Abstract
The Centers for Disease Control and Prevention’s Screen for Life campaign in March 1999 followed by the creation of National Colorectal Cancer Awareness Month in March 2000 heralded a surge in media attention to promote awareness about CRC and stimulate interest in screening. Our objective was to assess whether these campaigns have achieved their goal of educating the public about CRC and screening. The study sample was comprised of mostly unscreened, average-risk, English-speaking patients aged 50–75 years seen in an urban primary care setting. Knowledge was assessed using a 12-item true/false questionnaire based primarily on the content of key messages endorsed by the National Colorectal Cancer Roundtable (Cancer 95:1618–1628, 2002) and adopted in many of the media campaigns. Multiple linear regression was performed to identify demographic correlates of knowledge. A total of 356 subjects (83% <age 65, 58% female, 60% Black, 7% Hispanic, 60% ≤high school degree, 31% prior FOBT ) were surveyed. Most respondents (≥67%) were aware of who gets CRC, age to initiate screening, the goals of screening and potential benefits. Fewer were aware that removing polyps can prevent CRC and that both polyps and CRC may be asymptomatic. Knowledge scores were lower among Blacks and those with a high school degree or less. Race and education were independent correlates of knowledge. These data suggest that recent media campaigns have been effective in increasing public awareness about CRC risk and screening but important gaps in knowledge remain.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Screening is a cost-effective strategy for decreasing CRC incidence and mortality [1–3]. Despite widespread endorsement by authoritative groups [4–7], screening rates remain low. Data from the 2004 Behavior Risk Factor Surveillance Survey suggest that although screening rates have improved in recent years, 43% of Americans have not been screened within currently recommended time intervals [8]. Lack of patient knowledge about the public health significance of CRC, relevant risk factors, the benefits of screening and specific screening tests have been identified as an important barrier to participation [9–12], particularly among minority and low income populations [13–17].
In an effort to increase public awareness about CRC and stimulate interest in screening, the Centers for Disease Control and Prevention (CDC) and the Health Care Financing Administration launched its multimedia Screen for Life: National Colorectal Cancer Action Campaign on March 2, 1999 [18, 19]. The campaign incorporated several key messages based on an extensive review of existing literature, formative qualitative research involving more than 170 focus groups, and concept testing. Soon thereafter March was declared National Colorectal Cancer Awareness Month by presidential proclamation in 2000, which in turn prompted a surge in mass multimedia campaigns sponsored by various public heath departments, professional societies and advocacy groups, such as the American Cancer Society (ACS), to promote awareness about CRC risk and CRC screening. Many of these campaigns incorporated key messages employed in the Screen for Life campaign and later endorsed by the National Colorectal Cancer Roundtable (NCCRT) in its national strategic plan [20]. The NCCRT is a national coalition of more than 60 public, private and voluntary organizations co-founded by the CDC and ACS in 1997 to provide leadership, long-term planning and coordination of interventions for reducing CRC morbidity and mortality through education, early detection and prevention. By endorsing a core set of key messages, the NCCRT and its member organizations set forth to promote a coordinated and cohesive public education campaign aimed at dispelling widespread misconceptions about risk and stimulating interest in screening. The objective of this study was to assess the extent to which these campaigns have achieved this goal.
Methods
Subjects and Recruitment Process
The study sample was comprised of average-risk patients participating in a randomized clinical trial designed to assess the impact of an interactive, computer-based decision aid on shared decision-making and CRC screening behavior. Subjects were deemed eligible if they were 50–75 years of age, had no prior CRC screening other than fecal occult blood testing [FOBT], and were under the care of one the primary care providers at Boston Medical Center or the South Boston Community Health Center. Potential subjects meeting any of the following criteria were excluded: (1) prior CRC screening by any method other than FOBT; (2) high-risk condition (personal history of colorectal cancer or polyps, family history of colorectal cancer or polyps involving one or more first degree relatives, or chronic inflammatory bowel disease); (3) lack of fluency in written and spoken English (since decision aid and personalized risk assessment tool were developed in English only); or (4) comorbidities that preclude CRC screening by any recommended method.
