Abstract
Measurement of left ventricular (LV) mechanical dyssynchrony from single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) allows optimization of cardiac resynchronization therapy in heart failure patients. We compared the discriminatory ability and reproducibility of a new software method, Corridor 4DM (4DM) to the established method, Emory Cardiac Toolbox (ECTb) in normals and heart failure patients. LV dyssynchrony was measured in 100 control (Group 1) and 100 patients with LVEF <35% (Group 2) using time to peak thickening with first harmonic, fourth harmonic, and volume curve methods with the 4DM software, and compared to ECTb. Of the 3 4DM methods, first harmonic had the best correlation with the ECTb (R = 0.88, slope = 1.00, P < 0.0001, bias = −0.18° [95% CI: −20°; 16°] for phase standard deviation; and similarly for histogram bandwidth, while volume curve analysis had the greatest variation. The intra and inter-observer reproducibility for 4DM time to peak thickening with first harmonic was very good (R = 0.99, P < 0.0001 and coefficient of variability 10% [95% CI 9.2–12%] for intra-observer, and R = 0.97, P < 0.0001, coefficient of variability 16% [15–17%] for inter-observer, respectively). Finally, in patients with LVEF <35%, the area under the curve on receiver operator characteristic analysis was 0.93 [95% CI: 0.89–0.97] to detect significant mechanical dyssynchrony (i.e. standard deviation ≥43°) using 4DM versus ECTb. The 4DM-software provides an accurate and reproducible alternative method of dyssynchrony analysis of SPECT MPI for evaluation and management of heart failure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
In a research environment, dyssynchrony analysis by several different imaging modalities provides important information in the identification and optimization of patients with heart failure who may benefit from cardiac resynchronization therapy (CRT) [1, 2]. There have been several hundred published papers on left ventricular (LV) mechanical dyssynchrony using multi-imaging modalities within the last decade.
Phase analysis of gated single photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) has recently emerged as a robust, automated, and reproducible technique to quantify LV mechanical dyssynchrony [3]. Alternative techniques such as echocardiography do not reliably predict responders [1, 4]. Although the application of mechanical dyssynchrony in daily clinical decision making by any modality is still limited, the increasing use of CRT and the growing heart failure population identify an important clinical need.
Since SPECT MPI is frequently performed in the heart failure population to identify the presence of ischemia and viability, information on dyssynchrony is readily available in such patients without the need to do additional testing. Published data on SPECT MPI dyssynchrony has predominately relied on the Emory Cardiac Toolbox software (ECTb Atlanta, GA) to generate the dyssynchrony indices (phase standard deviation and histogram bandwidth), in diverse patient populations [3, 5–13], and with limited data using other software such as QGS [14]. A new software program for SPECT MPI dyssynchrony analysis that provides three different methods of analysis has been developed (Corridor4DM, 4DM Invia, Ann Arbor, MI) [15]. Since this software provides an alternative method of analysis to ECTb for research and clinical applications of dyssynchrony, the purpose of our study was to compare the 3 methods of dyssynchrony analysis available in Corridor 4DM with the ECTb (as reference method in out study), to expand the available clinical tools to measure mechanical dyssynchrony by SPECT MPI.
Methods and materials
Patient selection
From the prospective SPECT MPI clinical database maintained at the Cleveland Clinic and approved by the Institutional Review Board, we identified 2 consecutive groups of patients between April 2007 and February 2008. Group 1 (N = 100) had normal LV ejection fraction (EF) (≥50%), normal MPI, and QRS duration <120 ms; Group 2 (N = 100) had LVEF <35% with no restriction on QRS duration. All patients had a low dose rest/high dose stress Tc-99m tetrofosmin MPI with gated SPECT. Patients with hypertrophic cardiomyopathy, end-stage renal disease, congenital heart disease, and CRT were excluded. The demographics, co-morbidities and medications were entered into an IRB approved data base at the time of testing.
