Abstract
Purpose of the Review
Low-grade systemic inflammation increases residual cardiovascular risk. The pathogenesis of low-grade systemic inflammation is not well understood.
Recent Findings
Visceral adipose tissue accumulates when the subcutaneous adipose tissue can no longer store excess nutrients. Visceral adipose tissue inflammation initially facilitates storage of nutrients but with time become maladaptive and responsible for low-grade systemic inflammation. Control of low-grade systemic inflammation requires reversal of visceral adipose tissue accumulation with intense and sustained aerobic exercise or bariatric surgery. Alternatively, pharmacologic inhibition of the inflammatory signaling pathway may be considered.
Summary
Reversal visceral adipose tissue accumulation lowers residual cardiovascular risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with cardiovascular disease (CVD) remain at risk for subsequent CVD events despite intensive secondary prevention therapy [1]. Low-grade systemic inflammation enhances the residual CVD risk of patients who are receiving such therapy [2]. In the current obesity epidemic, accumulation of adipose tissue (AT), particularly visceral adipose tissue (VAT), is a common cause of low-grade systemic inflammation [3••]. Obese middle-aged individuals without hypertension (HTN), hyperlipidemia (HLD), and diabetes are at a much greater risk of CVD events than their lean counterparts [4]. Further, obesity is the only independent determinant of atherosclerosis progression in patients who are receiving guideline directed therapy for HTN and HLD [5]. Thus, obesity begets low-grade systemic inflammation that in turn may heighten CVD risk in patients with preexisting vascular disease.
The present review examines the diverse sites of AT accumulation as the balance between nutrient excess and energy expenditure deteriorates. The review then details the VAT transition from an adaptive to a maladaptive inflammatory state and emphasizes the role of the central nervous system (CNS) and bone marrow derived immune cells (BMDIC) in the pathobiology of VAT accumulation and inflammation (Fig. 1). Lastly, the different therapeutic approaches that aim at reversing VAT accumulation or minimizing the adverse effects of VAT on residual CVD risk are discussed.
Nutrient excess leads to neuro-inflammation and production of leptin and angiotensin II (Ang II) by subcutaneous adipose tissue (SAT). Acting on hypothalamic neurons and microglia, leptin and Ang II activate the sympathetic nervous system (SNS) and induce resistance to leptin’s anorexic effect through metabolic inflammation (meta-inflammation)-related negative regulatory pathways. Leptin resistance leads to protracted nutrient excess that promotes SAT expansion. Patients tend to accumulate visceral adipose tissue (VAT) when SAT can no longer expand and store nutrients. Increased SNS activity and Ang II levels promote recruitment/engraftment of bone marrow-derived immune cells (BMDIC) in the hypothalamus and VAT. Whether obesity leads to hypothalamic meta-inflammation or hypothalamic meta-inflammation regulates the susceptibility to obesity through leptin resistance remains to be determined
Accumulation of Adipose Tissue
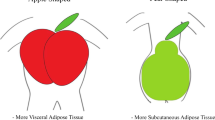
Body mass index, the ratio of body weight in kilograms over height in meter squared (BMI, kg/m2), is routinely used in clinical practice to define obesity and reveal the accumulation of AT [6]. Patients with a BMI ≥ 25 and < 30 kg/m2 are classified as overweight, and those with a BMI ≥ 30 kg/m2 are classified as obese. In men, AT preferentially accumulates in the trunk and upper body, whereas in women it preferentially accumulates in the hips and thighs [7••, 8]. Lipoprotein lipase activity, the rate-limiting step in AT accumulation from circulating triglycerides (TG), is greater in the abdominal region in men, whereas it is greater in the gluteal than in the abdominal region in women. Sex hormones, principally estrogens, affect regional AT accumulation and enhance the potency of anorexic signals such as leptin, cholecystokinin, and brain-derived neurotrophic factor (BDNF) while reducing the potency of orexigenic factors such as melanin-concentrating hormones and ghrelin [9]. Human AT expresses β 1-3 adrenergic receptors that exert a lipolytic effect and α 2 adrenergic receptors that have an anti-lipolytic effect. Estradiol increases α 2-adrenergic receptor expression in subcutaneous adipose tissue (SAT), but has no effect on intra-abdominal adipocytes [9]. Reversal of the β 1-2/α 2 adrenergic receptor ratio after the menopause promotes accumulation of intra-abdominal SAT and VAT that is associated with production of small low-density lipoprotein particles, thereby increasing CVD risk [10].
Adipose tissue accumulates in three compartments. The subcutaneous AT(SAT) accounts for 80–90% of total AT, whereas VAT and perivascular AT account for 5–15 and 2–3%, respectively [11]. SAT consists of superficial and deep layers. Metabolic and inflammatory genes are preferentially expressed in SAT superficial and deep layers, respectively [12,13,14]. Deep layers of the SAT undergo greater expansion when obesity develops and correlate more strongly than superficial layers with obesity-related insulin resistance and CVD [13]. Ectopic AT may also accumulate in the heart (myocardial, epicardial, and pericardial layers), liver (hepatic steatosis), pancreas, kidneys (renal sinus fat), and the abdomen (omental, mesenteric, and extraperitoneal) [11].
The term VAT refers to intra-abdominal accumulation of mesenteric and omental AT measured by a single slice CT at the level of L4–L5 or at the umbilicus [15]. Multiple slice imaging by MRI has shown that the amount of VAT varies in different slices [15]. Weight loss and resistance training programs lead to significant changes in the distribution of VAT area from the L3–L4 to the L2–L3 disc level following the interventions [16]. In the absence of intervention, a slice located 5–6 cm above L4–L5 disc provides the most accurate assessment of total VAT [17]. Waist circumference (WC) and waist to hip ratio (WHR) do not quantitatively reflect the amount of VAT [15]. However, an enlarged WC is a convenient qualitative signal of excess VAT in postmenopausal women [18]. Importantly, measurements of WC and WHR are somewhat operator dependent, and thus repeated measurements ideally should be performed by the initial operator [17].
Since only 5–15% of total AT resides in the visceral compartment, the total amount of VAT cannot be estimated from body weight or BMI [19]. The long-established paradigm that VAT accumulates when SAT can no longer expand to store more lipid has been recently challenged by the unexpected lack of correlation between intra-hepatic lipid accumulation and subcutaneous adipocyte size after 8 weeks of excess caloric intake [20,21,22]. At the population level, VAT accumulation may be inferred from a markedly elevated BMI that intimates near exhaustion of SAT storage capacity for lipid [23,24,25]. At the clinical level, a third of obese patients do not accumulate VAT and have no or minimal metabolic abnormalities. These patients are classified as metabolically healthy obese (MHO) [26, 27]. MHO appears to be a transitional state, however, as the adipokine profile (adiponectin/leptin/resistin) of MHO postmenopausal women is intermediate between that of normal weight postmenopausal women without and with metabolic abnormalities [28], and one third of MHO patients eventually develop metabolic abnormalities [29]. Further, MHO individuals have a higher risk of CAD, stroke, and heart failure than metabolically healthy normal weight individuals [30••]. In contrast, lean individuals with BMI < 30 kg/m2 may accumulate VAT and present with obesity-related metabolic abnormalities and are classified as metabolically obese normal weight persons [31].
Adipocyte hypertrophy mediates VAT expansion, whereas both adipocyte hyperplasia and hypertrophy contribute to SAT expansion in a depot-specific fashion: abdominal SAT expands through adipocyte hypertrophy, and femoral SAT expands through hyperplasia [20]. New adipocytes derived from pre-adipocytes account for 14–20% of cells in SAT [20]. Pre-adipocytes are associated with blood vessels and derive from endothelial cells or pericytes in AT [32]. They differentiate into adipocytes in response to insulin growth factor 1, glucocorticoids, and cyclic AMP [33]. Activation of the transcription factor CCATT enhancer-binding protein-β (C/EBPβ) triggers transcription of peroxisome proliferator-activated receptor-γ (PPARγ) and C/EBPα that activate genes required for the adipocyte phenotype [9, 22, 34, 35].
Pre-adipocytes can undergo senescence with aging and obesity and then release inflammatory cytokines, chemokines, and extracellular matrix proteases [36, 37]. T cell senescence may persist after loss of body weight and mediate chronic inflammation in AT due to continued production of osteopontin [38]. Contrary to conventional wisdom, the total number of adipose cells does not remain constant in adult SAT [39, 40]. However, when obesity develops in childhood or early adolescence, the number of adipocytes remains relatively constant thereafter [40].
Visceral Adipose Tissue
In adults, VAT largely comprises white energy storing adipocytes, with few brown energy dissipating adipocytes [41]. White adipocytes have large uni-locular lipid droplets and minimal uncoupling protein 1 (UCP1), while brown energy dissipating adipocytes have multi-locular lipid droplets and high UCP1 and mitochondrial content. The stromal vascular fraction (SVF) of AT contains immune cells, including resident macrophages which comprise up to 10–15% of AT cell population in lean persons and up to 40–50% in obese persons [42••, 43]. Sex affects VAT accumulation, with women having relatively less VAT and more SAT than men [44]. After controlling for total AT mass, age, and sex hormones, Caucasians have more VAT and less SAT than African-Americans [45,46,47]. VAT does not appear to be homogeneous: genome-wide arrays have shown that mesenteric pre-adipocytes have a greater capacity for replication and adipogenesis than omental pre-adipocytes [35].
Visceral AT accumulation is associated with a constellation of factors that increase CVD risk, including insulin resistance, hyperinsulinemia, increased small dense LDL and low HDL cholesterol, hypertriglyceridemia, diabetes, hypertension, inflammation, altered fibrinolysis, and endothelial dysfunction [23, 31, 48••, 49]. In contrast, SAT is not associated with metabolic abnormalities, and SAT accumulation does not increase CVD risk independently from BMI [50]. Further, liposuction with surgical removal of abdominal SAT has no effect on CVD risk [51]. After adjustment for general obesity measures (BMI, WC, WHR), only VAT remains associated with markers of systemic inflammation [50, 52]. Increased lipid turnover in VAT and reduced lipid turnover in SAT underlie the association between VAT and metabolic abnormalities [53]. Sympathetic nervous system (SNS) activation enhances inflammation. In men, the SNS is activated in visceral but not in subcutaneous obesity [54, 55]. In women, the SNS is not activated in visceral or subcutaneous obesity [56]. VAT is metabolically highly active and CVD risk correlates with VAT in both obese and metabolically unhealthy lean patients [57,58,59]. In the majority of obese patients, macrophage infiltration and release of cytokines/chemokines is greater in VAT than in SAT [60, 61]. Persistent blood pressure (BP) elevation, lower BP variability, and incident hypertension have been related to VAT [50, 62, 63]. VAT accumulation in Asian men may account for their increased cardiometabolic risk even in the presence of a normal BMI [31].
