Abstract
Sarcoidosis is a systemic inflammatory disorder characterised by tissue infiltration by mononuclear phagocytes and lymphocytes with associated non-caseating granuloma formation. Originally described as a disorder of the skin, sarcoidosis can involve any organ with wide-ranging clinical manifestations and disease course. Recent studies have provided new insights into the mechanisms involved in disease pathobiology, and we now know that sarcoidosis has a clear genetic basis largely involving human leukocyte antigen (HLA) genes. In contrast to Mendelian-monogenic disorders—which are generally due to specific and relatively rare mutations often leading to a single amino acid change in an encoded protein—sarcoidosis results from genetic variations relatively common in the general population and involving multiple genes, each contributing an effect of varying magnitude. However, an individual may have the necessary genetic profile and yet the disease will not develop unless an environmental or infectious factor is encountered. Genetics appears also to contribute to the huge variability in clinical phenotype and disease behaviour. Moreover, it has been established that sarcoidosis granulomatous inflammation is a highly polarized T helper 1 immune response that starts with an antigenic stimulus followed by T cell activation via a classic HLA class II-mediated pathway. A complex network of lymphocytes, macrophages, and cytokines is pivotal in the orchestration and evolution of the granulomatous process. Despite these advances, the aetiology of sarcoidosis remains elusive and its pathogenesis incompletely understood. As such, there is an urgent need for a better understanding of disease pathogenesis, which hopefully will translate into the development of truly effective therapies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The existence of a genetic predisposition to sarcoidosis is supported by several lines of evidence: (1) monozygotic twins are more often concordant for the disease than dizygotic twins [1, 2]; (2) familial clustering of the disease occurs in approximately 5–16 % of patients [3]; and (3) there are striking differences in disease prevalence and clinical manifestations across different geographic areas and racial groups [4]. Linkage, candidate gene, and genome-wide association studies have identified a number of susceptibility loci with the human leukocyte antigen (HLA) class II alleles representing the main contributor to disease susceptibility across patients of different ethnicity [5]. Sarcoidosis is not a single-gene disease; instead, a multitude of genes are believed to be involved, each contributing an effect of varying magnitude. Genetics is also likely to contribute to the wide variety of clinical manifestations and prognosis observed in this disease (Fig. 1). In this regard, some believe that sarcoidosis is a “family” of different disorders, including among the others Löfgren’s syndrome, chronic/progressive lung disease, and granulomatous uveitis, each with potentially distinct genetic associations [6]. Chronic beryllium disease could also be considered as a subset of the broad grouping “sarcoidosis” and almost certainly was historically [7].
Proposed model for the development of sarcoidosis. A variety of genetic variants may confer susceptibility to sarcoidosis, but the disease develops only in the context of a relevant exposure. Susceptibility genes contribute an effect of varying magnitude, depending on the function of their gene product and gene-gene interactions. The relevance of environmental exposures is likely to be influenced by their duration, intensity, timing or context. A similar model might also apply to disease phenotype
Antigen-Driven T Cell Response—the Trimolecular Complex
In order to elicit a granulomatous response, the sarcoid antigen/s must be processed by antigen presenting cells (APCs) (e.g. macrophages and dendritic cells), and a peptide fragment presented in the context of major histocompatibility complex (MHC) class II molecules, usually HLA-DR or HLA-DQ [8–10]. HLA molecules bind antigenic peptides within a groove composed of two α-helices and a floor of antiparallel β-strands to form a complex that is recognized by α/β+ T cell receptor (TCR)-expressing T cells [11]. The antigen-binding properties of the MHC class II peptide-binding groove are determined by polymorphic amino acid residues that form pockets interacting with the antigenic peptide side chains. Contrary to class I molecules (HLA-A, HLA-B, and HLA-C), which present endogenous peptides of 8–10 amino acid length to CD8+ T cells, HLA class II molecules (HLA-DP, HLA-DQ, and HLA-DR) bind longer exogenous peptides (their peptide-binding groove is open-ended) for recognition by CD4+ T cells [12–14]. These peptides, which are largely derived from polypeptides that have been phagocytized or internalized by endocytosis by APCs, are loaded onto HLA class II molecules for display on the cell surface [15–17]. The MHC molecule/peptide/TCR (the “trimolecular complex”) [9] interaction provides the first activation signal for the antigen-specific T cells. When co-stimulatory molecules, such as CD80 and CD86, provide a second signal, T cells are ready to orchestrate the immune response that culminates with granuloma formation [9, 18]. Indeed, lung T cells in sarcoidosis show numerous signs of (recent) activation, including reduced surface density of the CD3/TCR complex [19], IL-2 gene expression [20], spontaneous release of cytokines (e.g. interferon-γ [IFN-γ] and IL-2) [21, 22], as well as cell surface expression of HLA-DR and very late activation antigen-1 (VLA-1) [23].
The TCRs contain highly specific antigen recognition sites. The huge TCR variety for specific antigens derives from rearrangement of germ line variable (V), diversity (D), junctional (J) and constant (C) region elements of the TCR genes (αβ and γδ). Thus, antigen-specific responses result in the expansion of a limited number of T cells bearing specific TCRs (clonal or oligoclonal expansions). The expansion of T cells exhibiting a restricted repertoire of TCR αβ or γδ genes in the lung, blood and skin of sarcoidosis patients strongly suggests that a limited number of peptides are responsible for the selection and expansion of these particular T cells [24–29]. The most striking example of selective TCR usage in sarcoidosis was described by Grunewald and colleagues, who demonstrated a preferential accumulation of CD4+ T cells expressing the TCR AV2S3 gene segment in the lung of Scandinavian patients carrying the HLA-DRB1*0301 (DR-17) allele [25, 27, 30]. A preferential AV2S3 gene usage by CD4+ T cells has also been observed in sarcoidosis patients carrying the HLA-DRB3*0101 (i.e. DR52a) allele [25, 30]. The HLA-DRB1*0301 and HLA-DRB3*0101 alleles share identical amino acid sequences in the regions responsible for antigen binding and probably allow presentation of similar antigenic peptides and expansion of the same T cell population. The lung-accumulated AV2S3+ T cells show a higher degree of activation and differentiation than other bronchoalveolar lavage (BAL)-derived CD4+ T cells [31–33]. Of note, selective stimulation of AV2S3+ T cells has been correlated with sarcoidosis of acute onset and short duration, suggesting for these cells a protective role against the putative sarcoid antigen/s [34]. Investigations on the messenger RNA (mRNA) as well as protein level demonstrated that the AV2S3+ T cells have a very low expression of the T regulatory cell transcription factor forkhead box P3 (FoxP3), indicating that they are effector rather than regulatory cells [32, 33, 35]. This is confirmed by the demonstration that they produce T helper (Th) 1 cytokines [32]. Thus, they may act to eliminate a specific antigen, leading to disease resolution. After clinical recovery, the number of CD4+AV2S3+ cells in the BAL of sarcoidosis patients tends to normalise [36]. While the majority of studies have demonstrated overexpression of α/β TCR genes [37], an increased number of γ/δ+ TCR T lymphocytes has also been observed in the blood and BAL from patients with sarcoidosis [38]. The γ/δ TCR is potentially relevant to sarcoidosis as γ/δ+ T cells from normal individuals respond to mycobacterial heat shock proteins, and mycobacterial products are thought to play a role in at least a subset of sarcoidosis cases [39]. In addition, Vδ1+ T cells are clonally expanded in pulmonary sarcoidosis consistent with the concept that the disease results from persistent, specific antigenic (exogenous and/or self) stimulation that induce a cell-mediated immune response [29].
The Early Years
Because of the highly polymorphic nature of the HLA genes and the requirement for HLA molecules in the presentation of antigens to T cells, the search for HLA associations with sarcoidosis has been the focus of several studies. Hedfors and Möller initially reported an increased frequency of HL-A7 (now HLA-B7) in sarcoidosis patients (n = 50) compared to controls (n = 100) [40]. This was in contrast to Kueppers and colleagues, who analysed 132 patients and 600 controls but found no significant associations between HL-A antigens and sarcoidosis [41]. However, a couple of years later, HLA-B7 was found to associate with sarcoidosis, this time in a South Carolina Black population (28 patients vs 80 controls) [42]. HLA-B7 is now known to belong to a haplotype common in Caucasians, i.e. HLA-A*0301: B*0702: Cw*0701: DRB1*1501: DQA1*0102: DQB1*0602, which has at least in part been found to associate with a more chronic form of sarcoidosis [43]. In 1981, Smith and colleagues identified a link between carriage of HLA-B8 and spontaneous resolution and suggested that inherited factors relating to the immune system may influence the clinical phenotype of sarcoidosis [44]. This concept was further substantiated in a study by Hedfors and Lindström, who HLA-typed 19 sarcoidosis patients with an acute onset, bilateral hilar lymphadenopathy, ankle joint arthritis, and (in seven of them) also erythema nodosum (this combination of signs and symptoms is commonly referred to as Löfgren’s syndrome; Fig. 2). The authors found a strong association with HLA-B8/DR3 and concluded that such a strong association might be explained by an “immunogenetically determined handling of a postulated etiological antigen” [45]. Gardner and colleagues identified an association between B8/Cw7/DR3 and good prognosis in Caucasian but not black West Indian patients [46]. Krause and co-workers studied 42 sarcoidosis patients with arthritis and 134 ethnically matched controls and found a strong association with HLA-DR3 [47]. The authors proposed that genetic factors must be considered together with a postulated triggering antigen in sarcoidosis [47].
