Abstract
Currently, there is a significant rise in the development and clinical use of a unique class of pharmaceuticals termed as Biopharmaceuticals or Biologics, in the management of a range of disease conditions with, remarkable therapeutic benefits. However, there is an equally growing concern regarding development of adverse effects like immunogenicity in the form of anti-drug antibodies (ADA) production and hypersensitivity. Immunogenicity to biologics represents a significant hurdle in the continuing therapy of patients in a number of disease settings. Efforts focussed on the identification of factors that contribute towards the onset of immunogenic response to biologics have led to reductions in the incidence of immunogenicity. An in-depth understanding of the cellular and molecular mechanism underpinning immunogenic responses will likely improve the safety profile of biologics. This review addresses the mechanistic basis of ADA generation to biologics, with emphasis on the role of antigen processing and presentation in this process. The article also addresses the potential contribution of complement system in augmenting or modulating this response. Identifying specific factors that influences processing and presentation of biologic-derived antigens in different genotype and disease background may offer additional options for intervention in the immunogenic process and consequently, the management of immunogenicity to biologics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The last few decades has witnessed a significant expansion in the development by the pharmaceutical industry of a unique class of drugs, termed as Biopharmaceuticals or Biologics. Biologics are substances whose active component is derived from a biological source by being produced in microorganisms and cells (humans and animals) using biotechnology (Giezen et al. 2008; Rader 2008) and represents more than 30 % of licensed pharmaceutical products (DiMasi et al. 2010; Swinney and Anthony 2011). Biologics have expanded the range of options available for the treatment and management of complex diseases such as diabetes, cancer and autoimmune diseases (Schellekens 2008). Biologics consist of hormones (e.g. insulin, growth hormone, somatotropin), growth factors (e.g. erythropoietin), cytokines (e.g. interferons (IFNs), interleukin (IL)-2, granulo cyte macrophage colony stimulating factor (GM-CSF), vaccines, enzymes, antibodies (e.g. monoclonal antibodies (mAbs) against tumor necrosis factor (TNF)α, IL-2 receptor, lymphocyte function-associated antigen 1, epidermal growth factor receptor), fusion proteins (soluble receptors and cellular ligands) and hybrid proteins (e.g. diphtheria toxin: IL-2) (Giezen et al. 2008; L Revers 2010; Scherer et al. 2010). Based on their pharmacological action and therapeutic application, biologics have been categorized by Leader et al. (2008) into those with regulating activity (e.g. recombinant proteins, cytokines), specific targeting capability (e.g. mAbs), vaccines and diagnostics (Table 1).
Adverse Effects of Biologics: The Problem of Immunogenicity
Despite its therapeutic success, the incidence of adverse drug reactions to biologics is becoming increasingly evident (Weber 2004). These reactions can be grouped into those arising from either pharmacological or from non-pharmacological effects. The pharmacological associated adverse reactions are those which arise due to the interaction of the biologics with the intended target and are most often predictable, whereas the non-pharmacological are those which are not associated with the pharmacological action of the biologics (Clarke 2010). The latter includes immunotoxicity which comprises both immune response-mediated (immunogenicity, hypersensitivity and autoimmunity) and non immune response-mediated reactions like acute phase reactions (Clarke 2010). Adverse immunological reactions to Group I and II types (refer Table 1 for groups) of biologics are predominantly associated with long-term treatment regimens, and represent a growing concern to both regulatory bodies and the pharmaceutical industry. The immunotoxicity spectrum includes biologic-induced or biologic-associated infectious complications (Bongartz et al. 2006; Rychly and DiPiro 2005), unwanted immunostimulation (Suntharalingam et al. 2006), anti-drug antibody (ADA) generation (Aarskog et al. 2009; Li et al. 2001; Sorensen et al. 2003) and hypersensitivity reactions (Corona et al. 1999; Shopnick et al. 1996). To better understand, predict and manage immunotoxicity, an immunological classification of these reactions based on the pathologic mechanism was proposed (Pichler 2006; Scherer et al. 2010) and is listed in Table 2. In this article, we will be focussing on immunogenicity—Type β reaction which includes the production of ADA and subsequent neutralization and hypersensitivity reactions to Group I and II types of (non vaccine based) biologics. In particular, we emphasise the role of antigen processing and presentation in this misdirected immune response and consider approaches to predict and reduce such responses.
Anti-Drug Antibodies: Types, Subclasses and Clinical Outcomes
The development of ADA against biologics like IFNs (Janson et al. 1992; Kivisakk et al. 2000; Ronnblom et al. 1992; Scagnolari et al. 2002; Steis et al. 1991), erythropoietin (Casadevall et al. 2002; Weber et al. 2002), factor VIII (Hay et al. 2006b), factor IX (Warrier et al. 1997), insulin (Hirsch 2005), GM-CSF (Wadhwa et al. 2000) and anti-TNFα (Radstake et al. 2009; Svenson et al. 2007) results in compromised therapeutic efficacy and safety. An overt immune reaction to an exogenous version of an endogenous human protein or the failure of immune tolerance to self antigens could be the underlying triggers for ADA development (Goodnow 2001; Schellekens 2003). ADAs can be either binding antibodies (BAb) or neutralizing antibodies (NAb) and can alter pharmacokinetics, decrease the efficacy of the biologic and in some instances induce allergic reactions (Pedotti et al. 2001; Rosenberg 2003, 2006). BAb can either expedite the clearance of the biologic, termed clearing antibodies or they can prolong bioavailability, called sustaining antibodies (Ponce et al. 2009). The difference in effects between BAb and NAb is attributable to sites or epitopes on the therapeutic protein to which they bind. BAbs bind to epitopes that lie within regions of the biologic that do not participate in the interaction between the biologic and its respective receptor/target, whereas NAbs interact with the biologic by binding to epitope(s) that are functionally relevant for ligand–receptor interaction thus rendering the biologic inactive and compromising therapeutic efficacy (Bertolotto et al. 2002, 2004). As seen in response to IFNβ therapy, BAb titres are higher than Nab titres, tend to be produced much earlier during treatment (Scagnolari et al. 2002) and persist longer than NAbs (Bellomi et al. 2003). Based on a few studies, in approximately 40–75 % of positive cases, the NAb tends to disappear or is markedly reduced on continued and prolonged treatment (Hegen et al. 2012; Pungor et al. 1998; Rice et al. 1999). The generation of NAb, primarily of immunoglobulin (Ig)G isotype can cause life-threatening conditions as in the case of pure red cell aplasia by ADAs against erythropoietin (Casadevall et al. 2002) and thrombocytopenia by ADAs against thrombopoietin (Li et al. 2001). ADAs consist of low titre, transient IgM; high titre, persistent IgG (IgG1–IgG4) or IgE immunoglobulin isotypes (Baker et al. 2010; Baker and Jones 2007; Jefferis 2007; Singh 2011). Protein antigens predominantly trigger IgG1 and IgG3, whereas IgG2 antibodies are induced by carbohydrate-based antigens (Jefferis 2007). IgG4 is usually in response to chronic antigen stimulation (Jefferis 2007), and hence is commonly observed in response to long-term treatment with biologics. It is reported that the neutralizing property of IgG4 is higher compared to IgG1 and IgG2 ADA (Baker et al. 2010; Reding et al. 2002; Reding 2006). IgG-ADAs can also induce IgE-independent anaphylactic reactions (Finkelman 2007; Weber et al. 2002) and can include the activation of the complement system (Vultaggio et al. 2011). It is well known that IgE mediates lethal hypersensitivity reactions (Purcell and Lockey 2008). Despite the rarity of the incidence, IgE ADA-mediated anaphylactic response with recombinant human insulin (Chng et al. 1995; Kumar 1997) and various therapeutic mAbs (Stubenrauch et al. 2010; Vultaggio et al. 2010) clearly indicates its clinical significance. Previous exposure to substances within biologic formulations has also been reported to contribute to IgE-mediated immune reactions (Price and Hamilton 2007; Steele et al. 2005). IgM-based ADAs have also been reported with anti-TNFα mAbs (Vultaggio et al. 2010) and possibly during IFNα therapy (von Wussow et al. 1989). IgM antibodies are of low affinity, high avidity, transient, induced by multivalent antigens (Boyer et al. 1977; Minuk et al. 1983) and are capable of activating the complement system (Richard and Prang 2010). While the evidence regarding IgM-ADAs is rather limited, IgM antibodies against polyethylene glycol (PEG)—a multivalent modifying agent tagged to biologics to improve bioavailability has been reported (Richter and Akerblom 1984).
