Abstract
Despite decades of research, obesity and diabetes remain major health problems in the USA and worldwide. Among the many complications associated with diabetes is an increased risk of cardiovascular diseases, including myocardial infarction and heart failure. Recently, microRNAs have emerged as important players in heart disease and energy regulation. However, little work has investigated the role of microRNAs in cardiac energy regulation. Both human and animal studies have reported a significant increase in circulating free fatty acids and triacylglycerol, increased cardiac reliance on fatty acid oxidation, and subsequent decrease in glucose oxidation which all contributes to insulin resistance and lipotoxicity seen in obesity and diabetes. Importantly, MED13 was initially identified as a negative regulator of lipid accumulation in Drosophilia. Various metabolic genes were downregulated in MED13 transgenic heart, including sterol regulatory element-binding protein. Moreover, miR-33 and miR-122 have recently revealed as key regulators of lipid metabolism. In this review, we will focus on the role of microRNAs in regulation of cardiac and total body energy metabolism. We will also discuss the pharmacological and non-pharmacological interventions that target microRNAs for the treatment of obesity and diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity and diabetes are major health concerns that have reached epidemic proportions in the USA and worldwide [55]. The presence of obesity and diabetes is usually accompanied by cardiovascular complications [20]; among the many complications is the high risk of ischemic heart diseases [10] and heart failure (HF) [11]. Myocardial infarction accounts for approximately half of all deaths in patients with diabetes [34]. MicroRNAs have recently been identified as a potentially important pathway involved in the control of energy metabolism [25]. Grueter et al. proposed that miR-208a and its upstream regulator mediator complex subunit 13 (MED13) can modulate heart and total body energy metabolism. Furthermore, it has been shown that other MicroRNAs such as miR-103, miR-107, and miR-375 regulate insulin secretion from the pancreas and insulin sensitivity in peripheral tissues [14, 58]. Interestingly, pharmacological inhibition of miR-208a or overexpression of MED13 improves cardiac and total body insulin sensitivity and glucose metabolism in obese and diabetic mouse models [9, 25]. Although classical pharmacological and non-pharmacological treatment strategies can improve cardiac function and enhance survival chances in patients with heart disease, these attempts are ultimately inadequate to prevent disease progression [12]. Given the large number of patients with diabetes, it is important to find novel therapeutic strategies to treat cardiovascular diseases associated with obesity and diabetes.
Metabolic alterations and cardiac pathology in obesity
Heart has a high energy demand which depends mainly on oxidation of fatty acids to produce adenosine triphosphate (ATP) required for maintenance of its function [44]. The remainder of ATP production is derived from glycolysis, and the oxidation of glucose, lactate, and ketone bodies [12]. The presence of obesity and diabetes can markedly alter heart metabolic profile, making the heart to be more reliant on fatty acid oxidation as a source of energy (Fig. 1). The expansion of fatty acid oxidation is occurring mostly at the expense of glucose oxidation [11]. This reciprocal relationship between glucose and fatty acid oxidation was pointed out for the first time by Philip Randle lab in the 1960s [21]. In humans, positron emission tomography and 11C-palmitate imaging confirm the increase in cardiac fatty acid oxidation in obese [51] and diabetic patients [28]. High-fat diet-induced obese (DIO) mice developed left-sided heart hypertrophy and failure after 13 weeks of high fat feeding [50]. Important contributor to this cardiac malfunction is cardiac efficiency, which is the ratio of work performed by the heart to total cardiac oxygen consumption [44]. Fatty acid oxidation can influence cardiac efficiency [33]. In murine models of obesity and insulin resistance, cardiac efficiency was decreased as result of increased fatty acid oxidation [44, 46]. An important enzyme controlling the oxidation of fatty acid at the mitochondrial level is carnitine palmitoyltransferase-1 (CPT-1), the rate-limiting enzyme for the uptake of fatty acids. Malonyl-CoA, a potent allosteric inhibitor of CPT-1 [16], is synthesized by the enzyme acetyl-CoA carboxylase (ACC). Two isoforms of ACC have been identified, ACC1 and ACC2, with the later predominating in the heart [2]. ACC2-deleted hearts have a marked increase in muscle fatty acid oxidation rate [1]. Interestingly, sterol regulatory element-binding protein-1c (SREBP-1c) was suggested as a master activator of ACC1 and ACC2 transcription [18]. Moreover, SREBP-1c downregulation was accompanied by a decrease in levels of both ACC1 and ACC2 in diet-induced obesity mice treated with coffee polyphenols which contain caffeoyl quinic acids and feruloyl quinic acids [48]. SREBP-1c regulation of ACC1 in the liver is a basic step in the regulation of lipogenisis. In diabetes, expression of malonyl-CoA decarboxylase (MCD) is increased resulting in increased mitochondrial fatty acid uptake and oxidation [44]. Interestingly, MCD−/− mice are protected from diet-induced obesity [7]. A similar beneficial effect of MCD inhibition on glucose oxidation and insulin sensitivity was also recently reported.
