Abstract
Background
Obesity is an independent cardiovascular risk factor and a catalyst of other cardiovascular risk factors, such as hypertension, dyslipidemia, type 2 diabetes mellitus (DM2) and metabolic syndrome.
Methods
We analyzed cardiovascular risk in obese patients before and after sleeve gastrectomy (SG). To this end, we studied changes in body mass index (BMI), blood chemistry parameters that characterize the risk of atherosclerosis and instrumental parameters (objective markers of this risk), namely intima-media thickness (IMT) and flow-mediated dilation (FMD), the latter reflecting endothelial function. We also considered purely cardiac parameters—mitral annular plane systolic excursion (MAPSE) and tricuspid annular plane systolic excursion (TAPSE)—which describe cardiac risk more specifically than the ejection fraction. Alteration of one or more of these parameters determines an increase in cardiovascular morbidity and mortality.
Results
The results showed that weight loss, in patients undergoing SG, is accompanied by a reduced BMI and a marked improvement in blood chemistry, confirming what has already been shown in many other studies, but the most interesting finding was the effect of SG on the instrumental markers of atherosclerosis. In particular, carotid IMT was significantly reduced (p < 0.001) and FMD significantly improved. MAPSE and TAPSE also improved significantly at both follow-up assessments (p < 0.001).
Conclusions
This study suggests that SG should be considered from a broader perspective, i.e. as a weight loss treatment that also improves obesity-related morbidity and mortality, benefitting both the patient and, in an economic sense, the society as a whole.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is an independent cardiovascular risk factor as well as a catalyst of other cardiovascular risk factors, such as hypertension, dyslipidemia, type 2 diabetes mellitus (DM2) and metabolic syndrome [1, 2]. Obese individuals are at increased risk of atherosclerotic diseases [3], while patients with cardiovascular disease are often obese or overweight.
Obese patients are increasingly assessed for the presence of plurimetabolic syndrome, recognized as a leading cause of morbidity, mortality and impaired quality of life [4, 5].
All obesity-related diseases improve and, in the case of DM2 for example, often disappear if a person’s weight is normalized and especially if this result is maintained over time [6].
Bariatric surgery leads to rapid weight loss and body mass index (BMI) reduction in 50–60% of the cases, and many studies have shown significantly reduced mortality in bariatric patients [7, 8].
We investigated metabolic and instrumental changes in bariatric surgery patients, limiting our study, in this initial phase, to patients undergoing sleeve gastrectomy (SG), the technique most frequently used in our setting. SG, also known as vertical gastrectomy, involves dissection along the greater curvature and removal of the gastric fundus, leaving the antral-pyloric region and vagal innervation intact. Left with a drastically reduced stomach capacity, the patient feels full after ingesting even small amounts of food; the procedure also reduces the level of the ‘hunger hormone’ ghrelin [9].
The aim of this study was to record metabolic changes after SG, analyzing the results of blood tests and the behaviour of instrumental parameters recognized by the international scientific community as reliable for cardiovascular risk assessment. Numerous studies have confirmed their prognostic value [10–18].
Materials and Methods
The study, conducted at the Department of Surgical Sciences, “Sapienza” University of Rome, between January 2014 and December 2015, concerned 45 candidates for SG: 18 men and 27 women aged between 24 and 57 years, with a BMI of between 30 and 57.7 (Table 1). Exclusion criteria were insulin-dependent diabetes and overt cardiovascular disease. In the first case, patients, generally, are not obese and being the type 1 diabetes a cardiovascular risk factor could alter the results. In the second case, the alterations of the parameters could be derived from the underlying disease and not by obesity. Totally, 12 patients were excluded from the study. All the participants gave their informed consent, and IRB approval was obtained.
In all the subjects, we evaluated smoking habits, blood pressure (BP), the presence of DM2, lipid profile (triglycerides; total, LDL and HDL cholesterol), carotid intima-media thickness (IMT), flow-mediated dilation (FMD) (to evaluate endothelial function), ankle-brachial index (ABI), tricuspid annular plane systolic excursion (TAPSE) and mitral annular plane systolic excursion (MAPSE). Table 2 gives the reference values.
The echo-colour Doppler parameters collected have always been measured by the same operator. Carotid IMT was assessed by ultrasound examination, which was performed using a MyLab 70 (Esaote SpA) with 7.5 MHz linear probe, according to reported criteria [19]; IMT was measured bilaterally at the posterior wall of the common carotid artery, which was 1 cm from the bifurcation, and the highest value was used for analysis; values ≤0.8 mm were considered normal.