Immunological Processes that Underlie Development of ADAs
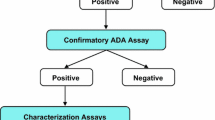
Anti-drug antibodies can be generated by both T cell-dependent (Td) and T cell-independent (Ti) pathways, which involves the production of antibodies by B cells with and without the assistance of T cells (De Groot and Scott 2007). In the Td pathway, T cells are activated by the recognition of the antigenic peptides derived from the biologic and presented by antigen-presenting cells (APCs) via the major histocompatibility complex (MHC) II complex. Activated T cells then stimulate B cells to generate antibodies against the biologic. An immune response to a biologic can involve rapid induction of a Td response leading to expansion of epitope-specific B cells (Bachmann et al. 1994). The Td pathway of antibody production results in a long lasting, high antibody titre response to foreign or exogenous therapeutic proteins. T cell subset polarization also determines therapeutic outcome to the ADA generated, where a Th2 response drives neutralizing IgG4 ADA compared to Th1 which mounts an IgG1 and IgG2-based ADA, which may in some instances be non-neutralizing in nature (Baker et al. 2010; Reding et al. 2002; Reding 2006).
The production of ADAs through the Ti pathway involves polyvalent antigens that bind to B cell receptors (BCRs) and induce receptor clustering (Vos et al. 2000). It is conceivable that an aggregated biologic that displays repeating epitopes can cluster BCRs, cause B cell activation and result in a Ti response (Batista and Harwood 2009; Depoil et al. 2009). Biologics can also be engulfed by blood-borne peripheral dendritic cells (DCs) which then migrate to the spleen. Here, these DCs present biologic-derived antigens to B cells in the splenic marginal zone (Balazs et al. 2002). Since, there is no T cell help in this mechanism, ADAs generated by this process will be of IgM isotype or low-affinity IgGs. The presence of additional signals either from danger signals (Toll-like receptors: TLRs) or antigen-specific T helper (Th) cells can lead to affinity maturation, class switching and a more potent IgG response (Bachmann and Zinkernagel 1997; Batista and Harwood 2009). This second signal or danger signal can be provided by impurities in the biologic formulations and inflammatory milieu associated with the disease condition. While each pathway is distinct, there is crosstalk or interactions between the pathways as illustrated in Fig. 1. Antigen laden marginal zone B cells (from the Ti pathway) can also function as APCs by presenting the biologic to T cells (Fehr et al. 1998), and is an example of how the Td and Ti pathways interact and synergise. Another event which can represent interaction between the pathways is B cell epitope spreading, which may play a role in the evolution of the specificity of the ADA during the treatment period. It is known that the presence of ADA-biologic immune complex (the ADAs generated from primary immune response to the biologic) can activate naive B cells to mount a secondary response (Goins et al. 2010). Improved uptake of the biologic by B cells due to the formation of ADA-biologic complex may induce potent Td antibody production directed against epitopes different from those of the primary response.
T cell-dependent and independent pathway involved in an immunogenic response. T cell-dependent pathway involves the uptake of biologics by antigen-presenting cells like immature dendritic cells (iDCs) and B cells. DCs process the biologic into peptides, mature and migrate to the T cell zone of the draining lymph nodes where they present the antigenic peptides to naive T cells expressing antigen-specific T cell receptors. This leads to T cell activation and proliferation. B cells can also take up biologic through their B cell receptor, process and present biologic-derived peptides to activated T cells that have migrated to the B cell zones. Activated T cells stimulate B cells resulting in the generation of antigen-specific antibody secreting plasma cells. T cell-independent pathway involves the direct stimulation of B cells by aggregated form of biologic. Marginal zone B cells can be stimulated by biologic bearing blood borne peripheral DCs. This pathway leads to generation of plasma cells that predominantly secrete IgM antibodies. Cross talk between these pathways contributes significantly towards the immunogenic response. ADA anti-drug antibodies, Ag antigen, bbDC – blood-borne peripheral dendritic cells, mDC mature dendritic cell, TCR T cell receptor, Th cell T helper cell, TLR Toll-like receptor
A body of evidence accrued over recent years has clearly implicated a variety of factors in ADA generation (either singly or in combination) and is listed in Table 3 (Kromminga and Schellekens 2005; Pichler 2006; Schellekens 2002). While it is generally accepted that the immune system selectively determines, predisposes and plays a pivotal role in initiating and propagating an immunogenic response to various biologics, the role of antigen processing and presentation processes as critical drivers of immunogenicity has not been fully appreciated and merits consideration.
Antigen Processing and Presentation as Key Events in Immunogenicity
Antigen processing and presentation of biologics are performed by professional APCs such as DCs, macrophages and B cells. Antigen processing and presentation involves two key events: (1) antigen capture that delivers antigens to the cellular antigen processing machinery and (2) antigen processing and presentation that generates antigenic peptides bound to MHC molecules for presentation to adaptive immune cells. The various factors associated with immunogenicity as listed in Table 3 could potentially exercise their influence by modulating antigen processing and presentation as shown schematically in Fig. 2.
Antigen processing and presentation central to immunogenic response. A variety of biologic-specific and patient-specific factors are associated with the onset and progression of immunogenicity to biologics. These factors exert their influence by modulating antigen processing and presentation events through altering antigen uptake, co-stimulatory molecule expression, maturation status and provision of immunogenic epitopes by APCs. APC antigen-presenting cell, HLA human leukocyte antigen
Antigen Uptake
The first step in antigen processing is the acquisition of extracellular antigens. APCs internalise antigen through phagocytosis, macropinocytosis and receptor-mediated endocytosis (Conner and Schmid 2003; Lanzavecchia 1990). Injection site of the biologic will determine the APC type that will be involved in antigen capture. Following subcutaneous injection of biologics, immature DCs in the epidermis phagocytose and process the protein via the MHC class II processing pathway. Antigens can be captured by a number of receptors such as Fc receptors (FcγR and FcεR), TLRs, members of the C-type lectin family (DEC-205, DCIR), Ig superfamily and heat shock protein receptors. The presence of pre-existing antibodies and circulating IgM or IgG facilitates uptake of therapeutic protein antigen by FcγRs. Furthermore, complement receptors might also enhance such endocytic processes (Bajtay et al. 2006). The binding of antibody–antigen complex to receptors on DCs or macrophages will also aid in antigen processing and presentation (Regnault et al. 1999). Engagement of receptors like TLRs enhance internalization of the complex thus facilitating antigen processing (Hayashi et al. 2001; Lankar et al. 2002). Formulation buffers can affect protein conformation of the biologic and thereby predisposing it to be internalised and processed by DCs (Jaber and Baker 2007; Jaber et al. 2007).
Physical modification/degradation including misfolding, unfolding, aggregation, oxidation and deamidation of biologics caused during purification, production, storage or formulation can predispose to immunogenic response by facilitating increased antigen uptake. It is clear that aggregates are a significant factor for immunogenic response as it is associated with increases in the incidence of immunogenicity (Antonelli and Dianzani 1999; Hermeling et al. 2004). This is probably due to their multiple epitopes attribute and/or changes to the structural conformation of the individual aggregated protein molecule (Kumar et al. 2011; Medzhitov and Janeway 2002; Rosenberg 2006; van Beers et al. 2010). The presence of antigenic epitopes in aggregates but not in monomer molecules (Kumar et al. 2011; Robbins et al. 1987) can directly stimulate B cells or can enhance its uptake by APCs (Jones et al. 2011). Aggregated biologics with multimeric structures can be also captured by blood-borne DCs and presented to marginal B cells (Fehr et al. 1997; Martin et al. 2001). Though the mechanism behind the predisposition of aggregated protein for capture is not completely defined, it is likely to be due to the presentation of B cell epitopes in a repetitive manner by the aggregated proteins. Aggregates could also induce immunogenicity through breaking existing immune tolerance towards monomeric version of the biologic (Braun et al. 1997; Moore and Leppert 1980). Oxidation contributes to immunogenicity by facilitating aggregate formation (Wang 2005). Several studies have shown that the oxidised form of the biologic was more immunogenic than non-oxidized form (Hochuli 1997; van Beers et al. 2011). The route of administration (in the case of an injected biologic) has been shown to have a profound effect on the onset of immunogenicity. Subcutaneous route was found to cause immunogenic response more frequently than other routes (Mohanan et al. 2010; Peng et al. 2009; Perini et al. 2001; Ross et al. 2000). Localization, prolonged presence, increased concentration and proximity to APCs when the biologic is delivered by the subcutaneous route could enable enhanced capture, processing and presentation of biologic-derived antigens by APCs thus leading to immunogenicity.
