Abstract
Purpose
Biologic molecules constitute a major part of the therapeutics portfolio across the pipeline of several biotech and pharmaceutical companies. They have the advantage of being more target-specific, and recent progress in protein engineering has allowed product designs on various platforms that befit the therapeutic indication and allow differentiation from competitor molecules. They are fundamentally large proteins, with complex structural heterogeneity arising from production using recombinant gene technology in cell lines. These biotherapeutics run the risk of being recognized as foreign by the host immune system, eliciting both B and T cell responses. The impact ranges from none to benign infusion reactions to life-threatening anaphylaxis, and with evolving modalities for such molecules in the pipeline, it is critical to understand the interplay of various risk factors that modulate the immune response. During risk assessment and mitigation strategies in drug development, risk factors are broadly classified arising from patient and product-related origins, and this review will focus on the product-related risk factors.
Methods
A basic primer on immune mechanisms underlying immunogenicity to a biotherapeutic is provided to highlight those aspects that are influenced by product attributes; this is followed by a more focused discussion of relevant and recently published works pertaining to each critical product attribute and the in vitro and in vivo methodologies utilized to assess their risk.
Results
Some product-related factors have an influence on the product’s immunogenicity. This varies with the type of biotherapeutic product, the disease background, and the diversities seen in the subjects.
Conclusion
This article highlights some of the experimental limitations on risk evaluation of individual product attributes and emphasizes that immunogenicity manifesting as an undesirable clinical outcome results from the cumulative effect of several risk factors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
With evolving protein biotherapeutic platforms, newer multi-domain biotherapeutics, and the escalating investment of resources and technology toward the development of efficacious biologic drugs with minimal adverse effects, the phenomenon of immunogenicity has gained added relevance and has been extensively reviewed by several groups [1,2,3,4,5,6].
Several approved protein therapeutics in the market are immunogenic in terms of inducing unwanted immune responses upon exposure to the drug regardless of any other consequential changes in patients. The consequences have varied, ranging from no clinical sequelae to varying levels of impact on safety and efficacy as shown in Table 1. Adverse effects vary from infusion reactions, cytokine release syndrome, anaphylaxis, functional abrogation of endogenous molecules where there is a cross reactivity with the biotherapeutic molecule as seen with erythropoietin, and altered pharmacokinetics due to either faster clearance or enhanced half-life of the biotherapeutic and functional neutralization as seen with some anti-TNFα and recent anti-PCSK9 monoclonal antibody therapies; several of these studies have been reviewed extensively in the past [7, 9, 10, 12,13,14,15,16, 19,20,21]. These responses are affected by both product and patient-related variables, some of which are summarized in Table 2. While not all product-related factors influence immunogenicity, those that do play a role can be assessed individually during drug product development. However any correlation of a single factor with a defined clinical outcome is considerably difficult to establish and requires trials to be conducted with different batches of drug product and other risk-associated variables to be rigorously controlled. Ultimately the risk of a pro-immunogenic clinical outcome is determined by the interaction of key risk-associated variables in the in vivo space. The paradigm of risk mitigation still rests on controlling those few variables that can be modulated during drug development. These include a thorough understanding of the drug’s mechanism of action in the context of the disease background on how it modulates immune responses, adopting a certain set of critical product quality attributes (CQA) best practices around product development, rigorous implementation of validated sensitive drug-tolerant antidrug antibody analytical methods, judicious design and execution of dosing strategies, and patient safety-centric clinical protocols.
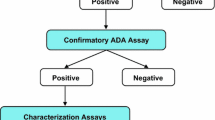
The presence of therapeutic-specific antidrug antibodies (ADA, also referred by others as anti-therapeutic antibodies) detectable in patient serum by validated assays is generally accepted by industry and health authorities as a measure of immunogenicity. The detection, reporting, and characterization of the ADA are done in a tiered manner after careful consideration of immunogenic risk factors [23,24,25]. Most adverse events subsequent to ADA formation such as pharmacological effects, impact on biotherapeutic exposure, or hypersensitivity reactions can be explained as a consequence of immune complexes between ADA and the biotherapeutic protein [22]. The emerging diversity in biotherapeutic platforms has given rise to a variety of therapeutics either made of proteins that include enzyme replacement therapy, monoclonal antibody (mAb) therapeutics, engineered recombinant proteins and their derivatives, fragment crystallizable region (Fc) linked proteins or nucleic acids, lipid nanoparticles, and living cells that include CAR-T cell therapies. Some of these therapeutics are multimodality agents that target more than one epitope of functional consequence. Regardless of the underlying platform technology, these agents can elicit an in vivo immune response following its administration to a subject and also have their own unique product-related attributes that influence immunogenicity. Since the volume of published data on the newer modalities is relatively smaller, this review will limit its scope to protein therapeutics referring to them as biotherapeutics. This review will also be limited by the paucity of publicly available data from clinical trials that attempt to connect differences in product formulations and process development aspects of any single biotherapeutic entity to risk outcomes in the clinic. Furthermore, recent advances in formulations containing more than one biotherapeutic for combination regimens in immuno-oncology will be out of scope for purposes of this review article.
Recent guidance pronouncements from Health Authorities (HA) have placed immunogenicity of therapeutic protein products under a higher level of scrutiny, and current trends and communications require drug developers to provide a product and patient-related immunogenicity risk assessment summary report as early as IND (investigational new drug) submission that should periodically get updated with data as progress is made in the development cycle until the product achieves marketing approval [26]. The most recent HA guidance document from 2019 recommended including the risk assessment report within the integrated immunogenicity summary report [27]. This review will focus on some of the product-related critical attributes (Table 2) that could be potential immunogenicity risk factors highlighting some recent studies that have investigated these factors. These studies should help in understanding the association of chemistry, manufacturing, and controls (CMC) aspects of the product with immunogenicity risk. Several excellent reviews have covered this subject in the past that can be referenced for additional details [18, 28,29,30,31,32].
Immunogenicity Background
Antidrug antibodies (ADAs) elicited in vivo to a biotherapeutic are produced by B cells, and their generation is fundamentally driven by two pathways that also interact with one another: (a) T-dependent pathway that utilizes T cell to help to activate B cells and (b) the T-independent pathway.
T Dependent Pathway
The T-dependent pathway involves activation of T cells (CD4+ helper T cells) by peptides derived from the biotherapeutic and presented to the T cells by antigen presenting cells (APC) in a class II MHC (major histocompatibility complex) restricted manner. Class II MHC-bearing cells include dendritic cells (DC), macrophages, and B cells which uptake, process, and present peptides derived from the biotherapeutic on their cell surface class II MHC molecules. Activated T cells produce specific cytokines that enhance B cell expansion and result in ADA production that are higher in affinity and titer and longer lasting. These cytokines also enable ADA isotype switching from IgM to IgG and affinity maturation resulting in high affinity IgG ADA to the biotherapeutic. This is the typical and most common type of ADA that mediates most of the deleterious immunogenicity effects. Peptide sequences that are more prone to be presented by multiple MHC alleles and thereby increase the T cell response are often referred to as T cell hotspots. Some B cells activated through the T-dependent pathway become long lasting memory cells that at a later time point of antigenic exposure are capable of maturing into long lasting plasma cells secreting antibody with same specific epitope recognition [17, 31]. It should be emphasized that B cell specificity is driven by both amino acid sequence and by the conformational uniqueness of the protein often involving noncontiguous portions of the biotherapeutic protein brought close to one another in three-dimensional space; in contrast, T cell specificity is dependent primarily on peptide sequence in the context of MHC restriction; therefore, epitopes recognized by the B cell and T cell receptors may or may not necessarily share the same peptide sequences.