Main alterations in energy metabolism-related tissues occurring in obesity. Fatty acids and glucose are the major fountains of energy production in the body. In obesity, dramatic changes in energy metabolism take place, such that fatty acids become the essential source of acetyl CoA for Krebs cycle. This switch leads to accumulation of fat in heart, muscles, liver, and adipose tissue. Fat accumulation along with increased inflammation ultimately results in whole body insulin resistance
Impaired balance between fatty acid uptake and utilization leads to accumulation of lipid metabolites such as ceramide, diacylglycerol (DAG), and triacylglycerol (TAG), which can have a deleterious effect on insulin signaling and cardiac function [44]. The increased levels of triacylglycerol are seen in hearts from obese human and rodents [8, 32], and several genetically modified obese and diabetic murine models [6]. However, the exact role of a TAG-induced lipotoxic cardiomyopathy is not fully understood. Accumulation of lipid intermediates such as diacylglycerol and ceramide in obese and diabetic heart can activate kinases that have detrimental impact on insulin signaling and cardiac function [19, 61], at the molecular level, lipotoxicity is due at least in part to the upregulation SREBP-1c [27], a transcription factor that upregulate genes involved in conversion of glucose to fatty acid and TAG in high fed state [22, 35]. SREBPs are synthesized as inactive precursors localized in membranes of endoplasmic reticulum (ER). Upon activation, SREBPs are cleaved and translocated into the nucleus [35]. Importantly, SREBP-1c was strongly correlated with intramyocyte lipid accumulation in patients with metabolic syndrome [38, 45]. Expression of the mitochondrial glycerol-3-phosphate acyltransferase (GPAT), which initiates the first commented step in phospholipid and TAG synthesis, is increased in response to SREBP-1c hepatic overexpression [41]. Previous studies suggested that GPAT1 knockout mice are protected from a high-fat diet-induced myocardial TAG accumulation. The final step in TAG biosynthesis is catalyzed by DAG acyltransferase (DGAT), which has been also suggested to be induced by SREBP-1c in liver [30] and skeletal muscles [43]. In the heart, increased DGAT1 mRNA expression was accompanied by increased myocardial TAG accumulation [68]. Interestingly, cyclin-dependent kinase 8 (CDK8) was identified as a novel regulator of SREBP-1c [13]. CDK8 is a nuclear serine-threonine kinase that is composed of four subunits; MED12 and MED13 compromise the major portion of CDK8 subcomplex [59]. Phosphorylation of SREBP-1c on threonine residue by CDK8 enhanced SREBP-1c degradation [13, 59]. CDK8 appears to be a highly conserved key inhibitor of de novo lipogenesis from Drosophila to mammals.
MicroRNAs as an emerging therapeutic target for obesity
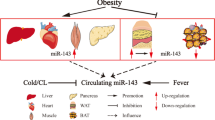
MicroRNAs (miRNAs) are a group of short, non-coding RNAs that can impress gene expression by repressing translation or promoting degradation of target mRNAs [59]. MiRNAs are one of the most abundant gene regulators in humans and have now been linked with a broad range of physiological and pathological processes, including obesity and diabetes (Fig. 2). Recent studies have revealed a key role for miRNAs in diabetes and insulin sensitivity. For example, miR-103 and miR-107 downregulate insulin sensitivity in peripheral tissues [58], inhibition of miR-103/107 leads to improved glucose homeostasis and insulin sensitivity in obese mice. miR-375 inhibits pancreatic insulin secretion in low-protein fed mice [14], which suggests that antagonizing miR-375 may enhance insulin secretion and improve glucose metabolism in diabetes. MED13 is one of the subunit components of mediator complex, which regulate thyroid hormone-dependent transcription [25]. Recently, cardiac-specific overexpression of MED13 or pharmacological inhibition of its upstream target miR-208a improves systemic insulin sensitivity and glucose tolerance in obese and diabetic mice [9, 25]. Interestingly, a follow-up study by the same group suggested MED13 as a suppressor of obesity; MED13 enhances fatty acid oxidation, lipid uptake, and mitochondrial number in WAT and liver [56]. Furthermore, suppression of miR-208a by the inhibitor of nutrient sensor kinase mTORC1 (rapamycin) attenuated weight gain and decreased body fat content through overexpression of cardiac MED13 mRNA in Zucker obese rats [62]. Collectively, these findings consolidate the theory of metabolic coordination between the heart and other organs, and it also pave the way for the development of novel treatment for metabolic disorders, such as obesity and diabetes. Chen et al. reported important role of mediator complex subunit 1 (MED1), another subunit of mediator complex, in the regulation of skeletal muscle glucose metabolism and insulin sensitivity [67]. Muscle-specific MED1 knockout mice display resistance to high-fat diet-induced obesity, improvement in whole body insulin sensitivity, and glucose tolerance. Surprisingly, the expression levels of UCP-1 were upregulated in MED1 knockout brown adipose tissues which associated with increased energy expenditure and mitochondrial content [67]. Interestingly, insulin can affect level of miRNAs expression in vascular smooth muscle cell; in particular, miR-208 was increased by insulin [31]. As obesity and diabetes are associated with myocardial insulin resistance, treatment of these underlying diseases may improve cardiac insulin sensitivity and function [70]. Both miR-208a and miR-451 are known regulators of cardiomyocyte size and both have been shown to dysregulate glucose metabolism and impair insulin sensitivity in diabetic and obese mice models [25, 40]. In support of this notion, a recent study by Kuwabara et al. [40] showed that deletion of miR-451 in mice ameliorates obesity-induced cardiac hypertrophy via activation of AMP-activated protein kinase (AMPK).
