Abstract
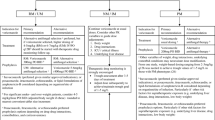
Voriconazole is an antifungal triazole that is the first-line agent for treatment of invasive aspergillosis. It is metabolized by CYP2C19, CYP2C9, and CYP3A4 and demonstrates wide interpatient variability in serum concentrations. Polymorphisms in CYP2C19 contribute to variability in voriconazole pharmacokinetics. Here, evidence is examined for the use of voriconazole therapeutic drug monitoring (TDM) and the role of CYP2C19 genotyping in voriconazole dosing. The majority of studies exploring the impact of voriconazole TDM on efficacy and safety have found TDM to be beneficial. However, most of these studies are observational, with only one being a randomized controlled trial. High-volume multicenter randomized controlled trials of TDM are currently not available to support definitive guidelines. There is a significant relationship in healthy volunteers between CYP2C19 genotype and voriconazole pharmacokinetics, but this association is markedly less visible in actual patients. While CYP2C19 genotype data may explain variability of voriconazole serum levels, they alone are not sufficient to guide initial dosing. The timeliness of availability of CYP2C19 genotype data in treatment of individual patients also remains challenging. Additional studies are needed before implementation of CYP2C19 genotyping for voriconazole dosing into routine clinical care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Voriconazole is an antifungal triazole approved by the FDA for the treatment of invasive aspergillosis, esophageal candidiasis, candidemia in non-neutropenic patients, disseminated Candida infections, and infections caused by Scedosporium apiospermum and Fusarium spp. [1]. Infectious Diseases Society of America (IDSA) guidelines recommend voriconazole as a first-line agent for the treatment of invasive aspergillosis and as an alternative agent for the treatment of candidemia [2, 3].
Voriconazole is metabolized in the liver by CYP3A4, CYP2C9, and CYP2C19 and demonstrates wide interpatient variability in serum concentrations [4, 5]. Polymorphisms in CYP2C19, but not in CYP3A5 or CYP2C9, have been reported to affect its pharmacokinetics [6, 7, 8•]. Other factors including age, liver function, and concomitant medications contribute to variability in voriconazole concentrations [4, 5]. In addition, voriconazole demonstrates saturable, non-linear pharmacokinetics in adults [9].
The field of pharmacogenomics seeks to understand variations in the response to medications based on inherited and acquired genetic differences between patients [10, 11]. The prospect of pharmacogenomics testing has been explored for a myriad of medications including CYP2C19 genotyping to aid voriconazole dosing [12•]. Guidelines from the Royal Dutch Pharmacists Association Pharmacogenetics Working Group recommend monitoring voriconazole serum concentrations in patients expressing the CYP2C19 poor metabolizer (PM) and CYP2C19 intermediate metabolizer phenotypes [13]. However, there is a paucity of guidelines for pharmacogenomic testing in patients treated with voriconazole. Common side effects of voriconazole include hepatotoxicity, neurotoxicity, blurry vision, skin rash, and hyperfluorosis [14]. Some of these adverse effects are more likely to occur at higher than necessary voriconazole serum/plasma concentrations, while low voriconazole levels may result in therapeutic failure [12•]. As such, voriconazole therapeutic drug monitoring (TDM) has become commonplace in the management of serious fungal infections. The objective of this review is to critically examine the evidence of the relationships among CYP2C19 genotype, voriconazole serum concentrations, and clinical outcomes.
CYP2C19 Polymorphisms
CYP2C19 catalyzes the metabolism of numerous commonly prescribed drugs including antidepressants, anticancer agents, clopidogrel, proton pump inhibitors, diazepam, and voriconazole [15–17]. The CYP2C19 gene exhibits significant ethnic differences in expression among the 34 identified alleles [18]. The fully functional allele (*1) is associated with normal CYP2C19 activity; individuals’ homozygous for this allele are considered extensive metabolizers (EM). Individuals who carry two null alleles are considered poor metabolizers (PMs). The two most common non-functional (null) alleles are CYP2C19*2 and CYP2C19*3, which account for 95 % of individuals considered PMs [19]. Additional null alleles include CYP2C19*4, CYP2C19*5, CYP2C19*6, and CYP2C19*8 [15, 20]. Approximately, 3–5 % of Caucasians, 12–23 % of Asians, 7 % of African Americans, and 0.9 % of Hispanics are CYP2C19 PMs, indicating that they encode non-functioning enzymes [21–24]. Conversely, intermediate metabolizers carry one null and one wild-type allele (i.e., CYP2C19*1/*3).
An allelic variant associated with increased CYP2C19 expression (CYP2C19*17) and catalytic activity has also been identified [25]. Individuals possessing this allelic variant are considered ultra-rapid metabolizers (URM) [17]. CYP2C19*17 is a relatively common allele in Europeans and Africans (18–27 and 10–26 % frequencies, respectively), yet it occurs infrequently in Asians (0.15–0.44 % prevalence) [17].
Voriconazole Concentrations and Efficacy/Toxicity
Voriconazole exhibits a narrow therapeutic index, non-linear pharmacokinetics, marked genotypic variability in CYP2C19 metabolizer status, and a high propensity for drug-drug interactions [5, 26]. Consequently, a fixed dose of voriconazole yields a myriad of plasma concentrations [27–29], which do not necessarily predict future concentrations even in the same individual [30, 31]. Voriconazole is also commonly used for fungal infections such as invasive aspergillosis that are associated with significant mortality among susceptible hosts. These factors underscore the need for voriconazole TDM. Indeed, the majority of studies that explore the impact of voriconazole TDM on efficacy and safety have found it to be beneficial. However, most of these studies are observational, with only one being a randomized, assessor-blinded, controlled trial [32•]. Furthermore, voriconazole TDM studies exhibit marked heterogeneity in quality and design, including assay techniques, voriconazole sampling methodology [29, 32•, 33], and target concentration ranges, all of which pose difficulties when comparing results across studies. Nonetheless, the IDSA guidelines support the use of voriconazole TDM [3].
Studies examining the role of voriconazole TDM have used a variety of voriconazole-exposure metrics. Most of the early studies reported random blood sampling. Voriconazole efficacy has been shown to correlate well in vivo with the AUC/MIC [34, 35] or mean unbound voriconazole concentration/MIC ratio [36]. However, these measurements entail repeated sampling and are difficult to perform in the clinical setting. Assessment of the trough/MIC ratio is a less robust, but more clinically achievable approach, which was found to predict clinical response in a 5000-patient Monte Carlo simulation using data from multiple phase 2 and phase 3 clinical trials [36].