Gated SPECT MPI
Gated SPECT MPI was obtained at rest (low dose 9–15 mCi) and stress (exercise or pharmacological) (high dose ~30–45 mCi) using Tc-99m tetrofosmin according to American Society of Nuclear Cardiology guidelines [16]. Using a dual-headed detector gamma camera with high resolution, low energy collimators, images were acquired in a 64 × 64 matrix with a step and shoot protocol, 180o elliptical orbit and 64 total projections. A window of ±15% was centered on the 140 keV gamma peak, and the gating was done with 16 frames per RR cycle. Imaging was started 30–60 min after resting or pharmacological stress (i.e. adenosine) and 10–20 min following exercise stress. Images were reconstructed by filtered back projection using Ramp and Butterworth filters (5th order Butterworth and cut-off frequency of 0.4 for gated images, and 3rd order Butterworth and cut-off frequency 0.66 for nongated tomograms). Scatter and attenuation correction were not performed. All images were reviewed for quality by a nuclear technologist and a board certified nuclear cardiologist.
The LV volumes, mass, and EF were measured from the higher dose stress gated images. The presence and extent of ischemia and infarction was assessed visually, and quantified using semi-automated polar maps as previously described [17, 18].
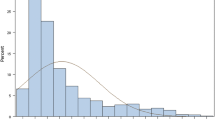
Phase analysis with Emory Toolbox
The phase standard deviation and histogram bandwidth were measured from the stress gated SPECT (higher counts due to hyperemia and higher tracer dose) by a single observer (WA). The method has been extensively described and reviewed [3, 19]. Briefly, 3-dimensional count distributions were extracted from each of the LV short -axis data sets and Fourier transformed to generated a 3-dimentional phase distribution (0–360°) spanning the entire R–R interval and represented on a histogram (Fig. 1). The phase standard deviation represented the standard deviation of the phase distribution, while the histogram bandwidth represented the duration of the cardiac cycle during which 95% of the myocardium initiated contraction [3].
Representative contractility histogram with the 4DM software. The upper panel has two representative histograms of a patient with normal LVEF, MPI and QRS duration <120 ms, showing narrow phase distribution with the ECTb (left) and 4DM software (right), respectively; while the lower panel shows the histograms of a patient with LVEF 30% and QRS < 120 ms but with significant mechanical dyssynchrony with both software. The phase standard deviation and 95% histogram bandwidth are expressed as % of the R–R interval in the 4DM software, and the corresponding values in degrees are derived by multiplying by 3.6 (360/100). 4DM (Corridor4DM software); BW (histogram bandwidth); ECTb (Emory cardiac toolbox); LVEF (left ventricular ejection fraction); MPI (myocardial perfusion imaging); SD (phase standard deviation)
Phase analysis with Corridor4DM
The dyssynchrony indices (phase standard deviation and histogram bandwidth) were generated with the 4DM software using three different methods. Method 1 estimates the time to peak thickening using a single harmonic fit (TPT-1), and is closely modeled to the algorithm used in the ECTb. In this method, the maximum myocardial intensity as a function of the gating interval is recorded from a 3-dimensional sampling of the LV myocardium. Each of the time-intensity curves are fitted to a first-order harmonic using Fourier analysis, from which the phase of the first-order harmonic approximates the time from end-diastole (typically the start of the cardiac cycle) to the time of the maximum counts for each region, which represents the peak of mechanical contraction. Even though the ECTb method defines the phase that measures the onset of mechanical contraction, the time point at which the maximal count curve crosses the DC or mean line [19], the time to peak mechanical contraction of Method 1 is the same as the onset of mechanical contraction of the ECTb method but shifted by +90 degrees. This is because the angular distance between the point of the increasing curve intersecting with the DC line and the maximum point of the first harmonic sinusoid is always a constant 90 degrees, as can be shown by taking the difference of the roots of a sinusoid and its derivative. By this equivalence, the temporal resolution of Method 1 is also 1/64 of a cardiac cycle whether 8 or 16 frames/cycle per used for image acquisition [20].