FMD was assessed according to the protocol of Corretti et al. [20]: a high-frequency (7.5 MHz) linear probe is used to visualize the brachial artery in a longitudinal section, near the elbow. The diameter of the artery is measured in basal conditions. A pneumatic cuff, inflated to a pressure higher than the subject’s systolic BP, is used to induce compression for 4–5 min, after which the cuff is deflated and the diameter of the artery is measured again at the following intervals: 20, 45 and 60 s, for up to 3 min. In most cases, maximum vasodilatation is reached 45–60 s after the test. FMD is calculated as the percentage difference between the maximum post-ischemic diameter, and the average basal diameter: FMD = [(post-ischemic diameter – basal diameter) / basal diameter] × 100. FMD values >9% were considered normal.
The ABI is the ratio of the systolic blood pressure measured at the ankle and the systolic blood pressure measured at the humeral artery and is normally between 0.9 and 1.3. We used tire sleeves appropriate in height and length to limb size. All the subjects underwent colour Doppler echocardiography performed with a 2.5 MHz sector probe (Esaote SpA) to study (1) TAPSE, an index of right ventricular systolic function, and (2) MAPSE, an index of the left ventricular systolic function. This information on ventricle longitudinal kinetics was acquired using an apical four-chamber view and applying the M-mode technique to the lines that pass through the side margins of the atrioventricular valves.
The instrumental investigations and blood tests were repeated 3 and 6 months after surgery, for comparison with the preoperative findings.
Statistical Analysis
The Shapiro-Wilk test showed that the instrumental and blood chemistry parameters were not normally distributed; therefore, appropriate non-parametric methods were used, in particular, Friedman’s one-way ANOVA by ranks. Correlations between continuous variables were determined by Spearman’s rho. The McNemar test for related samples (or Cochran’s Q test when appropriate) was used compare categorical data at the different time points.
The statistical comparison between diabetes/healthy and hypertensive/normal patients was performed separately at the three time points by means of Mann-Whitney U test for independent samples.
The level of significance was set at p < 0.05. The descriptive character of the analysis and the different aspects taken into consideration in the study prevent a straightforward application of Bonferroni correction for multiple testing. In any case, we reported the actual level of significance reached by any single test and these values are well below the Bonferroni corrected significance levels, and, most importantly, consistent to ‘strong effects’ in terms of ‘minimum Bayes factors’ [21, 22].
Results
The results of the study are summarized in Table 3. All the patients showed considerable weight loss, and thus marked BMI reduction, after SG. The BMI reduction, both from 0 to 3 months and from 3 to 6 months, was statistically significant (p < 0.001).
DM2 was present preoperatively in 44.4% of the patients; at 3 months, this rate was significantly lower (15.6%, p < 0.001); a further reduction (to 8.9%) was recorded at 6 months, although the difference, versus the rate at 3 months, was not significant.
Significant reductions were seen in all cholesterol measurements and in triglyceride values (p < 0.001) at both follow-ups, although the HDL cholesterol improvements were less marked.
Raised total cholesterol was found in 57.8% of the patients before surgery; post-operatively, hypercholesterolemia was found in 15.6% at 3 months and in 6.7% at 6 months. The difference between the preoperative and the 3-month values was significant (p < 0.001), while the further improvement, between 3 and 6 months, was not (p = 0.219).
Preoperatively, 71.1% of the patients had abnormal HDL cholesterol; this proportion was significantly smaller at 3 (35.6%, p < 0.001) and 6 months (13.3%, p = 0.002). LDL cholesterol was abnormal in 82.2% of the patients preoperatively, and in 57.8 and 26.7% at 3 and 6 months respectively. The difference between the baseline and the 3-month values was significant (p = 0.007) and the subsequent improvement even more so (p = 0.001).
Preoperatively, 60% of the patients had abnormal triglyceride levels; this rate improved after surgery, dropping to 33.3% at 3 months and 6.7% at 6 months. The difference between the baseline and 3-month values was significant (p < 0.001), as was the improvement between 3 and 6 months (p < 0.001).
Hypertension was found in 51% of the patients before surgery; this rate fell post-operatively, to 40% at 3 months and 28% at 6 months. The reduction in the number of hypertensives from baseline to 3 months was statistically significant (p = 0.016). The further reduction was not.
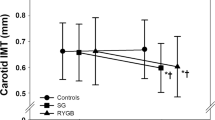
With regard to the instrumental parameters, 97.8% of the patients had an abnormal carotid IMT at baseline, 86.7% at 3 months and 66.7% at 6 months. The improvement at the first follow-up was not significant (p = 0.063), whereas it became significant at 6 months (p = 0.004).