Modern Times
Although the HLA allele distribution significantly differs across ethnic populations, subsequent studies, using more specific tools for HLA analysis and more rigorous disease definitions, have shown that certain HLA class II alleles associate with disease protection/risk across different populations. Specifically, HLA-DRB1*01 and DRB1*04 protect against disease in several Caucasian populations, while DRB1*03, DRB1*11, DRB1*12, DRB1*14 and DRB1*15 are risk factors for sarcoidosis [5, 7].
A number of studies have also confirmed the HLA-B8/DR3 association with Löfgren’s syndrome (LS) [48]. In addition to displaying distinct clinical manifestations, patients with LS can be further characterized according to the carriage of DRB1*03. Among LS patients in Sweden (where two thirds of them carry the DRB1*03 allele), disease resolution (defined as disease duration <2 years) was reported to occur in 95 % of DRB1*03+ patients, but only in 49 % of DRB1*03− [49]. Interestingly, a clustering of disease onset in January, April and May has been observed in DRB1*03+ but not DRB1*03− patients, suggesting a key role for season-specific antigens in the development of LS. The mechanisms through which DRB1*03 influence disease behaviour in LS is unknown. However, DRB1*03+ patients display a less pronounced Th1-type immune response with reduced levels of IFN-γ and tumor necrosis factor (TNF)-α [50], yet they may be able to mount a more effective and specific immune response against the postulated antigen/s [32]. Such an efficacious immune response includes lung accumulation of Th cells with expression of a specific TCR (AV2S3) [27] and production of several Th1 cytokines when stimulated with a specific mycobacterial antigen (mKatG) [32].
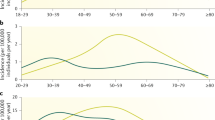
HLA-B8/DR3 is known to be part of the so-called 8.1 ancestral haplotype (HLA A*0101: B*0801: Cw*0701: DRB1*0301: DQA1*0501: DQB1*0201) which is quite common in Caucasians. Besides HLA, this haplotype includes or is linked to a large number of non-HLA genes of critical importance for the immune system. Sarcoidosis associations with class I genes were originally considered to be caused by linkage disequilibrium (LD) (e.g. the tendency for genetic variants located close to each other on the same chromosome to be associated within a population more often than if they were unlinked) with class II genes [7]. However, multiple logistic regression analysis revealed that both HLA-B7 and HLA-B8 increase the risk of sarcoidosis independently of class II genes [43]. Moreover, patients with the common allele combination HLA-A*3, B*07, DRB1*15 have been shown to be at significantly higher risk of developing chronic disease. Another common haplotype (HLA-A*01, B*08, DRB1*03), which is present in approximately 20 % of Swedish sarcoidosis patients, is associated almost invariably with resolving disease in Sweden [43] as well as with LS in Croatian sarcoidosis patients [51]. HLA class I alleles may thus have more influence on disease susceptibility and behaviour than previously thought (43, 51; Fig. 3). As seen above, HLA-DQB1 alleles are also linked to various HLA-DRB1 alleles, and in African Americans, HLA-DQB1 alleles were suggested to be more important for sarcoidosis associations than DRB1 alleles [52]. In particular, carriage of HLA-DQB1*0201 was found to be protective against the disease, while DQB1*0602 was linked to radiographic progression [10].
Gene map of the human leukocyte antigen (HLA) region. The HLA region spans approximately 4 × 106 nucleotides on chromosome 6p21.31–6p21.33, with class II, class III and class I genes located from the centromeric (Cen) to the telomeric (Tel) end. HLA class I molecules mediate immune responses against endogenous, whereas class II molecules are involved in the presentation of exogenous antigens to T helper cells. The HLA class III region contains a number of genes involved in immune response regulation, including tumour necrosis factor (TNF)-α and complement proteins (C2, C4)
Pockets
The peptide-binding groove of the HLA class II molecule consists of two α-helices, making up the walls of the groove, and a β-pleated sheet that constitutes the floor of the groove. Depending on the amino acids within the groove, different peptides will be bound. As such, certain amino acids at distinct positions may have a greater influence in antigen binding than others. In chronic beryllium disease, for example, there is a strong association between glutamic acid (Glu) at position 69, found primarily on HLA-DPB1*0201, and reactivity against beryllium and subsequently disease [53, 54]. The nature of the peptide(s) that in addition to beryllium binds to the HLA-DP molecule has recently started to be investigated [55, 56]. In the peptide-binding groove of the HLA molecule, a number of pockets are formed (P1, P4, P5, P7 and P9). Side chains of the amino acids may dig into the HLA molecule to improve anchoring of the peptide. In sarcoidosis, pockets number 4, 6 and 7 appear to be important for interacting with potential sarcoidosis-associated peptides. Foley and colleagues described that the protective DRB1*01 and DRB1*04 molecules have in common small hydrophobic residues at position 11 of antigen binding pocket 6, while non-protecting DRB1 molecules had instead hydrophilic residues at the same position [8]. Position 11 contains the only variable amino acid in pocket 6 and may influence substantially the binding capacity of the pocket. In a similar approach, Voorter and co-workers studied 149 Caucasian patients to search for distinct amino acids within the antigen-binding parts of DRB1 and DQB1 molecules and their associations with sarcoidosis risk. The patients were divided into those with a good prognosis (i.e. chest radiographic stage I) and those at risk for a more chronic disease (i.e. chest radiographic stage II–IV) [57]. The authors found the DRB1 residues Pro11, Arg13, Ser37 and Ala71 associated with both disease overall and chronic disease. Interestingly, all four residues are found on DRB1*1501. In addition, Ala71, which is part of the peptide binding pocket 4, allows preferential binding of non-charged aromatic residues and thereby specifically influences the HLA-bound peptide repertoire. Moreover, a HLA-DR Arg74 residue was found significantly more often in patients with radiographic stage I and good prognosis. DR Arg74 is also part of pocket 4 and is found almost exclusively on DRB1*0301, which is associated with good prognosis [58]. Arg74 determines the preferential binding of aspartic acid in pocket 4 of the DR molecule. Interestingly, DRB1 pocket 4 was also shown to be a common denominator for two different HLA molecules, both with a unique association with lung accumulated T cells expressing the AV2S3 TCR, further indicating specific antigenic peptide recognition by these cells in the lungs of sarcoidosis patients [30]. Pocket 7 has also been suggested to be important for association with sarcoidosis and for binding of specific peptides. In the US ACCESS study, HLA-DRB1 amino acid residue at position 47 (F47), which is located in pocket 7, appeared to independently contribute to the risk of sarcoidosis in white American patients [59]. Of note, HLA-DRB1-F47 was present on the three alleles most strongly associated with sarcoidosis, namely DRB1*1101, DRB1*1201 and DRB1*1501 [59].
Studies of Today
Wennerström and colleagues recently studied 188 patients and 224 controls in Finland and confirmed DRB1*1501 to be a risk factor for and DRB1*0101 to be protective against sarcoidosis [60]. While in contrast to previous studies DRB1*15 was not found to associate with persistent disease in Finnish patients, the authors confirmed a strong association between DRB1*0301 and good prognosis, particularly in patients without extra-pulmonary manifestations. Detailed analysis of HLA class II pockets revealed specific amino acid residues in pockets 4, 7 and 9 to associate with disease course; in particular, the amino acid at residue 71 of pocket 4 associated with disease prognosis.
Sato and colleagues studied 340 UK, 139 Dutch and 163 Japanese patients, and 354, 218 and 168 matched controls, respectively. In common for all three populations was the protective effect of HLA-DRB1*01 with a similar tendency for DRB1*04 in the Caucasian populations [61]. In addition, DRB1*12 associated with disease in UK and Dutch patients with a similar trend observed in Japanese patients, whereas DRB1*14 associated with disease only in Caucasian patients. Uveitis associated with DRB1*0803 in the Japanese population and with DRB1*04 in the UK population, while it was too rare amongst Dutch patients to provide meaningful results. In the Japanese cohort, DRB1*0803 was also significantly associated with neurosarcoidosis. The Dutch cohort was the only one that included a substantial proportion of patients with LS, again strongly associating with DRB1*03, as shown before in several reports [58]. The authors however found no particular amino acid position to associate with overall disease, pulmonary disease, LS or uveitis. More recently, Suzuki and colleagues studied 237 Japanese patients and 287 matched controls for any DRB1 or DQB1 allele associations; DRB1*0803 and DRB1*0901 were identified as risk alleles, irrespective of disease onset or phenotype [62]. Zhou and co-workers have recently reported in a study of 131 Chinese Han patients and 122 controls an association between HLA-DRB1*11 and disease risk, while DRB1*07 and HLA-B*13 were protective [63]. Of note, DRB1*11 confers susceptibility to sarcoidosis also in Indian [64] and Japanese patients [65]. Moreover, in the ACCESS study the HLA-DRB1*1101 allele associated with disease in both black and white American patients [59]. Finally, it is noteworthy that HLA-DRB1*11 has been found to associate with antigen presentation of distinct mycobacterial derived antigens ESAT-6 and mKatG [66], which have been proposed as sarcoidosis antigens [67].
