Abstract
Notwithstanding the presence of hypertension, obstructive sleep apnea, or both, obesity is associated with increased left ventricular (LV) mass. The effects of bariatric surgery on LV mass have been sparsely investigated by M-mode and two-dimensional (2D) echocardiography. Overall, Roux-en-Y gastric bypass, adjustable gastric banding, and sleeve gastrectomy reduce LV mass. However, the reduction in LV mass is extremely variable. Besides duration and severity of obesity, presence of hypertension, obstructive sleep apnea or both, and type of surgical procedures, the inaccuracy of M-mode and 2D echocardiography for assessment of LV mass contributes to the variable effects of bariatric surgery on LV mass. Three-dimensional (3D) echocardiography may obviate the limitations of M-mode 2D echocardiography for assessment of LV mass and allow an accurate appraisal of the effects of bariatric surgery on LV mass.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Obesity-associated left ventricular hypertrophy (LVH) has been extensively reviewed [1, 2, 3•, 4]. At variance with the conventional wisdom that correlates obesity with eccentric LVH, concentric LVH is now thought to be more prevalent than eccentric LVH in obese patients without hypertension or obstructive sleep apnea [5,6,7]. The effects of bariatric surgery on left ventricular mass (LVM) have been mostly reported after Roux-end-Y gastric bypass (RYGB) or adjustable gastric banding (AGB) surgery [8,9,10,11,12,13]. The most consistent effect of RYGB and AGB on the left ventricle is a reduction in LVM [12,13,14]. Reduction of LVM is clinically relevant, as it is associated with a lower cardiovascular risk independent of blood pressure (BP) changes [15,16,17]. Laparoscopic sleeve gastrectomy (LSG) is currently the most commonly performed surgical procedure for weight loss [18, 19]. It is easier to perform than RYGB and results in greater loss of body weight than laparoscopic AGB (LAGB) [20]. Because LSG has only recently emerged as the preferred bariatric surgical procedure, few reports are available regarding its effects on LV structure and function [21,22,23,24,25,26,27].
This review focuses on (1) the phenotypes and mechanisms of LV remodeling in obesity, (2) the effects of LSG and other bariatric surgical procedures on LVM in obesity, and (3) the limitations of two-dimensional (2D) echocardiography and increasing interest in real-time automated three-dimensional (3D) echocardiography for measurement of LVM as well as phenotypic classification of LVH in obesity.
LV Remodeling in Obesity
Pressure, volume, or pressure and volume cardiac overload alter LV structure and function, a process that is commonly referred to as LV remodeling [28]. Two-dimensional or 3D echocardiography allows serial measurements of LVM and geometry to assess progression of LV remodeling [29]. In contrast to CT angiography, 2D or 3D echocardiography does not expose patients to radiation, is less time consuming, and costs lower than cardiac magnetic resonance imaging (MRI) study. Echocardiographically, LVM is derived from linear measurements of LV end diastolic dimension (LVEDD) and LV posterior and septal wall thickness at end diastole (PWT, SWT) according to the formula: LVM (gram) = 0.8 × 1.04 × [(LVEDD + PWT + SWT) 3 − LVEDD3] [30]. Traditionally, LVM is normalized to body surface area (BSA) to derive the LVM index (LVMI). LVH is defined as an LVMI >115 g/m2 in men and >95 g/m2 in women. Further characterization into concentric or eccentric LVH is based on an index of LV concentricity known as relative wall thickness (RWT) which is the ratio of 2 × PWT over LVEDD. In the presence of LVH, an RWT >0.42 suggests concentric hypertrophy, while RWT ≤0.42 suggests eccentric hypertrophy. In obese patients, the prevalence of LVH depends on whether LVM is indexed to BSA, or to height [1]. As BSA depends on body weight, indexing LVM to BSA attenuates the effects of obesity on LVM. Thus, LVM is preferably indexed to height2.7 or to height1.7 in obese patients. The exponent that best identifies LVM as a cardiovascular risk marker in obese patients is 1.7 [31].
