Abstract
Left ventricular dyssynchrony (LVD) is an independent predictor of adverse cardiovascular events, death, and progression to heart failure. Myocardial perfusion imaging (MPI) with ECG-gated single-photon emission computed tomography (SPECT) can be used to diagnose LVD rapidly and automatically using phase analysis (PA). The objective of this study was to evaluate the prevalence and predictors of LVD in patients undergoing MPI. Clinical, electrocardiographic, and scintigraphic data from 1000 patients who underwent MPI with ECG-gated SPECT over a period of 1 year were analyzed retrospectively. TheEmoryCardiac Toolboxsoftware was used for PA, and LVD was diagnosed based on the following criteria: standard deviation of LV phase distribution ≥43° and/or phase histogram ≥140° in the resting and/or stress phase of the examination. Several variables were evaluated using univariate and multivariate analyses. The prevalence of LVD in the study population was 6.5 %, and the average age was 63.6 ± 12 years. The variables significantly associated with LVD were male gender, obesity, hypertension, diabetes, dyslipidemia, coronary artery disease (CAD), QRS interval ≥120 ms, LV dysfunction, and myocardial perfusion defects (especially fixed defects) on MPI. Although the PA parameters were greater at rest, both phases could be used for diagnosis. Multivariate analysis revealed that the variables significantly associated with LVD were male sex, obesity, history of CAD, and QRS interval ≥120 ms. The overall prevalence of LVD was 6.5 % in patients undergoing MPI in this study, and it reached 42 % in the presence of certain risk factors.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Synchronous left ventricular (LV) contraction, which is essential for heart function, serves as a major determinant of heart performance. The loss of contraction synchrony between the LV myocardial segments is known as LV dyssynchrony (LVD). The heterogeneous mechanical action caused by the uncoordinated contraction of the heart muscles is associated with changes in myocardial perfusion and concentric LV remodeling, leading to progressive ventricular dilation and deterioration of cardiac function [1–3].
LVD can occur without signs or symptoms of heart disease and with preserved ventricular function. In these patients, LVD is a marker of progression to heart failure (HF)and can help identify individuals at a higher risk of developing HF in the future [1, 4].
The detection of LVD in the pre-symptomatic stage can anticipate HF in genetically predisposed hearts [5]. Symptoms typically occur late during HF progression, and the subclinical stage is the optimal period for intervention [6].
MPI with ECG-gated single-photon emission computed tomography (SPECT) is widely performed to study myocardial viability and ischemia, assess chest pain, stratify cardiovascular risk, and locate infarcted areas [7].
Since the introduction of phase analysis (PA) in 2005, MPI has also been used to evaluate the parameters of cardiac synchrony, allowing the rapid and automatic diagnosis of ventricular dyssynchrony with high reproducibility, regardless of the examiner, and without additional discomfort to the patient [8, 9]. However, this feature is underused because the prevalence of LVD and the profile of patients to be evaluated are unknown. The most frequently used PA parameters for access to LVD are the phase histogram bandwidth (PHB) and phase standard deviation (PSD). PHB values ≥140° and/or PSD values ≥43° are indicators of significant LVD [10–15].
Materials and methods
This observational, retrospective study involved the analysis of an electronic database of 1,000 patients submitted to MPI with ECG-gated SPECT at rest and under stress. This study was conducted at the Center for Diagnostic Imaging (CDI) in Rio de Janeiro, Leblon, Brazil, over a 1-year period (from August 2013 to August 2014).
The inclusion criteria were as follows: over 18 years old, performance of MPI at rest and under stress on the same day, performance of the 12-lead electrocardiogram on the day of the MPI examination, and regular R–R intervals, allowing appropriate image acquisition via ECG-gated SPECT. The exclusion criteria were as follows: electrocardiograms with irregular rhythms (the presence of atrial or ventricular arrhythmias), patients with pacemakers, patients with implantable cardioverter-defibrillators, patients with cardiac resynchronization systems, and patients with a body mass index (BMI) ≥35 kg/m2.
