Abstract
The regenerating gene, Reg, was originally isolated from a rat regenerating islet complementary DNA (cDNA) library, and its human homologue was named REG Iα. Recently, we reported that REG Iα messenger RNA (mRNA), as well as its product, was overexpressed in ductal epithelial cells in the salivary glands of Sjögren’s syndrome patients. Furthermore, autoantibodies against REG Iα were found in the sera of Sjögren’s syndrome patients, and the patients who were positive for the anti-REG Iα antibody showed significantly lower saliva secretion than antibody-negative patients. We found the mechanism of REG Iα induction in salivary ductal epithelial cells. Reporter plasmid containing REG Iα promoter (−1190/+26) upstream of a luciferase gene was introduced into human NS-SV-DC and rat A5 salivary ductal cells. The cells were treated with several cytokines (interleukin (IL)-6, IL-8, etc.), upregulated in Sjögren’s syndrome salivary ducts, and the transcriptional activity was measured. IL-6 stimulation significantly enhanced the REG Iα promoter activity in both cells. Deletion analysis revealed that the −141∼−117 region of the REG Iα gene was responsible for the promoter activation by IL-6, which contains a consensus sequence for signal transducer and activator of transcription (STAT) binding. The introduction of small interfering RNA for human STAT3 abolished IL-6-induced REG Iα transcription. These results indicated that IL-6 stimulation induced REG Iα transcription through STAT3 activation and binding to the REG Iα promoter in salivary ductal cells. This dependence of REG Iα induction upon IL-6/STAT in salivary duct epithelial cells may play an important role in the pathogenesis/progression of Sjögren’s syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The salivary glands are exocrine glands that secrete saliva into the oral cavity, where components of saliva aid in digestion and prevent oral infection [1]. In humans, the majority of saliva is secreted from the parotid, submandibular, and sublingual glands, with minor contributions from numerous small accessory glands. For saliva production, activation of muscarinic receptors on the basolateral membrane of acinar cells results in fluid secretion into the ductal lumen, where the ion content is modulated as saliva travels along a series of collecting ducts into the main secretory duct, which empties into the oral cavity [1]. Salivary dysfunction induces dry mouse, oral infection, and poor nutrition and can significantly reduce quality of life [2]. Two primary causes of salivary dysfunction in humans are Sjögren’s syndrome, an autoimmune disease characterized by lymphocytic infiltration of the salivary gland and production of autoantibodies, and γ-radiation-induced dysfunction, an unintended consequence of treatment for head and neck cancers [3, 4]. Current treatments for salivary hypofunction (also known as “xerostomia”) include administration of sialogogues and saliva substitutes; however, these approaches are limited to only palliative therapies and not aimed at restoration of the function of damaged glands [5]. New strategies to treat xerostomia are being investigated to regenerate salivary glands and restore normal levels of saliva secretion [6, 7]. Therefore, a better understanding of the underlying mechanisms of both salivary gland inflammation in Sjögren’s syndrome and radiation therapy that results in tissue damage could reveal novel targets to prevent salivary gland degeneration and promote restoration of functional tissue.
Sjögren’s syndrome is a chronic autoimmune disease characterized by inflammation of exocrine glands, particularly the salivary and lacrimal glands [8–12]. Although the pathogenesis of exocrinopathy is not yet fully understood, infiltration of autoreactive lymphocytes and subsequent self-perpetuating immune-mediated loss of acinar and ductal cells is considered to be the cause of salivary and lacrimal gland dysfunction, resulting in xerostomia and xerophthalmia [13]. In addition, local or systemic overexpression of pro-inflammatory cytokines is involved with the pathogenesis [8–12]. In exocrine glands (such as salivary and lacrimal glands), pro-inflammatory cytokines such as interferon (IFN)α, IFNγ, tumor necrosis factor (TNF)α, interleukin (IL)-12, and IL-18, along with other cytokines important in T and B cell activation and autoantibody production, such as IL-6 and B cell-activating factor belonging to the tumor necrosis factor family (BAFF), are reported to be overexpressed. Autoantibodies may also play a role in the pathogenesis of Sjögren’s syndrome. A variety of autoantibodies, such as antibodies against SS-A/Ro, SS-B/La, α-fodrin, and acetylcholine muscarinic 3 receptor, have been detected in the sera of Sjögren’s syndrome patients [14]. It is unknown, however, whether any of the autoantibodies have a direct pathogenic role or are merely involved as a secondary response to another process.
Tissue injury leads cells to proliferate and differentiate to replace the dead cells, and inflammatory reactions are critical to this process [15]. Pancreatic β cell regeneration is induced by pancreatectomy [16], but such regeneration does not occur in the absence of inflammation [17, 18]. In the case of pancreatic duct obstruction [19, 20], leukemia inhibitory factor (LIF), a member of the IL-6-type cytokine family, is important in the control of proliferation of pancreatic duct cells [21].
It has previously been reported that experimental ligation of the main excretory duct of the salivary gland causes the apoptosis of acinar cells and the proliferation of duct cells in both rats and mice [22–24]. Moreover, reopening of the ligated main excretory duct induces the repopulation and morphological recovery to the normal state in the submandibular gland of rats [25, 26].
It is speculated that intercalated duct cells in the developing gland serve as the stem cells for the striated duct, granular convoluted tubule, and acinar cells, but this idea has not yet been completely established. Some of the striated duct cells are also considered to be the progenitor of granular convoluted tubule cells, since these cells have the highest susceptibility to thymidine labeling in the mouse submandibular gland [27].
The regenerating gene, Reg, was originally isolated from a rat regenerating islet complementary DNA (cDNA) library [28–30]. The Reg and Reg-related genes were isolated and revealed to constitute a multigene family, the Reg family, which consists of four subtypes (types I, II, III, and IV) based on the primary structures of the encoded proteins of the genes [29–31]. In humans, five functional REG family genes (REG Iα, REG Iβ, REG III, HIP/PAP, and REG IV) were isolated [29–31]. The Reg family gene products act as growth factors and promote cell proliferation and regeneration; therefore, they are considered to be important for various inflammatory diseases [29–31]. It has also been reported that the REG family gene expression was regulated by several cytokines or chemokines, such as IL-6, IL-8, IL-11, IL-22, IFNβ, IFNγ, and cytokine-induced neutrophil chemoattractant-2β (CINC-2β) [18, 32–37].
Recently, we reported that REG Iα messenger RNA (mRNA) as well as its product (REG Iα protein) was overexpressed in ductal epithelial cells in the minor salivary glands of Sjögren’s syndrome patients [38]. Furthermore, autoantibodies against REG Iα were found in the sera of Sjögren’s syndrome patients, and the patients with the anti-REG Iα autoantibody showed significant lower saliva secretion than the patients without the anti-REG Iα autoantibody [38]. We also showed that the mRNA levels of IL-6 and IL-8 were significantly higher in the Sjögren’s syndrome minor salivary glands than in normal minor salivary glands [38], suggesting that these cytokines may be involved in the overexpression of REG Iα mRNA in the Sjögren’s syndrome minor salivary glands. However, the precise mechanism by which REG Iα gene activation occurs in the Sjögren’s syndrome minor salivary gland cells has been elusive. This study was undertaken to reveal the role of cytokines in the REG Iα expression and subsequent intracellular mechanism for induction of REG Iα mRNA in salivary ductal cells of Sjögren’s syndrome patients.
Regenerating Gene
Rats on which Foglia [39] had performed a 90 % pancreatectomy exhibited glucosuria 1–3 months after the operation. The islets in the remaining pancreases of 90 % depancreatized rats were relatively less numerous and small size, and frequently exhibited fibrotic degeneration and degranulation [40, 41]. However, Yonemura et al. demonstrated that 90 % depancreatized rats administered daily with poly(ADP-ribose) polymerase (PARP) inhibitors, such as nicotinamide and 3-aminobenzamide, did not develop diabetes [16]. Three months after the partial pancreatectomy, the islets in the remaining pancreases of rats which had received the nicotinamide or 3-aminobenzamide injections were very much larger than the islets in the control. When the remaining pancreases were immunohistochemically stained, almost the entire area of the enlarged islets in nicotinamide- or 3-aminobenzamide-treated rats stained densely for insulin. On the other hand, cells staining for glucagon (α cells) and somatostatin (δ cells) were localized on the peripheries of the enlarged islets in the remaining pancreases of rats treated with PARP inhibitors. The immunohistochemical findings indicated that it was specifically the β cell population that increased in the islets of the remaining pancreases of PARP inhibitor-treated rats.