Role of miR-33 in lipid metabolism
miR-33 is the most abundant miRNA in lipoprotein particles, and it is widely suggested as a key regulator of lipid metabolism [49, 65]. The family of miR-33 sub grouped to miR-33a and miR-33b. Both miR-33a and miR-33b are located in intron 16 of human SREBP-2 and SREBP-1, respectively [23]. Goedeke et al. showed that miR-33 targets key enzymes of fatty acid uptake and metabolism including CPT-1, AMPK, and β-hydroxyacyl-CoA dehydrogenase (β-HAD). Furthermore, transfection of hepatic cells (Huh7) incubated in oleic acid with miR-33 significantly inhibits cellular fatty acid oxidation [53]. Consistent with this, previous studies from the same lab and others have shed the light on miR-33 as a novel treatment of obesity and diabetes [36, 54] (Fig. 3). In a more recent study, Karunakaran et al. [37] demonstrated that anti-miR33 therapy downregulates genes that enhance mitochondrial oxidative capacity and ATP production. This is maybe important to promote macrophage cholesterol efflux and therefore reduce atherosclerosis. However, inhibition of mitochondrial oxidative capacity in other tissues such as heart and skeletal muscles is detrimental which raises concerns about the efficiency of using anti-miR33 in the treatment of obesity and diabetes. In support, a subsequent study by the same group [57] proposed that therapeutic inhibition of miR-33 does not mend metabolic dysfunction in high-fat diet-induced obesity mice model. Anti-miR33 treatment for 20 weeks increased AMPK gene expression but did not affect mice body weight. These results suggest that targeting miR-33 may alter fatty acid metabolism without affecting metabolic dysregulation.
Proposed consequences of miR-33 inhibition on fatty acid oxidation and lipid accumulation. MiR-33 inhibition will lead to downregulation of sterol regulatory element-binding protein-1c (SREBP-1c), thereby decreasing triacylglycerol (TAG) biosynthesis. On the other hand, treatment with anti-miR-33 results in increased AMP-activated protein kinase (AMPK) activity. AMPK phosphorylates and represses acetyl-CoA carboxylase (AAC) activity and malonyl-CoA production, thereby relief the inhibition of fatty acid uptakes and ultimately leading to increased fatty acid oxidation
Role of miR-122 in lipid metabolism
miR-122 is a highly ample liver-specific miRNA that regulates lipid metabolism [29]. Its pharmacological inhibition or genetic deletion markedly reduced systemic and hepatic cholesterol and triglyceride (TG) accumulation. Furthermore, in vivo antisense targeting of miR-122 resulted in a marked overexpression of hepatic AMPK and activation of fatty acid β-oxidation [26]. In a recent clinical study, circulating miR-122 levels were more than threefold higher in obese young adults compared to lean subjects [52]. Levels of miR-122 in the serum were correlated with body weight, TG, and whole body insulin insensitivity [52]. However, another case-control study showed that liver miR-122 expression was tenfold lower in non-alcoholic steatohepatitis patients compared to control, and that overexpression of miR-112 in vitro improves hepatic cell function [5]. Furthermore, mRNA expression of β-oxidation genes LCAD and CPT1 were downregulated in obese dam breeds concomitant with a marked decrease in miR-122 expression [3]. In rats, 3-week treatment with proanthocyanidin significantly repressed miR-122 expression and improved postprandial TG serum levels in a dose-dependent manner [17]. Collectively, these results suggest antimiR-122 as an attractive therapeutic target for metabolic diseases, however, further in vivo investigations to dissect the pathways of miR-122 regulation has to be fully studied.
Role of miR-208a in cardiac diseases
Ischemic heart disease is a major chronic complication of obesity and diabetes. In particular, myocardial infarction accounts for approximately half of all deaths in patients with diabetes. Moreover, ischemia/reperfusion (I/R) injury increased the mortality rate twice in diabetic patients compared to nondiabetics [24, 42]. I/R injury is the cellular damage after blood supply returns to a previously viable ischemic tissue. Although multiple underlying mechanisms contribute to I/R injury, there is a strong interconnection between contractile malfunction and energy substrates used by the heart [60]. Following ischemia and during reperfusion, a greater reliance on fatty acids as a substrate for energy exacerbates cardiac function and ischemic injury [15]. In addition, glucose oxidation is significantly decreased secondary to the increase in fatty acid oxidation [15, 44]. During ischemia, glycolytic rate is increased and glycolysis is uncoupled from the mitochondrial oxidation of glucose, thereby increasing the production of protons, lactate and decreasing cardiac efficiency [15]. Preclinical and clinical studies suggested that miRNAs are correlated with ischemic heart diseases, including myocardial infarction. In particular, miR-208a was significantly increased in hearts from humans with stable coronary disease [64, 69]. In humans, plasma levels of miR-208 were increased 5-day postmyocardial infarction and remained elevated up to 3 months [47]. Furthermore, results from miRNA analysis revealed that miR-208 was upregulated in rat hearts 24 h after I/R injury. Moreover, cardiac miR-208a level was increased 2 days after reperfusion in C57BL mice. Interestingly, therapeutic targeting of miR-15, miR-24, and miR-320 improves cardiac function and reduces infarct size after ischemic injury. In rat hearts, miR-208 was specifically downregulated in postconditiong which suggests a potential therapeutic value of antimiR-208 against reperfusion injury [4].
