Abstract
Purpose of Review
Controversy surrounds the construct of food addiction. The current review examines neurobiological evidence for the existence of food addiction as a valid diagnosis.
Recent Findings
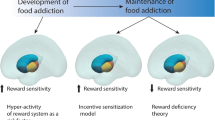
Recent neuroimaging studies suggest significant overlap in the areas of the brain that are activated in relation to both food and drug addiction. Specifically, areas of the brain implicated in executive functioning (e.g., attention, planning, decision-making, inhibition), pleasure and the experience of reward, and sensory input and motor functioning display increased activation among individuals with symptoms of both food and drug addiction.
Summary
Proposed symptoms of food addiction mirror those comprising other substance use disorder diagnoses, with similar psychological and behavioral sequelae. Results of neuroimaging studies suggest significant overlap in the areas of the brain that are activated in relation to both food and drug addiction, providing support for continued research into the construct of food addiction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past decade, the concept of “food addiction” has become a topic of both increasing interest and debate. In 2009, Gearhardt, Corbin, and Brownell [1] published the Yale Food Addiction Scale (YFAS), a questionnaire designed to evaluate the similarities between excessive consumption of certain foods and criteria for substance dependence, as defined in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) [2]. Since the preliminary validation of this instrument, studies on the concept of food addiction have increased exponentially, with over 1000 peer-reviewed papers published in the past 5 years. This surge in research has produced evidence suggesting that some people may experience addictive-like responses to certain foods, particularly processed foods that are high in fat and/or sugar [for reviews, see 3••, 4••]. The current literature on food addiction includes a variety of study populations and methodologies, including the use of both behavioral and neurobiological measures. This review specifically summarizes the most recent neurobiological studies examining the link between food composition and behavior with addictive-like responses in the human brain.
Search Strategy and Selection Criteria
The “all databases” option in EBSCOhost was used to search for peer-reviewed original research articles published between 2014 and 2019. Search terms used included “food addiction” and “brain.” The search produced 1223 articles, which was reduced to 90 after elimination of irrelevant or duplicate articles. Criteria were then refined to include only studies measuring brain activity in human subjects, resulting in 15 final articles. Findings were organized by the brain area/function that was examined in each study and are presented accordingly below. The characteristics of included studies are described in Table 1.
The majority of studies related to the association between food composition and addictive-like effects in the brain tested the effects of foods high in sugar (e.g., chocolate milkshake, sweetened drinks, chocolate cake) or processing (e.g., high-sugar/high-fat “snacks,” hotdogs) on brain activity in areas related to control/self-awareness and pleasure/reward, with some also including areas related to visual/sensory input and motor functioning. Of the studies included in this review, 11 included adult samples, 3 included children, and 1 included both adults and children.
Areas Related to Executive Control, Inhibition, and Self-Awareness
Findings from multiple neuroimaging studies have suggested a link between individual variables associated with food addiction (e.g., body weight status, compulsive or binge eating behaviors, food composition, YFAS symptoms) and neurological activity in areas of the brain associated with executive control, inhibition, and self-awareness. In general, these results mirror the findings from studies examining neurological activity in other substance use disorders (SUDs). For example, Imperatori and colleagues conducted an electroencephalographic (EEG) study comparing changes in brain wave patterns between overweight/obese adults with three or more symptoms of food addiction on the YFAS (n = 14) compared to those with fewer than three symptoms (n = 14) after a taste of chocolate milkshake [5]. The authors observed that participants with three or more food addiction symptoms showed increased theta power in the right inferior frontal gyrus and increased delta activity in the right middle frontal gyrus (i.e., areas associated with a loss of inhibitory control) [6, 7] compared to controls. Furthermore, participants with three or more YFAS symptoms also had increased functional connectivity in the alpha and theta bands of the fronto-parietal areas (i.e., areas associated with internal attention processes) [8], which in turn was positively correlated with total number of YFAS symptoms. According to the authors, these responses were similar to other findings that have suggested a role for alpha, theta, and delta frequencies in the context of substance use disorders, particularly with regard to craving and withdrawal [5, 9, 10]. For example, Reid and colleagues observed increased frontal theta and delta power in response to cocaine imagery among participants with cocaine dependence [11].