Circulating inflammatory markers like CRP and interleukin-6 (IL-6) are poor indices of VAT-related low-grade inflammation: CRP correlates more closely with the amount of SAT than VAT and only 30% of circulating IL-6 originates from AT [64,65,66]. Further, markers of AT inflammation such as reduction in adiponectin and increase in leptin levels do not reliably assess obesity-related low-level systemic inflammation [67]. Sex hormone binding protein level is inversely related to VAT in premenopausal overweight women [68]. Whether blood levels of classical monocytes reliably reflect CD11c+ macrophage infiltration in VAT needs to be confirmed [69].
The link between VAT accumulation and increased cardiometabolic risk remains poorly understood [52]. Although women have less VAT than men, the correlation between VAT accumulation and cardiometabolic risk is much stronger in women than men [19, 70]. Whether VAT accumulation is a manifestation of a general process that leads to metabolic and CVD or whether VAT accumulation plays a direct role in the development of these conditions is debated. A common view is that VAT accumulation signals the body’s inability to cope with continuous excessive caloric intake and triggers a downhill course of the obesity syndrome. Proposed specific causes of VAT accumulation such as increased hepatic free fatty acid (FFA) load, activation of the hypothalamic-pituitary adrenal axis and the endocannabinoid system, gonadal steroids, and epigenetic mechanisms have fallen out of favor or await supportive evidence [7••, 71].
Visceral Adipose Tissue Inflammation
As the gap between nutrient overload and reduced energy expenditure widens, unremitting visceral adipocyte hypertrophy leads to hypoxia, exposure to gut antigens, mechanical stress against a rigid extracellular matrix, immune cell infiltration, cytokine and chemokine secretion, and ultimately necrosis and inflammation in VAT [27]. The mechanisms and molecular signaling pathways of metabolic inflammation, i.e., meta-inflammation, have been extensively reviewed over the past decade [72,73,74,75,76,77, 78••, 79, 80••, 81,82,83,84,85]. The inflammatory responses of VAT and the central nervous system (CNS) to nutrient overload are reviewed here.
Adaptive VAT Inflammatory Response
Initially, the inflammatory response to adipocyte hypertrophy facilitates VAT expansion, remodeling, and lipid storage by stimulating angiogenesis and extracellular matrix degradation [76, 86••]. White adipocytes release FFA into the circulation for oxidation or storage by other cell types. Early in the AT inflammatory response, rapid AT expansion triggers lipid accumulation in and proliferation of resident macrophages [87]. White adipocytes secrete anti-inflammatory adipokines such as adiponectin, fibroblast growth factor-21 (FGF21), and IL-33 that activate innate lymphoid cells (ILC2’s) [81, 82]. In turn, IL-33-induced ILC2’s generate IL-5 and IL-13 that stimulate release of IL-4 by eosinophils to recruit alternatively activated resident macrophages with a potential for release of norepinephrine and stimulation of β3 adrenergic receptors, leading to activation of beige adipocytes [80, 88]. Norepinephrine may be imported and metabolized by sympathetic neuron-associated macrophages rather than released by AT macrophages [89]. As AT expands, the number of tolerance promoting B cells decreases, as does the number of anti-inflammatory type 1 natural killer T (NKT) cells, invariant (i) NKT cells, T helper 2 (TH2), and regulatory T cells (Tregs) [76, 83, 90]. TH2 cells and Tregs help to maintain macrophages in the alternatively activated state through secretion of IL-4 and Il-10 [83, 90]. Tregs-mediated maintenance of macrophages in the alternatively activated state requires expression of metabolic mediators such as PPAR γ and PPAR δ [77, 83]. Both innate and adaptive immune systems contribute to the inflammatory response to AT expansion [74, 75]. Promoting B cells influence both T cell and macrophage function in VAT [83, 91]. However, suppression of activated B and T cells in obese mice has no discernible effect on macrophage-mediated VAT inflammation [92].
Maladaptive VAT Inflammatory Response
The metabolic alterations associated with nutrient overload interact with immune function as AT expands [92, 93]. Alterations in circulating nutrients and metabolite signals influence macrophage polarization towards the classically activated state through nutrient sensing pathways such as AMPK and mTORC1 [83]. Continued adipocyte hypertrophy leads to adipocyte hypoxia and cell death, with production of pro-inflammatory signals such as monocyte chemotractant protein-1 (MCP1), C-X-C motif chemokine 12 (CXCCL12), retinol binding protein 4 (RBP4), leukotriene B4 (LKB4) colony stimulating factor 1 (Csf-1), and resistin that promote proliferation of classically activated macrophages and macrophage infiltration of white AT [77, 94••, 95, 96, 97••]. Insulin resistance correlates with increasing MCP1 production and thus may trigger inflammation in human VAT [98]. Reduced secretion of IL-10 and increased production of TNF-α and interferon (IFN) γ by iNKT cells also contribute to proliferation of classically activated macrophages that in turn release IL-6 and IL-1β [97••, 98]. Upregulation of major histocompatibility complex class II (MHCII) genes and leptin promote the T helper type 1 (Th1) phenotype [77]. T cells, Th1 cells, and macrophages form crown-like structures (CLS) that phagocytose dead adipocytes. B cells produce antibodies and activate T cells that in turn stimulate Th1 and effector T cells to release the pro-inflammatory cytokines TNF-α and IL-1β [77, 81, 82]. The receptor- and non-receptor-mediated triggers of AT inflammatory responses to nutrient overload/expansion are summarized in Fig. 2.
Unfolded proteins, excess nutrients, and hypoxia result in endoplasmic reticulum (ER) stress. ER stress activates a complex response, i.e., the unfolded protein response (UPR) that contributes to meta-inflammation by activating the inhibitor of κB kinase–β (IKK-β) through the inositol-requiring enzyme 1 (IRE-1) pathway. Increased adipose tissue oxidative stress, obesity-associated mitochondrial dysfunction (due to altered Ca++ signaling), and UPR are linked since ER malfunctions or oxidative stress can lead to mitochondrial dysfunction and vice versa. Hypoxia develops in adipose tissue where increasing levels of hypoxia-inducible factor-1α lead to nuclear factor-κB (NFκB) activation. Nutrients (saturated fatty acids) can indirectly activate pattern recognition receptors such as Toll-like receptors (TLR2 &4) that activate Jun N-terminal kinase (JNK) through myeloid differentiation factor 88 (MyD88) signaling. After adipocyte death, pathogen or danger-associated molecular patterns (PAMPs, DAMPs) and homeostasis-associated processes (HAMPs) activate an intracellular multi-protein signaling complex with nucleotide-binding leucin-rich repeat containing receptor 3 (NLRP3 inflamasome) that leads to activation of caspase-1.and secretion of pro-inflammatory IL-1β. Lastly, adipose-derived circulating miRNAs were recently shown to have systemic metabolic effects
The two-tier classification of macrophages (classical M1 and alternatively activated M2) observed in high-fat diet (HFD) murine models of obesity may not reflect the human condition where macrophages display a number of phenotypes according the metabolic environment [80••, 93]. Confronted with continuous nutrient overload, macrophages polarize towards the M1 state and activate a lysosomal program of lipid metabolism [93, 94••]. Inhibition of lysosomal function increases lipid accumulation in macrophages and reduces AT release of non-esterified fatty acids (FA) [79, 80••]. In AT with large adipocytes, macrophages play a major role in lipid catabolism [94••]. The role of macrophages in AT inflammation was first described in HFD murine models of obesity that contained abundant CLS around dying adipocytes [84]. However, human obesity is associated with fewer CLS, and macrophages play a lesser role in the adipocyte inflammatory response to nutrient overload/expansion in humans [84]. T cells rather than macrophages predominate in the inflammatory response of human AT to nutrient overload/expansion [107••, 108].
Neuro-inflammation
The hypothalamus contains several nuclei that control energy balance through two sets of leptin-sensitive neurons that have opposing actions [109,110,111]. The first consists of neuropeptide Y (NPY) and agouti-elated peptide (AgRP) neurons. Their activation stimulates caloric intake and reduces energy expenditure through the paracrine action of NPY and AgRP that decreases neuronal activity via GABAergic signaling [112]. The second set comprises proopiomelanocortin (POMC) and cocaine and amphetamine-related transcript (CART) neurons [109]. Activation of POMC/CART neurons decreases caloric intake and increases energy expenditure through release of α- melanocyte stimulating hormone that regulates caloric intake and activates melanocortin receptor-4 in the paraventricular nucleus [109, 113, 114]. Synaptic plasticity and neurogenesis affect the connectivity of AgRP/NPY and POMC/CART neurons [109].
Both neuronal sets have the long signaling form of the long form of the leptin receptor (LEPRb) [115, 116]. Increased leptin levels inhibit AgRP/NPY neurons and activate POMC/CART neurons [109, 116]. Obese patients develop leptin resistance as evidenced by persistence of high caloric intake despite obesity [117,118,119]. Importantly, nutrient overload may promote leptin resistance in the absence of obesity, and leptin resistance only targets energy homeostasis in obese individuals. Obesity does not affect leptin-mediated SNS activation or CNS upregulation [120,121,122,123]. Leptin resistance appears to be related to hypothalamic neuronal inflammation that develops within days of high FFA intake and persists with continued high FFA intake as neuronal inflammation spreads to glial cells [124, 125••, 126,127,128,129,130,131]. Hypothalamic and VAT inflammation share common signaling pathways that include Iκβ kinase-β/nuclear factor-κβ signaling, c-Jun-N-terminal kinase signaling, Toll-like receptor 4 signaling, endoplasmic reticulum stress, autophagy, and negative regulators such as suppressor of cytokine signaling 3 and protein tyrosine phosphatase 1B [128, 132, 133]. Hypothalamic inflammation affects the progression of obesity through leptin resistance. However, the time course and progression of the hypothalamic and VAT inflammatory response to nutrient overload are not directly related.
Over-nutrition may also mediate leptin resistance by altering the blood-brain barrier [134]. Hyperglycemia disassembles the specialized glial cells (tanycytes) that comprise the blood-cerebrospinal fluid barrier, thereby limiting leptin ingress into the hypothalamus [119]. Nutrient overload-induced neuro-inflammation [132, 135, 136] has also been noted in the hippocampus, cerebellum, amygdala, and brainstem of mice fed a HFD [136].
In HFD-induced murine models of obesity, microglial hypothalamic meta-inflammation regulates energy homeostasis [131]. Whether obesity leads to hypothalamic meta-inflammation or hypothalamic meta-inflammation regulates susceptibility to obesity through leptin resistance in humans is under active investigation [112].
Circulating Immune Cells
Obesity-associated sympathetic excitation bolsters bone marrow production of inflammatory cells that, attracted by local chemokines, infiltrate the CNS and VAT where they differentiate into macrophages [132, 136, 137]. Angiotensin II increases proliferation and differentiation of hematopoietic stem cells while decreasing their tissue engraftment [138, 139]. The spleen serves for storage and rapid deployment of bone marrow-derived immune cells [140]. The crosstalk between CNS, SAT, VAT, and bone marrow is outlined in Fig. 1. Prevention/reversal of VAT accumulation is a rational and direct approach to reducing low-grade systemic inflammation-related CVD risk.
