Abstract
Background
There have been few studies of tailored interventions to promote colorectal cancer (CRC) screening.
Purpose
We conducted a randomized trial of a tailored, interactive intervention to increase CRC screening.
Methods
Patients 50–70 years completed a baseline survey, were randomized to one of three groups, and attended a wellness exam after being exposed to a tailored intervention about CRC screening (tailored group), a public web site about CRC screening (web site group), or no intervention (survey-only group). The primary outcome was completion of any recommended CRC screening by 6 months.
Results
There was no statistically significant difference in screening by 6 months: 30%, 31%, and 28% of the survey-only, web site, and tailored groups were screened. Exposure to the tailored intervention was associated with increased knowledge and CRC screening self-efficacy at 2 weeks and 6 months. Family history, prior screening, stage of change, and physician recommendation moderated the intervention effects.
Conclusions
A tailored intervention was not more effective at increasing screening than a public web site or only being surveyed.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is an important cause of morbidity and mortality in the USA. The American Cancer Society estimates that in 2010, 142,570 Americans will develop CRC and 51,370 will die of the disease [1]. CRC screening can reduce both incidence and mortality through early detection and removal of precancerous lesions, and the American Cancer Society and other professional organizations recommend regular screening for average-risk persons 50 and older [2]. Although screening rates have increased from 39% to 55% between 2000 and 2008 [3, 4], they are below those reported for other cancer screening tests [3, 4].
Efforts to promote CRC screening in average-risk persons began in the 1980s [5] and accelerated in 1997 upon publication of consensus screening guidelines [6]. Systematic reviews and meta-analyses have summarized the effectiveness of CRC screening interventions conducted during different time periods: prior to 1997 [5], between 1966 and 1999 [7], between 1989 and 1994 [8], between 1997 and 1999 [9], and prior to 2005 [10–12]. Different classification systems were used to describe intervention effects, but in general, interventions were classified as patient-, physician-, or systems-directed. Consistent findings were that patient-directed reminders and reducing barriers to access increased CRC screening.
Many interventions were based on behavior change theories or models; however, the effect of using different theoretical constructs or methods was not often evaluated. More recently, there have been several systematic reviews or meta-analyses of one theoretical method, tailoring, that has been frequently used in cancer screening interventions [13–15]. Tailoring uses measured personal information to deliver messages that are directly relevant to a person’s expressed attitudes and beliefs [16, 17]. Because messages are based on personal information, they are hypothesized to be more likely to be attended to and to influence determinants of behavior compared with generic communications. Constructs from several theoretical models, including the health belief [18] and trans-theoretical [19] models, have been used to tailor health-related communications, and systematic reviews support the effectiveness of tailored communication in changing a number of health behaviors, including mammography [13–15] and Pap test screening [13]. Only the review by Albada et al. [15] assessed the effectiveness of tailored information to increase CRC screening with fecal occult blood testing (FOBT), but they concluded that the evidence was insufficient to support an effect of tailoring.
For tailored print materials, there generally is a lag between assessing a person’s attitudes and beliefs and delivering messages based on that information, thus increasing the chances that a person’s knowledge, attitudes, or beliefs may have changed. Telephone counseling, which has the benefit of immediacy and more personalized interaction, is expensive and is not easily incorporated into healthcare settings. Computer technology has begun to be used to deliver health education programs [15] and has an advantage over print materials for delivering tailored messages because it can deliver messages “in real time.” In this regard, it is similar to telephone or face-to-face delivery. In addition, computer technology is well suited to conveying information when there are multiple options, as is the case for CRC screening, because persons can self-tailor by selecting various “paths” through a program based on their interest in different tests so that information specific to that test can be communicated.
We used the trans-theoretical model as the organizing framework to design our intervention and to tailor messages because it has been used with other cancer screening behaviors and because at the time of our study in 2004, the prevalence of CRC screening was <50% [4], suggesting that awareness about CRC screening and readiness to screen were low in the general population. The stages of change construct from the trans-theoretical model takes into consideration a person’s readiness to adopt a behavior, and that information can be used to select determinants and tailor messages that are relevant to moving a person to act.
At the time our study was conducted, there were relatively few published reports that used tailored print or telephone counseling for CRC screening, and there were no tailored, interactive, computer-delivered CRC screening interventions. Furthermore, most CRC screening interventions promoted only FOBT rather than all available options [5, 7–12].
Our primary objective was to conduct a randomized controlled trial of a patient-directed, tailored, interactive, computer-delivered intervention to increase the primary outcome of CRC screening in a clinic setting. Other objectives were to: (1) evaluate the intervention effect on intermediate psychosocial variables that might influence screening, (2) assess moderation effects, and (3) conduct a process evaluation of intervention implementation.
Subjects and Methods
Selection and Recruitment of Study Sample
The study was conducted at Kelsey-Seybold Clinic by the Kelsey Research Foundation and The University of Texas-Houston School of Public Health. Kelsey-Seybold Clinic is the largest multi-specialty medical group practice in the greater Houston, Texas, area. It serves approximately 400,000 patients through a network of 19 clinics. It is similar to an integrated healthcare system in that it provides both primary and specialty care. The study protocol was approved by the Institutional Review Board at The University of Texas-Houston School of Public Health and is registered on clinicaltrials.gov (NCT01084746).
The study population was patients 50–70 years of age who had never been screened for CRC or who were overdue for CRC screening according to American Cancer Society guidelines in effect at the time of the study [20]. Other eligibility criteria were that patients had received care at Kelsey-Seybold Clinic within the past year; were English-speaking; had never been diagnosed with CRC, adenomatous polyps, Crohn’s disease, or ulcerative colitis; had a wellness exam scheduled or were willing to schedule one; were willing to complete a baseline survey; and agreed to come to the clinic 45 min before their exam to complete a study visit.