Schulte and colleagues published a functional magnetic resonance imaging (fMRI) study analyzing brain responses to images of highly processed foods [12]. The participants (44 women with BMIs in the overweight or obese ranges) participated in a cue-reactivity task in which they were shown pictures of household objects (control), minimally processed foods, and highly processed foods. While viewing the images, participants were asked to think about how much they wanted the item shown. The authors compared results between women who met YFAS 2.0 criteria for moderate-to-severe food addiction (n = 20) and those who did not (n = 24). Results indicated that women who met YFAS 2.0 criteria for food addiction had elevated activity in the superior frontal gyrus (i.e., an area associated with executive functioning and potentially craving among individuals with substance use disorder) [13, 14] when exposed to images of highly processed foods but showed reduced activity in response to minimally processed food images. Women who did not meet the criteria for food addiction displayed the opposite results. The authors concluded that women who meet criteria for clinically significant food addiction symptoms on the YFAS 2.0 experience unique brain responses to highly processed foods, similar to what is observed among individuals with SUD, when compared to women who are overweight or obese but not addicted to food.
Simon and colleagues also used fMRI to compare women who engage in binge eating (i.e., meet criteria for binge eating disorder or bulimia) to healthy controls [15]. They found increased activity in the prefrontal and orbitofrontal cortices (i.e., areas associated with executive functioning, including behavior regulation) [6] in response to a food reward task among the women who engage in binge eating compared to controls. Similarly, Kahathuduwa and colleagues conducted a 3-week randomized controlled trial (n = 32 adults with obesity) to compare the effects of a diet including only meal replacement shakes to a calorie-matched, portion-controlled solid food diet [16]. The variables of interest included fMRI food cue reactivity, fMRI functional connectivity, and other measures (e.g., YFAS, weight, cravings). The authors found that the liquid-only diet produced greater food cue reactivity in the bilateral dorsolateral prefrontal cortex and orbitofrontal cortex regions compared to the non-liquid, calorie-matched diet, concluding that this may reflect greater executive control in the areas of the brain that regulate food reward and ingestion.
Guzzardi and colleagues used PET scans to assess brain responses to food cues among 36 women with BMIs of 25 kg/m2 or greater (i.e., women in the overweight or obese ranges) [17]. The authors tested the women before and after a 3-month diet consisting of three meals and two snacks that totaled up to 1600 kcal/day (50% carbohydrates, 30% fats, and 20% proteins). They compared participants with “high” (3+ symptoms) versus “low” (< 3 symptoms) scores on the Yale Food Addiction Scale. At baseline, the authors reported observing a significant inverse relation between orbitofrontal activity and hunger ratings and YFAS severity in the high-YFAS group, as well as positive correlations between lipid consumption (measured by 24-h dietary recall) and brain activity in the orbitofrontal cortex, temporal cortex, and prefrontal cortex. However, after maintaining the prescribed diet for 3 months, the groups no longer displayed differences on any of the measures. They concluded that, while YFAS scores can distinguish differential responses in the brain to food cues, these differences may be eliminated through dietary changes.
He and associates used fMRI to test the relations between neural responses to the decision component of the Iowa Gambling Task, and dietary choices (high-fat/high-sugar snacks versus vegetables) reported on a food frequency questionnaire [18]. The sample included 23 healthy young adults and adolescents (ages 14–21). The authors found significant associations between dietary choices and brain responses during an affective decision-making task, such that greater vegetable intake correlated with greater activity in the left superior frontal gyrus, while greater intake of high-fat/high-sugar snacks correlated with reduced activity in the left frontal pole (i.e., an area associated with functions such as cognitive flexibility and motoring action outcomes) [19]. The authors concluded that different foods may be associated with an imbalanced response in the brain that affects both decision-making processes, similar to what is observed in individuals with other addictions.