Bariatric Surgery, Inflammation, and Cardiovascular Risk
Roux-en-Y Gastric Bypass (RYGB) Surgery
RYGB surgery consistently reduces circulating levels of CRP, IL-6, and IL-13 levels, while TNF-α levels are unaffected [141,142,143]. In a study of 65 morbidly obese patients, RYGB surgery decreased pro-inflammatory cytokines, including IL-18, soluble TNF-α receptor 2 (sTNFR2), and CRP in conjunction with a reduction in BMI from 49.2 to 31.9 kg/m2 [144]. Plasma concentrations of heat shock protein 60 (hsp60), an inflammatory and stress signaling protein, were reported to be lower 6–12 months after RYGB in a study of 53 obese women [145]. In addition to the decrease in circulating inflammatory mediators, RYGB surgery remodels body distribution of AT: 12 months after surgery, the reduction in VAT is relatively greater than that in SAT [146, 147]. VAT but not body weight continues to decrease after 12 months post-surgery [148]. Bariatric surgery reduces subcutaneous adipocyte size and LEPRb expression, but does not decrease adipocyte number [149]. Overall, bariatric surgery is associated with less weight loss in elderly male and diabetic patients [150, 151].
RYGB surgery is associated with a high remission rate of type II diabetes and reduces 10-year CVD risk by 40–50% in obese persons [152, 153]. However, observational studies and meta-analyses have shown that despite a low 10-year CVD risk, obese patients have a high lifetime CVD risk [151, 154,155,156,157]. Case-controlled studies with 10–12 year follow-up have shown that bariatric surgery (mostly RYGB) reduces fatal CVD outcomes in obese patients [158, 159••, 160]. In 418 obese patients who underwent RYGB and were followed for 12 years, remission of type 2 diabetes was 75% at 2 years, 62% at 6 years, and 51% at 12 years [158]. The Swedish Obese Subjects (SOS) study reported significant reductions in CV death, myocardial infarction, and stroke in 2010 obese patients who underwent bariatric surgery and were followed for a median duration of 14.7 years [159••]. Further, the Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently (STAMPEDE) trial demonstrated that 12 months of medical therapy plus bariatric surgery achieved glycemic control in significantly more patients than medical therapy alone [160].
The clear benefits of bariatric surgery on sustained weight loss and remission of type 2 diabetes point to the need for randomized trials of the procedure with mortality as a primary endpoint. Further, the long-term outcomes of bariatric surgical procedures, which are routinely not covered by third party payment, need to be monitored.
Sleeve Gastrectomy
Several lines of evidence point the favorable effects of laparoscopic sleeve gastrectomy (LSG) on low-grade systemic inflammation and VAT. Mean hs-CRP level fell from 8.8 to 2.6 mg/L at 12 months post-LSG in 197 obese patients with a median BMI of 46.8 kg/m2 [161]. In 110 morbidly obese women, high hs-CRP levels predicted the amount of VAT lost 1 year after LSG [162]. Six to 24 months after LSG, mRNA expression of inflammation-related genes in SAT decreased in 13 obese patients with a mean baseline BMI of 42.3 kg/m2 [163]. In contrast, mRNA expression of pro-inflammatory cytokines in SAT remained unchanged at 1 and 6–12 months in 17 obese patients with a mean baseline BMI of 46.3 kg/m2 who underwent RYGB (n = 7) or LSG (n = 10) [164]. These apparently discordant findings may be related to a predominant effect on of bariatric surgery on VAT rather than SAT in the latter study. The decrease in BMI and relative decrease in CRP levels were similar at 12 months in both studies: 13 versus 12 kg/m2 and 52 versus 66%, respectively.
Few studies have focused on the effects of LSG on CVD risk, and none has dealt with its effect on VAT. Reduced carotid artery intima-media thickness and increased brachial artery flow-mediated dilation following LSG provide indirect evidence of its beneficial effect on CVD risk [165, 166]. Further, a single-center study comparing LRYGB (n = 12) and LSG (n = 10) concluded that LRYGB is more effective in resolving low-grade systemic inflammation than is LSG [167]. Recent data indicate that bypass and sleeve gastrectomy have similar effects on weight loss and comorbid conditions through 5 years of follow-up [168]. Longer-term data are needed to ascertain which bariatric procedure is preferred for CVD risk reduction.
Physical Activity and Aerobic Exercise
Present data regarding the effect of physical activity on VAT are inconsistent. In the Framingham third-generation and Omni Ii cohorts, moderate-to-vigorous physical activity (MVPA) measured with accelerometers over a period of 5 days was associated with reduced VAT accumulation [169]. The association between physical activity and VAT reduction was greater in women than in men, and sedentary time was not associated with VAT accumulation [169]. In contrast, MVPA measured with accelerometers over a period of 4 days accounted for only 4% of the variance in VAT in another study of 82 adults with a mean BMI of 30.9 kg/m2 [170]. A significant inverse association was reported between MVPA and VAT in a study of 271 middle-aged African-American women and men [171]. Overall, vigorous physical activity sustained in time and intensity may lessen VAT accumulation, while sedentary behavior is unrelated to VAT.
Randomized controlled trials of aerobic exercise training clearly indicate a beneficial effect of training for ≥ 8-week duration on VAT accumulation, providing that caloric intake remains constant [172]. Whether sex affects the VAT response to aerobic exercise remains an unresolved issue. Similar decreases in WC were reported in men and women after 12 months of daily aerobic exercise for 60 min/day [173]. Brisk walking for 3 h/week for 12 months decreased intra- and subcutaneous abdominal fat in 168 postmenopausal women with a baseline BMI of 30.5 kg/m2 [174]. This study showed that VAT accumulation may regress without a concomitant decrease in BMI [174]. A systematic review of 35 studies with a total of 2145 patients showed that aerobic exercise induced VAT reduction but that resistance exercise reduced insulin resistance and lowered LDL cholesterol but did not affect VAT [175]. VAT reduction occurred without significant loss of body weight in 3 of the 35 studies. Aerobic exercise-induced reduction in VAT depends on exercise intensity and duration [176]. Jogging 20 miles/week was shown to decrease VAT by 6.9% compared to 1.7 and 2.5% for walking 12 miles/week and jogging 12 miles/week, respectively [176]. A recent study confirmed the beneficial effects of 80% aerobic and 20% resistance exercise training on VAT. A cohort of 278 overweight/mildly obese women and men who had been previously randomized to a Mediterranean/low-carbohydrate (MED/LC) diet or a low-fat (LF) diet for 6 months were then randomized in factorial 2 × 2 design to 80% aerobic and 20% resistance exercise training three times a week or no training for 12 months [177••]. The MED/LC and LF diets did not affect VAT, while the exercise/resistance training resulted in significant VAT reductions in patients randomized to both diets [177••]. Although weight loss has been reported to have a greater effect on markers of inflammation than aerobic or resistance exercise, present consensus favors diet with physical training over diet without physical training for reduction of obesity-related systemic inflammation [74, 178, 179]. Aerobic exercise decreases low-level systemic inflammation by reducing total AT especially VAT accumulation and by a direct anti-inflammatory effect as evidenced by increased release of IL-1 receptor antagonist and reduced hepatic production of the adaptor protein fetuin-A [180]. Preclinical studies point to the importance of exercise intensity, duration, and frequency for VAT and mitochondrial lipid metabolism remodeling [181]. Finally, moderate caloric restriction for 12 months failed to reduce VAT in the recent Calorie Restriction in Overweight Senior S: Response of Older Adults to Dieting Study (CRSSROADS) [182]. While adherence to a vigorous exercise program appears to be the most effective intervention for VAT reduction, many obese patients are unable to exercise vigorously.
Changes in VAT cannot be estimated from changes in SAT or body weight. Relative percent changes in visceral versus subcutaneous abdominal fat were reviewed in 61 weight loss studies [183]. Save for very-low-calorie diets that resulted in short-term preferential VAT loss, the method of weight loss had no bearing on relative reductions of VAT versus SAT [183]. In contrast, lifestyle modification that includes both healthy eating and aerobic exercise has been associated with preferential loss of VAT in obese and non-obese persons [184,185,186]. Of note, aerobic exercise for VAT reduction needs to be strenuous with more sessions per week than generally recommended for CVD risk reduction [173, 187].
Obesity is a major barrier to regular aerobic exercise [188]. Fearing negative comments, obese children are reluctant to participate in physical activities [189]. Similarly, obese adults tend to avoid exercise due to embarrassment in gyms and bias from fitness professionals. Morbidly obese patients may only be able to walk short distances, as the metabolic cost of walking on flat ground at moderate speed is close to their anaerobic threshold. Bariatric surgery-induced weight loss is a key step that may break the downward spiral from increase in body weight to steady decrease in physical activity [190].
Pharmacologic Reduction of Systemic Inflammation
The Justification for the Use of Statins in Prevention: an intervention Trial Evaluating Rosuvastatin (JUPITER) reported that lowering systemic inflammation with a statin reduced the incidence of major CVD events in patients with hs-CRP levels ≥ 2 mg/L, LDL cholesterol < 130 mg/dL, and no history of CVD [191]. The reduction in CVD events was twofold greater than that expected from the concomitant reduction in LDL cholesterol. The effect of colchicine, another commonly used anti-inflammatory therapy, on the risk of subsequent CVD events is currently being assessed in two randomized placebo controlled trials [192]. A targeted approach to the reduction of systemic inflammation was used in the Canakinumab Anti-inflammatory Thrombosis Outcome Study (CANTOS) [193]. Ten thousand patients with prior MI and hs-CRP ≥ 2 mg/L were randomized to three doses (50, 150, and 300 mg daily) of canakinumab, a monoclonal IL-1β antibody or to placebo. At a median follow-up of 3.7 years, patients receiving 150 mg of canakinumab experienced a 15% lower risk of major CVD events than patients receiving placebo [193]. Patients with hs-CRP < 2 mg/L while receiving canakinumab experienced a 31% lower risk of major CVD events, whereas patients with hs-CRP ≥ 2 mg/L did not experience any risk reduction [194]. The redundancy of inflammatory signaling pathways may thwart the pharmacological approaches to lessen obesity-related systemic inflammation and metabolic disorders. Canakinumab lowers the risk of CVD events but does not prevent the progression from pre-diabetes to diabetes [195].
Conclusion
Accumulation of VAT mediates obesity-associated low-grade systemic inflammation and CVD risk. In the absence of specific circulating markers for VAT, BMI is currently used as a surrogate for VAT. Adherence to an intensive aerobic exercise program is requisite for reduction of VAT-associated low-grade systemic inflammation and CVD risk. Bariatric surgery may allow morbidly obese patients with VAT accumulation to undertake intense aerobic exercise. The redundancy of obesity-related inflammatory signaling pathways presents a challenge to development of pharmacologic approaches to inhibiting low-grade systemic inflammation and thus preventing CVD in obese patients.