Between January 2004 and February 2006, participants were recruited through a multistep process. Foundation staff identified potentially eligible patients from the clinic administrative database and mailed invitation letters every 2 weeks to patients who had a wellness exam scheduled within the next month and to a random sample of patients who had not had a wellness exam in the past 12 months. The letter included a telephone number so that patients could decline participation. Patients who did not call and decline were telephoned within 2 weeks by Foundation staff and invited to enroll in the study. Those consenting were administered a verbal audio-taped Health Insurance Portability and Authorization Act (HIPPA) release and, if not already scheduled, were scheduled for a wellness exam. Patients were considered non-respondents if they could not be contacted after six telephone calls made during different days of the week and times of day. Contact information of enrolled participants was sent to the research staff at The University of Texas-Houston School of Public Health who made all further contacts with study participants. Two to 4 weeks before the wellness exam, participants were contacted and were asked to complete a baseline telephone survey.
Study Design
Randomization to one of three study groups occurred upon completion of the baseline survey and was stratified by gender and prior CRC screening status, i.e., never screened males, never screened females, overdue males, and overdue females. Four lists of random numbers were computer-generated, and participants were randomly assigned to one of three study groups by the interviewer using the appropriate list. One group received only the baseline and follow-up surveys (survey-only group). Another group viewed information about CRC screening on a publicly available web site (web site group). The third group viewed a tailored, interactive, computer-delivered intervention about CRC screening developed for this trial (tailored group).
The pre-exam study visit took place at clinic’s Health Information Center 45 min before the patient’s appointment. Participants signed an informed consent form (all three groups) and, when applicable, viewed the web site or tailored interventions on desktop computers in the Center. Web site and tailored intervention participants completed a ten-item self-administered survey to rate their experience immediately after their assigned intervention. All participants were invited to use the Center and take any educational materials of interest. All participants received $25 for attending the visit.
Participants were surveyed by telephone at 2 weeks and 6 months post-intervention. We randomly selected half of the survey-only group to complete the 2-week survey in order to assess potential cueing effects of being surveyed after the wellness visit on subsequent CRC screening behavior [21]. Participants completing the 6-month survey received $25.
Survey Development and Implementation
The baseline telephone survey included questions about eligibility, demographics, CRC and CRC screening, computer use, and psychosocial factors (described below). Psychosocial variables and questions about the exam visit were asked on the 2-week follow-up survey, and questions about the screening decision were included on the 6-month survey. Surveys were administered by the project director and research assistants using a computer-assisted telephone interview system that included a scripted introduction and transitions between sections of the survey. The project director trained the research assistants to administer the survey and monitored calls weekly to ensure adherence to the script. Training consisted of practice calls with research staff and observation of and feedback on survey administration. Survey administrators were blinded to study group status at 6 months. At the 2-week interview, staff was not blinded to study group status because some process evaluation questions were asked only of the tailored group.
Intervention Descriptions
The web site program was Screen for Life, an educational program developed by the Centers for Disease Control and Prevention as part of a larger awareness campaign to promote CRC screening [22] (http://www.cdc.gov/Features/ScreenforLife). The format was non-interactive and provided information and motivational messages about CRC and CRC screening including test options, frequently asked questions, questions to ask your provider, a podcast on the benefits of screening, and print material that could be downloaded. We chose this web site over others because it included some similar features to our program such as information and motivational messages about CRC screening, although the messages were not tailored to characteristics of the participants.
The tailored intervention program was developed using intervention mapping, a process for systematic health promotion program planning, implementation, and evaluation that incorporates theory and empiric evidence [23]. The behavior of interest was acquiring CRC screening; however, component behaviors included discussing CRC screening options with the primary care provider, scheduling CRC screening, seeking instrumental social support if needed, and following through with the test.
We used the trans-theoretical model as the primary theoretical framework and added additional constructs and predictors based on the literature and on qualitative data from our target population [24]. Constructs from the trans-theoretical model that were operationalized in the intervention were stage of change or readiness to complete CRC screening (precontemplation, contemplation, and preparation for action) and the relevant processes of change related to each stage (self-reevaluation, consciousness raising, environmental reevaluation, and self-liberation). Other trans-theoretical model constructs included were self-efficacy and pros and cons (decisional balance). Additional constructs found to be associated with CRC screening in the literature included knowledge, social influence, cancer worry, and comparative and absolute risk [25, 26].
The stages of change construct was used to tailor messages to the participant’s readiness to undertake screening and to develop messages to influence the determinants of stage movement and the processes of change for each stage. As depicted in Table 1, the determinants were targeted directly by theoretical change techniques operationalized by messages and activities delivered in the computer program. Processes of change are not explicit determinants of behavior; rather, they suggest determinants relevant to a particular stage and are used by individuals to move toward adoption or cessation of a behavior. Processes also are not theoretical change techniques to be used to stimulate movement from stage to stage but require stimulation by other theoretical techniques.
The theoretical change techniques were operationalized into intervention messages and delivered in a 15- to 25-min (depending on the user’s choices) interactive computer-delivered program. The program included techniques to influence the determinants or mediating constructs and other predictors of CRC screening uptake. Specific theory-informed change techniques were used for each determinant variable when the participant was measured to be in the stage of readiness that posited that determinant as potentially important (Table 1). The tailored program assessed stage of change three times and presented program components with specific messages targeting constructs appropriate to stage. Additionally, we tailored the role models in the video vignettes to the gender of the participant. Narrative feedback after the staging questions varied not only by stage but also by movement between stages, including backward movement and lack of movement. The program progressed across three narrative video vignettes that contained informational, role modeling, and narrative segments. The vignettes introduced two friends discussing a mutual friend who had recently been diagnosed with CRC and were stage-matched to the study participant so that one friend was in the same stage as the participant and the other was one stage ahead. At the end of the program, participants viewed a list of common concerns about CRC screening identified in the literature and selected up to three questions they would like to discuss with the physician. Two copies of a letter listing the questions and the patient’s stage of readiness for CRC screening were printed to facilitate patient–physician discussion about CRC screening.
The intervention used Macromedia Flash ActionScript 2.0 to program the logic. Data to track participants’ use of the intervention program or the web site were written to a Microsoft ACCESS database generated by Macromedia ColdFusion. Costs associated with intervention development have been described elsewhere [27].