Uptake of biotherapeutic proteins by APCs can be mediated by pinocytosis, Fc-receptor (FcR)-mediated endocytosis, or phagocytosis [33, 34]. In addition, depending on the APC cell type, toll-like receptors (TLR), some C-type lectins, and complement receptors can also mediate uptake. If the biotherapeutic is pre-complexed with a preexisting ADA or if it presents itself in an aggregated form as a consequence of local physiological milieu depending on the route of administration, its uptake could be enhanced. Some formulation buffers can influence the native protein conformational status and thereby predispose to antigen uptake. The effect of different formulation buffers for interferon beta 1-alpha (Rebif®) on antigen uptake and presentation by dendritic cells from normal healthy adult donors were compared using ex vivo T cell activation assays. These buffers differed in stabilizers that influence the overall tertiary and quaternary structure of the active ingredient and thus formation of aggregates [35]. Uptake by APC is followed by antigen processing and presentation where proteins are digested intracellularly in the endosomal compartments to generate peptides which then bind to class II MHC molecules and are translocated to the cell surface. Although these steps follow one another as described, they are independent intracellular processes and are not coupled. This leads to phenotypic changes in the DC associated with a mature form and is also accompanied by DC migration to locally draining lymph nodes where they present the peptides to naive T cells. Depending on a combination of the foreignness of the peptide sequence, the tolerogenic status of the host, and availability of specific T cell receptor (TCR) bearing T cells along with their costimulatory receptors, T cells get activated and provide the second stimulus that is needed to drive a rapid expansion of any B cells that might have recognized a drug-specific unrelated epitope [36]. Host MHC haplotype and peptide sequence-dependent neoantigens that constitute specific T cell epitopes together are the primary immunogenic drivers in this pathway; presence of either one alone does not constitute an immunogenic risk. The role of aggregation or poor solubility of a biotherapeutic protein in the in vivo compartments influence several steps in this pathway and will be discussed at greater length under the section of quality attributes.
T Independent Pathway
T-independent pathway generally involves direct binding of an aggregated antigen or an antigen with repeating epitopes [37] to the cell surface B cell receptors (BCR) inducing receptor clustering and internalization and leading to stimulation of B cells [38, 39]. A second mechanism involves ingestion of the biotherapeutic protein by specialized circulating dendritic cells [40] which later migrate to the spleen and present the protein to splenic marginal zone B cells. Without T cell help, such B cells typically secrete IgM ADA since they do not undergo class switching and they tend to be transient and of lower affinity. It is conceivable that a biologic presenting itself in an aggregated form could have a closer juxtaposition of epitopes arising from several therapeutic molecules in the aggregate which in turn have a higher propensity to cross-link BCR and a greater likelihood of T-independent stimulation of B cells. Such B cells upon encountering a second signal either through T cell help or stimulation through their TLR can rapidly mature through the T-dependent pathway leading to higher titer and longer lasting ADA [38]. It should be emphasized that both the above pathways are not exclusive; instead they interact and potentiate one another. For example class II MHC molecules on B cells can make them APC through BCR-mediated antigen uptake and processing and allowing them to present the derived peptides to epitope-specific T cells [36, 39].
Since a majority of biologics derive from fully humanized models or bear minor differences from a native endogenous molecule, the intrinsic foreignness of the sequence as an influence on immunogenicity has been considerably reduced with the caveat that neoantigenic epitopes could possibly arise by engineered point mutations or from linker sequences that link different protein domains in the biotherapeutic product. Sequences within the idiotypes of monoclonal antibody drugs can also be recognized as foreign depending on their divergence from germ line sequences. Therefore underlying a sustained and high titer polyclonal immunogenic response, there is usually some mechanism that leads to a break in tolerance – a phenomenon that prevents the host from reacting to self-derived antigens. In general, a greater abundance of the host endogenous protein leads to more complete tolerance and a higher bar to break it; thus, biotherapeutics that are recombinant versions of less abundant endogenous proteins are more at risk to have tolerance to them compromised [30, 31]. Some of the factors that lead to breakdown of tolerance arise from product quality and impurities and will be discussed at greater length in the subsequent sections.
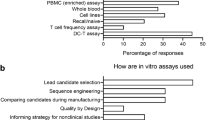
Product and Quality Attributes that Might Potentiate Risk
Foreignness of the Protein
Biotherapeutics that are developed as replacement therapy can be seen as foreign by the immune system in a patient who has a loss in function mutant form of the endogenous version and thereby has a higher likelihood of generating peptides that elicit a T cell reaction. Pharmacological efficacy for replacement biotherapeutics or enzyme replacement is largely driven by the sequence integrity of epitopes on the biotherapeutic that drives the specific drug receptor interaction. Quite often the loss of function mutations seen in patients affects the same epitopes. This leaves very little room to modulate the sequences that are required for efficacy and may also bear T cell activating epitopes. The strategy of risk mitigation in these situations involves methods to enable foreign protein tolerization in the host through dosing and drug delivery modifications [41]. Antibody-based biotherapeutics including multispecific modalities, engineered Fc domains, single chain fragments, single domain antibodies, and biotherapeutic recombinant endogenous proteins which are engineered as part of a larger fusion protein can create neoepitopes at the site of artificially inserted linkers as well as unmask cryptic epitopes. Polymorphism in primary sequence of the endogenous counterpart in human population or the presence of unnatural sequences not found in nature could constitute a risk for the presence of T cell activating epitopes [11, 42, 43]. Besides the novelty of idiotypic epitopes, allotypic differences in endogenous IgG could also make some patients exposed to potential T cell activating epitopes present in mAb or Fc-based biotherapeutics. Given that these are potentially immunogenic, there are in silico and in vitro tools for identification and immunogenicity prediction of such sequences [43, 44]. Most of the in silico tools center on the use of high-throughput computational approaches to map peptides derived from the biotherapeutic in various iterations with peptide sequence databases which identify sequences most likely to bind to various class II HLA haplotypes and potentially lead to T cell activation. It should be emphasized that this approach solely looks at peptide/MHC interaction with commonly present class II alleles and is limited by lack of information on the intracellular processing and presentation steps in APC, the presence of T cell receptors (TCR) specific facing epitopes on the peptides, and peptide MHC affinities. For these and other reasons, such in silico predictions may overpredict risk [45]. However this is a commonly used first step during early development and enables derisking through more informed candidate selection. Depending on the location and relevance of such sequences to the overall pharmacology, such sequences can be replaced and corrected during early development. In silico assessment is complemented by in vitro or ex vivo assays using peripheral blood mononuclear cells (PBMC) from a diverse cohort of normal healthy adult human donors representing a broad distribution of relevant class II MHC polymorphisms. These assays allow peptides to be naturally processed and presented. PBMC contain both APC and T cells and are cultured in vitro spiked with varying amounts of the drug product. Variations of this assay include isolation of dendritic cells which are pulsed with the biologic drug and then incubated with CD4+ T cells. Measures of T cell activation and proliferation reflect immunogenic potential of epitopes uncovered by in silico methods and thereby provide a certain degree of predictability to immunogenicity that might occur in the clinic [43, 44]. These methods also offer a reliable and easy to use tool to assess and compare immunogenic potential of different product lots that differ in manufacturing processes, formulations, excipients, and suspected contaminants and can compare immunogenicity resulting from different stress conditions impacting product solubility or aggregation [46]. Some of the major limitations of using PBMC from a subset of normal healthy donors include meaningful representation of HLA polymorphisms present within the targeted disease population and the inability to recreate the true complexities of in vivo cellular dynamics within the lymphoid organs where much of the T cell activation occurs. Pleiotropic mechanisms of action of the biotherapeutic on PBMC can affect data interpretation, and therefore experimental conditions and positivity criteria of the assay must be carefully decided [43, 47]. In vitro T cell activation assays remain a commonly used tool to inform early candidate selection, deimmunization through removal or modification of potential T cell activating epitopes, and optimization of physicochemical determinants in the final product formulation as part of the derisking strategy for immunogenicity [35, 48]. However engineering on potential T cell epitopes should be considered cautiously to preclude any unintended changes to the physiochemical properties and abrogation of intended pharmacological activity. Besides T cell activating epitopes, T cell regulatory epitopes (Tregitopes) are naturally present epitopes, present on IgG that bind to class II MHC, activate T regulatory (Tregs) cells, and modulate immune response by promoting immunosuppression and tolerance [49]. Presence of such designer epitopes introduced into biotherapeutics has been investigated as a possible deimmunizing strategy [50]. HLA-binding assays using product-derived peptide libraries and labeled tetramers that represent the α and β heterodimers of class II alleles have also been used as part of the immunogenicity prediction tool package. Peptides can be rank ordered based on their binding affinity to different class II alleles and then later tested in cell-based assays [43]. Unlike T cell epitopes, prediction of B cell epitopes is harder on proteins since B cells recognize both linear and conformational epitopes; well-spaced apart amino acid stretches could constitute a conformational epitope. Moreover B cells display far more clonal diversity than T cells, thus minimizing any strength of epitope prediction.