Examination protocol
The patients were referred for MPI with ECG-gated SPECT at rest and under stressby their doctors for various reasons.
The patients underwent MPI at rest and under stress on the same day (1-day protocol), with the resting phase preceding the stress phase. Stress was induced either pharmacologically (dipyridamole or dobutamine) or using a treadmill exercise test. The standard radiotracer used was 99mTc sestamibi, which was injected via a peripheral vein. The doses were 5–6 and 6–18 mCi at rest and during stress, respectively.
Image acquisition
ECG-gated SPECT images were acquired at rest and after stress 10 min after tracer injection using a Discovery 530 gamma camera (GE Healthcare®) equipped with a cadmium-zinc-telluride (CZT) solid-state detector and pinhole collimator with an image acquisition speed of 8 frames per cardiac cycle.
The rest and stress scan time was 6 and 3 min, respectively. After acquisition, the images were reconstructed using the short-axis orientation, and the Emory Cardiac Toolbox software (Emory University/Syntermed, Atlanta, Georgia, USA) was used for PA analysis.
Data collection
The clinical data collected included age, sex, weight (kg), height (m), BMI (kg/m2), history of hypertension, diabetes, dyslipidemia, and smoking, and personal or family history of coronary artery disease (CAD). Printed 12-lead electrocardiograms obtained at rest before the administration of the radiotracer were available for all the patients. The duration of the QRS interval on the ECG was measured in milliseconds using computer software; an interval <120 ms was considered normal. The MPI data collected included LV ejection fraction at rest and under stress, LV end-systolic volume and end-diastolic volume at rest and under stress, LV ejection fraction at rest and under stress, and pattern of myocardial perfusion in the report.
Criteria used for dyssynchrony diagnosis
The criteria used to diagnose LVD were PHB ≥140° and/or PSD ≥43°. A patient was considered as having LVD if any of these criteria was met either at rest or under stress.
Statistical analysis
Categorical variables are presented as absolute frequency (n), relative frequency (n), and percentage (%). Numerical variables are presented as mean, standard deviation (SD), median, and minimum and maximum values. The Chi square test was used to analyze the association of categorical variables with dyssynchrony. Similarly, we used the Student t test for numerical variables. The bivariate analysis was performed to evaluate the association of each variable with dyssynchrony. In order to compare different variables, we used the model multiple binary logistic regression. A p value <0.05 was considered to indicate statistical significance. The confidence interval for calculating prevalence was set at 95 %. Intraclass correlation coefficients were calculated between dyssynchrony parameters obtained at rest and under stress. All analyses were performed using the SPSS 17.0 (n)software for Windows (SPSS, Chicago, Illinois, USA).
Results
Data from a total of 1,100 patients were analyzed. One hundred patients were excluded based on BMI exceeding 34.9 kg/m2 (48 individuals), irregular electrocardiographic rhythm (42 individuals), and presence of implantable cardiac devices (primarily bicameral pacemakers, 10 individuals).
The clinical characteristics of the study population and their associations with LVD are shown in Table 1.
Men accounted for 56.9 % of the study sample, and prevalence of dyssynchrony in men was approximately 5 times higher than in women (Table 1).
The age of the patients ranged between 27 and 96 years, with an average of 63.6 years. Most participants (63.8 %) were over 59 years old. Although the prevalence of LVD was higher in the 60–69 years age group, there was no statistically significant correlation between age and dyssynchrony.
Obesity had a positive association with LVD. Individuals with a BMI of ≥30 kg/m2 accounted for only 23.5 % of the study sample, but the prevalence of dyssynchrony in this group was approximately 2 times higher than that in the non-obese individuals, and the prevalence ratio was 1.89. This study only evaluated patients witha BMI ≤34.9 kg/m2(grade I obesity), and a stronger association might have been found if grade II and morbidly obese individuals had been included.
Smoking, presence of symptoms, and family history of CAD were not significantly associated with LVD. In contrast, high blood pressure, diabetes, and dyslipidemia were significantly associated with LVD, with prevalence ratios more than twice greater than in unaffected individuals (Table 1).