Measures
CRC Screening Status
Using American Cancer Society guidelines in effect at the time of the study [20], we reviewed medical records and searched the administrative billing database at 12 and 24 months post-intervention to ascertain completion of any recommended CRC screening test. We recorded date and test type (FOBT, sigmoidoscopy, double-contrast barium enema, or colonoscopy) for all randomized study participants. If a patient completed more than one test, we used the date and type of the first test.
The project director and research assistants abstracted medical records without reference to group assignment. A protocol for data abstraction was developed and research assistants were trained in its use. Training consisted of reviewing a sample of the medical records and comparing results to those of the project director. Eighty-one charts (7%) were abstracted by three different abstracters to assess inter-rater agreement for the presence or absence of a CRC test in the medical record, test type, and date. Agreement between pairs of abstractors for the most recent test within guidelines was 98% (k = 0.96). Abstracted information was compared and inconsistencies were resolved by rechecking the medical record.
Participant Characteristics and Psychosocial Measures
We measured the following characteristics on the baseline survey: age, sex, race/ethnicity, marital status, education, income, employment status, type of insurance, family history of CRC, awareness and history of CRC screening, whether a physician had ever recommended CRC screening, CRC screening test preference, and frequency of computer use. We also measured psychosocial variables used in the intervention and shown in the literature to be associated with screening uptake [25, 26], including stage of change, self-efficacy, pros and cons, knowledge, social influence, worry about CRC, and absolute and comparative perceived risk of CRC. Stage of change was measured as precontemplation (not thinking about testing), contemplation, or preparation for action (committed to getting tested). Contemplation was measured using three categories: need to consider testing, think I should but am not quite ready, and think I will probably get tested. Knowledge was measured with four items and was scored “true or false”; correct answers were summed. Pros (α = 0.75, items = 8), cons (α = 0.78, items = 14), self-efficacy (α = 0.91, items = 8), and social influence (α = 0.65, items = 4) for getting CRC screening were measured using validated multi-item scales [28]. Items used to measure all psychosocial constructs focused on issues related to CRC and CRC screening. The measures demonstrated construct validity for subgroups in our sample based on gender, race (white and African American), and prior CRC screening (never screened and overdue) [28]. Variations of this instrument showed construct validity in three other studies with diverse samples [29–31]. Comparative and absolute perceived risk and cancer worry were measured with single items. All items were measured on a four-point scale.
Process Measures
We measured program reach, dose delivered, and dose received. Because all participants had to complete a baseline survey prior to randomization to be eligible for the trial, we measured reach as the proportion in the web site and tailored groups who attended the pre-exam study visit and completed the assigned intervention. Dose delivered was measured using computer software to track use of the web site or tailored intervention. We recorded time spent viewing the program and number of screens viewed.
Dose received was measured with a ten-item self-administered survey immediately after the intervention session that asked web site and tailored group participants to rate their experience with the web site or the computer program on how engaging, novel, clear, and easy to navigate and understand it was. They also were asked whether they identified with the characters, whether the program convinced them of the need for screening, whether it was difficult to concentrate on the material, whether they liked the format, and whether they would recommend the program to others. Opinions were measured on a five-point scale from “strongly agree” to “strongly disagree.”
At the 2-week follow-up survey, all participants were asked questions about the project, including recall of being exposed to new information, whether they sought more information about CRC screening, and the influence of the program on making a decision about CRC screening. We also asked whether they discussed CRC screening with their physician, whether their physician recommended CRC screening, and the importance of the doctor visit in deciding about CRC screening. Responses were measured on a four-point scale from “very important” to “not very important” or “yes or no.”
Outcome Analysis
Hypotheses
Our primary hypothesis was that a more personalized, tailored intervention would be more effective than a generic web site intervention and that both would be more effective than simply completing a survey. Specifically, we hypothesized that by 6 months post-intervention, CRC screening rates would be lowest in the survey-only group and highest in the tailored group with rates for the web site group intermediate. As secondary hypotheses, we examined the long-term effects of the intervention at 12 and 24 months as well as completion of specific CRC screening tests.
Sample Size
Sample size was based on the following assumptions and parameters: 0.05 significance level (α), 0.80 power (1 − β), and two-sided test of significance. Based on the literature at the time the study was conducted, we estimated the proportions of “never screened” patients who would complete CRC screening by the 6-month follow-up to be 5%, 10%, and 20% in the survey-only, web site, and tailored groups. The proportions of previously “ever screened” patients who would complete CRC screening by the 6-month follow-up were estimated to be 10%, 30%, and 40% in the three groups. Therefore, we estimated the overall proportion completing CRC screening as 7.5%, 20%, and 30% in the three groups. To compare survey-only and web site groups, based on two sample proportions, the minimum sample size was 118 in each group. To compare the survey-only and tailored groups, it was 47; for the web site and the tailored groups, it was 294 [32]. We estimated a 25% dropout rate from baseline to 6-month follow-up interview, and so we inflated our sample size from 294 to 368 per group.
Preliminary Analyses
We compared equivalence of the three groups on factors measured on the baseline survey. We then compared those who completed the intervention study visit and wellness exam with those who did not. We used chi-square or t tests for all comparisons. Statistical significance was based on p < 0.05 and was adjusted for multiple comparisons using the Bonferroni procedure [33].
Intention-to-Treat and Per Protocol Analyses
To test our primary and secondary hypotheses, we conducted intention-to-treat and per protocol or “as treated” analyses [34] using chi-square statistics and logistic regression. The intention-to-treat analyses included all participants who were randomized to a study group regardless of further participation. In the per protocol analyses, we only included participants who completed their pre-exam study visit and intervention (if assigned to the web site or tailored groups). For the test-specific analyses, we combined barium enema and sigmoidoscopy as there were too few participants receiving these tests to conduct separate analyses.