Biochemical and Biophysical Characteristics
From the CMC perspective, there are several steps after the determination of the primary molecular structure that are critical to the release of a finished marketable product that is both safe and efficacious. Many of these steps follow the principles of “quality by design,” whereby processes and specifications are determined by knowledge obtained through analysis of several biophysical and potency parameters. These steps help in defining a set of critical quality attributes (CQA) and critical process parameters that consistently leads to a desired end product. With relevance to mitigating potential immunogenicity risk from a product point of view, several components within the CQA can be addressed [32]. Not all attributes are equally critical from an immunogenicity perspective; only those that are known to be potentially impactful are discussed below. There are also process-related factors that may play a precursor role to some of these attributes and thereby indirectly influence immunogenicity of the product; these are discussed under a separate section. Although there will be no clear upfront unequivocal evidence linking any one such attribute to be of immunogenic potential during a drug development program, the risk-based approach warrants the application of general principles of what product qualities trigger either an adaptive and/or innate immune response and any lessons learned from the constantly evolving published data around this subject. There have been several excellent reviews on this subject, and this article will focus on the more recent findings around some of these characteristics [28,29,30,31,32].
Glycosylation and Other Posttranslational Modifications
Posttranslational modifications that occur on biotherapeutic proteins are determined by the expression system or cell line of choice utilized for production. Among these modifications, glycosylation is the commonest that can modulate immunogenic properties of the product [51, 52]. Majority of biotherapeutics currently in the development pipeline and in the market are produced in Chinese hamster ovary cell lines (CHO) although until a few year ago, murine myeloma (NS0) cell lines were also used. Unlike other xenogeneic-derived cell lines such as yeast and insect cell lines, these mammalian cell lines are believed to have glycan structures that more closely resemble native human glycans. However both NS0 and CHO (to a lesser degree) cell lines are known to express N-glycolylneuraminic acid (NGNA), a nonhuman sialic acid that gets incorporated into biotherapeutic proteins. This modified sialic acid is not found in humans and only slightly different (one extra oxygen atom) from N-acetylneuraminic acid that is native to humans; yet humans are known to have preexisting antibodies to N-glycolylneuraminic acid which could predispose patients to develop treatment emergent ADA [53]. Galactose -(α1–3)-galactose linkages present on the termini of sugar structures are known to react with a subset of preexisting antibodies present in the healthy population [54] residing within a certain geographical distribution and have been associated with adverse effects consequent to certain chimeric monoclonal antibody biotherapeutics like cetuximab that were produced in SP2/0 cells [8]. Severe anaphylactic reactions were seen due to preexisting IgE antibodies to this carbohydrate structure. A reason for the discontinuation of NS0 cells as production cell lines, this is also known to be expressed in such cell lines, but to a far lesser known extent in CHO cells. The same glycan structure was also attributed to immune responses seen to bovine thrombin product where contaminating bovine factor V elicited neutralizing antibodies that cross reacted with the endogenous factor V version in patients resulting in serious bleeding conditions [55].
Glycosylation introduces heterogeneity in the product that is dependent on cell culture conditions and therefore needs to be monitored during manufacturing. Glycoforms influence functional activity and also impact product stability, protein folding, and optimal biophysical characteristics [51]. While certain structural forms confer antigenicity, in many cases, they can minimize aggregation and also may mask an immunogenic epitope [56]. Since mammalian cell lines can make nonhuman glycans that could be immunogenic, derisking immunogenicity has included (a) reengineering such cell lines, e.g., CHO cells have been modified for reduced NGNA expression and yeast cells known for their high mannose sugars have also been reengineered for human glycosylation patterns [57, 58] as well as (b) developing human cell lines [59] which have been widely used in developing vaccines but have only recently been used for producing biotherapeutics. Such cell lines have a greater likelihood of maintaining similar posttranslational modifications as present on endogenous human proteins. Preserving the same glycosylation motifs is especially important with recombinant human protein biotherapeutics like GM-CSF, IFN-β1a, and IL-2 [28]. GM-CSF, produced in yeast-based expression systems, lacked O-linked glycosylation that is normally present on the endogenous protein and has resulted in ADA production reactive to epitopes on the protein chain that were exposed by the lack of O-glycosylation; although these ADA cross reacted with the native GM-CSF, they were non-neutralizing. Regulatory authority scrutiny on glycan structures on biopharmaceutical products is especially relevant for biosimilars. Back in 2008, FDA rejected an application from Genzyme to produce the drug Myozyme (alglucosidase alpha) for the treatment of Pompe disease from its 200-L scale facility despite having approved earlier the same product from the company’s 160-L scale facility. The FDA indicated that the carbohydrate structure of the products (specifically in this case, the composition of mannose-6-phosphate) manufactured at different scales was different and therefore not biologically equivalent. Immunogenicity rates and the proportion of those with neutralizing antibodies were different upon further investigations using the two similar versions of Myozyme [60].
In the case of recombinant IL-2 (Proleukin) made in E. coli, the lack of any form of glycosylation is believed to have made the product less soluble and thereby more immunogenic. Other forms of chemical modifications of relevance to immunogenicity include the attachment to polyethylene glycol (PEG) [61, 62] which is a commonly used covalent adduct to increase the half-life and thereby the bioavailability of certain biotherapeutics. While PEG itself is considered to suppress immunogenicity, naturally occurring preexisting anti-PEG antibodies are known to be present and described across several studies [61, 63]. In some instances, their titers have been elevated post exposure resulting in enhanced clearance of PEG-uricase and PEG-asparginase [64]. IgM ADA antibodies are more likely to be detected reactive to PEG than to the protein portion of the biotherapeutic [61].