We isolated regenerating islets from the remaining pancreases of 90 % depancreatized rats, which had received nicotinamide for 3 months and constructed a cDNA library. By differential hybridization screening of the regenerating islet cDNA library, we identified a novel gene, encoding a 165-amino acid protein that was expressed in regenerating islets, and the novel gene was named regenerating gene (Reg) [28]. The human REG gene was isolated from a human pancreas cDNA library [28, 29]. The Reg gene was expressed in regenerating islets, but not detected in normal islets, suggesting possible roles for the gene in replication, growth, and maturation of pancreatic β cells.
We next prepared recombinant rat Reg protein and administered it to 90 % depancreatized rats and found frequent mitosis in the islets of the remaining pancreases by increased incorporation of [3H] thymidine and frequent mitosis in the islets of the remaining pancreases [42]. We also observed that the islets in the Reg protein-treated rats were enlarged and almost all the islets stained positive for insulin. The administration of the human REG protein also ameliorated diabetes in nonobese diabetic (NOD) mice and increased the β cell mass [43]. In addition, human recombinant REG protein stimulated the 5-bromo-2′-deoxyuridine (BrdU) incorporation of pancreatic β cell in vitro in concentration-dependently, and anti-REG autoantibodies that attenuated the REG protein-induced BrdU incorporation were found in the sera of diabetic patients [44]. These results indicated that Reg protein stimulated the regeneration and/or growth of pancreatic β cells, thereby ameliorating animal diabetes.
Reg Receptor
We next isolated a cDNA for the Reg protein receptor from a rat islet cDNA library [45]. When the mammalian expression vector for the cDNA was constructed and introduced into rat RINm5F β cells, the incorporation of BrdU, as well as the cell numbers in response to the Reg protein, was significantly increased in the transformants. A homology search revealed that the cDNA was a homologue of a human multiple exostoses (EXT)-like gene, especially the human EXT-like gene 3 (EXTL3; over 97 % amino acid identity), indicating that the receptor was encoded by the EXTL3 gene and that it mediated growth signals of the Reg protein for β cell regeneration. After the report that the Extl3 gene encodes the Reg receptor [45], Acquatella-Tran Van Ba et al. confirmed that Extl3 is a Reg receptor [46], and several groups also reported Extl3 as a Reg protein receptor [47–51]. In a later study, further advances in the Reg receptor (Extl3) were reported; Reg receptor (Extl3) overexpression in pancreatic β cells as well as Reg protein addition to β cells induced the activating transcription factor-2 (ATF-2) activation [52], and a β cell-specific knockout for Extl3 resulted in abnormal islet morphology with reduced β cell proliferation [53].
The Reg receptor (EXTL3) mRNA expression was also detected in the liver, heart, kidney, spleen, thymus, stomach, small intestine, and colon, as well as pancreatic acinar and ductal cells, suggesting that the Reg-Reg receptor system is involved with a variety of cell types in addition to β cells [29, 30, 45–49].
Several Reg and Reg-related genes have been isolated and found to constitute a multigene family [29, 54]. Based on the primary structures of the Reg proteins, the members of the family are grouped into four subgroups, that is, types I, II, III, and IV [28–30, 54]. Type I Reg proteins are expressed in regenerating islets. Type I Reg has recently been reported to be expressed in human colorectal carcinomas and in rat gastric mucosa and enterochromaffin-like cells [29, 30, 55]. Type III Reg proteins have been suggested to be involved in cellular proliferation in intestinal Paneth’s granular cells, hepatocellular carcinomas, pancreatic acinar cells, keratinocytes, and Schwann cells, suggesting that the Reg family proteins may potentially be involved in the regeneration of several different cells and tissues [29, 30].
Regulation of Reg Gene Expression
The Reg I gene has been shown to be expressed only during islet regeneration, and Reg receptor expression was unchanged during islet regeneration [28–30, 45]. Accordingly, the regeneration and proliferation of pancreatic β cells appear to be primarily regulated by the Reg I gene expression. We revealed that the combined addition of IL-6 and dexamethasone increased the Reg I mRNA level and a further addition of nicotinamide and 3-aminobenzamide (both PARP inhibitors), increased the Reg I mRNA even more [18]. Progressive deletion of the 5′-flankling region of the rat Reg I gene revealed that the −81 to −70 region was essential for the activity of the Reg I promoter, and a gel mobility shift assay revealed that PARP was binding the sequence. The inhibition of PARP activity was shown to facilitate Reg I transcription by preventing excessive PARP self-poly(ADP-ribosyl)ation.
Most recently, we found that the combined addition of the IL-6 and dexamethasone-induced REG Iα and REG Iβ expression in human 1.1B4 β cells [56]. In the study, promoter assays revealed that a signal transduction and activation of transcription (STAT)-binding site in each promoter of REG Iα and REG Iβ was essential for the IL-6 + dexamethasone-induced promoter activation. An electrophoretic mobility shift assay and a chromatin immunoprecipitation assay revealed that IL-6 + dexamethasone stimulation increased STAT3 binding to the REG Iα promoter. Furthermore, introduction of small interfering RNA for STAT3 and AG490, a Janus kinase (JAK) 2 inhibitor, significantly inhibited the IL-6 + dexamethasone-induced expression of the REG Iα and REG Iβ. Therefore, the expression of REG Iα and REG Iβ appeared to be upregulated in human β cells under IL-6 + dexamethasone stimulation through the JAK/STAT pathway [56].
Reg Gene Family in Diseases
Reg proteins are expressed in regenerating islets and involved in β cell regeneration [28–30, 52, 57]. Reg was also shown to mediate gastric mucosal proliferation in rats [55, 58]. The expression of the REG Iα gene is closely related to the infiltrating property of gastric carcinoma, and it may be a prognostic indicator of differentiated adenocarcinoma of the stomach [59, 60]. Correlation between the expression of the REG family genes and cancer prognosis have been reported not only in gastric carcinomas but also in colon, esophagus, lung, liver, prostate, and head and neck cancers [61–66]. These correlations suggest that the Reg gene family is involved in cell growth in a variety of cell types other than pancreatic β cells and that the REG family gene expression in cancer tissues/cells might be a new cancer prognosis marker and/or a therapeutic target.
In addition, autoantibodies/autoimmunity against Reg family proteins and its potential mechanism were also reported in diabetes and in other autoimmune diseases, such as celiac disease and Sjögren’s syndrome [33, 38, 44, 67]. Autoimmunity against the Reg family protein(s) may be a new diagnostic marker and/or therapeutic target for immune-mediated diseases.
The Role of Autoimmunity Against Reg Protein in Sjögren’s Syndrome
It was reported that REG Iα was expressed in ductal epithelial cells in the minor salivary glands of patients with Sjögren’s syndrome [68]. Kimura et al. examined this REG Iα protein expression using immunohistochemistry for the REG Iα protein and found the REG Iα protein was highly expressed in ductal epithelial cells in the minor salivary glands of patients with Sjögren’s syndrome but rarely expressed in those of normal minor salivary glands [68]. It was suggested that REG Iα protein plays a role in the regeneration of the salivary glands of people with Sjögren’s syndrome, but whether autoimmunity against REG Iα protein was involved with the pathogenesis of Sjögren’s syndrome was not clear. It was also unclear which REG family gene(s) were expressed in the Sjögren’s syndrome patients.
We examined the expression of REG family genes in the minor salivary glands of Sjögren’s syndrome patients and screened anti-REG Iα autoantibodies in their sera. We prepared total RNA from formalin-fixed, paraffin-embedded minor salivary gland tissue specimens using an RNeasy FFPE kit and analyzed the mRNA levels of REG family genes (REG Iα, REG Iβ, REG III, HIP/PAP, and REG IV) using specific primers (5′-AGGAGAGTGGCACTGATGACTT-3′ and 5′-TAGGAGACCAGGGACCCACTG-3′ for REG Iα, 5′-GCTGATCTCCTCCCTGATGTTC-3′ and 5′-GGCAGCTGATTCGGGGATTA-3′ for REG Iβ, 5′-GAATATTCTCCCCAAACTG-3′ and 5′-GAGAAAAGCCTGAAATGAAG-3′ for REG III, 5′-AGAGAATATTCGCTTAATTCC-3′ and 5′-AATGAAGAGACTGAAATGACA-3′ for HIP/PAP, and 5′-ATCCTGGTCTGGCAAGTC-3′ and 5′-CGTTGCTGCTCCAAGTTA-3′ for REG IV) by quantitative real-time reverse transcriptase-polymerase chain reaction (qRT-PCR) [38]. No REG Iβ mRNA was detected in the minor salivary glands of either the controls or patients with primary Sjögren’s syndrome. Similarly, the mRNA levels of REG III, HIP/PAP, and REG IV did not differ between the minor salivary glands of controls and those of patients with primary Sjögren’s syndrome. In contrast, the mRNA level of REG Iα in the minor salivary glands of primary Sjögren’s syndrome patients was significantly higher than that in the controls. We then analyzed REG Iα protein expression in the minor salivary glands of primary Sjögren’s syndrome patients via immunohistochemistry, using an anti-REG I protein monoclonal antibody. REG Iα protein was detected in the ductal epithelial cells, whereas acinar cells were rarely detected.