The duration of the QRS interval was significantly associated with dyssynchrony (p < 0.001). Patients with a QRS interval ≥120 ms accounted for 5.4 % of the sample population, and the prevalence of LVD in this group was 24.1 %. The majority of individuals (94.6 %) had a narrow QRS interval (<120 ms), and the prevalence of LVD in this group was only 5.5 %. The prevalence ratio was 4.38.
There was a significant correlation between previous history of CAD and LVD. The prevalence of dyssynchrony among patients with CAD was approximately 5 times higher than in those without CAD (prevalence ratio: 4.44) (Table 1). Previous history of acute myocardial infarction (AMI) was the variable most strongly associated with LVD. Patients with AMI had a prevalence of dyssynchrony that was 7.26 times higher than in those without AMI. The prevalence of LVD among individuals who had undergone surgical revascularization was significantly higher than that in patients who underwent percutaneous coronary angioplasty (15.8 vs. 12.8 %).
With regard to the pattern of myocardial perfusion in the MPI examination report, fixed defects (suggestive of myocardial fibrosis) were more strongly associated with LVD. Only 73 reports described fixed defects,with a prevalence of dyssynchrony of 41.1 %. However, the correlation of dyssynchrony with reversible defects (compatible with presence of myocardial ischemia) did not seem to be significant: 61 reports described reversible defects, with a prevalence of 4.9 %. In addition, 48 reports described partially reversible defects (suggestive of ischemia associated with myocardial fibrosis) possibly due to presence of fibrosis (fixed defect), with a prevalence of LVD of 27.1 %. All associations were statistically significant (p < 0.001) (Table 2).
The presence of LV dysfunction correlated with LVD (p < 0.001). Patients with normal LV function (LV ejection fraction [LVEF] ≥45 %) accounted for the majority of the population (96.9 %), and the prevalence of LVD in this group was estimated to be 3.6 %. Furthermore, the prevalence of LVD was 95.2 % in patients with mild to moderate dysfunction (LVEF of 36–44 %) and 100 % among those with severe dysfunction (LVEF ≤35 %).
The patients with LVD showed higher average end-systolic and end-diastolic LV volumes. However, the differences in these parameters between the rest and stress phases were not statistically significant.
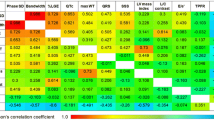
In this study, a multivariate analysis was performed using a logistic regression model to investigate the relationships between a number of variables and dyssynchrony. After the multivariate analysis, the variables that remained significantly associated with LVD were obesity, dyslipidemia, fixed and partially reversible perfusion defects, and LV dysfunction with an LVEF below 45 %.
A multivariate analysis was performed with risk factors present before the MPI examination used to calculate the expected prevalence of LVD. This analysis revealed that the variables significantly associated with LVD were male sex, obesity, history of CAD, and QRS interval ≥120 ms (Table 3).
Based on this analysis, the final predictive model was created for the expected prevalence of LVD before MPI according to the risk factors of the patients (Table 4).
According to this predictive model, the expected prevalence of LVD on MPI in men with a history of CAD and a normal QRS interval is approximately 15 %. In such patients, a QRS interval ≥120 ms increases the prevalence to 42 %. The expected prevalence of LVD in obese women with a history of CAD and a QRS interval of ≥120 ms is approximately 17.4 %.
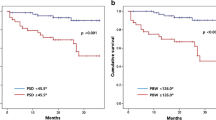
Regarding the PA measurements during stress and rest phases, although the PSD and PHB were greater at rest (27.6 vs. 20.2, p < 0.001; and 78.2 vs. 55.6, p < 0.001;respectively), LVD could be diagnosed under stress in all patients who were diagnosed at rest, with only minor differences in values. Thus, as shown in Fig. 1, the two phases were equally useful in the diagnosis, with intraclass correlation coefficients of 0.59 and 0.65, suggesting that both of them can be used.
