativeness of the cases, ascertainment of outcome data, and rate of sample loss. We have added a criterion concerning sample size, attributing one point for cohorts including more than 50 patients. The scale scores ranged from 0 (lowest grade) to 5 (highest grade). Studies with scores above the median (2) were classified as high-quality studies. Sensitivity analyses were performed for studies with modified NOS scores less than 3 or 3 and higher.
2.4 Statistical Analysis
Owing to the relative dearth of well-constructed studies regarding this topic, we decided a priori to include all studies in the meta-analysis regardless of study quality. The overall pooled estimate and 95% CI were obtained using either a fixed-effects (inverse variance methods) or random-effects (DerSimonian and Laird) meta-analysis model as appropriate depending on a test for heterogeneity. Significant heterogeneity of results was detected across studies as judged by a Cochrane Q statistic p value of < 0.05, an I2 statistic > 50%, or both. A two-sided p value of 0.05 was taken as significant. Begg rank correlation and funnel plot regression were used to assess for potential publication bias.
Potential influences on prevalence estimates were investigated using subgroup analyses and meta-regression. We assessed the influence on estimates of the following study-level variables identified a priori as potential sources of variation in the estimates of prevalence: (1) study settings (monocenter vs. multicenter vs. population based), (2) sample size (≥ or < the median number of patients [30]), and (3) study quality score (> or ≤ the median score [2]). Statistical analyses were conducted by using the Comprehensive Meta-Analysis software, Version 3.3 (Biostat, Inc., Englewood, NJ, USA).
3 Results
The literature search yielded 547 manuscripts. Five additional articles were identified from other sources. One hundred and ninety-seven articles were duplicates, and 320 were not related to comorbidities in PG. Full-text review was performed on the remaining 35 articles. Overall, 21 studies fulfilled the eligibility criteria and were included in the quantitative synthesis. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram is demonstrated in Fig. 1.
3.1 Study Characteristics
The 21 eligible studies comprised a total of 2611 patients with PG from 11 countries, encompassing participants of all ages, both male and female. Published years of studies ranged from 1985 to 2017, and the follow-up period covered the years 1970–2015. The mean age of patients with PG in the different study cohorts ranged between 48 years in Tunisia [17] and 71 years in Australia [18]. Apart from three studies from USA [19], Spain [20], and Tunisia [17], a female predominance was reported in all the remaining cohorts, with the female percentage ranging between 52% [21] and 79% [22]. One study was a prospective cohort study [21], whereas the remaining 20 were retrospective studies. Fourteen studies were monocentric, five studies were multicentric [12, 23,24,25,26], and two studies were population based [27, 28]. Quality assessment using the modified NOS revealed that the median score was 2, with seven studies scoring 3 or greater. The characteristics of the eligible studies are demonstrated in Table 1.
3.2 Overall Associated Systemic Diseases
The overall random-effects pooled prevalence of associated diseases among patients with PG was 56.8% (95% CI 45.5–67.4; I2 = 95.1%; p < 0.001) across the 21 studies. The prevalence of associated diseases ranged between 19.0% (95% CI 16.9–21.3) in Germany [28] and 86.2% (95% CI 68.5–94.7) in Australia [18] (Fig. 2).
3.3 Inflammatory Bowel Disease
The pooled prevalence of IBD was 17.6% (95% CI 13.0–22.7; I2 = 86.1%; p < 0.001) across all studies (Fig. 1 of the ESM). This combined estimate represents the leading underlying comorbidity in patients with PG. IBD was the most common associated disease in 13 out of the 21 eligible studies, and its prevalence ranged between 4.8% (95% CI 0.7–27.1) in Italy [21] and 42.3% (95% CI 25.2–61.5) in Spain [29] (Table 1).
