Abstract
Compared to the clear trend observed in previous years, the number of peer-reviewed articles published during 2015 and retrieved using the “autoimmunity” key word declined by 4 %, while remaining 5 % of immunology articles. On the other hand, a more detailed analysis of the published articles in leading immunology and autoimmunity journals revealed exciting scenarios, with fascinating lines of evidence being supported by convincing data and likely followed by rapid translational or clinical developments. As examples, the study of the microbiome, the development of new serum or other tissue biomarkers, and a more solid understanding of disease pathogenesis and tolerance breakdown mechanisms have been central issues in the past year. Furthermore and similar to the oncology field, progress in the understanding of single autoimmune condition is becoming most specific with psoriatic and rheumatoid arthritis being ideal paradigms with treatment options diverging after decades of common therapies, as illustrated by IL17-targeting approaches. The ultimate result of these advances is towards personalized medicine with an ideal approach being tailored on a single patient, based on a finely tuned definition of the immunogenetics, epigenetics, microbiome, and biomarkers. Finally, experimental reports suggest that cancer-associated immune mechanisms or the role of T and B cell subpopulations should be better understood in autoimmune diseases. While we hailed the 2014 literature in the autoimmunity world as part of an annus mirabilis, we should not be mistaken in the strong stimulus of research in autoimmunity represented by the 2015 articles that will be summarized in this article.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Was 2015 a Regular Year in Autoimmunity?
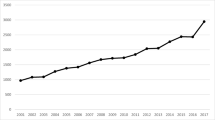
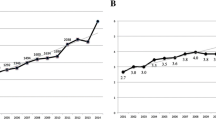
One year ago [1] and in previous years, we provided an overview of the publications dedicated to autoimmunity over 12 months and in 2015 confirmed a steady growth in the absolute number of papers on PubMed. The 2014 scenario was most surprising with the highest increase in the absolute number of publications (+28 %) compared to 2013 with a stable ratio with the immunology publications around 5 %. This year, a PubMed search was performed in May 2016 and retrieved 2595 articles published in English between January 1st and December 31st 2015 using “autoimmunity” as search word, and results are illustrated in Fig. 1. Among publications from 2015, we perused the major journals in the areas of immunology (Nature Immunology, Nature Medicine, Clinical and Experimental Immunology, Clinical Reviews in Allergy and Immunology) and autoimmunity (Autoimmunity, Autoimmunity Reviews, Journal of Autoimmunity) and arbitrarily selected those belonging to major clinical topics for further discussion. Quite obviously, this approach leads to an underrepresentation of rare disease [2–6], particularly vasculitidies [7–13] and sarcoidosis [14–22], or other fascinating issues such as the relationship with cancer both in terms of common mechanisms [23–26] or paraneoplastic autoimmunity [27–29]. Similarly, major cross-sectional issues are necessarily overlooked by the chosen approach, as well represented by T regulatory cells in the maintainance of peripheral tolerance [30–55] or new mechanisms of central tolerance, traditionally the subject of limited studies in human autoimmunity [55–66]. Quite interestingly, when we charted the number of 2015 publications including MeSH terms of major autoimmune diseases versus the reported highest prevalence rates [67], we observed a significant discrepancy with most frequent conditions being the subject of very few studies and vice versa (Fig. 2).
The chart illustrates the number of 2015 publications including MeSH terms of major autoimmune diseases versus the reported highest prevalence rates (per 100.000). The figure is intended to be indicative of the lack of association between these two figures and necessarily includes epidemiological studies based on different case finding methods
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) remained a hot topic for research in 2015 with a vast number of experimental articles and reviews being devoted to the mechanisms and the clinical features of the disease. There is now agreement that SLE onset requires a genetic [68, 69] or immunogenetic [70, 71] susceptibility on which environmental factors, as in the case of the microbiota [72, 73], oxidative stress [74], and infectious agents [75], but apparently not adjuvants [76], may act and induce immunosenescence [77] and favor tolerance breakdown via other mechanisms [78–80], similar to what was observed in other connective tissue diseases [81]. From a clinical standpoint, there is a lively discussion on SLE clinimetrics or natural history [82–86] and data were presented on glucocorticoid receptors influence on SLE therapy outcomes, and the therapeutic use of regulatory T cells, mesenchymal stem cells, B-cells or natural killer cells [87], targeting FcalphaRI [88], inhibiting calcium/calmodulin-dependent protein kinase IV specific for CD4(+) T cells via a nanolipogel system [89], B cell depletion via rituximab [90] or epratuzumab [91], and high- or low-dose steroids [92]. Finally, promising data were presented with the use of helminth-derived tuftsin-phosphorylcholine which may modulate the immune response and prove beneficial in SLE [93] as in other autoimmune diseases [94]. On the other hand, there were major contributions on crucial issues such as reproductive health in women with SLE [95, 96] or the manifestations and treatment of anti-phospholipid syndrome [97–101].
Among experimental articles, reports were of particular importance in dissecting the link between chronic inflammation and atherosclerosis in SLE. Black and Colleagues suggested that cholesterol may not be the only factor modulating inflammation and atherosclerosis in a normocholesterolemic lupus-prone mouse model [102], while others reported the increased recruitment of pro-inflammatory CD4+ CXCR3+ T cells into the arterial wall following IFN-alpha production by TLR 9-stimulated plasmacytoid dendritic cells [103], possibly via epigenetic mechanisms [104, 105] controlling type I INF [105] and other genes [74, 106], while IFN-gamma may also impact disease progression [107]. B cells and autoantibodies remain central to SLE pathogenesis and several experimental articles addressed this issue by investigating how pro-inflammatory factors, especially type I IFNalpha, are important in the B cell hyper-responsiveness to BCR crosslinking in SLE [108], the high number of B1 cells mediated by BLK expression [109], how, among numerous clinically relevant biomarkers [110–113], pentraxin 3 (PTX3) [114] is expressed in lupus nephritis, primarily if anti-PTX3 antibodies are absent and correlates with fibrosis [115], how the BAFF receptor TACI may act as a promising therapeutic target [116].
Rheumatoid Arthritis and Spondyloarthritis
The field of chronic arthritis includes two major players in rheumatoid arthritis (RA) and spondyloarthritis (SpA) which recognize different pathogenesis and clinical features with less typical manifestations [117] or comorbidities [118, 119] in these systemic conditions. In the case of RA, major hints to etiology are derived from the high specificity of serum antibodies directed at citrullinated peptides since the earliest reports [117, 120, 121], with the subsequent migration of inflammatory cells, including osteoclasts [122], causing synovitis and erosions [123]. From a genetic standpoint, RA-associated polymorphisms are linked to functionally relevant phenotypes [124] and may help, along with different biomarkers such as microRNA [125] or long non-coding RNA [126], to array patients according to the disease manifestations, as in the case of bone erosions [127]. Ultimately, this personalization becomes of great importance in selecting the ideal therapeutic approach, considering the growing number of options [128], now including intravenous immunoglobulins [129] or monoclonal antibodies against recently involved cytokines such as IL22 [130], IL27 [131], IL37 [132], or angiotensin II [133], with more attention on hard outcomes of treatment such as the prevention of cardiovascular events [134]. New exciting evidence with putative treatment development includes immunosuppressive strategies via tolerance induction in autoreactive T cells [135] or targeting memory T cells using specific differentially expressed surface molecules or downstream signaling pathway proteins [136].