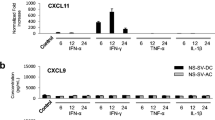
It has been reported that REG family gene expression was regulated by several cytokines or chemokines, such as IL-6, IL-8, IL-11, IL-22, IFNβ, IFNγ, and CXCL1 (CINC-2β) [18, 32–37, 56]. In order to investigate regulation of REG Iα gene expression in the minor salivary glands, we measured IL-6, IL-8, IL-11, IL-22, IL-22 receptor, IFNβ, IFNγ, CXCL1 (CINC-2β), IL-6 receptor, and gp130 mRNAs using specific primers (5′-GGTACATCCTCGACGGCATC-3′ and 5′-GCCTCTTTGCTGCTTTCACAC-3′ for IL-6, 5′-TAGCAAAATTGAGGCCAAGG-3′ and 5′-GGACTTGTGGATCCTGGCTA-3′ for IL-8, 5′-TCTCTCCTGGCGGACACG-3′ and 5′-AATCCAGGTTGTGGTCCCC-3′ for IL-11, 5′-GCAGGCTTGACAAGTCCAACT-3′ and 5′-GCCTCCTTAGCCAGCATGAA-3′ for IL-22, 5′-CTACATGTGCCGAGTGAAGA-3′ and 5′-ACATATCTGTAGCTCAGGTA-3′ for IL-22 receptor, 5′-CATTACCTGAAGGCCAAGGA-3′ and 5′-CAGCATCTGCTGGTTGAAGA-3′ for IFNβ, 5′-ATTCGGTAACTGACTTGAATGTCC-3′ and 5′-CTCTTCGACCTCGAAACAGC-3′ for IFNγ, 5′-GAAAGCTTGCCTCAATCCTG-3′ and 5′-TCCTAAGCGATGCTCAAACA-3′ for CXCL1, 5′-TGAGCTCAGATATCGGGCTGAAC-3′ and 5′-CGTCGTGGATGACACAGTGATG-3′ for IL-6 receptor, and 5′-AGGACCAAAGATGCCTCAACT-3′ and 5′-TTGGACAGTGAATGAAGATCG-3′ for gp130) via qRT-PCR [38]. The mRNA levels of IL-6 and IL-8 in primary Sjögren’s syndrome minor salivary glands were significantly higher than the levels in normal minor salivary glands. The mRNA levels of IL-11, IL-22, IL-22 receptor, IFNγ, CINC-2β, IL-6 receptor, and gp130 in minor salivary glands were not significantly different between primary Sjögren’s syndrome patients and normal controls. The mRNA of IFNβ was not detected in primary Sjögren’s syndrome minor salivary glands. These results suggested that the upregulation of IL-6 and IL-8 could induce overexpression of the REG Iα gene in primary Sjögren’s syndrome minor salivary glands.
We examined autoantibodies against the REG Iα protein (anti-REG Iα antibodies) in the sera from primary Sjögren’s syndrome patients and healthy controls by the immunoblot method, using diluted patient serum as a primary antibody in the screener blotter and an enhanced chemiluminescent detection system [38, 44, 69]. Eleven percent (13 of 117) of patients with primary Sjögren’s syndrome tested positive for anti-REG Iα antibodies, whereas only 2.2 % (6 out of 271) were positive in the controls. The group that was positive for anti-REG Iα antibodies had significantly lower saliva secretion than the negative group using an unstimulated Saxon test [70]. The ratio of destructive stage (stage 4, based on Rubin and Holt’s criteria) in sialography in the group that was positive for anti-REG Iα antibodies was significantly higher than that in the antibody-negative group. Furthermore, all the patients in the group that was positive for anti-REG Iα antibodies showed REG Iα expression in minor salivary gland ductal cells, whereas only 40 % in the antibody-negative group showed REG Iα expression in the minor salivary glands. These results suggest that autoimmunity to REG is associated with the regeneration of the ductal epithelial cells of the minor salivary glands in primary Sjögren’s syndrome patients.
Regulation of REG Gene Expression in Salivary Ductal Cells
We have reported that anti-REG Iα antibodies were found in the sera of primary Sjögren’s syndrome patients and correlated with clinical manifestations. We also reported that mRNA levels of IL-6 and IL-8 as well as REG Iα were significantly elevated, suggesting that IL-6 and IL-8 may be involved in the overexpression of REG Iα mRNA in minor salivary gland ductal cells [38] (Fig. 1). The precise mechanism of regulation of REG Iα gene expression in minor salivary gland ductal cells, however, has been elusive. The present study was undertaken to determine the role of cytokines and the intracellular mechanism for regulation of the REG Iα gene in the salivary ductal cells of Sjögren’s syndrome patients.
Possible involvement of IL-6/IL-8 in REG Iα gene expression. The mRNA levels of IL-6 and IL-8 were correlated with that of REG Iα in Sjögren’s syndrome salivary specimens [38]. However, the precise mechanism of regulation of REG Iα gene expression in minor salivary gland ductal cells has been elusive. We elucidate the role of cytokines (IL-6, IL-8, or both) and intracellular mechanism for regulation of REG Iα gene in the salivary ductal cells of Sjögren’s syndrome patients
Induction of REG Iα mRNA by IL-6
We previously reported that the mRNA levels of REG Iα, IL-6, and IL-8 in minor salivary glands of Sjögren’s syndrome patients were significantly increased [38]. According to previous reports, both IL-6 and IL-8 could induce REG Iα expression [34, 36]. In order to investigate whether IL-6 or IL-8 upregulates REG Iα in salivary ductal cells, we analyzed the REG Iα mRNA expression in human NS-SV-DC salivary ductal cells, simian virus 40-immortalized cells derived from human salivary ducts [71], after treatment of human IL-6 (20 ng/mL; Roche, Mannheim, Germany), human IL-8 (100 nM; Wako Pure Chemical, Osaka, Japan), dexamethasone (100 nM; MP Biochemicals, Santa Ana, CA) and the combination of them by real-time RT-PCR using human REG Iα-specific primers as described. The treatment of IL-6 but neither IL-8 nor dexamethasone induced the expression of REG Iα mRNA (Fig. 2) [72]. The combinations of IL-6 + dexamethasone or IL-6 + IL-8 showed no additional effect compared with IL-6 alone. These results indicate that human salivary ductal cells express REG Iα mRNA in response to stimulation of IL-6.
The mRNA levels of REG family and HGF genes in NS-SV-DC human salivary ductal cells (kindly provided by Dr. M. Azuma, Department of Oral Medicine, Tokushima University School of Dentistry, Tokushima, Japan, and maintained in Keratinocyte SFM (Life Technologies, Carlsbad, CA)) treated with IL-6 (20 ng/mL), dexamethasone (Dx; 100 nM), IL-8 (100 nM), IL-6 + Dx, or IL-6 + IL-8. The levels of REG family and HGF mRNAs were measured by real-time RT-PCR using β-actin as an endogenous control as described [56, 65, 66, 72, 91, 102–106] (Adopted from [72])
Activation of REG Iα Gene Promoter by IL-6
To determine whether the induction of REG Iα mRNA was caused by the activation of transcription, a 1216-base pair fragment containing 1190-base pair of the promoter region (−1190∼+26) of the human REG Iα gene [73] was fused to the luciferase reporter gene of pGL3-Basic vector and transfected into human NS-SV-DC and rat A5 [74, 75] salivary ductal cells using the Lipofectamine™ 2000 reagent. Six hours after transfection, cells were incubated with IL-6 or IL-8 for 24 h, and cell extracts were prepared for luciferase assay. Luciferase assay revealed that IL-6 stimulation significantly enhanced the REG Iα promoter activity not only in human NS-SV-DC cells (Fig. 3a) but also in rat A5 cells (Fig. 3b) [72]. Treatment with IL-8 did not alter the transcriptional activity of REG Iα in NS-SV-DC cells nor in A5 cells. These results clearly indicated that REG Iα mRNA was induced by IL-6 in salivary ductal cells at the transcriptional level.
