Abstract
Interleukin-6 (IL-6) is a proinflammatory cytokine that is multifunctional, with multifaceted effects. IL-6 signaling plays a vital role in the control of the differentiation and activation of T lymphocytes by inducing different pathways. In particular, IL-6 controls the balance between Th17 cells and regulatory T (Treg) cells. An imbalance between Treg and Th17 cells is thought to play a pathological role in various immune-mediated diseases. Deregulated IL-6 production and signaling are associated with immune tolerance. Therefore, methods of inhibiting IL-6 production, receptors, and signaling pathways are strategies that are currently being widely pursued to develop novel therapies that induce immune tolerance. This survey aims to provide an updated account of why IL-6 inhibitors are becoming a vital class of drugs that are potentially useful for inducing immune tolerance as a treatment for autoimmune diseases and transplant rejection. In addition, we discuss the effect of targeting IL-6 in recent experimental and clinical studies on autoimmune diseases and transplant rejection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
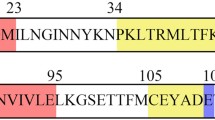
Interleukin-6 (IL-6), a B cell-stimulating factor that drives IgG production, is a phosphorylated glycoprotein with a molecular weight of 26 kDa. The human IL-6 gene is mapped to the 7p15-p21 chromosome, which was first cloned and reported by Hirano et al. in 1986 [1].
IL-6 is a classic proinflammatory cytokine that is pivotal in host immune responses, normal cell inflammatory processes, and the modulation of cellular growth. This cytokine is also regarded as a central mediator in chronic inflammatory human diseases and many autoimmune diseases, including multiple sclerosis, rheumatoid arthritis, and Crohn’s disease (CD) [2]. Furthermore, IL-6 modulates the resistance of T cells to apoptosis, induces the activation of T helper cells and controls the balance between Th17 cells and regulatory T (Treg) cells [3–5]. Therefore, suppression of IL-6 is seen as a rational strategy for the treatment of a wide range of diseases.
This review will focus on the role of IL-6 in immune tolerance, with a particular emphasis on the results of targeting IL-6 in recent experimental and clinical studies on autoimmune diseases and transplant rejection.
Biological Characteristics of IL-6
IL-6 is produced by various types of lymphoid and other cells, such as T and B lymphocytes, fibroblasts, monocytes, endothelial cells, keratinocytes, mesangial cells, and several tumor cells [6]. IL-6 regulates various physiological processes in multiple tissues, including the production of acute-phase proteins such as C-reactive protein, antigen-specific immune responses, host defense mechanisms, inflammation, and hematopoiesis [7]. Additionally, IL-6 acts as a maturing agent for B lymphocytes and stimulates the synthesis and secretion of immunoglobulins [7]. The cytokine also regulates T lymphocyte activation and differentiation [2]. IL-6 belongs to a family of positive growth regulators, which stimulates the proliferation and differentiation of myeloid cells, along with granulocyte-macrophage colony-stimulating factor, granulocyte colony-stimulating factor, interleukin-3 (IL-3) and interleukin-1 [8]. IL-6 also acts synergistically with IL-3 to support the formation of blast cell colonies and induces macrophage and megakaryocyte differentiation [9]. Moreover, IL-6 upregulates the production of vascular endothelial growth factor and is involved in the recruitment of mesenchymal vascular cells and neoangiogenesis [10].
IL-6 Receptors
There are two types of receptors for IL-6. One is the cell-membrane IL-6 receptor (IL-6R), and the other is the soluble IL-6 receptor (sIL-6R). IL-6R only exists on specific cells, such as macrophages, monocytes, hepatocytes, neutrophils, and T and B lymphocytes, under normal conditions [11]. IL-6R forms a low-affinity complex with glycoprotein 130 (gp130, also called CD130) and starts the intracellular signal (classical signaling) that results from binding to IL-6 [12]. sIL-6R is generated by the shedding of membrane-bound IL-6R via limited proteolysis of the ADAM (a disintegrin and metalloproteinase) gene family members ADAM10 and ADAM17 (90 %) and by mRNA alternative splicing (10 %) [13]. sIL-6R binds to IL-6 and then to the membrane receptor β chain-gp130, leading to signal transduction (transsignaling) [12]. sIL-6R mediates IL-6 signal transduction in a variety of cells, such as endothelial cells, neural cells, and smooth muscle cells, that only have gp130 on their surfaces [14].
IL-6 Signaling Pathways
IL-6 transmits its signals through its unique receptor system. IL-6 interacts with a cell-surface type I receptor complex consisting of the signal-transducing component gp130 and a ligand-binding glycoprotein termed IL-6Ra [12]. There are several signaling pathways for IL-6 [15]:
JAK/STAT3
The activation of Janus kinase (JAK) tyrosine kinases leads to the activation of signal transducer and activator of transcription 3 (STAT3) and tyrosine phosphorylation. After phosphorylation, STAT3 forms a dimer that is then translocated to the nucleus to transmit signals from the cell membrane [16]. The IL-6–JAK–STAT3 pathway regulates the expression of several genes, leading to the induction of proliferation and differentiation. The termination and modulation of this signaling pathway are mediated by the suppressors of cytokine signaling feedback inhibitors and protein inhibitors of activated STAT proteins. These suppressors are induced by activated STAT3 in normal cells under normal physiological conditions.
Ras/MAPK
Ras protein is activated in response to IL-6. Ras activation leads to hyperphosphorylation of mitogen-activated protein kinase (MAPK) and an increase in its serine/threonine kinase activity. MAPK then activates transcription factors that mediate diverse effects, including cell growth stimulation, acute-phase protein synthesis, and immunoglobulin synthesis, depending on the cell type [17].
PI3K/Akt
The enzyme phosphatidylinositol-3 kinase (PI3K) modifies certain phosphatidylinositides to phosphorylate phosphatidylinositol-4,5-bisphosphate (PIP2) into phosphatidylinositol-3,4,5-trisphosphate (PIP3). In turn, PIP3 phosphorylates and activates the serine/threonine kinase PkB/Akt, which is recruited to the plasma membrane [18]. Activated Akt phosphorylates several downstream targets to upregulate cellular survival-related signaling pathways [19].
IL-6 and Th17 Cells
The current consensus is that IL-6, together with transforming growth factor-β (TGF-β), induces Th17 differentiation [20, 21]. The combination of TGF-β and IL-6 induces the expression of orphan nuclear receptors (retinoid-related orphan receptor γt (RORγt) and retinoid-related orphan receptor α (RORα)), which are the key transcription factors that trigger the differentiation of the Th17 lineage [22, 23]. STAT3 regulates IL-6-induced expression of RORγt and RORα and interleukin-17 (IL-17) production [24, 25]. Although IL-6 activates both STAT3 and STAT1, it has been demonstrated that STAT3 activation is maintained while STAT1 activation is suppressed in Th17 cells [26].
IL-6 and Treg Cells
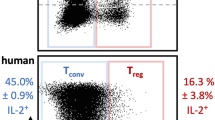
TGF-β is required for Th17 and Treg differentiation and can induce the expression of both Foxp3 and RORγt [27]. However, this induction exclusively leads to Treg differentiation, as Foxp3 can associate with RORγt and inhibit the transcriptional activation of RORγt [27]. In the presence of IL-6, this inhibition is abrogated, and Th17 differentiation is initiated [20, 21]. Thus, IL-6 acts as a potent proinflammatory cytokine by promoting Th17 differentiation and inhibiting Treg differentiation in T cells (Fig. 1). Therefore, control of IL-6 maintains the balance between Th17 and Treg cells and may induce immune tolerance [4].
Th17/Treg and Immune Homeostasis
Th17 cells play a crucial role in triggering inflammation and tissue injury in several autoimmune diseases [28]. Treg cells play a critical role in maintaining immune homeostasis and preventing autoimmune diseases [29, 30]. Therefore, a balance between Th17 and Treg cells is crucial for immune homeostasis [4].