Antigen Processing and Presentation
Antigen uptake is followed by antigen processing and the formation of peptide–MHC complexes. Antigens that have been captured and internalised are trafficked into endosomal compartments, and processed into peptides and are presented by APCs for T cell recognition. Based on studies in vaccine technology, it is emerging that aggregated forms of antigens can increase antigen processing thereby contributing to a more potent immunogenic response (Jones et al. 2011). The quality of the antigen presentation depends on the quality of the peptide-MHC complexes and there is a direct relationship between peptide-MHC complex stability and the immunogenic response (Lazarski et al. 2005). Human leukocyte antigen (HLA) haplotype and T cell epitopes are among the major contributors towards an immunogenic response against biologics. Specific HLA types have been found to be implicated in an ADA immunogenic response to biologics as listed in Table 4 (Barbosa et al. 2006; Buck et al. 2011; Ettinger et al. 2010; Hay et al. 1997; Hoffmann et al. 2008; Ohta et al. 1999; Praditpornsilpa et al. 2009; Simonney et al. 1985; Stickler et al. 2004). This suggests that there may be particular MHCs that are more able to complex with biologic-derived antigenic peptides. The contribution by the T cell epitopes within the biologic is equally pivotal to the immunogenic response. T cell epitope profiling studies have identified specific sequences of amino acids in various biologics which contribute towards immunogenicity (Jones et al. 2005; Parker et al. 2011; Stickler et al. 2004; van Haren et al. 2011). Hence, the potency of the peptide-MHC II complex on the surface of the APC to activate the T cells to initiate an immunogenic response is determined by a combination of the type of HLA and a compatible antigenic peptide that provides the T cell epitope.
Antigen presentation to initiate a T cell response by APCs is influenced by external stimuli and signals. Immature DCs which are highly endocytic but not very efficient at processing and presenting antigens undergo a maturation process in response to external signals or “danger signals” like TLR ligands (LPS, CPG motifs), inflammatory cytokines and complement (De Smedt et al. 1996; Sparwasser et al. 1998). These signals increase their efficiency for sustained processing and presentation of antigens. APCs activate naïve T cells by the recognition of antigenic peptide:MHC class II complex on their cell surface by T cell receptors and by the ligation of co-stimulatory receptor, CD28 on the T cell surface to the B7 co-stimulatory molecule on the APCs. The expression of co-stimulatory molecules on APCs can be induced by various factors present in the formulation (like excipients) of the biologics. Degradation products of excipients present in the formulation can increase co-stimulatory molecule expression on the surface of DCs (Mueller et al. 2009). The presence of reactive oxygen species either due to degradation products in the formulation or disease-associated inflammation can also provide the danger signals and up-regulate co-stimulatory molecules on the DCs (Rutault et al. 1999). Patients being treated with a biologic for immune disorders like autoimmunity or inflammatory disorder may be prone for developing immunogenicity. Increased expression of co-stimulatory molecules on APCs in patients with immune-mediated diseases may underlie such a predisposition (Anderson 2005). Altered co-stimulatory molecule expression and function of APCs have been reported in the elderly and hence, an immunogenic response towards the biologic might vary with age (Guy 2010; Pereira et al. 2011; Rafi et al. 2003; Shurin et al. 2007).
Break in Tolerance Underlies Immunogenicity
Tolerance is a mechanism by which immune cells are prevented from mounting a response against self antigens. Response against biologics which are considered to be similar to their endogenous counterparts could be due to the breaking of such immune tolerance. The presence of impurities such as endotoxins or microbial DNA in the biologic may act as danger signals and activate autoreactive B cells to self-antigens. The presence of foreign T cell epitopes coupled with self-antigens can also break tolerance towards the self antigen. Another important mode by which tolerance is broken is by repeated presentation of self-antigens (Chackerian et al. 2002) as is the case during biologic therapy. Aggregated antigens are also efficient in activating anergic B cells on repeated exposure (Kromminga and Schellekens 2005). In vivo experiments in transgenic mouse models have also indicated that the immunogenic response to aggregated proteins is due to the breaking of tolerance (Braun et al. 1997).
Does Complement Play a Role in Processing and Presentation of Biologic-Derived Antigens?
Complement—a group of plasma proteins can be activated by three pathways—classical, alternative and lectin pathways. Immune complexes are known to activate complement by the classical pathway. One of the primary effector responses following complement activation is the mediation of adaptive immune responses by anaphylatoxins (C3a and C5a). Activation of complement could occur as a result of the characteristics of the biologic such as the structure, aggregation ability and impurities in the formulation and the isotypes of the therapeutic antibody. Since, antibody–antigen complexes are known to activate the complement system by the classical pathway; the presence of ADA-biologic immune complexes may also activate complement pathways. Of all the immunoglobulins, only IgM and IgG can activate complement (Bindon et al. 1988). Immune complexes consisting of pentameric IgM are potent activators of complement and even low levels of IgM—as would be in the case of patients receiving their first doses of biologic—can bind to aggregated biologic and trigger complement activation. Of the IgG subclasses, IgG1 and IgG3 are potent activators of complement whereas IgG2 and IgG4 are weak activators (Bindon et al. 1988; Woof and Burton 2004). However, the presence of IgG4 along with IgG1 was reported to have amplified the immune complex-mediated complement activation response (Bergamaschini et al. 1996). IgG3 complexes can also activate complement potently by binding to C1q following spontaneous multimerization (Greenspan and Cooper 1992). Due to the potency of these isotypes, suboptimal levels of the biologic-immune complex aggregate can be sufficient to activate complement system. As ADAs are predominantly of the IgG isotype, it becomes increasingly relevant to explore the role of ADA immune complex-mediated complement activation and the role of the complement in the onset and propagation of immunogenicity. Our preliminary results suggest that such ADA-biologic immune complexes induce complement activation (manuscript in preparation). The presence of impurities of bacterial origin in the biologic can also activate complement system via the alternative pathway.
Activated complement factors such as C3a, C5a and C3d are potent factors that influence antibody responses by modulating DC, T cell and B cell function. APCs express a wide range of complement receptors, complement-regulatory proteins and complement are essential for optimal maturation and T cell activation by APCs (Hashimoto et al. 2010; Kerekes et al. 2001; Weaver et al. 2010; Zhou et al. 2006). Cyclic adenosine monophosphate production which is important for DC maturation, antigen presentation and cytokine synthesis is mediated by C3aR activation (Li et al. 2008). Complement also influences T cell responses by direct or indirect modulation of Th1/Th2 immunity (Kemper and Atkinson 2007). Local constitutive production of complement and its activated components are necessary for T cell viability, generation of IL-2 and for antigen-specific T cell priming (Kopf et al. 2002; Lalli et al. 2008; Strainic et al. 2008). Activated complement also has an immunomodulatory role in B cells by mediating antigen retention for B cell activation, antibody production and memory B cell formation (Carroll 2004; Fischer and Hugli 1997; Fleming et al. 2002; Ottonello et al. 1999; Reid et al. 2002). Complement system has also been implicated in the resolution of an immune response to prevent tissue damage and autoimmunity, and its role in T regulatory cells (Tregs) has also been described (O’Garra and Vieira 2004) further reiterating the potential role of complement in breaking tolerance. Owing to its multiple roles in adaptive immune response, it would be necessary to define the contribution of complement to the development of high affinity ADAs.
Predicting Immunogenicity by Exploring Factors Influencing Antigen Processing and Presentation
Characterisation and screening for physico-chemical determinants or formulation-based factors like impurities, heterogeneity, aggregate formation, oxidation and deamidation in the biologics will aid both in the prediction of immunogenicity and in the development of less immunogenic therapeutic agents. Moreover, predicting potential immunogenic epitopes in biologics will be an important and effective strategy to improve their safety and efficacy. A variety of preclinical immunogenicity screening strategies are being used during biologic development as listed in Table 5.