The optimal target concentration range for voriconazole is not clearly defined. The suggested lower end cut-off for efficacy has ranged widely between 0.25 mcg/mL [33] and 2.51 mcg/mL [37]. Most initial studies used a voriconazole concentration >1 mcg/mL as the lower cut-off on the basis of in vitro studies that reported voriconazole MICs between 0.5 and 1 mcg/mL for most Aspergillus spp. and Candida spp. [38, 39]. However, data now suggest a voriconazole concentration of 2 mcg/mL may be a more appropriate lower-end threshold concentration [40–42]. Because the unbound circulating fraction (40–50 %) of voriconazole is microbiologically active [29], such a recommendation seems pharmacologically plausible. Suggested upper-end threshold concentrations for voriconazole range from 4 to 7 mcg/mL and are based on concentrations above which toxicities were observed across studies. Studies reporting relationships among voriconazole concentrations and efficacy and toxicity are summarized in Table 1 and discussed in detail below [29, 31, 32•, 33, 36, 43, 44•, 45•, 46–50].
Voriconazole TDM and Efficacy
The only clinical trial investigating the impact of voriconazole TDM on the incidence of adverse drug events and treatment response was a 1:1 randomized, single-center study from South Korea. In this study, voriconazole dosage was adjusted using pre-specified algorithms based on trough voriconazole concentrations drawn on day 4 of therapy in the intervention group (55 of 110 patients) in which the targeted range was 1 to 5.5 mcg/mL [32•]. The control group received standard voriconazole dosing during the study. Although the incidence of adverse drug events did not differ significantly between groups (p = 0.97), the likelihood of voriconazole discontinuation due to adverse effects was fourfold higher among controls compared to the intervention group (p = 0.02). With the availability of voriconazole trough levels to guide dose adjustments, providers tended to continue voriconazole longer in the TDM arm despite the occurrence of a similar number of adverse events. Importantly, TDM was associated with a higher clinical response rate compared to no TDM (81 vs. 59 %, p = 0.04).
Several observational studies have also evaluated the role of voriconazole TDM (Table 1); the largest of which involved a secondary analysis of 825 subjects with yeast or mold infections from nine phase 2 and phase 3 clinical trials. At a mean plasma concentration (Cavg) <0.5 mcg/mL, the voriconazole response rate was 57 % compared to 74 % when Cavg was between 0.5 and 5 mcg/mL. Moreover, a non-linear relationship between Cavg and clinical response was determined by logistic regression (p < 0.003) [36]. Higher responses were seen with primary rather than salvage therapy, and with yeast rather than mold infections, and specifically within these groups with Candida spp. rather than Aspergillus spp. Although informative, this study combined patients and pathogens with widely different exposure-response relationships, making it difficult to extrapolate these results to other patient populations.
In a study of voriconazole TDM during 2388 treatment days in 52 patients at a single center, investigators found that trough concentrations >1 mcg/mL yielded a higher response rate (88 %) compared to troughs ≤1 mcg/mL (54 %; p = 0.02) [29]. The authors did not find a relationship between voriconazole dose and trough concentration, but did observe that trough concentrations were a significant predictor of clinical response (probability 0.7 at a trough of 1 mcg/mL). In a population pharmacokinetic analysis from 505 plasma concentration values from another 55 patients, the same authors reproduced this concentration-response relationship [44•]. In this study, plasma concentrations ranging from 1.5 to 4.5 mcg/mL were associated with a probability of response greater than 85 %. The relationship was statistically significant only when voriconazole was administered orally (p < 0.001), supporting variability in oral bioavailability as a major determinant of subtherapeutic voriconazole levels.
Similar findings have been observed in several multicenter studies. In an open-label study involving 201 adult patients, voriconazole trough concentrations were significantly lower (median 0.9 mcg/mL) in patients who failed treatment compared to those who responded (median 2.1 mcg/mL; p < 0.05) [45•]. Among those patients with proven or probable invasive fungal infections and voriconazole trough concentrations <1.7 mcg/mL, the treatment failure rate was 35 %, compared to a 6 % failure rate in patients with voriconazole concentrations ≥1.7 mcg/mL. In another multicenter study of 116 assessable patients with invasive aspergillosis, 3 out of 5 patients with voriconazole trough concentrations <0.25 mcg/mL failed to demonstrate any sustained meaningful treatment response, which underscores the importance of knowing when trough voriconazole concentrations are exceedingly low (<0.25 mcg/mL) [33]. Several others have found voriconazole TDM to beneficially influence treatment efficacy in studies involving relatively few patients (N < 50) [40, 51, 52].
In children 2 to 11 years old administered standard adult dosages (3 to 4 mg/kg every 12 h), voriconazole demonstrates linear pharmacokinetics, which has been attributed to higher first-pass metabolism and systemic metabolic rates in the pediatric population [53–55]. However, at the recommended dosage for ages 2 to 12 (7 to 8 mg/kg every 12 h), non-linear pharmacokinetics, as seen in adults, are observed [55, 56]. The inability to reach adequate levels at standard adult doses (especially in critically ill children [57]) and the variability in trough concentrations at recommended doses, suggests voriconazole TDM may also be helpful in children. Three pediatric studies using voriconazole target trough concentrations ≥1 mcg/mL demonstrated a relationship between voriconazole concentrations and efficacy [58–60].
Fewer studies have explored the usefulness of voriconazole TDM in the prophylactic setting (i.e., to reduce breakthrough fungal infections) [61–64]. Among 93 lung-transplant recipients receiving prophylactic voriconazole, absence of any trough values >1.5 mcg/mL was associated with a significantly greater number of respiratory cultures growing fungal species (p = 0.01) [61]. Notably, some of the positive cultures represented colonization, and the value of preventing fungal colonization remains unclear. A similar study in allogeneic hematopoietic stem cell transplant recipients with hematologic malignancies reported six cases of breakthrough candidiasis among 43 patients with voriconazole trough concentrations ≤2 mcg/mL and no cases among the 24 patients with concentrations >2 mcg/mL (p = 0.061) [62]. Both of these studies saw four breakthrough infections each with molds [61, 62]. Another study in immunocompromised patients failed to show any relationship between TDM of prophylactic voriconazole and efficacy, but involved cases with both prophylactic and therapeutic indications for voriconazole [63]. Current evidence is insufficient to recommend voriconazole target concentrations to ensure adequate prophylaxis.