While biosimilars and comorbidities constitute new challenges [137–139], the rapid growth in our understanding of the pathogenesis of psoriasis and psoriatic arthritis over the past decade has been paralleled by the development of specific treatments which are not derived from RA or other rheumatological conditions, as supported by the different immunogenetic profiles [140] which also differentiates from other skin inflammatory [141, 142] or fibrotic [143] diseases. Indeed, a recent report suggested a common HLA susceptibility background for psoriasis and graft-versus-host disease [144]. Furthermore, psoriasis is now considered an autoimmune disease based on the identification of LL37 as an autoantigen for T cells [145] in patients with aggressive disease and the associated decrease of circulating CD4 + CXCR3+ T cells which in turn accumulate in the inflamed skin [146] or the role of MCAM (CD146) T cells [147]. T cells in psoriatic disease are indeed quite unique [145] and their production of IL17 represent a key to systemic [148] and skin [149] chronic inflammation and psoriatic articular manifestations [150] while new mechanisms for Th17 cells to influence the antimicrobial response were identified within IL26 [151] and the role of neutrophil extracellular traps (NET) awaits further definition [152]. Ultimately, psoriatic arthritis represents a paradigm for the spectrum of seronegative SpA and data on entheropatic SpA and their serological [153, 154] and immunogenetic [155–157] profiles or the ocular manifestations [158] support the urgent need for a multidisciplinary approach to autoimmune diseases as data on new treatments also converge on common mechanisms [159, 160].
Neuroimmunology
As in previous years, the field of neuroimmunology includes multiple sclerosis (MS) as the most prominent condition and this is reflected by the large number of articles in 2015, spanning from genetic and epigenetic disease susceptibility [161, 162] to biomarkers [163, 164] to potentially revolutionary treatments using helminths [165] or embryonic stem cells [166], among other reports [167–172]. From a pathogenic standpoint, a few reports were of major interest during the past year. First, there is growing attention on the mechanisms of antigen-specific B cells driving the central nervous system autoimmunity [173] via IFNbeta [174]. Second, IL17 role is rapidly gaining attention as represented by its involvement in optic nerve injury during MS [175–177] while new agents such as IL7 should also be considered [178]. Third, TNF receptor deficiency and the intestinal microbiota diversity concur to induce demyelinating diseases and support the search for host immune-microbiota-directed measures to prevent and treat CNS-demyelinating autoimmune disorders [179]. Fourth, there are now novel approaches to reinstate tolerance in MS and these are mostly based on promiscuous gene expression in medullary thymic epithelial cells [180]. Finally, the impact of Th and Treg cells in MS is better understood and will likely lead to new therapeutic avenues [181–186].
What to Expect in 2016
As in previous years, during 2015, common themes across autoimmune diseases significantly outnumbered differences and the former were particularly intriguing, as in the case of immunogenetic determinants [13, 16, 70, 124, 140, 155, 161, 187–191] on disease susceptibility, or the role of the microbiota [72, 179, 192, 193] on disease onset and progression or on treatment response which ultimately result in personalized medicine. Nonetheless, we feel that other reports from our literature search may prove key to future discoveries and we may foresee new developments to stem from rare disease paradigms or from cancer-like mechanisms while futuristic treatments will likely become more established in specific subgroups of patients.
References
Selmi C (2015) Autoimmunity in 2014. Clin Rev Allergy Immunol 49:93–99
Ceresini G, Urban ML, Corradi D, Lauretani F, Marina M, Usberti E, Palmisano A, Buzio C, Vaglio A (2015) Association between idiopathic retroperitoneal fibrosis and autoimmune thyroiditis: a case-control study. Autoimmun Rev 14:16–22
van Schaarenburg RA, Schejbel L, Truedsson L, Topaloglu R, Al-Mayouf SM, Riordan A, Simon A, Kallel-Sellami M, Arkwright PD, Ahlin A, Hagelberg S, Nielsen S, Shayesteh A, Morales A, Tam S, Genel F, Berg S, Ketel AG, Merlijn Van Den Berg J, Kuijpers TW, Olsson RF, Huizinga TW, Lankester AC, Trouw LA (2015) Marked variability in clinical presentation and outcome of patients with C1q immunodeficiency. J Autoimmun 62:39–44
Almeida I, Silva SV, Fonseca AR, Silva I, Vasconcelos C, Lima M (2015) T and NK cell phenotypic abnormalities in systemic sclerosis: a cohort study and a comprehensive literature review. Clin Rev Allergy Immunol 49:347–369
Cozzani E, Gasparini G, Burlando M, Drago F, Parodi A (2015) Atypical presentations of bullous pemphigoid: clinical and immunopathological aspects. Autoimmun Rev 14:438–445
Floreani A, Franceschet I, Perini L, Cazzagon N, Gershwin ME, Bowlus CL (2015) New therapies for primary biliary cirrhosis. Clin Rev Allergy Immunol 48:263–272
Alba MA, Moreno-Palacios J, Beca S, Cid MC (2015) Urologic and male genital manifestations of granulomatosis with polyangiitis. Autoimmun Rev 14:897–902
Berti A, Campochiaro C, Cavalli G, Pepe G, Praderio L, Sabbadini MG, Dagna L (2015) Giant cell arteritis restricted to the limb arteries: an overlooked clinical entity. Autoimmun Rev 14:352–357
Chimenti MS, Ballanti E, Triggianese P, Perricone R (2015) Vasculitides and the complement system: a comprehensive review. Clin Rev Allergy Immunol 49:333–346
Greco A, Rizzo MI, De Virgilio A, Gallo A, Fusconi M, Ruoppolo G, Altissimi G, De Vincentiis M (2015) Churg-Strauss syndrome. Autoimmun Rev 14:341–348
Renauer P, Coit P, Sawalha AH (2016) Epigenetics and vasculitis: a comprehensive review. Clin Rev Allergy Immunol 50(3):357–66.