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Ridker PM. How common is residual inflammatory risk? Circ Res. 2017;120(4):617–9. https://doi.org/10.1161/CIRCRESAHA.116.310527.
Bohula EA, Giugliano RP, Leiter LA, Verma S, Park JG, Sever PS, et al. Inflammatory and cholesterol risk in the FOURIER Trial (further cardiovascular outcomes research with PCSK9 inhibition in patients with elevated risk). Circulation. 2018; https://doi.org/10.1161/CIRCULATIONAHA.118.034032.
•• Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Elevated C-reactive protein levels in overweight and obese adults. JAMA. 1999;282(22):2131–5. Strong evidence from the Third National Health and Nutrition Examintaton Survey that overweight and obesity are associated with inflammation as evidenced by elevated CRP levels.
Yan LL, Daviglus ML, Liu K, Stamler J, Wang R, Pirzada A, et al. Midlife body mass index and hospitalization and mortality in older age. JAMA. 2006;295(2):190–8. https://doi.org/10.1001/jama.295.2.190.
Sandfort V, Lai S, Ahlman MA, Mallek M, Liu S, Sibley CT, et al. Obesity is associated with progression of atherosclerosis during statin treatment. J Am Heart Assoc. 2016;5:e003621. https://doi.org/10.1161/JAHA.116.003621.
Gadde KM, Martin CK, Berthoud HR, Heymsfield SB. Obesity: pathophysiology and management. J Am Coll Cardiol. 2018;71(1):69–84. https://doi.org/10.1016/j.jacc.2017.11.011.4.1.20.
•• Després JP. Body fat distribution and risk of cardiovascular disease: an update. Circulation. 2012;126(10):1301–13. https://doi.org/10.1161/CIRCULATIONAHA.111.067264. The first compprehensive review of the pathophysiology of human visceral obesity with emphasis on measurement of waist circumfernce and the benefits of lifestyle interventions.
Tchoukalova YD, Koutsari C, Votruba SB, Tchkonia T, Giorgadze N, Thomou T, et al. Sex- and depot-dependent differences in adipogenesis in normal-weight humans. Obesity (Silver Spring). 2010;18(10):1875–80. https://doi.org/10.1038/oby.2010.56.
Palmer BF, Clegg DJ. The sexual dimorphism of obesity. Mol Cell Endocrinol. 2015;402:113–9. https://doi.org/10.1016/j.mce.2014.11.029.
Hodson L, Banerjee R, Rial B, Arlt W, Adiels M, Boren J, et al. Menopausal status and abdominal obesity are significant determinants of hepatic lipid metabolism in women. J Am Heart Assoc. 2015;4(10):e002258. https://doi.org/10.1161/JAHA.115.002258.
Gastaldelli A, Basta G. Ectopic fat and cardiovascular disease: what is the link? Nutr Metab Cardiovasc Dis. 2010;20(7):481–90. https://doi.org/10.1016/j.numecd.2010.05.005.
Cancello R, Zulian A, Gentilini D, Maestrini S, Della Barba A, Invitti C, et al. Molecular and morphologic characterization of superficial- and deep-subcutaneous adipose tissue subdivisions in human obesity. Obesity (Silver Spring). 2013;21(12):2562–70. https://doi.org/10.1002/oby.20417.
Marinou K, Hodson L, Vasan SK, Fielding BA, Banerjee R, Brismar K, et al. Structural and functional properties of deep abdominal subcutaneous adipose tissue explain its association with insulin resistance and cardiovascular risk in men. Diabetes Care. 2014;37(3):821–9. https://doi.org/10.2337/dc13-1353.
Abraham TM, Pedley A, Massaro JM, Hoffmann U, Fox CS. Association between visceral and subcutaneous adipose depots and incident cardiovascular disease risk factors. Circulation. 2015;132(17):1639–47. https://doi.org/10.1161/CIRCULATIONAHA.114.015000.
Tchernof A, Després JP. Pathophysiology of human visceral obesity: an update. Physiol Rev. 2013;93(1):359–404. https://doi.org/10.1152/physrev.00033.2011.
Idoate F, Ibañez J, Gorostiaga EM, García-Unciti M, Martínez-Labari C, Izquierdo M. Weight-loss diet alone or combined with resistance training induces different regional visceral fat changes in obese women. Int J Obes. 2011;35(5):700–13. https://doi.org/10.1038/ijo.2010.190.
Seimon RV, Wild-Taylor AL, Gibson AA, Harper C, McClintock S, Fernando HA, et al. Less waste on waist measurements: determination of optimal waist circumference measurement site to predict visceral adipose tissue in postmenopausal women with obesity. Nutrients. 2018;10(2) https://doi.org/10.3390/nu10020239.
Rubin R. Postmenopausal women with a “normal” BMI might be overweight or even obese. JAMA. 2018;319(12):1185–7. https://doi.org/10.1001/jama.2018.0423.
Elffers TW, de Mutsert R, Lamb HJ, de Roos A, Willems van Dijk K, Rosendaal FR, et al. Body fat distribution, in particular visceral fat, is associated with cardiometabolic risk factors in obese women. PLoS One. 2017;12(9):e0185403. https://doi.org/10.1371/journal.pone.0185403.
Johannsen DL, Tchoukalova Y, Tam CS, Covington JD, Xie W, Schwarz JM, et al. Effect of 8 weeks of overfeeding on ectopic fat deposition and insulin sensitivity: testing the “adipose tissue expandability” hypothesis. Diabetes Care. 2014;37(10):2789–97. https://doi.org/10.2337/dc14-0761.
Tchkonia T, Thomou T, Zhu Y, Karagiannides I, Pothoulakis C, Jensen MD, et al. Mechanisms and metabolic implications of regional differences among fat depots. Cell Metab. 2013;17(5):644–56. https://doi.org/10.1016/j.cmet.2013.03.008.
Smith U. Abdominal obesity: a marker of ectopic fat accumulation. J Clin Invest. 2015;125(5):1790–2. https://doi.org/10.1172/JCI81507.
Wormser D, Kaptoge S, Di Angelantonio E, Wood AM, Pennells L, Thompson A, et al. Separate and combined associations of body-mass index and abdominal adiposity with cardiovascular disease: collaborative analysis of 58 prospective studies. Lancet. 2011;377(9771):1085–95. https://doi.org/10.1016/S0140-6736(11)60105-0.
Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet. 2014;383(9921):970–83. https://doi.org/10.1016/S0140-6736(13)61836-X.
Khan SS, Ning H, Wilkins JT, Allen N, Carnethon M, Berry JD, et al. Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol. 2018; https://doi.org/10.1001/jamacardio.2018.0022.
Stefan N, Schick F, Häring HU. Measures of adiposity and fat distribution and risk of diabetes. JAMA. 2013;309(4):339–40. https://doi.org/10.1001/jama.2012.94335.
Blüher M. Adipose tissue inflammation: a cause or consequence of obesity-related insulin resistance? Clin Sci (Lond). 2016;130(18):1603–14. https://doi.org/10.1042/CS20160005.
Khan UI, Ogorodnikova AD, Xu L, Wang D, Wassertheil-Smoller S, Ho GY, et al. The adipokine profile of metabolically benign obese and at-risk normal weight postmenopausal women: the Women’s Health Initiative Observational Study. Obesity (Silver Spring). 2014;22(3):786–94. https://doi.org/10.1002/oby.20139.
Appleton SL, Seaborn CJ, Visvanathan R, Hill CL, Gill TK, Taylor AW, et al. Diabetes and cardiovascular disease outcomes in the metabolically healthy obese phenotype: a cohort study. Diabetes Care. 2013;36(8):2388–94. https://doi.org/10.2337/dc12-1971.
•• Caleyachetty R, Thomas GN, Toulis KA, Mohammed N, Gokhale KM, Balachandran K, et al. Metabolically healthy obese and incident cardiovascular disease events among 3.5 Million Men and Women. J Am Coll Cardiol. 2017;70(12):1429–37. https://doi.org/10.1016/j.jacc.2017.07.763. The metabolically heathy obese state was associated with long-term risk of cardiovascular events during a mean follow-up of 5.4 years.
Nazare JA, Smith JD, Borel AL, Haffner SM, Balkau B, Ross R, et al. Ethnic influences on the relations between abdominal subcutaneous and visceral adiposity, liver fat, and cardiometabolic risk profile: the international study of prediction of intra-abdominal adiposity and its relationship with cardiometabolic risk/intra-abdominal adiposity. Am J Clin Nutr. 2012;96(4):714–26. https://doi.org/10.3945/ajcn.112.035758.
Gupta RK, Mepani RJ, Kleiner S, Lo JC, Khandekar MJ, Cohen P, et al. Zfp423 expression identifies committed preadipocytes and localizes to adipose endothelial and perivascular cells. Cell Metab. 2012;15(2):230–9. https://doi.org/10.1016/j.cmet.2012.01.010.
Cawthorn WP, Scheller EL, MacDougald OA. Adipose tissue stem cells meet preadipocyte commitment: going back to the future. J Lipid Res. 2012;53(2):227–46. https://doi.org/10.1194/jlr.R021089.
Tang QQ, Lane MD. Adipogenesis: from stem cell to adipocyte. Annu Rev Biochem. 2012;81:715–36. https://doi.org/10.1146/annurev-biochem-052110-115718.
Tchkonia T, Lenburg M, Thomou T, Giorgadze N, Frampton G, Pirtskhalava T, et al. Identification of depot-specific human fat cell progenitors through distinct expression profiles and developmental gene patterns. Am J Physiol Endocrinol Metab. 2007;292(1):E298–307. https://doi.org/10.1152/ajpendo.00202.2006.
Guo W, Pirtskhalava T, Tchkonia T, Xie W, Thomou T, Han J, et al. Aging results in paradoxical susceptibility of fat cell progenitors to lipotoxicity. Am J Physiol Endocrinol Metab. 2007;292(4):E1041–51. https://doi.org/10.1152/ajpendo.00557.2006.
Freund A, Orjalo AV, Desprez PY, Campisi J. Inflammatory networks during cellular senescence: causes and consequences. Trends Mol Med. 2010;16(5):238–46. https://doi.org/10.1016/j.molmed.2010.03.003.
Shirakawa K, Endo J, Katsumata Y, Yamamoto T, Kataoka M, Isobe S, et al. Negative legacy of obesity. PLoS One. 2017;12(10):e0186303. https://doi.org/10.1371/journal.pone.0186303.
Tchoukalova YD, Votruba SB, Tchkonia T, Giorgadze N, Kirkland JL, Jensen MD. Regional differences in cellular mechanisms of adipose tissue gain with overfeeding. Proc Natl Acad Sci U S A. 2010;107(42):18226–31. https://doi.org/10.1073/pnas.1005259107.
Spalding KL, Arner E, Westermark PO, Bernard S, Buchholz BA, Bergmann O, et al. Dynamics of fat cell turnover in humans. Nature. 2008;453(7196):783–7. https://doi.org/10.1038/nature06902.