Some studies failed to demonstrate a relationship between voriconazole monitoring and efficacy [31, 41, 46, 65]. In these studies, the number of cases included in the efficacy analysis was low (maximum 53 cases). In one of the studies [41], the trough-efficacy correlation became statistically significant after excluding patients with refractory hematological conditions from the analysis. Another study [46] found a relationship between trough concentrations and efficacy 6 but not 12 weeks after commencing therapy. A meta-analysis of 12 studies was performed to investigate the optimal blood concentration range of voriconazole [43]. Analysis of the extracted data on voriconazole concentrations as a continuous variable from 3 of the 12 studies [41, 66, 67], and its relationship with efficacy, suggested that the distribution of voriconazole plasma concentrations did not differ significantly between treatment success and failure [weighted mean difference 1.95 (−2.18 to 1.84); p = 0.35]. The addition of one study [29] and dichotomous treatment of extracted data using graded cut-off values between 1 and 3 mcg/mL, demonstrated that a trough of 1 mcg/mL (including a subset analysis limited to cases of invasive aspergillosis), discriminated between treatment success and failure [OR 7.23 (2.84 to 18.37); p < 0.0001]. However, the limited number of studies actually analyzed as well as small sample sizes and observational nature, preclude strong conclusions about the drug concentration-efficacy relationship. Notwithstanding these underpowered studies, the majority of studies show a positive benefit of voriconazole TDM on efficacy.
Voriconazole TDM and Safety
Voriconazole can produce a variety of adverse effects that vary in severity. Hepatotoxicity, visual disturbances, visual hallucinations, and other neurologic disorders have been directly correlated with plasma concentrations of voriconazole (Table 1). A pooled PK/PD analysis of ten phase 2 and phase 3 clinical studies suggested a relationship between voriconazole concentrations and visual disturbances, which occurred in 16 % of patients when plasma voriconazole concentrations were <1 mcg/mL, and rose to 28 % at >9 mcg/mL [47]. Despite this relationship, the usefulness of TDM for this application is limited because voriconazole-associated visual disturbances are typically mild, reversible, and generally do not result in discontinuation of therapy [68]. Other neurological adverse effects including visual hallucinations and less commonly encephalopathy may be more debilitating. Their relationship to voriconazole concentrations has been studied as well, with almost all of these studies reporting a statistically significant positive correlation [29, 43, 44•, 45•, 48, 50, 69].
The association between plasma voriconazole concentrations and hepatotoxicity has been extensively investigated [29, 33, 41, 43, 44•, 45•, 46, 47, 49, 50, 70, 71]. Investigators reported that 6 of 22 patients with voriconazole concentrations >6 mcg/mL developed liver function test abnormalities, resulting in 1 death [33]. Based on these and other data, TDM was suggested to avoid voriconazole hepatotoxicity [71, 72], but this has not been unanimously accepted [73]. In the largest PK/PD analysis of voriconazole hepatotoxicity, investigators [47] reported a statistically significant relationship between voriconazole concentrations and risk of aspartate transaminase, alkaline phosphatase, and bilirubin elevation (p < 0.001), but this relationship was not observed for alanine transaminase (p = 0.17). More importantly, receiver-operator characteristic curves denoted poor prediction of any liver function tests abnormalities across a range of voriconazole concentrations [47]. One study has suggested that sustained elevated voriconazole concentrations might be associated with an increased risk of hepatotoxicity [49]. Nonetheless, the absolute incidence of hepatotoxicity with voriconazole use remains low and is comparable to that of other antifungal agents [74]. Thus, there is no universally acceptable concentration threshold, above which voriconazole-related hepatotoxicity is known to occur.
When used in the prophylactic setting, voriconazole toxicity must be weighed against its ability to reduce breakthrough invasive fungal infections. A study evaluating the role of voriconazole in preventing invasive fungal infections among lung transplant recipients demonstrated that toxicities were significant enough to warrant drug discontinuation in 27 % (25/93) of cases [61]. The usefulness of voriconazole TDM in the prophylactic setting requires further study.
Voriconazole Pharmacokinetics and CYP2C19 Polymorphisms
Studies in Healthy Volunteers
A study in healthy volunteers receiving voriconazole 200 or 300 mg po BID × 10 days found that voriconazole Cmax and AUC were increased in CYP2C19 PMs compared to EMs [75]. The impact of CYP2C19 genetic variants on voriconazole pharmacokinetics has been confirmed and characterized in a number studies in adult healthy volunteers (Table 2) [7, 8•, 76–80]. Pharmacokinetic parameters including half-life (t1/2) and AUC are significantly increased in CYP2C19 PM compared to CYP2C19 EM receiving oral voriconazole. In single-dose studies, the voriconazole t1/2 has ranged from 8.7 to 15.2 h in PM and 3.3 to 8.1 h in EM [7, 76, 77, 79, 80]. In a multiple-dose study, the voriconazole AUC0-T geometric mean ratio of PM to EM was 3.3 [8•]. This increase is consistent with the results of several single-dose studies, which determined that the voriconazole AUC0-∞ was 2.8 to 4.1 times higher in PM compared to EM [7, 8•, 76–80]. In single oral dose studies, significant reductions in voriconazole clearance have been observed in PM versus EM [7, 76–80]. A multiple-dose study reported that the voriconazole apparent oral clearance (Cl/F) decreased from 210 to 58.3 mL/min in EM compared to PM [8•]. However, changes in clearance in this trial were not subjected to statistical evaluation.
Alternations in voriconazole pharmacokinetics in CYP2C19 genetic variants has also been observed with intravenous voriconazole [8•, 78]. After a single dose (voriconazole 200 mg i.v.), the AUC0-∞ geometric mean ratio of PM to EM was 3.23 in healthy volunteers [8•]. In another single-dose study (voriconazole 400 mg i.v.), the AUC0-∞ was significantly increased and clearance significantly decreased in PM compared to EM [78]. However, in this study 6 out of 8 patients initially categorized as EM were later found to possess the CYP2C19*1/*17 genotype.