It is now well established that T cell epitopes within the protein sequence of the biologics contribute towards immunogenicity. Therefore, predicting the potential immunogenic T cell epitopes will lead to reductions in the incidence of immunogenicity. Prediction strategies used for designing effective vaccines and determining T cell epitopes in autoimmunity (De Groot and Berzofsky 2004; Inaba et al. 2006; Khan et al. 2006) can be adopted to predict immunogenicity to biologics. Screening for T cell epitopes in biologics early in drug development is being increasingly used by the pharmaceutical industry. A variety of in silico methods or computational tools to identify potential T cell epitopes within the biologic that have a higher propensity to bind to particular HLAs are being developed (De Groot and Moise 2007; De Groot and Martin 2009; Koren et al. 2007). An extensive discussion by Lafuente and Reche (2009) on various strategies practised in the prediction of peptide-MHC interaction clearly showcases the importance of T cell epitope mapping in predicting immunogenicity. Recently, a screening strategy aimed at harnessing the concept of neutral drift also shows promise for improved T cell epitope prediction (Cantor et al. 2011). A potential limitation of in silico prediction of immunogenic T cell epitopes is the lack of input from aspects of APC function such as antigen processing and eventual presentation of biologic-derived peptides to T cells. Therefore, in vitro/ex vivo assays with primary human cells that can integrate both APC function and T cell responses may uncover immunogenic epitopes more accurately and will be most relevant in predicting immunogenicity to biologics in humans. It is therefore crucial to integrate in silico predictive tools with in vitro and ex vivo testing using T cells and APCs from both primed and non-primed individuals across relevant MHC-II allotype cohorts to identify biologically meaningful epitopes and thereby improving prediction of immunogenicity to biologics.
Prediction of B cell epitopes has been very useful in the success of vaccine technology. This can be harnessed to identify B cell epitopes of biologics that represent targets for ADA. There are two types of B cell epitopes, linear and conformational. The latter type is of greater relevance constituting the majority of the B cell epitopes. Conformational epitopes consist of amino acids that are not contiguous in primary sequence, but are arranged together as an epitope by proximity arising through secondary/tertiary protein structure. In silico tools to predict B cell antigenic epitopes are available but are currently underexploited in immunogenicity prediction (El-Manzalawy et al. 2008; Kulkarni-Kale et al. 2005; Larsen et al. 2006; Saha et al. 2005; Schreiber et al. 2005; Sollner et al. 2008; Wang et al. 2011). Furthermore, antibody-specific epitope prediction methods with improved accuracy and biological relevance are becoming available (Zhao et al. 2011). A detailed report by El-Manzalawy and Honavar (2010) on B cell epitope prediction methods describes the technical nuances involved in this technology aimed at reducing immunogenic response to biologics.
HLA binding assay is another reliable in vitro validation system for predicting immunogenic epitopes as there is a close association between HLA binding and immunogenic profiles (McMurry et al. 2005). This assay uses peptides from biologics to measure the binding affinity of epitopes to the various MHC II molecules (McMurry et al. 2007; Reijonen et al. 2002; Steere et al. 2006). The predicted epitopes can also be validated by measuring T cell responses, especially when blood samples are available from patients already exposed to the biologic (Barbosa et al. 2006; Hobeika et al. 2005; Jaber and Baker 2007; Kamate et al. 2007).
Reducing Immunogenicity: Intervening in Antigen Processing and Presentation
A variety of strategies designed to reduce immunogenicity have been tested and are listed in Table 5. Humanization is a process by which biologics of non-human origin are re-engineered to minimize the non-human component which can reduce immunogenicity. Modifications in the amino acid sequence of protein, and changes to the constant and variable regions of therapeutic antibodies have led to a marked decrease in the immunogenicity of biologics. The development of chimeric and humanized antibodies has helped in achieving decreased immunogenicity. The need to eliminate physico-chemical determinants that favour immunogenicity is extensively discussed in a recent review (Singh 2011). Deimmunization by depletion of potential immunogenic T cell epitopes through protein sequence modification is another effective strategy in reducing immunogenicity (De Groot et al. 2005; Hay et al. 2006a; Parker et al. 2011; Tangri et al. 2005; Yeung et al. 2004). This technique led to the development of many deimmunized biologics, especially mAbs which are in various stages of clinical trials with encouraging results. However, caution needs to be exercised in using this strategy as it could lead to the generation of new potentially immunogenic epitopes. Recently, a report utilizing a strategy with improved prediction methods along with saturation mutagenesis was able to achieve protein sequences with decreased MHC II binding without compromising the function of the biologics (Cantor et al. 2011) represents a way forward in achieving improved safety in biologics. T cell epitopes associated with Tregs termed Tregitopes are being explored as a potential strategy to suppress immunogenicity (De Groot et al. 2008; De Groot and Martin 2009). Ex vivo and in vivo experiments using peptides with Tregitopes decreased the resulting immunogenic response to antigens (De Groot et al. 2008). Inclusion of Tregitopes can induce natural Tregs into a suppressive immune response to the biologic. This strategy paves a way for the generation of biologics with a less immunogenic adverse response. However, differentiating epitopes that are specific for Tregs from T helper cell epitopes may pose a significant hurdle and extensive studies in this developing area is warranted. Induction of tolerance can be another strategy to minimise immunogenicity. Administration of high concentration of biologics (antibodies), use of alternative routes like via the mucosal surfaces rather than subcutaneous route can decrease immunogenicity by the induction of peripheral tolerance through tolerizing DCs and expanding Tregs (Meritet et al. 2001a, b; Nagler-Anderson et al. 2001).
PEGylation and glycosylation are the two most common forms of modifications incorporated into the structure of biologics to reduce immunogenicity and improve therapeutic efficacy. The immunogenicity of large molecules like biologics can be minimized by modifying the therapeutic agent with PEG polymers. It is known that covalent attachment of PEG to biologics can reduce immunogenicity by interfering with processing and presentation and by masking immunogenic epitopes (Basu et al. 2006). Though PEG is generally non-immunogenic, there are reports which suggest that this is not always the case (Singh 2011). Anti-PEG antibodies have been detected in patients treated with PEGylated therapeutic enzymes (Armstrong et al. 2007; Ganson et al. 2006) and indicate the need to investigate the immunogenic mechanism triggered by PEG. There is growing evidence that such modification of biologics does not decrease the immunogenic potential (Jevsevar et al. 2010). Glycosylation is the most common form of post translation modification seen in half of all human proteins. Glycosylation of selective amino acid residues of the biologic interferes with MHC II restricted T cell recognition and through disrupting antigen processing by APCs (von Delwig et al. 2006). However, it can possibly increase immunogenicity by the generation of neopeptides as well (Singh 2011). There is a clear need for more detailed studies to validate these strategies and to develop new approaches that can target antigen processing/presentation for reduction of immunogenicity.
Concluding Remarks
The problem of immunogenicity has been under intense study but the contribution of antigen processing and presentation processes has not received enough attention. It is becoming clear that many of biologic-specific and patient-specific characteristics that are associated with higher incidence of immunogenicity have an impact on antigen processing and presentation mechanisms. Factors such as aggregate formation (either in vivo or in the formulation) or the presence of adjuvants in the formulation can enhance antigen capture, APC activation and lead to breaking of immune tolerance. The role of complement in augmenting or modulating immunogenicity through its effects on antigen processing is unexplored and merits detailed investigation. Much progress has been made in predicting and eliminating immunogenic epitopes contained within biologics. However, identifying factors that influence the processing and presentation of biologic-derived antigens including complement may offer additional options for intervention in the immunogenic process and consequently in the management of immunogenicity to biologics.
