Abstract
Background
Advances in multimodal treatment have improved survival of patients with nonmetastatic osteosarcoma. At the same time, implant design has improved the outcomes of limb salvage with modular endoprostheses. However, little is known about sports activity in long-term survivors with osteosarcoma.
Questions/purposes
We wanted to evaluate (1) sports activity levels in long-term survivors of osteosarcoma about the knee who received a modular tumor endoprosthesis; (2) to determine if activity level changed over time from initial reconstruction or (3) was predicted from sports activity level before diagnosis; and (4) if complications that occurred affected sports or contributed to prosthetic failures.
Methods
Between 1995 and 2005, we treated 120 patients for osteosarcoma about the knee with resection and modular endoprosthetic reconstruction; of those, 25 (21%) have died, six (5%) had an amputation, 39 (32%) did not speak German and so were ineligible, and 14 (12%) were either lost to followup or refused to participate, leaving 27 patients (14 females, 13 males; median age 19 years [range, 12–60 years); average followup 11 ± 4 years) (54% of the living, German-speaking cohort) for this analysis. Tumors were located in the distal femur (n = 16) and the proximal tibia (n = 11). Sports participation as well as the UCLA Activity Score and the modified Weighted Activity Score were assessed retrospectively. Moreover, postoperative complications were evaluated.
Results
Before the diagnosis of osteosarcoma and 1, 3, and 5 years and at the latest followup, respectively, after their reconstructions, 24 (89%), nine (33%), 20 (74%), and 24 patients (89%) were able to perform sports activities. There was a reduction in high-impact activities. Those patients with followup longer than 5 years had no changes in sports activity at their latest followup. Patients who had higher levels of sports activity levels before surgery generally had higher levels of activity at last followup (UCLA Activity Score: r = 0.62, p < 0.0005; modified Weighted Activity Score r = 0.49, p < 0.01). Fourteen patients (51%) underwent revision surgery. With the numbers available, complications had no effect on sports activity. No sports activity-related complications were found.
Conclusions
Some long-term survivors of osteosarcoma can achieve high levels of sports activity. Preoperative activity levels seem to influence the postoperative activity levels. This information is important to give realistic expectations for long-term survivors of osteosarcoma of the knee.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The 5-year oncologic survival rate of young patients with osteosarcoma is approximately 80% for patients presenting with no evidence of metastatic disease [4, 13].
In many instances, the emotional well-being among healthy adolescents is strongly associated with participation in sports activities [13]. Physical activity has become an important part of postcancer treatment as a rehabilitation tool for improving general well-being and increasing physical fitness through a significant reduction of treatment-related symptoms [2]. Especially physical fitness, psychological, and social well-being enable young athletic patients with cancer to regain control and form a strong cancer identity [1]. Moreover, positive expectations regarding the disease are associated with better health outcomes [15].
In previous studies, walking patterns as well as general activity and quality of life were assessed in patients with osteosarcoma [8, 19]; however, no detailed assessment of sports activity levels was performed and no data exist with regard to time course of sports activity levels postsurgery. Physical activity levels after elective joint arthroplasty have been well studied. Those patients however undergo surgery around the sixth decade, and general activity levels are less than would be expected for a young patient with tumor. They also have other comorbidities that may affect the ability to do sports. Furthermore, standard TKA is associated only with minor loss of bone mass and the total preservation of muscle mass [17]. Most of the patients can safely return to low-impact activities [11, 18]. However, there are little data on activity levels after joint reconstruction with modular tumor endoprostheses in patients with sarcoma [19]. To give patients a realistic expectation of what can be achieved years after surgery, it is essential to know what activities can be done and which factors affect sports activity.
Therefore, the purpose of this case series was to evaluate (1) sports activity levels in long-term survivors of osteosarcoma about the knee who received a modular tumor endoprostheses; and (2) to determine if activity level changed over time from initial reconstruction or (3) was predicted from sports activity level before diagnosis; and (4) if complications that occurred affected sports or contributed to prosthetic failures.