Luciferase assays in salivary ductal cells. Human NS-SV-DC cells (a) and rat A5 cells (derived from the salivary ducts of male Fischer 344 weanling rats, which were kindly provide by Dr. B.J. Baum of the National Institute of Dental and Craniofacial Research, NIH, Bethesda, MD, by treating explanted tissue clumps with 3-methylcholanthrene, and maintaining in DMEM supplemented with 10 % fetal bovine serum) (b) were transfected with constructs containing REG Iα promoter. After transfection, the cells were stimulated with IL-6 (20 ng/mL human IL-6 in NS-SV-DC cells or 200 ng/mL rat IL-6 in A5 cells) or IL-8 (100 nM human IL-8 in NS-SV-DC cells or 100 nM rat IL-8 in A5 cells); thereafter, the luciferase activities were measured as described [72, 104–106] (Adopted from [72]). The diagram represents relative luciferase activities to the untreated group. “Basic” was represents a promoterless construct, pGL3-Basic
Localization of IL-6-Responsible Region in the REG Iα Gene Promoter
In order to identify the region in the REG Iα gene promoter essential for the transcription of the REG Iα mRNA in response to IL-6 stimulation, progressive deletions of the REG Iα promoter into pGL3-Basic vector was performed. The promoter plasmids were transfected into human NS-SV-DC and rat A5 salivary ductal cells by lipofection method, and the transfected cells were stimulated by IL-6 as described above. The deletion down to position −141 did not attenuate IL-6-induced REG Iα promoter activity; however, an additional deletion to −117 caused a remarkable decrease in IL-6-induced promoter activity of REG Iα in both cells (Fig. 4) [72]. These results indicated that the promoter region of −141 to −117 of the REG Iα gene was responsible for the REG Iα promoter activation by IL-6.
Deletion analysis of human REG Iα promoter. Human NS-SV-DC cells (a) and rat A5 cells (b) were transfected with constructs containing various deletion mutants of REG Iα promoter. Constructs listed on ordinate are numbered according to their 5′ terminus in the REG Iα promoter. The transfected cells were stimulated with IL-6 (20 ng/mL human IL-6 in NS-SV-DC cells or 200 ng/mL rat IL-6 in A5 cells); thereafter, the luciferase activities were measured as described [72] (Adopted from [72]). The diagram represents relative luciferase activities to the untreated group of “−1190”
STAT3 Is a Key Factor for REG Iα Gene Transcription
A computer-aided search for sequences similar to known cis-acting elements revealed that the region of −141 to −117 of the REG Iα gene contains a consensus binding sequence for STAT. Site-directed mutagenesis of the STAT binding site was conducted within the luciferase construct of “−141.” The mutation constructs, in which the possible STAT binding site was destroyed, showed remarkable reductions in IL-6-induced promoter activities (Fig. 5). These results strongly suggested that STAT is the most important regulator for the REG Iα transcriptional activity by IL-6 in salivary ductal cells. In order to verify the role of STAT3 in IL-6-induced REG Iα induction, small interfering RNA (siRNA) for human STAT3 mRNA (5′-GCACCUUCCUGCUAAGAUUtt-3′) was introduced into NS-SV-DC cells using the Lipofectamine® RNAiMAX transfection reagent, and the IL-6-induced REG Iα mRNA expression was analyzed by real-time RT-PCR. As shown in Fig. 6, the introduction of siRNA for human STAT3 abolished not only IL-6-induced STAT3 upregulation but also IL-6-induced REG Iα upregulation, indicating that REG Iα gene transcription was induced by IL-6 through STAT3 binding to the STAT binding site located in −141 to −117 of the human REG Iα gene promoter [72].
(a) Alignment of REG Iα promoter region. Nucleotides insertions and substitutions in the cis-elements are indicated in RED (underlined). (b), (c) Effects of site-directed mutagenesis of the cis-elements within the REG Iα gene promoter. Human NS-SV-DC cells (b) and rat A5 cells (c) were transfected with the indicated constructs. Bar graph indicated relative luciferase activity to the untreated group of “−141”
Effects of STAT3-siRNA transfection on IL-6-induced REG Iα promoter activity in NS-SV-DC cells. After siRNA introduction, NS-SV-DC human salivary ductal cells were stimulated with IL-6 (20 ng/mL). The expression of (a) STAT3 (using specific primers: sense primer 5′-CAGGATGGCCCAATGGAATC-3′ and antisense primer 5′-CCCAGGAGATTATGAAACACC-3′) and (b) REG Iα mRNA was measured by real-time RT-PCR using β-actin as an endogenous control [56, 72] (Adopted from [72])
Conclusion
In the previous study, we reported that the REG Iα protein was overexpressed in ductal epithelial cells in the minor salivary glands of Sjögren’s syndrome patients, and that the saliva secretion was attenuated in Sjögren’s syndrome patients with autoantibodies to REG Iα [38]. We also showed the mRNA levels of IL-6 and IL-8 were significantly higher in the Sjögren’s syndrome minor salivary glands than those in normal minor salivary glands [38, 76]. In the present study, we showed that REG Iα overexpression in salivary ductal cells was induced by IL-6 but not by IL-8 at the transcriptional level.
IL-6, a potent pro-inflammatory cytokine, is involved in acute phase response, B cell proliferation and plasma cell formation, and T cell stimulation and recruitment [8, 77]. IL-6 is also regarded as a pivotal mediator in chronic inflammatory diseases and many autoimmune diseases, such as rheumatoid arthritis, multiple sclerosis, and Crohn’s disease [78]. High serum concentrations of IL-6 in primary Sjögren’s syndrome patients has been described, and the serum levels of IL-6 correlated with the degree of infiltration of lymphocytes in the salivary glands [10, 79, 80]. Binding of IL-6 to its receptor leads to homodimerization of an IL-6 receptor component gp130, resulting in the activation of JAK and subsequent phosphorylation of STAT3 [81]. STAT3 plays a crucial role in transmitting cytokine signals to the nucleus and promotes cell proliferation and anti-apoptosis [82–85]. Thus, the JAK/STAT pathway has been shown to be involved in carcinogenesis under a background of inflammation. Furthermore, accumulating evidence indicates that the JAK/STAT pathway may be involved in multiple immune functions: STAT1 and STAT4 mainly induce IFNγ expression in Th1 cells, STAT6 induces IL-4 expression in Th2 cells, and STAT3 induces IL-17 expression in Th17 cells [86].
Our results revealed that IL-6 stimulation enhanced REG Iα gene expression through STAT3 activation in salivary ductal cells. Involvement of STAT signaling in REG family gene expression has been reported by other groups in other cell systems: In gastric epithelial cells, Lee et al. described the IL-11/STAT3 signaling pathway was important in Helicobacter pylori CagA-directed REG 3γ (HIP/PAP) expression [35]. REG3A (HIP/PAP) was induced by IL-6 in pancreatic cancer cells (pancreatic ductal cells) through the JAK2/STAT3 pathway [87]. Sekikawa et al. showed that REG Iα gene expression was regulated by the IL-22/STAT3 pathway in colon cancer cells and by the IL-6/STAT3 pathway in gastric cancer cells [36, 88]. Most recently, we showed that REG Iα gene expression was activated in human pancreatic β cells by combined stimulation of IL-6 + dexamethasone via the JAK/STAT3 signaling [56]. These studies were implemented in gastrointestinal cell lines and pancreatic β cells, and to the best of our knowledge, this is the first report that revealed the association of the IL-6/STAT pathway and REG Iα expression in salivary ductal epithelial cells.
IL-8, also known as CXCL8, is a pro-inflammatory chemokine associated with the promotion of neutrophil chemotaxis and degranulation [89]. Several reports have indicated the involvement of IL-8 in pathogenesis of Sjögren’s syndrome. Cuello et al. described that minor salivary gland ductal epithelial cells of Sjögren’s syndrome patients highly expressed IL-8 [90]. As mentioned above, the levels of IL-8 were also reported to be correlated with REG gene expression in gastric cancer cells [34]. We also showed that the IL-8 mRNA was highly expressed in Sjögren’s syndrome minor salivary glands [38]. In the present study, however, we showed that IL-8 did not induce REG Iα expression in salivary ductal cells, suggesting that high levels of IL-8 in Sjögren’s syndrome minor salivary glands are not involved in their REG Iα upregulation.