Jastreboff and colleagues used fMRI to measure 38 adolescents’ neural responses to two different drinks, sweetened with glucose versus fructose (two different types of sugar), respectively [20]. The authors found that, in response to glucose, adolescents with obesity had decreased perfusion in the prefrontal cortex, whereas adolescents without obesity had the opposite response. After fructose ingestion, adolescents with obesity again had decreased perfusion in the prefrontal cortex. The authors concluded that adolescents with obesity may have reduced executive control (prefrontal cortex) in response to consuming either of these two sugars.
In a sample of 24 adolescents, Feldstein Ewing and associates used fMRI to examine (1) brain responses to low- versus high-calorie drinks, (2) the associations of those responses with other variables such as BMI and insulin resistance, and (3) the relation between self-reported food addiction symptoms and brain responses to a cue-exposure task [21]. For high-calorie beverages, the researchers observed an increased BOLD response in the orbitofrontal cortex, inferior frontal gyrus, and other temporal and frontoparietal regions. The authors reported that these brain responses to high-calorie drinks paralleled those seen in addiction neural pathways. Contrary to their predictions, however, there was no relation between self-reported food addiction symptoms and brain activation.
Finally, Boutelle and colleagues analyzed fMRI brain differences between children (ages 8–12), with and without obesity, while tasting sucrose and water [22]. Among children with obesity, the researchers observed greater activation in the medial frontal gyrus and middle frontal gyri to sucrose (sugar) compared to water. Children without obesity had the reverse response, such that these areas of the brain responded more to water than to sucrose. The authors also found that children with obesity recruited the medial, lateral frontal, and temporal regions bilaterally, compared to children without obesity.
Taken together, these findings suggest that brain processes involved in activities such as executive control, inhibition, and self-awareness can be affected by food cues and diet and that these effects may be different among those with higher weight status and/or binge- or addictive-like eating. Specifically, highly palatable/processed foods (e.g., high-sugar snacks, sweetened beverages) affect these areas differently than minimally processed foods (e.g., vegetables) in individuals with or without problematic eating behaviors. Furthermore, adults who report addictive-like or binge eating behaviors also appear to have opposite brain responses in these areas in response to highly palatable foods, compared to those who do not report these behaviors, and children with obesity may experience different responses compared to those without. Notably, two studies suggested that dietary changes may be able to reverse these effects in adults.
Areas Related to Pleasure and Reward
Similar to the aforementioned findings regarding the link between food addiction symptoms/correlates and brain areas associated with executive functioning and self-control, studies examining areas of the brain associated with pleasure and reward also demonstrate differential responses according to diet, weight status, and eating behaviors. Imperatori and colleagues’ study found that chocolate milkshake tasting produced not only changes in the right middle and right inferior frontal gyri but also in the right insula, an area typically associated with both pleasure and decision-making in the context of drug addiction [5, 23]. Similarly, in their study of adolescents and young adults, He and associates found that greater vegetable intake was associated with reduced activity in the right insular cortex during a decision-making task [18]. Greater intake of high-fat/high-sugar snacks, however, correlated with increased activity in the right insular cortex and ventral striatum (i.e., areas associated with reward and pleasure) [23, 24].
Jastreboff and colleagues found that adolescents with obesity had increased perfusion in the hypothalamus (i.e., associated with appetite and homeostasis) [25] in response to glucose, while those without obesity did not [20]. Furthermore, they reported that all adolescents in their sample had greater perfusion responses to fructose in the ventral striatum compared with the response to glucose consumption. Boutelle and colleagues similarly observed greater activation in the amygdala (i.e., an area associated with impulsive decision-making) [6] and bilateral insula to both sucrose and water among children with obesity, compared to controls [22]. In addition, children with obesity had greater responses to sucrose compared to water in areas such as the right amygdala and paracingulate gyrus (i.e., associated with general reward processing among individuals with substance dependence) [26], whereas in controls these areas responded more to water than to sucrose. The authors also found that children with obesity recruited the right putamen (i.e., associated with processing of reward) [26] more than controls; however, they did not have increased responses in the striatum as the authors had hypothesized. In an adolescent sample, Feldstein Ewing and associates also found greater BOLD responses to high-calorie beverages in the nucleus accumbens (i.e., another area associated with pleasure) [25] and right amygdala compared to a low-calorie beverage [21].