Aggregation and Precipitation
Among various product-related attributes, aggregation has been considered to be most strongly associated with immunogenicity. Protein biotherapeutics should ideally be present in their smallest naturally occurring monodispersed forms. Self-association can lead to aggregates ranging from as small as a dimer to sub-visible particles, and attempts have been made to standardize nomenclature and classification of aggregates to compare data across different laboratories [65]. The terms precipitation and aggregation have been used interchangeably in the literature that describes their links to immunogenicity. Indeed precipitation is characterized by an actual separation of the liquid and solid interphases leading to the formation of particles that could be of any size, while aggregation is a term indicating formation of multimers that could either still be in solution or may form particles. A variety of factors ranging from sequence liabilities for chemical modifications to environmental factors like storage temperature, concentration, pH, ionic strength, freeze/thaw, and mechanical shear affect these changes, and their full discussion is beyond the scope of this article.
Although aggregation has been linked to a higher immunogenicity risk, the actual mechanisms involved in their interaction with the immune system and the influence of their size, number, structure, and amount are either poorly understood or still being investigated [66]. Studies on antigenic epitopes in vaccine aggregates with closely placed repeating epitopes show that they can cross-link B cell receptors or induce pattern recognition TLR on APC and thereby lead to increased antigen uptake or T-independent B cell activation. This in turn can also influence antigen processing and presentation, thus providing an immuno-stimulatory signal [67]. For Fc-bearing monoclonal antibody biotherapeutics that are aggregated, cross-linking of FcR on APC and DC enhances antigen uptake and the diversity of peptides displayed by class II MHC [68]. Activated B cells and APC can in turn express T cell activation and recruitment markers, which in turn potentially leads to T cell-dependent ADA with higher titer and affinities [68, 69]. Computational analysis of protein sequences has also revealed aggregation prone regions that influence the risk for immunogenicity [70]. Most of the studies referenced above have induced aggregate formation under different stress conditions forming aggregates in sizes that are not typically found in drug formulations; furthermore they were tested using in vitro activation assays using naïve human PBMC.
ADA elicited by aggregates may or may not be reactive to the monomeric form of the biotherapeutic depending on whether native epitopes present on monomeric forms were preserved or masked on the aggregates. This could influence whether such aggregate emergent ADA may have neutralizing capability if it binds to a pharmacological active epitope on the aggregated protein. Denatured and misfolded proteins also aggregate and are more likely to generate novel epitopes and mask epitopes present on the monomer forms. These factors suggest that not all aggregates of the same protein would have similar immunogenic outcomes and that the causes and mechanisms behind aggregation, e.g., whether driven by pH or ionic changes in the formulation or due to chemical modifications in the protein itself, could lead to different conclusions.
The relationship between aggregated proteins and immunogenicity in the literature has not been consistently corroborated across different products, and instead the results have varied depending on the molecular structure and function of the biotherapeutic, the methods used to create aggregates, the type, size and concentration of the aggregates being studied, the methodologies to evaluate aggregation and exclude degradation products, the assays to assess immunogenicity, and finally on the host tolerance or reactivity to the biotherapeutic in question [28, 69, 71].
The impact of aggregate size on immunogenicity is hard to tease out from other aggregate characteristics. These are due to limitations in controlling other variables like different stressors used to trigger aggregation, levels of aggregation, aggregate size distribution, conformational perturbations, and potential chemical modifications in aggregates. Earlier studies that had shown higher molecular weight aggregates or higher particle sizes to be more capable of eliciting an immune reaction [69] have been challenged with findings from two recent studies in the past year. The first, looked at mAb dimers since they tend to be the more abundant form of mAb biotherapeutic product aggregates, concluded that they were no more immunogenic than unstressed monomers. The study looked at both formation of ADA as well as follicular T helper cells in draining lymph nodes in mouse studies [72]. In the second report, the same group generated and separated murine monoclonal IgG1 aggregates of varying sizes having similar characteristics from multiple stressors. The mAbs had no foreign epitopes, and the aggregates separated based on size ranged from soluble oligomers to micron size particles. These were subcutaneously dosed in mice fully tolerized to the unstressed IgG1 and where any immune response would most likely be driven by the aggregate size. ADA measurements confirmed no reactivity to unstressed IgG1 and indicated the submicron size (100–1000 nm) particles to be the most immunogenic as compared to soluble oligomers or particles > 1 μm suggesting that while there is a link between aggregate size and immunogenicity, the smaller particles could have a higher risk than larger ones [73]. Some reasons hypothesized in the report to support these findings include a better uptake and processing of the submicron particles by DCs and differences in surface epitope density that favor BCR cross-linking. Besides having a direct bearing on immunogenicity, drug product aggregates can also amplify the response of innate immune cells to contaminants that are innate immune response modulating impurities (IIRMI) [74]; this caveat should also be considered while drawing conclusions from PBMC-based assays evaluating different preparations.
PBMC activation assays and murine models have been used to study the immunogenic potential of aggregates [75]. A novel human IgG-tolerant and immune-competent mouse model has been described and used to study mAb biotherapeutic aggregates induced by several artificial stressor conditions. The results have shown aggregates can break self-tolerance in a size-dependent manner to monomeric IgG [76]; interestingly this model can also be used to evaluate immunogenicity to IgG biotherapeutics that were chemically modified. Results from such studies must take into consideration other factors that modulate an immunogenic response such as aggregate size and amount, biotherapeutic pharmacology, and route of administration to ascertain true clinical risk. Moreover some of the stress conditions and aggregate characteristics used in animal studies or in vitro assays may not be representative of aggregation occurring in vivo. Several reports on immunogenicity to recombinant interleukin and interferon biotherapeutics and its relationship to presence of aggregates have been unable to exclude the fact that this cytokine is pharmacologically an immuno-stimulant which could influence its immunogenicity [28]. Majority of in vitro and in vivo animal studies have been done with aggregates made ex vivo under various non-physiological stress conditions and are useful tools to evaluate drug preparations with different excipients and formulations. However following subcutaneous delivery into a subject, the excipients diffuse away faster than the protein, and it is critical to understand how the local tissue microenvironment could influence in vivo aggregate formation of a protein that might otherwise be well behaved in its formulation and whether there might be any consequences on immunogenicity. A recent study [76] took advantage of an IgG2 mAb that precipitated at neutral physiological pH and could also be fluorescently labeled to noninvasively track its retention in subcutaneous space and migration to the lymphoid organs to understand the role of in vivo precipitation and its effect on immunogenicity. Interestingly the authors show a dose-dependent drug retention in the macrophages present in the subcutaneous space which did not lead to any enhancement of either cell-based or a humoral immunogenic response. They concluded that the in vivo induced aggregation did not contribute to an increased risk in immunogenicity. Further studies exploring the in vivo dynamics with other mAbs of different isotypes using their model system would be helpful to see if their conclusions can be extended across different mAbs.
From a product safety perspective, biotherapeutic aggregation is a CQA and must be carefully controlled during all steps in the product’s generation, purification, formulation, handling, and storage in appropriate container systems. Methods to determine aggregation should be carefully evaluated and validated during lot release and stability evaluations. They should be complemented by methods that independently identify sub-visible particles over a wide range of sizes during storage. Minimizing aggregates with the use of membrane filters of defined pore sizes can also be supplemented with the use of specific adsorbents that bind to non-native IgG conformers and remove aggregation precursors in mAb biotherapeutic during manufacturing. This can permit long-term storage and minimize immunogenicity risk [77].