While FMD values were abnormal in all the patients preoperatively, only 13% showed impaired endothelial function at 3 months and 2.2% at 6 months. The difference between the preoperative and 3-month assessments was significant (p = 0.001), at odds with the improvement recorded between 3 and 6 months was not (p = 0.101).
The ABI rating has never detected values outside the normal range although there was an improvement of the values in the post-operative period, but not statistically significant.
Although MAPSE and TAPSE were within the normal range throughout the study, these parameters still showed slight, but significant, increases at both follow-up assessments (p < 0.001), indicating an improvement in the systolic function of the two ventricles.
We looked for correlations between the presence of diabetes and the instrumental parameters IMT and FMD. Preoperatively, diabetes was correlated with abnormal FMD (p = 0.009) and IMT (p = 0.001); however, these correlations were no longer significant at either follow-up (Table 4).
The presence of hypertension was also significantly correlated with abnormal IMT (p = 0.001) and FMD (p = 0.009) preoperatively. At 3 months, it was correlated only with abnormal IMT (p = 0.006); at 6 months, this correlation was even stronger (p = 0.001) (Table 5).
Discussion
The American Heart Association classifies obesity as a major and modifiable risk factor for cardiovascular disease [1]. Obesity is, indeed, frequently associated with cardiovascular diseases, such as cerebral and coronary artery diseases and with metabolic disorders, such as dyslipidemia, insulin resistance and DM2, also known as major atherosclerosis risk factors [23, 24].
Weight loss surgery has proved to reduce the incidence of comorbidities and its associated cardiovascular events. Several studies have shown hormonal and hemodynamic changes after bariatric surgery and the beneficial effects on long-term survival in obese patients [7, 8]. Originally proposed as the first stage of a hybrid malabsorptive procedure, over a very short period of time, SG has become an extremely popular bariatric procedure among both patients and surgeons. SG is associated with a high rate of remission of DM2 and other obesity-associated comorbidities, including hypertension, hyperlipidemia and sleep apnea. [9, 25].
In a recent paper published by Lupoli et al., the authors performed a meta-analysis evaluating changes in IMT, FMD and nitroglycerin-mediated dilatation (NMD) in obese patients after bariatric and metabolic surgery. Only ten articles met the inclusion criteria, and 314 obese patients were analyzed. The results highlighted how bariatric surgery is associated with a significant improvement of structural and functional markers of atherosclerosis and beneficial effects on subclinical atherosclerosis and on endothelial function. A significant reduction of carotid IMT (−0.17 mm), accompanied by a 5.6% increase in FMD, was also reported. However, the authors have identified some limitations of the study design: different types of bariatric surgery represent potential source of bias (the majority of the patients included undergoing gastric bypass); in addition, there was a generally high heterogeneity between articles [26].
The present study reports the impact of SG on comorbidities in addition to its effects on carotid IMT, FMD, ABI, TAPSE and MAPSE as instrumental parameters for cardiovascular risk assessment.
To our knowledge, no significant data on endothelial dysfunction after SG alone is currently available; however, certain publications have analyzed analogous data deriving from different surgical procedures (Roux-en-Y gastric bypass, SG, gastric banding [26, 27]). We analyzed 45 obese patients preoperatively and 3 and 6 months after the operation. The interest on the first post-operative period is related to the assumption that SG is not only a restrictive procedure; on the contrary, its post-operative changes are due to an intrinsic neurohormonal effect which is considered to be independent from the weight loss. In fact, we registered a dramatic remission of DM2 (65%) already noted on the third post-operative month differently from the nadir weight, which decreases later on (i.e. 12–18 months). Few papers analyze the early results of bariatric surgery on artery function. Domienik-Karłowicz et al. evaluated 40 obese patients before and 6 months after surgery the pulse wave velocity, FMD and NMD. The FMD (%) is reported to increase from 12.83 ± 5.15 to 17.52 ± 5.50 after surgery (p < 0.0001). [27] In our study, we registered an important amelioration of FMD rapidly at the third post-operative month while the improvement recorded between 3 and 6 months was not significant (p = 0.101). Similarly to DM2, a hormonal mechanism seems to be involved in inducing changes on endothelium functions.
Nevertheless, the normalization of carotid IMT was statistically significant after 6 months from SG.
Nowadays, we have non-invasive instrumental markers, namely IMT and FMD, capable of detecting, defining and monitoring this risk and documenting its reduction. Increased arterial IMT, especially carotid IMT, is associated with coronary lesions and predictive of cardiovascular events [14–30]. Ongoing research has shown it to be associated with cognitive disorders in cardiovascular patients [31].