Th17 Cells and Transplant Rejection
Th17 cells are very relevant to transplantation rejection in organ transplantation [31–33]. Rejection was still observed when the signaling pathways of Th1 and Th2 were inhibited in a mouse model of heart transplantation [34]. This rejection was not observed in a mouse model of heart transplantation with a deletion of Th17A [35]. The same results were observed in renal and lung transplantation [36, 37]. Several experimental studies have investigated the contribution of Th17 cells to the development of graft-versus-host disease (GVHD) and have made important observations in various animal models [38–44].
The Th17 differentiation pathway has been shown to play important roles in acute GVHD (aGVHD) [42, 45]. It was shown that the infusion of IL-17-deficient T cells could attenuate chronic GVHD (cGVHD) in the skin and salivary glands in a cGVHD model, which suggests that Th17 cells contribute to cGVHD development [46]. Taken together, these studies suggest that Th17 cells are involved in the development of GVHD and that this effect is mediated both through the direct effects of IL-17 and through indirect effects on the differentiation of other T cell subsets and their local recruitment to GVHD target organs. However, Th17 cells are not necessary for GVHD development, an observation suggesting that Th17 cells interact with other T cell subsets in the pathogenesis of GVHD, including proinflammatory and IFN-γ-releasing Th1 cells and immunosuppressive Treg cells. The importance of Th17 cells relative to the other T cell subsets in the pathogenesis of GVHD seems to differ between various target organs. This organ-dependent variation is likely at least partly caused by local organ-specific variations in the chemokine network and differences in the expression of chemotactic receptors by the various T cell subsets.
The expression of Th17 cells was observed to significantly increase in the phase of acute rejection in patients who had undergone liver transplantation [47]. The expression of Th17 cells significantly increased in patients who had undergone renal transplantation with acute rejection [48]. The expression of Th17 cells was observed in kidney tissues in patients with acute rejection in renal transplantation, although no expression was observed in kidney tissues in patients without rejection [49]. The same result was observed in patients who had undergone lung transplantation [50]. These findings demonstrate an increased Th17 cell population in patients with cGVHD, in addition to an inflammatory process [45, 51, 52]. Th17 cells are associated with cGVHD in patients following hematopoietic stem cell transplantation [53–55]. In one study, the TC and CC genotypes of rs81903036 in the IL-17 gene are associated with an increased risk of aGVHD in patients. Thus, these genetic polymorphisms have an influence on the association with GVHD, suggesting that immunogenetic factors affect Th17 differentiation [56]. A second study described circulating T cells derived from allotransplant recipients with severe treatment-induced cytopenia early after allotransplantation as able to release IL-17, and high levels were observed in patients who later developed aGVHD [57]. This was a small study, so the results should be interpreted with great care; however, the observations support the conclusion of the first study and suggest that IL-17 contributes to the development of aGVHD, at least in acute leukemia patients transplanted with peripheral blood stem cells from family donors and receiving myeloablative conditioning therapy. The number of Th17 cells in a stem cell collection could better predict the risk of aGVHD. A threshold of Th17 cells was not only correlated with cGVHD but was also associated with aGVHD [42, 46, 52, 58–63].
Treg Cells and Immune Tolerance
Treg cells can prevent graft rejection and induce transplantation tolerance [64]. Zheng et al. showed that Treg cells generated ex vivo can act as a vaccine that generates host suppressor cells with the potential to protect MHC-mismatched organ grafts from rejection [65]. In vivo, alloantigen-specific Treg cells have been shown to prevent rejection initiated by CD4+ T cells in both organ and bone marrow transplantation [66, 67]. Treg cells can exert a variety of actions on effector T cells, and especially inhibition of cell proliferation and cytokine and antibody production [68]. For certain donor-recipient combinations, CD8+ T cells have a crucial role in graft destruction during both the initiation and the effector phases of the response. Treg cells can suppress allograft rejection mediated by memory CD8+ T cells [69]. It has been shown that Treg cells play a pivotal role in transplantation tolerance [70]. Hall et al. demonstrated that upon receipt of a cardiac allograft, rats treated with cyclosporine developed graft-specific unresponsiveness and suppression, which was mediated by Treg cells [71]. Several other studies have also implicated Treg cells in the maintenance of transplantation tolerance [72–76]. Removal of Treg cells from normal mice enhanced graft rejection [77]. When Treg cells were inoculated together with naive T cells and transplanted into syngeneic T cell-deficient mice with allografts, graft survival was significantly prolonged [78]. Various treatments fail to induce allograft tolerance in the absence of the Treg subset, and the suppressive effects mediated by tolerant lymphocytes in adoptive transfer systems are neutralized [72, 75, 79]. Several other studies, such as studies using monoclonal antibodies (mAbs) against CD154, CD4, CD8, or intrathymic antigen inoculation, have demonstrated that transplantation tolerance-inducing methods led to the in vivo generation of Treg cells [66, 80–82]. Many types of immunosuppressive drugs, including nonspecific immunosuppressive drugs after transplantation, are used to avoid acute and chronic rejection in the clinic. These drugs usually consist of calcineurin inhibitors (such as cyclosporine, sirolimus, and tacrolimus), mycophenolate mofetil (MMF), and CD25-specific antibodies. These drugs can induce immune tolerance and the development of Treg cells in cases of organ transplantation [83–93].
Targeting IL-6 and Immune Tolerance
Ratajczak et al. demonstrated that the percentage of Th17 cells was not associated with any evidence of severe tissue damage at cGVHD onset [63]. However, in situ quantification of the Th17/Treg ratio showed that a high Th17/Treg ratio was correlated with severe clinical and pathological GVHD, which argued against a pathogenic role for the Th17 subset [94]. It is thus very important to induce immune tolerance to inhibit the production of Th17 cells and to promote the production of Treg cells. IL-6 has a very important role in regulating the balance between Th17 and Treg cells. The two T cell subsets play prominent roles in immune functions: Th17 cells are key players in the pathogenesis of autoimmune diseases, and Treg cells function to restrain excessive effector T cell responses. IL-6, together with TGF-β, induces the development of Th17 cells from Th0 cells, whereas IL-6 inhibits TGF-β-induced Treg differentiation [28, 29]. Thus, IL-6 acts as a potent proinflammatory cytokine toward T cells through the promotion of Th17 differentiation and the inhibition of Treg differentiation. A low Th17/Treg ratio is required in immune tolerance. Thus, targeting IL-6 is very important in immune tolerance (Fig. 2).
IL-6 blockade by anti-IL-6Ab or anti-IL-6RAb may modify a Th17/Treg imbalance. IL-6, together with TGF-β, induces Th17 differentiation from naive T cells, whereas IL-6 inhibits Treg differentiation. A Th17/Treg imbalance is believed to lead to the development of various autoimmune diseases and transplant rejection. Continuous treatment with anti-IL-6Ab or anti-IL-6RAb may repair such an imbalance. RORγ and RORα are master transcriptional regulators for Th17 cells, and Foxp3 is a master transcriptional regulator for Treg cells. Abbreviations: RORγ, retinoic acid receptor γ; RORα, retinoic acid receptor α; Foxp3: Forkhead box p3
Targeting IL-6 in Autoimmune Diseases
Preclinical and translational findings indicate that IL-6 plays an important role in autoimmune disorders, including rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), systemic sclerosis (SSc), polymyositis (PM), Takayasu arteritis (TA), giant cell arteritis (GCA), and Crohn’s disease (CD), and provides a biologic rationale for targeted therapeutic investigations [95–97]. Past success in treating certain diseases with drugs that antagonize IL-6 signaling has provided further support for a pathological role for IL-6. Targeted biological therapies include monoclonal antibodies (mAbs) directed against IL-6 and IL-6R, which are now widely studied for their efficacy in treating autoimmune diseases in which IL-6 has a central role.