Betz MJ, Enerbäck S. Human brown adipose tissue: what we have learned so far. Diabetes. 2015;64(7):2352–60. https://doi.org/10.2337/db15-0146.
•• Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003;112(12):1796–808. https://doi.org/10.1172/JCI19246. The first demonstration of increased adipose tissue macrophage numbers in obesity and the role macrophages play in activation of inflammatory pathways.
Cildir G, Akıncılar SC, Tergaonkar V. Chronic adipose tissue inflammation: all immune cells on the stage. Trends Mol Med. 2013;19(8):487–500. https://doi.org/10.1016/j.molmed.2013.05.001.
Tchoukalova YD, Koutsari C, Karpyak MV, Votruba SB, Wendland E, Jensen MD. Subcutaneous adipocyte size and body fat distribution. Am J Clin Nutr. 2008;87(1):56–63. https://doi.org/10.1093/ajcn/87.1.56.
Hoffman DJ, Wang Z, Gallagher D, Heymsfield SB. Comparison of visceral adipose tissue mass in adult African Americans and whites. Obes Res. 2005;13(1):66–74. https://doi.org/10.1038/oby.2005.9.
Bidulescu A, Liu J, Hickson DA, Hairston KG, Fox ER, Arnett DK, et al. Gender differences in the association of visceral and subcutaneous adiposity with adiponectin in African Americans: the Jackson Heart Study. BMC Cardiovasc Disord. 2013;13:9. https://doi.org/10.1186/1471-2261-13-9.
Carroll JF, Chiapa AL, Rodriquez M, Phelps DR, Cardarelli KM, Vishwanatha JK, et al. Visceral fat, waist circumference, and BMI: impact of race/ethnicity. Obesity (Silver Spring). 2008;16(3):600–7. https://doi.org/10.1038/oby.2007.92.
•• Pou KM, Massaro JM, Hoffmann U, Vasan RS, Maurovich-Horvat P, Larson MG, et al. Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: the Framingham Heart Study. Circulation. 2007;116(11):1234–41. https://doi.org/10.1161/CIRCULATIONAHA.107.710509. Cross sectional data support the associatin between visceral obesity and inflammation/oxidative stress. The role of visceral adipose tissue in inflammation is not accounted for by body mass index or waist circumference.
Britton KA, Massaro JM, Murabito JM, Kreger BE, Hoffmann U, Fox CS. Body fat distribution, incident cardiovascular disease, cancer, and all-cause mortality. J Am Coll Cardiol. 2013;62(10):921–5. https://doi.org/10.1016/j.jacc.2013.06.027.
Neeland IJ, Ayers CR, Rohatgi AK, Turer AT, Berry JD, Das SR, et al. Associations of visceral and abdominal subcutaneous adipose tissue with markers of cardiac and metabolic risk in obese adults. Obesity (Silver Spring). 2013;21(9):E439–47. https://doi.org/10.1002/oby.20135.
Goossens GH. The metabolic phenotype in obesity: fat mass, body fat distribution, and adipose tissue function. Obes Facts. 2017;10(3):207–15. https://doi.org/10.1159/000471488.
Despres JP Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444(712):881–7. https://doi.org/10.1038/nature05488.
Spalding KL, Bernard S, Näslund E, Salehpour M, Possnert G, Appelsved L, et al. Impact of fat mass and distribution on lipid turnover in human adipose tissue. Nat Commun. 2017;8:15253. https://doi.org/10.1038/ncomms15253.
Alvarez GE, Beske SD, Ballard TP, Davy KP. Sympathetic neural activation in visceral obesity. Circulation. 2002;106(20):2533–6.
Alvarez GE, Ballard TP, Beske SD, Davy KP. Subcutaneous obesity is not associated with sympathetic neural activation. Am J Physiol Heart Circ Physiol. 2004;287(1):H414–8. https://doi.org/10.1152/ajpheart.01046.2003.
Faulkner JL, Belin de Chantemèle EJ. Sex differences in mechanisms of hypertension associated with obesity. Hypertension. 2018;71(1):15–21. https://doi.org/10.1161/HYPERTENSIONAHA.117.09980.
Sam S. Differential effect of subcutaneous abdominal and visceral adipose tissue on cardiometabolic risk. Horm Mol Biol Clin Investig. 2018;33(1) https://doi.org/10.1515/hmbci-2018-0014.
Monteiro AM, Ferreira G, Duarte H. Metabolic activity in the visceral and subcutaneous adipose tissues by FDG-PET/CT in obese patients. Acta Medica Port. 2017;30(11):813–7.
Pérez-Pevida B, Díaz-Gutiérrez J, Miras AD, Silva C, Romero S, Salvador J, et al. High body adiposity drives glucose intolerance and increases cardiovascular risk in normoglycemic subjects. Obesity (Silver Spring). 2018;26(4):672–82. https://doi.org/10.1002/oby.22147.
Harman-Boehm I, Blüher M, Redel H, Sion-Vardy N, Ovadia S, Avinoach E, et al. Macrophage infiltration into omental versus subcutaneous fat across different populations: effect of regional adiposity and the comorbidities of obesity. J Clin Endocrinol Metab. 2007;92(6):2240–7. https://doi.org/10.1210/jc.2006-1811.
Pinnick KE, Nicholson G, Manolopoulos KN, McQuaid SE, Valet P, Frayn KN, et al. Distinct developmental profile of lower-body adipose tissue defines resistance against obesity-associated metabolic complications. Diabetes. 2014;63(11):3785–97. https://doi.org/10.2337/db14-0385.
Yano Y, Vongpatanasin W, Ayers C, Turer A, Chandra A, Carnethon MR, et al. Regional fat distribution and blood pressure level and variability: the Dallas Heart Study. Hypertension. 2016;68(3):576–83. https://doi.org/10.1161/HYPERTENSIONAHA.116.07876.
Chandra A, Neeland IJ, Berry JD, Ayers CR, Rohatgi A, Das SR, et al. The relationship of body mass and fat distribution with incident hypertension: observations from the Dallas Heart Study. J Am Coll Cardiol. 2014;64(10):997–1002. https://doi.org/10.1016/j.jacc.2014.05.057.
Schlecht I, Fischer B, Behrens G, Leitzmann MF. Relations of visceral and abdominal subcutaneous adipose tissue, body mass index, and waist circumference to serum concentrations of parameters of chronic inflammation. Obes Facts. 2016;9(3):144–57. https://doi.org/10.1159/000443691.
Mohamed-Ali V, Goodrick S, Rawesh A, Katz DR, Miles JM, Yudkin JS, et al. Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-alpha, in vivo. J Clin Endocrinol Metab. 1997;82(12):4196–200. https://doi.org/10.1210/jcem.82.12.4450.
Ridker PM. From C-reactive protein to interleukin-6 to interleukin-1: moving upstream to identify novel targets for atheroprotection. Circ Res. 2016;118(1):145–56. https://doi.org/10.1161/CIRCRESAHA.115.306656.
Seven E, Husemoen LL, Sehested TS, Ibsen H, Wachtell K, Linneberg A, et al. Adipocytokines, C-reactive protein, and cardiovascular disease: a population-based prospective study. PLoS One. 2015;10(6):e0128987. https://doi.org/10.1371/journal.pone.0128987.
Azrad M, Gower BA, Hunter GR, Nagy TR. Intra-abdominal adipose tissue is independently associated with sex-hormone binding globulin in premenopausal women. Obesity (Silver Spring). 2012;20(5):1012–5. https://doi.org/10.1038/oby.2011.375.
Wouters K, Gaens K, Bijnen M, Verboven K, Jocken J, Wetzels S, et al. Circulating classical monocytes are associated with CD11c. Sci Rep. 2017;7:42665. https://doi.org/10.1038/srep42665.
Thorand B, Baumert J, Döring A, Herder C, Kolb H, Rathmann W, et al. Sex differences in the relation of body composition to markers of inflammation. Atherosclerosis. 2006;184(1):216–24. https://doi.org/10.1016/j.atherosclerosis.2005.04.011.
Katz LS, Geras-Raaka E, Gershengorn MC. Heritability of fat accumulation in white adipocytes. Am J Physiol Endocrinol Metab. 2014;307(3):E335–44. https://doi.org/10.1152/ajpendo.00075.2014.
Horng T, Hotamisligil GS. Linking the inflammasome to obesity-related disease. Nat Med. 2011;17(2):164–5. https://doi.org/10.1038/nm0211-164.
Neels JG, Olefsky JM. Inflamed fat: what starts the fire? J Clin Invest. 2006;116(1):33–5. https://doi.org/10.1172/JCI27280.
Brestoff JR, Artis D. Immune regulation of metabolic homeostasis in health and disease. Cell. 2015;161(1):146–60. https://doi.org/10.1016/j.cell.2015.02.022.
Winer S, Winer DA. The adaptive immune system as a fundamental regulator of adipose tissue inflammation and insulin resistance. Immunol Cell Biol. 2012;90(8):755–62. https://doi.org/10.1038/icb.2011.110.
Osborn O, Olefsky JM. The cellular and signaling networks linking the immune system and metabolism in disease. Nat Med. 2012;18(3):363–74. https://doi.org/10.1038/nm.2627.
McNelis JC, Olefsky JM. Macrophages, immunity, and metabolic disease. Immunity. 2014;41(1):36–48. https://doi.org/10.1016/j.immuni.2014.05.010.
•• Reilly SM, Saltiel AR. Adapting to obesity with adipose tissue inflammation. Nat Rev Endocrinol. 2017;13(11):633–43. https://doi.org/10.1038/nrendo.2017.90. This review outlines the role of inflammation in the maladaptive responses to obesity and the lack of therapeutic success when targeting inflammation in the setting of obesity.
Saltiel AR, Olefsky JM. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest. 2017;127(1):1–4. https://doi.org/10.1172/JCI92035.
•• Hotamisligil GS. Foundations of immunometabolism and implications for metabolic health and disease. Immunity. 2017;47(3):406–20. https://doi.org/10.1016/j.immuni.2017.08.009. This clear summary of the pathobiology of the interface between metabolic disorders and innate and adaptive immunity provides a timeline of the major findings in the field of immunometabolism.
Hotamisligil GS. Inflammation, metaflammation and immunometabolic disorders. Nature. 2017;542(7640):177–85. https://doi.org/10.1038/nature21363.97.
Lumeng CN, Saltiel AR. Links between obesity and metabolic disease. J Clin Invest. 2011;121(6):2111–7. https://doi.org/10.1172/JCI57132.
Lee YS, Wollam J, Olefsky JM. An integrated view of immunometabolism. Cell. 2018;172(1–2):22–40. https://doi.org/10.1016/j.cell.2017.12.025.
Agrawal M, Kern PA, Nikolajczyk BS. The immune system in obesity: developing paradigms amidst inconvenient truths. Curr Diab Rep 2017;17(10):87. https://doi.org/10.1007/s11892-017-0917-9.