Obesity, metabolism, and cardiac disease: clinical implications
miRNAs are key transcriptional regulators of cellular signaling and metabolism, which make them promising targets for potential treatment of obesity and diabetes. Pharmacological inhibition of pathological mRNAs or activation of beneficial mRNAs by complementary oligonucleotides represents an interesting mean in clinical practice. Indeed, mice treated with antimiR-33 showed increased plasma HDL levels as a result of upregulation of ATP-binding cassette transporter ABCA1 expression [36, 54]. Moreover, inhibition of miR-33 by 2-F, 2-fluoro, o-methoxyethyl mixmer decreases VLDL and increases HDL in non-human primates [36]. These results show the promise of using antimiR-33 as a novel treatment of atherosclerosis. To increase stability, antagomir complementary to the mature targeted miRNA conjugated to cholesterol is used to enhance cellular uptake and stability [63]. Interestingly, inhibition of miR-122, which is another key player in liver lipid metabolism, by antagomir results in a significant decrease of triglyceride and fat accumulation in mice liver [26]. The use of antimiR-122 in humans as an attempt to treat hepatitis C virus infection proved to be safe in a recent clinical trial [39]. However, both the atherogenic LDL and the beneficial HDL were decreased in mice treated with antimiR-122, which raises concern about the safety of using antimiR-122 in the management of obesity-induced cardiovascular diseases in humans. Currently, there is a lack of knowledge about the cellular uptake and mechanisms of action of antimiRs. Consequently, antimiRs toxicity that raises from the off-target effect or undesirable gene changes underscores the challenges associated with antimiRs development. In this regard, previous studies suggested that inhibition of miR-208 enhanced cardiac function and reduced fibrosis in obesity-induced cardiac hypertrophy mice and rat models [63, 66]. However, unexpectedly, treatment with anti-miR208a protects mice from high-fat diet-induced obesity [9]. This is a perfect example that shows diversity of actions of miRNAs, which can range from regulation of myosin switching to modulation of energy metabolism.
Summary and conclusions
Obesity and diabetes are key risk factors for the development of ischemic heart disease and heart failure. There is a growing body of evidence demonstrating that metabolic abnormalities that accompany these diseases contribute to deleterious progression of cardiac function. Increased reliance on fatty acid oxidation along with decreased rate of glucose oxidation is the hallmark of diabetes and obesity. Increased fatty acid uptake and oxidation result in accumulation of lipid intermediates such as TAG and DAG, which can have an abstruse influence on insulin sensitivity and cardiac function. There is ongoing effort to validate metabolic modulators as a novel therapeutic approach for treatment of diabetes and obesity as well as heart diseases. Interestingly, MED13 and its upstream regulator miR-208a were suggested as a novel systemic regulator of energy metabolism which can control cardiac remodeling and obesity. Moreover, targeting other microRNAs such as miR-122 and miR-33 represents a promising treatment for atherosclerosis and steatohepatitis (Table 1). However, dissecting the precise genetic targets of microRNAs and the downstream effects of microRNAs modulation on the activity of key enzymes involved in fatty acid and glucose oxidation will clarify the potential for the use of microRNAs modulators as a new exciting therapeutic tool, as well as the feasibility of translating into clinical practice.
References
Abu-Elheiga L, Matzuk MM, Abo-Hashema KA, Wakil SJ (2001) Continuous fatty acid oxidation and reduced fat storage in mice lacking acetyl-CoA carboxylase 2. Science 291:2613–2616. doi:10.1126/science.1056843
Abu-Elheiga L, Wu H, Gu Z, Bressler R, Wakil SJ (2012) Acetyl-CoA carboxylase 2−/− mutant mice are protected against fatty liver under high-fat, high-carbohydrate dietary and de novo lipogenic conditions. J Biol Chem 287:12578–12588. doi:10.1074/jbc.M111.309559