Fredi M, Lazzaroni MG, Tani C, Ramoni V, Gerosa M, Inverardi F, Sfriso P, Caramaschi P, Andreoli L, Sinico RA, Motta M, Lojacono A, Trespidi L, Strigini F, Brucato A, Caporali R, Doria A, Guillevin L, Meroni PL, Montecucco C, Mosca M, Tincani A (2015) Systemic vasculitis and pregnancy: a multicenter study on maternal and neonatal outcome of 65 prospectively followed pregnancies. Autoimmun Rev 14:686–691
Takeuchi M, Kastner DL, Remmers EF (2015) The immunogenetics of Behcet’s disease: a comprehensive review. J Autoimmun 64:137–148
Baughman RP, Lower EE (2015) Treatment of sarcoidosis. Clin Rev Allergy Immunol 49:79–92
Chen ES, Moller DR (2015) Etiologies of sarcoidosis. Clin Rev Allergy Immunol 49:6–18
Grunewald J, Spagnolo P, Wahlstrom J, Eklund A (2015) Immunogenetics of disease-causing inflammation in sarcoidosis. Clin Rev Allergy Immunol 49:19–35
Jamilloux Y, Valeyre D, Lortholary O, Bernard C, Kerever S, Lelievre L, Neel A, Broussolle C, Seve P (2015) The spectrum of opportunistic diseases complicating sarcoidosis. Autoimmun Rev 14:64–74
Judson MA (2015) The clinical features of sarcoidosis: a comprehensive review. Clin Rev Allergy Immunol 49:63–78
Rossi G, Cavazza A, Colby TV (2015) Pathology of sarcoidosis. Clin Rev Allergy Immunol 49:36–44
Silva M, Nunes H, Valeyre D, Sverzellati N (2015) Imaging of sarcoidosis. Clin Rev Allergy Immunol 49:45–53
Spagnolo P (2015) Sarcoidosis: a critical review of history and milestones. Clin Rev Allergy Immunol 49:1–5
Wessendorf TE, Bonella F, Costabel U (2015) Diagnosis of sarcoidosis. Clin Rev Allergy Immunol 49:54–62
Blidner AG, Salatino M, Mascanfroni ID, Diament MJ, Bal De Kier Joffe E, Jasnis MA, Klein SM, Rabinovich GA (2015) Differential response of myeloid-derived suppressor cells to the nonsteroidal anti-inflammatory agent indomethacin in tumor-associated and tumor-free microenvironments. J Immunol 194:3452–3462
Campbell DJ (2015) Control of regulatory T cell migration function, and homeostasis. J Immunol 195:2507–2513
Hou TZ, Qureshi OS, Wang CJ, Baker J, Young SP, Walker LS, Sansom DM (2015) A transendocytosis model of CTLA-4 function predicts its suppressive behavior on regulatory T cells. J Immunol 194:2148–2159
Penaloza-Macmaster P, Provine NM, Blass E, Barouch DH (2015) CD4 T cell depletion substantially augments the rescue potential of PD-L1 blockade for deeply exhausted CD8 T cells. J Immunol 195:1054–1063
Gunawardena H (2015) The clinical features of myositis-associated autoantibodies: a review. Clin Rev Allergy Immunol. [Epub ahead of print]
Islam AD, Selmi C, Datta-Mitra A, Sonu R, Chen M, Gershwin ME, Raychaudhuri SP (2015) The changing faces of IgG4-related disease: clinical manifestations and pathogenesis. Autoimmun Rev 14:914–922
Tiniakou E, Mammen AL (2015) Idiopathic inflammatory myopathies and malignancy: a comprehensive review. Clin Rev Allergy Immunol. [Epub ahead of print]
Bell CJ, Sun Y, Nowak UM, Clark J, Howlett S, Pekalski ML, Yang X, Ast O, Waldhauer I, Freimoser-Grundschober A, Moessner E, Umana P, Klein C, Hosse RJ, Wicker LS, Peterson LB (2015) Sustained in vivo signaling by long-lived IL-2 induces prolonged increases of regulatory T cells. J Autoimmun 56:66–80
Caramalho I, Nunes-Silva V, Pires AR, Mota C, Pinto AI, Nunes-Cabaco H, Foxall RB, Sousa AE (2015) Human regulatory T-cell development is dictated by interleukin-2 and -15 expressed in a non-overlapping pattern in the thymus. J Autoimmun 56:98–110
Joly AL, Liu S, Dahlberg CI, Mailer RK, Westerberg LS, Andersson J (2015) Foxp3 lacking exons 2 and 7 is unable to confer suppressive ability to regulatory T cells in vivo. J Autoimmun 63:23–30
Liu J, Cao X (2015) Regulatory dendritic cells in autoimmunity: a comprehensive review. J Autoimmun 63:1–12
Lu FT, Yang W, Wang YH, Ma HD, Tang W, Yang JB, Li L, Ansari AA, Lian ZX (2015) Thymic B cells promote thymus-derived regulatory T cell development and proliferation. J Autoimmun 61:62–72
Nouel A, Pochard P, Simon Q, Segalen I, Le Meur Y, Pers JO, Hillion S (2015) B-cells induce regulatory T cells through TGF-beta/IDO production in a CTLA-4 dependent manner. J Autoimmun 59:53–60
Rissiek A, Baumann I, Cuapio A, Mautner A, Kolster M, Arck PC, Dodge-Khatami A, Mittrucker HW, Koch-Nolte F, Haag F, Tolosa E (2015) The expression of CD39 on regulatory T cells is genetically driven and further upregulated at sites of inflammation. J Autoimmun 58:12–20
Rosenzwajg M, Churlaud G, Mallone R, Six A, Derian N, Chaara W, Lorenzon R, Long SA, Buckner JH, Afonso G, Pham HP, Hartemann A, Yu A, Pugliese A, Malek TR, Klatzmann D (2015) Low-dose interleukin-2 fosters a dose-dependent regulatory T cell tuned milieu in T1D patients. J Autoimmun 58:48–58
Wang YH, Yang W, Yang JB, Jia YJ, Tang W, Gershwin ME, Ridgway WM, Lian ZX (2015) Systems biologic analysis of T regulatory cells genetic pathways in murine primary biliary cirrhosis. J Autoimmun 59:26–37
Alissafi T, Hatzioannou A, Ioannou M, Sparwasser T, Grun JR, Grutzkau A, Verginis P (2015) De novo-induced self-antigen-specific Foxp3+ regulatory T cells impair the accumulation of inflammatory dendritic cells in draining lymph nodes. J Immunol 194:5812–5824
Bending D, Giannakopoulou E, Lom H, Wedderburn LR (2015) Synovial regulatory T cells occupy a discrete TCR niche in human arthritis and require local signals to stabilize FOXP3 protein expression. J Immunol 195:5616–5624
Burns JC, Touma R, Song Y, Padilla RL, Tremoulet AH, Sidney J, Sette A, Franco A (2015) Fine specificities of natural regulatory T cells after IVIG therapy in patients with Kawasaki disease. Autoimmunity 48:181–188
Dhaeze T, Stinissen P, Liston A, Hellings N (2015) Humoral autoimmunity: a failure of regulatory T cells? Autoimmun Rev 14:735–741
Dwivedi M, Kemp EH, Laddha NC, Mansuri MS, Weetman AP, Begum R (2015) Regulatory T cells in vitiligo: implications for pathogenesis and therapeutics. Autoimmun Rev 14:49–56
Fuhrman CA, Yeh WI, Seay HR, Saikumar Lakshmi P, Chopra G, Zhang L, Perry DJ, McClymont SA, Yadav M, Lopez MC, Baker HV, Zhang Y, Li Y, Whitley M, von Schack D, Atkinson MA, Bluestone JA, Brusko TM (2015) Divergent phenotypes of human regulatory T cells expressing the receptors TIGIT and CD226. J Immunol 195:145–155
Gibson VB, Nikolic T, Pearce VQ, Demengeot J, Roep BO, Peakman M (2015) Proinsulin multi-peptide immunotherapy induces antigen-specific regulatory T cells and limits autoimmunity in a humanized model. Clin Exp Immunol 182:251–260
Hsu P, Santner-Nanan B, Hu M, Skarratt K, Lee CH, Stormon M, Wong M, Fuller SJ, Nanan R (2015) IL-10 potentiates differentiation of human induced regulatory T cells via STAT3 and Foxo1. J Immunol 195:3665–3674