Analyses of Intermediate Psychosocial Outcomes and Potential Moderators
We examined between- and within-group differences in psychosocial factors that were targeted in the intervention and could potentially mediate the intervention effect [26]. Psychosocial variables were measured at all three time points and included stage of change, knowledge, self-efficacy, pros, cons, social influence, cancer worry, and comparative and absolute perceived risk. We hypothesized that any intervention effect on CRC screening would be mediated, at least in part, by the psychosocial constructs that were addressed by specific messages and strategies in our tailored intervention. For these variables to have a clear effect on screening by 6 months, they would need to change between baseline and 2 weeks post-intervention; we also measured these variables at 6 months to assess delayed effects of the intervention on screening by 12 months. For stage of change, chi-square was used to test for statistical significance within and between groups using a three-category measure of stage, i.e., precontemplation, contemplation, and preparation. All other variables were tested using ANOVA for between-group differences. If the overall between-group difference was statistically significant at p < 0.10, we tested pairwise differences using the least significance difference method in an ANOVA model. For within-group comparisons, we compared baseline to 2 weeks and baseline to 6 months.
We used Mantel–Haenszel analyses and logistic regression to assess whether baseline characteristics or stage of change moderated the effect of the intervention on any recommended CRC test by 6, 12, and 24 months. In the logistic regression model, the three-level stage of change variable was measured as a continuous variable to show the effect of increasing stage on the likelihood of screening.
Process Analyses
For the rating survey administered immediately after the intervention, we used chi-square analysis to compare responses of participants in the web site and tailored groups (“strongly agree” vs. the four other categories). For the process measures on the 2-week survey, we compared responses among the three groups (“very important” vs. the three other categories).
Results
Recruitment, Participant Flow, and Baseline Data
Recruitment began in January 2004 and follow-up interviews were completed in August 2007. We mailed 10,352 invitations to potentially eligible patients (Fig. 1). Reasons patients did not enroll in the study were ineligibility (n = 4,121), refusal (n = 1,996), non-response (n = 1,727), invalid contact information (n = 629), too ill (n = 274), inability to reach the patient to complete a baseline survey before their clinic visit (n = 167), and deceased (n = 54). We attempted to obtain minimal information to confirm study eligibility from those who actively refused, but most people were unwilling to stay on the phone. We also were unable to collect data on eligible non-participants through medical records due to HIPAA policies.
CONSORT flow diagram. *The intention-to-treat analyses included all eligible participants who responded to the baseline survey and were randomized to a study group regardless of further participation. In the per protocol analyses, we only included participants who completed their pre-exam study visit (and intervention, if assigned to the web site or tailored group)
Of 1,384 patients enrolled at Kelsey-Seybold Clinic, 1,224 (88%) completed a baseline interview and were randomized to a study group (intention-to-treat analysis). Of the 1,224, 1,046 (85%) completed the pre-exam study visit and intervention assignment (per protocol analysis). Based on our required sample size of 294 per group, we had sufficient power to detect our primary hypothesized intervention effect in intention-to-treat and per protocol analyses.
Preliminary Analyses
After adjusting for multiple comparisons, there were no statistically significant baseline differences among the three groups on the background or psychosocial variables (Table 2). Likewise, participants in the survey-only group who were randomized to receive the 2-week survey were similar to those who were not. Our study sample was predominantly 50–59 years old, female, married, employed, had at least a high school education, reported income over $50,000 a year, and had private health insurance (Table 2). Almost half of our sample was African American, 35% were white, 12% were Hispanic, and 6% were other ethnicities. Seven percent reported having a first-degree relative with CRC, 92% were aware of CRC screening tests prior to study enrollment, 51% had previously been screened for CRC and were overdue, 50% reported that a doctor had “ever” recommended CRC screening, 41% stated a preference for colonoscopy, and over 80% used a computer daily or weekly.
Overall, the dropout rate was 15%. The dropout rate and characteristics of the dropouts did not differ by study group. Compared with all groups combined, those who enrolled but did not complete the study were less likely to have a college degree or more education (32% vs. 43%, χ 2 = 8.58, df = 2, p = 0.014), be in the contemplation stage of change (47% vs. 56%, χ 2 = 7.85, df = 2, p = 0.02), and less likely to be screened during the study (12% vs. 32%, χ 2 = 29.64, df = 2, p < 0.001). They also were more likely to be white (28% vs. 36%, χ 2 = 7.90, df = 2, p = 0.019).
There was no statistically significant cueing effect of the 2-week survey on subsequent screening completion among those in the survey-only group who were randomized to receive a 2-week survey. Screening rates were similar among those who did and did not receive the survey.
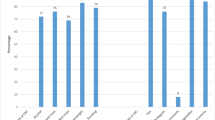
Intention-to-Treat and Per Protocol Analyses of CRC Screening Completion
In the intention-to-treat analyses for our primary outcome, completion of any CRC screening test by 6 months, there was no statistically significant difference in screening rates among the three groups, nor were any of the pairwise comparisons statistically significant (Table 3). Approximately 30% of participants in every group were screened by 6-month follow-up. Results of the per protocol analyses were similar; however, the prevalence of screening was slightly higher in all groups because dropouts were less likely to be screened. Likewise, intention-to-treat and per protocol results for the 12- and 24-month follow-up were similar in the three groups. For each test type (FOBT, colonoscopy, other), the pattern of results for both the intention-to-treat and per protocol analyses was similar to that observed in the overall analyses, i.e., there were no statistically significant differences for type of test completed among the three groups (Table 3).
Intermediate Psychosocial Outcomes Analyses
We examined the intervention effect on psychosocial factors targeted as potential mediators or intermediate outcomes. All three groups showed statistically significant positive stage movement from baseline to 2 weeks and baseline to 6 months (Table 4). There was a marginally significant between-group difference by 2 weeks (p = 0.066); by 6 months, the overall between-group difference was statistically significant (p = 0.005). In pairwise comparisons, the tailored (p = 0.001) and web site (p = 0.033) groups were more likely to be in preparation than the survey-only control group; there was no difference in stage distribution between the tailored and web site groups (p = 0.426).