Ulcerative colitis was the more frequent subtype with a pooled prevalence of 11.5% (95% CI 7.2–16.6; I2 = 83.7%; p < 0.001), and embodied the most common comorbidity in four studies [17, 20, 24, 29]. Crohn’s disease was less common in most cohorts, showing a pooled prevalence of 6.0% (95% CI 3.9–8.5; I2 = 66.5%; p < 0.001). Ulcerative colitis was more prevalent than Crohn’s disease in 70.6% of the cohorts that differentiated between the different subtypes of IBD (n = 17), whereas the distribution of the two subtypes was equal in 17.6% of these cohorts [10, 30, 31]. In the remaining two studies (11.8%) [18, 28], Crohn’s disease was more prevalent (Table 1).
3.4 Arthritis
The second leading associated disease was inflammatory arthritis, with a combined prevalence of 12.8% (95% CI 9.2–16.9; I2 = 82.9%; p < 0.001). The prevalence ranged between 0% [21] and 32.6% (95% CI 23.5–43.1) [19], and the disease was reported as the predominant associated disease in three studies, including two Australian cohorts [12, 18, 32] (Table 1; Fig. 2 of the ESM). Rheumatoid arthritis was the most common associated arthritis, with a pooled prevalence of 8.7% (95% CI 7.2–10.3; I2 = 67.7%; p < 0.001).
3.5 Hematological Malignancies
Hematological malignancies represented the third leading comorbid condition among patients with PG with a pooled prevalence of 8.9% (95% CI 6.5–11.6; I2 = 69.7%; p < 0.001). These conditions were the leading comorbidity in PG in three studies [11, 21, 22], and its prevalence ranged between 0% [20] and 25% (95% CI 11.7–45.6; Fig. 3 of the ESM) [22]. Monoclonal gammopathy was the most common specific hematological malignancy, and its pooled prevalence was 4.8% (95% CI 2.5–7.8; I2 = 75.9%; p < 0.001).
3.6 Solid Malignancies
Solid malignancies showed a pooled prevalence of 7.4% (95% CI 5.8–9.1; I2 = 79.5%; p < 0.001) among patients with PG at their presentation. Reported prevalence of these conditions ranged between 0% [10, 17, 20, 25, 33] and 20.7% (95% CI 8.2–37.0) [18], with three studies [23, 27, 28] lacking the precise prevalence (Fig. 4 of the ESM). No predilection for a specific solid tumor was observed across eligible studies.
3.7 Pathergy Phenomenon
In 16.3% (95% CI 7.7–27.1; I2 = 94.4%; p < 0.001) of patients with PG reported in the literature, the disease onset was attributed to the pathergy phenomenon. While two studies did not report the prevalence of this phenomenon [27, 28], its prevalence ranged between 0% [10, 17, 21, 23, 24] and 61.5% (95% CI 42.1–77.9) [32] in the remaining studies.
3.8 Exploration of Heterogeneity
Potential sources of heterogeneity were explored using a stratified analysis of the included studies. Pooling of estimates according to the study settings suggests an increase in the prevalence of associated diseases in monocenter (61.4%; 95% CI 50.1–71.7; I2 = 78.4%; p < 0.001) and multicenter (58.2%; 95% CI 42.8–72.2; I2 = 92.2%; p < 0.001) studies relative to population-based studies (25.2%; 95% CI 14.0–41.0; I2 = 96.4%; p < 0.001; Table 2).
3.9 Publication Bias
Publication bias was not detected as judged by the non-significant Begg rank correlation or funnel plot regression for the main outcome of the study (the prevalence of overall associated comorbidities; p = 0.314; Fig. 5 of the ESM).
4 Discussion
This is the first systematic review and meta-analysis aiming to summarize the prevalence of underlying diseases in PG. This study suggests that more than half of patients with PG present with a relevant underlying systemic disease, with IBD being the leading associated disease, followed by arthritis and hematological and solid malignancies. The pooled prevalence of the triggering pathergy phenomenon was as high as 16.3%.