Nearly three decades ago, measurements of RWT and LVM by 2D-guided M-mode echocardiography led to description of four patterns of LV remodeling in patients with hypertension (HTN) as detailed in Table 1 [32•]. By providing direct measurements of LVM and volume, cardiac MRI has allowed sub-classification of eccentric LVH into indeterminate and dilated phenotypes and of concentric LVH into non-dilated and phenotypes (Table 2) [33••]. Thus, a 4-tiered classification of LVH has been proposed, wherein both concentric and eccentric LVH are further sub-divided based on the presence or absence of LV dilation [34].
The clinical implications of the 4-tiered classification of LVH were evaluated in the Campana Salute Network (CSN) registry of 8848 hypertensive patients [35]. Forty-four percent of patients were women and 42% were obese. The LV phenotypes (derived from measurements of LVM and volume by 2D echocardiography) and their prevalence are detailed in Table 3. Patients with non-dilated concentric LVH and with non-dilated and dilated eccentric LVH had a two- to nine-fold higher risk of cardiac events than patients with normal LV. Patients with dilated concentric LVH were free of significant cardiovascular risk. The 4-tiered classification of LVH identified hypertensive patients with a low risk of all cause or cardiovascular mortality in the Losartan Intervention for Endpoint reduction (LIFE) study [36]. Patients with eccentric non-dilated LVH were at lower risk of all cause or cardiovascular mortality, whereas patients with eccentric dilated LVH and concentric non-dilated and dilated LVH were at higher risk [36]. Lastly, the predictive value of the 4-tiered classification of LVH was confirmed in 2377 adults aged ≥65 years from the Cardiovascular Health Study over a 10-year follow up period [37]. In summary, addition of 2D-guided M-mode echocardiography derived LVM and volume improved cardiovascular risk prediction over that derived from standard scores.
When LVM is indexed to height2.7 or height1.7, an increased prevalence of LVH in obesity becomes apparent. The prevalence of LVH steadily increases with BMI ranging from 13% in normotensive obese individuals to 69% in morbidly obese individuals with BMI ≥50 kg/m2 [11, 38]. Severe obesity as defined by a BMI ≥35 kg/m2 was initially linked to LV dilation [38, 39]. The hemodynamic load and neuro-hormonal activation that accompany severe obesity were thought to promote LV dilation [38]. Subsequently, the LVM-to-volume ratio was correlated with BMI, waist circumference, and fat mass (FM) in 5098 participants in the Multi-Ethnic Study of Atherosclerosis (MESA), with a stronger association in men than in women [40•, 41]. The increase in LVM-to-volume ratio was due to a disproportionate rise in LVM compared to LV volume. Accordingly, a new paradigm that associates obesity to concentric LV remodeling was proposed [6, 42, 43]. The new paradigm was confirmed in 4343 elderly participants without overt cardiovascular diseases in the ARIC (Atherosclerosis Risk in Communities) study [44]. In the biracial cohort of this study, obesity was associated with an increase in LVM and a relatively smaller increase in LV diameter. Cardiac remodeling resulted in impaired LV function in women but not in men [44]. Further, BMI was reported to be the only significant independent predictor of LVM indexed to height in 400 male firefighters [45]. Lastly, obesity independently increased the risk of LVH in 4290 hypertensive participants in the CSN registry [46].
The relative contribution of total body weight (TBW), fat free mass (FFM), and fat mass (FM) to LVM and LV function was recently investigated in 1189 participants in the Study of Health in Pomerania (SHIP) with a follow up period of 5 years [47]. Changes in LVM were shown to depend exclusively on changes in TBW and FM. An increase in FM was associated with LV concentric remodeling, while increases in TBW and FFM were associated with LV eccentric remodeling. Thus, body composition, and not total body weight, appears to determine the pattern of LV remodeling in obese patients.
Mechanisms of LV Remodeling in Obesity
Whether concentric or eccentric LV remodeling/LVH is the more prevalent phenotype in obesity remains an unresolved issue [3•]. The effects of duration of obesity and distribution of adipose tissue on LVM are difficult to estimate due to confounders, including HTN, obstructive sleep apnea, and oxidative stress that are frequently present in obese individuals [5, 48]. Overall, the mechanisms underlying LVH in obesity can be attributed to hemodynamic and non-hemodynamic factors (Fig. 1).