Method 2 uses the same time-intensity curve as in Method 1 but fits the curve to a continuous 4th order harmonic function (TPT-4), which includes the first 4 harmonics, from which the time from end-diastole to the maximum value is found to be the time to peak thickening. The temporal resolution of Method 2 is the same as that of Method 1 or less, since a 4th order harmonic is higher resolution function.
Method 3 is analogous to the method used in 3D echo to find the time to peak contraction (TPC). This method uses the 4DM estimated endocardial surfaces of the LV to estimate regional changes in volume during the cardiac cycle. Using a 3-dimensional hybrid cylindrical/spherical sampling, the regional volumes are computed for each frame, based on the respective formulas for a volume of a cylindrical or spherical wedge. Each regional volume as a function of the gating interval is fitted to a continuous 4th order harmonic function, which includes the first 4 harmonics, from which the time from end-diastole to the minimum value is found to be to analogous to the time to peak mechanical contraction.
The generated indices were displayed as percentage of the RR cycle, and converted into degrees by multiplying by 3.6 (360/100) (Fig. 1). The derived parameters were compared against those obtained by the ECTb. The intra- and inter-observer reproducibility of the phase were assessed by two blinded experienced readers who have re-read all 200 studies after 4 weeks of the first reading (WA and WJ).
Statistical analysis
A descriptive analysis was performed examining selected variables for each group. Continuous variables were expressed as means ± standard deviation, and categorical variables as percentages. The unpaired Student t test was used to compare continuous variables, and Pearson Chi-square test for categorical variables. Linear regression was used for the correlation of dyssynchrony indices between 4DM and ECTb, and Bland–Altman plots were generated to assess for bias. Receiver-operating characteristic (ROC) analysis was used to compare the results of the 4DM software versus the ECTb in diagnosing mechanical dyssynchrony. Intra and inter-observer reproducibility were assessed using the Spearman correlation coefficient, coefficient of variability and Bland–Altman plots for continuous variables. A P value < 0.05 was set a priori and considered statistically significant. All statistical analyses were performed using the Statistical Package for Social Sciences, version 11.5, for Windows (SPSS, Chicago, Illinois).
Results
There were 100 patients in Group 1 (age 65 ± 12 years, LVEF 70 ± 9%, all with normal perfusion and QRS < 120 ms) and 100 patients in Group 2 (age 68 ± 11 years, LVEF 29 ± 5%, 51% with prior myocardial infarction, and 17% with left bundle branch block). The pertinent demographics, co-morbidities, medications, and gated-SPECT MPI variables are displayed in Table 1.
Three different methods to generate dyssynchrony indices by the 4DM software were tested in all patients (N = 200). TPT-1 correlated best with the ECTb (R = 0.88, slope = 1.00, P < 0.0001, Bland–Altman bias = −1.8° [95% CI: −20°; 16°] for phase standard deviation; and R = 0.84, slope = 0.67, P < 0.0001, Bias = 22° [95% CI: −82°; 127°] for histogram bandwidth), while TPC showed the most variability and inconsistency (Fig. 2). Furthermore, the intra and interobserver reproducibility was high, particularly for TPT-1, R = 0.99, P < 0.0001 and coefficient of variability 10% (95% CI 9.2–12%) for intra-observer, and R = 0.97, P < 0.0001, coefficient of variability 16% (15–17%) for inter-observer, respectively for all patients (N = 200) (Fig. 3). For patients in Group 1, the correlation coefficient for intra and inter-observer reproducibility were R = 0.93 and 0.94, respectively; while for patients in Group2, the corresponding correlation coefficients were R = 0.99 and 0.96, respectively (P < 0.0001 for all values). In addition, the standard deviation and histogram bandwidth showed excellent correlation (R = 0.98 and R = 0.95, with 4DM and ECTb, respectively, P < 0.0001 for both) for all patients.