Subjects were recruited to participate in the randomized clinical trial by one of two methods. Patients due for screening were identified 2–4 weeks prior to a scheduled office visit and contacted directly by telephone or mail by one of the research assistants if deemed appropriate by the patient’s primary care provider. Those contacted by mail were asked to return a signed postcard acknowledging their interest. Alternatively, patients due for screening were identified by their provider at the time of a clinic visit and referred directly using an electronic “consent to contact” process. Regardless of the method used, potential subjects were ultimately contacted by phone by one of the research assistants, provided with a brief overview of the study, evaluated for eligibility and invited to participate using a passive informed consent process.
Study Design
Eligible subjects interested in participating in the randomized clinical trial were instructed to arrive one hour before a prearranged office visit with their provider. After obtaining informed consent, subjects were asked to complete a pretest comprised of 28 close-ended questions that assessed knowledge, beliefs, attitudes and behaviors related to CRC screening. The pretest was administered by one of three trained research assistants in a private office located in one of the ambulatory care clinics at Boston Medical Center or the South Boston Community Health Center. After completing the pretest, which took on average approximately 10 min, subjects were randomized to one of two intervention arms (decision aid plus personalized risk assessment tool with feedback or decision aid alone) and a control arm, each of which participated in an interactive computer session. Herein, we report our interim pretest knowledge data for the first 356 subjects.
The study protocol and recruitment process were both approved by the Institutional Review Board at both participating institutions.
Survey Instrument
The knowledge assessment subsection of the pretest included 12 questions (true/false don’t know) that asked about information conveyed in the NCCRT’s core set of key messages [20]. The individual questions are listed in Table 2. Most media campaigns, including the CDC’s “Screen for Life” and American Cancer Society’s “Polyp Man™” campaigns, incorporated many if not all of these messages. The only exception was the “colorectal cancer is the most common cause of cancer death among nonsmokers” message, which was promoted by the Massachusetts Department of Public Health in its statewide media campaigns [21].
Statistical Analyses
Descriptive statistics were used to characterize the study population, response data for individual knowledge questions and cumulative knowledge scores. The mean and standard deviation were calculated for continuous variable; frequencies and percentages were tabulated for categorical variable. Cumulative knowledge scores (range, 0–12) were derived by summing correct responses to the 12 individual knowledge questions. Associations between mean cumulative knowledge scores and demographic factors were analyzed using t-tests for two level categorical independent variables and analysis of variance (ANOVA) for more than two level categorical independent variables followed by Duncan’s pairwise comparisons. Multiple linear regression was performed to identify independent effects of correlates found significant in univariate analyses. Significance was defined at the P ≤ 0.05 level. All statistical analyses were performed using SAS 9.1.3 (SAS Institute, Inc., Cary, NC).
Results
Study Population
A total of 356 subjects were surveyed between March 8, 2005 and November 13, 2006. As shown in Table 1, the study population was predominantly under the age of 65 (83%), female (58%), Black (60%), and non-Hispanic (93%). A majority (60%) had attained more than a high school education. Only 31% had undergone FOBT in past; the remaining 69% had no prior screening experience.
Knowledge Scores
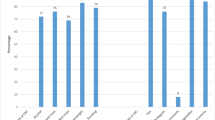
The overall mean cumulative knowledge score was 7.7 ± 2.7 (maximum score = 12). Scores for individual items are shown in Table 2. Most subjects were aware that both men and women are at risk (84%), risk increases after age 50 (71%), all racial and ethnic groups are affected (88%), the goal of screening is to find polyps and cancer before the onset of symptoms (82%), early-stage cancers may be curable with surgery (72%), screening should begin at age 50 (73%) and that CRC can occur in the absence of a family history (67%). Fewer patients were aware that both CRC (58%) and polyps (49%) may be asymptomatic, most CRC arises from polyps (52%), removing polyps can prevent CRC (46%), and CRC is the most common cause of cancer death among non-smokers (26%).
Demographic Correlates of Knowledge
Cumulative knowledge scores were associated with both race and education (Table 3). For race, scores were significantly higher for Whites compared to Blacks (8.3 ± 2.7 vs. 7.4 ± 2.5, P = 0.0016). For education, scores were significantly higher for subjects with more than a high school education compared to those with a high school degree or less (8.4 ± 2.6 vs. 7.3 ± 2.7, P = 0.0001). Both race (P = 0.005) and education (P = 0.005) were also found to be independent correlates of knowledge by multiple linear regression. Knowledge was not associated with age, sex, ethnicity, or prior FOBT.