Reg I gene was originally found to be expressed in rat regenerating islets but not in normal pancreatic islets [28]. RINm5F, a rat insulinoma-derived cell line, showed significant increase in cell numbers in the presence of Reg I/REG Iα protein [18, 29, 44, 91] via activating transcription factor-2/cyclin D1 pathway [52]. Human REG Iα protein administration ameliorated diabetes in NOD mice, with an increase in the β cell mass [43]. We generated transgenic mice expressing mouse Reg I, which was under an insulin promoter, showed increased [3H]thymidine incorporation in the pancreatic islets [92]. The Reg I transgene-carrying NOD mice were also generated by intercrossing the transgenic mice expressing Reg I in pancreatic β cells with NOD mice. The development of diabetes, judged by glucosuria at least two consecutive determinations, in the resultant Reg I transgenic NOD mice was significantly retarded. Additionally, anti-REG Iα autoantibodies, which were found in diabetic patient sera, were showed to retard the proliferation of pancreatic β cells in vitro [44]. These results suggest that Reg I/REG Iα protein stimulates the proliferation of pancreatic β cells. We previously reported that primary Sjögren’s syndrome patients with anti-REG antibodies showed significantly lower salivary secretion [38], suggesting that IL-6-induced REG Iα protein in salivary ductal cells is associated with regeneration of damaged ductal epithelial cells of minor salivary glands and that anti-REG autoantibodies attenuate the proliferation/regeneration of salivary ductal/acinar cells.
In the present study, we showed that the REG Iα gene was activated by the IL-6/STAT3 signaling in salivary duct epithelial cells. STAT binding element was reported not only in REG Iα promoter but also in other REG family promoters, such as REG Iβ, HIP/PAP, and REG III promoters [54, 56], suggesting possible activation of the genes in the salivary ducts of Sjögren’s syndrome patients through the IL-6/STAT3 axis. In our previous study, however, no REG Iβ mRNA was detected either in the control or the Sjögren’s syndrome salivary glands. The mRNA levels of REG III and HIP/PAP also were not different between the control and Sjögren’s syndrome salivary glands. In contrast, the mRNA level of REG Iα in the salivary glands of Sjögren’s syndrome patients was significantly higher than that of the controls [38]. In Sjögren’s syndrome, involvement of several cytokines other than IL-6, such as BAFF, IL-12/IL-23, and IFNα, was also reported [8]. Combination(s) of these cytokines with IL-6 may contribute to REG Iα-specific overexpression in salivary duct epithelial cells of Sjögren’s syndrome patients. As a result, anti-REG Iα autoantibodies were raised in Sjögren’s syndrome patients [38] and their salivary functions may be affected.
To alleviate xerostomia, which is one of chief manifestations of Sjögren’s syndrome, treatment with conventional systemic immunosuppressive drugs has been tried; however, the therapeutic effects were doubtful [93–96]. Recently, treatments with monoclonal antibodies which target inflammatory cytokines or cell surface antigens were developed in several autoimmune diseases [97, 98]. As IL-6 is shown to be highly expressed in the salivary glands of Sjögren’s syndrome patients, blocking the IL-6 signal by a monoclonal antibody against IL-6 receptor is expected to have beneficial effects [10]. Our results, however, suggested that IL-6 was associated with regeneration of ductal epithelial cells via REG Iα protein expression. Therefore, blocking IL-6 and/or its receptor may induce untoward effects. Rituximab, a chimeric anti-CD20 monoclonal antibody that binds to the B cell surface antigen CD20, has been shown to have beneficial effects for xerostomia of Sjögren’s syndrome patients in several trials [99, 100]. Rituximab therapy has also been shown to decrease autoantibody production [101]. It is possible that beneficial effects of rituximab for Sjögren’s syndrome were associated with B cell depletion and subsequent decrease of production of pathogenic autoantibodies, including anti-REG Iα autoantibodies.
In conclusion, the present study showed that REG Iα transcription in salivary ductal cells was stimulated by IL-6. Our study also demonstrated that STAT3 bound the consensus sequence of REG Iα promoter and regulated transcription in ductal epithelial cells in response to IL-6 stimulation (Fig. 7). It was suggested that overexpression of REG Iα protein in salivary ductal cells is dependent on the IL-6/STAT pathway and may play a role in the pathogenesis of Sjögren’s syndrome.
Possible mechanism of IL-6-induced REG Iα expression in salivary ductal epithelial cells (adopted from [72]) and its role in salivary dysfunction. IL-6 induced by inflammation and/or autoimmunity stimulates REG Iα transcription via the JAK/STAT pathway, leading to overexpression of REG Iα protein. As some of Sjögren’s syndrome patients have anti-REG Iα autoantibodies [38], salivary ductal cells expressing REG Iα protein are attacked by the autoantibodies, leading to dysfunction of saliva secretion [38]
References
Pedersen AM, Bardow A, Jensen SB, Nauntofte B (2002) Saliva and gastrointestinal functions of taste, mastication, swallowing and digestion. Oral Dis 8:117–129
Atkinson JC, Grisius M, Massey W (2005) Salivary hypofunction and xerostomia: diagnosis and treatment. Dent Clin North Am 49:309–326
Fox PC (1998) Acquired salivary dysfunction. Drugs and radiation. Ann NY Acad Sci 842:132–137
Brito-Zerón P, Sisó-Almirall A, Bové A, Kostov BA, Ramos-Casals M (2013) Primary Sjögren syndrome: an update on current pharmacotherapy options and future directions. Expert Opin Pharmacother 14:279–289
Vissink A, Mitchell JB, Baum BJ, Limesand KH, Jensen SB, Fox PC, Elting LS, Langendijk JA, Coppes RP, Reyland ME (2010) Clinical management of salivary gland hypofunction and xerostomia in head-and-neck cancer patients: successes and barriers. Int J Radiad Oncol Biol Phys 78:983–991
Lombaert IM, Brunsting JF, Wierenga PK, Faber H, Stokman MA, Kok T, Visser WH, Kampinga HH, de Haan G, Coppes RP (2008) Rescue of salivary gland function after stem cell transplantation in irradiated glands. PLoS One 3:e2063
Ogawa M, Oshima M, Imamura A, Sekine Y, Ishida K, Yamashita K, Nakajima K, Hirayama M, Tachikawa T, Tsuji T (2013) Functional salivary gland regeneration by transplantation of a bioengineered organ germ. Nat Commun 4:2498
Roescher N, Tak PP, Illei GG (2010) Cytokines in Sjögren’s syndrome: potential therapeutic targets. Ann Rheum Dis 69:945–948
Tincani A, Andreoli L, Cavazzana I, Doria A, Favero M, Fenini MG, Franceschini F, Lojacono A, Nascimbeni G, Santoro A, Semeraro F, Toniati P, Shoenfeld Y (2013) Novel aspects of Sjögren’s syndrome in 2012. BMC Med 11:93
Roescher N, Tak PP, Illei GG (2009) Cytokines in Sjögren’s syndrome. Oral Dis 15:519–526
Nikolov NP, Illei GG (2009) Pathogenesis of Sjögren’s syndrome. Curr Opin Rheumatol 21:465–470
Mariette X, Gottenberg JE (2010) Pathogenesis of Sjögren’s syndrome and therapeutic consequences. Curr Opin Rheumatol 22:471–477
Cornec D, Saraux A, Jousse-Joulin S, Pers JO, Boisramé-Gastrin S, Renaudineau Y, Gauvin Y, Roguedas-Contios AM, Genestet S, Chastaing M, Cochener B, Devauchelle-Pensec V (2015) The differential diagnosis of dry eyes, dry mouth, and parotidomegaly: a comprehensive review. Clin Rev Allergy Immunol 49:278–87