All three groups showed statistically significant within-group increases in knowledge scores from baseline to 2 weeks and baseline to 6 months (p < 0.001 for all comparisons). Between-group differences in knowledge scores were statistically significant at 2 weeks (p < 0.001) and 6 months (p = 0.005). Pairwise comparisons showed that the tailored group reported higher scores than the web site and survey-only groups by 2 weeks and 6 months (p < 0.004 for both comparisons); there was no difference between the web site and the survey-only groups at either time point.
From baseline to 2 weeks, the tailored (p < 0.001) and survey-only (p = 0.048) groups showed a statistically significant increase in self-efficacy scores; from baseline to 6 months, only the tailored group’s scores were significantly increased (p = 0.009). Between-group differences in self-efficacy scores were statistically significant at 2 weeks (p = 0.009) and were marginally significant at 6 months (p = 0.051). At 2 weeks, pairwise comparisons for self-efficacy showed that the tailored group scores were higher than those for the web site (p = 0.003) and survey-only (p = 0.006) groups, while scores for the web site and survey-only groups did not differ (p = 0.416). Although the magnitude of the differences decreased slightly by 6 months, the differences remained significant (Table 4).
There was a statistically significant between-group difference in the pros at 6 months (p = 0.037), with the web site group having slightly higher scores than the tailored (p = 0.071) or survey-only (p = 0.006) groups. By 6 months, the tailored group had lower cons scores than the web site (p = 0.049) or survey-only (p = 0.013) groups.
At baseline, cancer worry scores showed a marginally significant overall difference (p < 0.074). Pairwise comparisons showed that scores for the tailored group were significantly lower at baseline than scores for either of the other two groups, whose scores were similar. Although the tailored group showed a statistically significant increase in worry from baseline to 2 weeks (p < 0.001) and baseline to 6 months (p = 0.001), cancer worry scores were equivalent for all three groups at 2 weeks and 6 months. Between baseline and 2 weeks, the web site group perceived greater comparative CRC risk (p = 0.018) and the tailored group perceived greater absolute CRC risk (p = 0.006).
Moderator Analyses
We found no moderating effect of study group by age, sex, race/ethnicity, marital status, education, income, employment status, type of insurance, or computer use. Logistic regression and Mantel–Haenszel analyses showed that family history, prior CRC screening, and baseline stage of change were significant moderators of the intervention’s effect on any CRC screening by 6, 12, and 24 months post-intervention (Table 5). Participants in the tailored group with a family history, but not those in the other two groups, were more likely to be screened at all time points than those in the tailored group without a family history. Participants in the tailored and web site intervention groups who had been screened previously were more likely to be screened at all time points than those in their respective groups who had not been screened previously. For stage of change, there was a 21% or greater increase in any screening for each stage progression (e.g., precontemplation to contemplation) for those in the tailored group, but not the other two groups. Those in the tailored group were more likely to be screened by 12 months if they had ever received a physician recommendation compared with those who had not.
Process Evaluation Analyses
After randomization, 84% of participants in the tailored group and 86% of those in the web site group interacted with the program (program reach). Tailored group participants spent an average of 23 min viewing the program (range, 16–41 min), while web site group participants spent an average of 17 min navigating the web site (range, 4–54 min). Tailored group participants viewed an average of 12 computer screens (range, 10–14); web site group participants viewed an average of 17 screens (range, 1–106). Neither minutes spent viewing the program nor number of computer screens viewed was associated with CRC screening completion in either group.
On the rating survey administered to the web site and tailored groups immediately after the intervention, the tailored group was significantly more likely than the web site group to strongly agree with positive statements regarding characteristics of the program, including that it was engaging, clear, easy to navigate and understand, that it was easy to concentrate on the material, and that they identified with the characters and liked the format. There was no difference between the groups for questions about whether the information was new, whether the program persuaded them to be screened, and whether they would recommend it to others.
On the 2-week survey, participants in the tailored and web site groups were more likely than the survey-only group to report that the study made a difference in helping them decide to have CRC screening, seek out more information about CRC screening, and choose a specific CRC screening test. There were no group differences in CRC screening discussions with physicians, physician recommendation, or importance of the visit on CRC screening decision making.
Discussion
Findings for our computer-delivered intervention are generally consistent with those of most other patient-directed interventions that were conducted during the same time period and that used similar theoretical constructs and involved either tailored print [35–41] or telephone counseling. Only Basch et al. [42] found a positive effect of their tailored telephone intervention compared with generic mailed print materials by 6-month follow-up. Using a factorial design, Ling et al. [38] did not find an effect of a patient-directed tailored letter, but they did observe a positive effect of their multi-component intervention to change office practices. One component of the practice intervention was a telephone motivational interview conducted with the patient by clinic staff which, in essence, was a patient-directed tailored intervention. Collectively, these studies and the findings from a recent systematic review [15] do not provide strong or consistent support for the use of patient-directed tailored print or telephone interventions to increase CRC screening.
Although results of our moderator analyses should be considered post hoc, they may provide interesting hypotheses for future study. Our tailored intervention had a positive effect on CRC screening among specific subgroups. Participants in the tailored group were more likely to be screened if they reported a family history of CRC, received a physician recommendation, or progressed through the stages of change, suggesting that the tailored intervention motivated them to act. Participants in both the tailored and web site groups who had been previously screened also were more likely to be screened during the study. A modest positive effect of the tailored intervention also was observed on some of our intermediate psychosocial outcomes, and participants’ evaluation of the project at 2-week follow-up suggested that the tailored intervention had a more positive effect than the web site or just being surveyed. However, these differences in attitudes did not translate into greater use of CRC screening in the tailored group compared with the other study conditions.
We considered a number of possible explanations for our results, including statistical power, potential cueing effects of the surveys, fidelity of intervention implementation, and target of the intervention.
Statistical Power and Cueing Effects of the Surveys
Our dropout rate was 15%, lower than the 25% we estimated, and so we had adequate statistical power to detect our hypothesized intervention effect in intention-to-treat and per protocol analysis.
