Abstract
Purpose
To evaluate sporting activity following osteochondral autologous transfer (OAT) combined with valgus high tibial osteotomy (HTO) in young and active patients with focal osteochondral defects of the medial femoral condyle and concomitant varus malalignment.
Methods
Thirty patients with focal osteochondral defects of the medial femoral condyle and varus malalignment >2° were enrolled. All patients were active in sports on a regular base prior to surgery (lifetime), but were unable to perform sports at the time of surgery. Sporting activity 1 year preoperatively and at final follow-up was compared using a previously published sports questionnaire, which assesses sports level, number of sports disciplines, sports frequency, sports duration and the participation in 32 common sports disciplines. Additionally, the Tegner activity scale and the Activity Rating Scale were used.
Results
After a mean follow-up of 6.9 years (2.5–9.8; SD 2.4), 76.7 % of patients were participating in sports on a regular basis (Fig. 2). Compared to 1 year preoperatively, there was no difference (n.s.) with regard to sports, the number of sports disciplines, sports frequency and sports duration (Fig. 4). The median Tegner activity scale measured preoperatively 5.0 (2.0–7.0) and post-operatively 5.0 (4.0–7.0) points (Fig. 3), and the ARS changed from 5.7 to 5.3 points (n.s.). The different types of sports disciplines were comparable between 1 year preoperatively and at follow-up.
Conclusion
A high return to sports rate and an activity level comparable to the state at 1 year preoperatively can be expected in young and active patients after combined OAT and valgus HTO. This seems to be relevant in clinical practice when planning, indicating and performing these complex procedures.
Level of evidence
IV.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chondral and osteochondral defects in the loading surface of the medial femoral condyle are frequently seen in young and active patients [2, 16, 18]. These lesions significantly impair activities of daily living and sports participation and possibly finally end in symptomatic osteoarthritis [16, 22]. For this reason, several surgical options attempt to restore normal knee joint congruity in order to prevent further joint deterioration [8]. Multiple algorithms have been described for cartilage repair, and good clinical results can be achieved with microfracture, implantation of autologous chondrocytes (ACI) or osteochondral autologous transfer (OAT) [12, 34]. Until today, OAT is the only procedure so far that provides real hyaline cartilage and allows replacing pathologic subchondral bone in focal osteochondral defects in a single-staged procedure [8, 14].
Cartilage restoration procedures may only be successful if concomitant pathologies are identified and simultaneously corrected [15]. In particular, varus malalignment—known as an independent risk factor for osteoarthritis—might lead to consecutive overloading of repaired cartilage defects in the medial tibiofemoral compartment [7, 24]. For this reason, cartilage repair techniques have been successfully combined with unloading valgus high tibial osteotomy (HTO) [3, 4, 25, 36]. These complex procedures have shown high survival rates, with failure being defined as conversion to partial or total knee arthroplasty (TKA) [25, 36]. However, since these patients are generally young and active, surgical treatment should not only attempt to delay TKA but also to improve activities of daily living and ideally restore the ability to participate in sports. Unfortunately, only little knowledge exists about sports participation after cartilage repair combined with unloading osteotomies. However, this information seems to be relevant to discuss the expectable post-operative outcome and to adequately give patients advice. For this reason, the purpose of this study was to evaluate sporting activity after combined OAT and valgus HTO in a young and active patient cohort suffering from symptomatic deep focal osteochondral femoral defects with concomitant varus malalignment since these data are missing until today.
The hypothesis of this study was that this combined procedure enables patients to perform sport at least on a recreational level.