Shimobayashi M, Albert V, Woelnerhanssen B, Frei IC, Weissenberger D, Meyer-Gerspach AC, et al. Insulin resistance causes inflammation in adipose tissue. J Clin Invest. 2018;128(4):1538–50. https://doi.org/10.1172/JCI96139.
•• Wernstedt Asterholm I, Tao C, Morley TS, Wang QA, Delgado-Lopez F, Wang ZV, et al. Adipocyte inflammation is essential for healthy adipose tissue expansion and remodeling. Cell Metab. 2014;20(1):103–18. https://doi.org/10.1016/j.cmet.2014.05.005. Adipose tissue inflammation facilitates healthy adipogenesis, including adipose tissue expansion and remdeling.
Muir LA, Kiridena S, Griffin C, DelProposto JB, Geletka L, Martinez-Santibañez G, et al. Frontline Science: rapid adipose tissue expansion triggers unique proliferation and lipid accumulation profiles in adipose tissue macrophages. J Leukoc Biol. 2018;103(4):615–28. https://doi.org/10.1002/JLB.3HI1017-422R.
Nguyen KD, Qiu Y, Cui X, Goh YP, Mwangi J, David T, et al. Alternatively activated macrophages produce catecholamines to sustain adaptive thermogenesis. Nature. 2011;480(7375):104–8. https://doi.org/10.1038/nature10653.
Pirzgalska RM, Seixas E, Seidman JS, Link VM, Sánchez NM, Mahú I, et al. Sympathetic neuron-associated macrophages contribute to obesity by importing and metabolizing norepinephrine. Nat Med. 2017;23(11):1309–18. https://doi.org/10.1038/nm.4422.
Lynch L, Michelet X, Zhang S, Brennan PJ, Moseman A, Lester C, et al. Regulatory iNKT cells lack expression of the transcription factor PLZF and control the homeostasis of T(reg) cells and macrophages in adipose tissue. Nat Immunol. 2015;16(1):85–95. https://doi.org/10.1038/ni.3047.
Kucharska AM, Pyrżak B, Demkow U, Cells in Obesity RT. Adv Exp Med Biol. 2015;866:35–40. https://doi.org/10.1007/5584_2015_147.
Subramanian M, Ozcan L, Ghorpade DS, Ferrante AW, Tabas I. Suppression of adaptive immune cell activation does not alter innate immune adipose inflammation or insulin resistance in obesity. PLoS One. 2015;10(8):e0135842. https://doi.org/10.1371/journal.pone.0135842.
Pan Y, Tian T, Park CO, Lofftus SY, Mei S, Liu X et al. Survival of tissue-resident memory T cells requires exogenous lipid uptake and metabolism. Nature 2017;543(7644):252–256.
•• Xu X, Grijalva A, Skowronski A, van Eijk M, Serlie MJ, Ferrante AW. Obesity activates a program of lysosomal-dependent lipid metabolism in adipose tissue macrophages independently of classic activation. Cell Metab. 2013;18(6):816–30. https://doi.org/10.1016/j.cmet.2013.11.001. Expansion of adipose tissue induces a program of lysosome biogenesis in adipose tissue macrophages across models of obesity.
Amano SU, Cohen JL, Vangala P, Tencerova M, Nicoloro SM, Yawe JC, et al. Local proliferation of macrophages contributes to obesity-associated adipose tissue inflammation. Cell Metab. 2014;19(1):162–71. https://doi.org/10.1016/j.cmet.2013.11.017.
Lumeng CN, Deyoung SM, Bodzin JL, Saltiel AR. Increased inflammatory properties of adipose tissue macrophages recruited during diet-induced obesity. Diabetes. 2007;56(1):16–23. https://doi.org/10.2337/db06-1076.
•• Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest. 2007;117(1):175–84. https://doi.org/10.1172/JCI29881. A landmark paper regarding classical and alternatively activated macrophage phenotypes in high-fat diet mouse models of obesity.
Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest. 2003;112(12):1821–30. https://doi.org/10.1172/JCI19451.
Yang L, Calay ES, Fan J, Arduini A, Kunz RC, Gyfi SP, et al. METABOLISM. S-Nitorsylation links obesity-associated inflammation to endoplasmic reticulum dysfunction. Science. 2015;349:500–6. https://doi.org/10.1126/science.aaa0079.
Bondia-Pons I, Ryan L, Martinez JA. Oxidative stress and inflammation interactions in human obesity. J Physiol Biochem. 2012;68:701–11. https://doi.org/10.1007/s13105-012-0154-2.
Heinonen S, Buzkova J, Muniandy M, Kaksonen R, Ollikainen M, Ismail K, et al. Impaired mitochondrial biogenesis in adipose tissue in acquired obesity. Diabetes. 2015;64:3135–45. https://doi.org/10.2337/db14-1937.
Hahn WS, Kuzmicic J, Burrill JS, Donoghue MA, Foncea R, Jensen MD, et al. Proinflammatory cytokines differentially regulate adipocyte mitochondrial metabolism, oxidative stress and dynamics. Am J Physiol Endocrinol Metab. 2014;306:E1033–45. https://doi.org/10.1152/ajpendo.00422.2013.
Lee YS, Kim JW, Osborne O, Oh DY, Sasik R, Schenk S, et al. Increased adipocyte O2 consumption triggers HIF-1, causing inflammation and insulin resistance in obesity. Cell. 2014;157:1339–52. https://doi.org/10.1016/j.cell.2014.05.012.
Fessler MB, Rudell LL, Brown JM. Toll-like receptor signaling links dietary fatty acids to the metabolic syndrome. Curr Opin Lipidol. 2009;20:379–85. https://doi.org/10.109/MOL.0b013e32832fa5c4.
Stienstra R, Joosten LA, Koenen T, van Tits B, van Diepen JA, van den Berg SA, et al. The inflammasome-mediated caspase-1 activation controls adipocyte differentiation and insulin sensitivity. Cell Metab. 2010;12:593–605. https://doi.org/10.1016/j.cmet.2010.11.011.
Thomou T, Mori MA, Dreyfuss JM, Konishi M, Sagakushi M, Wolfrum C, et al. Adipose-derived circulation miRNAs regulate gene expression in other tissues. Nature. 2017;542:450–5. https://doi.org/10.1038/nature21365.
•• McLaughlin T, Liu LF, Lamendola C, Shen L, Morton J, Rivas H, et al. T-cell profile in adipose tissue is associated with insulin resistance and systemic inflammation in humans. Arterioscler Thromb Vasc Biol. 2014;34(12):2637–43. https://doi.org/10.1161/ATVBAHA.114.304636. Shift in the ratio of pro-to anti-inflammatory T cells supports the adaptive immune system contribution to adipose tissue inflammation in obesity.
Wu H, Ghosh S, Perrard XD, Feng L, Garcia GE, Perrard JL et al. T-cell accumulation and regulated on activation, normal T cell expressed and secreted upregulation in adipose tissue in obesity. Circulation 2007;115(8):1029–38. https://doi.org/10.1161/CIRCULATIONAHA.106.638379.
Williams LM. Hypothalamic dysfunction in obesity. Proc Nutr Soc. 2012;71(4):521–33. https://doi.org/10.1017/S002966511200078X.
Shimizu H, Inoue K, Mori M. The leptin-dependent and -independent melanocortin signaling system: regulation of feeding and energy expenditure. J Endocrinol. 2007;193(1):1–9. https://doi.org/10.1677/JOE-06-0144.
Hall JE, da Silva AA, do Carmo JM, Dubinion J, Hamza S, Munusamy S, et al. Obesity-induced hypertension: role of sympathetic nervous system, leptin, and melanocortins. J Biol Chem. 2010;285(23):17271–6. https://doi.org/10.1074/jbc.R110.113175.
Thaler JP, Guyenet SJ, Dorfman MD, Wisse BE, Schwartz MW. Hypothalamic inflammation: marker or mechanism of obesity pathogenesis? Diabetes. 2013;62(8):2629–34. https://doi.org/10.2337/db12-1605.
Shi Z, Li B, Brooks VL. Role of the paraventricular nucleus of the hypothalamus in the sympathoexcitatory effects of leptin. Hypertension. 2015;66(5):1034–41. https://doi.org/10.1161/HYPERTENSIONAHA.115.06017.
Rahmouni K. Cardiovascular regulation by the arcuate nucleus of the hypothalamus: neurocircuitry and signaling systems. Hypertension. 2016;67(6):1064–71. https://doi.org/10.1161/HYPERTENSIONAHA.115.06425.
Bell BB, Harlan SM, Morgan DA, Guo DF, Rahmouni K. Differential contribution of POMC and AgRP neurons to the regulation of regional autonomic nerve activity by leptin. Mol Metab. 2018;8:1–12. https://doi.org/10.1016/j.molmet.2017.12.006.
Kwon O, Kim KW, Kim MS. Leptin signalling pathways in hypothalamic neurons. Cell Mol Life Sci. 2016;73(7):1457–77. https://doi.org/10.1007/s00018-016-2133-1.
Prior LJ, Eikelis N, Armitage JA, Davern PJ, Burke SL, Montani JP, et al. Exposure to a high-fat diet alters leptin sensitivity and elevates renal sympathetic nerve activity and arterial pressure in rabbits. Hypertension. 2010;55(4):862–8. https://doi.org/10.1161/HYPERTENSIONAHA.109.141119.
Katagiri H, Yamada T, Oka Y. Adiposity and cardiovascular disorders: disturbance of the regulatory system consisting of humoral and neuronal signals. Circ Res. 2007;101(1):27–39. https://doi.org/10.1161/CIRCRESAHA.107.151621.
de Git KC, Adan RA. Leptin resistance in diet-induced obesity: the role of hypothalamic inflammation. Obes Rev. 2015;16(3):207–24. https://doi.org/10.1111/obr.12243.
Armitage JA, Burke SL, Prior LJ, Barzel B, Eikelis N, Lim K, et al. Rapid onset of renal sympathetic nerve activation in rabbits fed a high-fat diet. Hypertension. 2012;60(1):163–71. https://doi.org/10.1161/HYPERTENSIONAHA.111.190413.
Dragano NR, Haddad-Tovolli R, Velloso LA. Leptin, neuroinflammation and obesity. Front Horm Res. 2017;48:84–96. https://doi.org/10.1159/000452908.
Xue B, Thunhorst RL, Yu Y, Guo F, Beltz TG, Felder RB, et al. Central renin-angiotensin system activation and inflammation induced by high-fat diet sensitize angiotensin II-elicited hypertension. Hypertension. 2016;67(1):163–70. https://doi.org/10.1161/HYPERTENSIONAHA.115.06263.
Xue B, Yu Y, Zhang Z, Guo F, Beltz TG, Thunhorst RL, et al. Leptin mediates high-fat diet sensitization of angiotensin II-elicited hypertension by upregulating the brain renin-angiotensin system and inflammation. Hypertension. 2016;67(5):970–6. https://doi.org/10.1161/HYPERTENSIONAHA.115.06736.