Discussion
Public education campaigns have long been used to increase awareness about CRC and stimulate interest in screening, but their overall effectiveness remains unproven. Our study suggests that the surge in media attention heralded by the CDC’s Screen for Life campaign in 1999 has been effective in increasing public awareness about certain aspects of CRC screening and dispelling several misconceptions about risk. More specifically, we found that a diverse population of English-speaking average risk patients without prior screening experience (except possibly FOBT) seen in an urban, ambulatory care setting were aware that CRC affects both men and women of all racial and ethnic groups even in the absence of a family history, that risk increases after age 50, that screening should begin at age 50, that the goal of screening is to detect presymptomatic polyps and cancers, and that CRC is curable if detected early. Moreover, although racial disparities in knowledge were observed, overall knowledge for minority groups was relatively high.
Our findings contradict the results of several recently published studies suggesting that patient knowledge about CRC screening remains poor, despite the heightened media attention [12, 22–24]. In contradistinction to our study, most of these studies focused primarily on knowledge about particular screening tests rather than more general knowledge about CRC and screening [12, 22, 23]. The NCCRT specifically recommended against including information about specific CRC tests in public awareness campaigns because of concerns that communities across the country may be ill-prepared to deliver the full range of recommended screening options and because individuals have varying insurance coverage for the different tests [20]. Instead, the NCCRT recommends that these campaigns should promote awareness about screening in general and stimulate communication with a health care provider, who in turn could assume responsibility for discussing the pros and cons of various screening options within a shared decision-making framework. Another noteworthy difference is that at least two of these studies used qualitative methods (e.g., focus groups or face-to-face interviews) with open-ended questions to assess knowledge rather than the quantitative approach used in our study [23, 24]. One notable exception was the National Institute of Health’s 2002–2003 Health Information National Trends Survey (HINTS), which found that knowledge about age at which to initiate screening was relatively poor compared to our findings but knowledge about the goals of screening in terms of early detection was comparable [12, 22]. A third noteworthy difference is that each of these studies varied with respect to study population and setting. Consequently, it is important to acknowledge that the generalizeability of our findings may be limited to English-speaking populations seen in an urban, ambulatory care setting.
Our study has several other noteworthy limitations. First, because the study population consisted of subjects recruited to participate in a clinical trial assessing the impact of an interactive, computer-based decision aid on shared decision-making and adherence to CRC screening, concern about potential selection bias is warranted. Even though these subjects had no prior screening experience (other than possible FOBT), it is possible that they were better informed than patients not participating in the clinical trial. Second, it is impossible to validate that multimedia campaigns were the principle source of information for these patients. Although most acknowledged that the lack of a provider recommendation was the primary reason for not being screened in the past (data not shown), other sources of information, such as friends, relatives or acquaintances with CRC might be responsible. Regardless, we speculate that many of these sources, if not the participants themselves, acquired at least some of their information from the more than 4 billion Screen for Life audience impressions (the number of times the spots have been seen or heard by audience members) aired since March 1999 [25], Katie Couric’s highly publicized personal crusade (and nationally televised colonoscopy) on NBC’s Today Show, the American Cancer Society and Ad Council’s humorous “Polyp Man™” campaign, the Colon Cancer Alliance’s Colossal Colon annual nationwide tour, or the explosion of articles in the lay press and Internet during the time frame of interest. Thirdly, it is widely accepted that media campaigns alone are unlikely to change behavior and so it remains unknown whether increased knowledge translates into increased adherence. Nevertheless, the surge in demand for colonoscopy after Katie Couric’s Today Show media campaign in 2000 [26], as well as recent trends in use of colorectal cancer screening tests nationwide [8], suggests that the two may be causally related.
Despite its limitations, our study’s findings have important implications for future media campaigns. First, the observation that knowledge scores were significantly lower among non-Whites highlights the need for more effective, targeted media campaigns capable of reaching at-risk minority groups, as noted by Powe et al. [27]. Increased airplay of existing public service announcements (PSAs) in English and Spanish over radio stations or television channels that appeal to the target groups alone is unlikely to succeed, since this tactic has been employed in the Screen for Life campaign since March 2005. Instead, new PSAs could be developed that use credible minority spokespersons (e.g., celebrities or role models) to deliver key messages in a culturally and linguistically appropriate manner that resonates with the target population. To that end, the CDC has featured Oscar-Award winning actor Morgan Freeman and Academy Award-winning actor Jimmy Smits in its more recent Screen for Life public service announcements in hope of reaching African American and Hispanic audiences, respectively, more effectively [19]. Novel channels of delivery should also be explored such as the primetime television melodramas and situational comedies, movie trailers and the Internet.