Materials and methods
Data acquisition
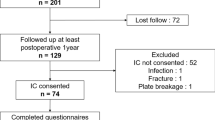
Between 1998 and 2008, OAT of the medial femoral condyle combined with valgus HTO was performed in 135 patients at our institution. All patients suffered from symptomatic focal high-grade osteochondral defects (ICRS grade IV, ICRS OCD grade III/IV [6]) of the medial femoral condyle and showed varus malalignment of more than 2° measured on a full-leg weight-bearing radiograph without radiological signs of osteoarthritis (Kellgren & Lawrence <1) [19]. Eighty-six of these patients had neither ligamentous instability nor meniscal pathologies. Seventy-four of them were previously analysed to determine the functional outcome and the survival rate (defined as the conversion rate to partial or total knee arthroplasty) after a mean follow-up of 7.5 years. [25] To specifically analyse sporting activity after combined OAT and valgus HTO in young and active patients, patients from this cohort were included for the present study, if they were participating in sports on a regular base prior to surgery (lifetime), if they had a follow-up of at least 2 years and if they were aged <40 years at the time of surgery. Thirty out of the previous reported 74 patients fulfilled the inclusion criteria and were enrolled for further evaluation (Fig. 1).
Patients
The mean age at the time of surgery was 31 years [19–39; Standard Deviation (SD) 6.0] and the mean Body-Mass-Index measured 25 kg/m2 (21–32; SD 2.5). The left knee was affected in 11 (37 %) and the right knee in 19 (63 %) cases. The mean preoperative varus malalignment was 4.6° (2°–9°; SD 2.0), and the mean defect size (measured intraoperatively) was 20.5 mm (8–33; SD 8.8) in diameter (mean surface 3.3 cm2). Osteochondritis dissecans was diagnosed in 24 patients (80 %), and 6 lesions (20 %) were posttraumatic. Twenty-four patients (80 %) had previous operations on the affected knee. Cartilage defects had been surgically addressed before in 11 patients (36 %; 9 subchondral bone marrow stimulation techniques, 1 OAT procedures, 1 ACI procedure), and 6 patients (20 %) had a previous partial resection of the medial meniscus.
Operative technique
A diagnostic arthroscopy was performed to evaluate the chondral status and to rule out any preclusive concomitant abnormalities. Subsequently, a medial parapatellar arthrotomy was performed to expose the defect of the medial femoral condyle. Its diameter was measured precisely to determine size and number of the required autografts. The OAT procedure was performed using the osteochondral autologous transfer system (OATS, Arthrex Naples USA). Therefore, the defect was prepared with a cylindrical hollow chisel, and the cylinders were harvested from the lateral edge of the trochlea and transferred “press-fit” into the prepared osteochondral defect zone in order to restore the entire defect with stable chondral and osseous borders adjacent to the plugs. Size and number of the transferred cylinders were variable depending on the defect size: one osteochondral plug was transferred in 11 patients (36.7 %), 2 plugs in 10 patients (33.3 %) and 3 plugs in 9 patients (30.0 %). The diameter of the plugs ranged from 8 to 13 mm.
Subsequently, a slight overcorrecting valgus HTO (2°–4° valgus) was performed. Sixteen patients (53 %), who were operated before 2004, were treated with a lateral closed-wedge osteotomy (conventional non-locking L-plate, Zimmer; Freiburg, Germany) as described by El-Azab et al [9]. The remaining 14 patients (47 %) were treated with a valgus-producing medial open-wedge osteotomy (Tomofix, Synthes; Solothurn, Switzerland or Peek Power Plate, Arthrex; Naples, USA) using the technique described by Hinterwimmer et al. [17]
Post-operatively, a 6-week period of non-weight-bearing followed by stepwise increasing load of 20 kg/week up to the patient’s body weight was recommended. The range of motion was not restricted, and physiotherapy twice a week as well as continuous passive motion on a motor splint was recommended for 6–8 weeks. Return to sport was allowed after the osteotomy has radiologically healed completely. Depending on range of motion, pain, effusion and muscular status, contact sports were cleared.
Hardware removal due to local soft tissue irritation and pain was performed in 21 patients (in 86 % of all medial open-wedge and in 56 % of all lateral closed-wedge osteotomies).