De Souza CT, Araujo EP, Bordin S, Ashimine R, Zollner RL, Boschero AC, et al. Consumption of a fat-rich diet activates a proinflammatory response and induces insulin resistance in the hypothalamus. Endocrinology. 2005;146(10):4192–9. https://doi.org/10.1210/en.2004-1520.
•• Thaler JP, Yi CX, Schur EA, Guyenet SJ, Hwang BH, Dietrich MO, et al. Obesity is associated with hypothalamic injury in rodents and humans. J Clin Invest. 2012;122(1):153–62. https://doi.org/10.1172/JCI59660. The first evidence of increased mediobasal hypothalamic gliosis in obese humans by magnetic resonance imaging.
Douglass JD, Dorfman MD, Fasnacht R, Shaffer LD, Thaler JP. Astrocyte IKKβ/NF-κB signaling is required for diet-induced obesity and hypothalamic inflammation. Mol Metab. 2017;6(4):366–73. https://doi.org/10.1016/j.molmet.2017.01.010.
Tran DQ, Tse EK, Kim MH, Belsham DD. Diet-induced cellular neuroinflammation in the hypothalamus: mechanistic insights from investigation of neurons and microglia. Mol Cell Endocrinol. 2016;438:18–26. https://doi.org/10.1016/j.mce.2016.05.015.
Douglass JD, Dorfman MD, Thaler JP. Glia: silent partners in energy homeostasis and obesity pathogenesis. Diabetologia. 2017;60(2):226–36. https://doi.org/10.1007/s00125-016-4181-3.
Maldonado-Ruiz R, Fuentes-Mera L, Camacho A. Central modulation of neuroinflammation by neuropeptides and energy-sensing hormones during obesity. Biomed Res Int. 2017;2017:7949582. https://doi.org/10.1155/2017/7949582.
Dragano NRV, Solon C, Ramalho AF, de Moura RF, Razolli DS, Christiansen E, et al. Polyunsaturated fatty acid receptors, GPR40 and GPR120, are expressed in the hypothalamus and control energy homeostasis and inflammation. J Neuroinflammation. 2017;14(1):91. https://doi.org/10.1186/s12974-017-0869-7.
Valdearcos M, Robblee MM, Benjamin DI, Nomura DK, Xu AW, Koliwad SK. Microglia dictate the impact of saturated fat consumption on hypothalamic inflammation and neuronal function. Cell Rep. 2014;9(6):2124–38. https://doi.org/10.1016/j.celrep.2014.11.018.
Aguilar-Valles A, Inoue W, Rummel C, Luheshi GN. Obesity, adipokines and neuroinflammation. Neuropharmacology 2015;96(Pt A):124–134. https://doi.org/10.1016/j.neuropharm.2014.12.023.
Le Thuc O, Stobbe K, Cansell C, Nahon JL, Blondeau N, Rovère C. Hypothalamic inflammation and energy balance disruptions: spotlight on chemokines. Front Endocrinol (Lausanne). 2017;8:197. https://doi.org/10.3389/fendo.2017.00197.
Buckman LB, Hasty AH, Flaherty DK, Buckman CT, Thompson MM, Matlock BK, et al. Obesity induced by a high-fat diet is associated with increased immune cell entry into the central nervous system. Brain Behav Immun. 2014;35:33–42. https://doi.org/10.1016/j.bbi.2013.06.007.
Guillemot-Legris O, Muccioli GG. Obesity-induced neuroinflammation: beyond the hypothalamus. Trends Neurosci. 2017;40(4):237–53. https://doi.org/10.1016/j.tins.2017.02.005.
Gluck ME, Alonso-Alonso M, Piaggi P, Weise CM, Jumpertz-von Schwartzenberg R, Reinhardt M, et al. Neuromodulation targeted to the prefrontal cortex induces changes in energy intake and weight loss in obesity. Obesity (Silver Spring). 2015;23(11):2149–56. https://doi.org/10.1002/oby.21313.
Santisteban MM, Ahmari N, Carvajal JM, Zingler MB, Qi Y, Kim S, et al. Involvement of bone marrow cells and neuroinflammation in hypertension. Circ Res. 2015;117(2):178–91. https://doi.org/10.1161/CIRCRESAHA.117.305853.
Kim S, Zingler M, Harrison JK, Scott EW, Cogle CR, Luo D, et al. Angiotensin II regulation of proliferation, differentiation, and engraftment of hematopoietic stem cells. Hypertension. 2016;67(3):574–84. https://doi.org/10.1161/HYPERTENSIONAHA.115.06474.
Penn MS, Swaminath D. Novel role of bone marrow stem cells in systemic disease. Circ Res. 2015;117(2):119–20. https://doi.org/10.1161/CIRCRESAHA.117.306852.
Swirski FK, Nahrendorf M, Etzrodt M, Wildgruber M, Cortez-Retamozo V, Panizzi P, et al. Identification of splenic reservoir monocytes and their deployment to inflammatory sites. Science. 2009;325(5940):612–6. https://doi.org/10.1126/science.1175202.
Illán-Gómez F, Gonzálvez-Ortega M, Orea-Soler I, Alcaraz-Tafalla MS, Aragón-Alonso A, Pascual-Díaz M, et al. Obesity and inflammation: change in adiponectin, C-reactive protein, tumour necrosis factor-alpha and interleukin-6 after bariatric surgery. Obes Surg. 2012;22(6):950–5. https://doi.org/10.1007/s11695-012-0643.
Schmatz R, Bitencourt MR, Patias LD, Beck M, da C Alvarez G, Zanini D et al. Evaluation of the biochemical, inflammatory and oxidative profile of obese patients given clinical treatment and bariatric surgery. Clin Chim Acta 2017;465:72–79. https://doi.org/10.1016/j.cca.2016.12.012.
Williams DB, Hagedorn JC, Lawson EH, Galanko JA, Safadi BY, Curet MJ, et al. Gastric bypass reduces biochemical cardiac risk factors. Surg Obes Relat Dis. 2007;3(1):8–13. https://doi.org/10.1016/j.soard.2006.10.003.
Vilarrasa N, Vendrell J, Sánchez-Santos R, Broch M, Megia A, Masdevall C, et al. Effect of weight loss induced by gastric bypass on proinflammatory interleukin-18, soluble tumour necrosis factor-alpha receptors, C-reactive protein and adiponectin in morbidly obese patients. Clin Endocrinol. 2007;67(5):679–86. https://doi.org/10.1111/j.1365-2265.2007.02945.x.
Sell H, Poitou C, Habich C, Bouillot JL, Eckel J, Clément K. Heat shock protein 60 in obesity: effect of bariatric surgery and its relation to inflammation and cardiovascular risk. Obesity (Silver Spring). 2017;25(12):2108–14. https://doi.org/10.1002/oby.22014.
Gaborit B, Jacquier A, Kober F, Abdesselam I, Cuisset T, Boullu-Ciocca S, et al. Effects of bariatric surgery on cardiac ectopic fat: lesser decrease in epicardial fat compared to visceral fat loss and no change in myocardial triglyceride content. J Am Coll Cardiol. 2012;60(15):1381–9. https://doi.org/10.1016/j.jacc.2012.06.016.
Korner J, Punyanitya M, Taveras C, McMahon DJ, Kim HJ, Inabnet W, et al. Sex differences in visceral adipose tissue post-bariatric surgery compared to matched non-surgical controls. Int J Body Compos Res. 2008;6(3):93–9.
Toro-Ramos T, Goodpaster BH, Janumala I, Lin S, Strain GW, Thornton JC, et al. Continued loss in visceral and intermuscular adipose tissue in weight-stable women following bariatric surgery. Obesity (Silver Spring). 2015;23(1):62–9. https://doi.org/10.1002/oby.20932.
Tamez M, Ramos-Barragan V, Mendoza-Lorenzo P, Arrieta-Joffe P, López-Martínez S, Rojano-Rodríguez ME, et al. Adipocyte size and leptin receptor expression in human subcutaneous adipose tissue after Roux-en-Y gastric bypass. Obes Surg. 2017;27(12):3330–2. https://doi.org/10.1007/s11695-017-2930-0.
Torquati A, Wright K, Melvin W, Richards W. Effect of gastric bypass operation on Framingham and actual risk of cardiovascular events in class II to III obesity. J Am Coll Surg. 2007;204(5):776–82; discussion 82-3. https://doi.org/10.1016/j.jamcollsurg.2006.12.038.
Benotti PN, Wood GC, Carey DJ, Mehra VC, Mirshahi T, Lent MR, et al. Gastric bypass surgery produces a durable reduction in cardiovascular disease risk factors and reduces the long-term risks of congestive heart failure. J Am Heart Assoc. 2017;6(5) https://doi.org/10.1161/JAHA.116.005126.
Benraouane F, Litwin SE. Reductions in cardiovascular risk after bariatric surgery. Curr Opin Cardiol. 2011;26(6):555–61. https://doi.org/10.1097/HCO.0b013e32834b7fc4.
Mackey RH, Belle SH, Courcoulas AP, Dakin GF, Deveney CW, Flum DR, et al. Distribution of 10-year and lifetime predicted risk for cardiovascular disease prior to surgery in the longitudinal assessment of bariatric surgery-2 study. Am J Cardiol. 2012;110(8):1130–7. https://doi.org/10.1016/j.amjcard.2012.05.054.
Batsis JA, Sarr MG, Collazo-Clavell ML, Thomas RJ, Romero-Corral A, Somers VK, et al. Cardiovascular risk after bariatric surgery for obesity. Am J Cardiol. 2008;102(7):930–7. https://doi.org/10.1016/j.amjcard.2008.05.040.
Heneghan HM, Meron-Eldar S, Brethauer SA, Schauer PR, Young JB. Effect of bariatric surgery on cardiovascular risk profile. Am J Cardiol. 2011;108(10):1499–507. https://doi.org/10.1016/j.amjcard.2011.06.076.
Gloy VL, Briel M, Bhatt DL, Kashyap SR, Schauer PR, Mingrone G, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and meta-analysis of randomised controlled trials. BMJ. 2013;f5934:347.
Boido A, Ceriani V, Cetta F, Lombardi F, Pontiroli AE. Bariatric surgery and prevention of cardiovascular events and mortality in morbid obesity: mechanisms of action and choice of surgery. Nutr Metab Cardiovasc Dis. 2015;25(5):437–43. https://doi.org/10.1016/j.numecd.2015.01.011.
Adams TD, Davidson LE, Hunt SC. Weight and metabolic outcomes 12 years after gastric bypass. N Engl J Med. 2018;378(1):93–6. https://doi.org/10.1056/NEJMc1714001.
•• Sjöström L, Peltonen M, Jacobson P, Sjöström CD, Karason K, Wedel H, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307(1):56–65. https://doi.org/10.1001/jama.2011.1914. The Swedish Obese Study showed that over a period of 14 years bariatric surgery reduced cardiovascular deaths and cardiovascular events in obese persons.