Two studies have produced conflicting data on the effect of the CYP2C19*17 allele on voriconazole pharmacokinetics [7, 77]. Unfortunately, only volunteers who were heterozygous for the CYP2C19*17 allele (CYP2C19*1/*17) and not homozygous (CYP2C19*17/*17) were enrolled in these trials. One study of healthy volunteers receiving a single oral voriconazole dose (200 mg) demonstrated a significant increase in apparent Cl/F and a decrease in AUC0-∞ in EM (CYPC19*1/*1) compared to URM (CYP2C19*1/*17) [77]. In contrast, an analysis of the placebo groups from two drug interaction studies reported no statistical differences for AUC0-∞, apparent Cl/F, or t1/2 when comparing EM (CYPC19*1/*1) to URM (CYP2C19*1/*17, CYP2C19*2/*17) [7]. Based on the results of these trials, it was proposed that the CYP2C19*17 allele may possibly lead to subtherapeutic voriconazole concentrations [81].
Studies in Patients
In contrast to the mostly positive results reported in healthy volunteers, studies on the impact of CYP2C19 genetic variants on voriconazole concentrations in patients have demonstrated conflicting results (Table 3). While retrospective studies have indicated an association between CYP2C19 genotype and voriconazole concentrations [83, 85, 87, 88], several prospective studies have reported no association [50, 84]. For example, a retrospective study in adults reported a minimum observed concentration (Cmin) of 3.67 mg/L and 1.98 mg/L in PM and EM, respectively (p < 0.05) [87]. However, in a prospective observational trial in adult Korean patients, median trough concentrations were not significantly different in EM and PM (2.12 and 2.75 mg/L, respectively, p = 0.859) [84].
The different results in patients compared to healthy volunteers may be due to confounding factors present in patients such as drug interactions, comorbidities, and organ dysfunction [89]. Additionally, the CYP2C19 genotype does not appear to account for all of the intrinsic variability in voriconazole pharmacokinetics between individuals. An analysis of placebo groups from two healthy volunteer studies revealed that the CYP2C19 genotype explained 49 and 39 % of variability in voriconazole apparent Cl/F and AUC0-∞, respectively [7]. Similarly, in a retrospective review of cystic fibrosis lung transplant recipients, the CYP2C19 genotype only explained 38 % of variability in voriconazole maintenance dose [83].
Several studies indicate that the CYP2C19*17 allele may lead to subtherapeutic voriconazole concentrations [82, 83, 85]. In cystic fibrosis lung transplant recipients, the proportion of below range concentrations was 37.9 and 15.6 % in CYP2C19*17 and CYP2C19*1 groups, respectively (p < 0.01) [83]. In a retrospective study, immunocompromised patients with cancer possessing the CYP2C19*17/*17 genotype had lower median dose-normalized trough concentrations than those with the CYP2C19*1/*1 genotype [88]. In that study, all of the patients with the CYP2C19*17/*17 genotype (N = 4) failed to achieve therapeutic voriconazole concentrations. Furthermore, in a retrospective study of patients with voriconazole levels ≤0.2 mcg/mL and excluding those receiving enzyme inducers, allogeneic stem cell transplant or liver transplant patients, inadequate dosing, or timing of levels, the CYP2C19*1/*17 or CYPC219*17/*17 genotypes were found in 8 out of 10 patients (80 %) [90]. In complicated dosing settings such as obesity genetic screening may also be informative and clinically helpful. For example, sustained elevations in voriconazole serum concentrations in an obese patient despite appropriate adjusted weight-based dosing were attributed to a CYP2C19 homozygous PM genotype (CYP2C19*2/*2) [91].
Several studies have described voriconazole pharmacokinetics in immunocompromised pediatric patients with CYP2C19 polymorphisms [89, 92]. When comparing pediatric PMs to EMs, the increase in voriconazole AUC was consistent with the results observed in adults [89, 92]. However, the genotypic variability observed in these patients precluded statistical analysis.
Other important issues related to the CYP2C19 genotype include the association between genotype and efficacy or toxicity and CYP2C19 genotype-guided dosing of voriconazole. Clinical studies have reported that the CYP2C19 genotype is not associated with the efficacy or toxicity of voriconazole (Table 3). Investigators found no significant difference among CYP2C19 genotypes in treatment response, all-cause, and invasive aspergillus mortality [86•]. The authors concluded that with therapeutic drug monitoring, an association was not observed between CYP2C19 genotype and voriconazole efficacy. Multiple studies have failed to find an association between CYP2C19 genotype and adverse effects [70, 82–84, 86•] including hepatotoxicity [70, 82]. Nonetheless, several investigators have proposed voriconazole dosing based on CYP2C19 genotype. Matsumoto et al. recommended an initial voriconazole dose of 7.2 to 8.9 mg/kg/day and 4.4 to 6.5 mg/kg/day in CYP2C19 wild type and CYP2C19 non-wild type, respectively, in Japanese patients [70]. Wang et al. suggested a voriconazole dose of 200 mg orally or intravenously twice daily in PM and voriconazole 300 mg orally twice daily or 200 mg intravenously twice daily in non-PM [87]. However, to our knowledge, a strategy of prospective CYP2C19 genotyping to select an initial voriconazole dose has not been validated prospectively.
Discussion/Conclusion
In this review, we describe the evidence supporting the use of voriconazole TDM and the role of CYP2C19 genotyping for voriconazole dosing. The impact of voriconazole TDM on safety and efficacy is still not entirely clear. Most evidence to date was acquired retrospectively in the absence of a non-TDM comparison group and with discretionary post-concentration dosage adjustments. The cost associated with voriconazole TDM is the only identifiable barrier to its routine use. The only randomized controlled trial that assessed the role of voriconazole TDM was from a single center and underpowered to detect differences in their primary outcome of adverse events [32•]. High-volume multicenter randomized controlled trials in this area are currently not available to support definitive guidelines. Until then, we support routine voriconazole TDM given substantial retrospective and prospective observational data supporting its benefit in regards to efficacy, avoidance of neurotoxicity, and minimizing discontinuation of therapy.