Kahathuduwa and associates found that their liquid-only diet also resulted in increased food cue reactivity in the following reward-related regions: the anterior cingulate cortex, the left insular cortex, and the bilateral nucleus accumbens compared to controls [16]. They also found that the intervention was associated with negative food cue reactivity modulation in the amygdala and nucleus accumbens. Guzzardi and colleagues observed that, prior to their calorie-controlled dietary intervention, the high-YFAS group had greater activity in reward regions of the brain (i.e., the hypothalamus, thalamus, midbrain, and putamen) in response to palatable food cues (e.g., chocolate cake) compared to the low-YFAS group [17]. In addition, they found a significant positive correlation between lipid consumption and activation in the thalamus, hypothalamus, midbrain, and orbitofrontal cortex among the high-YFAS participants. These differences disappeared post-intervention.
Using fMRI, Kilpatrick and associates [27] investigated the differential effects of consuming juice sweetened with sugar versus Truvia (a zero-calorie sweetener derived from the stevia leaf) on the brainstem vagal pathways and hypothalamus in women with and without obesity. They found that, after consuming the drink with sugar, both groups showed greater blood oxygen level-dependent fluctuations in the highest frequency band of the nucleus tractus solitarius (involved in visceral input and homeostasis) compared to Truvia. Additionally, women with obesity (n = 11) had increased connectivity between the putamen, cerebellum, and the right lateral hypothalamus, along with weaker connectivity between gustatory-related brain regions and homeostasis, compared to women without obesity (n = 11). Furthermore, women with obesity gave lower self-reported taste ratings to both drinks (which did not subjectively differ in taste) compared to women without obesity, suggesting that their perceived hedonic response was lower. The authors concluded that women with obesity may have enhanced coordination between the lateral hypothalamus low frequency oscillations and those in the reward centers and weaker coordination between the lateral hypothalamus low frequency oscillations and those in the gustatory and homeostatic regions of the brain.
Smith and colleagues examined activation of the dorsal anterior cingulate cortex (i.e., associated with emotion and reward-based decisions) [28], and its functional connectivity with the anterior insula during a decision-making task [29]. Twenty adult men and women were shown two foods and asked to “choose the healthier option” (e.g., hotdog versus shrimp, cheeseburger versus salad) while undergoing fMRI. The authors found that dorsal anterior cingulate cortex activation correlated with self-reported high-fat food cravings and desire to eat. Additionally, participants who reported greater self-control over eating were more likely to have negative functional connectivity between the dorsal anterior cingulate cortex and the right anterior insula. The authors concluded that these brain patterns suggest a “greater response conflict” [29, p. 692] during a healthy eating decision-making task, as well as identifying a significant relationship between self-reported control over eating and the strength of signaling from the body, mediated by the insula. In other words, individuals who have weaker insula-mediated signaling from their bodies may be more prone to feeling out of control with their eating.
Geliebter, Benson, Pantazatos, Hirsch, and Carnell compared neural responses via fMRI to high-calorie and low-calorie food cues in women with and without binge eating disorder and with and without obesity [30]. Women with binge eating, regardless of body weight, displayed hyper-responsivity of the dorsal anterior cingulate cortex in the presence of highly palatable food cues. In previous studies, heightened anterior cingulate cortex reactivity has also correlated with greater food addiction scores in the presence of a milkshake [31], as well as in cocaine users when presented with drug-related stimuli [30, 32]. Similarly, using fMRI, Simon and colleagues found heightened activity of the posterior cingulate cortex, as well as in areas of the orbitofrontal cortex, in individuals with binge eating-related disorders during a food reward task [15].
De Ridder et al. compared the EEGs of 14 individuals with alcohol use disorder, 20 healthy weight individuals, and 46 individuals with obesity who were further divided into “low food addiction” risk (low-risk FA) and “high food addiction” risk (high-risk FA) based on a median split on the YFAS [33•]. High-risk FA participants with obesity displayed neural activity similar to individuals with alcohol use disorder measured by EEG, including activity in the dorsal and pregenual anterior cingulate cortex and the posterior cingulate, among other areas. Notably, anterior cingulate cortex activity in the low-risk FA participants with obesity showed a different pattern, which the authors concluded may suggest that individuals with obesity and food addiction symptoms may have neural patterns that are distinct from individuals with obesity without food addiction symptoms. Addictive-like eating, therefore, may be a distinct phenotype present in select individuals, as opposed in to the general population with obesity.