Abbreviations
- ADA:
-
Anti-drug antibody
- APC:
-
Antigen-presenting cells
- BAb:
-
Binding antibody
- BCR:
-
B cell receptor
- BMP7:
-
Bone morphogenetic protein-7
- C1q:
-
Complement component 1q
- C3a:
-
Complement factor 3a
- C3aR:
-
Complement 3a receptor
- C3d:
-
Complement factor 3d
- C5a:
-
Complement factor 5a
- CD:
-
Cluster of differentiation
- CpG:
-
Deoxy-cytidylate-phosphate-deoxy-guanylate
- DCs:
-
Dendritic cells
- EGFR:
-
Epidermal growth factor receptor
- FcγR:
-
Fc gamma receptor
- GH:
-
Growth hormone
- GHRH:
-
Growth-hormone-releasing hormone
- GM-CSF:
-
Granulocyte macrophage colony stimulating factor
- GnRH:
-
Gonadotrophin-releasing hormone
- HIV:
-
Human immunodeficiency virus
- HLA:
-
Human leukocyte antigen
- HPV:
-
Human papilloma virus
- IFN:
-
Interferon
- Ig:
-
Immunoglobulin
- IL:
-
Interleukin
- LFA:
-
Lymphocyte function-associated antigen
- LPS:
-
Lipopolysaccharides
- mAb:
-
Monoclonal antibody
- MHC:
-
Major histocompatibility complex
- NAb:
-
Neutralizing antibody
- PDGF:
-
Platelet-derived growth factor
- PEG:
-
Polyethylene glycol
- PSA:
-
Prostate-specific antigen
- Rh:
-
Rhesus factor
- Td:
-
T cell-dependent
- Th:
-
T helper cells
- Ti:
-
T cell-independent
- TAG-72:
-
Tumor-associated glycoprotein 72
- TLR:
-
Toll-like receptor
- TNFα:
-
Tumor necrosis factor alpha
- Tregs:
-
T regulatory cells
- VEGF:
-
Vascular endothelial growth factor
References
Aarskog NK, Maroy T, Myhr KM et al (2009) Antibodies against interferon-beta in multiple sclerosis. J Neuroimmunol 212:148–150
Anderson PJ (2005) Tumor necrosis factor inhibitors: clinical implications of their different immunogenicity profiles. Semin Arthritis Rheum 34(5 Suppl 1):19–22
Antonelli G, Dianzani F (1999) Development of antibodies to interferon beta in patients: technical and biological aspects. Eur Cytokine Netw 10:413–322
Armstrong JK, Hempel G, Koling S et al (2007) Antibody against poly(ethylene glycol) adversely affects PEG-asparaginase therapy in acute lymphoblastic leukemia patients. Cancer 110:103–111
Bachmann MF, Zinkernagel RM (1997) Neutralizing antiviral B cell responses. Annu Rev Immunol 15:235–270
Bachmann MF, Kundig TM, Kalberer CP et al (1994) How many specific B cells are needed to protect against a virus? J Immunol 152:4235–4241
Bajtay Z, Csomor E, Sandor N et al (2006) Expression and role of Fc- and complement-receptors on human dendritic cells. Immunol Lett 104:46–52
Baker MP, Jones TD (2007) Identification and removal of immunogenicity in therapeutic proteins. Curr Opin Drug Discov Devel 10:219–227
Baker MP, Reynolds HM, Lumicisi B et al (2010) Immunogenicity of protein therapeutics: the key causes, consequences and challenges. Self Nonself 1:314–322
Balazs M, Martin F, Zhou T et al (2002) Blood dendritic cells interact with splenic marginal zone B cells to initiate T-independent immune responses. Immunity 17:341–352
Barbosa MD, Vielmetter J, Chu S et al (2006) Clinical link between MHC class II haplotype and interferon-beta (IFN-beta) immunogenicity. Clin Immunol 118:42–50
Basu A, Yang K, Wang M et al (2006) Structure-function engineering of interferon-beta-1b for improving stability, solubility, potency, immunogenicity, and pharmacokinetic properties by site-selective mono-PEGylation. Bioconjug Chem 17:618–630
Batista FD, Harwood NE (2009) The who, how and where of antigen presentation to B cells. Nat Rev Immunol 9:15–27
Bellomi F, Scagnolari C, Tomassini V et al (2003) Fate of neutralizing and binding antibodies to IFN beta in MS patients treated with IFN beta for 6 years. J Neurol Sci 215:3–8
Bergamaschini L, Santangelo T, Faricciotti A et al (1996) Study of complement-mediated anaphylaxis in humans. The role of IgG subclasses (IgG1 and/or IgG4) in the complement-activating capacity of immune complexes. J Immunol 156:1256–1261
Bertolotto A, Malucchi S, Sala A et al (2002) Differential effects of three interferon betas on neutralising antibodies in patients with multiple sclerosis: a follow up study in an independent laboratory. J Neurol Neurosurg Psychiatry 73:148–153
Bertolotto A, Sala A, Malucchi S et al (2004) Biological activity of interferon betas in patients with multiple sclerosis is affected by treatment regimen and neutralising antibodies. J Neurol Neurosurg Psychiatry 75:1294–1299
Bindon CI, Hale G, Bruggemann M et al (1988) Human monoclonal IgG isotypes differ in complement activating function at the level of C4 as well as C1q. J Exp Med 168:127–142
Bongartz T, Sutton AJ, Sweeting MJ et al (2006) Anti-TNF antibody therapy in rheumatoid arthritis and the risk of serious infections and malignancies: systematic review and meta-analysis of rare harmful effects in randomized controlled trials. JAMA 295:2275–2285
Boyer KM, Cherry JD, Noble GR (1977) IgM and IgG antibody responses following immunization of children and adults with influenza A/NJ/76 vaccines. Dev Biol Stand 39:303–308
Braun A, Kwee L, Labow MA et al (1997) Protein aggregates seem to play a key role among the parameters influencing the antigenicity of interferon alpha (IFN-alpha) in normal and transgenic mice. Pharm Res 14:1472–1478
Buck D, Cepok S, Hoffmann S et al (2011) Influence of the HLA-DRB1 genotype on antibody development to interferon beta in multiple sclerosis. Arch Neurol 68:480–487
Cantor JR, Yoo TH, Dixit A et al (2011) Therapeutic enzyme deimmunization by combinatorial T-cell epitope removal using neutral drift. Proc Natl Acad Sci USA 108:1272–1277
Carroll MC (2004) The complement system in B cell regulation. Mol Immunol 41:141–146
Casadevall N, Nataf J, Viron B et al (2002) Pure red-cell aplasia and antierythropoietin antibodies in patients treated with recombinant erythropoietin. N Engl J Med 346:469–475
Chackerian B, Lenz P, Lowy DR et al (2002) Determinants of autoantibody induction by conjugated papillomavirus virus-like particles. J Immunol 169:6120–6126
Chng HH, Leong KP, Loh KC (1995) Primary systemic allergy to human insulin: recurrence of generalized urticaria after successful desensitization. Allergy 50:984–987
Clarke JB (2010) Mechanisms of adverse drug reactions to biologics. In Uetrecht J (ed) Adverse drug reactions. Springer, Berlin, pp 454–472
Conner SD, Schmid SL (2003) Regulated portals of entry into the cell. Nature 422:37–44
Corona T, Leon C, Ostrosky-Zeichner L (1999) Severe anaphylaxis with recombinant interferon beta. Neurology 52:425
De Groot AS, Berzofsky JA (2004) From genome to vaccine–new immunoinformatics tools for vaccine design. Methods 34:425–428
De Groot AS, Martin W (2009) Reducing risk, improving outcomes: bioengineering less immunogenic protein therapeutics. Clin Immunol 131:189–201
De Groot AS, Moise L (2007) Prediction of immunogenicity for therapeutic proteins: state of the art. Curr Opin Drug Discov Devel 10:332–340
De Groot AS, Scott DW (2007) Immunogenicity of protein therapeutics. Trends Immunol 28:482–490
De Groot AS, Knopp PM, Martin W (2005) De-immunization of therapeutic proteins by T-cell epitope modification. Dev Biol 122:171–194
De Groot AS, Moise L, McMurry JA et al (2008) Activation of natural regulatory T cells by IgG Fc-derived peptide “Tregitopes”. Blood 112:3303–3311
De Smedt T, Pajak B, Muraille E et al (1996) Regulation of dendritic cell numbers and maturation by lipopolysaccharide in vivo. J Exp Med 184:1413–1424
Depoil D, Weber M, Treanor B et al (2009) Early events of B cell activation by antigen. Sci Signal 2:pt1
DiMasi JA, Feldman L, Seckler A et al (2010) Trends in risks associated with new drug development: success rates for investigational drugs. Clin Pharmacol Ther 87:272–277
El-Manzalawy Y, Honavar V (2010) Recent advances in B-cell epitope prediction methods. Immunome Res 6(Suppl 2):S2
El-Manzalawy Y, Dobbs D, Honavar V (2008) Predicting linear B-cell epitopes using string kernels. J Mol Recognit 21:243–255