All participants completed a baseline survey, and many of the questions referred to CRC and CRC screening. Thus, it is possible that the survey had the unintended consequence of serving as a cue to action [21] by raising awareness and underscoring the importance of screening, particularly since our study was conducted during a time when there were an increasing number of public health campaigns about CRC and CRC screening. Because we did not have a no-contact control group, there is no direct way to know for sure whether or not the baseline survey increased motivation or served as a cue to action to be screened. Screening completion was similar among participants randomized to complete the 2-week survey compared with those who were not, indicating that the 2-week post-intervention survey itself did not influence subsequent screening behavior. We chose not to have a no-contact control group because systematic reviews show that minimal cue interventions such as reminders are effective at increasing cancer screening behaviors including FOBT [10]; therefore, it can be argued that some form of a minimal cue should be the standard of care, and the baseline survey may have served that purpose. The challenge for researchers is to develop strategies that increase screening rates above what can be accomplished with minimal cues.
Intervention Development and Implementation Fidelity
We used a systematic approach to develop and implement the intervention [23]. We targeted theoretical constructs and those predictors that have been shown in cross-sectional and prospective studies to be associated with CRC screening [25, 26], and we conducted focus groups with the target population [24] to ensure that all relevant determinants were identified. We wrote performance and learning objectives and developed matrices to ensure that all determinants were addressed in the intervention. The performance and learning objectives addressed the identified determinants using relevant theoretical methods and strategies. We successfully delivered the tailored and web site interventions to over 80% of the enrolled participants. Thus, the intervention was designed and implemented as planned.
Theoretical Framework and Targets of the Intervention
Our intervention was patient-directed and focused primarily on individual-level cognitive and psychosocial determinants drawn from the trans-theoretical model and constructs and predictors from the literature on CRC screening and other cancer screening behaviors published at the time this intervention was designed in 2003. However, awareness and uptake of CRC screening have been increasing [4, 43], and so the trans-theoretical model probably was not the most useful theoretical framework at this point in the adoption curve for CRC screening. At baseline, over one third of our sample was in contemplation and over one half was in preparation. At 2 weeks post-intervention, over 70% in the tailored and web site groups and 65% of the survey-only group were in preparation. This shift in stage of readiness suggests that participants were motivated to act, and it is possible that a more goal-directed, planning-oriented intervention strategy such as stimulating implementation intentions would have been a better choice for our participants’ stage of readiness. In such an intervention, a patient could develop a step-by-step plan to complete screening [44, 45]. Alternatively, patient navigation interventions that assist patients throughout the process (e.g., scheduling an appointment, telephone support to address barriers and concerns) might have been more successful in moving those in preparation to action [46]. Such interventions would likely have identified potential healthcare system or other barriers warranting attention by the navigator and patient.
The dynamics of the patient–physician encounter also may have deterred patients from being screened. Our intervention encouraged patients to decide to get screened and to talk to their physician about test options, implying they would make a decision in consultation with their physician. However, in a qualitative study conducted during the trial, we audio-taped 64 patient–physician visits and found that although CRC screening was brought up in almost every encounter, there was little or no discussion of options and little evidence of shared decision making [47]. In fact, most physicians recommended colonoscopy, thus countering messages in the intervention that the patient had options. We did not anticipate that physicians would recommend colonoscopy as the preferred option. A national survey of primary care physicians conducted in 2000 did not show such a strong preference for colonoscopy [48], although this trend had changed by 2007 [49]. Physicians’ emphasis on colonoscopy in our study and others [50] raises a question about whether the focus of promotion efforts should be on choosing among test options or limiting the choices [51–53]. To date, we know very little about whether CRC screening adherence is increased or decreased under circumstances where patients are given multiple options, are asked to choose one option, or are offered only one option without consideration of their preference. Studies using decision aids to clarify a patient’s preferences and values may better prepare patients to discuss their preferred test with their physician [54], but to date, findings from studies of decision aids have shown inconsistent results regarding whether or not they increase CRC screening [55–57].
Healthcare system barriers to CRC screening also may have played a role in the low screening rates by presenting obstacles that patients were not able to overcome. For example, although all patients had insurance, coverage varied by type of plan, and the amount of the co-pay for certain tests appeared to be a barrier for some patients [47]. But even when colonoscopy was recommended, there was no clear timeline or plan for scheduling an exam. In fact, patients were told different things about scheduling, and there was confusion about whose responsibility it was to schedule an exam. Although the intervention addressed barriers, it did not facilitate navigation through the actual barriers encountered, and it appears that the intervention was effective only for the most motivated patients (e.g., those with prior screening or family history).
Collectively, these observations suggest that a patient-directed intervention focused primarily on motivational messages rather than planning may not be effective in clinic settings where physicians’ beliefs and preferences and healthcare system barriers need to be addressed in conjunction with patients’ preferences and other circumstances.
Strengths and Limitations
Strengths of our study include that we measured screening completion using medical records and that we conducted both intention-to-treat and per protocol analyses. We also examined changes in intermediate psychosocial variables over the short and long terms, and we conducted a detailed process evaluation of the intervention. Limitations include that our findings can be generalized only to persons who have access to and use healthcare and that our analyses of intermediate variables should be considered exploratory due to the likelihood of type 2 error.
Conclusions
Our results show that in a clinic setting, a patient-directed tailored intervention based on the trans-theoretical model was not more effective at increasing CRC screening than a public web site or only being surveyed. Positive changes in some of the intermediate psychosocial variables, although favoring the tailored group, did not translate into increased screening. We need to better understand what occurs between physicians’ and patients and what system factors can be modified to increase adherence. To date, as a research community, we have yet to identify an intervention approach for CRC screening that is consistently more effective than usual care or minimal cues despite using the best available theoretical evidence and state-of-the-science methods [25].
References
American Cancer Society. Cancer Facts & Figures 2010. Atlanta, GA: American Cancer Society; 2010.
Levin B, Lieberman DA, McFarland B et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: A joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA: Cancer J Clin 2008 March 5; 58: 130-160.