HLA-Type in Relation to Phenotypes
Some HLA-DRB1 alleles influence clinical phenotype and disease behaviour. The best example is probably Löfgren’s syndrome, which in several reports has been shown to associate with a benign disease course [45, 49, 51]. In Sweden, the influence of DRB1*03 on disease course is so strong that it is now used as a biomarker of good prognosis [68]. On the other hand, HLA-DRB1*15 has been suggested to predispose to a chronic form of the disease [69–71]. Sarcoidosis uveitis has been shown to associate with DRB1*0401 in the ACCESS study, in both black and white Americans [59]. Similarly, DRB1*0401 is a risk factor for uveitis in Japanese and UK subjects [61], as well as in Scandinavian patients in whom DRB1*0401 homozygosity confers a substantially increased risk for uveitis [72]. Although very few, patients with Heerfordt’s syndrome—characterized by fever, parotid or salivary gland enlargement, cranial nerve palsy and uveitis—were also shown to associate with DRB1*0401 [72]. On the other hand, lung-predominant sarcoidosis was found to associate with DRB1*12 and DRB1*14 [57]. Cardiac sarcoidosis is associated with HLA-DQB1*0601 in Japanese patients [73]. Finally, HLA-DQB1*0602, which is in strong LD with DRB1*1501, has been shown to associate with splenomegaly in Japanese patients [74], and with small fibre neuropathy in Caucasians [75]. HLA associations with sarcoidosis are summarized in Table 1.
Conflicting results with regard to HLA associations have many plausible explanations, besides the well-known interethnic differences between study populations. Patient sampling and other methodological aspects may also affect the results and complicate data evaluations. Further, it is likely that a diagnosis of “sarcoidosis” covers several distinct disease entities, each with their own separate genetic association and exposure history.
Other Genetic Associations with Sarcoidosis
A number of non-HLA genes have also been associated with risk of disease or phenotype (5, 7; Table 2). One example is the finding of a sarcoidosis risk variant within the butyrophilin-like 2 (BTNL2) gene [62, 80, 85–92]. BTNL2 is structurally similar to the co-stimulatory molecule CD80 (B7-1) but in contrast to CD80 it is believed to act as an inhibitory molecule for T cells. Accordingly, defective BTNL2 function might result in an exaggerated T cell activation. Another example is annexin A11 (ANXA11) [80–84]. The functional relevance of the risk variant detected in sarcoidosis patients is not known, but it has been proposed that it may affect the survival of inflammatory cells. Other reported genetic associations include, amongst others, the cytokines TNF and transforming growth factor (TGF)-β, and the IL-23 receptor, as well as different Toll-like receptor (TLR) genes (Table 2). Several of these gene variants are not unique to sarcoidosis, but associate also with other inflammatory disorders [6].
Immunopathogenesis of Sarcoidosis Granulomatous Inflammation
Granuloma formation is regarded as a means of defending the host from persistent irritants of either exogenous or endogenous origin. In fact, the causative agent is walled off and sequestered by cells of macrophage lineage allowing it to be contained, if not destroyed altogether [124]. However, these cells may also prime the adaptive immune system by displaying foreign antigens on the surface of MHC class I or II molecules. Depending on both pathogen and host factors, the adaptive immune response is usually dominated by either a type 1 T helper (Th1), Th2 or Th17 cell response [125, 126]. Sarcoidosis is mediated by a predominantly Th1 immune response in which a complex network of lymphocytes, macrophages, cytokines and chemokines mount an immune response that culminates with granuloma formation ([127]; Table 3). In experimental models, granulomatous inflammation is downregulated with clearance of antigen [128]. Conversely, if the antigen persists, continuing activation of T cells leads to further accumulation of macrophages, which can give rise to epithelioid cells (large cells with a pale nucleus and abundant cytoplasm) or fuse to form giant multinucleated cells [129]. Macrophages are integral in both formation of granuloma and in promoting a Th1 immune response. The initial triggering of macrophages occurs via activation of so-called pattern-recognition receptors, recognizing evolutionary conserved molecular patterns of different classes of pathogens. The best characterized family of such receptors are TLRs. Enhanced or altered responses to TLR2 stimulation have been observed in cells from the lung and blood of sarcoidosis patients [130–132]. TLR2 has also been demonstrated to have a role in granuloma formation, both in animal models [130, 132] and in a human in vitro model of mycobacterial granulomas [133]. A critical role for aggregates of the acute-phase reactant serum amyloid A (SAA) to regulate granuloma formation in sarcoidosis has been proposed by Moller and colleagues; they found SAA to be expressed to a much higher degree in sarcoid granulomas than in granulomas in other diseases [130]. The same study also demonstrated that SAA stimulated BAL cells from sarcoidosis patients to a higher degree of cytokine release than cells from control subjects, partly by interaction with TLR2, and also promoted experimental Th1-mediated granulomatous inflammation. Macrophages exert their effects mainly by producing a number of chemokines and cytokines, such as CCL2 (monocyte chemotactic protein 1 (MCP1)), CCL3 (macrophage inflammatory protein-1α (MIP-1α)), CCL4 (macrophage inflammatory protein-1β (MIP-1β)), CCL5 (regulated on activation, normal T cell expressed and secreted (RANTES)), IL-8, IL-12, IL-15 and IP-10 [134]. In addition, macrophages produce IL-1, IL-15 and TNF-α, which induces endothelial cell-T cell interaction by up-regulating the expression of adhesion molecules on the endothelium [135]. TNF-α is a critical mediator of granuloma formation and maintenance through induction of CD4+ T cell proliferation and survival. In active pulmonary sarcoidosis, alveolar macrophages spontaneously release TNF [136], and higher levels of this cytokine have been observed in patients with severe/progressive disease compared with those with inactive disease [137]. The mechanisms responsible for the evolution of sarcoid granulomas to fibrosis are poorly understood but abnormal apoptotic-signalling pathways, loss of regulatory response as well as the development of a more Th2-like environment are likely to be involved (136; Table 4).
Sarcoidosis Antigens
A mycobacterial aetiology of sarcoidosis has long been proposed, based on clinical and histological similarities with tuberculosis. Evidence for the presence of mycobacteria in sarcoidosis lesions have been obtained by PCR, and a meta-analysis of 31 such studies found that the odds of detecting mycobacterial nucleic acids were at least ten times higher in sarcoidosis tissues compared to control tissues [138]. Using a mass spectrometry approach to analyse sarcoidosis tissues, a specific mycobacterial protein, catalase-peroxidase (mKatG), was found to be present in a majority of sarcoidosis samples and to be the target of B cell responses in half of the patients [67]. Other studies have also found evidence of specific mycobacterial proteins in sarcoidosis tissue [139, 140]. Sarcoidosis patients have been found to harbour blood and lung T cell responses to mycobacterial proteins, including mKatG, ESAT-6, antigen-85A and heat shock proteins [141–144]. A preferential stimulation by mKatG of the TCR AV2S3+ T cells which accumulate in the lungs of HLA-DRB1*03+ patients has been reported (32; Fig. 4). Propionibacterial aetiology has also been proposed, although it remains more controversial. In support of this aetiopathogenetic hypothesis is the presence of propionibacterial DNA in sarcoidosis tissues [145] and cellular immune responses to Propionibacterium acnes in a subset of sarcoidosis patients [146]. It is plausible that there is not one single aetiologic agent in sarcoidosis, but that different environmental agents, including non-organic substances, may lead to sarcoidosis granulomatous inflammation [147]. In an effort to directly identify the antigenic peptides presented by HLA molecules on antigen-presenting cells in the lungs of sarcoidosis patients, Wahlström and colleagues analyzed by liquid chromatography-mass spectrometry BAL cells from 16 HLA-DRB1*0301+ sarcoidosis patients and identified a number of peptides bound to the HLA-DR molecules, including peptides derived from well-known autoantigens such as vimentin and ATP synthase [148]. In a follow-up study, a prominent T cell response to vimentin was found in peripheral blood of a subset of patients having the same HLA type [149]. Thus, at least in some patients, autoimmunity may contribute to the inflammation in sarcoidosis. One possible explanation for such responses, which may be chronic or transient, is “molecular mimicry” with pathogen-derived molecules breaking tolerance to self-antigens.
Proposed model of how qualitative differences in T cell responses to the mycobacterial protein mKatG may promote distinct clinical outcomes in patient subgroups. In HLA-DRB1*0301+ patients, mKatG-specific T cells have the ability to produce a multifunctional Th1 cytokine profile (IFN-γ and TNF). Reduced expression of T regulatory cell transcriptor factor FoxP3 in AV2S3+ T cells suggests an effector rather than a regulatory function for this T cell subset, leading to eradication of the inciting antigen and disease resolution. Conversely, in HLA-DRB1*0301− patients, mKatG-specific T cells produce a single-functional Th1 cytokine profile (IFN-γ), which together with increased FoxP3+ regulatory T cells leads to antigen persistence and chronic disease. This figure is based on the results reported in references 25, 27, 31–34, 141 and 144 (courtesy Maria Wikén)
Th1 Polarization
An established immunologic feature of sarcoidosis is that the CD4+ lymphocytes that trigger granuloma formation are strongly Th1 polarized. Indeed, the expression of both IFN-γ—a cytokine produced by Th1 cells—and a number of Th1-promoting cytokines, such as IL-12, IL-15, IL-18 and IL-27—is up-regulated at sites of sarcoidosis granulomatous inflammation [150–153]. In addition, a study of cytokine expression in lymph nodes has demonstrated a spatial rearrangement of cytokine-producing cells, with IL-1β, TNF-α and IFN-β being localized to the granuloma itself, and other cytokines, such as IL-1α, IL-2 and IL-6 being distributed more randomly [154].