The current knowledge about associated comorbidities in PG is severely hampered by the paucity of well-designed large-scale studies. The common teaching textbooks and expert reviews report an association with underlying diseases between 50 and 70% of the patients [34,35,36]. Older textbooks reported such an association in up to 80% of the patients [37]. Although our pooled synthesis lends weight to the current knowledge with regard to the overall prevalence of associated diseases, the distribution of these diseases is discordant [36]. While the prevalence of inflammatory arthritis and hematological malignancies were evaluated in a recent textbook at 20 and 15–25% [36], respectively, the corresponding pooled estimates of these conditions in our study were 12.8 and 8.9%. The tendency of the current literature to overestimate the prevalence of arthritis and hematological malignancies is paralleled with a tendency to underestimate the prevalence of solid malignancies. Intriguingly, the pooled prevalence of solid malignancies was as high as 7.4%. The pathergy phenomenon has previously been reported in about 30% of patients with pre-existing PG [36, 38]. The pooled prevalence of pathergy in our analysis (16.3%) reflects only patients in whom the onset of PG was attributed directly to this phenomenon. This may explain the lower estimate relative to the literature.
In a stratified analysis, the prevalence of associated systemic diseases was higher in hospital-based studies (both monocenter and multicenter studies) as compared with population-based studies. This observation may be attributed to ascertainment bias, as individuals in a tertiary-care setting may be more likely to be diagnosed with PG in a setting of concurrent disease, or equally might be more likely to have a minor manifestation of an associated disease or asymptomatic disease investigated once they are diagnosed with PG [27]. In addition, a selection bias in hospital-based studies leading to overestimation of underlying diseases is highly probable.
This study has several limitations to consider. The majority of studies in this review were retrospective and observational, with several methodological limitations. Moreover, the pooled studies had different inclusion/exclusion criteria, sample sizes, sampling approaches, and geographic locations. Owing to the high level of heterogeneity among most of the comparisons, results should be interpreted with caution. Although the funnel plot did not reveal the existence of publication bias in the current study, this test is difficult to understand in an observational study of prevalence.
5 Conclusions
Underlying systemic disease is present in approximately 57% of patients with PG. IBD, arthritis, and hematological and solid malignancies are the leading associated diseases. Relative to the current literature, the pooled prevalence of arthritis and hematological diseases is lower, while the prevalence of solid malignancies is higher than believed. These findings confirm the association of PG with solid malignancies.
References
Marzano AV, Ishak RS, Saibeni S, Crosti C, Meroni PL, Cugno M. Autoinflammatory skin disorders in inflammatory bowel diseases, pyoderma gangrenosum and Sweet’s syndrome: a comprehensive review and disease classification criteria. Clin Rev Allergy Immunol. 2013;45:202–10.
Marzano AV, Damiani G, Ceccherini I, Berti E, Gattorno M, Cugno M. Autoinflammation in pyoderma gangrenosum and its syndromic form (pyoderma gangrenosum, acne and suppurative hidradenitis). Br J Dermatol. 2017;176:1588–98.
Marzano AV, Fanoni D, Antiga E, Quaglino P, Caproni M, Crosti C, et al. Expression of cytokines, chemokines and other effector molecules in two prototypic autoinflammatory skin diseases, pyoderma gangrenosum and Sweet’s syndrome. Clin Exp Immunol. 2014;178:48–56.
Marzano AV, Cugno M, Trevisan V, Fanoni D, Venegoni L, Berti E, et al. Role of inflammatory cells, cytokines and matrix metalloproteinases in neutrophil-mediated skin diseases. Clin Exp Immunol. 2010;162:100–7.
Braswell SF, Kostopoulos TC, Ortega-Loayza AG. Pathophysiology of pyoderma gangrenosum (PG): an updated review. J Am Acad Dermatol. 2015;73:691–8.
Marzano AV, Borghi A, Meroni PL, Cugno M. Pyoderma gangrenosum and its syndromic forms: evidence for a link with autoinflammation. Br J Dermatol. 2016;175(5):882–91.