Validation of the 4DM-software against the ECTb. Three different methods of the 4DM-software were tested against the ECTb (panels a, b and c respectively for each method). Linear regression and Bland–Altman plots are shown in the upper and lower rows for each method, respectively. ECTb (Emory Cardiac Toolbox); R (correlation coefficient); SD (phase standard deviation); SEE (standard error of the estimate); TPC (time to peak contraction); TPT-1 (time to peak thickening using first harmonic); TPT-4 (time to peak thickening using fourth harmonic)
Intra and Inter-observer reproducibility. The intra and inter-observer reproducibility was very good as depicted in the linear regression plot (upper row) and in the Bland–Altman plot (bottom row) for method 1 (time to peak thickening with first harmonic) (N = 200). R (Correlation coefficient); SD (phase standard deviation)
Group 2 patients with cardiomyopathy had a significantly higher phase standard deviation and histogram bandwidth (4DM) than the control Group (Fig. 4). Similar values were found with the ECTb (standard deviation 41° ± 20° versus 7.9° ± 4.8°, and bandwidth 123° ± 67° versus 24° ± 11°, for group 2 versus group 1, respectively, P < 0.0001 for both). Also, in patients with cardiomyopathy, those with wide QRS had higher dyssynchrony indices than those with narrow QRS duration (Fig. 4).
Dyssynchrony indices in normal cohort and patients with cardiomyopathy. There is significant increase in dyssynchrony indices by phase analysis using the 4DM software (TPT-1 method) in patients with cardiomyopathy (group 2, mean LVEF 29 ± 5%) versus normal cohort (N = 100 in each group). Patients with QRS > 120 ms had more significant dyssynchrony. LVEF (left ventricular ejection fraction); TPT-1 (time to peak thickening with first harmonic)
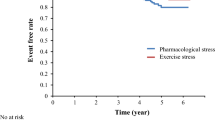
The area under the curve (AUC) on ROC analysis was 0.97 (95% CI: 0.95–0.99) to differentiate normal versus abnormal synchrony, using a phase standard deviation cut-off of 17.5° = mean + 2× standard deviation from Group 1 with ECTb (N = 200), and 0.93(0.89–0.97) to detect significant mechanical dyssynchrony (i.e. SD ≥ 43°) [12] in patients with cardiomyopathy (Group 2, Fig. 5).
Receiver operating curve analysis showing diagnostic accuracy in detecting mechanical dyssynchrony. Receiver operating curve analysis with 95% confidence intervals lines showing diagnostic accuracy of the 4DM-software (TPT-1) in detecting mechanical dyssynchrony using different cut-off values versus the Emory cardiac tool box (as gold standard). AUC (area under the curve); LVEF (left ventricular ejection fraction); ROC (receiver operator curve); SD (standard deviation)
Discussion
Our results show that SPECT MPI dyssynchrony phase analysis indices obtained by the 4DM software using the first harmonic method of analysis provide comparable results to those obtained using the well established ECTb. The method is able to discriminate between normals and patients with cardiomyopathies and is highly reproducible. Although mechanical dyssynchrony is not routinely measured in daily clinical decision makings, the frequency with which SPECT MPI is being performed in the heart failure population makes this a readily available technique to predict response to CRT and optimize patient selection [1, 2, 21].
Since the majority of the published work on mechanical dyssynchrony with phase analysis on gated SPECT has relied on a single software program, ECTb, the availability of alternative methods of software analysis such as 4DM, will make the technique more widely available. Results have also been published using a 3rd software program QGS [14].
Of the three potential methods of analysis by 4DM, TPT-1 correlated best with the ECTb, and had the highest intra and inter-observer reproducibility, and least bias (Fig. 2). The results were somewhat expected as the TPT-1 algorithm is most similar in principle to the algorithm (i.e. time-intensity curves fitted to a single harmonic) used in the ECTb, although they differed with the timing of phase angle measurements, i.e. time to peak contraction versus onset of mechanical contraction. Correlation between TPT-4 and ECTb was also good, but showed an increase in bias in the SD value compared to TPT-1, which is expected since adding further harmonics increases noise. The TPC method is analogous to the method used with real time 3D echocardiography; however, it correlated the least with ECTb, most likely due to the inaccurate edge detection associated with the relatively low count SPECT data sets.