Huang Y, Yang Z, Huang C, Mcgowan J, Casper T, Sun D, Born WK, O’Brien RL (2015) Gammadelta T cell-dependent regulatory T cells prevent the development of autoimmune keratitis. J Immunol 195:5572–5581
Jones A, Opejin A, Henderson JG, Gross C, Jain R, Epstein JA, Flavell RA, Hawiger D (2015) Peripherally induced tolerance depends on peripheral regulatory T cells that require hopx to inhibit intrinsic IL-2 expression. J Immunol 195:1489–1497
Mohammadnia-Afrouzi M, Zavaran Hosseini A, Khalili A, Abediankenari S, Hosseini V, Maleki I (2015) Decrease of CD4(+) CD25(+) CD127(low) FoxP3(+) regulatory T cells with impaired suppressive function in untreated ulcerative colitis patients. Autoimmunity 48:556–561
Petrillo MG, Ronchetti S, Ricci E, Alunno A, Gerli R, Nocentini G, Riccardi C (2015) GITR+ regulatory T cells in the treatment of autoimmune diseases. Autoimmun Rev 14:117–126
Rossetti M, Spreafico R, Saidin S, Chua C, Moshref M, Leong JY, Tan YK, Thumboo J, van Loosdregt J, Albani S (2015) Ex vivo-expanded but not in vitro-induced human regulatory T cells are candidates for cell therapy in autoimmune diseases thanks to stable demethylation of the FOXP3 regulatory T cell-specific demethylated region. J Immunol 194:113–124
Singh Y, Garden OA, Lang F, Cobb BS (2015) MicroRNA-15b/16 enhances the induction of regulatory T cells by regulating the expression of rictor and mTOR. J Immunol 195:5667–5677
Yaciuk JC, Pan Y, Schwarz K, Pan ZJ, Maier-Moore JS, Kosanke SD, Lawrence C, Farris AD (2015) Defective selection of thymic regulatory T cells accompanies autoimmunity and pulmonary infiltrates in Tcra-deficient mice double transgenic for human La/Sjogren’s syndrome-B and human La-specific TCR. J Immunol 194:1514–1522
Yu F, Sharma S, Edwards J, Feigenbaum L, Zhu J (2015) Dynamic expression of transcription factors T-bet and GATA-3 by regulatory T cells maintains immunotolerance. Nat Immunol 16:197–206
Charbonnier LM, Wang S, Georgiev P, Sefik E, Chatila TA (2015) Control of peripheral tolerance by regulatory T cell-intrinsic notch signaling. Nat Immunol 16:1162–1173
Chuprin A, Avin A, Goldfarb Y, Herzig Y, Levi B, Jacob A, Sela A, Katz S, Grossman M, Guyon C, Rathaus M, Cohen HY, Sagi I, Giraud M, McBurney MW, Husebye ES, Abramson J (2015) The deacetylase Sirt1 is an essential regulator of aire-mediated induction of central immunological tolerance. Nat Immunol 16:737–745
Kil LP, Corneth OB, de Bruijn MJ, Asmawidjaja PS, Krause A, Lubberts E, van Loo PF, Hendriks RW (2015) Surrogate light chain expression beyond the pre-B cell stage promotes tolerance in a dose-dependent fashion. J Autoimmun 57:30–41
King JK, Philips RL, Eriksson AU, Kim PJ, Halder RC, Lee DJ, Singh RR (2015) Langerhans cells maintain local tissue tolerance in a model of systemic autoimmune disease. J Immunol 195:464–476
Lind EF, Millar DG, Dissanayake D, Savage JC, Grimshaw NK, Kerr WG, Ohashi PS (2015) miR-155 upregulation in dendritic cells is sufficient to break tolerance in vivo by negatively regulating SHIP1. J Immunol 195:4632–4640
Nguyen TT, Elsner RA, Baumgarth N (2015) Natural IgM prevents autoimmunity by enforcing B cell central tolerance induction. J Immunol 194:1489–1502
Reinert-Hartwall L, Honkanen J, Salo HM, Nieminen JK, Luopajarvi K, Harkonen T, Veijola R, Simell O, Ilonen J, Peet A, Tillmann V, Knip M, Vaarala O, Group DS, Group DS (2015) Th1/Th17 plasticity is a marker of advanced beta cell autoimmunity and impaired glucose tolerance in humans. J Immunol 194:68–75
Schaffert SA, Loh C, Wang S, Arnold CP, Axtell RC, Newell EW, Nolan G, Ansel KM, Davis MM, Steinman L, Chen CZ (2015) mir-181a-1/b-1 modulates tolerance through opposing activities in selection and peripheral T cell function. J Immunol 195:1470–1479
Williams JM, Bonami RH, Hulbert C, Thomas JW (2015) Reversing tolerance in isotype switch-competent anti-insulin B lymphocytes. J Immunol 195:853–864
Wong EB, Soni C, Chan AY, Domeier PP, Shwetank, Abraham T, Limaye N, Khan TN, Elias MJ, Chodisetti SB, Wakeland EK, Rahman ZS (2015) B cell-intrinsic CD84 and Ly108 maintain germinal center B cell tolerance. J Immunol 194:4130–4143
Xu X, Zhang S, Jin R, Wang K, Li P, Lin L, Dong J, Hao J, Zhang Y, Sun X, Pang X, Qian X, Zhang J, Wu H, Zhang Y, Ge Q (2015) Retention and tolerance of autoreactive CD4(+) recent thymic emigrants in the liver. J Autoimmun 56:87–97
Yuan X, Dee MJ, Altman NH, Malek TR (2015) IL-2Rbeta-dependent signaling and CD103 functionally cooperate to maintain tolerance in the gut mucosa. J Immunol 194:1334–1346
Cooper GS, Bynum ML, Somers EC (2009) Recent insights in the epidemiology of autoimmune diseases: improved prevalence estimates and understanding of clustering of diseases. J Autoimmun 33:197–207
Relle M, Weinmann-Menke J, Scorletti E, Cavagna L, Schwarting A (2015) Genetics and novel aspects of therapies in systemic lupus erythematosus. Autoimmun Rev 14:1005–1018
Goury A, Meghraoui-Kheddar A, Belmokhtar K, Vuiblet V, Ortillon J, Jaisson S, Devy J, Le Naour R, Tabary T, Cohen JH, Schmidt AM, Rieu P, Toure F (2015) Deletion of receptor for advanced glycation end products exacerbates lymphoproliferative syndrome and lupus nephritis in B6-MRL Fas lpr/j mice. J Immunol 194:3612–3622
Ghodke-Puranik Y, Niewold TB (2015) Immunogenetics of systemic lupus erythematosus: a comprehensive review. J Autoimmun 64:125–136
Pontillo A, Reis EC, Liphaus BL, Silva CA, Carneiro-Sampaio M (2015) Inflammasome polymorphisms in juvenile systemic lupus erythematosus. Autoimmunity 48:434–437
Johnson BM, Gaudreau MC, Al-Gadban MM, Gudi R, Vasu C (2015) Impact of dietary deviation on disease progression and gut microbiome composition in lupus-prone SNF1 mice. Clin Exp Immunol 181:323–337
Gaudreau MC, Johnson BM, Gudi R, Al-Gadban MM, Vasu C (2015) Gender bias in lupus: does immune response initiated in the gut mucosa have a role? Clin Exp Immunol 180:393–407
Strickland FM, Li Y, Johnson K, Sun Z, Richardson BC (2015) CD4(+) T cells epigenetically modified by oxidative stress cause lupus-like autoimmunity in mice. J Autoimmun 62:75–80
Slight-Webb SR, Bagavant H, Crowe SR, James JA (2015) Influenza a (H1N1) virus infection triggers severe pulmonary inflammation in lupus-prone mice following viral clearance. J Autoimmun 57:66–76
Annable T, Tomassian T, Jain S, Leibbrandt M, Cooke MP, Deane JA (2015) Using poly I:C as an adjuvant does not induce or exacerbate models of systemic lupus erythematosus. Autoimmunity 48:29–39
Tahir S, Fukushima Y, Sakamoto K, Sato K, Fujita H, Inoue J, Uede T, Hamazaki Y, Hattori M, Minato N (2015) A CD153 + CD4+ T follicular cell population with cell-senescence features plays a crucial role in lupus pathogenesis via osteopontin production. J Immunol 194:5725–5735