Wollina U. Clinical management of pyoderma gangrenosum. Am J Clin Dermatol. 2002;3:149–58.
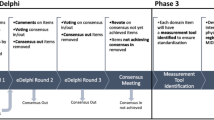
Maverakis E, Ma C, Shinkai K, Fiorentino D, Callen JP, Wollina U, et al. Diagnostic criteria of ulcerative pyoderma gangrenosum: a Delphi Consensus of International Experts. JAMA Dermatol. 2018. https://doi.org/10.1001/jamadermatol.2017.5980 (epub ahead of print).
Reichrath J, Bens G, Bonowitz A, Tilgen W. Treatment recommendations for pyoderma gangrenosum: an evidence-based review of the literature based on more than 350 patients. J Am Acad Dermatol. 2005;53:273–83.
Hasselmann DO, Bens G, Tilgen W, Reichrath J. Pyoderma gangrenosum: clinical presentation and outcome in 18 cases and review of the literature. J Dtsch Dermatol Ges. 2007;5:560–4.
Al Ghazal P, Körber A, Klode J, Dissemond J. Investigation of new co-factors in 49 patients with pyoderma gangrenosum. Dtsch Dermatol Ges. 2012;10:251–7.
Al Ghazal P, Herberger K, Schaller J, Strölin A, Hoff N-P, Goerge T, et al. Associated factors and comorbidities in patients with pyoderma gangrenosum in Germany: a retrospective multicentric analysis in 259 patients. Orphanet J Rare Dis. 2013;8:136.
Newcombe RG. Two-sided confidence intervals for the single proportion: comparison of seven methods. Stat Med. 1998;17:857–72.
Stang A. Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–5.
Barbosa KGN, de Macedo Bernardino Í, d’Avila S, Ferreira EFE, Ferreira RC. Systematic review and meta-analysis to determine the proportion of maxillofacial trauma resulting from different etiologies among children and adolescents. Oral Maxillofac Surg. 2017;21:131–45.
Hermont AP, Oliveira PA, Martins CC, Paiva SM, Pordeus IA, Auad SM. Tooth erosion and eating disorders: a systematic review and meta-analysis. PLoS One. 2014;9:e111123.
Mlika RB, Riahi I, Fenniche S, Mokni M, Raouf Dhaoui M, Dess N, et al. Pyoderma gangrenosum: a report of 21 cases. Int J Dermatol. 2002;41:65–8.
Cabalag MS, Wasiak J, Lim SW, Raiola FB. Inpatient management of pyoderma gangrenosum: treatments, outcomes, and clinical implications. Ann Plast Surg. 2015;74:354–60.
Powell FC, Schroeter AL, Su WP, Perry HO. Pyoderma gangrenosum: a review of 86 patients. Q J Med. 1985;55:173–86.
Suárez-Pérez JA, Herrera-Acosta E, López-Navarro N, Vilchez-Márquez F, Prieto JD, Bosch RJ, et al. Pyoderma gangrenosum: a report of 15 cases and review of the literature. Actas Dermosifiliogr. 2012;103:120–6.
Marzano AV, Trevisan V, Lazzari R, Crosti C. Pyoderma gangrenosum: study of 21 patients and proposal of a “clinicotherapeutic” classification. J Dermatolog Treat. 2011;22:254–60.
Pereira N, Brites MM, Goncalo M, Tellechea O, Figueiredo A. Pyoderma gangrenosum: a review of 24 cases observed over 10 years. Int J Dermatol. 2013;52:938–45.
Bennett ML, Jackson JM, Jorizzo JL, Fleischer AB Jr, White WL, Callen JP. Pyoderma gangrenosum: a comparison of typical and atypical forms with an emphasis on time to remission. Case review of 86 patients from 2 institutions. Medicine (Baltimore). 2000;79:37–46.