A second implication of our findings is that media campaigns to date have been relatively ineffective in increasing awareness among less educated patient populations independent of race. Although the CDC found that the public preferred fact-based messages to other approaches in its formative studies [18], alternative formats for conveying key information (e.g., storytelling, humor or analogy) may be required for lower literacy and less educated groups. Novel channels for message delivery, such as those described for reaching minority populations in the foregoing paragraph, may also be effective in reaching this subset of individuals.
A third important implication is that media campaigns to date have also been ineffective in communicating several key messages. In particular, many patients were unaware that most cancers arise from pre-existing polyps and that removing polyps may prevent CRC, thus inferring that the “get the polyp, get the cure” message promoted in the “Polyp Man™” campaign is poorly understood by a sizeable proportion of the target population. Curiously, many patients were also unaware that both polyps and early stage cancers may be asymptomatic even though most were aware that the goal of screening is to detect presymptomatic disease. Not surprising, most patients were unaware that CRC is the leading cause of cancer-related death in non-smokers, since this was not one of the key messages conveyed in most of the more publicized national mass media campaigns. Based on these findings, formative studies are needed to assist in the design of new messages capable of better informing the public about the importance of polyps from the perspective of CRC prevention and presymptomatic detection of disease.
In conclusion, our data suggest that the recent surge in media attention has been effective in educating the public about certain aspects of CRC screening and dispelling certain misconceptions about risk. Nevertheless, these campaigns have been less effective in reaching certain segments of society, particularly Blacks and the less educated, and in communicating key messages about the importance of polyps and asymptomatic nature of early disease. Hence, novel sources, channels and formats for message delivery should be explored to minimize gaps in diffusion. Since the ultimate goal is to increase screening rates, future media campaigns should be linked with both community outreach and provider-based interventions to maximize effectiveness.
References
Winawer, S. J., Fletcher, R. H., Miller, L., et al. (1997). Colorectal cancer screening: Clinical guidelines and rationale. Gastroenterology, 112, 594–642.
Pignone, M., Saha, S., Hoerger, T., & Mandelblatt, J. (2002). Cost-effectiveness analyses of colorectal cancer screening: A systematic review for the U.S. Preventive Services Task Force. Annals of Internal Medicine, 137, 96–104.
Maciosek, M. V., Solberg, L. I., Coffield, A. B., Edwards, N. M., & Goodman, M. J. (2006). Colorectal cancer screening: Health impact and cost effectiveness. American journal of Preventive Medicine, 31, 80–89.
Rex, D. K., Johnson, D. A., Lieberman, D. A., Burt, R. W., & Sonnenberg, A. (2000). Colorectal cancer prevention 2000: Screening recommendations of the American College of Gastroenterology. American College of Gastroenterology. American Journal of Gastroenterology, 95, 868–877.
Winawer, S., Fletcher, R., Rex, D., et al. (2003). Colorectal cancer screening and surveillance: clinical guidelines and rationale-Update based on new evidence. Gastroenterology, 124, 544–560.
Smith, R. A., Cokkinides, V., von Eschenbach, A. C., et al. (2002). American Cancer Society guidelines for the early detection of cancer. CA: A Cancer Journal for Clinicians, 52, 8–22.
Pignone, M., Rich, M., Teutsch, S. M., Berg, A. O., & Lohr, K. N. (2002). Screening for colorectal cancer in adults at average risk: A summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine, 137, 132–141.
Centers for Disease Control and Prevention (2006). Increased use of colorectal cancer tests–United States, 2002 and 2004. MMWR Morbidity and Mortality Weekly Report, 55, 308–311.
Vernon, S. W. (1997). Participation in colorectal cancer screening: A review. Journal of the National Cancer Institute, 89, 1406–1422.
Klabunde, C. N., Schenck, A. P., & Davis, W. W. (2006). Barriers to colorectal cancer screening among Medicare consumers. American Journal of Preventive Medicine, 30, 313–319.