Outcome measures
Patients were evaluated retrospectively using a sport-specific questionnaire, which has been used by several authors before [21, 27, 33]. The questionnaire evaluates the patients’ pre- and post-operative engagement in 32 different sports and recreational activities, the sports frequency (defined as sessions per week), sports duration (defined as hours per week), the number of sports disciplines and sports level (no sports, recreational, professional or competitive). All patients were asked to characterize their sporting activity at 1 year before surgery and at the final follow-up. In addition, the Tegner activity scale and the Activity Rating Scale [16] were used to compare sports participation 1 year preoperatively and at final follow-up [23, 37].
Patients were asked whether pain occurs “never”, “occasionally” or “regularly” during sporting activities.
The Ethics Committee of the medical school of the “Technische Universität München” approved the study from an ethical and legal point of view (IRB Nr. 5606/12).
Statistical analysis
Statistical analysis was performed with IBM SPSS Statistics software for Windows (version 21.0, SPSS Inc. Chicago, Illinois).
The Wilcoxon signed-rank test for related samples was used to compare changes in the sports frequency, sports duration, sports level, number of sports disciplines, Tegner Score and ARS between 1 year preoperative and final follow-up.
Correlations were tested using bivariate Pearson’s correlation coefficient. A p value <0.05 was considered to indicate statistical significance.
An a priori power analysis was calculated with a return to sports rate of 30 %. It established a sample size of 22 patients for a power of 80 % and an Alpha of 0.05.
Results
All patients were available for evaluation. The mean follow-up of the patient cohort was 6.9 years (2.5–9.8; SD 2.4).
Of all patients, 76.7 % participated in sports on a regular base 1 year preoperatively. At the time of the index procedure, no patient was able to participate in sporting activities due to symptoms related to the osteochondral defect of the medial femoral condyle. At the time of the final follow-up, 23 patients were engaged in sports, giving a return to sports rate of 76.7 % (Fig. 2). The Tegner activity scale showed no statistically significant increase and measured preoperatively median 5.0 (2.0–7.0) and post-operatively 5.0 (4.0–7.0) points (Fig. 3), and the ARS changed from 5.7 to 5.3 points (n.s.) (Table 1). Sports participation 1 year preoperatively and at final follow-up is shown in Table 1.
There was a significant negative correlation between age and post-operative sports frequency (Pearson´s correlation coefficient: r = −0.369, p = 0.045).
The number of previous surgeries showed a significant negative correlation with the post-operative Tegner Score (r = −0.444, p = 0.014).
There was a significant positive correlation between post-operative sports frequency and post-operative sports duration (r = 0.771, p = 0.000). There was no significant correlation between defect-size and post-operative sports activity (Tegner Score, ARS, sports frequency, sports duration).
With regard to the 32 evaluated sport disciplines, a comparable distribution was found at 1 year preoperatively and points (Fig. 4). The top three activities performed post-operatively were “cycling”, “swimming” and “fitness-training”.
Ten patients (33.3 %) stated to never feel pain during sports in their operated knee, 12 patients (40.0 %) reported about pain occurring occasionally, and 8 participants (26.7 %) had pain regularly.
Discussion
The main finding of this study is that OAT combined with valgus HTO allows young and active patients to return to sports at a level comparable to the situation 1 year preoperatively.
The formulated goals of cartilage repair procedures are to relief pain and symptoms, to restore the cartilage surface in order to avoid further joint degeneration, and to re-establish the ability to participate in sporting activities [1]. In an increasingly active population, the treatment of these defects remains a surgical challenge [26]. This is aggravated in case of concomitant pathologies that need to be addressed to optimize the biomechanical conditions in order to minimize the risk of failure. Varus malalignment—known as a serious risk factor for failure of cartilage repair procedures in the medial compartment [4, 11, 28]—can successfully be eliminated by an additional unloading valgus HTO [4, 15, 20, 25, 36].