IL-12, one of the most potent Th1-promoting cytokines, induces Th1 differentiation from naive T cells and Th1 proliferation. BAL cells from sarcoidosis patients display enhanced (spontaneous) expression of IL-12 protein and mRNA [155], with higher levels observed in individuals with active disease compared with both those with inactive disease and healthy controls [156–158]. IL-15 is a cytokine with functions similar to IL-12, and its secretion from BAL and peripheral cells is significantly higher in patients with active sarcoidosis compared with those with inactive disease and healthy controls [159]. IL-18 is essential for optimal induction of IFN-γ expression in T cells and natural killer (NK) cells [160]. IL-18 and IL-18R expression is increased in the lung of sarcoidosis patients and is associated with higher expression of IFN-γ and IL-2 as well as local T cell activation [152, 160]. IL-27, a cytokine involved in T cell activation and induction of IFN-γ, is also overexpressed in sarcoidosis [153]. In turn, IFN-γ enhances macrophage accessory functions, and thereby synergizes with other pro-inflammatory cytokines, such as TNF-α, to facilitate cellular trafficking and recruitment to disease sites [161]. In addition, IFN-γ up-regulates the expression of co-stimulatory molecules, which optimize T cell activation, and increases TNF-α release from appropriately triggered macrophages [162]. The role of IFN-γ in granulomatous inflammation is supported by the observation that granulomas do not develop in IFN-γ knockout mice exposed to termophilic bacteria [163]. The notion of Th1 polarization as a key feature of sarcoidosis is substantiated further by the occurrence of new onset or recrudescent disease following treatments with biologic agents that promote a Th1 response (e.g. IFN-α and IFN-γ) [164, 165] as well as by the observed down-regulation of several cytokines, chemokines and chemokine receptors associated with Th2 responses at disease sites in patients with sarcoidosis [155, 166]. IFN-γ is a likely contributor to the Th1-type cytokine profile in sarcoidosis by suppressing the Th2 lymphocyte response [167].
Th17 Cells
Th17 cells, i.e. T cells producing IL-17 as their signature cytokine, were found to constitute a separate lineage 10 years ago and have been implicated in several inflammatory and autoimmune diseases. They have also been shown to be essential for pulmonary granuloma formation in response to mycobacterial infection in mice [168, 169]. This prompted investigations in sarcoidosis patients, were a couple of studies found Th17 cells in increased frequencies in blood and in BAL fluid, and also to be present in the granuloma [170–172]. Th17 cells specific for the mycobacterial protein ESAT-6 were found to be present in blood and BAL of sarcoidosis patients [172], while another study found that IL-17 responses to the mycobacterial protein mKatG were higher in BAL cells from sarcoidosis patients with Löfgren’s syndrome compared to non-Löfgren’s patients [173]. The same study also demonstrated the highest levels of IL-17 in BAL fluid of HLA-DRB1*03+ Löfgren’s patients, i.e. patients with a very good prognosis. The frequencies of Th17 cells producing IFN-γ, an example of “hybrid” T cells combining characteristics of two lineages, have also been compared between sarcoidosis patients and healthy controls, however with conflicting results [172, 174].
Regulatory T Cells
Regulatory T cells (Tregs) maintain immune homeostasis by inhibiting APCs and effector T cell function [175]. Both natural constitutive (nTregs) and adaptive (antigen-specific) induced (iTregs) forms of Tregs have been described, which overall represent about 5–10 % of circulating CD4+ T cells in healthy subjects [176]. However, there is no marker allowing nTregs or iTregs to be analysed separately. Most Tregs express FoxP3, which is regarded as a “master regulator” of Treg differentiation, as well as high levels of CD25. In sarcoidosis, tissue-, blood- and BAL-derived FoxP3+ T cells appear to exhibit an impaired ability to suppress TNF-α, IFN-γ and IL-2 production and are not effective in inhibiting granuloma formation in vitro [177, 178]. At the same time, peripheral Treg cells exert powerful antiproliferative activity that may account for the “immune paradox of sarcoidosis” [177] (e.g. extensive granulomatous inflammation and cytokine secretion associated with a state of anergy as indicated by the lack of reaction to skin antigen tests and ex vivo exposure to common recall antigens in peripheral blood) [179, 180]. However, another study found sarcoidosis Tregs to have a reduced ability to suppress proliferation [181]. Moreover, Idali and colleagues have reported a reduced expression of FoxP3 in CD4+FoxP3+ BAL T cells of sarcoidosis patients consistent with a reduced function of Tregs [35]. Decreased BAL Treg numbers have been associated with both a favourable prognosis and a chronic (active) disease course [33, 182], suggesting that further studies are needed to elucidate the role of dysfunctional Tregs in the pathogenesis of sarcoidosis.
CD1d-restricted natural killer T (NKT) cells represent another important regulatory T cell subset. Ho and colleagues have shown that NKT cells are absent or significantly reduced in the peripheral blood of patients with classical sarcoidosis (but not in those presenting acutely with features of Löfgren’s syndrome) [183]. Notably, there was no difference in the proportion of CD1d-restricted NKT cells between peripheral blood and lungs, suggesting that the peripheral blood deficiency is not due to sequestration of these cells in the lungs. Furthermore, CD1d expression on APC of patients was normal; thus, the deficiency of CD1d-restricted NKT cells is not due to abnormal CD1d expression. The results of a follow-up study by the same group suggest that the deficiency in NKT cells may lead to reduced IL-10 production by monocytes, resulting in an exaggerated T cell proliferation [184].
Progression to Fibrosis
Chronic granulomatous inflammation can lead to fibrosis of the lung, heart and liver in patients with sarcoidosis. Fibrosis requires the recruitment and proliferation of fibroblasts, leading to extracellular deposition of collagen matrix products [185]. Excessive chemokine production has been associated with progressive pulmonary fibrosis [186]. Indeed, a number of mediators that are found at sites of sarcoid granulomatous inflammation (e.g. fibronectin) are chemoattractant for fibroblasts, whereas macrophage-produced transforming growth factor-β (TGF-β), insulin growth factor-1 (IGF-1) and platelet-derived growth factor (PDGF) induce fibroblast proliferation and collagen matrix deposition [187, 188]. The Th1-defining cytokine IFN-γ, which is highly expressed at disease sites, has direct antifibrotic effects [189], whereas Th2 cytokines, such as IL-4 and IL-13, promote fibrogenesis [190]. Accordingly, it has been suggested that a local shift from Th1 to Th2 cytokine predominance may favour progression to chronic, fibrotic disease [191, 192]. However, the relevant pathways involved in the fibrotic outcome in sarcoidosis remain uncertain [193, 194].
Concluding Remarks
While the search for the sarcoidosis antigen/s continues, it seems inevitable that the development of the disease is determined by a complex interplay between host/genetic factors and the antigen/s. In addition, genetic abnormalities that confer disease risk are likely to be largely separate from those that influence specific disease manifestations. Therefore, if sarcoidosis genetics is to move forward, it is imperative that meticulous databases of phenotypically well-defined patients continue to be constructed. Some of the genes that could potentially affect an individual’s susceptibility to disease and the course of any established disease have been identified. Much work remains to be done, but a fuller understanding of the genetic basis of sarcoidosis is likely to open up new therapeutic avenues, both for the treatment of this and other granulomatous disorders.