Klabunde C. Trends in the use and quality of colorectal cancer screening in the U.S. Presented at the NIH State-of-the-Science Conference: Enhancing Use and Quality of Colorectal Cancer Screening, February 2–4, 2010.Bethesda, MD, 47–51. 2-2-2010. National Cancer Institute; NIH.
Meissner HI, Breen NL, Klabunde CN, Vernon SW. Patterns of colorectal cancer screening uptake among men and women in the US. Cancer Epidemiol Biomarkers Prev 2006; 15: 389–394.
Vernon SW. Participation in colorectal cancer screening: A review. J Natl Cancer Inst 1997; 89: 1406–1422.
Winawer SJ, Fletcher RH, Miller L et al. Colorectal cancer screening: Clinical guidelines and rationale. Gastroenterology 1997; 112: 594–642.
Stone EG, Morton SC, Hulscher MEJL et al. Interventions that increase use of adult immunization and cancer screening services: A meta-analysis. Ann Intern Med 2002; 136: 641–651.
Snell JL, Buck EL. Increasing cancer screening: A meta-analysis. Prev Med 1996; 25: 702–707.
Peterson SK, Vernon SW. A review of patient and physician adherence to colorectal cancer screening guidelines. Semin Colon Rectal Surg 2000; 11: 58–72.
Baron RC, Rimer BK, Breslow RA et al. Client-directed interventions to increase community demand for breast, cervical, and colorectal cancer screening. Am J Prev Med 2008; 35: S34–S55.
Baron RC, Rimer BK, Coates RC et al. Client-directed interventions to increase community access to breast, cervical, and colorectal cancer screening. Am J Prev Med 2008; 35: S56–S66.
Sabatino SA, Habarta N, Baron RC et al. Interventions to increase recommendation and delivery of screening for breast, cervical, and colorectal cancers by healthcare providers: Systematic reviews of provider assessment and feedback and provider incentives. Am J Prev Med 2008; 35: S67–S74.
Noar SM, Benac CN, Harris MS. Does tailoring matter? Meta-analytic review of tailored print health behavior change interventions. Psychol Bull 2007; 133: 673–693.
Sohl SJ, Moyer A. Tailored interventions to promote mammography screening: A meta-analytic review. Prev Med 2007; 45: 252–261.
Albada A, Ausems MGEM, Bensing JM, van Dulmen S. Tailored information about cancer risk and screening: A systematic review. Patient Educ Couns 2009 November; 77: 155–171.
Kreuter MW, Farrell D, Olevitch L, Brennan L. Tailoring health messages: Customizing communication with computer technology. Mahwah, NJ: Lawrence Erlbaum Associates; 2000.
Kreuter MW, Strecher VJ, Glassman B. One size does not fit all: The case for tailoring print materials. Ann Behav Med 1999; 21: 276–283.
Janz NK, Becker MH. The health belief model: A decade later. Health Educ Q 1984; 11: 1–47.
Diclemente CC, Prochaska JO. Toward a comprehensive transtheoretical model of change. In: Miller WR, Heather N, editors. Treating Addictive Behaviors. 2nd ed. New York, NY: Plenum Press; 2002. p. 3–24.
Smith RA, von Eschenbach A, Wender R et al. American Cancer Society guidelines for the early detection of cancer: Update of early detection guidelines for prostate, colorectal, and endometrial cancers. CA: Cancer J Clin 2001; 51: 38–75.
Godin G, Sheeran P, Conner M, Germain M. Asking questions changes behavior: Mere measurement effects on frequency of blood donation. Health Psychol 2008 March; 27: 179–184.
Jorgensen CM, Gelb CA, Merritt TL, Seeff LC. Observations from the CDC: CDC’s screen for life- a national colorectal cancer action campaign. J Womens Health Gend Based Med 2001; 10: 417–423.
Bartholomew LK, Parcel GS, Kok G, Gottlieb N, Fernandez ME. Planning Health Promotion Programs: An Intervention Mapping Approach 3rd edition. (in press). San Francisco,CA: Jossey-Bass; 2011.
Greisinger A, Hawley ST, Bettencourt JL, Perz CA, Vernon SW. Primary care patients’ understanding of colorectal cancer screening. Cancer Detect Prev 2006; 30: 67–74.
Vernon SW, McQueen A. Colorectal cancer screening. In: Jimmie C. Holland, William S. Breitbart, Paul B. Jacobsen, Marguerite S. Lederberg, Matthew J. Loscalzo, Ruth McCorkle, editors. Psycho-oncology. 2nd ed. ed. New York,NY: Oxford University Press; 2010. p. 71–83.
McQueen A, Vernon SW, Myers RE, Watts BG, Lee ES, Tilley BC. Correlates and predictors of colorectal cancer screening among male automotive workers. Cancer Epidemiol Biomarkers Prev 2007; 16: 500–509.
Lairson DR, Chang Y-C, Bettencourt JL, Vernon SW, Greisinger A. Estimating development cost for a tailored interactive computer program to enhance colorectal cancer screening compliance. JAMIA 2006 September; 13: 476–484.
McQueen A, Tiro JA, Vernon SW. Construct validity and invariance of four factors associated with colorectal cancer screening across gender, race, and prior screening. Cancer Epidemiol Biomarkers Prev 2008; 17: 2231–2237.
Vernon SW, Myers RE, Tilley BC. Development and validation of an instrument to measure factors related to colorectal cancer screening adherence. Cancer Epidemiol Biomarkers Prev 1997; 6: 825–832.
Ritvo P, Myers R, Del Giudice ML et al. Factorial validity and invariance of a survey measuring psychosocial correlates of colorectal cancer screening in Ontario, Canada--a replication study. Cancer Epidemiol Biomarkers Prev 2008 November; 17: 3279–3283.
Tiro JA, Vernon SW, Hyslop T, Myers RE. Factorial validity and invariance of a survey measuring psychosocial correlates of colorectal cancer screening among African Americans and Caucasians. Cancer Epidemiol Biomarkers Prev 2005; 14: 2855–2861.
Roserner B. Fundamentals of Biostatistics, 5th edition. Pacific Grove, CA: Duxbury; 2000.