In general, open cartilage surgery plus additional osteotomy results in a complex procedure with a long and extensive post-operative rehabilitation period. Although these combined procedures have shown high survival rates and improvement of functional outcome scores in long-term studies, there is a lack of data about post-operative sports participation [25, 36]. However, this aspect seems to be an important outcome parameter, since most patients are young and active with a high demand on the post-operative result. Most of the patients of this study participated in sports on a regular base one year before surgery. At the time of the operation, however, none of the patients was able to perform sports anymore. At the final follow-up, 76.7 % of the patients were highly active and performed mean 2.6 sessions with all in all 5.3 h per week. There was no difference in terms of post-operatively performed sessions or hours per week compared to the recorded data 1 year preoperatively. Moreover, there was no difference when comparing the level or the distribution pattern of the different performed activities. Thus, combined OAT plus valgus HTO re-allows patients for reaching the same athletic level as 1 year before surgery without regularly occurring pain during sporting activities in 73.3 %.
Correlation analysis showed that younger patients reach a higher post-operative sports frequency. Additionally, patients with less previous surgeries show higher post-operative Tegner Scores. This can be taken into account, when indicating HTO plus OAT. Although there was no significant correlation between defect-size and post-operative sports activity, OAT may lead to donor-site morbidity. This problem seems to be relevant especially in obese patients [29].
Marrow stimulating techniques (e.g. microfracture) are mainly used in chondral lesions smaller than 2 cm2—often as a first-line treatment [8]. This technique leads to fibrocartilage tissue, shows good clinical long-term results and was successfully combined with valgus HTO in case of concomitant varus malalignment [34–36]. However, our study population had deep focal and larger osteochondral lesions, for which reason OAT was chosen as the adequate surgical option. Better clinical results were seen after OAT compared with microfracture in these patients [12, 13].
Autologous chondrocyte transplantation can successfully be used in larger lesions, but is mainly limited by the depth of the defect [3, 30, 32]. This 2-step procedure can be combined with autologous cancellous bone grafting, but has remained an expensive technique [31, 38]. Good clinical midterm results of ACI plus HTO are reported in case of medial chondral femoral lesions and varus malalignment [3].
OAT is combined with a slight overcorrecting valgus HTO in case of symptomatic deep focal osteochondral lesions in the medial femoral condyle and concomitant varus malalignment of >2° in our department [10]. This treatment algorithm is consistent with biomechanical data, which show an equal load distribution between the medial and lateral compartment on cadaveric knees between 0° and 4° of valgus [24]. There are no data available about the amount of varus deviation that can be tolerated in case of osteochondral resurfacing. However, Bode et al. [4] investigated on the additional effect of an unloading osteotomy in patients treated with ACI in the medial femoral condyle and varus deviation of 1°–5° and found a significant higher survivor-rate in patients treated with an additional HTO.
In 2009 Salzmann et al. and in 2013 Bonnin et al. reported about sporting activity after HTO for the treatment of medial compartment knee osteoarthritis in patients older than those in the presented study [5, 33]. In general, good clinical results were seen, and a return to sports and recreational activities similar to the preoperative level were stated [33]. Thus, independent of the indication for unloading of the medial compartment and the patients’ age, patients usually adapt successfully to the changed post-operative joint biomechanics and return to their previous sports level. Limitations of the presented study are its retrospective design and the lack of a control group. Further, the study population is heterogeneous, and patients were treated either by lateral closed-wedge or medial open-wedge osteotomy. But, unloading of the transferred cylinders can be reached with both techniques. Third, this study does not provide information about the varus malalignment that can be tolerated, and the ideal biomechanical axis remains unclear. This topic has to be addressed in future trials.
Conclusion
A high return to sports rate and an activity level comparable to the state at 1 year preoperatively can be expected in young and active patients treated by OAT plus valgus HTO to address deep focal osteochondral femoral defects with additional mild-to-moderate varus malalignment. This adds relevant information when planning, indicating and performing these complex procedures.