References
Familial associations in sarcoidosis (1973) A report to the Research Committee of the British Thoracic and Tuberculosis Association. Tubercle 54:87–98
Sverrild A, Backer V, Kyvik KO et al (2008) Heredity in sarcoidosis: a registry-based twin study. Thorax 63:894–896
Rybicki BA, Kirkey KL, Major M et al (2001) Familial risk ratio of sarcoidosis in African-American sibs and parents. Am J Epidemiol 153:188–193
Hosoda Y, Yamaguchi M, Hiraga Y (1997) Global epidemiology of sarcoidosis. What story do prevalence and incidence tell us? Clin Chest Med 18:681–694
Fischer A, Grunewald J, Spagnolo P, Nebel A, Schreiber S, Müller-Quernheim J (2014) Genetics of sarcoidosis. Semin Respir Crit Care Med 35:296–306
Spagnolo P, Richeldi L, du Bois RM (2008) Environmental triggers and susceptibility factors in idiopathic granulomatous diseases. Semin Respir Crit Care Med 29:610–619
Spagnolo P, Grunewald J (2013) Recent advances in the genetics of sarcoidosis. J Med Genet 50:290–297
Foley PJ, McGrath DS, Puscinska E et al (2001) Human leukocyte antigen-DRB1 position 11 residues are a common protective marker for sarcoidosis. Am J Respir Cell Mol Biol 25:272–277
Moller DR, Chen ES (2002) Genetic basis of remitting sarcoidosis: triumph of the trimolecular complex? Am J Respir Cell Mol Biol 27:391–395
Iannuzzi MC, Maliarik MJ, Poisson LM, Rybicki BA (2003) Sarcoidosis susceptibility and resistance HLA-DQB1 alleles in African Americans. Am J Respir Crit Care Med 167:1225–1231
Wang JH, Reinherz EL (2002) Structural basis of T cell recognition of peptides bound to MHC molecules. Mol Immunol 38:1039–1049
Appella E, Padlan EA, Hunt DF (1995) Analysis of the structure of naturally processed peptides bound by Class I and Class II major histocompatibility complex molecules. EXS 73:105–119
Norment AM, Salter RD, Parham P, Engelhard VH, Littman DR (1988) Cell-cell adhesion mediated by CD8 and MHC class I molecules. Nature 336:79–81
Doyle C, Strominger JL (1987) Interaction between CD4 and class II MHC molecules mediates cell adhesion. Nature 330:256–259
Brachet V, Pehau-Arnaudet G, Desaymard C, Raposo G, Amigorena S (1999) Early endosomes are required for major histocompatibility complex Class II transport to peptide-loading compartments. Mol Biol Cell 10:2891–2904
Lich JD, Elliott JF, Blum JS (2000) Cytoplasmic processing is a prerequisite for presentation of an endogenous antigen by major histocompatibility complex Class II proteins. J Exp Med 191:1513–1524
Ramachandra L, Harding CV (2000) Phagosomes acquire nascent and recycling Class II MHC molecules but primarily use nascent molecules in phagocytic antigen processing. J Immunol 164:5103–5112
Schwartz JC, Zhang X, Nathenson SG, Almo SC (2002) Structural mechanisms of costimulation. Nat Immunol 3:427–434
du Bois RM, Kirby M, Balbi B, Saltini C, Crystal RG (1992) T-lymphocytes that accumulate in the lung in sarcoidosis have evidence of recent stimulation of the T-cell antigen receptor. Am Rev Respir Dis 145:1205–1211
Muller-Quernheim J, Saltini C, Sondermeyer P, Crystal RG (1986) Compartmentalized activation of the interleukin 2 gene by lung T lymphocytes in active pulmonary sarcoidosis. J Immunol 137:3475–3483
Pinkston P, Bitterman PB, Crystal RG (1983) Spontaneous release of interleukin-2 by lung T lymphocytes in active pulmonary sarcoidosis. N Engl J Med 308:793–800
Robinson BW, McLemore TL, Crystal RG (1985) Gamma interferon is spontaneously released by alveolar macrophages and lung T lymphocytes in patients with pulmonary sarcoidosis. J Clin Invest 75:1488–1495
Hunninghake GW, Crystal RG (1981) Pulmonary sarcoidosis: a disorder mediated by excess helper T-lymphocyte activity at sites of disease activity. N Engl J Med 305:429–434
Forman JD, Klein JT, Silver RF, Liu MC, Greenlee BM, Moller DR (1994) Selective activation and accumulation of oligoclonal V beta-specific T cells in active pulmonary sarcoidosis. J Clin Invest 94:1533–1542
Grunewald J, Janson CH, Eklund A et al (1992) Restricted V alpha 2.3 gene usage by CD4+ T lymphocytes in bronchoalveolar lavage fluid from sarcoidosis patients correlates with HLA-DR3. Eur J Immunol 22:129–135
Moller DR, Konishi K, Kirby M, Balbi B, Crystal RG (1988) Bias toward use of a specific T cell receptor beta-chain variable region in a subgroup of individuals with sarcoidosis. J Clin Invest 82:1183–1191
Grunewald J, Olerup O, Persson U, Ohrn MB, Wigzell H, Eklund A (1994) T-cell receptor variable region gene usage by CD4+ and CD8+ T cells in bronchoalveolar lavage fluid and peripheral blood of sarcoidosis patients. Proc Natl Acad Sci U S A 91:4965–4969
Jones CM, Lake RA, Wijeyekoon JB, Mitchell DM, du Bois RM, O’Hehir RE (1996) Oligoclonal V gene usage by T lymphocytes in bronchoalveolar lavage fluid from sarcoidosis patients. Am J Respir Cell Mol Biol 14:470–477
Forrester JM, Newman LS, Wang Y, King TE Jr, Kotzin BL (1993) Clonal expansion of lung V delta 1+ T cells in pulmonary sarcoidosis. J Clin Invest 91:292–300
Grunewald J, Wahlstrom J, Berlin M, Wigzell H, Eklund A, Olerup O (2002) Lung restricted T cell receptor AV2S3+ CD4+ T cell expansions in sarcoidosis patients with a shared HLA-DR beta chain conformation. Thorax 57:348–352
Katchar K, Wahlström J, Eklund A, Grunewald J (2001) Highly activated T-cell receptor AV2S3(+) CD4(+) lung T-cell expansions in pulmonary sarcoidosis. Am J Respir Crit Care Med 163:1540–1545
Wikén M, Ostadkarampour M, Eklund A et al (2012) Antigen-specific multifunctional T-cells in sarcoidosis patients with Lofgren’s syndrome. Eur Respir J 40:110–121
Wikén M, Grunewald J, Eklund A, Wahlström J (2012) Multiparameter phenotyping of T-cell subsets in distinct subgroups of patients with pulmonary sarcoidosis. J Intern Med 271:90–103
Grunewald J, Berlin M, Olerup O et al (2000) Lung T-helper cells expressing T-cell receptor AV2S3 associate with clinical features of pulmonary sarcoidosis. Am J Respir Crit Care Med 161:814–818
Idali F, Wahlström J, Müller-Suur C, Eklund A, Grunewald J (2008) Analysis of regulatory T cell associated forkhead box P3 expression in the lungs of patients with sarcoidosis. Clin Exp Immunol 152:127–137
Planck A, Eklund A, Grunewald J (2003) Markers of activity in clinically recovered human leukocyte antigen-DR17-positive sarcoidosis patients. Eur Respir J 21:52–57
Spagnolo P, du Bois RM (2007) Genetics of sarcoidosis. Clin Dermatol 25:242–249
Balbi B, Moller DR, Kirby M, Holroyd KJ, Crystal RG (1990) Increased numbers of T-lymphocytes with gamma delta1 antigen receptors in a subgroup of individuals with pulmonary sarcoidosis. J Clin Invest 85:1353–1361
Brownell I, Ramírez-Valle F, Sanchez M, Prystowsky S (2011) Evidence for mycobacteria in sarcoidosis. Am J Respir Cell Mol Biol 45:899–905
Hedfors E, Möller E (1973) HL-A antigens in sarcoidosis. Tissue Antigens 3:95–98
Kueppers F, Brackertz D, Mueller-Eckhardt C (1972) HL-A antigens in sarcoidosis and rheumatoid arthritis. Lancet 2:1425
McIntyre JA, McKee KT, Loadholt CB, Mercurio S, Lin I (1977) Increased HLA-B7 antigen frequency in South Carolina blacks in association with sarcoidosis. Transplant Proc 9:173–176
Grunewald J, Eklund A, Olerup O (2004) Human leukocyte antigen class I alleles and the disease course in sarcoidosis patients. Am J Respir Crit Care Med 169:696–702
Smith MJ, Turton CW, Mitchell DN, Turner-Warwick M, Morris LM, Lawler SD (1981) Association of HLA B8 with spontaneous resolution in sarcoidosis. Thorax 36:296–298
Hedfors E, Lindström F (1983) HLA-B8/DR3 in sarcoidosis. Correlation to acute onset disease with arthritis. Tissue Antigens 22:200–203
Gardner J, Kennedy HG, Hamblin A, Jones E (1984) HLA associations in sarcoidosis: a study of two ethnic groups. Thorax 39:19–22
Krause A, Goebel KM (1987) Class II MHC antigen (HLA-DR3) predisposes to sarcoid arthritis. J Clin Lab Immunol 24:25–27
Lofgren S, Lundback H (1952) The bilateral hilar lymphoma syndrome; a study of the relation to tuberculosis and sarcoidosis in 212 cases. Acta Med Scand 142:265–273
Grunewald J, Eklund A (2009) Löfgren’s syndrome. Human Leukocyte Antigen strongly influences the disease course. Am J Respir Crit Care Med 179:307–312
Idali F, Wikén M, Wahlström J et al (2006) Reduced Th1 response in the lungs of HLA-DRB1*0301 patients with pulmonary sarcoidosis. Eur Respir J 27:451–459
Grubić Z, Zunec R, Peros-Golubicić T et al (2007) HLA class I and class II frequencies in patients with sarcoidosis from Croatia: role of HLA-B8, -DRB1*0301, and -DQB1*0201 haplotype in clinical variations of the disease. Tissue Antigens 70:301–306