Schauer PR, Bhatt DL, Kirwan JP, Wolski K, Aminian A, Brethauer SA, et al. Bariatric surgery versus intensive medical therapy for diabetes—5-year outcomes. N Engl J Med. 2017;376(7):641–51. https://doi.org/10.1056/NEJMoa1600869.
Randell EW, Twells LK, Gregory DM, Lester KK, Daneshtalab N, Dillon C, et al. Pre-operative and post-operative changes in CRP and other biomarkers sensitive to inflammatory status in patients with severe obesity undergoing laparoscopic sleeve gastrectomy. Clin Biochem. 2018;52:13–9. https://doi.org/10.1016/j.clinbiochem.2017.10.010.
Carbone F, Nulli Migliola E, Bonaventura A, Vecchié A, De Vuono S, Ricci MA, et al. High serum levels of C-reactive protein (CRP) predict beneficial decrease of visceral fat in obese females after sleeve gastrectomy. Nutr Metab Cardiovasc Dis. 2018; https://doi.org/10.1016/j.numecd.2018.01.014.
Trachta P, Dostálová I, Haluzíková D, Kasalický M, Kaválková P, Drápalová J, et al. Laparoscopic sleeve gastrectomy ameliorates mRNA expression of inflammation-related genes in subcutaneous adipose tissue but not in peripheral monocytes of obese patients. Mol Cell Endocrinol. 2014;383(1–2):96–102. https://doi.org/10.1016/j.mce.2013.11.013.
Hagman DK, Larson I, Kuzma JN, Cromer G, Makar K, Rubinow KB, et al. The short-term and long-term effects of bariatric/metabolic surgery on subcutaneous adipose tissue inflammation in humans. Metabolism. 2017;70:12–22. https://doi.org/10.1016/j.metabol.2017.01.030.
Tromba L, Tartaglia F, Carbotta S, Sforza N, Pelle F, Colagiovanni V, et al. The role of sleeve gastrectomy in reducing cardiovascular risk. Obes Surg. 2017;27(5):1145–51. https://doi.org/10.1007/s11695-016-2441-4.
Sturm W, Tschoner A, Engl J, Kaser S, Laimer M, Ciardi C, et al. Effect of bariatric surgery on both functional and structural measures of premature atherosclerosis. Eur Heart J. 2009;30(16):2038–43. https://doi.org/10.1093/eurheartj/ehp211.
Iannelli A, Anty R, Schneck AS, Tran A, Gugenheim J. Inflammation, insulin resistance, lipid disturbances, anthropometrics, and metabolic syndrome in morbidly obese patients: a case-control study comparing laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy. Surgery. 2011;149(3):364–70. https://doi.org/10.1016/j.surg.2010.08.013.
Arterburn D, Gupta A. Comparing the outcomes of sleeve gastrectomy and Roux-en-Y gastric bypass for severe obesity. JAMA. 2018;319(3):235–7. https://doi.org/10.1001/jama.2017.20449.
Murabito JM, Pedley A, Massaro JM, Vasan RS, Esliger D, Blease SJ, et al. Moderate-to-vigorous physical activity with accelerometry is associated with visceral adipose tissue in adults. J Am Heart Assoc. 2015;4(3):e001379. https://doi.org/10.1161/JAHA.114.001379.
Keating SE, Parker HM, Pavey TG, Baker MK, Caterson ID, George J, et al. Objectively quantified physical activity and sedentary behavior in predicting visceral adiposity and liver fat. J Obes. 2016;2016:2719014. https://doi.org/10.1155/2016/2719014.
McGrath S, Brazel D, Dugas L, Cao G, Durazo-Arvizu R, Luke A. Physical activity and central adiposity in a cohort of African-American adults. BMC Obes. 2017;4:34. https://doi.org/10.1186/s40608-017-0170-4.
Kay SJ, Fiatarone Singh MA. The influence of physical activity on abdominal fat: a systematic review of the literature. Obes Rev. 2006;7(2):183–200. https://doi.org/10.1111/j.1467-789X.2006.00250.x.
McTiernan A, Sorensen B, Irwin ML, Morgan A, Yasui Y, Rudolph RE, et al. Exercise effect on weight and body fat in men and women. Obesity (Silver Spring). 2007;15(6):1496–512. https://doi.org/10.1038/oby.2007.178.
Irwin ML, Yasui Y, Ulrich CM, Bowen D, Rudolph RE, Schwartz RS, et al. Effect of exercise on total and intra-abdominal body fat in postmenopausal women: a randomized controlled trial. JAMA. 2003;289(3):323–30.
Ismail I, Keating SE, Baker MK, Johnson NA. A systematic review and meta-analysis of the effect of aerobic vs. resistance exercise training on visceral fat. Obes Rev. 2012;13(1):68–91. https://doi.org/10.1111/j.1467-789X.2011.00931.x.
Slentz CA, Aiken LB, Houmard JA, Bales CW, Johnson JL, Tanner CJ, et al. Inactivity, exercise, and visceral fat. STRRIDE: a randomized, controlled study of exercise intensity and amount. J Appl Physiol (1985). 2005;99(4):1613–8. https://doi.org/10.1152/japplphysiol.00124.2005.
•• Gepner Y, Shelef I, Schwarzfuchs D, Zelicha H, Tene L, Yaskolka Meir A, et al. Effect of distinct lifestyle interventions on mobilization of fat storage pools: CENTRAL Magnetic Resonance Imaging Randomized Controlled Trial. Circulation. 2018;137(11):1143–57. https://doi.org/10.1161/CIRCULATIONAHA.117.030501. A moderate program of physical activity including 80% aerobic and 20% resistance training reduced visceral adipose tissue, while iso-caloric low-fat or Mediterranean/low-carbohydrate diets did not.
Nicklas BJ, Ambrosius W, Messier SP, Miller GD, Penninx BW, Loeser RF, et al. Diet-induced weight loss, exercise, and chronic inflammation in older, obese adults: a randomized controlled clinical trial. Am J Clin Nutr. 2004;79(4):544–51. https://doi.org/10.1093/ajcn/79.4.544.
Azarbal F, Stefanick ML, Assimes TL, Manson JE, Bea JW, Li W, et al. Lean body mass and risk of incident atrial fibrillation in post-menopausal women. Eur Heart J. 2016;37(20):1606–13. https://doi.org/10.1093/eurheartj/ehv423.
Lancaster GI, Febbraio MA. The immunomodulating role of exercise in metabolic disease. Trends Immunol. 2014;35(6):262–9. https://doi.org/10.1016/j.it.2014.02.008.
Rocha-Rodrigues S, Rodríguez A, Becerril S, Ramírez B, Gonçalves IO, Beleza J, et al. Physical exercise remodels visceral adipose tissue and mitochondrial lipid metabolism in rats fed a high-fat diet. Clin Exp Pharmacol Physiol. 2017;44(3):386–94. https://doi.org/10.1111/1440-1681.12706.
Ard JD, Gower B, Hunter G, Ritchie CS, Roth DL, Goss A, et al. Effects of calorie restriction in obese older adults: the CROSSROADS Randomized Controlled Trial. J Gerontol A Biol Sci Med Sci. 2017;73(1):73–80. https://doi.org/10.1093/gerona/glw237.
Chaston TB, Dixon JB. Factors associated with percent change in visceral versus subcutaneous abdominal fat during weight loss: findings from a systematic review. Int J Obes. 2008;32(4):619–28. https://doi.org/10.1038/sj.ijo.0803761.
Borel AL, Nazare JA, Smith J, Alméras N, Tremblay A, Bergeron J, et al. Visceral and not subcutaneous abdominal adiposity reduction drives the benefits of a 1-year lifestyle modification program. Obesity (Silver Spring). 2012;20(6):1223–33. https://doi.org/10.1038/oby.2011.396.
Thomas EL, Brynes AE, McCarthy J, Goldstone AP, Hajnal JV, Saeed N, et al. Preferential loss of visceral fat following aerobic exercise, measured by magnetic resonance imaging. Lipids. 2000;35(7):769–76.
Villeneuve N, Pelletier-Beaumont E, Nazare JA, Lemieux I, Alméras N, Bergeron J, et al. Interrelationships between changes in anthropometric variables and computed tomography indices of abdominal fat distribution in response to a 1-year physical activity-healthy eating lifestyle modification program in abdominally obese men. Appl Physiol Nutr Metab. 2014;39(4):503–11. https://doi.org/10.1139/apnm-2013-0270.
Myers J. Cardiology patient pages. Exercise and cardiovascular health. Circulation. 2003;107(1):e2–5.
Vartanian LR, Novak SA. Internalized societal attitudes moderate the impact of weight stigma on avoidance of exercise. Obesity (Silver Spring). 2011;19(4):757–62. https://doi.org/10.1038/oby.2010.234.
Williams EP, Mesidor M, Winters K, Dubbert PM, Wyatt SB. Overweight and obesity: prevalence, consequences, and causes of a growing public health problem. Curr Obes Rep. 2015;4(3):363–70. https://doi.org/10.1007/s13679-015-0169-4.
Phillips ML, Lewis MC, Chew V, Kow L, Slavotinek JP, Daniels L, et al. The early effects of weight loss surgery on regional adiposity. Obes Surg. 2005;15(10):1449–55. https://doi.org/10.1381/096089205774859353.
Ridker PM, Danielson E, Fonseca FA, Genest J, Gotto AM, Kastelein JJ, et al. Rosuvastatin to prevent vascular events in men and women with elevated C-reactive protein. N Engl J Med. 2008;359(21):2195–207. https://doi.org/10.1056/NEJMoa0807646.
Ridker PM, Narula J. Will reducing inflammation reduce vascular event rates? JACC Cardiovasc Imaging. 2018;11(2 Pt 2):317–9. https://doi.org/10.1016/j.jcmg.2017.10.001.
Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017;377(12):1119–31. https://doi.org/10.1056/NEJMoa1707914.
Ridker PM, MacFadyen JG, Everett BM, Libby P, Thuren T, Glynn RJ, et al. Relationship of C-reactive protein reduction to cardiovascular event reduction following treatment with canakinumab: a secondary analysis from the CANTOS randomised controlled trial. Lancet. 2018;391(10118):319–28. https://doi.org/10.1016/S0140-6736(17)32814-3.
Everett BM, Donath MY, Pradhan AD, Thuren T, Pais P, Nicolau JC, et al. Anti-inflammatory therapy with canakinumab for the prevention and management of diabetes. J Am Coll Cardiol. 2018; https://doi.org/10.1016/j.jacc.2018.03.002.
Acknowledgments
The authors are extremely grateful to Dr. Alan Tall for his careful reading of the manuscript and his insightful comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Hypertension and Obesity
Rights and permissions
About this article
Cite this article
Le Jemtel, T.H., Samson, R., Milligan, G. et al. Visceral Adipose Tissue Accumulation and Residual Cardiovascular Risk. Curr Hypertens Rep 20, 77 (2018). https://doi.org/10.1007/s11906-018-0880-0
Published:
DOI: https://doi.org/10.1007/s11906-018-0880-0