Kroemer and colleagues’ longitudinal imaging study suggested that variability in nucleus accumbens response to highly palatable food stimuli may predict eating behavior and weight over time [34]. Participants (n = 34) underwent three fMRI sessions (hungry, fixed meal, ad libitum using a milkshake) and were asked to rate their hunger and fullness, provide anthropometric data and blood samples, complete questionnaires, participate in a “behavioral test” where they were presented with a milkshake and pasta, and instructed to eat ad libitum. Study procedures were replicated 1 year later. Results indicated that greater variability in nucleus accumbens response to milkshakes was associated with higher BMI and higher variance in food intake and glucose levels.
Finally, Eisenstein and colleagues conducted a PET scan study to investigate the relation between central dopamine (D2) receptor binding, emotional eating, and eating related to reward among 22 participants with obesity compared to 17 healthy weight adults [35]. They found that eating in response to negative affect positively correlated with striatal D2 binding, independent of BMI category (i.e., healthy or obese), suggesting that emotional eating may be related to differences in dopaminergic system functioning.
The above studies on reward and pleasure in addictive-like eating suggest that these areas of the brain (e.g., ventral striatum, nucleus accumbens, insula, cingulate cortex, etc.) are differentially activated by food (i.e., increased activation with highly palatable foods and drinks), weight status (i.e., increased reward response to highly palatable foods among people with higher weight status), and maladaptive eating behaviors (i.e., increased reward response to highly palatable foods among people with problematic eating behaviors). Importantly, differential reward responses to palatable foods appear to be more consistently influenced by maladaptive eating behaviors (e.g., addictive-like eating, binge eating, emotional eating) than by weight status.
Areas Related to Sensory Input and Motor Functioning
Several studies also analyzed brain responses in areas related to sensory input and motor functioning, due to the significant roles of these areas in both eating behaviors and addictive disorders [e.g., 36, 37, 38, 39]. For example, in their sample of adolescents, Feldstein Ewing and colleagues found positive associations between BMI and brain responses in the central operculum and right post-central gyrus [21]. They also found a link between insulin resistance and brain responses in the superior parietal lobe, left occipitofrontal cortex, and bilateral middle/superior temporal gyrus. Taken together, these results suggest that adolescents may display differing responses to high-calorie beverages in visual and/or touch-related areas of the brain based on levels of insulin sensitivity and BMI.
Similarly, in their study of overweight/obese women (described previously), Guzzardi and associates used PET scanning and found greater activity in the occipital cortex among the high-YFAS group during food cue exposure at baseline [17]. They also found a significant association between lipid consumption and postcentral gyrus activity. Similar to the results described in the section on executive control/attention, these differences also disappeared post-intervention. Finally, Kahathuduwa and colleagues found that their liquid diet produced greater food cue reactivity in the primary motor cortex compared to the control diet, which the authors concluded may suggest increased “readiness to eat” [16]. This pattern of findings related to sensory and motor areas of the brain also appears to mirror the patterns of activation described in the drug addiction literature.