Bland JM, Altman DG. Statistics notes: Multiple significance tests: The Bonferroni method. BMJ 1995 January 21; 310: 170.
Le Henanff A, Giraudeau B, Baron G, Ravaud P. Quality of reporting of noninferiority and equivalence randomized trials. JAMA 2006; 295: 1147–1151.
Myers RE, Sifri R, Hyslop T et al. A randomized controlled trial of the impact of targeted and tailored interventions on colorectal cancer screening. Cancer 2007; 110: 2083–2091.
Marcus AC, Mason M, Wolfe P, Rimer BK, Lipkus IM. The efficacy of tailored print materials in promoting colorectal cancer screening: Results from a randomized trial involving callers to the National Cancer Institute’s Cancer Information Service. J Health Commun 2005; 10: 83–104.
Rawl SM, Champion VL, Scott LL et al. A randomized trial of two print interventions to increase colon cancer screening among first-degree relatives. Patient Educ Couns 2008; 71: 215–227.
Ling BS, Schoen RE, Trauth JM et al. Physicians encouraging colorectal screening: A randomized controlled trial of enhanced office and patient management on compliance with colorectal cancer screening. Arch Intern Med 2009 January 12; 169: 47–55.
Lipkus IM, Skinner CS, Dement J et al. Increasing colorectal cancer screening among individuals in the carpentry trade: Test of risk communication interventions. Prev Med 2005; 40: 489–501.
Campbell MK, James AS, Hudson MA et al. Improving multiple behaviors for colorectal cancer prevention among African American church members. Health Psychol 2004 September; 23: 492–502.
Costanza ME, Luckmann R, Stoddard AM, White MJ, Stark JR, Avrunin JS. Using tailored telephone counseling to accelerate the adoption of colorectal cancer screening. Cancer Detect Prev 2007; 31: 191–198.
Basch CE, Wolf RL, Brouse CH et al. Telephone outreach to increase colorectal cancer screening in an urban minority population. Am J Public Health 2006; 96: 2246–2253.
Schroy PC, III, Glick JT, Robinson PA, Lydotes MA, Evans SR, Emmons KM. Has the surge in media attention increased public awareness about colorectal cancer and screening? J Community Health 2008 February; 33: 1–9.
Gollwitzer PM. Implementation intentions: Strong effects of simple plans. Am Psychol 1999 July; 54: 493–503.
Gollwitzer PM, Sheeran P. Implementation intentions and goal achievement: A meta-analysis of effects and processes. Adv Exp Soc Psychol 2006; 38: 69–119.
Dohan D, Schrag D. Using navigators to improve care of underserved patients: Current practices and approaches. Cancer 2005; 104: 848–855.
McQueen A, Bartholomew LK, Greisinger AJ et al. Behind Closed Doors: Physician-Patient Discussions About Colorectal Cancer Screening. J Gen Intern Med 2009 September 18; 24: 1228–1235.
Klabunde CN, Frame PS, Meadow A, Jones E, Nadel MR, Vernon SW. A national survey of primary care physicians’ colorectal cancer screening recommendations and practices. Prev Med 2003; 36: 352–362.
Klabunde CN, Lanier D, Nadel MR, McLeod C, Yuan G, Vernon SW. Colorectal cancer screening by primary care physicians: Recommendations and practices, 2006–2007. Am J Prev Med 2009 July; 37: 8–16.
Lafata JE, Divine G, Moon C, Williams LK. Patient-physician colorectal cancer screening discussions and screening use. Am J Prev Med 2006; 31: 202–209.
Neugut AI, Lebwohl B. Screening for colorectal cancer: The glass is half full. Am J Public Health 2009 April; 99: 592–4.
Woolf SH, Jones RM, Rothemich SF, Krist A. The priority is screening, not colonoscopy. Am J Public Health 2009 December; 99: 2117–8.
Lance P. Colorectal cancer screening: Confusion reigns. Cancer Epidemiol Biomarkers Prev 2008; 17: 2205–2207.
Schroy PC, Emmons K, Peters E et al. The impact of a novel computer-based decision aid on shared decision making for colorectal cancer screening: A randomized trial. Med Decis Making 2010 May 18. Available at: URL: http://mdm.sagepub.com/content/early/2010/05/10/0272989X10369007. Access verified 12/7/2010.
Pignone MP, Harris RP, Kinsinger LS. Videotape-based decision aid for colon cancer screening: A randomized, controlled trial. Ann Intern Med 2000; 133: 761–769.
Ruffin MT, Fetters MD, Jimbo M. Preference-based electronic decision aid to promote colorectal cancer screening: Results of a randomized controlled trial. Prev Med 2007 October; 45: 267–73.
Dolan JG, Frisina S. Randomized controlled trial of a patient decision aid for colorectal cancer screening. Med Decis Making 2002; 22: 125–139.
Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: Theory, research, and practice. 4th ed. San Francisco: Jossey-Bass; 2008. p. 97–121.
Michie S, Johnston M, Francis J, Hardeman W, Eccles M. From theory to intervention: Mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol 2008; 57: 660–80.
Mevissen FEF, Meertens RM, Ruiter RAC, Feenstra H, Schaalma HP. HIV/STI risk communication: The effects of scenario-based risk information and frequency-based risk information on perceived susceptibility to chlamydia and HIV. J Health Psychol 2009; 14: 78–87.
Suls J, Martin R, Wheeler L. Social comparison: Why, with whom, and with what effect? Curr Dir Psychol Sci 2002; 11: 159–63.
Acknowledgments
This project was supported by National Institutes of Health (RO1 NCI RO1 CA97263).
Conflict of Interest Statement
The authors have no conflict of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Vernon, S.W., Bartholomew, L.K., McQueen, A. et al. A Randomized Controlled Trial of a Tailored Interactive Computer-Delivered Intervention to Promote Colorectal Cancer Screening: Sometimes More is Just the Same. ann. behav. med. 41, 284–299 (2011). https://doi.org/10.1007/s12160-010-9258-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12160-010-9258-5