Ettinger RA, James EA, Kwok WW et al (2010) HLA-DR-restricted T-cell responses to factor VIII epitopes in a mild haemophilia A family with missense substitution A2201P. Haemophilia 16:44–55
Fehr T, Bachmann MF, Bucher E et al (1997) Role of repetitive antigen patterns for induction of antibodies against antibodies. J Exp Med 185:1785–1792
Fehr T, Naim HY, Bachmann MF et al (1998) T-cell independent IgM and enduring protective IgG antibodies induced by chimeric measles viruses. Nat Med 4:945–948
Finkelman FD (2007) Anaphylaxis: lessons from mouse models. J Allergy Clin Immunol 120:506–515
Fischer WH, Hugli TE (1997) Regulation of B cell functions by C3a and C3a(desArg): suppression of TNF-alpha, IL-6, and the polyclonal immune response. J Immunol 159:4279–4286
Fleming SD, Shea-Donohue T, Guthridge JM et al (2002) Mice deficient in complement receptors 1 and 2 lack a tissue injury-inducing subset of the natural antibody repertoire. J Immunol 169:2126–2133
Ganson NJ, Kelly SJ, Scarlett E et al (2006) Control of hyperuricemia in subjects with refractory gout, and induction of antibody against poly(ethylene glycol) (PEG), in a phase I trial of subcutaneous PEGylated urate oxidase. Arthritis Res Ther 8:R12
Giezen TJ, Mantel-Teeuwisse AK, Straus SM et al (2008) Safety-related regulatory actions for biologicals approved in the United States and the European Union. JAMA 300:1887–1896
Goins CL, Chappell CP, Shashidharamurthy R et al (2010) Immune complex-mediated enhancement of secondary antibody responses. J Immunol 184:6293–6298
Goodnow CC (2001) Pathways for self-tolerance and the treatment of autoimmune diseases. Lancet 357:2115–2121
Greenspan NS, Cooper LJ (1992) Intermolecular cooperativity: a clue to why mice have IgG3? Immunol Today 13:164–168
Guy B (2010) Strategies to improve the effect of vaccination in the elderly: the vaccine producer’s perspective. J Comp Pathol 142(Suppl 1):S133–S137
Hashimoto M, Hirota K, Yoshitomi H et al (2010) Complement drives Th17 cell differentiation and triggers autoimmune arthritis. J Exp Med 207:1135–1143
Hay CR, Ollier W, Pepper L et al (1997) HLA class II profile: a weak determinant of factor VIII inhibitor development in severe haemophilia A UKHCDO Inhibitor Working Party. Thromb Haemost 77:234–237
Hay C, Recht M, Carcao M et al (2006a) Current and future approaches to inhibitor management and aversion. Semin Thromb Hemost 32(Suppl 2):15–21
Hay CR, Brown S, Collins PW et al (2006b) The diagnosis and management of factor VIII and IX inhibitors: a guideline from the United Kingdom Haemophilia Centre Doctors Organisation. Br J Haematol 133:591–605
Hayashi F, Smith KD, Ozinsky A et al (2001) The innate immune response to bacterial flagellin is mediated by Toll-like receptor 5. Nature 410:1099–1103
Hegen H, Schleiser M, Gneiss C et al (2012) Persistency of neutralizing antibodies depends on titer and interferon-beta preparation. Mult Scler 18:610–615
Hermeling S, Crommelin DJ, Schellekens H et al (2004) Structure-immunogenicity relationships of therapeutic proteins. Pharm Res 21:897–903
Hirsch IB (2005) Insulin analogues. N Engl J Med 352:174–183
Hobeika AC, Morse MA, Osada T et al (2005) Enumerating antigen-specific T-cell responses in peripheral blood: a comparison of peptide MHC Tetramer, ELISpot, and intracellular cytokine analysis. J Immunother 28:63–72
Hochuli E (1997) Interferon immunogenicity: technical evaluation of interferon-alpha 2a. J Interferon Cytokine Res 17(Suppl 1):S15–S21
Hoffmann S, Cepok S, Grummel V et al (2008) HLA-DRB1*0401 and HLA-DRB1*0408 are strongly associated with the development of antibodies against interferon-beta therapy in multiple sclerosis. Am J Hum Genet 83:219–227
Inaba H, Martin W, De Groot AS et al (2006) Thyrotropin receptor epitopes and their relation to histocompatibility leukocyte antigen-DR molecules in Graves’ disease. J Clin Endocrinol Metab 91:2286–2294
Jaber A, Baker M (2007) Assessment of the immunogenicity of different interferon beta-1a formulations using ex vivo T-cell assays. J Pharm Biomed Anal 43:1256–1261
Jaber A, Driebergen R, Giovannoni G et al (2007) The Rebif new formulation story: it’s not trials and error. Drugs R D 8:335–348
Janson ET, Ronnblom L, Ahlstrom H et al (1992) Treatment with alpha-interferon versus alpha-interferon in combination with streptozocin and doxorubicin in patients with malignant carcinoid tumors: a randomized trial. Ann Oncol 3:635–638
Jefferis R (2007) Antibody therapeutics: isotype and glycoform selection. Expert Opin Biol Ther 7:1401–1413
Jevsevar S, Kunstelj M, Porekar VG (2010) PEGylation of therapeutic proteins. Biotechnol J 5:113–128
Jones TD, Phillips WJ, Smith BJ et al (2005) Identification and removal of a promiscuous CD4 + T cell epitope from the C1 domain of factor VIII. J Thromb Haemost 3:991–1000
Jones JC, Settles EW, Brandt CR et al (2011) Virus aggregating peptide enhances the cell-mediated response to influenza virus vaccine. Vaccine 29:7696–7703
Kamate C, Lenting PJ, van den Berg HM et al (2007) Depletion of CD4+/CD25high regulatory T cells may enhance or uncover factor VIII-specific T-cell responses in healthy individuals. J Thromb Haemost 5:611–613
Kemper C, Atkinson JP (2007) T-cell regulation: with complements from innate immunity. Nat Rev Immunol 7:9–18
Kerekes K, Cooper PD, Prechl J et al (2001) Adjuvant effect of gamma-inulin is mediated by C3 fragments deposited on antigen-presenting cells. J Leukoc Biol 69:69–74
Khan AM, Miotto O, Heiny AT et al (2006) A systematic bioinformatics approach for selection of epitope-based vaccine targets. Cell Immunol 244:141–147
Kivisakk P, Alm GV, Fredrikson S et al (2000) Neutralizing and binding anti-interferon-beta (IFN-beta) antibodies. A comparison between IFN-beta-1a and IFN-beta-1b treatment in multiple sclerosis. Eur J Neurol 7:27–34
Kopf M, Abel B, Gallimore A et al (2002) Complement component C3 promotes T-cell priming and lung migration to control acute influenza virus infection. Nat Med 8:373–378
Koren E, De Groot AS, Jawa V et al (2007) Clinical validation of the “in silico” prediction of immunogenicity of a human recombinant therapeutic protein. Clin Immunol 124:26–32
Kromminga A, Schellekens H (2005) Antibodies against erythropoietin and other protein-based therapeutics: an overview. Ann N Y Acad Sci 1050:257–265
Kulkarni-Kale U, Bhosle S, Kolaskar AS (2005) CEP: a conformational epitope prediction server. Nucleic Acids Res 33(Web Server issue):W168–171
Kumar D (1997) Lispro analog for treatment of generalized allergy to human insulin. Diabetes Care 20:1357–1359
Kumar S, Singh SK, Wang X et al (2011) Coupling of aggregation and immunogenicity in biotherapeutics: T- and B-cell immune epitopes may contain aggregation-prone regions. Pharm Res 28:949–961
L Revers EF (2010) An introduction to biologics and biosimilars. Part I: Biologics: what are they and where do they come from? Can Pharmacists J 143:134–139
Lafuente EM, Reche PA (2009) Prediction of MHC-peptide binding: a systematic and comprehensive overview. Curr Pharm Des 15:3209–3220
Lalli PN, Strainic MG, Yang M et al (2008) Locally produced C5a binds to T cell-expressed C5aR to enhance effector T-cell expansion by limiting antigen-induced apoptosis. Blood 112:1759–1766
Lankar D, Vincent-Schneider H, Briken V et al (2002) Dynamics of major histocompatibility complex class II compartments during B cell receptor-mediated cell activation. J Exp Med 195:461–472
Lanzavecchia A (1990) Receptor-mediated antigen uptake and its effect on antigen presentation to class II-restricted T lymphocytes. Annu Rev Immunol 8:773–793
Larsen JE, Lund O, Nielsen M (2006) Improved method for predicting linear B-cell epitopes. Immunome Res 2:2