Fenton K (2015) The effect of cell death in the initiation of lupus nephritis. Clin Exp Immunol 179:11–16
Mackern-Oberti JP, Obreque J, Mendez GP, Llanos C, Kalergis AM (2015) Carbon monoxide inhibits T cell activation in target organs during systemic lupus erythematosus. Clin Exp Immunol 182:1–13
Li D, Guo B, Wu H, Tan L, Chang C, Lu Q (2015) Interleukin-17 in systemic lupus erythematosus: a comprehensive review. Autoimmunity 48:353–361
Chaigne B, Lasfargues G, Marie I, Huttenberger B, Lavigne C, Marchand-Adam S, Maillot F, Diot E (2015) Primary Sjogren’s syndrome and occupational risk factors: a case-control study. J Autoimmun 60:80–85
Ceccarelli F, Perricone C, Massaro L, Cipriano E, Alessandri C, Spinelli FR, Valesini G, Conti F (2015) Assessment of disease activity in systemic lupus erythematosus: lights and shadows. Autoimmun Rev 14:601–608
Beca S, Rodriguez-Pinto I, Alba MA, Cervera R, Espinosa G (2015) Development and validation of a risk calculator to differentiate flares from infections in systemic lupus erythematosus patients with fever. Autoimmun Rev 14:586–593
Mosca M, Tani C, Carli L, Vagnani S, Possemato N, Delle Sedie A, Cagnoni M, D’Aniello D, Riente L, Caramella D, Bombardieri S (2015) The role of imaging in the evaluation of joint involvement in 102 consecutive patients with systemic lupus erythematosus. Autoimmun Rev 14:10–15
Sarbu N, Alobeidi F, Toledano P, Espinosa G, Giles I, Rahman A, Yousry T, Capurro S, Jager R, Cervera R, Bargallo N (2015) Brain abnormalities in newly diagnosed neuropsychiatric lupus: systematic MRI approach and correlation with clinical and laboratory data in a large multicenter cohort. Autoimmun Rev 14:153–159
Piga M, Peltz MT, Montaldo C, Perra D, Sanna G, Cauli A, Mathieu A (2015) Twenty-year brain magnetic resonance imaging follow-up study in systemic lupus erythematosus: factors associated with accrual of damage and central nervous system involvement. Autoimmun Rev 14:510–516
Liao J, Chang C, Wu H, Lu Q (2015) Cell-based therapies for systemic lupus erythematosus. Autoimmun Rev 14:43–48
Liu C, Kanamaru Y, Watanabe T, Tada N, Horikoshi S, Suzuki Y, Liu Z, Tomino Y (2015) Targeted IgA Fc receptor I (FcalphaRI) therapy in the early intervention and treatment of pristane-induced lupus nephritis in mice. Clin Exp Immunol 181:407–416
Otomo K, Koga T, Mizui M, Yoshida N, Kriegel C, Bickerton S, Fahmy TM, Tsokos GC (2015) Cutting edge: nanogel-based delivery of an inhibitor of CaMK4 to CD4+ T cells suppresses experimental autoimmune encephalomyelitis and lupus-like disease in mice. J Immunol 195:5533–5537
Roccatello D, Sciascia S, Baldovino S, Rossi D, Alpa M, Naretto C, Di Simone D, Simoncini M, Menegatti E (2015) A 4-year observation in lupus nephritis patients treated with an intensified B-lymphocyte depletion without immunosuppressive maintenance treatment-clinical response compared to literature and immunological re-assessment. Autoimmun Rev 14:1123–1130
Dorner T, Shock A, Goldenberg DM, Lipsky PE (2015) The mechanistic impact of CD22 engagement with epratuzumab on B cell function: implications for the treatment of systemic lupus erythematosus. Autoimmun Rev 14:1079–1086
Ruiz-Arruza I, Barbosa C, Ugarte A, Ruiz-Irastorza G (2015) Comparison of high versus low-medium prednisone doses for the treatment of systemic lupus erythematosus patients with high activity at diagnosis. Autoimmun Rev 14:875–879
Bashi T, Blank M, Ben-Ami Shor D, Fridkin M, Versini M, Gendelman O, Volkov A, Barshak I, Shoenfeld Y (2015) Successful modulation of murine lupus nephritis with tuftsin-phosphorylcholine. J Autoimmun 59:1–7
Bashi T, Bizzaro G, Ben-Ami Shor D, Blank M, Shoenfeld Y (2015) The mechanisms behind helminth’s immunomodulation in autoimmunity. Autoimmun Rev 14:98–104
Ostensen M, Andreoli L, Brucato A, Cetin I, Chambers C, Clowse ME, Costedoat-Chalumeau N, Cutolo M, Dolhain R, Fenstad MH, Forger F, Wahren-Herlenius M, Ruiz-Irastorza G, Koksvik H, Nelson-Piercy C, Shoenfeld Y, Tincani A, Villiger PM, Wallenius M, von Wolff M (2015) State of the art: reproduction and pregnancy in rheumatic diseases. Autoimmun Rev 14:376–386
Viall CA, Chamley LW (2015) Histopathology in the placentae of women with antiphospholipid antibodies: a systematic review of the literature. Autoimmun Rev 14:446–471
Abreu MM, Danowski A, Wahl DG, Amigo MC, Tektonidou M, Pacheco MS, Fleming N, Domingues V, Sciascia S, Lyra JO, Petri M, Khamashta M, Levy RA (2015) The relevance of “non-criteria” clinical manifestations of antiphospholipid syndrome: 14th international congress on antiphospholipid antibodies technical task force report on antiphospholipid syndrome clinical features. Autoimmun Rev 14:401–414
Alijotas-Reig J, Ferrer-Oliveras R, Ruffatti A, Tincani A, Lefkou E, Bertero MT, Coloma-Bazan E, de Carolis S, Espinosa G, Rovere-Querini P, Kuzenko A, Valverde EE, Robles A, Cervera R, Canti V, Fredi M, Gil-Aguado A, Lundelin K, Llurba E, Melnychuk T, Nalli C, Picardo E, Silvestro E, del Ross T, Farran-Codina I (2015) The European Registry on Obstetric Antiphospholipid Syndrome (EUROAPS): a survey of 247 consecutive cases. Autoimmun Rev 14:387–395
Arnaud L, Mathian A, Devilliers H, Ruffatti A, Tektonidou M, Forastiero R, Pengo V, Lambert M, Lefevre G, Martinez-Zamora MA, Balasch J, Wahl D, Amoura Z (2015) Patient-level analysis of five international cohorts further confirms the efficacy of aspirin for the primary prevention of thrombosis in patients with antiphospholipid antibodies. Autoimmun Rev 14:192–200
Denas G, Jose SP, Bracco A, Zoppellaro G, Pengo V (2015) Antiphospholipid syndrome and the heart: a case series and literature review. Autoimmun Rev 14:214–222
Raso S, Sciascia S, Kuzenko A, Castagno I, Marozio L, Bertero MT (2015) Bridging therapy in antiphospholipid syndrome and antiphospholipid antibodies carriers: case series and review of the literature. Autoimmun Rev 14:36–42
Black LL, Srivastava R, Schoeb TR, Moore RD, Barnes S, Kabarowski JH (2015) Cholesterol-independent suppression of lymphocyte activation, autoimmunity, and glomerulonephritis by apolipoprotein a-I in normocholesterolemic lupus-prone mice. J Immunol 195:4685–4698
Clement M, Charles N, Escoubet B, Guedj K, Chauveheid MP, Caligiuri G, Nicoletti A, Papo T, Sacre K (2015) CD4 + CXCR3+ T cells and plasmacytoid dendritic cells drive accelerated atherosclerosis associated with systemic lupus erythematosus. J Autoimmun 63:59–67
Meroni PL, Penatti AE (2016) Epigenetics and systemic lupus erythematosus: unmet needs. Clin Rev Allergy Immunol 50(3):367–76.