IL-6 is one of the key cytokines involved in the development of RA. Seven phase III clinical trials of anti-IL-6RAb demonstrated its efficacy both as a monotherapy and in combination with disease-modifying antirheumatic drugs for adult patients with moderate to severe RA [97–103]. A Cochrane database systematic review concluded that anti-IL-6RAb-treated patients taking concomitant methotrexate compared with placebo were four times more likely to achieve American College of Rheumatology (ACR)-defined 50 % improvement and 11 times more likely to achieve disease activity score remission [104]. Moreover, radiological damage of joints was significantly inhibited by the treatment [97, 103]. As a result, anti-IL-6RAb has now been approved for the treatment of RA in more than 90 countries worldwide. A Japanese study demonstrated the safety and tolerability of anti-IL-6RAb monotherapy in RA patients [105]. A systemic literature review also demonstrated the safety and tolerability of treatment with anti-IL-6RAb at 6 mg kg−1 [106].
IL-6 plays a pathological role in SLE [107–109]. Treatment with anti-IL-6RAb also represents a promising therapy for SLE patients and mice. In murine SLE models, IL-6 blockade with anti-IL-6RAb or anti-IL-6Ab prevents the onset and progression of the disease [110, 111]. An open-label phase I dosage-escalation study showed that the disease activity in 8 of 15 evaluable patients with SLE significantly improved with treatment with different doses of anti-IL-6RAb (2 mg kg−1 for four patients, 4 mg kg−1 for six patients, and 8 mg kg−1 for six patients) [112]. The other clinical studies also showed that IL-6 plays a pathological role in SLE and that treatment with anti-IL-6RAb was effective for SLE patients [113–117].
IL-6 expression is reportedly high in the sera of SSc patients, and its elevation correlates with the skin score [118]. Treatment with anti-IL-6RAb appears to be a promising therapy for SSc patients. The clinical effect of anti-IL-6RAb was examined in two SSc patients who had been resistant to conventional treatment regimens. Both patients showed softening of the skin and thinning of the collagen fiber bundles in the dermis during histological examination [119].
The expression of IL-6 was found in the sera and in infiltrating mononuclear cells in the muscles of PM patients [120, 121]. IL-6 blockade by either gene knockout or anti-IL-6RAb administration showed a preventive or therapeutic effect on myositis in models of experimental myositis induced by myosin or C protein [122, 123]. In the clinic, two PM patients who had been refractory to corticosteroids and immunosuppressive drugs were treated with anti-IL-6RAb. The level of creatine phosphokinase was normal, and high-intensity zones disappeared in the thigh muscles, based on magnetic resonance images [124]. Thus, anti-IL-6RAb may also be effective as a novel drug for refractory PM.
IL-6 is clearly involved in the development of TA and GCA [125, 126]. Clinical manifestations and abnormal laboratory findings were improved after treatment with anti-IL-6RAb for a woman with refractory active TA [127]. Rapid remission was observed in five patients with GCA and two patients with TA when they received treatment with anti-IL-6RAb [128]. IL-6 has also been demonstrated to play a significant role in CD development [129]. In a colitis mouse model, anti-IL-6RAb prevented the occurrence of signs and symptoms of colitis [130]. A pilot randomized trial showed that a high clinical response was achieved for patients with active CD who received treatment with anti-IL-6RAb [131]. Anti-IL-6RAb is also efficacious for the treatment of other autoimmune diseases [132–134].
Targeting IL-6 and Transplantation Tolerance
As we report above, Th17 cells and IL-6 contribute to the mechanisms of rejection after transplantation and IL-6 is a vital factor in the imbalance of Th17 and Treg cells [4, 20–27]. IL-17 participates in the process of acute rejection of organ transplantation [51, 135]. Treg cells can induce immune tolerance after transplantation [64–79]. Thus, the investigation of Th17 and Treg cells in GVHD is especially important [136]. Indeed, in several animal models of disease, anti-IL-6R antibodies have been demonstrated to suppress antigen-specific Th17 differentiation and to induce antigen-specific Treg cells [4, 134, 137–139].
Tawara et al. used a series of complementary knockout and antibody blockade strategies to analyze the impact of IL-6 in multiple clinically relevant murine models of GVHD [140]. The results showed that deficiency in IL-6 in donor T cells led to prolongation of survival. Complete inhibition of IL-6 with anti-mouse IL-6R caused a decrease in GVHD and an even greater reduction in GVHD-induced mortality and preserved a sufficient graft-versus-tumor effect. The reduction in GVHD was independent of the direct effects on T cell effector expansion and donor Treg cells. Huu et al. examined the effects of anti-IL-6R mAb on either the prevention or the treatment of murine sclerodermatous cGVHD (Scl-cGVHD) in a murine model [141]. The researchers found that administration of anti-IL-6RAb attenuated the development of severe Scl-cGVHD and fibrosis. Thus, IL-6 blockade may be an effective approach for preventing Scl-cGVHD and treating cGVHD and scleroderma in humans. Noguchi et al. showed that anti-IL-6R treatment can inhibit the pathogenesis of CD4+ T cell-mediated lethal GVHD against minor histocompatibility antigen [142]. Chen et al. reported that inhibition of the IL-6 signaling pathway by antibody-mediated blockade of the IL-6R markedly reduces the pathological damage attributable to GVHD in a murine model [143]. Jagged2-signaling and TLR signals, except the above pathways described, also joined the mechanism of IL-6 for transplantation rejection through upregulation of IL-6; additionally, blocking IL-6 can induce immune tolerance and increase the graft survival [144, 145].
In the clinic, a patient with GVHD presenting with abdominal pain and diarrhea had been refractory to all known treatments, but after tocilizumab was administered at 8 mg/kg every 2 weeks, the symptoms improved in conjunction with histological improvement [146]. A 65-year-old woman who had suffered from acquired hemophilia A derived from cGVHD was successfully treated with anti-IL-6RAb [133]. Drobyski et al. used tocilizumab (an anti-IL-6R mAb) to treat eight patients with refractory aGVHD (n = 6) or cGVHD (n = 2) once every 3–4 weeks [147]. The majority of patients with aGVHD had grade IV organ involvement of the skin or gastrointestinal tract, whereas both patients with cGVHD had long-standing severe skin sclerosis at the time of treatment. Four patients (67 %) with aGVHD had either partial or complete responses that were apparent within the first 56 days of therapy. One patient with cGVHD had a significant response to therapy, whereas the second had stabilization of disease that allowed for a modest reduction in immunosuppressive medication use. These results indicate that tocilizumab has activity in the treatment of steroid-refractory GVHD. However, Roddy et al. reported nine patients who had steroid-refractory GVHD and received tocilizumab therapy [148]. All patients had GI involvement, and six patients had two organs involved. The median aGVHD grade was 3 (range 3–4). Two patients (22 %) had a complete response, and two had mixed responses, with CR in one organ but no response in another. Only one of nine patients survived. Six patients (67 %) died from aGVHD. These clinical results showed that tocilizumab has a degree of activity in the treatment of steroid-refractory aGVHD but may not be significantly better than other available agents. Therefore, certain clinical trials are being performing for the treatment of GVHD with anti-IL-6RAb in patients who have undergone allogeneic HSCT because tocilizumab is FDA-approved for treating RA but not GVHD [149].
Effect of IL-6 and Targeting IL-6 on Memory B Cell Class Switching and Other T Cell Subsets
IL-6 is a pleiotropic cytokine and has broad biologic activities in various components of the immune system [150, 151]. IL-6 was initially identified as B cell stimulatory factor 2, which is important for the development of antibody-producing plasma cells [152].