While a significant relationship exists in healthy volunteers between CYP2C19 genotype and voriconazole pharmacokinetics, including AUC, Cl/F, and t1/2, this association is markedly less apparent in actual patients. Studies also indicate that CYP2C19 genotype is not related to the efficacy or toxicity of voriconazole. Additional studies are needed before routine CYP2C19 genotyping is performed to facilitate initial dose selection of voriconazole. Finally, there is no validated model that allows for an accurate initial dosage of voriconazole based upon CYP2C19 allelic profile. While CYP2C19 genotype data may explain variability of voriconazole serum levels, they alone are not sufficient to guide initial dosing. This is in agreement with several reviews that state further research is needed before the widespread implementation of clinical voriconazole pharmacogenomics [12•, 14, 93, 94].
The logistics of timeliness of data from TDM and genotyping remain a continued challenge to patient care. While the “turn around” time for TDM data has improved in both reference laboratories and in hospital laboratories, availability of genotyping data remains difficult. Genotyping data are typically not available for patients as a guide to initial dosing in patients receiving voriconazole therapy.
If the current data are insufficient to recommend CYP2C19 genotyping for all patients, when should it be performed? We feel that institutional resources should first be used to implement voriconazole TDM with a reasonable turnaround time. Once voriconazole TDM is implemented, CYP2C19 genotyping, if available, may be a useful adjunct to assist in characterizing the voriconazole disposition of select patients with particularly unpredictable concentrations and a clinical need for aggressive treatment. As a reminder, alternative specimens than blood are needed for CYP2C19 genotyping in allogeneic stem cell or liver transplantation patients and those who have recently received heterologous blood transfusions [95]. We also note that genotyping may be useful in specific clinical situations such as dosing of voriconazole in critically ill patients (especially for patients from ethnicities associated with high rates of PM status such as Asians), in patients on multiple interacting medications, in obese patients receiving intravenous voriconazole, and in selected pediatric patients in whom therapeutic levels are difficult to obtain. In patients receiving initial doses of voriconazole above manufacturer recommendations, CYP2C19 genotyping may be helpful to identify PMs and thereby prevent excessive levels and toxicity. Furthermore, the presence of the CYP2C19*17 allele in critically ill patients may lead to the decision to administer combination antifungal therapy until therapeutic levels of voriconazole are achieved. Knowledge of the CYP2C19 genotype may also aid in the management of voriconazole vincristine drug interactions. In PMs, the half-life of voriconazole may be prolonged, requiring the drug to be held longer than 24 to 48 h before starting vincristine to avoid this serious drug interaction [96, 97]. Similar recommendations were recently made by others assessing of the role of pharmacogenomic screening of patients with hematological malignancies [14].
In conclusion, CYP2C19 genotyping to aid voriconazole dosing is an appealing concept, but further studies are needed before this practice is widely implemented into routine clinical care.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Product information. Vfend (voriconazole). New York: Pfizer; 2014.
Walsh TJ, Anaissie EJ, Denning DW, et al. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin Infect Dis. 2008;46:327–60.
Pappas PG, Kauffman CA, Andes D, et al. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:503–35.
Theuretzbacher U, Ihle F, Derendorf H. Pharmacokinetic/pharmacodynamic profile of voriconazole. Clin Pharmacokinet. 2006;45:649–63.
Andes D, Pascual A, Marchetti O. Antifungal therapeutic drug monitoring: established and emerging indications. Antimicrob Agents Chemother. 2009;53:24–34.
Geist MJ, Egerer G, Burhenne J, Mikus G. Safety of voriconazole in a patient with CYP2C9*2/CYP2C9*2 genotype. Antimicrob Agents Chemother. 2006;50:3227–8.
Weiss J, Ten Hoevel MM, Burhenne J, et al. CYP2C19 genotype is a major factor contributing to the highly variable pharmacokinetics of voriconazole. J Clin Pharmacol. 2009;49:196–204.
Lee S, Kim BH, Nam WS, et al. Effect of CYP2C19 polymorphism on the pharmacokinetics of voriconazole after single and multiple doses in healthy volunteers. J Clin Pharmacol. 2012;52:195–203. A healthy volunteer study in adults that characterized the pharmacokinetics of single (oral and intravenous) and multiple dose (oral) voriconazole in patients with CYP2C19 polymorphisms.
Purkins L, Wood N, Ghahramani P, Greenhalgh K, Allen MJ, Kleinermans D. Pharmacokinetics and safety of voriconazole following intravenous- to oral-dose escalation regimens. Antimicrob Agents Chemother. 2002;46:2546–53.
Wang L, McLeod HL, Weinshilboum RM. Genomics and drug response. N Engl J Med. 2011;364:1144–53.
Evans WE, McLeod HL. Pharmacogenomics—drug disposition, drug targets, and side effects. N Engl J Med. 2003;348:538–49.
Owusu Obeng A, Egelund EF, Alsultan A, Peloquin CA, Johnson JA. CYP2C19 polymorphisms and therapeutic drug monitoring of voriconazole: are we ready for clinical implementation of pharmacogenomics? Pharmacotherapy. 2014;34:703–18. A recent and extensive review describing the pharmacogenomics of voriconazole.
http://www.pharmgkb.org/drug/PA10233#tabview=tab0&subtab=31. Accessed 4 Feb 2015.
Chau MM, Kong DC, van Hal SJ, et al. Consensus guidelines for optimizing antifungal drug delivery and monitoring to avoid toxicity and improve outcomes in patients with haematological malignancy. Intern Med J. 2014;44:1364–88.
Desta Z, Zhao X, Shin JG, Flockhart DA. Clinical significance of the cytochrome P450 2C19 genetic polymorphism. Clin Pharmacokinet. 2002;41:913–58.
Ingelman-Sundberg M. Pharmacogenetics of cytochrome P450 and its applications in drug therapy: the past, present and future. Trends Pharmacol Sci. 2004;25:193–200.
Hirota T, Eguchi S, Ieri I. Impact of genetic polymorphisms in CYP2C9 and CYP2C19 on the pharmacokinetics of clinically used drugs. Drug Metab Pharmacokinet. 2013;28:28–37.
http://www.cypalleles.ki.se/cyp2c19.htm. Accessed 10 Jan 2015.
Frye RF. In: McLeod HL, DeVane CL, Haga SB, editors. Pharmacogenetics of oxidative drug metabolism and its clinical applications in pharmacogenomics: applications to patient care. Lenexa: American College of Clinical Pharmacy; 2009. p. 32–53.
Bertisson L. Geographical/interracial differences in polymorphic drug oxidation. Current state of knowledge of cytochromes P450 (CYP) 2D6 and 2C19. Clin Pharmacokinet. 1995;29:192–209.