Rybicki BA, Maliarik MJ, Poisson LM et al (2003) The major histocompatibility complex gene region and sarcoidosis susceptibility in African Americans. Am J Respir Crit Care Med 167:444–449
Richeldi L, Sorrentino R, Saltini C (1993) HLA-DPB1 glutamate 69: a genetic marker of beryllium disease. Science 262:242–244
Silveira LJ, McCanlies EC, Fingerlin TE et al (2012) Chronic beryllium disease, HLA-DPB1, and the DP peptide binding groove. J Immunol 189:4014–4023
Falta MT, Pinilla C, Mack DG et al (2013) Identification of beryllium-dependent peptides recognized by CD4+ T cells in chronic beryllium disease. J Exp Med 210:1403–1418
Petukh M, Wu B, Stefl S et al (2014) Chronic Beryllium Disease: revealing the role of beryllium ion and small peptides binding to HLA-DP2. PLoS One 9:e111604
Voorter CE, Amicosante M, Berretta F, Groeneveld L, Drent M, van den Berg-Loonen EM (2007) HLA class II amino acid epitopes as susceptibility markers of sarcoidosis. Tissue Antigens 70:18–27
Grunewald J, Brynedal B, Darlington P et al (2010) Different HLA-DRB1 allele distributions in distinct clinical subgroups of sarcoidosis patients. Respir Res 11:25
Rossman MD, Thompson B, Frederick M et al (2003) HLA-DRB1*1101: a significant risk factor for sarcoidosis in blacks and whites. Am J Hum Genet 73:720–735
Wennerström A, Pietinalho A, Vauhkonen H et al (2012) HLA-DRB1 allele frequencies and C4 copy number variation in Finnish sarcoidosis patients and associations with disease prognosis. Hum Immunol 73:93–100
Sato H, Woodhead FA, Ahmad T et al (2010) Sarcoidosis HLA class II genotyping distinguishes differences of clinical phenotype across ethnic groups. Hum Mol Genet 19:4100–4111
Suzuki H, Ota M, Meguro A et al (2012) Genetic characterization and susceptibility for sarcoidosis in Japanese patients: risk factors of BTNL2 gene polymorphisms and HLA class II alleles. Invest Ophthalmol Vis Sci 53:7109–7115
Zhou Y, Shen L, Zhang Y, Jiang D, Li H (2011) Human leukocyte antigen-A, -B, and -DRB1 alleles and sarcoidosis in Chinese Han subjects. Hum Immunol 72:571–575
Sharma SK, Balamurugan A, Pandey RM, Saha PK, Mehra NK (2003) Human leukocyte antigen-DR alleles influence the clinical course of pulmonary sarcoidosis in Asian Indians. Am J Respir Cell Mol Biol 29:225–231
Ishihara M, Ohno S, Ishida T et al (1994) Molecular genetic studies of HLA class II alleles in sarcoidosis. Tissue Antigens 43:238–241
Oswald-Richter KA, Culver DA, Hawkins C et al (2009) Cellular responses to mycobacterial antigens are present in bronchoalveolar lavage fluid used in the diagnosis of sarcoidosis. Infect Immun 77:3740–3748
Song Z, Marzilli L, Greenlee M et al (2005) Mycobacterial catalase-peroxidase is a tissue antigen and target of the adaptive immune response in systemic sarcoidosis. J Exp Med 201:755–767
Grunewald J (2012) HLA associations and Löfgren’s syndrome. Expert Rev Clin Immunol 8:55–62
Berlin M, Fogdell-Hahn A, Olerup O, Eklund A, Grunewald J (1997) HLA-DR predicts the prognosis in Scandinavian patients with pulmonary sarcoidosis. Am J Respir Crit Care Med 156:1601–1605
Sato H, Grutters JC, Pantelidis P et al (2002) HLA-DQB1*0201: a marker for good prognosis in British and Dutch patients with sarcoidosis. Am J Respir Cell Mol Biol 27:406–412
Voorter CE, Drent M, van den Berg-Loonen EM (2005) Severe pulmonary sarcoidosis is strongly associated with the haplotype HLA-DQB1*0602-DRB1*150101. Hum Immunol 66:826–835
Darlington P, Haugom-Olsen H, von Sivers K et al (2012) T-cell phenotypes in bronchoalveolar lavage fluid, blood and lymph nodes in pulmonary sarcoidosis—indication for an airborne antigen as the triggering factor in sarcoidosis. J Intern Med 272:465–471
Naruse TK, Matsuzawa Y, Ota M et al (2000) HLA-DQB1*0601 is primarily associated with the susceptibility to cardiac sarcoidosis. Tissue Antigens 56:52–57
Sato H, Nagai S, du Bois RM et al (2007) HLA-DQB1 0602 allele is associated with splenomegaly in Japanese sarcoidosis. J Intern Med 262:449–457
Voorter CE, Drent M, Hoitsma E, Faber KG, van den Berg-Loonen EM (2005) Association of HLA DQB1 0602 in sarcoidosis patients with small fiber neuropathy. Sarcoidosis Vasc Diffuse Lung Dis 22:129–32
Martinetti M, Tinelli C, Kolek V et al (1995) “The sarcoidosis map”: a joint survey of clinical and immunogenetic findings in two European countries. Am J Respir Crit Care Med 152:557–564
Bogunia-Kubik K, Tomeczko J, Suchnicki K, Lange A (2001) HLA-DRB1*03, DRB1*11 or DRB1*12 and their respective DRB3 specificities in clinical variants of sarcoidosis. Tissue Antigens 57:87–90
Grunewald J, Eklund A (2001) Human leukocyte antigen genes may outweigh racial background when generating a specific immune response in sarcoidosis. Eur Respir J 17:1046–1048
Darlington P, Tallstedt L, Padyukov L et al (2011) HLA-DRB1* alleles and symptoms associated with Heerfordt’s syndrome in Sarcoidosis. Eur Respir J 38:1151–1157
Adrianto I, Lin CP, Hale JJ et al (2012) Genome-wide association study of African and European Americans implicates multiple shared and ethnic specific loci in sarcoidosis susceptibility. PLoS ONE 7:e43907
Hofmann S, Franke A, Fischer A et al (2008) Genome-wide association study identifies ANXA11 as a new susceptibility locus for sarcoidosis. Nat Genet 40:1103–1106
Li Y, Pabst S, Kubisch C, Grohé C, Wollnik B (2010) First independent replication study confirms the strong genetic association of ANXA11 with sarcoidosis. Thorax 65:939–940
Mrazek F, Stahelova A, Kriegova E et al (2011) Functional variant ANXA11 R230C: true marker of protection and candidate disease modifier in sarcoidosis. Genes Immun 12:490–494
Levin AM, Iannuzzi MC, Montgomery CG et al (2013) Association of ANXA11 genetic variation with sarcoidosis in African Americans and European Americans. Genes Immun 14:13–18
Valentonyte R, Hampe J, Huse K et al (2005) Sarcoidosis is associated with a truncating splice site mutation in BTNL2. Nat Genet 37:357–364
Rybicki BA, Walewski JL, Maliarik MJ et al (2005) The BTNL2 gene and sarcoidosis susceptibility in African Americans and Whites. Am J Hum Genet 77:491–499
Li Y, Wollnik B, Pabst S et al (2006) BTNL2 gene variant and sarcoidosis. Thorax 61:273–274
Spagnolo P, Sato H, Grutters JC et al (2007) Analysis of BTNL2 genetic polymorphisms in British and Dutch patients with sarcoidosis. Tissue Antigens 70:219–227
Morais A, Lima B, Peixoto MJ, Alves H, Marques A, Delgado L (2012) BTNL2 gene polymorphism associations with susceptibility and phenotype expression in sarcoidosis. Respir Med 106:1771–1777
Milman N, Svendsen CB, Nielsen FC, van Overeem Hansen T (2011) The BTNL2 A allele variant is frequent in Danish patients with sarcoidosis. Clin Respir J 5:105–111
Wijnen PA, Voorter CE, Nelemans PJ, Verschakelen JA, Bekers O, Drent M (2011) Butyrophilin-like 2 in pulmonary sarcoidosis: a factor for susceptibility and progression? Hum Immunol 72:342–347
Wennerström A, Pietinalho A, Lasota J et al (2013) Major histocompatibility complex class II and BTNL2 associations in sarcoidosis. Eur Respir J 42:550–553
Fischer A, Schmid B, Ellinghaus D et al (2012) A novel sarcoidosis risk locus for Europeans on chromosome 11q13.1. Am J Respir Crit Care Med 186:877–885
Takada T, Suzuki E, Ishida T et al (2001) Polymorphism in RANTES chemokine promoter affects extent of sarcoidosis in a Japanese population. Tissue Antigens 58:293–298
Fischer A, Valentonyte R, Nebel A et al (2008) Female-specific association of C-C chemokine receptor 5 gene polymorphisms with Löfgren’s syndrome. J Mol Med (Berl) 86:553–561
Fridlender ZG, Schwartz A, Kohan M, Amir G, Glazer M, Berkman N (2010) Association between CD14 gene polymorphisms and disease phenotype in sarcoidosis. Respir Med 104:1336–1343
Franke A, Fischer A, Nothnagel M et al (2008) Genome-wide association analysis in sarcoidosis and Crohn’s disease unravels a common susceptibility locus on 10p12.2. Gastroenterology 135:1207–1215
Heron M, van Moorsel CHM, Grutters JC et al (2011) Genetic variation in GREM1 is a risk factor for fibrosis in pulmonary sarcoidosis. Tissue Antigens 77:112–117
Heron M, Grutters JC, van Moorsel CH et al (2009) Variation in IL7R predisposes to sarcoid inflammation. Genes Immun 10:647–653
Fischer A, Nothnagel M, Franke A et al (2011) Association of inflammatory bowel disease risk loci with sarcoidosis, and its acute and chronic subphenotypes. Eur Respir J 37:610–616
Kim HS, Choi D, Lim LL et al (2011) Association of interleukin 23 receptor gene with sarcoidosis. Dis Markers 31:17–24