The measured phase angles with ECTb are done at onset of mechanical contraction versus peak contraction with 4DM, which explains the variability in the measured phase angles. However, the standard deviation of the phase angle distribution in a given cardiac cycle, which is the dyssynchrony index, remains comparable, although both techniques and measures are not interchangeable. Hence, for serial measurements, the same software should be used for comparison. In addition, 4DM derived phase standard deviation and 95% histogram bandwidth had excellent correlation since one defines the other, as previously published with the ECTb [3, 5–7, 11, 22].
In this study, stress gated images (obtained with high tracer dose) were used to derive dyssynchrony indices. While most published studies have used resting gated MPI (also obtained with high dose tracer) to derive phase SD and bandwidth, our resting images were obtained from low dose tracer (same day protocol). Low tracer dose images have low counts, and hence the phase analysis could be more prone to artifacts, noise, and falsely higher indices. In fact, recent study have shown that dyssynchrony indices obtained from low tracer dose rest images are significantly larger as compared to those obtained from high tracer dose stress gated images [23].
Study limitations
This study has the limitations as a retrospective study from a single tertiary center. Also, it does not offer clinical data yet using the new software, although such studies are currently in progress.
The stress gated SPECT MPI was used in this study as opposed to conventional rest gated studies because the higher tracer dose provided better images and counts as discussed in the method section. The performance of gated images at least 30–45 min after peak stress minimized potential error caused by ischemia and stunning as 25% of patients in group 2 had at least moderate (≥10%) and 13% had severe (≥20%) reversible perfusion defects. In fact, recent study have shown no difference in dyssynchrony indices obtained from stress versus rest gated SPECT in patients with ischemia, including those with moderate to large reversible perfusion defect size [9]9. Furthermore, despite the very good correlation and minimal bias, there was still some variation in the results. Possible explanations are that the software use different algorithms (onset of mechanical contraction versus peak contraction to derive phase angle), presence of artifacts, arrhythmias, and improper border tracking. We opted however not to exclude any data point, which strengthened our findings. Although the software is automated, the intra and inter-observer variability was not insignificant. The main reason is that there is an operator dependancy when selecting the image planes and apex, which can be somewhat challenging in images with large perfusion defect size. This variability was also reported using the ECTb when assessing dyssynchrony on serial images and follow-up studies, and was significantly smaller when the parameters were measured using side by side processing [22]. In fact, similar intra and inter observer error is seen when generating LV volumes and EF despite having an automated software. Future studies to assess the reproducibility of the 4DM software with serial gated imaging, as well as optimizing selection of patients for resynchronization therapy based on a standard deviation threshold are warranted.
Furthermore, we did not have an independent reference standard used to define dyssynchrony. Although we compared two software using gated SPECT to derive dyssynchrony parameters, the ECTb was validated in prior studies against echocardiography. The poor reproducibility of echocardiography derived dyssynchrony parameters, however, at least with tissue Doppler imaging, have put in question whether echocardiography is indeed the standard reference method [4]. Hence, many currently feel that phase analysis, at least because of its automaticity, great reproducibility, and ability to average over several RR intervals is a better tool for mechanical dyssynchrony.
In addition, we did not include patients with mild-moderate LV dysfunction. While the new software showed difference in mechanical dyssynchrony in patients with normal and abnormal LVEF, between narrow and wide QRS (Fig. 4), further data are warranted to show whether it can discriminate bundle branch block or right ventricular pacing from normal electrical conductance (shown in a small subset of patients, Fig. 4), and whether it is predictive of clinical outcomes. Such studies are being conducted. Also, the effective temporal resolution of this new software needs to be tested and verified, similar to the ECTb [20].
Future directions
The same algorithm of the 4DM dyssynchrony toolbox can be extrapolated to gated PET images which have higher counts per pixel, better spatial and temporal resolution, and theoretically should have less noise and more accurate data. The prognostic value of such parameters in patients with cardiomyopathy is of great interest and is in progress.