Yoshimi R, Ueda A, Ozato K, Ishigatsubo Y (2012) Clinical and pathological roles of Ro/SSA autoantibody system. Clin Dev Immunol 2012:606195
Tsirogianni AK, Moutsopoulos NM, Moutsopoulos HM (2006) Wound healing: immunological aspects. Injury 37(Suppl 1):S5–S12
Yonemura Y, Takashima T, Miwa K, Miyazaki I, Yamamoto H, Okamoto H (1984) Amelioration of diabetes mellitus in partially depancreatized rats by poly(ADP-ribose) synthetase inhibitors. Evidence of islet B-cell regeneration. Diabetes 33:401–404
Lampeter EF, Gurniak M, Brocker U, Klemens C, Tubes M, Friemann J, Kolb H (1995) Regeneration of beta-cells in response to islet inflammation. Exp Clin Endocrinol Diabetes 103(Suppl 2):74–78
Akiyama T, Takasawa S, Nata K, Kobayashi S, Abe M, Shervani NJ, Ikeda T, Nakagawa K, Unno M, Matsuno S, Okamoto H (2001) Activation of Reg gene, a gene for insulin-producing β-cell regeneration: poly(ADP-ribose) polymerase binds Reg promoter and regulates the transcription by autopoly(ADP-ribosyl)ation. Proc Natl Acad Sci USA 98:48–53
Rosenberg L (1998) Induction of islet cell neogenesis in the adult pancreas: the partial duct obstruction model. Microsc Res Tech 43:337–346
Hao E, Lee SH, Levine F (2013) Efficient β-cell regeneration by a combination of neogenesis and replication following β-cell ablation and reversal of pancreatic duct ligation. Stem Cells 31:2388–2395
De Breuck S, Baeyens L, Bouwens L (2006) Expression and function of leukaemia inhibitory factor and its receptor in normal and regenerating rat pancreas. Diabetologia 49:108–116
Walker NI, Gobé GC (1987) Cell death and cell proliferation during atrophy of the rat parotid gland induced by duct obstruction. J Pathol 153:333–344
Takahashi S, Nakamura S, Suzuki R, Islam N, Domon T, Yamamoto T, Wakita M (2000) Apoptosis and mitosis of parenchymal cells in the duct-ligated rat submandibular gland. Tissue Cell 32:457–463
Hisatomi Y, Okumura K, Nakamura K, Matsumoto S, Satoh A, Nagano K, Yamamoto T, Endo F (2004) Flow cytometric isolation of endodermal progenitors from mouse salivary gland differentiate into hepatic and pancreatic lineages. Hepatology 39:667–675
Ahn JS, Camden JM, Schrader AM, Redman RS, Turner JT (2000) Reversible regulation of P2Y2 nucleotide receptor expression in the duct-ligated rat submandibular gland. Am J Physiol Cell Physiol 279:C286–C294
Takahashi S, Shinzato K, Nakamura S, Domon T, Yamamoto T, Wakita M (2004) Cell death and cell proliferation in the regeneration of atrophied rat submandibular glands after duct ligation. J Oral Pathol Med 33:23–29
Denny PC, Chai Y, Klauser DK, Denny PA (1993) Parenchymal cell proliferation and mechanisms for maintenance of granular duct and acinar cell populations in adult male mouse submandibular gland. Anat Rec 235:475–485
Terazono K, Yamamoto H, Takasawa S, Shiga K, Yonemura Y, Tochino Y, Okamoto H (1988) A novel gene activated in regenerating islets. J Biol Chem 263:2111–2114
Okamoto H, Takasawa S (2002) Recent advances in the Okamoto model: the CD38-cyclic ADP-ribose signal system and the regenerating gene protein (Reg)-Reg receptor system in β-cells. Diabetes 51:S462–S473
Takasawa S (2016) Regenerating gene (REG) product and its potential clinical usage. Expert Opin Ther Targets 20:541–550
Zhang YW, Ding LS, Lai MD (2003) Reg gene family and human diseases. World J Gastroenterol 9:2635–2641
Kazumori H, Ishihara S, Hoshino E, Kawashima K, Moriyama N, Suetsugu H, Sato H, Adachi K, Fukuda R, Watanabe M, Takasawa S, Okamoto H, Fukui H, Chiba T, Kinoshita Y (2000) Neutrophil chemoattractant 2β regulates expression of the Reg gene in injured gastric mucosa in rats. Gastroenterology 119:1610–1622
Planas R, Alba A, Carrillo J, Puertas MC, Ampudia R, Pastor X, Okamoto H, Takasawa S, Gurr W, Pujol-Borrell R, Verdaguer J, Vives-Pi M (2006) Reg (regenerating) gene overexpression in islets from non-obese diabetic mice with accelerated diabetes; role of IFNβ. Diabetologia 49:2379–2387
Yoshino N, Ishihara S, Rumi MA, Ortega-Cava CF, Yuki T, Kazumori H, Takasawa S, Okamoto H, Kadowaki Y, Kinoshita Y (2005) Interleukin-8 regulates expression of Reg protein in Helicobacter pylori-infected gastric mucosa. Am J Gastroenterol 100:2157–2166
Lee KS, Kalantzis A, Jackson CB, O’Connor L, Murata-Kamiya N, Hatakeyama M, Judd LM, Giraud AS, Menheniott TR (2012) Helicobacter pylori CagA triggers expression of the bactericidal lectin REG3γ via gastric STAT3 activation. PLoS One 7:e30786
Sekikawa A, Fukui H, Suzuki K, Karibe T, Fujii S, Ichikawa K, Tomita S, Imura J, Shiratori K, Chiba T, Fujimori T (2010) Involvement of the IL-22/REG Iα axis in ulcerative colitis. Lab Invest 90:496–505
Sekikawa A, Fukui H, Fujii S, Nanakin A, Kanda N, Uenoyama Y, Sawabu T, Hisatsune H, Kusaka T, Ueno S, Nakase H, Seno H, Fujimori T, Chiba T (2005) Possible role of REG Iα protein in ulcerative colitis and colitic cancer. Gut 54:1437–1444
Yoshimoto K, Fujimoto T, Itaya-Hironaka A, Miyaoka T, Sakuramoto-Tsuchida S, Yamauchi A, Takeda M, Kasai T, Nakagawara K, Nonomura A, Takasawa S (2013) Involvement of autoimmunity to REG, a regeneration factor, in patients with primary Sjögren’s syndrome. Clin Exp Immunol 174:1–9
Foglia VG (1944) Charcteristicas de la diabetes en la rata. Revista de la Sociedad Argentina de Biologia 20:21–37
Martin JM, Lacy PE (1963) The prediabetic period in partially pancreatectomized rats. Diabetes 12:238–242
Clark A, Bown E, King T, Vanhegan RI, Turner RC (1982) Islet changes induced by hyperglycemia in rats. Effect of insulin or chlorpropamide therapy. Diabetes 31:319–325
Watanabe T, Yonemura Y, Yonekura H, Suzuki Y, Miyashita H, Sugiyama K, Moriizumi S, Unno M, Tanaka O, Kondo H, Bone AJ, Takasawa S, Okamoto H (1994) Pancreatic beta-cell replication and amelioration of surgical diabetes by Reg protein. Proc Natl Acad Sci USA 91:3589–3592
Gross DJ, Weiss L, Reibstein I, van den Brand J, Okamoto H, Clark A, Slavin S (1998) Amelioration of diabetes in nonobese diabetic mice with advanced disease by linomide-induced immunoregulation combined with Reg protein treatment. Endocrinology 139:2369–2374
Shervani NJ, Takasawa S, Uchigata Y, Akiyama T, Nakagawa K, Noguchi N, Takada H, Takahashi I, Yamauchi A, Ikeda T, Iwamoto Y, Nata K, Okamoto H (2004) Autoantibodies to REG, a beta-cell regeneration factor, in diabetic patients. Eur J Clin Invest 34:752–758
Kobayashi S, Akiyama T, Nata K, Abe M, Tajima M, Shervani NJ, Unno M, Matsuno S, Sasaki H, Takasawa S, Okamoto H (2000) Identification of a receptor for Reg (Regenerating gene) protein, a pancreatic beta-cell regeneration factor. J Biol Chem 275:10723–10726
Acquatella-Tran Van Ba I, Marchal S, François F, Silhol M, Lleres C, Michel B, Benyamin Y, Verdier JM, Trousse F, Marcilhac A (2012) Regenerating islet-derived 1α (Reg-1α) protein is new neuronal secreted factor that stimulates neurite outgrowth via exostosin Tumor-like 3 (EXTL3) receptor. J Biol Chem 287:4726–4739
Kazumori H, Ishihara S, Fukuda R, Kinoshita Y (2002) Localization of Reg receptor in rat fundic mucosa. J Lab Clin Med 139:101–108
Kiji T, Dohi Y, Takasawa S, Okamoto H, Nonomura A, Taniguchi S (2005) Activation of regenerating gene Reg in rat and human hearts in response to acute stress. Am J Physiol Heart Circ Physiol 289:H277–H284
Bluth MH, Patel SA, Dieckgraefe BK, Okamoto H, Zenilman ME (2006) Pancreatic regenerating protein (reg I) and reg I receptor mRNA are upregulated in rat pancreas after induction of acute pancreatitis. World J Gastroenterol 12:4511–4516