Scott SA, Sangkuhl K, Stein CM, et al. Clinical Pharmacogenetics Implementation Consortium guidelines for CYP2C19 genotype and clopidogrel therapy: 2013 update. Clin Pharmacol Ther. 2013;94:317–23.
Strom CM, Goos D, Crossley B, et al. Testing for variants in CYP2C19: population frequencies and testing experience in a clinical laboratory. Genet Med. 2012;14:95–100.
Sugimoto K, Uno T, Yamazaki H, Tateishi T. Limited frequency of the CYP2C19*17 allele and its minor role in a Japanese population. Br J Clin Pharmacol. 2008;65:437–9.
Andes D, Lepak A. Editorial commentary: antifungal therapeutic drug monitoring progress: getting it right the first time. Clin Infect Dis. 2012;55:391–3.
Sim SC, Risinger C, Dahl ML, et al. A common novel CYP2C19 gene variant causes ultrarapid drug metabolism relevant for the drug response to proton pump inhibitors and antidepressants. Clin Pharmacol Ther. 2006;79:103–13.
Johnston A. The pharmacokinetics of voriconazole. Br J Clin Pharmacol. 2003;56 Suppl 1:1.
Trifilio S, Pennick G, Pi J, et al. Monitoring plasma voriconazole levels may be necessary to avoid subtherapeutic levels in hematopoietic stem cell transplant recipients. Cancer. 2007;109:1532–5.
Bruggemann RJ, Donnelly JP, Aarnoutse RE, et al. Therapeutic drug monitoring of voriconazole. Ther Drug Monit. 2008;30:403–11.
Pascual A, Calandra T, Bolay S, Buclin T, Bille J, Marchetti O. Voriconazole therapeutic drug monitoring in patients with invasive mycoses improves efficacy and safety outcomes. Clin Infect Dis. 2008;46:201–11.
Trifilio SM, Yarnold PR, Scheetz MH, Pi J, Pennick G, Mehta J. Serial plasma voriconazole concentrations after allogeneic hematopoietic stem cell transplantation. Antimicrob Agents Chemother. 2009;53:1793–6.
Racil Z, Winterova J, Kouba M, et al. Monitoring trough voriconazole plasma concentrations in haematological patients: real life multicentre experience. Mycoses. 2012;55:483–92.
Park WB, Kim NH, Kim KH, et al. The effect of therapeutic drug monitoring on safety and efficacy of voriconazole in invasive fungal infections: a randomized controlled trial. Clin Infect Dis. 2012;55:1080–7. Randomized, assessor-blinded, controlled, single center trial evaluating clinical utility of therapeutic drug monitoring for voriconazole in invasive fungal infections found reduced drug discontinuation due to adverse events and improved treatment response.
Denning DW, Ribaud P, Milpied N, et al. Efficacy and safety of voriconazole in the treatment of acute invasive aspergillosis. Clin Infect Dis. 2002;34:563–71.
Goodwin ML, Drew RH. Antifungal serum concentration monitoring: an update. J Antimicrob Chemother. 2008;61:17–25.
Andes D, Marchillo K, Stamstad T, Conklin R. In vivo pharmacokinetics and pharmacodynamics of a new triazole, voriconazole, in a murine candidiasis model. Antimicrob Agents Chemother. 2003;47:3165–9.
Troke PF, Hockey HP, Hope WW. Observational study of the clinical efficacy of voriconazole and its relationship to plasma concentrations in patients. Antimicrob Agents Chemother. 2011;55:4782–8.
Howard A, Hoffman J, Sheth A. Clinical application of voriconazole concentrations in the treatment of invasive aspergillosis. Ann Pharmacother. 2008;42:1859–64.
Johnson LB, Kauffman CA. Voriconazole: a new triazole antifungal agent. Clin Infect Dis. 2003;36:630–7.
Pfaller MA, Diekema DJ, Rex JH, et al. Correlation of MIC with outcome for Candida species tested against voriconazole: analysis and proposal for interpretive breakpoints. J Clin Microbiol. 2006;44:819–26.
Smith J, Safdar N, Knasinski V, et al. Voriconazole therapeutic drug monitoring. Antimicrob Agents Chemother. 2006;50:1570–2.
Ueda K, Nannya Y, Kumano K, et al. Monitoring trough concentration of voriconazole is important to ensure successful antifungal therapy and to avoid hepatic damage in patients with hematological disorders. Int J Hematol. 2009;89:592–9.
Davies-Vorbrodt S, Ito JI, Tegtmeier BR, Dadwal SS, Kriengkauykiat J. Voriconazole serum concentrations in obese and overweight immunocompromised patients: a retrospective review. Pharmacotherapy. 2013;33:22–30.
Hamada Y, Seto Y, Yago K, Kuroyama M. Investigation and threshold of optimum blood concentration of voriconazole: a descriptive statistical meta-analysis. J Infect Chemother. 2012;18:501–7.
Pascual A, Csajka C, Buclin T, et al. Challenging recommended oral and intravenous voriconazole doses for improved efficacy and safety: population pharmacokinetics-based analysis of adult patients with invasive fungal infections. Clin Infect Dis. 2012;55:381–90. A population-pharmacokinetics analysis involving 55 patients with invasive mycoses suggested that a therapeutic range for voriconazole plasma concentrations between 1.5 and 4.5 mg/L provided a >85% probability of response and <15% probability of neurotoxicity.
Dolton MJ, Ray JE, Chen SC, Ng K, Pont LG, McLachlan AJ. Multicenter study of voriconazole pharmacokinetics and therapeutic drug monitoring. Antimicrob Agents Chemother. 2012;56:4793–9. In a multicenter retrospective study of the relationships between voriconazole concentrations and clinical outcomes and adverse events in 201 patients, treatment success was significantly greater at voriconazole concentrations ≥1.7 mcg/mL (p < 0.01) and neurotoxicity occurred more frequently at concentrations >5 mcg/mL (p < 0.01).
Chu HY, Jain R, Xie H, Pottinger P, Fredricks DN. Voriconazole therapeutic drug monitoring: retrospective cohort study of the relationship to clinical outcomes and adverse events. BMC Infect Dis. 2013;13:105.