Patients and Methods
The study was approved by the local ethic committee and was done in accordance with the Declaration of Helsinki.
Patients
Inclusion criteria for this study were (1) osteosarcoma of the knee and reconstruction with a modular endoprosthesis at followup of 5 to 15 years; (2) age 12 to 65 years at the time of surgery; and (3) German-speaking (Austria, Germany, Switzerland). Data were retrieved from the institution’s Bone and Soft Tissue Tumor Registry and complemented by thorough chart reviews. All tumors in the patients were diagnosed by the local department of pathology.
A total of 120 patients had an osteosarcoma located around the knee, distal femur, or proximal tibia and received endoprosthetic reconstruction with a modular endoprosthesis. In 25 cases, the patients had died and six patients had a subsequent amputation of the affected limb, because of infection, local recurrence, or failure of the prosthesis. From the remaining 89 patients, 50 were German-speaking. We excluded non-German-speaking patients from other countries to avoid language based bias. Forty-one patients fulfilled the criteria to be included in the study. Eight patients were lost to followup. Six patients refused participation in the study. Four of these patients were in good condition, one had neuropathy, and one had to undergo revision surgery because of bushing wear. Overall there were 27 patients (14 females, 13 males) with a mean age at the time of surgery of 25.5 ± 13.5 years and a median of 18.8 years (range, 12.6–60.1 years) (Fig. 1). In 16 cases (nine females, seven males), the tumor was located in the distal femur and in 11 cases (five females, six males) in the proximal tibia. The average followup was 11.2 ± 3.7 years (range, 5.3–15.6 years). In 26 patients, a conventional high-grade osteosarcoma and in one patient a parosteal G2 osteosarcoma in a person who received chemotherapy were included.
Six patients were treated according to the Cooperative Osteosarcoma Study (COSS 86) [22], 17 patients received the modified treatment of the Cooperative Osteosarcoma Study (COSS 96) [3], and two each were treated according to the principles of the European and American Osteosarcoma Study (EURAMOS) [21] and EUROpean Bone Over 40 Sarcoma Study (EURO-BOSS) [4].
Surgical Technique
Tumor resection was carried out according to the principles of Enneking et al. [7]. All patients were treated with cementless modular tumor endoprostheses. Twenty-four patients received a Kotz Modular Femur Tibia Reconstruction System® (KMFTR; Howmedica International, Inc, Kiel, Germany) fixed hinge, a Global Modular Reconstruction System (Stryker Osteonics, Kiel, Germany) rotating hinge, one of them a distal femur, and the other one a proximal tibia. One patient received an extendable KMFTR (Stryker Howmedica Osteonics, Kiel, Germany) with its main component located at the proximal tibia. She received the prosthesis at age 13.5 years. Three years later the system was changed to a standard KMFTR. The patient has a total followup of 15.58 years and therefore was included. In six patients (three distal femurs, two proximal tibias, and one patient with an extraarticular resection of the distal femur and proximal tibia), an augmentation of the insufficient extensor apparatus with the Ligament Augmentation and Reconstruction System (LARS®, Arc sur Tille, France) was used [6]. In five patients, the extensor apparatus was reconstructed with a pedicled gastrocnemius flap.
Outcome Parameters
The sports activity levels and the performed athletic activities before diagnosis of the osteosarcoma as well as postoperatively until the time of the latest followup were assessed retrospectively in the course of an interview designed for this study. One person (NWL) did the interview by telephone contact. The UCLA Activity Score [24] and the modified Weighted Activity Score [16] as well as the type of sports, the frequency per week, and the duration of each training session were assessed retrospectively at the latest followup for the time before diagnosis (-1), the first year after surgery (+1), 3 years after surgery (+3), and 5 years after surgery and the time of followup (+5/latest followup). In addition, we performed a database analysis. We determined impact levels according to Mont et al. [16] who developed a questionnaire for assessing regular participation in sports based on corresponding impact points to the Knee Society recommendations of 1999 [10]: 1 recommended, 2 recommended with experience, and 3 not recommended: low impact (hiking, swimming, golf, bicycling, aerobics, dancing), intermediate impact (skating, tennis, skiing, weightlifting machines), and high impact (soccer, volleyball, jogging, martial arts, hockey, gymnastics, basketball) [16].