Coit P, Yalavarthi S, Ognenovski M, Zhao W, Hasni S, Wren JD, Kaplan MJ, Sawalha AH (2015) Epigenome profiling reveals significant DNA demethylation of interferon signature genes in lupus neutrophils. J Autoimmun 58:59–66
Coit P, Renauer P, Jeffries MA, Merrill JT, McCune WJ, Maksimowicz-Mckinnon K, Sawalha AH (2015) Renal involvement in lupus is characterized by unique DNA methylation changes in naive CD4+ T cells. J Autoimmun 61:29–35
Shaabani N, Honke N, Dolff S, Gorg B, Khairnar V, Merches K, Duhan V, Metzger S, Recher M, Barthuber C, Hardt C, Proksch P, Haussinger D, Witzke O, Lang PA, Lang KS (2015) IFN-gamma licenses CD11b(+) cells to induce progression of systemic lupus erythematosus. J Autoimmun 62:11–21
Chang NH, Li TT, Kim JJ, Landolt-Marticorena C, Fortin PR, Gladman DD, Urowitz MB, Wither JE (2015) Interferon-alpha induces altered transitional B cell signaling and function in systemic lupus erythematosus. J Autoimmun 58:100–110
Wu YY, Georg I, Diaz-Barreiro A, Varela N, Lauwerys B, Kumar R, Bagavant H, Castillo-Martin M, El Salem F, Maranon C, Alarcon-Riquelme ME (2015) Concordance of increased B1 cell subset and lupus phenotypes in mice and humans is dependent on BLK expression levels. J Immunol 194:5692–5702
Bonanni A, Vaglio A, Bruschi M, Sinico RA, Cavagna L, Moroni G, Franceschini F, Allegri L, Pratesi F, Migliorini P, Candiano G, Pesce G, Ravelli A, Puppo F, Martini A, Tincani A, Ghiggeri GM (2015) Multi-antibody composition in lupus nephritis: isotype and antigen specificity make the difference. Autoimmun Rev 14:692–702
Yaniv G, Twig G, Shor DB, Furer A, Sherer Y, Mozes O, Komisar O, Slonimsky E, Klang E, Lotan E, Welt M, Marai I, Shina A, Amital H, Shoenfeld Y (2015) A volcanic explosion of autoantibodies in systemic lupus erythematosus: a diversity of 180 different antibodies found in SLE patients. Autoimmun Rev 14:75–79
Seret G, Canas F, Pougnet-Di Costanzo L, Hanrotel-Saliou C, Jousse-Joulin S, Le Meur Y, Saraux A, Valeri A, Putterman C, Youinou P, Rojas-Villarraga A, Anaya JM, Renaudineau Y (2015) Anti-alpha-actinin antibodies are part of the anti-cell membrane antibody spectrum that characterize patients with lupus nephritis. J Autoimmun 61:54–61
Rekvig OP (2015) Anti-dsDNA antibodies as a classification criterion and a diagnostic marker for systemic lupus erythematosus: critical remarks. Clin Exp Immunol 179:5–10
Cieslik P, Hrycek A (2015) Pentraxin 3 as a biomarker of local inflammatory response to vascular injury in systemic lupus erythematosus. Autoimmunity 48:242–250
Bassi N, Del Prete D, Ghirardello A, Gatto M, Ceol M, Zen M, Bettio S, Mantovani A, Iaccarino L, Punzi L, Doria A (2015) PTX3, anti-PTX3, and anti-C1q autoantibodies in lupus glomerulonephritis. Clin Rev Allergy Immunol 49:217–226
Figgett WA, Deliyanti D, Fairfax KA, Quah PS, Wilkinson-Berka JL, MacKay F (2015) Deleting the BAFF receptor TACI protects against systemic lupus erythematosus without extensive reduction of B cell numbers. J Autoimmun 61:9–16
Fox DA (2015) Citrullination: a specific target for the autoimmune response in rheumatoid arthritis. J Immunol 195:5–7
Lerner A, Matthias T (2015) Rheumatoid arthritis-celiac disease relationship: joints get that gut feeling. Autoimmun Rev 14:1038–1047
Cunha BM, Mota LM, Pileggi GS, Safe IP, Lacerda MV (2015) HIV/AIDS and rheumatoid arthritis. Autoimmun Rev 14:396–400
Schellekens GA, de Jong BA, van den Hoogen FH, van de Putte LB, van Venrooij WJ (2015) Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. 1998. J Immunol 195:8–16
Gudmann NS, Hansen NU, Jensen AC, Karsdal MA, Siebuhr AS (2015) Biological relevance of citrullinations: diagnostic, prognostic and therapeutic options. Autoimmunity 48:73–79
Baum R, Gravallese EM (2015) Bone as a target organ in rheumatic disease: impact on osteoclasts and osteoblasts. Clin Rev Allergy Immunol. [Epub ahead of print]
Nevius E, Gomes AC, Pereira JP (2015) Inflammatory cell migration in rheumatoid arthritis: a comprehensive review. Clin Rev Allergy Immunol. [Epub ahead of print]
Messemaker TC, Huizinga TW, Kurreeman F (2015) Immunogenetics of rheumatoid arthritis: understanding functional implications. J Autoimmun 64:74–81
Churov AV, Oleinik EK, Knip M (2015) MicroRNAs in rheumatoid arthritis: altered expression and diagnostic potential. Autoimmun Rev 14:1029–1037
Wu GC, Pan HF, Leng RX, Wang DG, Li XP, Li XM, Ye DQ (2015) Emerging role of long noncoding RNAs in autoimmune diseases. Autoimmun Rev 14:798–805
Han TU, Lee HS, Kang C, Bae SC (2015) Association of joint erosion with SLC22A4 gene polymorphisms inconsistently associated with rheumatoid arthritis susceptibility. Autoimmunity 48:313–317
Zampeli E, Vlachoyiannopoulos PG, Tzioufas AG (2015) Treatment of rheumatoid arthritis: unraveling the conundrum. J Autoimmun 65:1–18
Katz-Agranov N, Khattri S, Zandman-Goddard G (2015) The role of intravenous immunoglobulins in the treatment of rheumatoid arthritis. Autoimmun Rev 14:651–658
Xie Q, Huang C, Li J (2015) Interleukin-22 and rheumatoid arthritis: emerging role in pathogenesis and therapy. Autoimmunity 48:69–72
Meka RR, Venkatesha SH, Dudics S, Acharya B, Moudgil KD (2015) IL-27-induced modulation of autoimmunity and its therapeutic potential. Autoimmun Rev 14:1131–1141
Xu WD, Zhao Y, Liu Y (2015) Insights into IL-37, the role in autoimmune diseases. Autoimmun Rev 14:1170–1175
Chang Y, Wei W (2015) Angiotensin II in inflammation, immunity and rheumatoid arthritis. Clin Exp Immunol 179:137–145
Hollan I, Dessein PH, Ronda N, Wasko MC, Svenungsson E, Agewall S, Cohen-Tervaert JW, Maki-Petaja K, Grundtvig M, Karpouzas GA, Meroni PL (2015) Prevention of cardiovascular disease in rheumatoid arthritis. Autoimmun Rev 14:952–969
Schinnerling K, Soto L, Garcia-Gonzalez P, Catalan D, Aguillon JC (2015) Skewing dendritic cell differentiation towards a tolerogenic state for recovery of tolerance in rheumatoid arthritis. Autoimmun Rev 14:517–527
Bhargava P, Calabresi PA (2015) Novel therapies for memory cells in autoimmune diseases. Clin Exp Immunol 180:353–360