IL-6 causes polyclonal B cell activation, plasmacytosis, and B cell neoplasia, which constitutes an important link between adaptive and innate immunity by mediating the B cell responses involved in autoimmunity [153]. IL-6 is central for the induction and/or maintenance of plasma cells that produce immunoglobulin subclasses. In IL-6, knockout mice have shown a marked reduction in B cell immune responses, particularly reductions in the levels of IgG1, IgG2a, and IgG3 on immunization with a T cell-dependent antigen [154, 155]. A recent study showed that antibody production is indirectly promoted by B cell helper capabilities of CD4+ T cells through increased IL-21 production with IL-6 stimulation [156]. The role of B cells in the pathogenesis of RA has also become more widely appreciated in the recent years [157]. B cell differentiation and selection in the inflamed synovium, including the formation of ectopic follicular structures, is a key finding in RA [158]. Treatment of the B cell compartment for patients with RA with anti-IL-6RAb showed that anti-IL-6RAb induced a significant reduction in the frequency of peripheral preswitch and postswitch memory B cells, and the number of IgG+ and IgA+ B cells declined and correlated well with reduced serum immunoglobulin levels [159–161].
The immunologic responses for transplantation rejection are mainly regulated by T cell subsets, especially helper T cells [162]. In particular, CD4+ T cells play a central role in transplantation rejection [37, 163–166]. CD4+ T helper cells can be subdivided into Th1, Th2, Th17, and Treg subsets based on the production of signature cytokines on activation. In the case of the Th1/Th2 dichotomy, the characteristic cytokines are the following: IFN-γ (Th1) versus IL-4, IL-5 (Th2), Th1 increased GVHD, and Th2 decreased GVHD [167–169]. IL-6 inhibited Th1 responses and enhanced Th2 responses [130, 170–173].
Conclusion
IL-6 contributes to the mechanisms of autoimmune diseases and transplantation rejection. The balance between Treg and Th17 cells is mediated by IL-6. Inhibition of IL-6 production, receptors, and signaling pathways are strategies to develop novel therapies for inducing immune tolerance. Currently, more attention should be paid to transplantation rejection, especially in GVHD prevention of haploidentical hematopoietic stem cell transplantation for the treatment of anti-IL-6 Ab or anti-IL-6RAb. Therefore, large, well-designed, double-blinded, randomized, and controlled clinical trials should be performed to verify the role of inhibition of the interleukin-6 signaling pathway in transplantation tolerance.
References
Hirano T, Yasukawa K, Harada H et al (1986) Complementary DNA for a novel human interleukin (BSF-2) that induces B lymphocytes to produce immunoglobulin. Nature 324(6092):73–76
Neurath MF, Finotto S (2011) IL-6 signaling in autoimmunity, chronic inflammation and inflammation-associated cancer. Cytokine Growth Factor Rev 22(2):83–89
Heikkila K, Ebrahim S, Lawlor DA (2008) Systematic review of the association between circulating interleukin-6 (IL-6) and cancer. Eur J Cancer 44(7):937–945
Kimura A, Kishimoto T (2010) IL-6: regulator of Treg/Th17 balance. Eur J Immunol 40(7):1830–1835
Toshio T, Atsushi O, Yoshihito S, Masashi N, Atsushi K, Tadamitsu K (2012) Therapeutic implications of tocilizumab, a humanized anti-interleukin-6 receptor antibody, for various immune-mediated diseases: an update review. Curr Rheumatol Rev 8(3):209–226
Naka T, Nishimoto N, Kishimoto T (2002) The paradigm of IL-6: from basic science to medicine. Arthritis Res 4(Suppl 3):S233–S242
Kishimoto T (2006) Interleukin-6: discovery of a pleiotropic cytokine. Arthritis Res Ther 8(Suppl 2):S2
Hassan HT, Drexler HG (1995) Interleukins and colony stimulating factors in human myeloid leukemia cell lines. Leuk Lymphoma 20(1–2):1–15
Heike T, Nakahata T (2002) Ex vivo expansion of hematopoietic stem cells by cytokines. Biochim Biophys Acta 1592(3):313–321
Tartour E, Pere H, Maillere B et al (2011) Angiogenesis and immunity: a bidirectional link potentially relevant for the monitoring of antiangiogenic therapy and the development of novel therapeutic combination with immunotherapy. Cancer Metastasis Rev 30(1):83–95
Smith AJ, Humphries SE (2009) Cytokine and cytokine receptor gene polymorphisms and their functionality. Cytokine Growth Factor Rev 20(1):43–59
Garbers C, Hermanns HM, Schaper F et al (2012) Plasticity and cross-talk of interleukin 6-type cytokines. Cytokine Growth Factor Rev 23(3):85–97
Chalaris A, Garbers C, Rabe B, Rose-John S, Scheller J (2011) The soluble interleukin 6 receptor: generation and role in inflammation and cancer. Eur J Cell Biol 90(6):484–494
Rose-John S, Scheller J, Elson G, Jones SA (2006) Interleukin-6 biology is coordinated by membrane-bound and soluble receptors: role in inflammation and cancer. J Leukoc Biol 80(2):227–236
Ataie-Kachoie P, Pourgholami MH, Morris DL (2013) Inhibition of the IL-6 signaling pathway: a strategy to combat chronic inflammatory diseases and cancer. Cytokine Growth Factor Rev 24(2):163–173
Heinrich PC, Behrmann I, Haan S, Hermanns HM, Muller-Newen G, Schaper F (2003) Principles of interleukin (IL)-6-type cytokine signalling and its regulation. Biochem J 374(Pt. 1):1–20
Nakajima T, Kinoshita S, Sasagawa T et al (1993) Phosphorylation at threonine-235 by a ras-dependent mitogen-activated protein kinase cascade is essential for transcription factor NF-IL6. Proc Natl Acad Sci U S A 90(6):2207–2211
Hennessy BT, Smith DL, Ram PT, Lu Y, Mills GB (2005) Exploiting the PI3K/AKT pathway for cancer drug discovery. Nat Rev Drug Discov 4(12):988–1004
Chien CM, Lin KL, Su JC et al (2010) Naphtho[1,2-b] furan-4,5-dione induces apoptosis of oral squamous cell carcinoma: involvement of EGF receptor/PI3K/Akt signaling pathway. Eur J Pharmacol 636(1–3):52–58
Bettelli E, Carrier Y, Gao W et al (2006) Reciprocal developmental pathways for the generation of pathogenic effector TH17 and regulatory T cells. Nature 441(7090):235–238
Mangan PR, Harrington LE, O’Quinn DB et al (2006) Transforming growth factor-beta induces development of the T(H)17 lineage. Nature 441(7090):231–234
Ivanov II, McKenzie BS, Zhou L et al (2006) The orphan nuclear receptor 6. IL-6 and Tregs RORgt directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell 126(6):1121–1133
Yang XO, Pappu BP, Nurieva R et al (2008) T helper 17 lineage differentiation is programmed by orphan nuclear receptors RORa and RORg. Immunity 28(1):29–39
Diveu C, McGeachy MJ, Boniface K et al (2009) IL-27 blocks RORc expression to inhibit lineage commitment of Th17 cells. J Immunol 182(9):5748–5756
Mathur AN, Chang HC, Zisoulis DG et al (2007) Stat3 and Stat4 direct development of IL-17-secreting Th cells. J Immunol 178(8):4901–4907
Kimura A, Naka T, Kishimoto T (2007) IL-6-dependent and -independent pathways in the development of interleukin 17-producing T helper cells. Proc Natl Acad Sci U S A 104(29):12099–12104
Zhou L, Lopes JE, Chong MM et al (2008) TGF-beta-induced Foxp3 inhibits T(H)17 cell differentiation by antagonizing RORgammat function. Nature 453(192):236–240