Klabunde, C. N., Vernon, S. W., Nadel, M. R., Breen, N., Seeff, L. C., & Brown, M. L. (2005). Barriers to colorectal cancer screening: A comparison of reports from primary care physicians and average-risk adults. Medical Care, 43, 939–944.
McQueen, A., Vernon, S. W., Meissner, H. I., Klabunde, C. N., & Rakowski, W. (2006). Are there gender differences in colorectal cancer test use prevalence and correlates?. Cancer Epidemiology, Biomarkers & Prevention, 15, 782–791.
Lipkus, I. M., Rimer, B. K., Lyna, P. R., Pradhan, A. A., Conaway, M., & Woods-Powell, C. T. (1996). Colorectal screening patterns and perceptions of risk among African-American users of a community health center. Journal of Community Health, 21, 409–427.
Lipkus, I. M., Lyna, P. R., & Rimer, B. K. (2000). Colorectal cancer risk perceptions and screening intentions in a minority population. Journal of the National Medical Association, 92, 492–500.
James, A. S., Campbell, M. K., & Hudson, M. A. (2002). Perceived barriers and benefits to colon cancer screening among African Americans in North Carolina: How does perception relate to screening behavior? Cancer Epidemiology, Biomarkers & Prevention, 11, 529–534.
Holmes-Rovner, M., Williams, G. A., Hoppough, S., Quillan, L., Butler, R., & Given, C. W. (2002). Colorectal cancer screening barriers in persons with low income. Cancer Practice, 10, 240–247.
Wee, C. C., McCarthy, E. P., & Phillips, R. S. (2005). Factors associated with colon cancer screening: The role of patient factors and physician counseling. Preventive Medicine, 41, 23–29.
Jorgensen, C. M., Gelb, C. A., Merritt, T. L., & Seeff, L. C. (2001). Observations from the CDC: CDC’s screen for life: A National Colorectal Cancer Action Campaign. Journal of Women's Health & Gender-Based Medicine, 10, 417–422.
Centers for Disease Control and Prevention. Screen for life campaign. Available from URL: http://www.cdc.gov/cancer/colorectal/sfl/ [accessed April 1, 2007].
Levin, B., Smith, R. A., Feldman, G. E., et al. (2002). Promoting early detection tests for colorectal carcinoma and adenomatous polyps: A framework for action: the strategic plan of the National Colorectal Cancer Roundtable. Cancer, 95, 1618–1628.
Massachusetts Department of Public Health. Colorectal cancer. Available from URL: http://www.mass.gov/dph/cancer/colorectal_cancer.htm [accessed April 1, 2007].
Ford, J. S., Coups, E. J., & Hay, J. L. (2006). Knowledge of colon cancer screening in a national probability sample in the United States. Journal of Health Communication, 11(Suppl 1), 19–35.
Shokar, N. K., Vernon, S. W., & Weller, S. C. (2005). Cancer and colorectal cancer: knowledge, beliefs, and screening preferences of a diverse patient population. Family Medicine, 37, 341–347.
Greiner, K. A., Born, W., Nollen, N., & Ahluwalia, J. S. (2005). Knowledge and perceptions of colorectal cancer screening among urban African Americans. Journal of General Internal Medicine, 20, 977–983.
Centers for Disease Control and Prevention. Colorectal cancer campaign overview—2007. Available from URL: http://www.cdc.gov/cancer/colorectal/pdf/backgrounder_2007.pdf [accessed April 4, 2007].
Cram, P., Fendrick, A. M., Inadomi, J., Cowen, M. E., Carpenter, D., & Vijan, S. (2003). The impact of a celebrity promotional campaign on the use of colon cancer screening: The Katie Couric effect. Archives of Internal Medicine, 163, 1601–1605.
Powe, B. D., Finnie, R., & Ko, J. (2006). Enhancing knowledge of colorectal cancer among African Americans: why are we waiting until age 50? Gastroenterology Nursing, 29, 42–49.
Acknowledgment
Grant support provided by Agency for Healthcare Research and Quality grant RO1HS013912 (P. C. Schroy).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schroy, P.C., Glick, J.T., Robinson, P.A. et al. Has the Surge in Media Attention Increased Public Awareness About Colorectal Cancer and Screening?. J Community Health 33, 1–9 (2008). https://doi.org/10.1007/s10900-007-9065-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-007-9065-5