Discussion
LVD has an important prognostic value. In patients with HF, its presence indicatesan increased risk of malignant arrhythmias and death from all causes, regardless of the LVEF [5]. In asymptomatic patients without evidence of heart disease and with normal LVEF, LVD is an early marker of progression of LV dysfunction, and it helps to identify individuals at a higher risk of developing HF [4–6].
LVD can be diagnosed by MPI quickly and automatically based on PA parameters obtained using software. The technique does not depend on the examiner, it is easily accessible, and it allows a retrospective evaluation [10–20].
In this study, the variables most closely associated with LVD were male sex, presence of hypertension, diabetes, dyslipidemia, and obesity, QRS interval ≥120 ms, history of CAD (primarily acute myocardial infarction), LV dysfunction (LVEF <45 %), and presence of myocardial perfusion defects, especially of the fixed type(suggestive of myocardial fibrosis).
Although older age was previously found to be associated with LVD [4], no statistically significant association was detected in the present study. The average age of the study group was 63.6 years, and the prevalence of LVD was higher in the 60–69 years age group.
In this study, gender male was an independent predictor of LVD as previously described 1. During the cardiac aging process, women are more likely to preserve myocardial mass and structure, whereas men tend to have greater myocyte cell loss and cellular reactive hypertrophy. These sex‐related differences may also reflect different mechanisms of dyssynchrony induction among the two gender groups [1].
Presence of symptoms (including chest pain or dyspnea) and family history of CAD showed no correlations with LVD. Smoking showed a weak association with LVD, which was not statistically significant.
Obesity was significantly associated with LVD both in the univariate and multivariate analyses. The prevalence of LVD in individuals with a BMI <30 kg/m2 was 5.4 %, and it was almost twice higher in obese individuals (10.2 %).
The duration of the QRS interval was associated with LVD in both the univariate and multivariate analyses. The prevalence of LVD in patients with a QRS interval ≥120 ms was 24.1 %, approximately five times higher than in patients with a QRS interval <120 ms (5.5 %). This finding confirms the hypothesis that electrical dyssynchrony can cause mechanical dyssynchrony.
In the logistic regression model, the QRS interval was not associated with LVD, probably because this analysis included data on MPIusing ECG-gated SPECT. Approximately 60 % of the patients with a QRS interval ≥120 ms had fixed defects and/or LV dysfunction, and these variables were associated with LVD in the multivariate analysis.
Hypertension, diabetes, and dyslipidemia are known causes of LVD. In the present study, these risk factors were associated with LVD, and their prevalence ratio was more than two times higher than that in normal subjects.
Previous history of CAD showed a statistically significant association with LVD. The prevalence of LVD in patients with AMI was 7.26 times higher than in individuals without AMI. Myocardial revascularization was also associated with LVD, and the prevalence of LVD was slightly higher in patients who underwent surgical revascularization compared with those who underwent percutaneous revascularization (15.8 vs. 12.8).
Based on the examination reports of patients who underwent MPI with gated SPECT, presence of fixed perfusion defects (suggestive of myocardial fibrosis) had the strongest correlation with LVD. Reversible defects (compatible with myocardial ischemia) showed a positive but weaker association. Therefore, LVD on MPI appears to be more strongly associated with presence of fibrotic scarring than presence of myocardial ischemia.
Based on the examination reports, most patients (96.9 %) had a normal LVEF (≥45 %), and the prevalence of LVD in this group was only 3.6 %. In contrast, 70.6 % of the patients with mild to moderate dysfunction and all the patients with severe LV dysfunction (LVEF ≤35 %) had LVD.
In agreement with the results of previous studies, the PA parameters were higher in the resting phase, as physical effort optimizes the timing of intraventricular contraction [21–23]. These findings were thought to be related to stress-induced increased hyperemia leading to more signal and less noise during phase analysis, but also to improved LV contractility that can occur with vasodilator testing [24]. Some research suggests that this relationship is reversed in the presence of myocardial ischemia, with values in the stress phase exceeding those in the rest phase [23]. Such a relationship was not observed in the current study, which demonstrated that PA parameters in subjects with ischemia were greater at rest than under stress. In the above investigations, 201TI was used as a radiotracer, and the fact that image acquisition began 5 min after injection, allowing early assessment of the stress phase, was used to justify this finding. Although 99mTc sestamibi was used in the present study, data acquisitions also began early after stress induction, and therefore our data contradict the previous results.