Korn T, Bettelli E, Oukka M, Kuchroo VK (2009) IL-17 and Th17 Cells. Annu Rev Immunol 27(1):485–517
Wing K, Sakaguchi S (2010) Regulatory T cells exert checks and balances on self tolerance and autoimmunity. Nat Immunol 11(1):7–13
Sakaguchi S, Ono M, Setoguchi R et al (2006) Foxp3+CD25+CD4+ natural regulatory T cells in dominant self tolerance and autoimmune disease. Immunol Rev 212:8–27
Chadha R, Heidt S, Jones ND, Wood KJ (2011) Th17: contributors to allograft rejection and a barrier to the induction of transplantation tolerance. Transplantation 91(9):939–945
Atalar K, Afzali B, Lord G, Lombardi G (2009) Relative roles of Th1 and Th17 effector cells in allograft rejection. Curr Opin Organ Transplant 14(1):23–29
Hanidziar D, Koulmanda M (2010) Inflammation and the balance of Treg and Th17 cells in transplant rejection and tolerance. Curr Opin Organ Transplant 15(4):411–415
Benghiat FS, Charbonnier LM, Vokaer B, De Wilde V, Le Moine A (2009) Interleukin 17-producing T helper cells in alloimmunity. Transplant Rev 23(1):11–18
Gorbacheva V, Fan R, Li X, Valujskikh A (2010) Interleukin-17 promotes early allograft inflammation. Am J Pathol 177(3):1265–1273
Braun RK, Molitor-Dart M, Wigfield C et al (2009) Transfer of tolerance to collagen type V suppresses T-helper-cell-17 lymphocyte-mediated acute lung transplant rejection. Transplantation 88(12):1341–1348
Faust SM, Lu G, Marini BL et al (2009) Role of T cell TGFbeta signaling and IL-17 in allograft acceptance and fibrosis associated with chronic rejection. J Immunol 183(11):7297–7306
Hill GR, Olver SD, Kuns RD et al (2010) Stem cell mobilization with G-CSF induces type 17 differentiation and promotes scleroderma. Blood 116(5):819–828
Iclozan C, Yu Y, Liu C et al (2010) T helper17 cells are sufficient but not necessary to induce acute graft-versus-host disease. Biol Blood Marrow Transplant 16(2):170–178
Carlson MJ, West ML, Coghill JM, Panoskaltsis-Mortari A, Blazar BR, Serody JS (2009) In vitro-differentiated TH17 cells mediate lethal acute graft-versus-host disease with severe cutaneous and pulmonary pathologic manifestations. Blood 113(6):1365–1374
Chen X, Vodanovic-Jankovic S, Johnson B, Keller M, Komorowski R, Drobyski WR (2007) Absence of regulatory T-cell control of TH1 and TH17 cells is responsible for the autoimmune-mediated pathology in chronic graft-versus-host disease. Blood 110(10):3804–3813
Yi T, Zhao D, Lin CL et al (2008) Absence of donor Th17 leads to augmented Th1 differentiation and exacerbated acute graft-versus-host disease. Blood 112(5):2101–2110
Murphy WJ, Welniak LA, Taub DD et al (1998) Differential effects of the absence of interferon-gamma and IL-4 in acute graft-versus-host disease after allogeneic bone marrow transplantation in mice. J Clin Invest 102(9):1742–1748
Yang YG, Dey BR, Sergio JJ, Pearson DA, Sykes M (1998) Donor-derived interferon gamma is required for inhibition of acute graft-versus-host disease by interleukin 12. J Clin Invest 102(12):2126–2135
Yi T, Chen Y, Wang L et al (2009) Reciprocal differentiation and tissue-specific pathogenesis of Th1, Th2, and Th17 cells in graft-versus host disease. Blood 114(14):3101–3112
Dander E, Balduzzi A, Zappa G et al (2009) Interleukin-17-producing T-helper cells as new potential player mediating graft-versus-host disease in patients undergoing allogeneic stem-cell transplantation. Transplantation 88(11):1261–1272
Nishimori H, Maeda Y, Teshima T et al (2012) Synthetic retinoid Am80 ameliorates chronic graft-versus-host disease by down-regulating Th1 and Th17. Blood 119(1):285–295
Fbrega E, Lopez-Hoyos M, San Segundo D, Casafont F, Benito MJ, Pons-Romero F (2009) Effect of immunosuppressant blood levels on serum concentration of interleukin-17 and-23 in stable liver transplant recipients. Transplant Proc 41(3):1025–1027
Hsieh HG, Loong CC, Lui WY, Chen A, Lin CY (2001) IL-17 expression as a possible predictive parameter for subclinical renal allograft rejection. Transpl Int 14(5):287–298
Loong CC, Hsieh HG, Lui WY, Chen A, Lin CY (2002) Evidence for the early involvement of interleukin 17 in human and experimental renal allograft rejection. J Pathol 197(3):322–332
Vanaudenaerde BM, Dupont LJ, Wuyts WA et al (2006) The role of interleukin interleukin-17 during acute rejection after lung transplantation. Eur Respir J 27(4):779–787
Zhao XY, Xu LL, Lu SY, Huang XJ (2011) IL-17-producing T cells contribute to acute graft-versus-host disease in patients undergoing unmanipulated blood and marrow transplantation. Eur J Immunol 41(2):514–526
Zhao XY, Lv M, Xu LL, Qian X, Huang XJ (2013) Donor Th17 cells and IL-21 may contribute to the development of chronic graft-versus-host disease after allogeneic transplantation. Eur J Immunol 43(3):838–850
Weisdorf D, Zhang MJ, Arora M, Horowitz MM, Rizzo JD, Eapen M (2012) Graft-versus-host disease induced graft-versus-leukemia effect: greater impact on relapse and disease-free survival after reduced intensity conditioning. Biol Blood Marrow Transplant 18(11):1727–1733
Baron F, Labopin M, Niederwieser D et al (2012) Impact of graft-versus-host disease after reduced-intensity conditioning allogeneic stem cell transplantation for acute myeloid leukemia: a report from the acute leukemia working party of the European group for blood and marrow transplantation. Leukemia 26(12):2462–2468
Coghill JM, Sarantopoulos S, Moran TP, Murphy WJ, Blazar BR, Serody JS (2011) Effector CD4+ T cells, the cytokines they generate, and GVHD: something old and something new. Blood 117(12):3268–3276
Carvalho A, Cunha C, Di Ianni M et al (2010) Prognostic significance of genetic variants in the IL-23/Th17 pathway for the outcome of T cell-depleted allogeneic stem cell transplantation. Bone Marrow Transplant 45(11):1645–1652
Liseth K, Sjo M, Paulsen K, Bruserud O, Ersvaer E (2010) Early pre-engraftment, functional, in vitro responsiveness of T lymphocytes in allotransplanted, acute leukemia patients: proliferation and release of a broad profile of cytokines, possibly predictive of graft-versus-host disease. Eur Cytokine Netw 21(1):40–49
Kappel LW, Goldberg GL, King CG et al (2009) IL-17 contributes to CD4-mediated graft-versus-host disease. Blood 113(4):945–952
Yu Y, Wang D, Liu C et al (2011) Prevention of GVHD while sparing GVL effect by targeting Th1 and Th17 transcription factor T-bet and RORγt. Blood 118(18):5011–5020
Teshima T, Maeda Y, Ozaki K (2011) Regulatory T-cells and IL-17-producing cells in graft-versus-host disease. Immunotherapy 3(7):833–852
Broady R, Yu J, Chow V et al (2010) GVHD is associated with the expansion of tissue-localized Th1 and not Th17 cells. Blood 116(25):5748–5751
Ratajczak P, Janin A, Peffault de Latour R et al (2010) Th17/Treg ratio in human graft-versus-host disease. Blood 116(7):1165–1171
Zhang Y, Liu C, Yang XM, Lv Y (2007) Role and mechanisms of CD4+CD25+ regulatory T cells in the induction and maintenance of transplantation tolerance. Transplant Immunol 17(2):120–129