Lazarski CA, Chaves FA, Jenks SA et al (2005) The kinetic stability of MHC class II:peptide complexes is a key parameter that dictates immunodominance. Immunity 23:29–40
Leader B, Baca QJ, Golan DE (2008) Protein therapeutics: a summary and pharmacological classification. Nat Rev Drug Discov 7:21–39
Li J, Yang C, Xia Y et al (2001) Thrombocytopenia caused by the development of antibodies to thrombopoietin. Blood 98:3241–3248
Li K, Anderson KJ, Peng Q et al (2008) Cyclic AMP plays a critical role in C3a-receptor-mediated regulation of dendritic cells in antigen uptake and T-cell stimulation. Blood 112:5084–5094
Martin F, Oliver AM, Kearney JF (2001) Marginal zone and B1 B cells unite in the early response against T-independent blood-borne particulate antigens. Immunity 14:617–629
McMurry J, Sbai H, Gennaro ML et al (2005) Analyzing Mycobacterium tuberculosis roteomes for candidate vaccine epitopes. Tuberculosis 85:95–105
McMurry JA, Gregory SH, Moise L et al (2007) Diversity of Francisella tularensis Schu4 antigens recognized by T lymphocytes after natural infections in humans: identification of candidate epitopes for inclusion in a rationally designed tularemia vaccine. Vaccine 25:3179–3191
Medzhitov R, Janeway CA Jr (2002) Decoding the patterns of self and nonself by the innate immune system. Science 296:298–300
Meritet JF, Maury C, Tovey MG (2001a) Effect of oromucosal administration of IFN-alpha on allergic sensitization and the hypersensitive inflammatory response in animals sensitized to ragweed pollen. J Interferon Cytokine Res 21:583–593
Meritet JF, Maury C, Tovey MG (2001b) Induction of tolerance to recombinant therapeutic proteins. J Interferon Cytokine Res 21:1031–1038
Minuk GY, Hoofnagle JH, McAuliffe VJ et al (1983) IgM antibody responses to hepatitis B surface antigen in recipients of hepatitis B virus vaccine. J Infect Dis 148:330
Mohanan D, Slutter B, Henriksen-Lacey M et al (2010) Administration routes affect the quality of immune responses: a cross-sectional evaluation of particulate antigen-delivery systems. J Control Release 147:342–349
Moore WV, Leppert P (1980) Role of aggregated human growth hormone (hGH) in development of antibodies to hGH. J Clin Endocrinol Metab 51:691–697
Mueller R, Karle A, Vogt A et al (2009) Evaluation of the immuno-stimulatory potential of stopper extractables and leachables by using dendritic cells as readout. J Pharm Sci 98:3548–3561
Nagler-Anderson C, Terhoust C, Bhan AK et al (2001) Mucosal antigen presentation and the control of tolerance and immunity. Trends Immunol 22:120–122
O’Garra A, Vieira P (2004) Regulatory T cells and mechanisms of immune system control. Nat Med 10:801–805
Ohta H, Takahashi I, Kojima T et al (1999) Histocompatibility antigens and alleles in Japanese haemophilia A patients with or without factor VIII antibodies. Tissue Antigens 54:91–97
Ottonello L, Corcione A, Tortolina G et al (1999) rC5a directs the in vitro migration of human memory and naive tonsillar B lymphocytes: implications for B cell trafficking in secondary lymphoid tissues. J Immunol 162:6510–6517
Parker AS, Griswold KE, Bailey-Kellogg C (2011) Optimization of therapeutic proteins to delete T-cell epitopes while maintaining beneficial residue interactions. J Bioinform Comput Biol 9:207–229
Pedotti R, Mitchell D, Wedemeyer J et al (2001) An unexpected version of horror autotoxicus: anaphylactic shock to a self-peptide. Nat Immunol 2:216–222
Peng A, Gaitonde P, Kosloski MP et al (2009) Effect of route of administration of human recombinant factor VIII on its immunogenicity in Hemophilia A mice. J Pharm Sci 98:4480–4484
Pereira LF, de Souza AP, Borges TJ et al (2011) Impaired in vivo CD4 + T cell expansion and differentiation in aged mice is not solely due to T cell defects: decreased stimulation by aged dendritic cells. Mech Ageing Dev 132:187–194
Perini P, Facchinetti A, Bulian P et al (2001) Interferon-beta (INF-beta) antibodies in interferon-beta1a- and interferon-beta1b-treated multiple sclerosis patients. Prevalence, kinetics, cross-reactivity, and factors enhancing interferon-beta immunogenicity in vivo. Eur Cytokine Netw 12:56–61
Pichler WJ (2006) Adverse side-effects to biological agents. Allergy 61:912–920
Ponce R, Abad L, Amaravadi L et al (2009) Immunogenicity of biologically-derived therapeutics: assessment and interpretation of nonclinical safety studies. Regul Toxicol Pharmacol 54:164–182
Praditpornsilpa K, Kupatawintu P, Mongkonsritagoon W et al (2009) The association of anti-r-HuEpo-associated pure red cell aplasia with HLA-DRB1*09-DQB1*0309. Nephrol Dial Transplant 24:1545–1549
Price KS, Hamilton RG (2007) Anaphylactoid reactions in two patients after omalizumab administration after successful long-term therapy. Allergy Asthma Proc 28:313–319
Pungor E Jr, Files JG, Gabe JD et al (1998) A novel bioassay for the determination of neutralizing antibodies to IFN-beta1b. J Interferon Cytokine Res 18:1025–1030
Purcell RT, Lockey RF (2008) Immunologic responses to therapeutic biologic agents. J Investig Allergol Clin Immunol 18:335–342
Rader RA (2008) (Re)defining biopharmaceutical. Nat Biotechnol 26:743–751
Radstake TR, Svenson M, Eijsbouts AM et al (2009) Formation of antibodies against infliximab and adalimumab strongly correlates with functional drug levels and clinical responses in rheumatoid arthritis. Ann Rheum Dis 68:1739–1745
Rafi A, Castle SC, Uyemura K et al (2003) Immune dysfunction in the elderly and its reversal by antihistamines. Biomed Pharmacother 57:246–250
Reding MT (2006) Immunological aspects of inhibitor development. Haemophilia 12 (Suppl 6):30–35; discussion 35–36
Reding MT, Lei S, Lei H et al (2002) Distribution of Th1- and Th2-induced anti-factor VIII IgG subclasses in congenital and acquired hemophilia patients. Thromb Haemost 88:568–575
Regnault A, Lankar D, Lacabanne V et al (1999) Fcgamma receptor-mediated induction of dendritic cell maturation and major histocompatibility complex class I-restricted antigen presentation after immune complex internalization. J Exp Med 189:371–380
Reid RR, Woodcock S, Shimabukuro-Vornhagen A et al (2002) Functional activity of natural antibody is altered in Cr2-deficient mice. J Immunol 169:5433–5440
Reijonen H, Novak EJ, Kochik S et al (2002) Detection of GAD65-specific T-cells by major histocompatibility complex class II tetramers in type 1 diabetic patients and at-risk subjects. Diabetes 51:1375–1382
Rice GP, Paszner B, Oger J et al (1999) The evolution of neutralizing antibodies in multiple sclerosis patients treated with interferon beta-1b. Neurology 52:1277–1279
Richard J, Prang N (2010) The formulation and immunogenicity of therapeutic proteins: product quality as a key factor. Drugs 13:550–558
Richter AW, Akerblom E (1984) Polyethylene glycol reactive antibodies in man: titer distribution in allergic patients treated with monomethoxy polyethylene glycol modified allergens or placebo, and in healthy blood donors. Int Arch Allergy Appl Immunol 74:36–39
Robbins DC, Cooper SM, Fineberg SE et al (1987) Antibodies to covalent aggregates of insulin in blood of insulin-using diabetic patients. Diabetes 36:838–841
Ronnblom LE, Janson ET, Perers A et al (1992) Characterization of anti-interferon-alpha antibodies appearing during recombinant interferon-alpha 2a treatment. Clin Exp Immunol 89:330–335
Rosenberg AS (2003) Immunogenicity of biological therapeutics: a hierarchy of concerns. Dev Biol 112:15–21
Rosenberg AS (2006) Effects of protein aggregates: an immunologic perspective. AAPS J 8:E501–E507
Ross C, Clemmesen KM, Svenson M et al (2000) Immunogenicity of interferon-beta in multiple sclerosis patients: influence of preparation, dosage, dose frequency, and route of administration. Danish Multiple Sclerosis Study Group. Ann Neurol 48:706–712