Complications
We classified our complications according to a comprehensive failure mode classification of tumor endoprostheses [12]. In addition, we recorded service operations because of bushing wear and polyethylene wear components of the endoprosthesis. Furthermore, we recorded oncological complications such as metastases and local recurrence.
Statistical Analysis
Statistical analysis was performed using GraphPad Prism 5.0 software (San Diego, CA, USA). Repeated-measures analysis of variance (ANOVA) with Bonferroni’s multiple comparison post hoc test was used to assess statistical significance between all investigated scores at pre- and postoperative time points. Repeated-measures two-way ANOVA was used to assess the effects of the presence and absence of complications on all scores at multiple time points. Spearman rank correlation was used to assess the correlation between the various scores at matching time points. A p value < 0.05 was considered statistically significant.
Results
Twenty-four patients (89%) were performing regular athletic activity before diagnosis. The most popular sports were bicycling (59%), swimming (37%), jogging (33%), alpine skiing (30%), soccer (22%), and basketball (19%). Fifteen patients (55%) were participating in high-impact sports. In the first, third, and fifth years postoperatively, nine (33%) 20 (74%), and 24 (89%) patients, respectively, performed sports on a regular basis. At the latest followup, the most common sports were cycling/exercise biking (59%), swimming (33%), alpine skiing/snowboarding (15%), fitness training (fitness center) (26%), hiking/Nordic walking (22%), and walking (> 3 km) (7%) (Table 1). One patient continued with jogging and another one was playing soccer 5 years postsurgery (7.4% participating in high-impact sports).
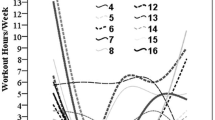
The mean UCLA score showed a 52% (3.52 ± 2.15/7.22 ± 2.26) reduction (p < 0.001) after 1 year postsurgery when compared with preosteosarcoma levels. When compared with 1-year postoperative levels, there was a significant 30% (4.59 ± 2.04/3.52 ± 2.15) (p < 0.05) increase at 3 years postsurgery and 50% (5.30 ± 1.88/4.59 ± 2.04) (p < 0.05) increase 5 years postsurgery and at the latest followup respectively (Fig. 2A). The modified Weighted Activity Score showed an 80% (1.59 ± 3.29/20.44 ± 17.40) reduction (p > 0.001) at 1 year postoperatively when compared with preosteosarcoma levels at 1 year postsurgery. However, no significant postoperative change could be detected in the following years (Fig. 2B). Furthermore, the frequency of the sports performed as well as their duration changed. Cycling and swimming were performed less often in the years after surgery compared with prediagnosis levels. Interestingly, hiking was performed more often after surgery than before the diagnosis and workouts at the gym were longer but at the same rate in the years after surgery. Most patients achieved their maximum activity levels at 5 years postsurgery. Both the patient with the expandable prosthesis and the patient with the replacement of the distal femur and proximal tibia had median sports activity levels. Therefore, there were no statistical outliers.
Patients who were more active before diagnosis were also most active postoperatively (Fig. 3). Increased preoperative sports activity levels and the long-term followup sports activity levels were correlated in the UCLA score (r = 0.62, p < 0.0005) and the modified Weighted Activity Score (r = 0.49, p < 0.01).
Surprisingly, with numbers available we observed no difference with regard to functional outcome and sports activity levels for the UCLA score and the modified Weighted Activity Score between distal femoral and proximal tibia replacement and therefore data were presented as one group.
With the numbers available, there were no differences in age as well as in sports activity levels of patients with prosthesis-related complications (51.9%) and without (Table 2).