Conclusion
In conclusion, the 4DM TPT-1 software provides a semi-automated and reproducible tool to derive dyssynchrony indices with comparable results with the ECTb. Future studies to assess its reproducibility in serial imaging, whether it optimizes patient selection for resynchronization and impacts clinical decision making are warranted.
References
AlJaroudi W, Chen J, Jaber WA, Lloyd SG, Cerqueira M, Marwick T (2011) Non-echocardiographic imaging of cardiac resynchronization therapy. Circ CV Imaging 4:334–343
Boogers MJ, Chen J, van Bommel RJ, Borleffs CJ, Dibbets-Schneider P, van der Hiel B, Al Younis I, Schalij MJ, van der Wall EE, Garcia EV, Bax JJ (2011) Optimal left ventricular lead position assessed with phase analysis on gated myocardial perfusion SPECT. Eur J Nucl Med Mol Imaging 38:230–238
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL, Iskandrian AE (2005) Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol 12:687–695
Chung E, Leon A, Tavazzi L, Sun J, Nihoyannopoulos P, Merlino J, Abraham W, Ghio S, Leclercq C, Bax JJ, Yu C, Gorcsan Jr, St John Sutton M, De Sutter J, Murillo J (2008) Results of the predictors of response to CRT (PROSPECT) trial. Circulation 117:2608–2616
Trimble MA, Borges-Neto S, Smallheiser S, Chen J, Honeycutt EF, Shaw LK, Heo J, Pagnanelli RA, Tauxe EL, Garcia EV, Esteves F, Seghatol-Eslami F, Kay GN, Iskandrian AE (2007) Evaluation of left ventricular mechanical dyssynchrony as determined by phase analysis of ECG-gated SPECT myocardial perfusion imaging in patients with left ventricular dysfunction and conduction disturbances. J Nucl Cardiol 14:298–307
Trimble MA, Borges-Neto S, Honeycutt EF, Shaw LK, Pagnanelli R, Chen J, Iskandrian AE, Garcia EV, Velazquez EJ (2008) Evaluation of mechanical dyssynchrony and myocardial perfusion using phase analysis of gated SPECT imaging in patients with left ventricular dysfunction. J Nucl Cardiol 15:663–670
Trimble MA, Velazquez EJ, Adams GL, Honeycutt EF, Pagnanelli RA, Barnhart HX, Chen J, Iskandrian AE, Garcia EV, Borges-Neto S (2008) Repeatability and reproducibility of phase analysis of gated single-photon emission computed tomography myocardial perfusion imaging used to quantify cardiac dyssynchrony. Nucl Med Commun 29:374–381
Aljaroudi W, Aggarwal H, Venkataraman R, Heo J, Iskandrian AE, Hage FG (2010) Impact of left ventricular dyssynchrony by phase analysis on cardiovascular outcomes in patients with end-stage renal disease. J Nucl Cardiol 17:1058–1064
Aljaroudi W, Koneru J, Heo J, Iskandrian AE (2011) Impact of ischemia on left ventricular dyssynchrony by phase analysis of gated single photon emission computed tomography myocardial perfusion imaging. J Nucl Cardiol 18:36–42
Aljaroudi W, Koneru J, Iqbal F, Aggarwal H, Heo J, Iskandrian AE (2010) Left ventricular mechanical dyssynchrony by phase analysis of gated single photon emission computed tomography in end-stage renal disease. Am J Cardiol 106:1042–1047
Aljaroudi WA, Hage FG, Hermann D, Doppalapudi H, Venkataraman R, Heo J, Iskandrian AE (2010) Relation of left-ventricular dyssynchrony by phase analysis of gated SPECT images and cardiovascular events in patients with implantable cardiac defibrillators. J Nucl Cardiol 17:398–404
Henneman MM, Chen J, Dibbets-Schneider P, Stokkel MP, Bleeker GB, Ypenburg C, van der Wall EE, Schalij MJ, Garcia EV, Bax JJ (2007) Can LV dyssynchrony as assessed with phase analysis on gated myocardial perfusion SPECT predict response to CRT? J Nucl Med 48:1104–1111