Levetan CS, Upham LV, Deng S, Laury-Kleintop L, Kery V, Nolan R, Quinlan J, Torres C, El-Hajj RJ (2008) Discovery of a human peptide sequence signaling islet neogenesis. Endocr Panct 14:1075–1083
Hara K, Fukui H, Sun C, Kitayama Y, Eda H, Yamasaki T, Kondo T, Tomita T, Oshima T, Watari J, Fujimori T, Miwa H (2015) Effect of REG Iα protein on angiogenesis in gastric cancer tissues. Oncol Rep 33:2183–2189
Takasawa S, Ikeda T, Akiyama T, Nata K, Nakagawa K, Shervani NJ, Noguchi N, Murakami-Kawaguchi S, Yamauchi A, Takahashi I, Tomioka-Kumagai T, Okamoto H (2006) Cyclin D1 activation through ATF-2 in Reg-induced pancreatic β-cell regeneration. FEBS Lett 580:585–591
Takahashi I, Noguchi N, Nata K, Yamada S, Kaneiwa T, Mizumoto S, Ikeda T, Sugihara K, Asano M, Yoshikawa T, Yamauchi A, Shervani NJ, Uruno A, Kato I, Unno M, Sugahara K, Takasawa S, Okamoto H, Sugawara A (2009) Important role of heparan sulfate in postnatal islet growth and insulin secretion. Biochem Biophys Res Commun 383:113–118
Nata K, Liu Y, Xu L, Ikeda T, Akiyama T, Noguchi N, Kawaguchi S, Yamauchi A, Takahashi I, Shervani NJ, Onogawa T, Takasawa S, Okamoto H (2004) Molecular cloning, expression and chromosomal localization of a novel human REG family gene, REG III. Gene 340:161–170
Asahara M, Mushiake S, Shimada S, Fukui H, Kinoshita Y, Kawanami C, Watanabe T, Tanaka S, Ichikawa A, Uchiyama Y, Narushima Y, Takasawa S, Okamoto H, Tohyama M, Chiba T (1996) Reg gene expression is increased in rat gastric enterochromaffin-like cells following water immersion stress. Gastroenterology 111:45–55
Yamauchi A, Itaya-Hironaka A, Sakuramoto-Tsuchida S, Takeda M, Yoshimoto K, Miyaoka T, Fujimura T, Tsujinaka H, Tsuchida C, Ota H, Takasawa S (2015) Synergistic activations of REG Iα and REG Iβ promoters by IL-6 and glucocorticoids through JAK/STAT pathway in human pancreatic β cells. J Diabetes Res 2015:173058
Hill T, Krougly O, Nikoopour E, Bellemore S, Lee-Chan E, Fouser LA, Hill DJ, Singh B (2013) The involvement of interleukin-22 in the expression of pancreatic beta cell regenerative Reg genes. Cell Regen (Lond) 2:2
Miyaoka Y, Kadowaki Y, Ishihara S, Ose T, Fukuhara H, Kazumori H, Takasawa S, Okamoto H, Chiba T, Kinoshita Y (2004) Transgenic overexpression of Reg protein caused gastric cell proliferation and differentiation along parietal cell and chief cell lineages. Oncogene 23:3572–3579
Yonemura Y, Sakurai S, Yamamoto H, Endou Y, Kawamura T, Bandou E, Elnemr A, Sugiyama K, Sasaki T, Akiyama T, Takasawa S, Okamoto H (2003) REG gene expression is associated with the infiltrating growth of gastric carcinoma. Cancer 98:1394–1400
Dhar DK, Udagawa J, Ishihara S, Otani H, Kinoshita Y, Takasawa S, Okamoto H, Kubota H, Fujii T, Tachibana M, Nagasue N (2004) Expression of regenerating gene I in gastric adenocarcinomas: correlation with tumor differentiation status and patient survival. Cancer 100:1130–1136
Macadam RC, Sarela AI, Farmery SM, Robinson PA, Markham AF, Guillou PJ (2000) Death from early colorectal cancer is predicted by the presence of transcripts of the REG gene family. Br J Cancer 83:188–195
Harada K, Zen Y, Kanemori Y, Chen TC, Chen MF, Yeh TS, Jan YY, Masuda S, Nimura Y, Takasawa S, Okamoto H, Nakanuma Y (2001) Human REG I gene is up-regulated in intrahepatic cholangiocarcinoma and its precursor lesions. Hepatology 33:1036–1042
Hayashi K, Motoyama S, Koyota S, Koizumi Y, Wang J, Takasawa S, Itaya-Hironaka A, Sakuramoto-Tsuchida S, Maruyama K, Saito H, Minamiya Y, Ogawa J, Sugiyama T (2008) REG I enhances chemo- and radiosensitivity in squamous cell esophageal cancer cells. Cancer Sci 99:2491–2495
Hayashi T, Matsubara A, Ohara S, Mita K, Hasegawa Y, Usui T, Arihiro K, Norimura S, Sentani K, Oue N, Yasui W (2009) Immunohistochemical analysis of Reg IV in urogenital organs: Frequent expression of Reg IV in prostate cancer and potential utility as serum tumor marker. Oncol Rep 21:95–100
Masui T, Ota I, Itaya-Hironaka A, Takeda M, Kasai T, Yamauchi A, Sakuramoto-Tsuchida S, Mikami S, Yane K, Takasawa S, Hosoi H (2013) Expression of REG III and prognosis in head and neck cancer. Oncol Rep 30:573–578
Kimura M, Naito H, Tojo T, Itaya-Hironaka A, Dohi Y, Yoshimura M, Nakagawara K, Takasawa S, Taniguchi S (2013) REG Iα gene expression is linked with the poor prognosis of lung adenocarcinoma and squamous cell carcinoma patients via discrete mechanisms. Oncol Rep 30:2625–2631
Vives-Pi M, Takasawa S, Pujol-Autonell I, Planas R, Cabre E, Ojanguren I, Montraveta M, Santos AL, Ruiz-Ortiz E (2013) Biomarkers for diagnosis and monitoring of celiac disease. J Clin Gastroenterol 47:308–313
Kimura T, Fukui H, Sekikawa A, Yamagishi H, Ichikawa K, Tomita S, Fujii S, Imura J, Kawamata H, Chiba T, Imai Y, Fujimori T (2009) Involvement of REG Iα protein in the regeneration of ductal epithelial cells in the minor salivary glands of patients with Sjögren’s syndrome. Clin Exp Immunol 155:16–20
Ikehata F, Satoh J, Nata K, Tohgo A, Nakazawa T, Kato I, Kobayashi S, Akiyama T, Takasawa S, Toyota T, Okamoto H (1998) Autoantibodies against CD38 (ADP-ribosyl cyclase/cyclic ADP-ribose hydrolase) that impair glucose-induced insulin secretion in noninsulin-dependent diabetes patients. J Clin Invest 102:395–401
Kohler PF, Winter ME (1985) A quantitative test for xerostomia. The Saxon test, an oral equivalent of the Schirmer test. Arthritis Rheum 28:1128–1132
Azuma M, Sato M (1994) Morphogenesis of normal human salivary gland cells in vitro. Histol Histopathol 9:781–790
Fujimura T, Fujimoto T, Itaya-Hironaka A, Miyaoka T, Yoshimoto K, Yamauchi A, Sakuramoto-Tsuchida S, Kondo S, Takeda M, Tsujinaka H, Azuma M, Tanaka Y, Takasawa S (2015) Interleukin-6/STAT pathway is responsible for the induction of gene expression of REG Iα, a new auto-antigen in Sjögren’s syndrome patients, in salivary duct epithelial cells. Biochem Biophys Rep 2:69–74
Watanabe T, Yonekura H, Terazono K, Yamamoto H, Okamoto H (1990) Complete nucleotide sequence of human reg gene and its expression in normal and tumoral tissues. The reg protein, pancreatic stone protein, and pancreatic thread protein are one and the same product of the gene. J Biol Chem 265:7432–7439
Zheng C, Baum BJ (2012) Including the p53 ELAV-like protein-binding site in vector cassettes enhances transgene expression in rat submandibular gland. Oral Dis 18:477–484
Hoque AT, Liu X, Kagami H, Swaim WD, Wellner RB, O’Connell BC, Ambudkar IS, Baum BJ (2000) Construction and function of a recombinant adenovirus encoding a human aquaporin 1-green fluorescent protein fusion product. Cancer Gene Ther 7:476–485
Fujimoto T, Yoshimoto K, Fujimura T, Takeda M, Itaya-Hironaka A, Takasawa S (2014) New aspects of mechanism of salivary gland dysfunction in Sjögren’s syndrome. In: Hernandez EM (ed) Sjögren’s syndrome: symptoms, treatment options and potential health complications. Nova Scientific Publishers, Inc., New York, pp 125–158
Van Belle TL, Pagni PP, Liao J, Sachithanantham S, Dave A, Bel Hani A, Manenkova Y, Amirian N, Yang C, Morin B, Zhang H, Campbell IL, von Herrath MG (2014) Beta-cell specific production of IL6 in conjunction with a mainly intracellular but not mainly surface viral protein causes diabetes. J Autoimmun 55:24–32
Zhang C, Zhang X, Chen XH (2014) Inhibition of the interleukin-6 signaling pathway: a strategy to induce immune tolerance. Clin Rev Allergy Immunol 47:163–173