Baselga-Escudero L, Blade C, Ribas-Latre A, Casanova E, Salvado MJ, Arola L, Arola-Arnal A (2014) Chronic supplementation of proanthocyanidins reduces postprandial lipemia and liver miR-33a and miR-122 levels in a dose-dependent manner in healthy rats. J Nutr Biochem 25:151–156. doi:10.1016/j.jnutbio.2013.09.014
Baskin KK, Grueter CE, Kusminski CM, Holland WL, Bookout AL, Satapati S, Kong YM, Burgess SC, Malloy CR, Scherer PE, Newgard CB, Bassel-Duby R, Olson EN (2014) MED13-dependent signaling from the heart confers leanness by enhancing metabolism in adipose tissue and liver. EMBO Mol Med 6:1610–1621. doi:10.15252/emmm.201404218
Benatti RO, Melo AM, Borges FO, Ignacio-Souza LM, Simino LA, Milanski M, Velloso LA, Torsoni MA, Torsoni AS (2014) Maternal high-fat diet consumption modulates hepatic lipid metabolism and microRNA-122 (miR-122) and microRNA-370 (miR-370) expression in offspring. Br J Nutr 111:2112–2122. doi:10.1017/S0007114514000579
Bugger H, Riehle C, Jaishy B, Wende AR, Tuinei J, Chen D, Soto J, Pires KM, Boudina S, Theobald HA, Luptak I, Wayment B, Wang X, Litwin SE, Weimer BC, Abel ED (2012) Genetic loss of insulin receptors worsens cardiac efficiency in diabetes. J Mol Cell Cardiol 52:1019–1026. doi:10.1016/j.yjmcc.2012.02.001
Campbell FM, Kozak R, Wagner A, Altarejos JY, Dyck JR, Belke DD, Severson DL, Kelly DP, Lopaschuk GD (2002) A role for peroxisome proliferator-activated receptor alpha (PPARalpha) in the control of cardiac malonyl-CoA levels: reduced fatty acid oxidation rates and increased glucose oxidation rates in the hearts of mice lacking PPARalpha are associated with higher concentrations of malonyl-CoA and reduced expression of malonyl-CoA decarboxylase. J Biol Chem 277:4098–4103. doi:10.1074/jbc.M106054200
Carley AN, Atkinson LL, Bonen A, Harper ME, Kunnathu S, Lopaschuk GD, Severson DL (2007) Mechanisms responsible for enhanced fatty acid utilization by perfused hearts from type 2 diabetic db/db mice. Arch Physiol Biochem 113:65–75. doi:10.1080/13813450701422617
Chen W, Zhang X, Birsoy K, Roeder RG (2010) A muscle-specific knockout implicates nuclear receptor coactivator MED1 in the regulation of glucose and energy metabolism. Proc Natl Acad Sci U S A 107:10196–10201. doi:10.1073/pnas.1005626107
Chvokov AV (2012) The myocardial revascularization in patients with diabetes mellitus and the ischemic heart disease. Khirurgiia (Mosk) (4): 55–58
Czuriga I, Borbely A, Czuriga D, Papp Z, Edes I (2012) Heart failure with preserved ejection fraction (diastolic heart failure). Orv Hetil 153:2030–2040. doi:10.1556/OH.2012.29506
Deedwania PC, Carbajal E (2012) Evidence-based therapy for heart failure. Med Clin North Am 96:915–931. doi:10.1016/j.mcna.2012.07.010
Donner AJ, Ebmeier CC, Taatjes DJ, Espinosa JM (2010) CDK8 is a positive regulator of transcriptional elongation within the serum response network. Nat Struct Mol Biol 17:194–201. doi:10.1038/nsmb.1752
Dumortier O, Hinault C, Gautier N, Patouraux S, Casamento V, Van Obberghen E (2014) Maternal protein restriction leads to pancreatic failure in offspring: role of misexpressed microRNA-375. Diabetes 63:3416–3427. doi:10.2337/db13-1431
Dyck JR, Cheng JF, Stanley WC, Barr R, Chandler MP, Brown S, Wallace D, Arrhenius T, Harmon C, Yang G, Nadzan AM, Lopaschuk GD (2004) Malonyl coenzyme a decarboxylase inhibition protects the ischemic heart by inhibiting fatty acid oxidation and stimulating glucose oxidation. Circ Res 94:e78–e84. doi:10.1161/01.RES.0000129255.19569.8f
Dyck JR, Hopkins TA, Bonnet S, Michelakis ED, Young ME, Watanabe M, Kawase Y, Jishage K, Lopaschuk GD (2006) Absence of malonyl coenzyme A decarboxylase in mice increases cardiac glucose oxidation and protects the heart from ischemic injury. Circulation 114:1721–1728. doi:10.1161/CIRCULATIONAHA.106.642009
Esau C, Davis S, Murray SF, Yu XX, Pandey SK, Pear M, Watts L, Booten SL, Graham M, McKay R, Subramaniam A, Propp S, Lollo BA, Freier S, Bennett CF, Bhanot S, Monia BP (2006) miR-122 regulation of lipid metabolism revealed by in vivo antisense targeting. Cell Metab 3:87–98
Field FJ, Born E, Murthy S, Mathur SN (2002) Polyunsaturated fatty acids decrease the expression of sterol regulatory element-binding protein-1 in CaCo-2 cells: effect on fatty acid synthesis and triacylglycerol transport. Biochem J 368:855–864. doi:10.1042/BJ20020731