Inoue S, Furuta JI, Fujisawa Y, Onizawa S, Ito S, Sakiyama M, et al. Pyoderma gangrenosum and underlying diseases in Japanese patients: a regional long-term study. J Dermatol. 2017;44:1281–4.
Binus AM, Qureshi AA, Li VW, Winterfield LS. Pyoderma gangrenosum: a retrospective review of patient characteristics, comorbidities and therapy in 103 patients. Br J Dermatol. 2011;165:1244–50.
Jockenhöfer F, Herberger K, Schaller J, Hohaus KC, Stoffels-Weindorf M, Ghazal PA, et al. Tricenter analysis of cofactors and comorbidity in patients with pyoderma gangrenosum. J Dtsch Dermatol Ges. 2016;14:1023–30.
Langan SM, Groves RW, Card TR, Gulliford MC. Incidence, mortality, and disease associations of pyoderma gangrenosum in the United Kingdom: a retrospective cohort study. J Invest Dermatol. 2012;132:2166–70.
Jockenhofer F, Klode J, Kroger K, Roesch A, Al Ghazal P, Dissemond J. Patients with pyoderma gangrenosum: analyses of the German DRG data from 2012. Int Wound J. 2016;13:951–6.
Vidal D, Puig L, Gilaberte M, Alomar A. Review of 26 cases of classical pyoderma gangrenosum: clinical and therapeutic features. J Dermatolog Treat. 2004;15:146–52.
Von Den Driesch P. Pyoderma gangrenosum: a report of 44 cases with follow-up. Br J Dermatol. 1997;137:1000–5.
Ye MJ, Ye JM. Pyoderma gangrenosum: a review of clinical features and outcomes of 23 cases requiring inpatient management. Dermatol Res Pract. 2014;2014:461467.
Saracino A, Kelly R, Liew D, Chong A. Pyoderma gangrenosum requiring inpatient management: a report of 26 cases with follow up. Australas J Dermatol. 2011;52:218–21.
Vacas AS, Torre AC, Bollea-Garlatti ML, Warley F, Galimberti RL. Pyoderma gangrenosum: clinical characteristics, associated diseases, and responses to treatment in a retrospective cohort study of 31 patients. Int J Dermatol. 2017;56:386–91.
Callen JP, Jackson JM. Pyoderma gangrenosum: an update. Rheum Dis Clin North Am. 2007;33:787–802.
Jackson JM, Callen JP. Pyoderma gangrenosum: an expert commentary. Expert Rev. Dermatol. 2006;1:391–400.
Davis MDP, Moschella SL. Neutrophilic dermatoses. In: Bolognia J, Schaffer J, Cerroni L, editors. Dermatology. 4th ed. Philadelphia; Elsevier; 2017. p. 453–71.
Wolff K, Stingl G. Pyoderma gangrenosum. In: Freedberg I, Eisen A, Wolff K, editors. Fitzpatrick’s dermatology in general medicine. 5th ed. New York (NY): McGraw-Hill; 1999. p. 2207–13.
Jackson JM, Callen JP. Pyoderma gangrenosum: background, epidemiology, prognosis. 2017. Available from: https://emedicine.medscape.com/article/1123821-overview. Accessed 20 Dec 2017.
Adisen E, Erduran F, Gurer MA. Pyoderma gangrenosum: a report of 27 patients. Int J Low Extrem Wounds. 2016;15:148–54.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for the conduct of this study or the preparation of this article.
Conflict of interest
Khalaf Kridin, Arnon D. Cohen, and Kyle T. Amber have no conflicts of interest directly relevant to the content of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kridin, K., Cohen, A.D. & Amber, K.T. Underlying Systemic Diseases in Pyoderma Gangrenosum: A Systematic Review and Meta-Analysis. Am J Clin Dermatol 19, 479–487 (2018). https://doi.org/10.1007/s40257-018-0356-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-018-0356-7