Azevedo VF, Meirelles Ede S, Kochen Jde A, Medeiros AC, Miszputen SJ, Teixeira FV, Damiao AO, Kotze PG, Romiti R, Arnone M, Magalhaes RF, Maia CP, de Carvalho AV (2015) Recommendations on the use of biosimilars by the Brazilian Society of Rheumatology, Brazilian Society of Dermatology, Brazilian Federation of Gastroenterology and Brazilian Study Group on Inflammatory Bowel Disease—focus on clinical evaluation of monoclonal antibodies and fusion proteins used in the treatment of autoimmune diseases. Autoimmun Rev 14:769–773
Cantini F, Nannini C, Niccoli L, Iannone F, Delogu G, Garlaschi G, Sanduzzi A, Matucci A, Prignano F, Conversano M, Goletti D, Safebio A (2015) Guidance for the management of patients with latent tuberculosis infection requiring biologic therapy in rheumatology and dermatology clinical practice. Autoimmun Rev 14:503–509
Lubrano E, Cantini F, Costanzo A, Girolomoni G, Prignano F, Olivieri I, Scarpa R, Spadaro A, Atzeni F, Narcisi A, Ricceri F, Sarzi-Puttini P (2015) Measuring psoriatic disease in clinical practice. An expert opinion position paper. Autoimmun Rev 14:864–874
Harden JL, Krueger JG, Bowcock AM (2015) The immunogenetics of psoriasis: a comprehensive review. J Autoimmun 64:66–73
Recke A, Vidarsson G, Ludwig RJ, Freitag M, Moller S, Vonthein R, Schellenberger J, Haase O, Gorg S, Nebel A, Flachsbart F, Schreiber S, Lieb W, Glaser R, Benoit S, Sardy M, Eming R, Hertl M, Zillikens D, Konig IR, Schmidt E, Ibrahim S, German AGSG (2015) Allelic and copy-number variations of FcgammaRs affect granulocyte function and susceptibility for autoimmune blistering diseases. J Autoimmun 61:36–44
Liang Y, Chang C, Lu Q (2015) The genetics and epigenetics of atopic dermatitis-filaggrin and other polymorphisms. Clin Rev Allergy Immunol. [Epub ahead of print]
Jafarinejad-Farsangi S, Farazmand A, Mahmoudi M, Gharibdoost F, Karimizadeh E, Noorbakhsh F, Faridani H, Jamshidi AR (2015) MicroRNA-29a induces apoptosis via increasing the Bax:Bcl-2 ratio in dermal fibroblasts of patients with systemic sclerosis. Autoimmunity 48:369–378
Sonntag K, Eckert F, Welker C, Muller H, Muller F, Zips D, Sipos B, Klein R, Blank G, Feuchtinger T, Schumm M, Handgretinger R, Schilbach K (2015) Chronic graft-versus-host-disease in CD34(+)-humanized NSG mice is associated with human susceptibility HLA haplotypes for autoimmune disease. J Autoimmun 62:55–66
Diani M, Altomare G, Reali E (2015) T cell responses in psoriasis and psoriatic arthritis. Autoimmun Rev 14:286–292
Lima XT, Oliveira RT, Braga FG, Magalhaes RF, Mamoni RL, Blotta MH (2015) Circulating levels of chemokines in psoriasis. Autoimmunity 48:57–60
Dagur PK, McCoy JP Jr (2015) Endothelial-binding, proinflammatory T cells identified by MCAM (CD146) expression: characterization and role in human autoimmune diseases. Autoimmun Rev 14:415–422
Isailovic N, Daigo K, Mantovani A, Selmi C (2015) Interleukin-17 and innate immunity in infections and chronic inflammation. J Autoimmun 60:1–11
Jones SA, Perera DN, Fan H, Russ BE, Harris J, Morand EF (2015) GILZ regulates Th17 responses and restrains IL-17-mediated skin inflammation. J Autoimmun 61:73–80
Ebihara S, Date F, Dong Y, Ono M (2015) Interleukin-17 is a critical target for the treatment of ankylosing enthesitis and psoriasis-like dermatitis in mice. Autoimmunity 48:259–266
Meller S, Di Domizio J, Voo KS, Friedrich HC, Chamilos G, Ganguly D, Conrad C, Gregorio J, Le Roy D, Roger T, Ladbury JE, Homey B, Watowich S, Modlin RL, Kontoyiannis DP, Liu YJ, Arold ST, Gilliet M (2015) T(H)17 cells promote microbial killing and innate immune sensing of DNA via interleukin 26. Nat Immunol 16:970–979
Pinegin B, Vorobjeva N, Pinegin V (2015) Neutrophil extracellular traps and their role in the development of chronic inflammation and autoimmunity. Autoimmun Rev 14:633–640
Karczewski J, Swora-Cwynar E, Rzymski P, Poniedzialek B, Adamski Z (2015) Selected biologic markers of inflammation and activity of Crohn’s disease. Autoimmunity 48:318–327
Bonneau J, Dumestre-Perard C, Rinaudo-Gaujous M, Genin C, Sparrow M, Roblin X, Paul S (2015) Systematic review: new serological markers (anti-glycan, anti-GP2, anti-GM-CSF Ab) in the prediction of IBD patient outcomes. Autoimmun Rev 14:231–245
de Lange KM, Barrett JC (2015) Understanding inflammatory bowel disease via immunogenetics. J Autoimmun 64:91–100
Maroni L, van de Graaf SF, Hohenester SD, Oude Elferink RP, Beuers U (2015) Fucosyltransferase 2: a genetic risk factor for primary sclerosing cholangitis and Crohn’s disease—a comprehensive review. Clin Rev Allergy Immunol 48:182–191
Zhang ZT, Ma XJ, Zong Y, Du XM, Hu JH, Lu GC (2015) Is the CARD8 rs2043211 polymorphism associated with susceptibility to Crohn’s disease? a meta-analysis. Autoimmunity 48:524–531
Generali E, Cantarini L, Selmi C (2015) Ocular involvement in systemic autoimmune diseases. Clin Rev Allergy Immunol 49:263–270
Ben-Ami Shor D, Bashi T, Lachnish J, Fridkin M, Bizzaro G, Barshak I, Blank M, Shoenfeld Y (2015) Phosphorylcholine-tuftsin compound prevents development of dextransulfate-sodium-salt induced murine colitis: implications for the treatment of human inflammatory bowel disease. J Autoimmun 56:111–117
Chong M, Fonacier L (2015) Treatment of eczema: corticosteroids and beyond. Clin Rev Allergy Immunol. [Epub ahead of print]
Hollenbach JA, Oksenberg JR (2015) The immunogenetics of multiple sclerosis: a comprehensive review. J Autoimmun 64:13–25
Zhang Z, Zhang R (2015) Epigenetics in autoimmune diseases: pathogenesis and prospects for therapy. Autoimmun Rev 14:854–863
D’Ambrosio A, Pontecorvo S, Colasanti T, Zamboni S, Francia A, Margutti P (2015) Peripheral blood biomarkers in multiple sclerosis. Autoimmun Rev 14:1097–1110
Fitzner B, Hecker M, Zettl UK (2015) Molecular biomarkers in cerebrospinal fluid of multiple sclerosis patients. Autoimmun Rev 14:903–913
Weinstock JV (2015) Do we need worms to promote immune health? Clin Rev Allergy Immunol 49:227–231
Su M, Song Y, He Z, Hu R, Rood D, Lai L (2015) Administration of embryonic stem cell-derived thymic epithelial progenitors expressing MOG induces antigen-specific tolerance and ameliorates experimental autoimmune encephalomyelitis. J Autoimmun 58:36–47
Cusick MF, Libbey JE, Oh L, Jordan S, Fujinami RS (2015) Acthar gel treatment suppresses acute exacerbations in a murine model of relapsing-remitting multiple sclerosis. Autoimmunity 48:222–230