The size of the modular tumor endoprosthesis had some influence on sports activity (rs = −0.467, p < 0.014) for the UCLA Activity Score at 5 years postsurgery. The larger the prosthesis, the lower the activity level. No significant correlation for the size of the prosthesis and the modified Weighted Activity Score was found.
Furthermore, no sports-related complications, like injuries of the ankle, ligaments of the contralateral knee, or periprosthetic fracture, were observed. We observed metastases to the lung in one patient, who is 3 years without evidence of disease after hemipneumectomy. Four patients slightly limped and one patient was not performing any sports and used a brace.
In general, low-impact sports were performed by most of the patients. No differences in sports activity levels in patients with fixed hinged or rotating hinge tumor endoprostheses were observed.
Discussion
Osteosarcoma mainly affects adolescents and young adults [9]. Emotional well-being among healthy adolescents is often strongly associated with participation in sports activities [20]. Currently we know little about the ability of long-term survivors returning to sports activity after modular tumor endoprosthesis of the knee. Therefore, the purpose was to evaluate sports activity and to determine if activity level changed over time from initial reconstruction or was predicted from sports activity level before diagnosis and if complications that occurred affected sports or contributed to prosthetic failures. Approximately 89% of our patients were regularly participating in athletic activity before osteosarcoma as well as 5 years postoperatively and at the latest followup. This indicates that sport is a very important part of the life of these young patients. Only few patients were able to perform any sports in the first year postsurgery. Interestingly, sport activity increased at each time period up to 5 years postsurgery.
There are several limitations to this study. We only included German-speaking, healthy long-term survivors, therefore causing selection bias, to avoid language-based bias. We had to exclude patients from abroad who were initially treated at our department, because communication was not possible and because they were lost to followup. As a result of the small size of our study population, sex-specific issues could not be addressed. Likewise, those who chose to participate were those who were more athletically involved at diagnosis. These issues almost certainly represent a high-end estimate of sports participation; patients whose health status was worse than those who participated here almost certainly do not engage in sports to the same degree. Our findings are not representative of the entire tumor population. Furthermore, our results might be different from studies in other countries with other cultural backgrounds and different attitudes toward sports. It is possible that the sport level in German populations differs in type and intensity with those of other nationalities. The age distribution of our patients included older patients, which might not be comparable to the standard age distribution of patients with osteosarcoma in general. Our data were compiled by a recall interview, which may have introduced recall bias regarding sports activities at diagnosis and earlier in the followup periods. The study sample size is too small to give general recommendations with regard to sport activities. We currently recommend only low-impact activities to our patients.
Sheiko et al. [19] reported that children undergoing limb salvage procedures for bone tumors demonstrate significantly less daily activity and lower activity levels than age-matched control subjects. They were the first to publish data on sports activity after prosthetic and allograft reconstruction of the proximal femur, the distal femur, and the proximal tibia in adolescents with osteosarcoma, Ewing’s sarcoma, and other malignancies. The study assessed walking patterns as well as the Activity Scale for Kids. However, it is hard to compare with our results because of the different assessment, the heterogeneity of procedures, location of the tumor, and type of sarcoma.
We observed a decrease in activity levels in the first postoperative year and from then on a steady increase up until first 5 years after surgery. The activity levels reached 5 years or later after surgery were higher than at the other postoperative time periods. A change from high-impact to low-impact athletic activity was observed. Only two patients (7.4%) were able to return to high-impact sports (jogging, soccer) and approximately more than one-third to moderate-impact sports (alpine skiing, fitness training). More than two-thirds were able to return to low-impact sports (biking, swimming, Nordic walking) at the latest followup. These changes over time were also measured using sports activity scores that showed a significant reduction in the first year postsurgery compared with preosteosarcoma levels and a steady increase in activity levels up until 5 years postsurgery when maximum levels were achieved. Winter et al. [23] compared activity levels of survivors of leukemia and bone tumors with a healthy control group by analyzing the number of daily gait cycles. This study demonstrated that activity levels in cancer survivors, especially in patients with bone tumors, are dramatically reduced.