Heron M, Grutters JC, Van Moorsel CHM et al (2009) Effect of variation in ITGAE on risk of sarcoidosis, CD103 expression, and chest radiography. Clin Immunol 133:117–125
Piotrowski WJ, Górski P, Pietras T, Fendler W, Szemraj J (2011) The selected genetic polymorphisms of metalloproteinases MMP2, 7, 9 and MMP inhibitor TIMP2 in sarcoidosis. Med Sci Monit 17:CR598–CR607
Hattori T, Konno S, Takahashi A et al (2010) Genetic variants in mannose receptor gene (MRC1) confer susceptibility to increased risk of sarcoidosis. BMC Med Genet 11:151
Daniil Z, Mollaki V, Malli F et al (2013) Polymorphisms and haplotypes in MyD88 are associated with the development of sarcoidosis: a candidate-gene association study. Mol Biol Rep 40:4281–4286
Hofmann S, Fischer A, Till A, GenPhenReSa Consortium et al (2011) A genome-wide association study reveals evidence of association with sarcoidosis at 6p12.1. Eur Respir J 38:1127–1135
Hill MR, Papafili A, Booth H et al (2006) Functional prostaglandin-endoperoxide synthase 2 polymorphism predicts poor outcome in sarcoidosis. Am J Respir Crit Care Med 174:915–922
Lopez-Campos JL, Rodriguez-Rodriguez D, Rodriguez-Becerra E et al (2009) Cyclooxygenase-2 polymorphisms confer susceptibility to sarcoidosis but are not related to prognosis. Respir Med 103:427–433
Hofmann S, Fischer A, Nothnagel M et al (2013) A genome-wide association analysis reveals chromosome 12q13.3-q14.1 as a new risk locus for sarcoidosis. Eur Respir J 41:888–900
Jonth AC, Silveira L, Fingerlin TE et al (2007) ACCESS Group. TGF-beta 1variants in chronic beryllium disease and sarcoidosis. J Immunol 179:4255–4262
Pabst S, Fränken T, Schönau J et al (2011) Transforming growth factor beta gene polymorphisms in different phenotypes of sarcoidosis. Eur Respir J 38:169–175
Kruit A, Grutters JC, Ruven HJ et al (2006) Transforming growth factor-β gene polymorphisms in sarcoidosis patients with and without fibrosis. Chest 129:1584–1591
Veltkamp M, van Moorsel CH, Rijkers GT, Ruven HJ, Grutters JC (2012) Genetic variation in the Toll-like receptor gene cluster (TLR10-TLR1-TLR6) influences disease course in sarcoidosis. Tissue Antigens 79:25–32
Pabst S, Bradler O, Gillissen A, Nickenig G, Skowasch D, Grohe C (2013) Toll-like receptor-9 polymorphisms in sarcoidosis and chronic obstructive pulmonary disease. Adv Exp Med Biol 756:239–245
Seitzer U, Swider C, Stüber F et al (1997) Tumour necrosis factor alpha promoter gene polymorphism in sarcoidosis. Cytokine 9:787–790
McDougal KE, Fallin MD, Moller DR, ACCESS Research Group et al (2009) Variation in the lymphotoxin-alpha/tumor necrosis factor locus modifies risk of erythema nodosum in sarcoidosis. J Invest Dermatol 129:1921–1926
Labunski S, Posern G, Ludwig S, Kundt G, Bröcker EB, Kunz M (2001) Tumour necrosis factor-alpha promoter polymorphism in erythema nodosum. Acta Derm Venereol 81:18–21
Medica I, Kastrin A, Maver A, Peterlin B (2007) Role of genetic polymorphisms in ACE and TNF-alpha gene in sarcoidosis: a metaanalysis. J Hum Genet 52:836–847
Grutters JC, Sato H, Pantelidis P et al (2002) Increased frequency of the uncommon tumor necrosis factor -857 T allele in British and Dutch patients with sarcoidosis. Am J Respir Crit Care Med 165:1119–1124
Niimi T, Tomita H, Sato S et al (1999) Vitamin D receptor gene polymorphism in patients with sarcoidosis. Am J Respir Crit Care Med 160:1107–1109
Morohashi K, Takada T, Omori K, Suzuki E, Gejyo F (2003) Vascular endothelial growth factor gene polymorphisms in Japanese patients with sarcoidosis. Chest 123:1520–1526
Seyhan EC, Cetinkaya E, Altin S et al (2008) Vascular endothelial growth factor gene polymorphisms in Turkish patients with sarcoidosis. Tissue Antigens 72:162–165
Pabst S, Karpushova A, Dìaz-Lacava A et al (2010) VEGF gene haplotypes are associated with sarcoidosis. Chest 137:156–163
Williams GT, Williams WJ (1983) Granulomatous inflammation - a review. J Clin Pathol 36:723–733
Romagnani S (2006) Regulation of the T cell response. Clin Exp Allergy 36:1357–1366
Chen ES, Moller DR (2011) Sarcoidosis - scientific progress and clinical challenges. Nat Rev Rheumatol 7:457–467
Zissel G (2014) Cellular activation in the immune response of sarcoidosis. Semin Respir Crit Care Med 35:307–315
Orme IM, Cooper AM (1999) Cytokine/chemokine cascades in immunity to tuberculosis. Immunol Today 20:307–312
Boros DL (1978) Granulomatous inflammations. Prog Allergy 24:183–267
Chen ES, Song Z, Willett MH et al (2010) Serum amyloid A regulates granulomatous inflammation in sarcoidosis through Toll-like receptor-2. Am J Respir Crit Care Med 181:360–373
Wikén M, Grunewald J, Eklund A, Wahlström J (2009) Higher monocyte expression of TLR2 and TLR4, and enhanced pro-inflammatory synergy of TLR2 with NOD2 stimulation in sarcoidosis. J Clin Immunol 29:78–89
Gabrilovich MI, Walrath J, van Lunteren J et al (2013) Disordered Toll-like receptor 2 responses in the pathogenesis of pulmonary sarcoidosis. Clin Exp Immunol 173:512–522
Puissegur MP, Lay G, Gilleron M et al (2007) Mycobacterial lipomannan induces granuloma macrophage fusion via a TLR2-dependent, ADAM9- and beta1 integrin-mediated pathway. J Immunol 178:3161–3169
Gerke AK, Hunninghake G (2008) The immunology of sarcoidosis. Clin Chest Med 29:379–390
Agostini C, Semenzato G (1998) Cytokines in sarcoidosis. Semin Respir Infect 13:184–196
Bachwich PR, Lynch JP 3rd, Larrick J, Spengler M, Kunkel SL (1986) Tumor necrosis factor production by human sarcoid alveolar macrophages. Am J Pathol 125:421–425
Strausz J, Männel DN, Pfeifer S, Borkowski A, Ferlinz R, Müller-Quernheim J (1991) Spontaneous monokine release by alveolar macrophages in chronic sarcoidosis. Int Arch Allergy Appl Immunol 96:68–75
Gupta D, Agarwal R, Aggarwal AN, Jindal SK (2007) Molecular evidence for the role of mycobacteria in sarcoidosis: a meta-analysis. Eur Respir J 30:508–516
Dubaniewicz A, Dubaniewicz-Wybieralska M, Sternau A et al (2006) Mycobacterium tuberculosis complex and mycobacterial heat shock proteins in lymph node tissue from patients with pulmonary sarcoidosis. J Clin Microbiol 44:3448–3451
Oswald-Richter KA, Beachboard DC, Seeley EH et al (2012) Dual analysis for mycobacteria and propionibacteria in sarcoidosis BAL. J Clin Immunol 32:1129–1140
Chen ES, Wahlström J, Song Z et al (2008) T cell responses to mycobacterial catalase-peroxidase profile a pathogenic antigen in systemic sarcoidosis. J Immunol 181:8784–8796
Drake WP, Dhason MS, Nadaf M et al (2007) Cellular recognition of Mycobacterium tuberculosis ESAT-6 and KatG peptides in systemic sarcoidosis. Infect Immun 75:527–530
Dubaniewicz A, Trzonkowski P, Dubaniewicz-Wybieralska M, Dubaniewicz A, Singh M, Myśliwski A (2007) Mycobacterial heat shock protein-induced blood T lymphocytes subsets and cytokine pattern: comparison of sarcoidosis with tuberculosis and healthy controls. Respirology 12:346–354
Oswald-Richter KA, Beachboard DC, Zhan X et al (2010) Multiple mycobacterial antigens are targets of the adaptive immune response in pulmonary sarcoidosis. Respir Res 11:161
Eishi Y, Suga M, Ishige I et al (2002) Quantitative analysis of mycobacterial and propionibacterial DNA in lymph nodes of Japanese and European patients with sarcoidosis. J Clin Microbiol 40:198–204
Ebe Y, Ikushima S, Yamaguchi T et al (2000) Proliferative response of peripheral blood mononuclear cells and levels of antibody to recombinant protein from Propionibacterium acnes DNA expression library in Japanese patients with sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 17:256–265
Chen ES, Moller DR (2014) Etiologic role of infectious agents. Semin Respir Crit Care Med 35:285–295
Wahlström J, Dengjel J, Persson B et al (2007) Identification of HLA-DR-bound peptides presented by human bronchoalveolar lavage cells in sarcoidosis. J Clin Invest 117:3576–3582
Wahlström J, Dengjel J, Winqvist O et al (2009) Autoimmune T cell responses to antigenic peptides presented by bronchoalveolar lavage cell HLA-DR molecules in sarcoidosis. Clin Immunol 133:353–363
Zissel G, Prasse A, Muller-Quernheim J (2007) Sarcoidosis—immunopathogenetic concepts. Semin Respir Crit Care Med 28:3–14
Agostini C, Trentin L, Facco M et al (1996) Role of IL-15, IL-2, and their receptors in the development of T cell alveolitis in pulmonary sarcoidosis. J Immunol 157:910–918
Greene CM, Meachery G, Taggart CC et al (2000) Role of IL-18 in CD4+ T lymphocyte activation in sarcoidosis. J Immunol 165:4718–4724