Conclusion: Neuroimaging Research Supports the Construct of Food Addiction
At this time, “food addiction” remains primarily a theoretical construct, which is not included as an official diagnosis in the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition [40] or the International Statistical Classification of Diseases and Related Health Problems, 11th Edition [41]. However, research continues to accumulate supporting the food addiction phenotype observed in clinical practice. Proposed symptoms for food addiction mirror those comprising other substance use disorder diagnoses, with similar psychological and behavioral sequelae. Further, as reviewed here, neuroimaging studies suggest significant overlap in the areas of the brain that are activated in relation to both food and drug addiction. Specifically, areas of the brain implicated in executive functioning (e.g., attention, planning, decision-making, inhibition) show similar patterns in both groups. Similarly, as seen among individuals with substance use disorders, the pleasure center of the brain and areas associated with the experience of reward demonstrate heightened activity and increased sensitivity among individuals with symptoms of food addiction. Finally, the brain regions associated with sensory input and motor functioning display increased activation among individuals with symptoms of both food and drug addiction, which may contribute to “triggers” or other cues that increase their readiness to use the substance (whether food or drugs). In summary, these findings provide support for continued research into the construct of food addiction, with the goal of developing diagnostic criteria that might be used in clinical care to aid in assessment and treatment planning for individuals suffering with this condition.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale food addiction scale. Appetite. 2009;52(2):430–6. https://doi.org/10.1016/j.appet.2008.12.003.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author; 2000. doi:https://doi.org/10.1176/appi.books.9780890423349.
•• Gordon EL, Ariel-Donges AH, Bauman V, Merlo LJ. What is the evidence for “food addiction?” a systematic review. Nutrients. 2018;10(4):477. https://doi.org/10.3390/nu10040477This systematic review discusses peer-reviewed research with the intent of evaluating the validity of the food addiction concept. It evaluates the ways in which food addiction research findings do and do not support a resemblance to substance use disorder.
•• Pursey KM, Davis C, Burrows TL. Nutritional aspects of food addiction. Curr Addict Rep. 2017;4(2):142–50. https://doi.org/10.1007/s40429-017-0139-xThis review summarizes findings related to food composition and addictive-like symptoms. Its findings suggest that hyper-palatable, highly processed foods with a combination of fat and sugar are more likely to be associated with an addictive response. While glycemic load and total fat content also appear to play a role, evidence was not strong for an association between high-sugar-only foods and food addiction.
Imperatori C, Fabbricatore M, Innamorati M, Farina B, Quintiliani MI, Lamis DA, et al. Modification of EEG functional connectivity and EEG power spectra in overweight and obese patients with food addiction: an eLORETA study. Brain Imaging Behav. 2015;9(4):703–16. https://doi.org/10.1007/s11682-014-9324-x.
Crews FT, Boettiger CA. Impulsivity, frontal lobes and risk for addiction. Pharmacol Biochem Behav. 2009;93(3):237–47. https://doi.org/10.1016/j.pbb.2009.04.018.
Parvaz MA, Alia-Klein N, Woicik PA, Volkow ND, Goldstein RZ. Neuroimaging for drug addiction and related behaviors. Rev Neurosci. 2011;22(6):609–24. https://doi.org/10.1515/RNS.2011.055.
Lückmann HC, Jacobs HI, Sack AT. The cross-functional role of frontoparietal regions in cognition: internal attention as the overarching mechanism. Prog Neurobiol. 2014;116:66–86. https://doi.org/10.1016/j.pneurobio.2014.02.002.
Knyazev GG. Motivation, emotion, and their inhibitory control mirrored in brain oscillations. Neurosci Biobehav Rev. 2007;31(3):377–95. https://doi.org/10.1016/j.neubiorev.2006.10.004.
Knyazev GG. EEG delta oscillations as a correlate of basic homeostatic and motivational processes. Neurosci Biobehav Rev. 2012;36(1):677–95. https://doi.org/10.1016/j.neubiorev.2011.10.002.
Reid MS, Prichep LS, Ciplet D, O'Leary S, Tom M, Howard B, et al. Quantitative electroencephalographic studies of cue-induced cocaine craving. Clin Electroencephalogr. 2003;34(3):110–23. https://doi.org/10.1016/j.nutres.2014.09.010.
Schulte EM, Yokum S, Jahn A, Gearhardt AN. Food cue reactivity in food addiction: a functional magnetic resonance imaging study. Physiol Behav. 2019;208:112574. https://doi.org/10.1016/j.physbeh.2019.112574.
Boisgueheneuc FD, Levy R, Volle E, Seassau M, Duffau H, Kinkingnehun S, et al. Functions of the left superior frontal gyrus in humans: a lesion study. Brain. 2006;129(12):3315–28. https://doi.org/10.1093/brain/awl244.