This study evaluated the prevalence of dyssynchrony in a non-selected population patients undergoing MPI. The findings obtained in patients with normal ventricular function indicate that such patients may develop dysfunction in the future, and closer monitoring may be recommended. Further study is required to confirm this hypothesis.
Conclusions
LVD is an important and relatively frequent prognostic marker, with a prevalence of 6.5 %. Furthermore, the prevalence of LVD can reach 42 % in the presence of some risk factors. MPI can be used to diagnose LVD without causing additional discomfort to patients undergoing the examination, and both the rest and stress phases can be utilized for this purpose.
Limitations
This was a single-center study, although it was conducted at a major reference center in Brazil. The study population, which included individuals with suspected CAD and/or risk factors that necessitated MPI with ECG-gated SPECT, may not fully represent the general population.
References
Sharma RK, Volpe G, Rosen BD, Donekal S, Fernandes V, Wu CO et al (2014) Prognostic implications of left ventricular dyssynchrony for major adverse cardiovascular events in asymptomatic women and men: the multi-ethnic study of atherosclerosis. J Am Heart Assoc 3:1–12
Ovadia M, Abudayyeh I (2014) Risk stratification by quantitation of LV dyssynchrony: a new branch of the field of nuclear cardiology. J Nucl Cardiol 21:747–752
Brandão SCS, Giorgi MCP, Nishioka SAD, Meneghetti JC (2011) Papel da medicina nuclear na terapia de ressincronização cardíaca. Rev Bras Ecocardiogr 24:62–72
Rosen BD, Fernandes VRS, Nasir K, Helle-Valle T, Bluemke DA, Lima JAC et al (2009) Age, increased left ventricular mass, and lower regional myocardial perfusion are related to greater extent of myocardial dyssynchrony in asymptomatic individuals: the multi-ethnic study of atherosclerosis. Circulation 120:859–866
Yamada S, Arrell K, Kane GC, Nelson TJ, Perez-Terzic CM, Behfar A et al (2013) Mechanical dyssynchrony precedes QRS widening in ATP-sensitive K + channel–deficient dilated cardiomyopathy. J Am Heart Assoc 2:1–12
Piran S, Liu P, Morales A, Hershberger RE (2012) Where genome meets phenome: rationale for integrating genetic and protein biomarkers in the diagnosis and management of dilated cardiomyopathy and heart failure. J Am Coll Cardiol 60:283–289
Chen J, Garcia EV, Bax JJ, Iskandrian AE, Borges-Neto S, Soman P (2011) SPECT myocardial perfusion imaging for the assessment of left ventricular mechanical dyssynchrony. J Nucl Cardiol 18:685–694
Frais MA, Botvinick EH, Shosa DW, O’Connell WJ, Sheinman MM, Hattner RS et al (1982) Phase image characterization of ventricular contraction in left and right bundle branch block. Am J Cardiol 50:95–105
Cooke CD, Garcia EV, Cullom SJ, Faber TL, Pettigrew R (1994) Determining the accuracy of calculating systolic wall thickening using a fast Fourier transform approximation: a simulation study based on canine and patient data. J Nucl Med 35:1185–1192
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe L et al (2005) Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol 12:687–695
Zafrir N, Nevzorov R, Bental T, Strasberg B, Gutstein A, Mats I et al (2014) Prognostic value of left ventricular dyssynchrony by myocardial perfusion-gated SPECT in patients with normal and abnormal left ventricular functions. J Nucl Cardiol 21:532–540
Atchley AE, Trimble MA, Samad Z, Shaw LK, Pagnanelli R, Chen J et al (2009) Use of phase analysis of gated SPECT perfusion imaging to quantify dyssynchrony in patients with mild-to-moderate left ventricular dysfunction. J Nucl Cardiol 16:888–894