There are no well-reported clinical studies linking ADA generation in human subjects directly with presence of drug aggregates because of the many other confounding and inextricable determinants of immunogenicity that are simultaneously present. Even in nonclinical animal models, there are only few studies [72, 73, 76] that have looked at any association with immunogenicity or attempted to characterize the aggregates being studied. The term “aggregation leads to immunogenicity” should not necessarily a catch all phrase for aggregates since several aspects of aggregation of the same biotherapeutic protein can differentially influence in vivo immune response ranging from rapid clearance of the aggregates or some minimal immune response with no cross reactivity to the monomers or a response from both the adaptive and innate arms of the immune system with possible pharmacological abrogation.
Impurities
Impurities with adjuvant-like properties derived from the manufacturing process if present in the product may lead to an immune response even in the absence of a classical ADA reactive to the biotherapeutic protein itself. Such impurities (often called innate immune response modulating impurities or IIRMIs) include host cell protein (HCP), high-mobility group proteins (HMGB1), lipopolysaccharides (LPS), and bacterial DNA derived from E. coli. They can activate pattern recognition receptors (PRR) that recognize diverse sets of molecular patterns resulting in the production of pro-inflammatory cytokines as well as increased antigen processing and presentation by APC. One of the best characterized families of such receptors is the toll-like receptor (TLR) present on innate immune cells and when engaged can lead to serious adverse reactions [28, 78, 79]. Among the various IFNβ preparations in the market, Betaferon and Extavia were shown to be more immunogenic than the related product Avonex. This was found to be due to the presence of impurities that activated TLR2 and TLR4 but not TLR5 and TLR9 and most probably indicative of bacterial endotoxin and a second IIRMI; this correlated to the higher rates of clinical immunogenicity to Betaferon [80]. Cell-based assays have been developed that can monitor IIRMIs in the final product following any changes to manufacturing or provide a comparison with different related products and thereby serve as a reliable tool in immunogenicity risk assessment methodologies [80].
With the use of mammalian cells for the production of biologics and the current improvements in manufacturing controls and checks, the risk of such microbial-related contamination has been reduced to very low levels; however, these are critical product quality attributes in any drug development program; cell-derived HCP content is routinely monitored during different stages of manufacturing. It should be emphasized that a nonspecific immune reaction elicited by contaminants as described above can provide costimulation and break immunological tolerance and thereby enhance the incidence and titer of product-specific ADA formation triggered in the host [81]. However there have been reports based on in vitro PBMC activation assays and in silico algorithms that suggest that in some instances, high levels of HCP in some monoclonal biotherapeutics do not increase risk of immunogenicity. These mAb preps had a mixture of at least 25 or greater CHO-derived HCPs present in varying amounts and identified by proteomic-based MS assays. Immunogenicity risk could be related to their final concentration in the drug products, risk assessment scores derived from sequence analysis using in silico algorithms, and the degree of CHO-unique epitope content indicative of their foreignness to humans [78].
Process-related factors indirectly impacting CQA
This section highlights some of the downstream processing events following the purification of the drug product up to its availability as a filled drug product in containers ready for use at the clinic or pharmacy. These factors may indirectly impact some of the product attributes and thereby could play a role in its immunogenicity.
Excipients
Most biologics formulations contain excipients which are added to prolong their shelf life and overcome product degradation or biophysical changes due to long-term storage or any stress conditions such as temperature fluctuations. Some of these excipients are not biologically inert and may either have a direct impact by eliciting an allergic reaction in the host or may have an indirect impact by inducing changes such as aggregation or oxidation in the biotherapeutic product itself. There are no recent studies that clearly implicate excipients playing a role in product immunogenicity; however, their potential to do so should not be ignored. A well-described review of existing literature can be referenced here [28].
Chemical modifications and degradation
The biotherapeutic protein itself may undergo chemical changes that might lead to immune recognition of ectopically created neoepitopes. These are chemically derived product impurities resulting from oxidation, deamidation, or deimination and also include degradation products following protease clipping. There are very few reports directly linking such modifications to an overt product-specific immune response. They are considered as risk factors since they can potentially alter protein conformation and promote aggregation or change the dynamics of antigen intake, processing, and peptide presentation in vivo [28, 82]. Moreover immune tolerance to endogenous proteins can be broken following similar chemical changes on a recombinant therapeutic homolog that can occur in vivo and leading to auto antibody formation. Such chemical changes on the biotherapeutic product also referred to as biotransformation may occur in vivo like in a physiologically impaired environment as in inflamed tissues [83] rendering them immunogenic. It is the changes that happen in vitro during manufacturing that need to be monitored and minimized. Product impurities also include protease cleaved truncated products that could unmask an epitope or potentially create neoepitopes.
Container closure considerations
These concerns arise from potential structural changes in the biotherapeutic arising as a consequence of its physical interaction with the container or its closure such as the stopper or with different components in the infusion system such as syringes, bags, or catheters. The biotherapeutic could undergo surface adsorption with them over a prolonged period of time or may interact with leachables arising from one or more of these container materials. Such leachables include metals, plastic, and antioxidants. These interactions can potentially alter structural integrity of biotherapeutic product and its possible immunogenicity. Interfaces with glass or air can denature proteins, thereby leading to aggregation and immunogenicity. At high pH formulations, glass containers may generate microparticles that get coated with the biotherapeutic product presenting itself in an immunogenic manner [84]. Leached materials can either act as an adjuvant or they may chemically modify the product making it more immunogenic. Metal oxides that leach from syringes leading to protein aggregation and eluates from rubber stoppers with potential immunomodulatory properties can in both instances promote an immunogenic reaction to the active product. A description of container components, any leachables, formulation, and excipients must be provided using multiple analytical techniques to be assured of their compatibility with each product and are typically done under both stressed as well as real-time conditions. Stability studies done on the product are predicated on the use of appropriate containers and formulations used with the product under real-time storage conditions and must demonstrate product stability with no propensity for aggregation, thereby mitigating immunogenicity risk [85]. A more detailed perspective on emerging technologies and future approaches to assign relative immunogenicity risk to particulate material has been described by Bee JS et al. [86].
In order to investigate the effect of protein particulates on immunogenicity, a recent study prepared such particulates by adsorbing an IgG2 murine monoclonal antibody with materials in the container or syringe such as silicone oil micro-droplets, glass, and aluminum hydroxide microparticles, administered them subcutaneously into mice, and showed that they were capable of eliciting higher ADA responses than particle-free mAb preparations [87].
One of the most serious and notable examples of an adverse reaction was reported during a change in the formulation for Epogen when human serum albumen was replaced with PS80 (polysorbate) as a protein stabilizer in its formulation. This resulted in unusually higher levels of leachables from the uncoated stoppers of pre filled syringes containing the drug. It is only believed that these leachables acted as adjuvants triggering an ADA response to Epogen leading to pure red cell aplasia (PRCA) [10, 88] since there were other studies that showed PS80-derived extractables and leachables in real time did not present a danger signal to dendritic cells [89]. Risk mitigation strategies included the use of coated stoppers and improved handling that subsequently reduced the incidence of this adverse event. It must also be noted that there were reports of in silico identification of immunogenic epitopes in erythropoietin [90], thus emphasizing the notion that while risk associated with most of these product factors may not be realized in isolation, their relevance to immunogenicity is underscored when present in combination with several other factors such as sequence liabilities, presence of adjuvants, and route of administration occurring at the same time.