Rutault K, Alderman C, Chain BM et al (1999) Reactive oxygen species activate human peripheral blood dendritic cells. Free Radic Biol Med 26:232–238
Rychly DJ, DiPiro JT (2005) Infections associated with tumor necrosis factor-alpha antagonists. Pharmacotherapy 25:1181–1192
Saha S, Bhasin M, Raghava GP (2005) Bcipep: a database of B-cell epitopes. BMC Genomics 6:79
Scagnolari C, Bellomi F, Turriziani O et al (2002) Neutralizing and binding antibodies to IFN-beta: relative frequency in relapsing-remitting multiple sclerosis patients treated with different IFN-beta preparations. J Interferon Cytokine Res 22:207–213
Schellekens H (2002) Bioequivalence and the immunogenicity of biopharmaceuticals. Nat Rev Drug Discov 1:457–462
Schellekens H (2003) Immunogenicity of therapeutic proteins. Nephrol Dial Transplant 18:1257–1259
Schellekens H (2008) Recombinant human erythropoietins, biosimilars and immunogenicity. J Nephrol 21:497–502
Scherer K, Spoerl D, Bircher AJ (2010) Adverse drug reactions to biologics. J Dtsch Dermatol Ges 8:411–426
Schreiber A, Humbert M, Benz A et al (2005) 3D-Epitope-Explorer (3DEX): localization of conformational epitopes within three-dimensional structures of proteins. J Comput Chem 26:879–887
Shopnick RI, Kazemi M, Brettler DB et al (1996) Anaphylaxis after treatment with recombinant factor VIII. Transfusion 36:358–361
Shurin MR, Shurin GV, Chatta GS (2007) Aging and the dendritic cell system: implications for cancer. Crit Rev Oncol Hematol 64:90–105
Simonney N, De Bosch N, Argueyo A et al (1985) HLA antigens in hemophiliacs A with or without factor VIII antibodies in a Venezuelan Mestizo population. Tissue Antigens 25:216–219
Singh SK (2011) Impact of product-related factors on immunogenicity of biotherapeutics. J Pharm Sci 100:354–387
Sollner J, Grohmann R, Rapberger R et al (2008) Analysis and prediction of protective continuous B-cell epitopes on pathogen proteins. Immunome Res 4:1
Sorensen PS, Ross C, Clemmesen KM et al (2003) Clinical importance of neutralising antibodies against interferon beta in patients with relapsing-remitting multiple sclerosis. Lancet 362:1184–1191
Sparwasser T, Koch ES, Vabulas RM et al (1998) Bacterial DNA and immunostimulatory CpG oligonucleotides trigger maturation and activation of murine dendritic cells. Eur J Immunol 28:2045–2054
Steele RH, Limaye S, Cleland B et al (2005) Hypersensitivity reactions to the polysorbate contained in recombinant erythropoietin and darbepoietin. Nephrology 10:317–320
Steere AC, Klitz W, Drouin EE et al (2006) Antibiotic-refractory Lyme arthritis is associated with HLA-DR molecules that bind a Borrelia burgdorferi peptide. J Exp Med 203:961–971
Steis RG, Smith JW 2nd, Urba WJ et al (1991) Loss of interferon antibodies during prolonged continuous interferon-alpha 2a therapy in hairy cell leukemia. Blood 77:792–798
Stickler M, Valdes AM, Gebel W et al (2004) The HLA-DR2 haplotype is associated with an increased proliferative response to the immunodominant CD4(+) T-cell epitope in human interferon-beta. Genes Immun 5:1–7
Strainic MG, Liu J, Huang D et al (2008) Locally produced complement fragments C5a and C3a provide both costimulatory and survival signals to naive CD4+ T cells. Immunity 28:425–435
Stubenrauch K, Wessels U, Birnboeck H et al (2010) Subset analysis of patients experiencing clinical events of a potentially immunogenic nature in the pivotal clinical trials of tocilizumab for rheumatoid arthritis: evaluation of an antidrug antibody ELISA using clinical adverse event-driven immunogenicity testing. Clin Ther 32:1597–1609
Suntharalingam G, Perry MR, Ward S et al (2006) Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N Engl J Med 355:1018–1028
Svenson M, Geborek P, Saxne T et al (2007) Monitoring patients treated with anti-TNF-alpha biopharmaceuticals: assessing serum infliximab and anti-infliximab antibodies. Rheumatology 46:1828–1834
Swinney DC, Anthony J (2011) How were new medicines discovered? Nat Rev Drug Discov 10:507–519
Tangri S, Mothe BR, Eisenbraun J et al (2005) Rationally engineered therapeutic proteins with reduced immunogenicity. J Immunol 174:3187–3196
van Beers MM, Jiskoot W, Schellekens H (2010) On the role of aggregates in the immunogenicity of recombinant human interferon beta in patients with multiple sclerosis. J Interferon Cytokine Res 30:767–775
van Beers MM, Sauerborn M, Gilli F et al (2011) Oxidized and aggregated recombinant human interferon beta is immunogenic in human interferon beta transgenic mice. Pharm Res 28:2393–2402
van Haren SD, Herczenik E, ten Brinke A et al (2011) HLA-DR-presented peptide repertoires derived from human monocyte-derived dendritic cells pulsed with blood coagulation factor VIII. Mol Cell Proteomics 10:M110.002246
von Delwig A, Altmann DM, Isaacs JD et al (2006) The impact of glycosylation on HLA-DR1-restricted T cell recognition of type II collagen in a mouse model. Arthritis Rheum 54:482–491
von Wussow P, Jakschies D, Freund M et al (1989) Humoral response to recombinant interferon-alpha 2b in patients receiving recombinant interferon-alpha 2b therapy. J Interferon Res 9(Suppl 1):S25–S31
Vos Q, Lees A, Wu ZQ et al (2000) B-cell activation by T-cell-independent type 2 antigens as an integral part of the humoral immune response to pathogenic microorganisms. Immunol Rev 176:154–170
Vultaggio A, Matucci A, Nencini F et al (2010) Anti-infliximab IgE and non-IgE antibodies and induction of infusion-related severe anaphylactic reactions. Allergy 65:657–661
Vultaggio A, Maggi E, Matucci A (2011) Immediate adverse reactions to biologicals: from pathogenic mechanisms to prophylactic management. Curr Opin Allergy Clin Immunol 11:262–268
Wadhwa M, Meager A, Dilger P et al (2000) Neutralizing antibodies to granulocyte-macrophage colony-stimulating factor, interleukin-1alpha and interferon-alpha but not other cytokines in human immunoglobulin preparations. Immunology 99:113–123
Wang W (2005) Protein aggregation and its inhibition in biopharmaceutics. Int J Pharm 289:1–30
Wang Y, Wu W, Negre NN et al (2011) Determinants of antigenicity and specificity in immune response for protein sequences. BMC Bioinformatics 12:251
Warrier I, Ewenstein BM, Koerper MA et al (1997) Factor IX inhibitors and anaphylaxis in hemophilia B. J Pediatr Hematol Oncol 19:23–27
Weaver DJ Jr, Reis ES, Pandey MK et al (2010) C5a receptor-deficient dendritic cells promote induction of Treg and Th17 cells. Eur J Immunol 40:710–721
Weber RW (2004) Adverse reactions to biological modifiers. Curr Opin Allergy Clin Immunol 4:277–283
Weber G, Gross J, Kromminga A et al (2002) Allergic skin and systemic reactions in a patient with pure red cell aplasia and anti-erythropoietin antibodies challenged with different epoetins. J Am Soc Nephrol 13:2381–2383
Woof JM, Burton DR (2004) Human antibody-Fc receptor interactions illuminated by crystal structures. Nat Rev Immunol 4:89–99
Yeung VP, Chang J, Miller J et al (2004) Elimination of an immunodominant CD4+ T cell epitope in human IFN-beta does not result in an in vivo response directed at the subdominant epitope. J Immunol 172:6658–6665
Zhao L, Wong L, Li J (2011) Antibody-specified b-cell epitope prediction in line with the principle of context-awareness. IEEE/ACM Trans Comput Biol Bioinform 8:1483–1494
Zhou W, Patel H, Li K et al (2006) Macrophages from C3-deficient mice have impaired potency to stimulate alloreactive T cells. Blood 107:2461–2469
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Sethu, S., Govindappa, K., Alhaidari, M. et al. Immunogenicity to Biologics: Mechanisms, Prediction and Reduction. Arch. Immunol. Ther. Exp. 60, 331–344 (2012). https://doi.org/10.1007/s00005-012-0189-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00005-012-0189-7