We also found that patients who performed more sports preoperatively tended to exercise more postoperatively as well. Similar to our findings, Chatterji et al. [5] reported that those who did more sports before TKA were more active postoperatively (r = 0.482, p < 0.001). One explanation is that patients performing sports before surgery were more likely to return to sports because they were motivated to participate in athletic activity in the first place. This motivation may have influenced their postoperative rehabilitation to facilitate postoperative success.
We found that complications had no influence on the patients’ sports activity levels with the numbers available. Although a reoperation was definitely a setback with regard to the activity levels, it did not affect the activity levels in the long term. We had a high rate of complications among our patients, which led to a revision of the prosthesis rate in 50% of the patients. Mittermayer et al. [14] reported that 19 of 41 patients (46.3%) treated with a modular tumor endoprosthesis had a second surgery because of major complications within a mean followup of 11.5 years. Furthermore, one patient had metastases. We found that the ability to participate in sports activity in a regular fashion was not affected. The type of complication and the time of occurrence had little influence on the activity level of our patients. Moreover, the level of sports activity had no influence on revision rate and structural failures. None of the patients reported sports-related injuries. Nevertheless, we do not know for sure if patients who do more activities increase the likelihood or at least reduce the time to bushing failure or stem loosening. None of the patients reported sports-related injuries like periprosthetic fracture or injuries of the ankle or ligaments of the contralateral knee.
In summary, we conclude that selected long-term survivors of osteosarcoma can reach high levels of sports activity although the types of activities may change over time. With the numbers available, complications did not result in a sustained decrease in sports activity levels in the long term and patients who did more sports preoperatively tended to do more postoperatively.
References
Adamsen L, Andersen C, Midtgaard J, Moller T, Quist M, Rorth M. Struggling with cancer and treatment: young athletes recapture body control and identity through exercise: qualitative findings from a supervised group exercise program in cancer patients of mixed gender undergoing chemotherapy. Scand J Med Sci Sports. 2009;19:55–66.
Adamsen L, Quist M, Midtgaard J, Andersen C, Moller T, Knutsen L, Tveteras A, Rorth M. The effect of a multidimensional exercise intervention on physical capacity, well-being and quality of life in cancer patients undergoing chemotherapy. Support Care Cancer. 2006;14:116–127.
Bielack S, Kempf-Bielack B, Schwenzer D, Birkfellner T, Delling G, Ewerbeck V, Exner GU, Fuchs N, Gobel U, Graf N, Heise U, Helmke K, von Hochstetter AR, Jurgens H, Maas R, Munchow N, Salzer-Kuntschik M, Treuner J, Veltmann U, Werner M, Winkelmann W, Zoubek A, Kotz RI. [Neoadjuvant therapy for localized osteosarcoma of extremities. Results from the Cooperative osteosarcoma study group COSS of 925 patients] [in German]. Klin Padiatr. 1999;211:260–270.
Carrle D, Bielack SS. Current strategies of chemotherapy in osteosarcoma. Int Orthop. 2006;30:445–451.
Chatterji U, Ashworth MJ, Lewis PL, Dobson PJ. Effect of total knee arthroplasty on recreational and sporting activity. ANZ J Surg. 2005;75:405–408.
Dominkus M, Sabeti M, Toma C, Abdolvahab F, Trieb K, Kotz RI. Reconstructing the extensor apparatus with a new polyester ligament. Clin Orthop Relat Res. 2006;453:328–334.
Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–246.
Frances JM, Morris CD, Arkader A, Nikolic ZG, Healey JH. What is quality of life in children with bone sarcoma? Clin Orthop Relat Res. 2007;459:34–39.
Geller DS, Gorlick R. Osteosarcoma: a review of diagnosis, management, and treatment strategies. Clin Adv Hematol Oncol. 2010;8:705–718.