Conclusions
Given the multifactorial genesis of an immune response to a biologic (Table 1) and the need for a multifaceted approach to risk mitigation strategies, choosing the biotherapeutic and expression platforms, controlling product selection, performing diligent characterization, monitoring various processes during manufacturing, checking for impurities especially those with adjuvant properties in the formulation, and executing validated release testing methods are some practices that are already in place in drug development programs, and they also offer direct opportunities to be leveraged to minimize an aberrant immune response to the biologic product. Many biotherapeutics need to be repeatedly administered, sometimes over a patient’s lifetime, and as a result, an ADA response can be an expected outcome. It is also true that some subjects do and others do not develop clinically significant ADA with little known of the underlying molecular basis. Besides looking at CMC factors, sponsors must also take into account the underlying disease pathology, pharmacological activity of the product, genetic differences and HLA allelic variants, and the presence of natural antibodies in the patient population for a complete immunogenicity risk assessment. However such patient-dependent factors are rarely used as patient selection criteria in clinical trials and mostly give little room for modulation besides a few investigational methods to induce tolerance or interfere with B and T cell activation that still need further confirmation [41]. Individual heterogeneity can impact either their immune response to treatment or their manifestation of any immunological adverse effects. Thus clinical trials very seldom use any host-dependent immunogenicity risk factors as selection criteria for study enrollment. Therefore due diligence from a CMC perspective provides the manufacturer one way to minimize immunogenicity risk, potentially decreasing both incidence and intensity of an immune response if not eliminate immunogenicity. Furthermore the use of animal studies to study immunogenicity while useful for lead selection and to understand which process improvements or formulations are least immunogenic is generally not considered to be predictive of immune responses in humans. A fundamental step to reduce the risk of immunogenicity is in selecting the right product. In this regard a first step is a judicious evidence-based selection of the lead candidate focusing on its sequence and the modular structures created by recombinant engineering. Risk mitigation is initiated through rational drug design approaches that incorporate computational identification and elimination of residues with propensities for chemical modification or those conferring a predisposition to aggregation [70] or poor solubility or instability. Similarly removal of sequence liabilities for T cell recognition or inclusion of Treg-specific sequences that suppress T cell responses could be implemented through site-specific mutagenesis, although potency and epitope specificity traits of the product could constrain the extent to which the lead drug candidate can be modified. In other words, besides the classical safety and efficacy endpoints that drive the success of a drug program, the capability to make a marketable product from a molecule as defined by traits described in this review also weighs significantly on a program’s success.
Summary
All biotherapeutics can potentially induce immunogenicity in the patient which can vary from low affinity low titer ADA with no clinical impact to clinically and therapeutically impactful ADA. With higher scrutiny on patient safety-related outcomes, immunogenicity risk assessment is becoming a necessary and evolving process in biologics drug development programs. This article has highlighted product-related attributes that can be managed early and throughout the development cycle to potentially mitigate immunogenicity risk. While no one single factor is predictive of immunogenicity, their risk is contextual to several other coexisting factors. However diligent monitoring of each factor can minimize overall adverse clinical consequences of immunogenicity.
References
Van Schouwenburg PA, Rispens T, Wolbink GJ. Immunogenicity of anti-TNF biologic therapies for rheumatoid arthritis. Nat Rev Rheumatol. 2013;9:164–72.
Clarke JB. Mechanisms of adverse drug reactions to biologics. Handb Exp Pharmacol. 2010;196:453–74.
Chong BH, Choi PY-I, Khachigian L, Perdomo J. Drug-induced immune thrombocytopenia. Hematol Oncol Clin N Am. 2013;27:521–40.
Deehan M, Garces S, Kramer D, Baker MP, Rat D, Roettger Y, et al. Managing unwanted immunogenicity of biologicals. Autoimmun Rev. 2015;14:569–74.
Schellekens H. The immunogenicity of therapeutic proteins. Discov Med. 2010;9(49):560–4.
Leach MW, Rottman JB, Hock MB, Finco D, Rojko JL, Beyer JC. Immunogenicity/hypersensitivity of biologics. Toxicol Pathol. 2014;42(1):293–300.
Vultaggio A, Nencini F, Pratesi S, Petroni G, Maggi E, Matucci A. Manifestations of antidrug antibodies response: hypersensitivity and infusion reactions. J Interf Cytokine Res. 2014;34(12):946–52.
Chung CH, Mirakhur B, Chan E, Le QT, Berlin J, Morse M, et al. Cetuximab-induced anaphylaxis and IgE specific for galactose-alpha-1,3-galactose. N Engl J Med. 2008;358(11):1109–17.
Chirmule N, Jawa V, Meibohm B. Immunogenicity to therapeutic proteins: impact on PK/PD and efficacy. AAPS J. 2012;14(2):296–302.
Casadevall N, Nataf J, Viron B, Kolta A, Kiladjian JJ, Martin-Dupont P, et al. Pure red-cell aplasia and antierythropoietin antibodies in patients treated with recombinant erythropoietin. N Engl J Med. 2002;346(7):469–75.
De Groot AS, Scott DW. Immunogenicity of protein therapeutics. Trends Immunol. 2007;28(11):482–90.
Krieckaert C, Rispens T, Wolbink G. Immunogenicity of biological therapeutics: from assay to patient. Curr Opin Rheumatol. 2012;24(3):306–11.
Ridker PM, Tardif JC, Amarenco P, Duggan W, Glynn RJ, Jukema JW, et al. Yunis C; SPIRE Investigators. Lipid-reduction variability and antidrug-antibody formation with bococizumab. N Engl J Med. 2017;376(16):1517–26.
Kromminga A, Schellekens H. Antibodies against erythropoietin and other protein-based therapeutics: an overview. Ann N Y Acad Sci. 2005;1050:257–65.
Sorensen PS, Ross C, Clemmesen KM, Bendtzen K, Frederiksen JL, Jensen K, et al. Clinical importance of neutralizing antibodies against interferon beta in patients with relapsing-remitting multiple sclerosis. Lancet. 2003;362(9391):1184–91.
Anderson PJ. Tumor necrosis factor inhibitors: clinical implications of their different immunogenicity profiles. Semin Arthritis Rheum. 2005;34(5 Suppl1):19–22.
Sethu S, Govindappa K, Alhaidari M, Pirmohamed M, Park K, Sathish J. Immunogenicity to biologics: mechanisms, prediction and reduction. Arch Immunol Ther Exp (Warsz). 2012;60(5):331–44.
Sathish JG, Sethu S, Bielsky MC, de Haan L, French NS, Govindappa K, et al. Challenges and approaches for the development of safer immunomodulatory biologics. Nat Rev Drug Discov. 2013;12(4):306–24.
Aarskog NK, Marøy T, Myhr KM, Vedeler CA. Antibodies against interferon-beta in multiple sclerosis. J Neuroimmunol. 2009;212(1–2):148–50.
Li J, Yang C, Xia Y, Bertino A, Glaspy J, Roberts M, et al. Thrombocytopenia caused by the development of antibodies to thrombopoietin. Blood. 2001;98(12):3241–8.
Maneiro JR, Salgado E, Gomez-Reino JJ. Immunogenicity of monoclonal antibodies against tumor necrosis factor used in chronic immune-mediated inflammatory conditions: systematic review and meta-analysis. JAMA Intern Med. 2013;173(15):1416–28.
Krishna M, Nadler SG. The role of anti-drug immune complexes. Front Immunol. 2016;7:21.
Koren E, Smith HW, Shores E, Shankar G, Finco-Kent D, Rup B, et al. Recommendations on risk-based strategies for detection and characterization of antibodies against biotechnology products. J Immunol Methods. 2008;333(1–2):1–9.
Rup B, Pallardy M, Sikkema D, Albert T, Allez M, Broet P, et al. Consortium, Standardizing terms, definitions and concepts for describing and interpreting unwanted immunogenicity of biopharmaceuticals: recommendations of the innovative medicines initiative ABIRISK consortium. Clin Exp Immunol. 2015;181(3):385–400.