Zheng SG, Meng L, Wang JH et al (2006) Transfer of regulatory T cells generated ex vivo modifies graft rejection through induction of tolerogenic CD4+CD25+ cells in the recipient. Int Immunol 18(2):279–289
Kingsley CI, Karim M, Bushell AR, Wood KJ (2002) CD25+CD4+ regulatory T cells prevent graft rejection: CTLA-4- and IL-10-dependent immunoregulation of alloresponses. J Immunol 168(3):1080–1086
Hoffmann P, Ermann J, Edinger M, Fathman CG, Strober S (2002) Donor-type CD4(+)CD25(+) regulatory T cells suppress lethal acute graft-versus-host disease after allogeneic bone marrow transplantation. J Exp Med 196(3):389–399
Sakaguchi S (2004) Naturally arising CD4+ regulatory T cells for immunologic self-tolerance and negative control of immune responses. Annu Rev Immunol 22(4):531–562
Dai Z, Li Q, Wang Y et al (2004) CD4+CD25+ regulatory T cells suppress allograft rejection mediated by memory CD8+ T cells via a CD30-dependent mechanism. J Clin Invest 113(2):310–317
Trenado A, Charlotte F, Fisson S et al (2003) Recipient-type specific CD4+CD25+ regulatory T cells favor immune reconstitution and control graft-versus-host disease while maintaining graft-versus-leukemia. J Clin Invest 112(11):1688–1696
Hall BM, Pearce NW, Gurley KE, Dorsch SE (1990) Specific unresponsiveness in rats with prolonged cardiac allograft survival after treatment with cyclosporine. III. Further characterization of the CD4+ suppressor cell and its mechanisms of action. J Exp Med 171(1):141–157
Hara M, Kingsley CI, Niimi M et al (2001) IL-10 is required for regulatory T cells to mediate tolerance to alloantigens in vivo. J Immunol 166(6):3789–3796
Taylor PA, Noelle RJ, Blazar BR (2001) CD4(+)CD25(+) immune regulatory cells are required for induction of tolerance to alloantigen via costimulatory blockade. J Exp Med 193(11):1311–1318
Gregori S, Casorati M, Amuchastegui S, Smiroldo S, Davalli AM, Adorini L (2001) Regulatory T cells induced by 1 alpha, 25-dihydroxyvitamin D3 and mycophenolate mofetil treatment mediate transplantation tolerance. J Immunol 167(4):1945–1953
Sanchez-Fueyo A, Weber M, Domenig C, Strom TB, Zheng XX (2002) Tracking the immunoregulatory mechanisms active during allograft tolerance. J Immunol 168(5):2274–2281
Graca L, Cobbold SP, Waldmann H (2002) Identification of regulatory T cells in tolerated allografts. J Exp Med 195(12):1641–1646
Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M (1995) Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol 155(3):1151–1164
Sakaguchi S, Sakaguchi N, Shimizu J et al (2001) Immunologic tolerance maintained by CD25+CD4+ regulatory T cells: their common role in controlling autoimmunity, tumor immunity, and transplantation tolerance. Immunol Rev 182(1):18–32
Zheng XX, Sanchez-Fueyo A, Sho M, Domenig C, Sayegh MH, Strom TB (2003) Favorably tipping the balance between cytopathic and regulatory T cells to create transplantation tolerance. Immunity 19(4):503–514
van Maurik A, Herber M, Wood KJ, Jones ND (2002) Cutting edge: CD4+CD25+ alloantigen-specific immunoregulatory cells that can prevent CD8+ T cell mediated graft rejection: implications for anti-CD154 immunotherapy. J Immunol 169(10):5401–5404
Trani J, Moore DJ, Jarrett BP et al (2003) CD25+ immunoregulatory CD4 T cells mediate acquired central transplantation tolerance. J Immunol 170(1):279–286
Graca L, Thompson S, Lin CY, Adams E, Cobbold SP, Waldmann H (2002) Both CD4(+)CD25(+) and CD4(+)CD25(−) regulatory cells mediate dominant transplantation tolerance. J Immunol 168(11):5558–5565
Demirkiran A, Kok A, Kwekkeboom J et al (2006) Low circulating regulatory T-cell levels after acute rejection in liver transplantation. Liver Transplant 12(2):277–284
Thornton AM (2006) Signal transduction in CD4+CD25+ regulatory T cells: CD25 and IL-2. Front Biosci 11:921–927
Zorn E, Nelson EA, Mohseni M et al (2006) IL-2 regulates FOXP3 expression in human CD4+CD25+ regulatory T cells through a STAT dependent mechanism and induces the expansion of these cells in vivo. Blood 108(5):1571–1579
Larsen CP, Elwood ET, Alexander DZ et al (1996) Long-term acceptance of skin and cardiac allografts after blocking CD40 and CD28 pathways. Nature 381(6581):434–438
Takatsuki M, Uemoto S, Inomata Y et al (2001) Weaning of immunosuppression in living donor liver transplant recipients. Transplantation 72(3):449–454
Shoji T, Muniappan A, Guenther DA et al (2005) Long-term acceptance of porcine pulmonary allografts without chronic rejection. Transplant Proc 37(1):72–74
Han CH, Li HF, Wang YX et al (2005) The influence of mycophenolate mofetil upon the maturation and allostimulatory activity of cultured dendritic cell progenitors and the effects of tolerance induction in allograft recipients. Zhonghua YiXue ZaZhi 85(19):1327–1332
Huang WH, Yan Y, Li J, De Boer B, House AK, Bishop GA (2003) A short course of mycophenolate immunosuppression inhibits rejection, but not tolerance, of rat liver allografts in association with inhibition of interleukin-4 and alloantibody responses. Transplantation 76(8):1159–1165
Kish DD, Gorbachev AV, Fairchild RL (2005) CD8+ T cells produce IL-2, which is required for CD4+CD25+ T cell regulation of effector CD8+ T cell development for contact hypersensitivity responses. J Leukoc Biol 78(3):725–735
Jones TR, Ha J, Williams MA et al (2002) The role of the IL-2 pathway in costimulation blockade-resistant rejection of allografts. J Immunol 168(3):1123–1130
Blaha P, Bigenzahn S, Koporc Z et al (2003) The influence of immunosuppressive drugs on tolerance induction through bone marrow transplantation with costimulation blockade. Blood 101(7):2886–2893
Malard F, Bossard C, Brissot E (2014) Increased Th17/Treg ratio in chronic liver GVHD. Bone Marrow Transplant. doi:10.1038/bmt.2013.215
Tanaka T, Narazaki M, Kishimoto T (2011) Anti-interleukin-6 receptor antibody, tocilizumab, for the treatment of autoimmune diseases. FEBS Lett 585(23):3699–3709
Tanaka T, Narazaki M, Kishimoto T (2012) Therapeutic targeting of the interleukin-6 receptor. Annu Rev Pharmacol Toxicol 52:199–219
Nishimoto N, Hashimoto J, Miyasaka N et al (2007) Study of active controlled monotherapy used for rheumatoid arthritis, an IL-6 inhibitor (SAMURAI): evidence of clinical and radiographic benefit from an x-ray reader-blinded randomized controlled trial of tocilizumab. Ann Rheum Dis 66(9):1162–1167
Genovese MC, McKay JD, Nasonov EL et al (2008) Interleukin-6 receptor inhibition with tocilizumab reduces disease activity in rheumatoid arthritis with inadequate response to disease-modifying antirheumatic drugs: the tocilizumab in combination with traditional disease modifying antirheumatic drug therapy study. Arthritis Rheum 58(10):2968–2980
Emery P, Keystone E, Tony HP et al (2008) IL-6 receptor inhibition with tocilizumab improves treatment outcomes in patients with rheumatoid arthritis refractory to antitumor necrosis factor biologicals: results from a 24-week multicentre randomized placebo controlled trial. Ann Rheum Dis 67(11):1516–1523
Smolen JS, Beaulieu A, Rubbert-Roth A et al (2008) Effect of interleukin-6 receptor inhibition with tocilizumab in patients with rheumatoid arthritis (OPTION study): a double blind, placebo-controlled, randomized trial. Lancet 371(9617):987–997