Healy WL, Iorio R, Lemos MJ. Athletic activity after joint replacement. Am J Sports Med. 2001;29:377–388.
Healy WL, Sharma S, Schwartz B, Iorio R. Athletic activity after total joint arthroplasty. J Bone Joint Surg Am. 2008;90:2245–2252.
Henderson ER, Groundland JS, Pala E, Dennis JA, Wooten R, Cheong D, Windhager R, Kotz RI, Mercuri M, Funovics PT, Hornicek FJ, Temple HT, Ruggieri P, Letson GD. Failure mode classification for tumor endoprostheses: retrospective review of five institutions and a literature review. J Bone Joint Surg Am. 2011;93:418–429.
Luetke A, Meyers PA, Lewis I, Juergens H. Osteosarcoma treatment—where do we stand? A state of the art review. Cancer Treat Rev. 2014;40:523–532.
Mittermayer F, Krepler P, Dominkus M, Schwameis E, Sluga M, Heinzl H, Kotz R. Long-term followup of uncemented tumor endoprostheses for the lower extremity. Clin Orthop Relat Res. 2001;388:167–177.
Mondloch MV, Cole DC, Frank JW. Does how you do depend on how you think you’ll do? A systematic review of the evidence for a relation between patients’ recovery expectations and health outcomes. CMAJ. 2001;165:174–179.
Mont MA, Marker DR, Seyler TM, Gordon N, Hungerford DS, Jones LC. Knee arthroplasties have similar results in high- and low-activity patients. Clin Orthop Relat Res. 2007;460:165–173.
Murray DG. Total knee arthroplasty. Clin Orthop Relat Res. 1985;192:59–68.
Papalia R, Del Buono A, Zampogna B, Maffulli N, Denaro V. Sport activity following joint arthroplasty: a systematic review. Br Med Bull. 2012;101:81–103.
Sheiko M, Bjornson K, Lisle J, Song K, Eary JF, Conrad EU 3rd. Physical activity assessment in adolescents with limb salvage. J Pediatr. 2012;161:1138–1141.
Steptoe A, Butler N. Sports participation and emotional wellbeing in adolescents. Lancet. 1996;347:1789–1792.
Whelan J, Seddon B, Perisoglou M. Management of osteosarcoma. Curr Treat Options Oncol. 2006;7:444–455.
Winkler K, Bielack S, Delling G, Salzer-Kuntschik M, Kotz R, Greenshaw C, Jurgens H, Ritter J, Kusnierz-Glaz C, Erttmann R. Effect of intraarterial versus intravenous cisplatin in addition to systemic doxorubicin, high-dose methotrexate, and ifosfamide on histologic tumor response in osteosarcoma (study COSS-86). Cancer. 1990;66:1703–1710.
Winter C, Muller C, Brandes M, Brinkmann A, Hoffmann C, Hardes J, Gosheger G, Boos J, Rosenbaum D. Level of activity in children undergoing cancer treatment. Pediatr Blood Cancer. 2009;53:438–443.
Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895.
Acknowledgments
We thank Prof M. Dominkus for being in charge of the local tumor registry for many years providing necessary basic information. Furthermore, we thank the former and present secretaries of the tumor registry, Mag. T. Zettl and O. Wallner, respectively.
Author information
Authors and Affiliations
Corresponding author
Additional information
One of the authors certifies that he (RW) may receive payments or benefits of less than USD 10,000, during the study period, from Stryker Osteonics (Kiel, Germany).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research ® editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
About this article
Cite this article
Lang, N.W., Hobusch, G.M., Funovics, P.T. et al. What Sports Activity Levels Are Achieved in Patients With Modular Tumor Endoprostheses of Osteosarcoma About the Knee?. Clin Orthop Relat Res 473, 847–854 (2015). https://doi.org/10.1007/s11999-014-3788-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11999-014-3788-2