Larousserie F, Pflanz S, Coulomb-L’Herminé A, Brousse N, Kastelein R, Devergne O (2004) Expression of IL-27 in human TH1-associated granulomatous diseases. J Pathol 202:164–171
Devergne O, Emilie D, Peuchmaur M, Crevon MC, D’Agay MF, Galanaud P (1992) Production of cytokines in sarcoid lymph nodes: preferential expression of interleukin-1 beta and interferon-gamma genes. Hum Pathol 23:317–323
Moller DR, Forman JD, Liu MC et al (1996) Enhanced expression of IL-12 associated with TH1 cytokine profiles in active pulmonary sarcoidosis. J Immunol 156:4952–4960
Shigehara K, Shijubo N, Ohmichi M et al (2000) Enhanced mRNA expression of Th1 cytokines and IL-12 in active pulmonary sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 17:151–157
Kim DS, Jeon YG, Shim TS et al (2000) The value of interleukin-12 as an activity marker of pulmonary sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 17:271–276
Minshall EM, Tsicopoulos A, Yasruel Z et al (1997) Cytokine mRNA gene expression in active and nonactive pulmonary sarcoidosis. Eur Respir J 10:2034–2039
Zissel G, Bäumer I, Schlaak M, Müller-Quernheim J (2000) In vitro release of interleukin-15 by broncho-alveolar lavage cells and peripheral blood mononuclear cells from patients with different lung diseases. Eur Cytokine Netw 11:105–112
Shigehara K, Shijubo N, Ohmichi M et al (2000) Increased levels of interleukin-18 in patients with pulmonary sarcoidosis. Am J Respir Crit Care Med 162:1979–1982
Agostini C, Meneghin A, Semenzato G (2002) T-lymphocytes and cytokines in sarcoidosis. Curr Opin Pulm Med 8:435–440
Agostini C, Trentin L, Perin A et al (1999) Regulation of alveolar macrophage-T cell interactions during Th1-type sarcoid inflammatory process. Am J Physiol 277:L240–L250
Gudmundsson G, Hunninghake GW (1997) Interferon-gamma is necessary for the expression of hypersensitivity pneumonitis. J Clin Invest 99:2386–2390
Leclerc S, Myers RP, Moussalli J, Herson S, Poynard T, Benveniste O (2003) Sarcoidosis and interferon therapy: report of five cases and review of the literature. Eur J Intern Med 14:237–243
Spagnolo P, Zeuzem S, Richeldi L, du Bois RM (2010) The complex interrelationships between chronic lung and liver disease: a review. J Viral Hepat 17:381–390
Walker C, Bauer W, Braun RK et al (1994) Activated T cells and cytokines in bronchoalveolar lavages from patients with various lung diseases associated with eosinophilia. Am J Respir Crit Care Med 150:1038–1048
Chensue SW, Warmington K, Ruth JH, Lukacs N, Kunkel SL (1997) Mycobacteria and schistosomal antigen-elicited granuloma formation in IFN-γ and IL-4 knockout mice. J Immunol 159:3565–3573
Umemura M, Yahagi A, Hamada S et al (2007) IL-17-mediated regulation of innate and acquired immune response against pulmonary Mycobacterium bovis bacille Calmette-Guerin infection. J Immunol 178:3786–3796
Okamoto Yoshida Y, Umemura M, Yahagi A et al (2010) Essential role of IL-17A in the formation of a mycobacterial infection-induced granuloma in the lung. J Immunol 184:4414–4422
Facco M, Cabrelle A, Teramo A et al (2011) Sarcoidosis is a Th1/Th17 multisystem disorder. Thorax 66:144–150
Ten Berge B, Paats MS, Bergen IM et al (2012) Increased IL-17A expression in granulomas and in circulating memory T cells in sarcoidosis. Rheumatology (Oxford) 51:37–46
Richmond BW, Ploetze K, Isom J et al (2013) Sarcoidosis Th17 cells are ESAT-6 antigen specific but demonstrate reduced IFN-γ expression. J Clin Immunol 33:446–455
Ostadkarampour M, Eklund A, Moller D et al (2014) Higher levels of interleukin IL-17 and antigen-specific IL-17 responses in pulmonary sarcoidosis patients with Löfgren’s syndrome. Clin Exp Immunol 178:342–352
Tøndell A, Moen T, Børset M, Salvesen Ø, Rø AD, Sue-Chu M (2014) Bronchoalveolar lavage fluid IFN-γ + Th17 cells and regulatory T cells in pulmonary sarcoidosis. Mediators Inflamm 2014:438070
Sakaguchi S, Miyara M, Costantino CM, Hafler DA (2010) FOXP3+ regulatory T cells in the human immune system. Nat Rev Immunol 10:490–500
Sakaguchi S (2005) Naturally arising Foxp3-expressing CD25 + CD4+ regulatory T cells in immunological tolerance to self and non-self. Nat Immunol 6:345–352
Miyara M, Amoura Z, Parizot C et al (2006) The immune paradox of sarcoidosis and regulatory T cells. J Exp Med 203:359–370
Taflin C, Miyara M, Nochy D et al (2009) FoxP3+ regulatory T cells suppress early stages of granuloma formation but have little impact on sarcoidosis lesions. Am J Pathol 174:497–508
Mathew S, Bauer KL, Fischoeder A, Bhardwaj N, Oliver SJ (2008) The anergic state in sarcoidosis is associated with diminished dendritic cell function. J Immunol 181:746–755
Ahmadzai H, Cameron B, Chui JJ, Lloyd A, Wakefield D, Thomas PS (2012) Peripheral blood responses to specific antigens and CD28 in sarcoidosis. Respir Med 106:701–709
Rappl G, Pabst S, Riemann D et al (2011) Regulatory T cells with reduced repressor capacities are extensively amplified in pulmonary sarcoid lesions and sustain granuloma formation. Clin Immunol 140:71–83
Prasse A, Zissel G, Lützen N et al (2010) Inhaled vasoactive intestinal peptide exerts immunoregulatory effects in sarcoidosis. Am J Respir Crit Care Med 182:540–548
Ho LP, Urban BC, Thickett DR, Davies RJ, McMichael AJ (2005) Deficiency of a subset of T-cells with immunoregulatory properties in sarcoidosis. Lancet 365:1062–1072
Crawshaw A, Kendrick YR, McMichael AJ, Ho LP (2014) Abnormalities in iNKT cells are associated with impaired ability of monocytes to produce IL-10 and suppress T-cell proliferation in sarcoidosis. Eur J Immunol 44:2165–2174
Baughman RP, Nagai S, Balter M et al (2011) Defining the clinical outcome status (COS) in sarcoidosis: Results of WASOG task force. Sarcoidosis Vasc Diffuse Lung Dis 28:56–64
Ziegenhagen MW, Schrum S, Zissel G et al (1998) Increased expression of proinflammatory chemokines in bronchoalveolar lavage cells of patients with progressing idiopathic pulmonary fibrosis and sarcoidosis. J Investig Med 46:223–231
Salez F, Gosset P, Copin MC, Lamblin Degros C, Tonnel AB, Wallaert B (1998) Transforming growth factor-beta1 in sarcoidosis. Eur Respir J 12:913–919
Homma S, Nagaoka I, Abe H et al (1995) Localization of platelet-derived growth factor and insulin-like growth factor I in the fibrotic lung. Am J Respir Crit Care Med 152:2084–2089
Elias JA, Freundlich B, Kern JA, Rosenbloom J (1990) Cytokine networks in the regulation of inflammation and fibrosis in the lung. Chest 97:1439–1445
Chensue SW, Warmington K, Ruth J, Lincoln P, Kuo MC, Kunkel SL (1994) Cytokine responses during mycobacterial and schistosomal antigen-induced pulmonary granuloma formation. Production of Th1 and Th2 cytokines and relative contribution of tumor necrosis factor. Am J Pathol 145:1105–1113
Wahlstrom J, Katchar K, Wigzell H, Olerup O, Eklund A, Grunewald J (2001) Analysis of intracellular cytokines in CD4+ and CD8+ lung and blood T cells in sarcoidosis. Am J Respir Crit Care Med 163:115–121
Kunkel SL, Lukacs NW, Strieter RM, Chensue SW (1996) Th1 and Th2 responses regulate experimental lung granuloma development. Sarcoidosis Vasc Diffuse Lung Dis 13:120–128
Conron M, du Bois R (2001) Immunological mechanisms in sarcoidosis. Clin Exp Allergy 31:543–554
Spagnolo P, Luppi F, Roversi P, Cerri S, Fabbri LM, Richeldi L (2012) Sarcoidosis: challenging diagnostic aspects of an old disease. Am J Med 125:118–125
Acknowledgments
This work was supported by the Swedish Heart-Lung Foundation (grant number 20100254), the Swedish Research Council (grant number K2013-57X-14182-12-3), through the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and Karolinska Institutet (grant number 20120025) and Karolinska Institutet.
Compliance with Ethical standards
ᅟ
Conflict of Interest
Paolo Spagnolo serves as consultant for Roche and has received consulting fees from Boehringer Ingelheim. Johan Grunewald, Jan Wahlström and Anders Eklund declare that they have no conflict of interest.
Research involving Human Participants and/or Animals
N/A
Informed consent
N/A
Author information
Authors and Affiliations
Corresponding author
Additional information
Johan Grunewald and Paolo Spagnolo contributed equally to this work.
Rights and permissions
About this article
Cite this article
Grunewald, J., Spagnolo, P., Wahlström, J. et al. Immunogenetics of Disease-Causing Inflammation in Sarcoidosis. Clinic Rev Allerg Immunol 49, 19–35 (2015). https://doi.org/10.1007/s12016-015-8477-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-015-8477-8