Nishimoto N, Miyasaka N, Yamamoto K et al (2009) Study of active controlled tocilizumab monotherapy for rheumatoid arthritis patients with an inadequate response to methotrexate (SATORI): significant reduction in disease activity and serum vascular endothelial growth factor by IL-6 receptor inhibition therapy. Mod Rheumatol 19(1):12–19
Jones G, Sebba A, Gu J et al (2010) Comparison of tocilizumab monotherapy versus methotrexate monotherapy in patients with moderate to severe rheumatoid arthritis: the AMBITION study. Ann Rheum Dis 69(1):88–96
Kremer JM, Blanco R, Brzosko M et al (2011) Tocilizumab inhibits structural joint damage in rheumatoid arthritis patients with inadequate responses to methotrexate: results from the double-blind treatment phase of a randomized placebo-controlled trial of tocilizumab safety and prevention of structural joint damage at one year. Arthritis Rheum 63(3):609–621
Singh JA, Beg S, Lopez-Olivo MA (2010) Tocilizumab for rheumatoid arthritis. Cochrane Database Syst Rev 7(7):CD008331
Nishimoto N, Ito K, Takagi N (2010) Safety and efficacy profiles of tocilizumabmonotherapy in Japanese patients with rheumatoid arthritis: meta-analysis of six initial trials and five long-term extensions. Mod Rheumatol 20(3):222–232
Campbell L, Chen C, Bhagat SS, Parker RA, Ostor AJ (2011) Risk of adverse events including serious infections in rheumatoid arthritis patients treated with tocilizumab: a systemic literature review and meta-analysis of randomized controlled trials. Rheumatology 50(3):552–562
Linker-Israeli M, Deans RJ, Wallace DJ, Prehn J, Ozeri-Chen T, Klinenberg JR (1991) Elevated levels of endogenous IL-6 in systemic lupus erythematosus: a putative role in pathogenesis. J Immunol 147(1):117–123
Iwano M, Dohi K, Hirata E et al (1993) Urinary levels of IL-6 in patients with active lupus nephritis. Clin Nephrol 40(1):16–21
Hirohata S, Miyamoto T (1990) Elevated levels of interleukin-6 in cerebrospinal fluid from patients with systemic lupus erythematosus and central nervous system involvement. Arthritis Rheum 33(5):644–649
Mihara M, Takagi N, Takeda Y, Ohsugi Y (1998) IL-6 receptor blockage inhibits the onset of autoimmune kidney disease in NZB/WF1 mice. Clin Exp Immunol 112(5):397–402
Liang B, Gardner DB, Griswold DE, Bugelski PJ, Song XY (2008) Anti-interleukin-6 monoclonal antibody inhibits autoimmune responses in a murine model of systemic lupus erythematosus. Immunology 119(3):296–305
Illei GG, Shirota Y, Yarboro CH et al (2010) Tocilizumab in systemic lupus erythematosus: data on safety, preliminary efficacy, and impact on circulating plasma cells from an open label phase I dosage-escalation study. Arthritis Rheum 62(2):542–552
Ball EM, Gibson DS, Bell AL, Rooney MR (2014) Plasma IL-6 levels correlate with clinical and ultrasound measures of arthritis in patients with systemic lupus erythematosus. Lupus 23(1):46–56
Eilertsen GØ, Nikolaisen C, Becker-Merok A, Nossent JC (2011) Interleukin-6 promotes arthritis and joint deformation in patients with systemic lupus erythematosus. Lupus 20(6):607–613
Maeshima K, Ishii K, Torigoe M et al (2012) Successful tocilizumab and tacrolimus treatment in a patient with rheumatoid arthritis complicated by systemic lupus erythematosus. Lupus 21(9):1003–1006
Makol A, Gibson LE, Michet CJ (2012) Successful use of interleukin-6 antagonist tocilizumab in a patient with refractory cutaneous lupus and urticarial vasculitis. J Clin Rheumatol 18(2):92–95
Kamata Y, Minota S (2012) Successful treatment of massive intractable pericardial effusion in a patient with systemic lupus erythematosus with tocilizumab. BMJ Case Rep 2012
Hasegawa M, Sato S, Fujimoto M, Ihn H, Kikuchi K, Takehara K (1998) Serum levels of interleukin 6 (IL-6), oncostatin M, soluble IL-6 receptor, and soluble gp130 in patients with systemic sclerosis. J Rheumatol 25(2):308–313
Shima Y, Kuwahara Y, Murota H et al (2010) The skin of patients with systemic sclerosis softened during the treatment with anti-IL-6 receptor antibody tocilizumab. Rheumatology 49(12):2408–2412
Lundberg I, Ulfgren AK, Nyberg P, Andersson U, Klareskog L (1997) Cytokine production in muscle tissue of patients with idiopathic inflammatory myopathies. Arthritis Rheum 40(5):865–874
Lepidi H, Frances V, Figarella-Branger D, Bartoli C, Machado-Baeta A, Pellissier JF (1998) Local expression of cytokines in idiopathic inflammatory myopathies. Neuropathol Appl Neurobiol 24(1):73–79
Scuderi F, Mannella F, Marino M, Provenzano C, Bartoccioni E (2006) IL-6-deficient mice show impaired inflammatory response in a model of myosin-induced experimental myositis. J Neuroimmunol 176(1–2):9–15
Okiyama N, Sugihara T, Iwakura Y, Yokozeki H, Miyasaka N, Kohsaka H (2009) Therapeutic effects of interleukin-6 blockade in a murine model of polymyositis that does not require interleukin-17A. Arthritis Rheum 60(8):2505–2512
Narazaki M, Hagihara K, Shima Y, Ogata A, Kishimoto T, Tanaka T (2011) Therapeutic effect of tocilizumab on two patients with polymyositis. Rheumatology 50(7):1344–1346
Salvarani C, Cantini F, Hunder GG (2008) Polymyalgia rheumatica and giant-cell arteritis. Lancet 372(9634):234–245
Noris M, Daina E, Gamba S, Bonazzola S, Remuzzi G (1999) Interleukin-6 and RANTES in Takayasu arteritis: a guide for therapeutic decisions? Circulation 100(1):55–60
Nishimoto N, Nakahara H, Yoshio-Hoshino N, Mima T (2008) Successful treatment of a patient with Takayasu arteritis using a humanized anti-interleukin-6 receptor antibody. Arthritis Rheum 58(4):1197–1200
Seitz M, Reichenbach S, Bonel HM, Adler S, Wermelinger F, Villiger PM (2011) Rapid induction of remission in large vessel vasculitis by IL-6 blockade. A case series. Swiss Med Wkly 141:w13156
Ito H (2004) Novel therapy for Crohn’s disease targeting IL-6 signaling. Expert Opin Ther Targets 8(4):287–294
Yamamoto M, Yoshizaki K, Kishimoto T, Ito H (2000) IL-6 is required for the development of Th1 cell-mediated murine colitis. J Immunol 164(9):4878–4882
Ito H, Takazoe M, Fukuda Y et al (2004) A pilot randomized trial of a human anti-interleukin-6 receptor monoclonal antibody in active Crohn’s disease. Gastroenterology 126(4):989–996
Kawai M, Hagihara K, Hirano T et al (2009) Sustained response to tocilizumab, anti-interleukin-6 receptor antibody, in two patients with refractory relapsing polychondritis. Rheumatology 48(3):318–319
Nishida S, Kawasaki T, Kashiwagi H et al (2011) Successful treatment of acquired hemophilia A, complicated by chronic GVHD, with tocilizumab. Mod Rheumatol 21(4):420–422
Serada S, Fujimoto M, Mihara M et al (2008) IL-6 blockade inhibits the induction of myelin antigen-specific Th17 cells and Th1 cells in experimental autoimmune encephalomyelitis. Proc Natl Acad Sci U S A 105(26):9041–9046
Yao Z, Painter SL, Fanslow WC et al (1995) Cutting edge: human IL-17: a novel cytokine derived from T-cells. J Immunol 155(12):5483–5486
Normanton M, Marti LC (2013) Current data on IL-17 and Th17 cells and implications for graft versus host disease. Einstein (Sao Paulo) 11(2):237–246