Fillmore N, Lopaschuk GD (2012) Targeting mitochondrial oxidative metabolism as an approach to treat heart failure. Biochim Biophys Acta. doi:10.1016/j.bbamcr.2012.08.014
Fonseca VA (2009) Defining and characterizing the progression of type 2 diabetes. Diabetes Care 32(Suppl 2):S151–S156. doi:10.2337/dc09-S301
GARLAND PB, RANDLE PJ, NEWSHOLME EA (1963) Citrate as an intermediary in the inhibition of phosphofructokinase in rat heart muscle by fatty acids, ketone bodies, pyruvate, diabetes, and starvation. Nature 200:169–170
Ge Y, Zhang Y, Li R, Chen W, Li Y, Chen G (2011) Berberine regulated Gck, G6pc, Pck1 and Srebp-1c expression and activated AMP-activated protein kinase in primary rat hepatocytes. Int J Biol Sci 7:673–684
Goedeke L, Vales-Lara FM, Fenstermaker M, Cirera-Salinas D, Chamorro-Jorganes A, Ramirez CM, Mattison JA, de Cabo R, Suarez Y, Fernandez-Hernando C (2013) A regulatory role for microRNA 33* in controlling lipid metabolism gene expression. Mol Cell Biol 33:2339–2352. doi:10.1128/MCB.01714-12
Grinev MV, Bromberg BB (2012) Ischemia-reperfusion—a universal mechanism of pathogenesis of critical states in emergency surgery. Vestn Khir Im I I Grek 171:94–100
Grueter CE, van Rooij E, Johnson BA, DeLeon SM, Sutherland LB, Qi X, Gautron L, Elmquist JK, Bassel-Duby R, Olson EN (2012) A cardiac microRNA governs systemic energy homeostasis by regulation of MED13. Cell 149:671–683. doi:10.1016/j.cell.2012.03.029
Gul R, Mahmood A, Luck C, Lum-Naihe K, Alfadda AA, Speth RC, Pulakat L (2015) Regulation of cardiac miR-208a, an inducer of obesity, by rapamycin and nebivolol. Obesity (Silver Spring) 23:2251–2259. doi:10.1002/oby.21227
Haas JT, Miao J, Chanda D, Wang Y, Zhao E, Haas ME, Hirschey M, Vaitheesvaran B, Farese RV Jr, Kurland IJ, Graham M, Crooke R, Foufelle F, Biddinger SB (2012) Hepatic insulin signaling is required for obesity-dependent expression of SREBP-1c mRNA but not for feeding-dependent expression. Cell Metab 15:873–884. doi:10.1016/j.cmet.2012.05.002
Herrero P, Peterson LR, McGill JB, Matthew S, Lesniak D, Dence C, Gropler RJ (2006) Increased myocardial fatty acid metabolism in patients with type 1 diabetes mellitus. J Am Coll Cardiol 47:598–604. doi:10.1016/j.jacc.2005.09.030
Hsu SH, Wang B, Kota J, Yu J, Costinean S, Kutay H, Yu L, Bai S, La Perle K, Chivukula RR, Mao H, Wei M, Clark KR, Mendell JR, Caligiuri MA, Jacob ST, Mendell JT, Ghoshal K (2012) Essential metabolic, anti-inflammatory, and anti-tumorigenic functions of miR-122 in liver. J Clin Invest 122:2871–2883. doi:10.1172/JCI63539
Ikeda S, Miyazaki H, Nakatani T, Kai Y, Kamei Y, Miura S, Tsuboyama-Kasaoka N, Ezaki O (2002) Up-regulation of SREBP-1c and lipogenic genes in skeletal muscles after exercise training. Biochem Biophys Res Commun 296:395–400
Iozzo P, Chareonthaitawee P, Dutka D, Betteridge DJ, Ferrannini E, Camici PG (2002) Independent association of type 2 diabetes and coronary artery disease with myocardial insulin resistance. Diabetes 51:3020–3024
Itani SI, Ruderman NB, Schmieder F, Boden G (2002) Lipid-induced insulin resistance in human muscle is associated with changes in diacylglycerol, protein kinase C, and IkappaB-alpha. Diabetes 51:2005–2011
Jaswal JS, Keung W, Wang W, Ussher JR, Lopaschuk GD (2011) Targeting fatty acid and carbohydrate oxidation—a novel therapeutic intervention in the ischemic and failing heart. Biochim Biophys Acta. doi:10.1016/j.bbamcr.2011.15.1
Jelesoff NE, Feinglos M, Granger CB, Califf RM (1997) Outcomes of diabetic patients following acute myocardial infarction: a review of the major thrombolytic trials. J Cardiovasc Risk 4:100–111
Jeon TI, Osborne TF (2012) SREBPs: metabolic integrators in physiology and metabolism. Trends Endocrinol Metab 23:65–72. doi:10.1016/j.tem.2011.10.004
Karunakaran D, Thrush AB, Nguyen MA, Richards L, Geoffrion M, Singaravelu R, Ramphos E, Shangari P, Ouimet M, Pezacki JP, Moore KJ, Perisic L, Maegdefessel L, Hedin U, Harper ME, Rayner KJ (2015a) Macrophage mitochondrial energy status regulates cholesterol efflux and is enhanced by anti-miR33 in atherosclerosis. Circ Res 117:266–278. doi:10.1161/CIRCRESAHA.117.305624