Kloks C, Berger C, Cortez P, Dean Y, Heinrich J, Bjerring Jensen L, et al. A fit-for-purpose strategy for the risk-based immunogenicity testing of biotherapeutics: a European industry perspective. J Immunol Methods. 2015;417:1–9.
U.S. Department of Health and Human Services. Food and Drug Administration. Guidance for Industry: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/immunogenicity-assessment-therapeutic-protein-products. Immunogenicity Assessment for therapeutic protein products. Accessed Aug 2014.
U.S. Department of Health and Human Services. Food and Drug Administration. Guidance for Industry: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/immunogenicity-testing-therapeutic-protein-products-developing-and-validating-assays-anti-drug. Immunogenicity testing of therapeutic protein products - developing and validating assays for anti-drug antibody detection. Accessed Jan 2019.
Singh SK. Impact of product-related factors on immunogenicity of biotherapeutics. J Pharm Sci. 2011;100(2):354–87.
Richard J, Prang N. The formulation and immunogenicity of therapeutic proteins: Product quality as a key factor. IDrugs. 2010;13(8):550–8.
Singh SK, Cousens LP, Alvarez D, Mahajan PB. Determinants of immunogenic response to protein therapeutics. Biologicals. 2012;40(5):364–8.
Baker MP, Reynolds HM, Lumicisi B, Bryson CJ. Immunogenicity of protein therapeutics: The key causes, consequences and challenges. Self Nonself. 2010;1(4):314–22.
Van Beers MM, Bardor M. Minimizing immunogenicity of biopharmaceuticals by controlling critical quality attributes of proteins. Biotechnol J. 2012;7(12):1473–84.
Bajtay Z, Csomor E, Sándor N, Erdei A. Expression and role of Fc- and complement-receptors on human dendritic cells. Immunol Lett. 2006;104(1–2):46–52.
Regnault A, Lankar D, Lacabanne V, Rodriguez A, Théry C, Rescigno M, et al. Fc gamma receptor-mediated induction of dendritic cell maturation and major histocompatibility complex class I-restricted antigen presentation after immune complex internalization. J Exp Med. 1999;189(2):371–80.
Jaber A, Baker M. Assessment of the immunogenicity of different interferon beta-1a formulations using ex vivo T-cell assays. J Pharm Biomed Anal. 2007;43:4 1256–1261.
Goins CL, Chappell CP, Shashidharamurthy R, Selvaraj P, Jacob J. Immune complex-mediated enhancement of secondary antibody responses. J Immunol. 2010;184(11):6293–8.
Fehr T, Bachmann MF, Bucher E, Kalinke U, Di Padova FE, Lang AB, et al. Role of repetitive antigen patterns for induction of antibodies against antibodies. J Exp Med. 1997;185(10):1785–92.
Batista FD, Harwood NE. The who, how and where of antigen presentation to B cells. Nat Rev Immunol. 2009;9(1):15–27.
Fogdell-Hahn A. Antidrug antibodies: B cell immunity against therapy. Scand J Immunol. 2015;82(3):184–90.
Balázs M, Martin F, Zhou T, Kearney J. Blood dendritic cells interact with splenic marginal zone B cells to initiate T-independent immune responses. Immunity. 2002;17(3):341–52.
Salazar-Fontana L, Desai DD, Khan TA, Pillutla RC, Prior S, Ramakrishnan R, et al. Approaches to mitigate the unwanted immunogenicity of therapeutic proteins during drug development. AAPS J. 2017;19(2):377–85.
De Groot AS, Moise L. Prediction of immunogenicity for therapeutic proteins: state of the art. Curr Opin Drug Discov Dev. 2007;10(3):332–40.
Jawa V, Cousens LP, Awwad M, Wakshull E, Kropshofer H, De Groot AS. T-cell dependent immunogenicity of protein therapeutics: preclinical assessment and mitigation. Clin Immunol. 2013;149(3):534–55.
Gokemeijer J, Jawa V, Mitra-Kaushik S. How close are we to profiling immunogenicity risk using in silico algorithms and in vitro methods? : an industry perspective. AAPS J. 2017;19(6):1587–92.
Bryson CJ, Jones TD, Baker MP. Prediction of immunogenicity of therapeutic proteins: validity of computational tools. BioDrugs. 2010;24(1):1–8.
Zurdo J, Arnell A, Obrezanova O, Smith N, Gómez de la Cuesta R, Gallagher TR, et al. Early implementation of QbD in biopharmaceutical development: a practical example. Biomed Res Int. 2015;2015:605427.
Wullner D, Zhou L, Bramhall E, Kuck A, Goletz TJ, Swanson S, et al. Considerations for optimization and validation of an in vitro PBMC derived T cell assay for immunogenicity prediction of biotherapeutics. Clin Immunol. 2010;137(1):5–14.
Holgate RG, Weldon R, Jones TD, Baker MP. Characterisation of a novel anti-CD52 antibody with improved efficacy and reduced immunogenicity. PLoS One. 2015;10(9):e0138123.
De Groot AS, Moise L, McMurry JA, Wambre E, Van Overtvelt L, Moingeon P, et al. Activation of natural regulatory T cells by IgG Fc-derived peptide "Tregitopes". Blood. 2008;112(8):3303–11.
Su Y, Rossi R, De Groot AS, Scott DW. Regulatory T cell epitopes (Tregitopes) in IgG induce tolerance in vivo and lack immunogenicity per se. J Leukoc Biol. 2013;94(2):377–83.
Jefferis R. Antibody therapeutics: isotype and glycoform selection. Expert Opin Biol Ther. 2007;7(9):1401–13.
Kuriakose A, Chirmule N, Nair P. Immunogenicity of biotherapeutics: causes and association with posttranslational modifications. J Immunol Res. 2016:1298473
Ghaderi D, Taylor RE, Padler-Karavani V, Diaz S, Varki A. Implications of the presence of N-glycolylneuraminic acid in recombinant therapeutic glycoproteins. Nat Biotechnol. 2010;28(8):863–7.
Galili U, Macher BA, Buehler J, Shohet SB. Human natural anti-alpha-galactosyl IgG. II. The specific recognition of alpha (1----3)-linked galactose residues. J Exp Med. 1985;162(2):573–82.
Kessler CM, Ortel TL. Recent developments in topical thrombins. Thromb Haemost. 2009;102(1):15–24.
Wei X, Decker JM, Wang S, Hui H, Kappes JC, Wu X, et al. Antibody neutralization and escape by HIV-1. Nature. 2003;422(6929):307–12.
Chenu S, Grégoire A, Malykh Y, Visvikis A, Monaco L, Shaw L, et al. Reduction of CMP-N-acetylneuraminic acid hydroxylase activity in engineered Chinese hamster ovary cells using an antisense-RNA strategy. Biochim Biophys Acta. 2003;1622(2):133–44.
Hamilton SR, Davidson RC, Sethuraman N, Nett JH, Jiang Y, Rios S, et al. Humanization of yeast to produce complex terminally sialylated glycoproteins. Science. 2006;313(5792):1441–3.
Dumont J, Euwart D, Mei B, Estes S, Kshirsagar R. Human cell lines for biopharmaceutical manufacturing: history, status, and future perspectives. Crit Rev Biotechnol. 2016;36(6):1110–22.
Fournier J. A review of glycan analysis requirements. BioPharm Int. 2015;28(10):32–7.