Kishimoto T (2010) IL-6: from its discovery to clinical applications. Int Immunol 22(5):347–352
Hohki S, Ohguro N, Haruta H et al (2010) Blockade of interleukin-6 signaling suppresses experimental autoimmune uveoretinitis by the inhibition of inflammatory Th17 responses. Exp Eye Res 91(2):162–170
Fujimoto M, Serada S, Mihara M et al (2008) Interleukin-6 blockade suppresses autoimmune arthritis in mice by the inhibition of inflammatory Th17 responses. Arthritis Rheum 58(12):3710–3719
Tawara I, Koyama M, Liu C et al (2011) Interleukin-6 modulates graft-versus-host responses after experimental allogeneic bone marrow transplantation. Clin Cancer Res 17(1):77–88
Huu DL, Matsushita T, Jin G et al (2012) IL-6 blockade attenuates the development of murine sclerodermatous chronic graft-versus-host disease. J Invest Dermatol 132(12):2752–2761
Noguchi D, Wakita D, Ohkuri T et al (2011) Blockade of IL-6-signaling inhibits the pathogenesis of CD4+ T cell-mediated lethal graft-versus-host reaction against minor histocompatibility antigen. Immunol Lett 136(2):146–155
Chen X, Das R, Komorowski R et al (2009) Blockade of interleukin-6 signaling augments regulatory T-cell reconstitution and attenuates the severity of graft-versus-host disease. Blood 114(4):891–900
Chen L, Ahmed E, Wang T et al (2009) TLR signals promote IL-6/IL-17-dependent transplant rejection. J Immunol 182(10):6217–6225
Riella LV, Yang J, Chock S et al (2013) Jagged2-signaling promotes IL-6-dependent transplant rejection. Eur J Immunol 43(6):1449–1458
Gergis U, Arnason J, Yantiss R et al (2010) Effectiveness and safety of tocilizumab, an anti-interleukin-6 receptor monoclonal antibody, in a patient with refractory GI graft-versus-host disease. J Clin Oncol 28(30):602–604
Drobyski WR, Pasquini M, Kovatovic K et al (2011) Tocilizumab for the treatment of steroid refractory graft-versus-host disease. Biol Blood Marrow Transplant 17(12):1855–1877
Roddy JVF, Haverkos BM, McBride A, et al (2013) Tocilizumab in the treatment of steroid refractory graft versus host disease: a single institutional experience. 2013; ASH (abstract): 2067
Tanaka T, Kishimoto T (2012) Targeting interleukin-6: all the way to treat autoimmune and inflammatory diseases. Int J Biol Sci 8(9):1227–1236
Fonseca JE, Santos MJ, Canhao H, Choy E (2009) Interleukin-6 as a key player in systemic inflammation and joint destruction. Autoimmun Rev 8(7):538–542
Lipsky PE (2006) Interleukin-6 and rheumatic diseases. Arthritis Res Ther 8(Suppl 2):S4
Muraguchi A, Hirano T, Tang B (1998) The essential role of B cell stimulatory factor 2 (BSF-2/IL-6) for the terminal differentiation of B cells. J Exp Med 167(2):332–344
Jones SA (2005) Directing transition from innate to acquired immunity: defining a role for IL-6. J Immunol 175(6):3463–34638
Wu Y, El Shikh ME, El Sayed RM, Best AM, Szakal AK, Tew JG (2009) IL-6 produced by immune complex-activated follicular dendritic cells promotes germinal center reactions, IgG responses and somatic hypermutation. Int Immunol 21(6):745–756
Kopf M, Herren S, Wiles MV, Pepys MB, Kosco-Vilbois MH (1998) Interleukin 6 influences germinal center development and antibody production via a contribution of C3 complement component. J Exp Med 188(10):1895–1906
Dienz O, Eaton SM, Bond JP et al (2009) The induction of antibody production by IL-6 is indirectly mediated by IL-21 produced by CD4+ T cells. J Exp Med 206(1):69–78
Silverman GJ, Carson DA (2003) Roles of B cells in rheumatoid arthritis. Arthritis Res Ther 5(Suppl 4):S1–S6
Silverman GJ, Boyle DL (2008) Understanding the mechanistic basis in rheumatoid arthritis for clinical response to anti-CD20 therapy: the B-cell roadblock hypothesis. Immunol Rev 223(1):175–185
Roll P, Muhammad K, Schumann M (2011) In vivo effects of the anti-interleukin-6 receptor inhibitor tocilizumab on the B cell compartment. Arthritis Rheum 63(5):1255–1264
Snir A, Kessel A, Haj T, Rosner I, Slobodin G, Toubi E (2011) Anti-IL-6 receptor antibody (tocilizumab): a B cell targeting therapy. Clin Exp Rheumatol 29(4):697–700
Muhammad K, Roll P, Seibold T (2011) Impact of IL-6 receptor inhibition on human memory B cells in vivo: impaired somatic hypermutation in preswitch memory B cells and modulation of mutational targeting in memory B cells. Ann Rheum Dis 70(8):1507–1510
Nakagiri T, Inoue M, Minami M, Shintani Y, Okumura M (2012) Immunology mini-review: the basics of Th17 and interleukin-6 in transplantation. Transplant Proc 44(4):1035–1040
Bishop DK, Shelby J, Eichwald EJ (1992) Mobilization of T lymphocytes following cardiac transplantation: evidence that CD4-positive cells are required for cytotoxic T lymphocyte activation, inflammatory endothelial development, graft infiltration, and acute allograft rejection. Transplantation 53(4):849–857
Shizuru JA, Seydel KB, Flavin TF (1990) Induction of donor-specific unresponsiveness to cardiac allografts in rats by pretransplant anti-CD4 monoclonal antibody therapy. Transplantation 50(3):366–373
Krieger NR, Yin DP, Fathman CG (1996) CD4+ but not CD8+ cells are essential for allorejection. J Exp Med 184(5):2013–2018
Booth AJ, Grabauskiene S, Wood SC, Lu G, Burrell BE, Bishop DK (2011) IL-6 promotes cardiac graft rejection mediated by CD4+ Cells. J Immunol 187(11):5764–5771
Zhang C, Chen XH, Zhang X et al (2011) Human umbilical cord blood-derived stromal cells, a new resource in the suppression of acute graft-versus-host disease in haploidentical stem cell transplantation in sublethally irradiated mice. J Biol Chem 286(15):13723–13732
Black SM, Schott ME, Batdorf BH (2010) IL-4 induces protection of vascular endothelial cells against killing by complement and mellitin through lipid biosynthesis. Eur J Immunol 40(3):803–812
Bishop DK, Chan Wood S, Eichwald EJ, Orosz CG (2001) Immunobiology of allograft rejection in the absence of IFN-γ: CD8+ effector cells develop independently of CD4+ cells and CD40-CD40 ligand interactions. J Immunol 166(5):3248–3255
Dodge IL, Carr MW, Cernadas M, Brenner MB (2003) IL-6 production by pulmonary dendritic cells impedes Th1 immune responses. J Immunol 170(9):4457–4464
Diehl S, Anguita J, Hoffmeyer A et al (2000) Inhibition of Th1 differentiation by IL-6 is mediated by SOCS1. Immunity 13(6):805–815
Rinco'n M, Anguita J, Nakamura T, Fikrig E, Flavell RA (1997) Interleukin (IL)-6 directs the differentiation of IL-4-producing CD4+ T cells. J Exp Med 185(3):461–469
Joseph SB, Miner KT, Croft M (1998) Augmentation of naive, Th1 and Th2 effector CD4 responses by IL-6, IL-1 and TNF. Eur J Immunol 28(1):277–289
Acknowledgments
This study was funded by grants from the National Natural Science Foundation (no. 81170529) and the special foundation for the “1130 project” of Xinqiao Hospital of Third Military Medical University.
Conflict of Interest
The authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, C., Zhang, X. & Chen, XH. Inhibition of the Interleukin-6 Signaling Pathway: A Strategy to Induce Immune Tolerance. Clinic Rev Allerg Immunol 47, 163–173 (2014). https://doi.org/10.1007/s12016-014-8413-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12016-014-8413-3