Karunakaran D, Richards L, Geoffrion M, Barrette D, Gotfrit RJ, Harper ME, Rayner KJ (2015b) Therapeutic inhibition of miR-33 promotes fatty acid oxidation but does not ameliorate metabolic dysfunction in diet-induced obesity. Arterioscler Thromb Vasc Biol 35:2536–2543. doi:10.1161/ATVBAHA.115.306404
Knebel B, Haas J, Hartwig S, Jacob S, Kollmer C, Nitzgen U, Muller-Wieland D, Kotzka J (2012) Liver-specific expression of transcriptionally active SREBP-1c is associated with fatty liver and increased visceral fat mass. PLoS One 7:e31812. doi:10.1371/journal.pone.0031812
Krutzfeldt J, Rajewsky N, Braich R, Rajeev KG, Tuschl T, Manoharan M, Stoffel M (2005) Silencing of microRNAs in vivo with ‘antagomirsʼ. Nature 438:685–689
Kuwabara Y, Horie T, Baba O, Watanabe S, Nishiga M, Usami S, Izuhara M, Nakao T, Nishino T, Otsu K, Kita T, Kimura T, Ono K (2015) MicroRNA-451 exacerbates lipotoxicity in cardiac myocytes and high-fat diet-induced cardiac hypertrophy in mice through suppression of the LKB1/AMPK pathway. Circ Res 116:279–288. doi:10.1161/CIRCRESAHA.116.304707
Lewin TM, de Jong H, Schwerbrock NJ, Hammond LE, Watkins SM, Combs TP, Coleman RA (2008) Mice deficient in mitochondrial glycerol-3-phosphate acyltransferase-1 have diminished myocardial triacylglycerol accumulation during lipogenic diet and altered phospholipid fatty acid composition. Biochim Biophys Acta 1781:352–358. doi:10.1016/j.bbalip.2008.05.001
Liu X, Wei J, Peng DH, Layne MD, Yet SF (2005) Absence of heme oxygenase-1 exacerbates myocardial ischemia/reperfusion injury in diabetic mice. Diabetes 54:778–784
Liu L, Shi X, Bharadwaj KG, Ikeda S, Yamashita H, Yagyu H, Schaffer JE, Yu YH, Goldberg IJ (2009) DGAT1 expression increases heart triglyceride content but ameliorates lipotoxicity. J Biol Chem 284:36312–36323. doi:10.1074/jbc.M109.049817
Lopaschuk GD, Ussher JR, Folmes CD, Jaswal JS, Stanley WC (2010) Myocardial fatty acid metabolism in health and disease. Physiol Rev 90:207–258. doi:10.1152/physrev.00015.2009
Marfella R, Di Filippo C, Portoghese M, Barbieri M, Ferraraccio F, Siniscalchi M, Cacciapuoti F, Rossi F, D'Amico M, Paolisso G (2009) Myocardial lipid accumulation in patients with pressure-overloaded heart and metabolic syndrome. J Lipid Res 50:2314–2323. doi:10.1194/jlr.P900032-JLR200
Mazumder PK, O'Neill BT, Roberts MW, Buchanan J, Yun UJ, Cooksey RC, Boudina S, Abel ED (2004) Impaired cardiac efficiency and increased fatty acid oxidation in insulin-resistant ob/ob mouse hearts. Diabetes 53:2366–2374
Montgomery RL, Hullinger TG, Semus HM, Dickinson BA, Seto AG, Lynch JM, Stack C, Latimer PA, Olson EN, van Rooij E (2011) Therapeutic inhibition of miR-208a improves cardiac function and survival during heart failure. Circulation 124:1537–1547. doi:10.1161/CIRCULATIONAHA.111.030932
Murase T, Misawa K, Minegishi Y, Aoki M, Ominami H, Suzuki Y, Shibuya Y, Hase T (2011) Coffee polyphenols suppress diet-induced body fat accumulation by downregulating SREBP-1c and related molecules in C57BL/6J mice. Am J Physiol Endocrinol Metab 300:E122–E133. doi:10.1152/ajpendo.00441.2010
Najafi-Shoushtari SH, Kristo F, Li Y, Shioda T, Cohen DE, Gerszten RE, Naar AM (2010) MicroRNA-33 and the SREBP host genes cooperate to control cholesterol homeostasis. Science 328:1566–1569. doi:10.1126/science.1189123
Park SY, Cho YR, Kim HJ, Higashimori T, Danton C, Lee MK, Dey A, Rothermel B, Kim YB, Kalinowski A, Russell KS, Kim JK (2005) Unraveling the temporal pattern of diet-induced insulin resistance in individual organs and cardiac dysfunction in C57BL/6 mice. Diabetes 54:3530–3540
Peterson LR, Herrero P, Schechtman KB, Racette SB, Waggoner AD, Kisrieva-Ware Z, Dence C, Klein S, Marsala J, Meyer T, Gropler RJ (2004) Effect of obesity and insulin resistance on myocardial substrate metabolism and efficiency in young women. Circulation 109:2191–2196. doi:10.1161/01.CIR.0000127959.28627.F8
Pirola CJ, Fernandez Gianotti T, Castano GO, Mallardi P, San Martino J, Mora Gonzalez Lopez Ledesma M, Flichman D, Mirshahi F, Sanyal AJ, Sookoian S (2015) Circulating microRNA signature in non-alcoholic fatty liver disease: from serum non-coding RNAs to liver histology and disease pathogenesis. Gut 64:800–812. doi:10.1136/gutjnl-2014-306996