References
Alford JW (2005) Cartilage restoration, part 1: basic science, historical perspective, patient evaluation, and treatment options. Am J Sports Med 33(2):295–306
Aroen A, Loken S, Heir S, Alvik E, Ekeland A, Granlund OG, Engebretsen L (2004) Articular cartilage lesions in 993 consecutive knee arthroscopies. Am J Sports Med 32(1):211–215
Bauer S, Khan RJK, Ebert JR, Robertson WB, Breidahl W, Ackland TR, Wood DJ (2012) Knee joint preservation with combined neutralising high tibial osteotomy (HTO) and matrix-induced autologous chondrocyte implantation (MACI) in younger patients with medial knee osteoarthritis: a case series with prospective clinical and MRI follow-up over 5 years. Knee 19(4):431–439
Bode G, Schmal H, Pestka JM, Ogon P, Sudkamp NP, Niemeyer P (2013) A non-randomized controlled clinical trial on autologous chondrocyte implantation (ACI) in cartilage defects of the medial femoral condyle with or without high tibial osteotomy in patients with varus deformity of less than 5 degrees. Arch Orthop Trauma Surg 133(1):43–49
Bonnin MP, Laurent JR, Zadegan F, Badet R, Pooler Archbold HA, Servien E (2013) Can patients really participate in sport after high tibial osteotomy? Knee Surg Sports Traumatol Arthrosc 21(1):64–73
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85-A(Suppl 2):58–69
Brouwer GM, van Tol AW, Bergink AP, Belo JN, Bernsen RMD, Reijman M, Pols HAP, Bierma-Zeinstra SMA (2007) Association between valgus and varus alignment and the development and progression of radiographic osteoarthritis of the knee. Arthritis Rheum 56(4):1204–1211
Cole BJ, Pascual-Garrido C, Grumet RC (2009) Surgical management of articular cartilage defects in the knee. J Bone Joint Surg Am 91(7):1778–1790
El-Azab H, Glabgly P, Paul J, Imhoff AB, Hinterwimmer S (2010) Patellar height and posterior tibial slope after open- and closed-wedge high tibial osteotomy: a radiological study on 100 patients. Am J Sports Med 38(2):323–329
Feucht MJ, Minzlaff P, Saier T, Cotic M, Sudkamp NP, Niemeyer P, Imhoff AB, Hinterwimmer S (2014) Degree of axis correction in valgus high tibial osteotomy: proposal of an individualised approach. Int Orthop. doi:10.1007/s00264-014-2442-7
Ghazavi MT, Pritzker KP, Davis AM, Gross AE (1997) Fresh osteochondral allografts for post-traumatic osteochondral defects of the knee. J Bone Joint Surg Br 79(6):1008–1013
Gudas R, Gudaite A, Pocius A, Gudiene A, Cekanauskas E, Monastyreckiene E, Basevicius A (2012) Ten-year follow-up of a prospective, randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint of athletes. Am J Sports Med 40(11):2499–2508
Gudas R, Kalesinskas RJ, Kimtys V, Stankevičius E, Toliušis V, Bernotavičius G, Smailys A (2005) A prospective randomized clinical study of mosaic osteochondral autologous transplantation versus microfracture for the treatment of osteochondral defects in the knee joint in young athletes. Arthroscopy 21(9):1066–1075
Hangody L, Fules P (2003) Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am 85-A(Suppl 2):25–32
Hangody L, Vasarhelyi G, Hangody LR, Sukosd Z, Tibay G, Bartha L, Bodo G (2008) Autologous osteochondral grafting—technique and long-term results. Injury 39(Suppl 1):S32–S39
Heir S, Nerhus TK, Røtterud JH, Løken S, Ekeland A, Engebretsen L, Arøen A (2010) Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med 38(2):231–237
Hinterwimmer S, Beitzel K, Paul J, Kirchhoff C, Sauerschnig M, von Eisenhart-Rothe R, Imhoff AB (2011) Control of posterior tibial slope and patellar height in open-wedge valgus high tibial osteotomy. Am J Sports Med 39(4):851–856
Hjelle K, Solheim E, Strand T, Muri R, Brittberg M (2002) Articular cartilage defects in 1,000 knee arthroscopies. Arthroscopy 18(7):730–734
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16(4):494–502