Garavan H, Pankiewicz J, Bloom A, Cho JK, Sperry L, Ross TJ, et al. Cue-induced cocaine craving: neuroanatomical specificity for drug users and drug stimuli. Am J Psychiatr. 2000;157(11):1789–98. https://doi.org/10.1176/appi.ajp.157.11.1789.
Simon JJ, Skunde M, Walther S, Bendszus M, Herzog W, Friederich HC. Neural signature of food reward processing in bulimic-type eating disorders. Soc Cogn Affect Neurosci. 2016;11(9):1393–401. https://doi.org/10.1093/scan/nsw049.
Kahathuduwa CN, Davis T, O'Boyle M, Boyd LA, Chin SH, Paniukov D, et al. Effects of 3-week total meal replacement vs. typical food-based diet on human brain functional magnetic resonance imaging food-cue reactivity and functional connectivity in people with obesity. Appetite. 2018;120:431–41. https://doi.org/10.1016/j.appet.2017.09.025.
Guzzardi MA, Garelli S, Agostini A, Filidei E, Fanelli F, Giorgetti A, et al. Food addiction distinguishes an overweight phenotype that can be reversed by low calorie diet. Eur Eat Disord Rev. 2018;26(6):657–70. https://doi.org/10.1002/erv.2652.
He Q, Xiao L, Xue G, Wong S, Ames SL, Xie B, et al. Altered dynamics between neural systems sub-serving decisions for unhealthy food. Front Neurosci. 2014;8:350. https://doi.org/10.3389/fnins.2014.00350.
Koechlin E. Frontal pole function: what is specifically human? Trends Cogn Sci. 2011;15(6):241. https://doi.org/10.1016/j.tics.2011.04.005.
Jastreboff AM, Sinha R, Arora J, Giannini C, Kubat J, Malik S, et al. Altered brain response to drinking glucose and fructose in obese adolescents. Diabetes. 2016;65(7):1929–39. https://doi.org/10.2337/db15-1216.
Feldstein Ewing SW, Claus ED, Hudson KA, Filbey FM, Jimenez EY, Lisdahl KM, et al. Overweight adolescents’ brain response to sweetened beverages mirrors addiction pathways. Brain Imaging Behav. 2017;11(4):925–35. https://doi.org/10.1007/s11682-016-9564-z.
Boutelle KN, Wierenga CE, Bischoff-Grethe A, Melrose AJ, Grenesko-Stevens E, Paulus MP, et al. Increased brain response to appetitive tastes in the insula and amygdala in obese compared with healthy weight children when sated. Int J Obes. 2015;39(4):620–8. https://doi.org/10.1038/ijo.2014.206.
Naqvi NH, Bechara A. The insula and drug addiction: an interoceptive view of pleasure, urges, and decision-making. Brain Struct Funct. 2010;214(5–6):435–50. https://doi.org/10.1007/s00429-010-0268-7.
Kelley AE. Ventral striatal control of appetitive motivation: role in ingestive behavior and reward-related learning. Neurosci Biobehav Rev. 2004;27(8):765–76. https://doi.org/10.1016/j.neubiorev.2003.11.015.
Schoenberg MR, Scott JG. The little black book of neuropsychology: a syndrome-based approach. New York: Springer; 2011. https://doi.org/10.1007/978-0-387-76978-3.
García-García I, Horstmann A, Jurado MA, Garolera M, Chaudhry SJ, Margulies DS, et al. Reward processing in obesity, substance addiction and non-substance addiction. Obes Rev. 2014;15(11):853–69. https://doi.org/10.1111/obr.12221.
Kilpatrick LA, Coveleskie K, Connolly L, Labus JS, Ebrat B, Stains J, et al. Influence of sucrose ingestion on brainstem and hypothalamic intrinsic oscillations in lean and obese women. Gastroenterology. 2014;146(5):1212–21. https://doi.org/10.1053/j.gastro.2014.01.023.
Shenhav A, Botvinick MM, Cohen JD. The expected value of control: an integrative theory of anterior cingulate cortex function. Neuron. 2013;79(2):217–40. https://doi.org/10.1016/j.neuron.2013.07.007.