Myler H, Hruska MW, Srinivasan S, Cooney E, Kong G, Dodge R, et al. Anti-PEG antibody bioanalysis: a clinical case study with PEG-IFN-λ-1a and PEG-IFN-α2a in naive patients. Bioanalysis. 2015;7(9):1093–106.
Krishna M, Palme H, Duo J, Lin Z, Corbett M, Dodge R, et al. Development and characterization of antibody reagents to assess anti-PEG IgG antibodies in clinical samples. Bioanalysis. 2015;7(15):1869–83.
Hershfield MS, Ganson NJ, Kelly SJ, Scarlett EL, Jaggers DA, Sundy JS. Induced and pre-existing anti-polyethylene glycol antibody in a trial of every 3-week dosing of pegloticase for refractory gout, including in organ transplant recipients. Arthritis Res Ther. 2014;16(2):R63.
Garay RP, El-Gewely R, Armstrong JK, Garratty G, Richette P. Antibodies against polyethylene glycol in healthy subjects and in patients treated with PEG-conjugated agents. Expert Opin Drug Deliv. 2012;9(11):1319–23.
Narhi LO, Schmit J, Bechtold-Peters K, Sharma D. Classification of protein aggregates. J Pharm Sci. 2012;101(2):493–8.
Moussa EM, Panchal JP, Moorthy BS, Blum JS, Joubert MK, Narhi LO, et al. Immunogenicity of Therapeutic Protein Aggregates. J Pharm Sci. 2016;105(2):417–30.
Jones JC, Settles EW, Brandt CR, Schultz-Cherry S. Virus aggregating peptide enhances the cell-mediated response to influenza virus vaccine. Vaccine. 2011;29(44):7696–703.
Rombach-Riegraf V, Karle AC, Wolf B, Sordé L, Koepke S, Gottlieb S, et al. Aggregation of human recombinant monoclonal antibodies influences the capacity of dendritic cells to stimulate adaptive T cell responses in vitro. PLoS One. 2014;9(1):e86322.
Joubert MK, Hokom M, Eakin C, Zhou L, Deshpande M, Baker MP, et al. Highly aggregated antibody therapeutics can enhance the in vitro innate and late-stage T cell immune responses. J Biol Chem. 2012;287(30):25266–79.
Kumar S, Singh SK, Wang X, Rup B, Gill D. Coupling of aggregation and immunogenicity in biotherapeutics: T- and B cell immune epitopes may contain aggregation-prone regions. Pharm Res. 2011;28(5):949–61.
Marszal E, Fowler E. Workshop on predictive science of the immunogenicity aspects of particles in biopharmaceutical products. J Pharm Sci. 2012;101(10):3555–9.
Kijanka G, Bee JS, Schenerman MA, Korman SA, Wu Y, Slütter B, et al. Monoclonal antibody dimers induced by low pH, heat, or light exposure are not immunogenic upon subcutaneous administration in a mouse model. J Pharm Sci. 2019. https://doi.org/10.1016/j.xphs.2019.04.021.
Kijanka G, Bee JS, Korman SA, Wu Y, Roskos LK, Schenerman MA, et al. Submicron size particles of a murine monoclonal antibody are more immunogenic than soluble oligomers or micron size particles upon subcutaneous administration in mice. J Pharm Sci. 2018;107(11):2847–59.
Polumuri SK, Haile LA, Ireland DDC, Verthelyi D. Aggregates of IVIG or Avastin, but not HSA, modify the response to model innate immune response modulating impurities. Sci Rep. 2018;8(1):11477.
Bi V, Jawa V, Joubert MK, Kaliyaperumal A, Eakin C, Richmond K, et al. Development of a human antibody tolerant mouse model to assess the immunogenicity risk due to aggregated biotherapeutics. J Pharm Sci. 2013;102(10):3545–55.
Kinderman F, Yerby B, Jawa V, Joubert MK, Joh NH, Malella J, et al. Impact of precipitation of antibody therapeutics after subcutaneous injection on pharmacokinetics and immunogenicity. J Pharm Sci. 2019;108(6):1953–63.
Senga Y, Honda S. Suppression of aggregation of therapeutic monoclonal antibodies during storage by removal of aggregation precursors using a specific adsorbent of non-native IgG conformers. Bioconjug Chem. 2018;29(10):3250–61.
Jawa V, Joubert MK, Zhang Q, Deshpande M, Hapuarachchi S, Hall MP, et al. Evaluating immunogenicity risk due to host cell protein impurities in antibody-based biotherapeutics. AAPS J. 2016;18(6):1439–52.
Haile LA, Puig M, Kelley-Baker L, Verthelyi D. Detection of innate immune response modulating impurities in therapeutic proteins. PLoS One. 2015;10(4):e0125078.
Haile LA, Polumuri SK, Rao R, Kelley-Baker L, Kryndushkin D, Rajaiah R, et al. Cell based assay identifies TLR2 and TLR4 stimulating impurities in interferon beta. Sci Rep. 2017;7(1):10490.
Verthelyi D, Wang V. Trace levels of innate immune response modulating impurities (IIRMIs) synergize to break tolerance to therapeutic proteins. PLoS One. 2010;5(12):e15252.
Carrasco-Marín E, Paz-Miguel JE, López-Mato P, Alvarez-Domínguez C, Leyva-Cobián F. Oxidation of defined antigens allows protein unfolding and increases both proteolytic processing and exposes peptide epitopes which are recognized by specific T cells. Immunology. 1998;95(3):314–21.
Huang L, Lu J, Wroblewski VJ, Beals JM, Riggin RM. In vivo deamidation characterization of monoclonal antibody by LC/MS/MS. Anal Chem. 2005;77(5):1432–9.
Fradkin AH, Carpenter JF, Randolph TW. Glass particles as an adjuvant: a model for adverse immunogenicity of therapeutic proteins. J Pharm Sci. 2011;100(11):4953–64.
Markovic I. Evaluation of safety and quality impact of extractable and leachable substances in therapeutic biologic protein products: a risk-based perspective. Expert Opin Drug Saf. 2007;6(5):487–91.
Bee JS, Goletz TJ, Ragheb JA. The future of protein particle characterization and understanding its potential to diminish the immunogenicity of biopharmaceuticals: a shared perspective. J Pharm Sci. 2012;101(10):3580–5.
Shomali M, Tanriverdi S, Freitag AJ, Engert J, Winter G, Siedler M, et al. Dose levels in particulate-containing formulations impact anti-drug antibody responses to murine monoclonal antibody in mice. J Pharm Sci. 2015;104(5):1610–21.
Macdougall IC. Pure red cell aplasia with anti-erythropoietin antibodies occurs more commonly with one formulation of epoetin alfa than another. Curr Med Res Opin. 2004;20(1):83–6.
Mueller R, Karle A, Vogt A, Kropshofer H, Ross A, Maeder K, et al. Evaluation of the immuno-stimulatory potential of stopper extractables and leachables by using dendritic cells as readout. J Pharm Sci. 2009;98(10):3548–61.
De Groot AS, McMurry J, Moise L. Prediction of immunogenicity: in silico paradigms, ex vivo and in vivo correlates. Curr Opin Pharmacol. 2008;8(5):620–6.
Acknowledgements
The author would like to acknowledge Gerry Kolaitis and Surendran Rajendran for critically reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares he has no conflict of interest.
Informed Consent
This article does not contain any information that refers to any individual study participants. This article does not contain any studies with human participants or animals performed by the author.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Krishna, M. Product-Related Factors and Immunogenicity of Biotherapeutics. J Pharm Innov 15, 219–231 (2020). https://doi.org/10.1007/s12247-019-09423-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12247-019-09423-2