Kohn L, Sauerschnig M, Iskansar S, Lorenz S, Meidinger G, Imhoff AB, Hinterwimmer S (2013) Age does not influence the clinical outcome after high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 21(1):146–151
Kraus TM, Martetschlager F, Muller D, Braun KF, Ahrens P, Siebenlist S, Stockle U, Sandmann GH (2012) Return to sports activity after tibial plateau fractures: 89 cases with minimum 24-month follow-up. Am J Sports Med 40(12):2845–2852
Maletius W, Messner K (1996) The effect of partial meniscectomy on the long-term prognosis of knees with localized, severe chondral damage. A twelve- to fifteen-year followup. Am J Sports Med 24(3):258–262
Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF (2001) Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med 29(2):213–218
Mina C, Garrett WE Jr, Pietrobon R, Glisson R, Higgins L (2008) High tibial osteotomy for unloading osteochondral defects in the medial compartment of the knee. Am J Sports Med 36(5):949–955
Minzlaff P, Feucht MJ, Saier T, Schuster T, Braun S, Imhoff AB, Hinterwimmer S (2013) Osteochondral autologous transfer combined with valgus high tibial osteotomy: long-term results and survivorship analysis. Am J Sports Med 41(10):2325–2332
Mithoefer K, Hambly K, Della Villa S, Silvers H, Mandelbaum BR (2009) Return to sports participation after articular cartilage repair in the knee: scientific evidence. Am J Sports Med 37(Suppl 1):167S–176S
Naal FD, Fischer M, Preuss A, Goldhahn J, von Knoch F, Preiss S, Munzinger U, Drobny T (2007) Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med 35(10):1688–1695
Oakeshott RD, Farine I, Pritzker KP, Langer F, Gross AE (1988) A clinical and histologic analysis of failed fresh osteochondral allografts. Clin Orthop Relat Res 233:283–294
Paul J, Sagstetter A, Kriner M, Imhoff AB, Spang J, Hinterwimmer S (2009) Donor-site morbidity after osteochondral autologous transplantation for lesions of the talus. J Bone Joint Surg Am 91(7):1683–1688
Peterson L, Brittberg M, Kiviranta I, Akerlund EL, Lindahl A (2002) Autologous chondrocyte transplantation. Biomechanics and long-term durability. Am J Sports Med 30(1):2–12
Peterson L, Minas T, Brittberg M, Lindahl A (2003) Treatment of osteochondritis dissecans of the knee with autologous chondrocyte transplantation: results at two to ten years. J Bone Joint Surg Am 85-A(Suppl 2):17–24
Peterson L, Vasiliadis HS, Brittberg M, Lindahl A (2010) Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med 38(6):1117–1124
Salzmann GM, Ahrens P, Naal FD, El-Azab H, Spang JT, Imhoff AB, Lorenz S (2009) Sporting activity after high tibial osteotomy for the treatment of medial compartment knee osteoarthritis. Am J Sports Med 37(2):312–318
Steadman JR, Briggs KK, Rodrigo JJ, Kocher MS, Gill TJ, Rodkey WG (2003) Outcomes of microfracture for traumatic chondral defects of the knee: average 11-year follow-up. Arthroscopy 19(5):477–484
Sterett WI, Steadman JR (2004) Chondral resurfacing and high tibial osteotomy in the varus knee. Am J Sports Med 32(5):1243–1249
Sterett WI, Steadman JR, Huang MJ, Matheny LM, Briggs KK (2010) Chondral resurfacing and high tibial osteotomy in the varus knee: survivorship analysis. Am J Sports Med 38(7):1420–1424
Tegner Y, Lysholm J (1985) Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res 198:43–49
Vijayan S, Bartlett W, Bentley G, Carrington RW, Skinner JA, Pollock RC, Alorjani M, Briggs TW (2012) Autologous chondrocyte implantation for osteochondral lesions in the knee using a bilayer collagen membrane and bone graft: a two- to eight-year follow-up study. J Bone Joint Surg Br 94(4):488–492
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Minzlaff, P., Feucht, M.J., Saier, T. et al. Can young and active patients participate in sports after osteochondral autologous transfer combined with valgus high tibial osteotomy?. Knee Surg Sports Traumatol Arthrosc 24, 1594–1600 (2016). https://doi.org/10.1007/s00167-014-3447-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-014-3447-x