Smith R, Alkozei A, Killgore WD. Conflict-related dorsomedial frontal cortex activation during healthy food decisions is associated with increased cravings for high-fat foods. Brain Imaging Behav. 2018;12(3):685–96. https://doi.org/10.1007/s11682-017-9726-7.
Geliebter A, Benson L, Pantazatos SP, Hirsch J, Carnell S. Greater anterior cingulate activation and connectivity in response to visual and auditory high-calorie food cues in binge eating: preliminary findings. Appetite. 2016;96:195–202. https://doi.org/10.1016/j.appet.2015.08.009.
Gearhardt AN, Yokum S, Orr PT, Stice E, Corbin WR, Brownell KD. Neural correlates of food addiction. Arch Gen Psychiatry. 2011;68(8):808–16. https://doi.org/10.1001/archgenpsychiatry.2011.32.
Wexler BE, Gottschalk CH, Fulbright RK, Prohovnik I, Lacadie CM, Rounsaville BJ, et al. Functional magnetic resonance imaging of cocaine craving. Am J Psychiatr. 2001;158(1):86–95. https://doi.org/10.1176/appi.ajp.158.1.86.
• De Ridder D, Manning P, Leong SL, Ross S, Sutherland W, Horwath C, et al. The brain, obesity and addiction: an EEG neuroimaging study. Sci Rep. 2016;6:34122. https://doi.org/10.1038/srep34122This study compared individuals with substance use disorder, healthy weight, and obesity with and without food addiction symptoms. Findings suggested similarities between participants with food addiction symptoms and those with substance use disorders. They also found differences between obese participants with and without food addiction symptoms, suggesting that addictive-like brain changes are associated with eating behaviors above and beyond weight status.
Kroemer NB, Sun X, Veldhuizen MG, Babbs AE, de Araujo IE, Small DM. Weighing the evidence: variance in brain responses to milkshake receipt is predictive of eating behavior. Neuroimage. 2016;128:273–83. https://doi.org/10.1016/j.neuroimage.2015.12.031.
Eisenstein SA, Bischoff AN, Gredysa DM, Antenor-Dorsey JA, Koller JM, Al-Lozi A, et al. Emotional eating phenotype is associated with central dopamine D2 receptor binding independent of body mass index. Sci Rep. 2015;5:11283. https://doi.org/10.1038/srep11283.
Batterink L, Yokum S, Stice E. Body mass correlates inversely with inhibitory control in response to food among adolescent girls: an fMRI study. Neuroimage. 2010;52(4):1696–703. https://doi.org/10.1016/j.neuroimage.2010.05.059.
Hanlon CA, Dowdle LT, Naselaris T, Canterberry M, Cortese BM. Visual cortex activation to drug cues: a meta-analysis of functional neuroimaging papers in addiction and substance abuse literature. Drug Alcohol Depend. 2014;143:206–12. https://doi.org/10.1016/j.drugalcdep.2014.07.028.
Kahathuduwa CN, Boyd LA, Davis T, O'Boyle M, Binks M. Brain regions involved in ingestive behavior and related psychological constructs in people undergoing calorie restriction. Appetite. 2016;107:348–61. https://doi.org/10.1016/j.appet.2016.08.112.
Stice E, Yokum S, Bohon C, Marti N, Smolen A. Reward circuitry responsivity to food predicts future increases in body mass: moderating effects of DRD2 and DRD4. Neuroimage. 2010;50(4):1618–25. https://doi.org/10.1016/j.neuroimage.2010.01.081.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington: Author; 2013. https://doi.org/10.1176/appi.books.9780890425596.
World Health Organization. International statistical classification of diseases and related health problems. 11th ed: World Health Organization; 2019. https://icd.who.int/. Accessed 30 Jan 2020.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Nutrition and the Brain
Rights and permissions
About this article
Cite this article
Gordon, E.L., Lent, M.R. & Merlo, L.J. The Effect of Food Composition and Behavior on Neurobiological Response to Food: a Review of Recent Research. Curr Nutr Rep 9, 75–82 (2020). https://doi.org/10.1007/s13668-020-00305-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13668-020-00305-5