Chen J, Bax JJ, Henneman MM, Boogers MJ, Boogers MJ, Garcia EV (2008) Is nuclear imaging a viable alternative technique to assess dyssynchrony? Europace 10:101–105
Henneman MM, Chen J, Ypenburg C, Dibbets P, Bleeker GB, Boersma E et al (2007) Phase analysis of gated myocardial perfusion single-photon emission computed tomography compared with tissue Doppler imaging for the assessment of left ventricular dyssynchrony. J Am Coll Cardiol 49:1708–1714
Marsan NA, Henneman MM, Chen J, Ypenburg C, Dibbets P, Ghio S et al (2008) Left ventricular dyssynchrony assessed by two three-dimensional imaging modalities: phase analysis of gated myocardial perfusion SPECT and tri-plane tissue Doppler imaging. Eur J Nucl Med Mol Imaging 35:166–173
Trimble MA, Velazquez EJ, Adams George L, Honeycutt Emily F et al (2008) Repeatability and reproducibility of phase analysis of gated SPECT myocardial perfusion imaging used to quantify cardiac dyssynchrony. Nucl Med Commun 29:374–381
Lin X, Xu H, Zhao X, Folks RD, Garcia EV, Soman P et al (2010) Repeatability of left ventricular dyssynchrony and function parameters in serial gated myocardial perfusion SPECT studies. J Nucl Cardiol 17:811–816
Trimble MA, Borges-Neto S, Honeycutt EF, Shaw LK, Pagnanelli R, Chen J et al (2008) Evaluation of mechanical dyssynchrony and myocardial perfusion using phase analysis of gated SPECT imaging in patients with left ventricular dysfunction. J Nucl Cardiol 15:663–670
Samad Z, Atchley AE, Trimble MA, Sun JL, Shaw LK, Pagnanelli R et al (2011) Prevalence and predictors of mechanical dyssynchrony as defined by phase analysis in patients with left ventricular dysfunction undergoing gated SPECT myocardial perfusion imaging. J Nucl Cardiol 18:24–30
Chen J, Kalogeropoulos AP, Verdes L, Butler J, Garcia EV (2011) Left-ventricular systolic and diastolic dyssynchrony as assessed by multi-harmonic phase analysis of gated SPECT myocardial perfusion imaging in patients with end-stage renal disease and normal LVEF. J Nucl Cardiol 18:299–308
Chen CC, Huang WS, Hung GU, Chen WC, Kao CH, Chen J (2013) Left ventricular dyssynchrony evaluated by Tl-201 gated SPECT myocardial perfusion imaging: a comparison with Tc-99m sestamibi. Nucl Med Commun 34:229–232
Harmandeep S, Patel CD, Sharma P, Naik N, Singh S, Narang R (2015) Does perfusion pattern influence stress-induced changes in left ventricular mechanical dyssynchrony on thallium-201-gated SPECT myocardial perfusion imaging? J Nucl Cardiol 22:36–43
Chen CC, Shen TY, Chang MC, Hung GU, Chen WC, Kao CH et al (2012) Stress-induced myocardial ischemia is associated with early post-stress left ventricular mechanical dyssynchrony as assessed by phase analysis of Tl-201 gated SPECT myocardial perfusion imaging. Eur J Nucl Med Mol Imaging 39:1904–1909
AlJaroudi W, Alraies MC, DiFilippo F, Brunken RC, Cerqueira MD, Jaber WA (2012) Effect of stress testing on left ventricular mechanical synchrony by phase analysis of gated positron emission tomography in patients with normal myocardial perfusion. Eur J Nucl Med Mol Imaging 39:665–672
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no financial or other conflict of interest.
Ethical standards
The institutional review board approved the study and informed consent was obtained from all patients.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Rights and permissions
About this article
Cite this article
Tavares, A., Peclat, T. & Lima, R.S.L. Prevalence and predictors of left intraventricular dyssynchrony determined by phase analysis in patients undergoing gatedSPECT myocardial perfusion imaging. Int J Cardiovasc Imaging 32, 845–852 (2016). https://doi.org/10.1007/s10554-015-0833-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-015-0833-5