Tan K, Brayshaw N, Tomaszewski K, Troke P, Wood N. Investigation of the potential relationships between plasma voriconazole concentrations and visual adverse events or liver function test abnormalities. J Clin Pharmacol. 2006;46:235–43.
Imhof A, Schaer DJ, Schanz U, Schwarz U. Neurological adverse events to voriconazole: evidence for therapeutic drug monitoring. Swiss Med Wkly. 2006;136:739–42.
Suzuki Y, Tokimatsu I, Sato Y, et al. Association of sustained high plasma trough concentration of voriconazole with the incidence of hepatotoxicity. Clin Chim Acta. 2013;424:119–22.
Zonios D, Yamazaki H, Murayama N, et al. Voriconazole metabolism, toxicity, and the effect of cytochrome P450 2C19 genotype. J Infect Dis. 2014;209:1941–8.
Miyakis S, van Hal SJ, Ray J, Marriott D. Voriconazole concentrations and outcome of invasive fungal infections. Clin Microbiol Infect. 2010;16:927–33.
Gomez-Lopez A, Cendejas-Bueno E, Cuesta I, et al. Voriconazole serum levels measured by high-performance liquid chromatography: a monocentric study in treated patients. Med Mycol. 2012;50:439–45.
Walsh TJ, Karlsson MO, Driscoll T, et al. Pharmacokinetics and safety of intravenous voriconazole in children after single- or multiple-dose administration. Antimicrob Agents Chemother. 2004;48:2166–72.
Chen J, Chan C, Colantonio D, Seto W. Therapeutic drug monitoring of voriconazole in children. Ther Drug Monit. 2012;34:77–84.
Karlsson MO, Lutsar I, Milligan PA. Population pharmacokinetic analysis of voriconazole plasma concentration data from pediatric studies. Antimicrob Agents Chemother. 2009;53:935–44.
Walsh TJ, Driscoll T, Milligan PA, et al. Pharmacokinetics, safety, and tolerability of voriconazole in immunocompromised children. Antimicrob Agents Chemother. 2010;54:4116–23.
Alffenaar JW, Doedens RA, Groninger E, Kosterink JG. High-dose voriconazole in a critically ill pediatric patient with neuroblastoma. Pediatr Infect Dis J. 2008;27:189–90.
Neely M, Rushing T, Kovacs A, Jelliffe R, Hoffman J. Voriconazole pharmacokinetics and pharmacodynamics in children. Clin Infect Dis. 2010;50:27–36.
Choi SH, Lee SY, Hwang JY, et al. Importance of voriconazole therapeutic drug monitoring in pediatric cancer patients with invasive aspergillosis. Pediatr Blood Cancer. 2013;60:82–7.
Soler-Palacin P, Frick MA, Martin-Nalda A, et al. Voriconazole drug monitoring in the management of invasive fungal infection in immunocompromised children: a prospective study. J Antimicrob Chemother. 2012;67:700–6.
Mitsani D, Nguyen MH, Shields RK, et al. Prospective, observational study of voriconazole therapeutic drug monitoring among lung transplant recipients receiving prophylaxis: factors impacting levels of and associations between serum troughs, efficacy, and toxicity. Antimicrob Agents Chemother. 2012;56:2371–7.
Trifilio S, Singhal S, Williams S, et al. Breakthrough fungal infections after allogeneic hematopoietic stem cell transplantation in patients on prophylactic voriconazole. Bone Marrow Transplant. 2007;40:451–6.
Pieper S, Kolve H, Gumbinger HG, Goletz G, Wurthwein G, Groll AH. Monitoring of voriconazole plasma concentrations in immunocompromised paediatric patients. J Antimicrob Chemother. 2012;67:2717–24.
Barreto JN, Beach CL, Wolf RC, et al. The incidence of invasive fungal infections in neutropenic patients with acute leukemia and myelodysplastic syndromes receiving primary antifungal prophylaxis with voriconazole. Am J Hematol. 2013;88:283–8.
Lee YJ, Lee SO, Choi SH, et al. Initial voriconazole trough blood levels and clinical outcomes of invasive aspergillosis in patients with hematologic malignancies. Med Mycol. 2013;51:324–30.
Hagiwara E, Shiihara J, Matsushima A, et al. Usefulness of monitoring plasma voriconazole concentration in patients with chronic necrotizing pulmonary aspergillosis. Nihon Kokyuki Gakkai Zasshi. 2009;47:93–7.
Okuda T, Okuda A, Watanabe N, Takao M, Takayanagi K. Retrospective serological tests for determining the optimal blood concentration of voriconazole for treating fungal infection. Yakugaku Zasshi. 2008;128:1811–8.
Boucher HW, Groll AH, Chiou CC, Walsh TJ. Newer systemic antifungal agents: pharmacokinetics, safety and efficacy. Drugs. 2004;64:1997–2020.
Zonios DI, Gea-Banacloche J, Childs R, Bennett JE. Hallucinations during voriconazole therapy. Clin Infect Dis. 2008;47:e7–10.
Matsumoto K, Ikawa K, Abematsu K, et al. Correlation between voriconazole trough plasma concentration and hepatotoxicity in patients with different CYP2C19 genotypes. Int J Antimicrob Agents. 2009;34:91–4.
Trifilio S, Ortiz R, Pennick G, et al. Voriconazole therapeutic drug monitoring in allogeneic hematopoietic stem cell transplant recipients. Bone Marrow Transplant. 2005;35:509–13.
Potoski BA, Brown J. The safety of voriconazole. Clin Infect Dis. 2002;35:1273–5.
Lutsar I, Hodges MR, Tomaszewski K, Troke PF, Wood ND. Safety of voriconazole and dose individualization. Clin Infect Dis. 2003;36:1087–8.
Walsh TJ, Pappas P, Winston DJ, et al. Voriconazole compared with liposomal amphotericin B for empirical antifungal therapy in patients with neutropenia and persistent fever. N Engl J Med. 2002;346:225–34.
Ikeda Y, Umemura K, Kondo K, Sekiguchi K, Miyoshi S, Nakashima M. Pharmacokinetics of voriconazole and cytochrome P450 2C19 genetic status. Clin Pharmacol Ther. 2004;75:587–8.
Mikus G, Schöwel V, Drzewinska M, et al. Potent cytochrome P450 2C19 genotype-related interaction between voriconazole and the cytochrome P450 3A4 inhibitor ritonavir. Clin Pharmacol Ther. 2006;80:126–35.