FMD is an index of arterial function. The vascular endothelium is an actual organ that performs many functions: anti-inflammatory, antithrombotic, anticoagulatory, antihypertrophic and, especially, vasomotor. The latter function depends on the capacity of endothelial cells, which is subjected to an ischemic stimulus, to produce nitric oxide (NO), which induces endothelium-dependent vasodilation (FMD) of the artery. Endothelial dysfunction is a crucial factor in atherogenesis, and its prognostic value is high [32, 33]. FMD and IMT are normalized after SG in our study, at both follow-ups. These results suggest that FMD could be a useful early marker of cardiovascular risk, while IMT could serve as a late marker, probably indicative of a stabilization of this risk.
MAPSE and TAPSE were normal at baseline in the entire sample, partly because patients with heart disease were excluded; these parameters, nevertheless, improved significantly after SG, demonstrating unequivocally that weight loss improves cardiac function.
We found statistically significant correlations between hypertension and instrumental parameters, especially in IMT—thickening probably constitutes the reaction of the intima and media to the hypertensive insult on the arterial wall. The increase in IMT is age related, which supports the idea that IMT is a late marker of cardiovascular risk, which depends on the duration of exposure to hypertension. FMD, which significantly correlated with hypertension before surgery, showed no significant relationships after SG, either with hypertension or blood chemistry values. We believe this can be explained by the speed with which both FMD and lipid/blood sugar profiles were normalized after SG.
With the exception of HDL cholesterol (higher in women both before and after SG), we found no significant gender differences in blood chemistry. This absence of gender differences needs to be substantiated in a larger population. With regard to the HDL cholesterol values in the women, it should be noted that most of the women in the study were premenopausal and thus enjoyed the beneficial effects of oestrogen on lipid metabolism [34].
Conclusions
The initial results of our ongoing research show that bariatric surgery is important not only in weight reduction but also in correcting cardiovascular risk factors and reducing the risk of death. SG should, therefore, probably be considered from a broader perspective, i.e. as a weight loss treatment that can also improve obesity-related morbidity and mortality, benefitting both the patient and, in an economic sense, the society as a whole. The instrumental markers described, which were used in combination with blood tests, provide an objective method (inexpensive and readily available) for evaluating cardiovascular risk in the obese, for documenting its reduction after SG, and for monitoring the outcome over time. It nevertheless requires careful execution (according to the guidelines) and standardization.
References
Eckel RH, Krauss RM. American Heart Association call to action: obesity as a major risk factor for coronary heart disease. AHA Nutrition Committee. Circulation. 1998;97(21):2099–100.
Sowers JR. Obesity as a cardiovascular risk factor. Am J Med. 2003;115(Suppl 8A):37S–41S.
Grundy SM. Obesity, metabolic syndrome, and cardiovascular disease. J Clin Endocrinol Metab. 2004;89:2595–600.
Hubert HB, Feinleib M, McNamara PM, et al. Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation. 1983;67(5):968–77.
Chang HW, Li YH, Hsieh CH, et al. Association of body mass index with all-cause mortality in patients with diabetes: a systemic review and meta-analysis. Cardiovasc Diagn Ther. 2016 Apr;6(2):109–19.
Ghanim H, Aljada A, Hofmeyer D, et al. Circulating mononuclear cells in the obese are in a proinflammatory state. Circulation. 2004;110(12):1564–71.
Boido A, Ceriani V, Cetta F, et al. Bariatric surgery and prevention of cardiovascular events and mortality in morbid obesity: mechanisms of action and choice of surgery. Nutr Metab Cardiovasc Dis. 2015 May;25(5):437–43.
Goday A, Benaiges D, Parri A, et al. Can bariatric surgery improve cardiovascular risk factors in the metabolically healthy but morbidly obese patient? Surg Obes Relat Dis. 2014 Sep-Oct;10(5):871–6.
Casella G, Abbatini F, Calì B, et al. Ten-year duration of type 2 diabetes as prognostic factor for remission after sleeve gastrectomy. Surg Obes Relat Dis. 2011 Nov-Dec;7(6):697–702.
Aloi M, Tromba L, Di Nardo G, et al. Premature subclinical atherosclerosis in pediatric inflammatory bowel disease. J Pediatr. 2012 Oct;161(4):589–94.
Aloi M, Tromba L, Rizzo V, et al. Aortic intima-media thickness as an early marker of atherosclerosis in children with inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2015 Jul;61(1):41–6.
Berni A, Giuliani A, Tartaglia F, et al. Effect of vascular risk factors on increase in carotid and femoral intima-media thickness. Identification of a risk scale. Atherosclerosis. 2011;216:109–14.