Ding X, Yan Y, Li X, Li K, Ciric B, Yang J, Zhang Y, Wu S, Xu H, Chen W, Lovett-Racke AE, Zhang GX, Rostami A (2015) Silencing IFN-gamma binding/signaling in astrocytes versus microglia leads to opposite effects on central nervous system autoimmunity. J Immunol 194:4251–4264
Esposito S, Di Pietro GM, Madini B, Mastrolia MV, Rigante D (2015) A spectrum of inflammation and demyelination in acute disseminated encephalomyelitis (ADEM) of children. Autoimmun Rev 14:923–929
Hoffmann FS, Kuhn PH, Laurent SA, Hauck SM, Berer K, Wendlinger SA, Krumbholz M, Khademi M, Olsson T, Dreyling M, Pfister HW, Alexander T, Hiepe F, Kumpfel T, Crawford HC, Wekerle H, Hohlfeld R, Lichtenthaler SF, Meinl E (2015) The immunoregulator soluble TACI is released by ADAM10 and reflects B cell activation in autoimmunity. J Immunol 194:542–552
Huang XL, Zhang L, Li JP, Wang YJ, Duan Y, Wang J (2015) MicroRNA-150: a potential regulator in pathogens infection and autoimmune diseases. Autoimmunity 48:503–510
Yang Y, Winger RC, Lee PW, Nuro-Gyina PK, Minc A, Larson M, Liu Y, Pei W, Rieser E, Racke MK, Lovett-Racke AE (2015) Impact of suppressing retinoic acid-related orphan receptor gamma t (ROR)gammat in ameliorating central nervous system autoimmunity. Clin Exp Immunol 179:108–118
Parker Harp CR, Archambault AS, Sim J, Ferris ST, Mikesell RJ, Koni PA, Shimoda M, Linington C, Russell JH, Wu GF (2015) B cell antigen presentation is sufficient to drive neuroinflammation in an animal model of multiple sclerosis. J Immunol 194:5077–5084
Schubert RD, Hu Y, Kumar G, Szeto S, Abraham P, Winderl J, Guthridge JM, Pardo G, Dunn J, Steinman L, Axtell RC (2015) IFN-beta treatment requires B cells for efficacy in neuroautoimmunity. J Immunol 194:2110–2116
Knier B, Rothhammer V, Heink S, Puk O, Graw J, Hemmer B, Korn T (2015) Neutralizing IL-17 protects the optic nerve from autoimmune pathology and prevents retinal nerve fiber layer atrophy during experimental autoimmune encephalomyelitis. J Autoimmun 56:34–44
Herold M, Posevitz V, Chudyka D, Hucke S, Gross C, Kurth F, Leder C, Loser K, Kurts C, Knolle P, Klotz L, Wiendl H (2015) B7-H1 selectively controls TH17 differentiation and central nervous system autoimmunity via a novel Non-PD-1-mediated pathway. J Immunol 195:3584–3595
Zhang X, Tao Y, Chopra M, Dujmovic-Basuroski I, Jin J, Tang Y, Drulovic J, Markovic-Plese S (2015) IL-11 induces Th17 cell responses in patients with early relapsing-remitting multiple sclerosis. J Immunol 194:5139–5149
Arbelaez CA, Glatigny S, Duhen R, Eberl G, Oukka M, Bettelli E (2015) IL-7/IL-7 receptor signaling differentially affects effector CD4+ T cell subsets involved in experimental autoimmune encephalomyelitis. J Immunol 195:1974–1983
Miller PG, Bonn MB, Franklin CL, Ericsson AC, Mckarns SC (2015) TNFR2 deficiency acts in concert with Gut microbiota to precipitate spontaneous sex-biased central nervous system demyelinating autoimmune disease. J Immunol 195:4668–4684
Alvarez I, Collado JA, Colobran R, Carrascal M, Ciudad MT, Canals F, James EA, Kwok WW, Gartner M, Kyewski B, Pujol-Borrell R, Jaraquemada D (2015) Central T cell tolerance: identification of tissue-restricted autoantigens in the thymus HLA-DR peptidome. J Autoimmun 60:12–19
Bhela S, Kempsell C, Manohar M, Dominguez-Villar M, Griffin R, Bhatt P, Kivisakk-Webb P, Fuhlbrigge R, Kupper T, Weiner H, Baecher-Allan C (2015) Nonapoptotic and extracellular activity of granzyme B mediates resistance to regulatory T cell (treg) suppression by HLA-DR-CD25hiCD127lo tregs in multiple sclerosis and in response to IL-6. J Immunol 194:2180–2189
Carbajal KS, Mironova Y, Ulrich-Lewis JT, Kulkarni D, Grifka-Walk HM, Huber AK, Shrager P, Giger RJ, Segal BM (2015) Th cell diversity in experimental autoimmune encephalomyelitis and multiple sclerosis. J Immunol 195:2552–2559
Chalmin F, Rochemont V, Lippens C, Clottu A, Sailer AW, Merkler D, Hugues S, Pot C (2015) Oxysterols regulate encephalitogenic CD4(+) T cell trafficking during central nervous system autoimmunity. J Autoimmun 56:45–55
De Rosa V, Galgani M, Porcellini A, Colamatteo A, Santopaolo M, Zuchegna C, Romano A, De Simone S, Procaccini C, La Rocca C, Carrieri PB, Maniscalco GT, Salvetti M, Buscarinu MC, Franzese A, Mozzillo E, La Cava A, Matarese G (2015) Glycolysis controls the induction of human regulatory T cells by modulating the expression of FOXP3 exon 2 splicing variants. Nat Immunol 16:1174–1184
Huss DJ, Mehta DS, Sharma A, You X, Riester KA, Sheridan JP, Amaravadi LS, Elkins JS, Fontenot JD (2015) In vivo maintenance of human regulatory T cells during CD25 blockade. J Immunol 194:84–92
Langston PK, Yang M, Bierbach U, Parsonage D, Poole LB, Price MJ, Grayson JM (2015) Au-ACRAMTU-PEt3 alters redox balance to inhibit T cell proliferation and function. J Immunol 195:1984–1994
Bossini-Castillo L, Lopez-Isac E, Martin J (2015) Immunogenetics of systemic sclerosis: defining heritability, functional variants and shared-autoimmunity pathways. J Autoimmun 64:53–65
Hersh AO, Prahalad S (2015) Immunogenetics of juvenile idiopathic arthritis: a comprehensive review. J Autoimmun 64:113–124
Lee HJ, Li CW, Hammerstad SS, Stefan M, Tomer Y (2015) Immunogenetics of autoimmune thyroid diseases: a comprehensive review. J Autoimmun 64:82–90
Noble JA (2015) Immunogenetics of type 1 diabetes: a comprehensive review. J Autoimmun 64:101–112
Webb GJ, Siminovitch KA, Hirschfield GM (2015) The immunogenetics of primary biliary cirrhosis: a comprehensive review. J Autoimmun 64:42–52
Ma HD, Wang YH, Chang C, Gershwin ME, Lian ZX (2015) The intestinal microbiota and microenvironment in liver. Autoimmun Rev 14:183–191
Consolandi C, Turroni S, Emmi G, Severgnini M, Fiori J, Peano C, Biagi E, Grassi A, Rampelli S, Silvestri E, Centanni M, Cianchi F, Gotti R, Emmi L, Brigidi P, Bizzaro N, De Bellis G, Prisco D, Candela M, D’Elios MM (2015) Behcet’s syndrome patients exhibit specific microbiome signature. Autoimmun Rev 14:269–276
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Selmi, C. Autoimmunity in 2015. Clinic Rev Allerg Immunol 51, 110–119 (2016). https://doi.org/10.1007/s12016-016-8576-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-016-8576-1