Hulkkonen J, Pertovaara M, Antonen J, Pasternack A, Hurme M (2001) Elevated interleukin-6 plasma levels are regulated by the promoter region polymorphism of the IL6 gene in primary Sjögren’s syndrome and correlate with the clinical manifestations of the disease. Rheumatology (Oxford) 40:656–661
Szodoray P, Alex P, Brun JG, Centola M, Jonsson R (2004) Circulating cytokines in primary Sjögren’s syndrome determined by a multiplex cytokine array system. Scand J Immunol 59:592–599
Hirano T, Ishihara K, Hibi M (2000) Roles of STAT3 in mediating the cell growth, differentiation and survival signals relayed through the IL-6 family of cytokine receptors. Oncogene 19:2548–2556
Bromberg J (2002) Stat proteins and oncogenesis. J Clin Invest 109:1139–1142
Grandis JR, Drenning SD, Zeng Q, Watkins SC, Melhem MF, Endo S, Johnson DE, Huang L, He Y, Kim JD (2000) Constitutive activation of Stat3 signaling abrogates apoptosis in squamous cell carcinogenesis in vivo. Proc Natl Acad Sci USA 97:4227–4232
Song JI, Grandis JR (2000) STAT signaling in head and neck cancer. Oncogene 19:2489–2495
Rahaman SO, Harbor PC, Chernova O, Barnett GH, Vogelbaum MA, Haque SJ (2002) Inhibition of constitutively active Stat3 suppresses proliferation and induces apoptosis in glioblastoma multiforme cells. Oncogene 21:8404–8413
Ghoreschi K, Laurence A, O’Shea JJ (2009) Janus kinases in immune cell signaling. Immunol Rev 228:273–287
Liu X, Wang J, Wang H, Yin G, Liu Y, Lei X, Xiang M (2015) REG3A accelerates pancreatic cancer cell growth under IL-6-associated inflammatory condition: involvement of a REG3A-JAK2/STAT3 positive feedback loop. Cancer Lett 362:45–60
Sekikawa A, Fukui H, Fujii S, Ichikawa K, Tomita S, Imura J, Chiba T, Fujimori T (2008) REG Iα protein mediates an anti-apoptotic effect of STAT3 signaling in gastric cancer cells. Carcinogenesis 29:76–83
Waugh DJ, Wilson C (2008) The interleukin-8 pathway in cancer. Clin Cancer Res 14:6735–6741
Cuello C, Palladinetti P, Tedla N, Di Girolamo N, Lloyd AR, McCluskey PJ, Wakefield D (1998) Chemokine expression and leucocyte infiltration in Sjögren’s syndrome. Br J Rheumatol 37:779–783
Ota H, Itaya-Hironaka A, Yamauchi A, Sakuramoto-Tsuchida S, Miyaoka T, Fujimura T, Tsujinaka H, Yoshimoto K, Nakagawara K, Tamaki S, Takasawa S, Kimura H (2013) Pancreatic β cell proliferation by intermittent hypoxia via up-regulation of Reg family genes and HGF gene. Life Sci 93:664–672
Unno M, Nata K, Noguchi N, Narushima Y, Akiyama T, Ikeda T, Nakagawa K, Takasawa S, Okamoto H (2002) Production and characterization of Reg knockout mice: reduced proliferation of pancreatic β-cells in Reg knockout mice. Diabetes 51:S478-S483
Reksten TR, Brokstad KA, Jonsson R, Brun JG, Jonsson MV (2011) Implications of long-term medication of oral steroids and antimalarial drugs in primary Sjögren’s syndrome. Int Immunopharmacol 11:2125–2129
Price EJ, Rigby SP, Clancy U, Venables PJ (1998) A double blind placebo controlled trial of azathioprine in the treatment of primary Sjögren’s syndrome. J Rheumatol 25:896–899
Skopouli FN, Jagiello P, Tsifetaki N, Moutsopoulos HM (1996) Methotrexate in primary Sjögren’s syndrome. Clin Exp Rheumatol 14:555–558
Nakayamada S, Saito K, Umehara H, Ogawa N, Sumida T, Ito S, Minota S, Nara H, Kondo H, Okada J, Mimori T, Yoshifuji H, Sano H, Hashimoto N, Sugai S, Tanaka Y (2007) Efficacy and safety of mizoribine for the treatment of Sjögren’s syndrome: a multicenter open-label clinical trial. Mod Rheumatol 17:464–469
Mócsai A, Kovács L, Gergely P (2014) What is the future of targeted therapy in rheumatology: biologics or small molecules. BMC Med 12:43
Cornec D, Jamin C, Pers JO (2014) Sjögren’s syndrome: where do we stand, and where shall we go? J Autoimmun 51:109–14
Meijer JM, Meiners PM, Vissink A, Spijkervet FK, Abdulahad W, Kamminga N, Brouwer E, Kallenberg CG, Bootsma H (2010) Effectiveness of rituximab treatment in primary Sjögren’s syndrome: a randomized, double-blind, placebo-controlled trial. Arthritis Rheum 62:960–968
Carubbi F, Cipriani P, Marreli A, Benedetto P, Ruscitti P, Berardicurti O, Pantano I, Liakouli V, Alvaro S, Alunno A, Manzo A, Ciccia F, Gerli R, Triolo G, Giacomelli R (2013) Efficacy and safety of rituximab treatment in early primary Sjögren’s syndrome: a prospective, multi-center, follow-up study. Arthritis Res Ther 15:R172
Váncsa A, Szabó Z, Szamosi S, Bodnár N, Végh E, Gergely L, Szucs G, Szántó S, Szekanecz Z (2013) Longterm effects of rituximab on B cell counts and autoantibody production in rheumatoid arthritis: use of high-sensitivity flow cytometry for more sensitive assessment of B cell depletion. J Rheumatol 40:565–571
Yamauchi A, Takahashi I, Takasawa S, Nata K, Noguchi N, Ikeda T, Yoshikawa T, Shervani NJ, Suzuki I, Uruno A, Unno M, Okamoto H, Sugawara A (2009) Thiazolidinediones inhibit REG Iα gene transcription in gastrointestinal cancer cells. Biochem Biophys Res Commun 379:743–748
Takasawa S, Kuroki M, Nata K, Noguchi N, Ikeda T, Yamauchi A, Ota H, Itaya-Hironaka A, Sakuramoto-Tsuchida S, Takahashi I, Yoshikawa T, Shimosegawa T, Okamoto H (2010) A novel ryanodine receptor expressed in pancreatic islets by alternative splicing from type 2 ryanodine receptor gene. Biochem Biophys Res Commun 397:140–145
Ota H, Tamaki S, Itaya-Hironaka A, Yamauchi A, Sakuramoto-Tsuchida S, Morioka T, Takasawa S, Kimura H (2012) Attenuation of glucose-induced insulin secretion by intermittent hypoxia via down-regulation of CD38. Life Sci 90:206–211
Nakagawa K, Takasawa S, Nata K, Yamauchi A, Itaya-Hironaka A, Ota H, Yoshimoto K, Sakuramoto-Tsuchida S, Miyaoka T, Takeda M, Unno M, Okamoto H (2013) Prevention of Reg I-induced β-cell apoptosis by IL-6/dexamethasone through activation of HGF gene regulation. Biochim Biophys Acta 1833:2988–2995
Tsujinaka H, Itaya-Hironaka A, Yamauchi A, Sakuramoto-Tsuchida S, Ota H, Takeda M, Fujimura T, Takasawa S, Ogata N (2015) Human retinal pigment epithelial cell proliferation by the combined stimulation of hydroquinone and advanced glycation end-products via up-regulation of VEGF gene. Biochem Biophys Rep 2:123–131
Acknowledgments
The authors are grateful to Dr. Masayuki Azuma from the Tokushima University School of Dentistry for providing NS-SV-DC human salivary ductal cells and Dr. Bruce J. Baum from the National Institute of Dental and Craniofacial Research, NIH for providing A5 rat salivary ductal cells. We are also grateful to Drs. Shinobu Nakamura and Yoshiko Dohi from the Nara Medical University for encouragement. This work was supported in part by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology, Japan, and Japan Science and Technology Agency.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Takanori Fujimura, Takashi Fujimoto, Asako Itaya-Hironaka, Tomoko Miyaoka, Kiyomi Yoshimoto, Sumiyo Sakuramoto-Tsuchida, Akiyo Yamauchi, Maiko Takeda, Hiroki Tsujinaka, Yasuhito Tanaka, and Shin Takasawa declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Fujimura, T., Fujimoto, T., Itaya-Hironaka, A. et al. Significance of Interleukin-6/STAT Pathway for the Gene Expression of REG Iα, a New Autoantigen in Sjögren’s Syndrome Patients, in Salivary Duct Epithelial Cells. Clinic Rev Allerg Immunol 52, 351–363 (2017). https://doi.org/10.1007/s12016-016-8570-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-016-8570-7