Verma S, Buchanan MR, Anderson TJ. Endothelial function testing as a biomarker of vascular disease. Circulation. 2003;108:2054–9.
Chambless LE, Heiss G, Folsom AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Epidemiol. 1997;146:483–94.
O’Leary DH, Polak JF, Kronmal RA, et al. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. 1999 Jan 7;340(1):14–22.
Adel W, Roushdy AM, Nabil M. Mitral annular plane systolic excursion-derived ejection fraction: a simple and valid tool in adult males with left ventricular systolic dysfunction. Echocardiography. 2016 Feb;33(2):179–84.
Matos J, Kronzon I, Panagopoulos G, et al. Mitral annular plane systolic excursion as a surrogate for left ventricular ejection fraction. J Am Soc Echocardiogr. 2012 Sep;25(9):969–74.
Nguyen T, Cao L, Movahed A. Altered right ventricular contractile pattern after cardiac surgery: monitoring of septal function is essential. Echocardiography. 2014 Oct;31(9):1159–65.
Allan PL, Mowbray PI, Lee AJ, et al. Relationship between carotid intima-media thickness and symptomatic and asymptomatic peripheral arterial disease. The Edinburgh Artery Study. Stroke. 1997 Feb;28(2):348–53.
Corretti MC, Anderson TJ, Benjamin EJ, et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol. 2002;39:257–65.
Nuzzo R. Scientific method: statistical errors. Nature. 2014 Feb 13;506(7487):150–2.
Goodman SN. Of P-values and Bayes: a modest proposal. Epidemiology. 2001;12(3):295–7.
Maggio CA, Pi-Sunyer FX. The prevention and treatment of obesity. Application to type 2 diabetes. Diabetes Care. 1997;20:1744–66.
Keaney Jr JF, Larson MG, Vasan RS, et al. Obesity and systemic oxidative stress: clinical correlates of oxidative stress in the Framingham Study. Arterioscler Thromb Vasc Biol. 2003;23(3):434–9.
Cavarretta E, Casella G, Calì B, et al. Cardiac remodeling in obese patients after laparoscopic sleeve gastrectomy. World J Surg. 2013 Mar;37(3):565–72.
Lupoli R, Di Minno MN, Guidone C, et al. Effects of bariatric surgery on markers of subclinical atherosclerosis and endothelial function: a meta-analysis of literature studies. Int J Obes. 2016 Mar;40(3):395–402.
Domienik-Karłowicz J, Lisik W, Rymarczyk Z, et al. The short-term effect of bariatric surgery on non-invasive markers of artery function in patients with metabolic syndrome. Diabetol Metab Syndr. 2015 Sep 16;7:76.
Lind L, Zethelius B, Sundbom M, et al. Vasoreactivity is rapidly improved in obese subjects after gastric bypass surgery. Int J Obes. 2009;33:1390–5.
Tschoner A, Sturm W, Gelsinger C, et al. Long-term effects of weight loss after bariatric surgery on functional and structural markers of atherosclerosis. Obesity (Silver Spring). 2013;21:1960–5.
Matthias W, Lorenz MD, et al. Prediction of clinical cardiovascular events with carotid IMT. A systematic review and meta-analysis. Circulation. 2007;115:459–67.
Frazier DT, Seider T, Bettcher BM, et al. The role of carotid intima-media thickness in predicting longitudinal cognitive function in an older adult cohort. Cerebrovasc Dis. 2014;38(6):441–7.
Widlansky ME, Gokce N, Keaney F, et al. The clinical implications of endothelial dysfunction. J Am Coll Cardiol. 2003;42:1149–60.
Farb MG, Tiwari S, Karki S, et al. Cyclooxygenase inhibition improves endothelial vasomotor dysfunction of visceral adipose arterioles in human obesity. Obesity (Silver Spring). 2014 Feb;22(2):349–55.
Tromba L, Tartaglia F, Blasi S, et al. Is carotid stenosis in women a gender-related condition? J Women’s Health (Larchmt). 2016;25(4):348–54.
Acknowledgments
Thanks to Mrs. Catherine Wrenn for her assistance and for the translation of the paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Human Rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
An erratum to this article is available at http://dx.doi.org/10.1007/s11695-016-2456-x.
Rights and permissions
About this article
Cite this article
Tromba, L., Tartaglia, F., Carbotta, S. et al. The Role of Sleeve Gastrectomy in Reducing Cardiovascular Risk. OBES SURG 27, 1145–1151 (2017). https://doi.org/10.1007/s11695-016-2441-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-016-2441-4