Samad Z, Atchley AE, Trimble MA, Sun JL, Shaw LK, Pagnanelli R, Chen J, Garcia EV, Iskandrian AE, Velazquez EJ, Borges-Neto S (2010) Prevalence and predictors of mechanical dyssynchrony as defined by phase analysis in patients with left ventricular dysfunction undergoing gated SPECT myocardial perfusion imaging. J Nucl Cardiol 18:24–30
Boogers MM, Van Kriekinge SD, Henneman MM, Ypenburg C, Van Bommel RJ, Boersma E, Dibbets-Schneider P, Stokkel MP, Schalij MJ, Berman DS, Germano G, Bax JJ (2009) Quantitative gated SPECT-derived phase analysis on gated myocardial perfusion SPECT detects left ventricular dyssynchrony and predicts response to cardiac resynchronization therapy. J Nucl Med 50:718–725
Ficaro EP, Lee BC, Kritzman JN, Corbett JR (2007) Corridor4DM: the Michigan method for quantitative nuclear cardiology. J Nucl Cardiol 14:455–465
Hansen CL, Goldstein RA, Akinboboye OO, Berman DS, Botvinick EH, Churchwell KB, Cooke CD, Corbett JR, Cullom SJ, Dahlberg ST, Druz RS, Ficaro EP, Galt JR, Garg RK, Germano G, Heller GV, Henzlova MJ, Hyun MC, Johnson LL, Mann A, McCallister BD Jr, Quaife RA, Ruddy TD, Sundaram SN, Taillefer R, Ward RP, Mahmarian JJ (2007) Myocardial perfusion and function: single photon emission computed tomography. J Nucl Cardiol 14:e39–e60
Germano G, Kiat H, Kavanagh PB, Moriel M, Mazzanti M, Su HT, Van Train KF, Berman DS (1995) Automatic quantification of ejection fraction from gated myocardial perfusion SPECT. J Nucl Med 36:2138–2147
Iskandrian AE, Garcia EV, Faber T, Mahmarian JJ (2009) Automated assessment of serial SPECT myocardial perfusion images. J Nucl Cardiol 16:6–9
Chen J, Boogers MM, Bax JJ, Soman P, Garcia EV (2010) The use of nuclear imaging for cardiac resynchronization therapy. Curr Cardiol Rep 12:185–191
Chen J, Faber TL, Cooke CD, Garcia EV (2008) Temporal resolution of multiharmonic phase analysis of ECG-gated myocardial perfusion SPECT studies. J Nucl Cardiol 15:383–391
Friehling M, Chen J, Saba S, Bazaz R, Schwartzman D, Adelstein EC, Garcia E, Follansbee W, Soman P (2011) A prospective pilot study to evaluate the relationship between acute change in LV synchrony after cardiac resynchronization therapy and patient outcome using a single-injection gated-SPECT protocol. Circ Cardiovasc Imaging 4:532–539
Lin X, Xu H, Zhao X, Folks RD, Garcia EV, Soman P, Chen J (2010) Repeatability of left ventricular dyssynchrony and function parameters in serial gated myocardial perfusion SPECT studies. J Nucl Cardiol 17:811–816
AlJaroudi W, Jaber WA, Cerqueira M (2011) Effect of tracer dose on left ventricular mechanical dyssynchrony indices by phase analysis of gated single photon emission computed tomography myocardial perfusion imaging. J Nucl Cardiol (in press)
Conflict of interest
None of the authors has a financial or any other conflict of interest with the application vendors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
AlJaroudi, W., Jaber, W.A., Grimm, R.A. et al. Alternative methods for the assessment of mechanical dyssynchrony using phase analysis of gated single photon emission computed tomography myocardial perfusion imaging. Int J Cardiovasc Imaging 28, 1385–1394 (2012). https://doi.org/10.1007/s10554-011-9963-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-011-9963-6