Rayner KJ, Esau CC, Hussain FN, McDaniel AL, Marshall SM, van Gils JM, Ray TD, Sheedy FJ, Goedeke L, Liu X, Khatsenko OG, Kaimal V, Lees CJ, Fernandez-Hernando C, Fisher EA, Temel RE, Moore KJ (2011a) Inhibition of miR-33a/b in non-human primates raises plasma HDL and lowers VLDL triglycerides. Nature 478:404–407. doi:10.1038/nature10486
Rayner KJ, Sheedy FJ, Esau CC, Hussain FN, Temel RE, Parathath S, van Gils JM, Rayner AJ, Chang AN, Suarez Y, Fernandez-Hernando C, Fisher EA, Moore KJ (2011b) Antagonism of miR-33 in mice promotes reverse cholesterol transport and regression of atherosclerosis. J Clin Invest 121:2921–2931. doi:10.1172/JCI57275
Smith KB, Smith MS (2016) Obesity statistics. Prim Care 43(1):121–35, ix. doi:10.1016/j.pop
Sun X, Feinberg MW (2014) MicroRNA-management of lipoprotein homeostasis. Circ Res 115:2–6. doi:10.1161/CIRCRESAHA.114.304228
Thakral S, Ghoshal K (2015) miR-122 is a unique molecule with great potential in diagnosis, prognosis of liver disease, and therapy both as miRNA mimic and antimir. Curr Gene Ther 15:142–150
Trajkovski M, Hausser J, Soutschek J, Bhat B, Akin A, Zavolan M, Heim MH, Stoffel M (2011) MicroRNAs 103 and 107 regulate insulin sensitivity. Nature 474:649–653. doi:10.1038/nature10112
Udali S, Guarini P, Moruzzi S, Choi SW, Friso S (2012) Cardiovascular epigenetics: from DNA methylation to microRNAs. Mol Asp Med. doi:10.1016/j.mam.2012.08.001
Ussher JR, Lopaschuk GD (2009) Targeting malonyl CoA inhibition of mitochondrial fatty acid uptake as an approach to treat cardiac ischemia/reperfusion. Basic Res Cardiol 104:203–210. doi:10.1007/s00395-009-0003-9
Ussher JR, Folmes CD, Keung W, Fillmore N, Jaswal JS, Cadete VJ, Beker DL, Lam VH, Zhang L, Lopaschuk GD (2012) Inhibition of serine palmitoyl transferase I reduces cardiac ceramide levels and increases glycolysis rates following diet-induced insulin resistance. PLoS One 7:e37703. doi:10.1371/journal.pone.0037703
van der Ree MH, van der Meer AJ, de Bruijne J, Maan R, van Vliet A, Welzel TM, Zeuzem S, Lawitz EJ, Rodriguez-Torres M, Kupcova V, Wiercinska-Drapalo A, Hodges MR, Janssen HL, Reesink HW (2014) Long-term safety and efficacy of microRNA-targeted therapy in chronic hepatitis C patients. Antivir Res 111:53–59. doi:10.1016/j.antiviral.2014.08.015
van Rooij E, Sutherland LB, Qi X, Richardson JA, Hill J, Olson EN (2007) Control of stress-dependent cardiac growth and gene expression by a microRNA. Science 316:575–579
Widera C, Gupta SK, Lorenzen JM, Bang C, Bauersachs J, Bethmann K, Kempf T, Wollert KC, Thum T (2011) Diagnostic and prognostic impact of six circulating microRNAs in acute coronary syndrome. J Mol Cell Cardiol 51:872–875. doi:10.1016/j.yjmcc.2011.07.011
Yang Z, Cappello T, Wang L (2015) Emerging role of microRNAs in lipid metabolism. Acta Pharm Sin B 5:145–150. doi:10.1016/j.apsb.2015.01.002
Zampetaki A, Mayr M (2012) MicroRNAs in vascular and metabolic disease. Circ Res 110:508–522. doi:10.1161/CIRCRESAHA.111.247445
Zhang Y, Wang Y, Wang X, Zhang Y, Eisner GM, Asico LD, Jose PA, Zeng C (2011) Insulin promotes vascular smooth muscle cell proliferation via microRNA-208-mediated downregulation of p21. J Hypertens 29:1560–1568. doi:10.1097/HJH.0b013e328348ef8e
Zhao X, Feng D, Wang Q, Abdulla A, Xie XJ, Zhou J, Sun Y, Yang ES, Liu LP, Vaitheesvaran B, Bridges L, Kurland IJ, Strich R, Ni JQ, Wang C, Ericsson J, Pessin JE, Ji JY, Yang F (2012) Regulation of lipogenesis by cyclin-dependent kinase 8-mediated control of SREBP-1. J Clin Invest 122:2417–2427. doi:10.1172/JCI61462
Zile MR, Mehurg SM, Arroyo JE, Stroud RE, DeSantis SM, Spinale FG (2011) Relationship between the temporal profile of plasma microRNA and left ventricular remodeling in patients after myocardial infarction. Circ Cardiovasc Genet 4:614–619. doi:10.1161/CIRCGENETICS.111.959841
Zuanetti G, Latini R, Maggioni AP, Santoro L, Franzosi MG (1993) Influence of diabetes on mortality in acute myocardial infarction: data from the GISSI-2 study. J Am Coll Cardiol 22:1788–1794
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alrob, O.A., Khatib, S. & Naser, S.A. MicroRNAs 33, 122, and 208: a potential novel targets in the treatment of obesity, diabetes, and heart-related diseases. J Physiol Biochem 73, 307–314 (2017). https://doi.org/10.1007/s13105-016-0543-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13105-016-0543-z