Wang G, Lei HP, Li Z, et al. The CYP2C19 ultra-rapid metabolizer genotype influences the pharmacokinetics of voriconazole in healthy male volunteers. Eur J Clin Pharmacol. 2009;65:281–5.
Scholz I, Oberwittler H, Riedel KD, et al. Pharmacokinetics, metabolism and bioavailability of the triazole antifungal agent voriconazole in relation to CYP2C19 genotype. Br J Clin Pharmacol. 2009;68:906–15.
Shi HY, Yan J, Zhu WH, et al. Effects of erythromycin on voriconazole pharmacokinetics and association with CYP2C19 polymorphism. Eur J Clin Pharmacol. 2010;66:1131–6.
Lei HP, Wang G, Wang LS, et al. Lack of effect of Ginkgo biloba on voriconazole pharmacokinetics in Chinese volunteers identified as CYP2C19 poor and extensive metabolizers. Ann Pharmacother. 2009;43:726–31.
Dolton MJ, McLachlan AJ. Clinical importance of the CYP2C19*17 variant allele for voriconazole. Br J Clin Pharmacol. 2011;71:137–8.
Levin MD, den Hollander JG, van der Holt B, et al. Hepatotoxicity of oral and intravenous voriconazole in relation to cytochrome P450 polymorphisms. J Antimicrob Chemother. 2007;60:1104–7.
Berge M, Guillemain R, Trégouet DA, et al. Effect of cytochrome P450 2C19 genotype on voriconazole exposure in cystic fibrosis lung transplant patients. Eur J Clin Pharmacol. 2011;67:253–60.
Kim SH, Yim DS, Choi SM, et al. Voriconazole-related severe adverse events: clinical application of therapeutic drug monitoring in Korean patients. Int J Infect Dis. 2011;15:e753–8.
Narita A, Muramatsu H, Sakaguchi H, et al. Correlation of CYP2C19 phenotype with voriconazole plasma concentration in children. J Pediatr Hematol Oncol. 2013;35:e219–23.
Kim SH, Lee DG, Kwon JC, et al. Clinical impact of cytochrome P450 2C19 genotype on the treatment of invasive aspergillosis under routine therapeutic drug monitoring of voriconazole in a Korean population. Infect Chemother. 2013;45:406–14. A prospective observational study found with routine therapeutic drug monitoring there was no significant relationship between CYP2C19 genotype and outcome or toxicity with voriconazole in patients with invasive aspergillosis.
Wang T, Zhu H, Sun J, et al. Efficacy and safety of voriconazole and CYP2C19 polymorphism for optimised dosage regimens in patients with invasive fungal infections. Int J Antimicrob Agents. 2014;44:436–42.
Hicks JK, Crews KR, Flynn P, et al. Voriconazole plasma concentrations in immunocompromised pediatric patients vary by CYP2C19 diplotypes. Pharmacogenomics. 2014;15:1065–78.
Driscoll TA, Frangoul H, Nemecek ER, et al. Comparison of pharmacokinetics and safety of voriconazole intravenous-to-oral switch in immunocompromised adolescents and healthy adults. Antimicrob Agents Chemother. 2011;55:5780–9.
Hassan A, Burhenne J, Riedel KD, et al. Modulators of very low voriconazole concentrations in routine therapeutic drug monitoring. Ther Drug Monit. 2011;33:86–93.
Moriyama B, Jarosinski P, Figg WD, et al. Pharmacokinetics of intravenous voriconazole in obese patients: implications of CYP2C19 homozygous poor metabolizer genotype. Pharmacotherapy. 2013;33:e19–22.
Mori M, Kobayashi R, Kato K, et al. Pharmacokinetics and safety of voriconazole intravenous-to-oral switch regimens in immunocompromised japanese pediatric patients. Antimicrob Agents Chemother. 2015;59:1004–13.
Dolton MJ, McLachlan AJ. Optimizing azole antifungal therapy in the prophylaxis and treatment of fungal infections. Curr Opin Infect Dis. 2014;27:493–500.
Dolton MJ, McLachlan AJ. Voriconazole pharmacokinetics and exposure-response relationships: assessing the links between exposure, efficacy and toxicity. Int J Antimicrob Agents. 2014;44:183–93.
http://www.mayomedicallaboratories.com/test-catalog/Clinical+and+Interpretive/62996. Assessed 29 Jan 2015.
Moriyama B, Henning SA, Leung J, et al. Adverse interactions between antifungal azoles and vincristine: review and analysis of cases. Mycoses. 2012;55:290–7.
Moriyama B, Falade-Nwulia O, Leung J, et al. Prolonged half-life of voriconazole in a CYP2C19 homozygous poor metabolizer receiving vincristine chemotherapy: avoiding a serious adverse drug interaction. Mycoses. 2011;54:e877–9.
Acknowledgments
This work was supported in part by the intramural research program of the National Institutes of Health. The opinions expressed in this paper are the authors’ and do not reflect those of the National Institutes of Health (NIH) Clinical Center, NIH, Department of Health and Human Services, or the Federal government. Dr. Walsh is a Scholar of the Henry Schueler Foundation and a Scholar of Pediatric Infectious Diseases of the Sharpe Family Foundation. The assistance of Judith Welsh, NIH Library, Office of the Director for the library research is gratefully acknowledged.
Compliance With Ethics Guidelines
ᅟ
Conflict of Interest
Sameer Kadri, Stacey A. Henning, Robert L. Danner, and Scott R. Penzak declare that they have no conflict of interest.
Brad Moriyama owns a stock in Merck.
Thomas J. Walsh has received research grants from Novartis, Astellas, Merck, ContraFect, Pfizer, Cubist, Theravance, and consultancy fees from Vestagen, ICo Therapeutics, Inc., Trius, Sigma Tau, Astellas, and Drais Pharmaceuticals, ContraFect, Novartis, Pfizer, Methylgene, and Cubist.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pharmacology and Pharmacodynamics of Antifungal Agents
Rights and permissions
About this article
Cite this article
Moriyama, B., Kadri, S., Henning, S.A. et al. Therapeutic Drug Monitoring and Genotypic Screening in the Clinical Use of Voriconazole. Curr Fungal Infect Rep 9, 74–87 (2015). https://doi.org/10.1007/s12281-015-0219-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12281-015-0219-0