In addition to obesity-related renin-angiotensin-aldosterone and sympathetic nervous system activation, the high sodium load that accompanies high caloric intake tends to increase central blood volume, stroke volume, and cardiac output, and thereby promotes eccentric LVH [49]. Co-morbidities like HTN and obstructive sleep apnea add pressure overload to volume overload in obese patients, thereby promoting the concentric LVH phenotype [50]. While the concentric LVH phenotype does occur in obese patients free of co-morbidities [51, 52••], it is much more prevalent when obesity is associated with HTN. The effects of obesity and HTN on LVM are additive and interactive. Thus, in order to achieve effective LVH regression, therapy should target both weight loss and BP reduction in obese patients with HTN [1, 53•]. Similarly, all of the components of the metabolic syndrome (HTN, dyslipidemia, glucose intolerance, and obesity) contribute to increased LVM and need to be addressed in order to achieve substantial LVH regression [54].
Regional fat distribution is a key determinant of the LV remodeling phenotype in obesity [55]. Concentric LVH is linked to the amount of visceral adipose tissue (VAT) [41, 52••, 53•, 55]. Cardiac MRI assessment showed that concentric LV remodeling and VAT area are significantly related after adjustment for age, sex, ethnic background, HTN, diabetes, and lean body mass [52••]. Persistent elevation of systolic BP and reduced BP variability are associated with VAT and thereby tend to promote concentric LVH [56]. Lastly, both LVM and the amount of epicardial adipose tissue (EAT) increase with BMI [57,58,59]. However, the correlation between EAT and LVM is closer than that between LVM and BMI [57,58,59]. The precise mechanism delineating the contribution of EAT to LVH remains to be investigated.
Endocrine and paracrine release of inflammatory cytokines, angiotensin II, leptin, and adipokines by VAT also fosters development of concentric LVH in obese individuals [52••]. Macrophages infiltrate VAT and secrete large amounts of pro-inflammatory cytokines that, in turn, affect LV function and adverse remodeling [60, 61]. After adjusting for BMI and waist circumference, VAT remains significantly associated with C-reactive protein, interleukin-6, isoprostanes (marker of oxidative stress), and monocyte chemotractant protein-1 [62]. Further, the association between hyperglycemia/insulin resistance and LVH is primarily mediated by elevated BMI [63].
LV Mass After Laparoscopic Sleeve Gastrectomy
LSG has only gained wide acceptance as preferred surgical procedure for weight loss in the past few years. As a result, the effect of LSG on LV has not yet been extensively evaluated. The published literature provides an assessment of LVM post LSG in only 132 patients. Five single centers obtained 2D echocardiography and clinical parameters at baseline and at 6 to 12 months after LSG in groups of 8–51 patients [21,22,23,24,25]. All patients were BMI ≥35 kg/m2 at baseline, and mean LV ejection fraction (LVEF) was 60% (range 55–63). BMI decreased from 46.6 kg/m2 at baseline to 33.4 kg/m2 at 6–12 months after LSG. LVM, derived by the Penn Convention [64], decreased from 218.4 to 181.4 g, an average reduction of 15% (7–21%). In four of the five studies, LSG did not significantly alter LVEF, with increases in LVEF ranging from 1.3 to 3.3% [21,22,23, 25]. A 10% LVEF increase was reported in the only study that specifically enrolled obese patients with poorly controlled diabetes [24]. In this study, average HbA1c improved from 9.2% at baseline to 6.7% at 12 months following LSG. Only two of these five studies reported LV end diastolic volume (LVEDV) before and after LSG [22, 23]. Following LSG, LVEDV decreased from 126 to 119 mL and from 147 to 143 mL, respectively [22, 23]. All studies reported improvement in LV diastolic function after LSG, but none accounted for changes in cardiac loading conditions after LSG. The heterogeneity of 2D echocardiographic LV measurements and patient populations in these five studies precludes any attempt at meta-analysis.
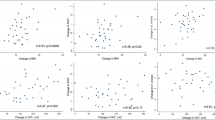
LVM was evaluated by 3D echocardiography at baseline and after bariatric surgery in 52 patients, of whom 18 underwent LSG and 34 underwent laparoscopic RYGB (LRYGB) [26]. BMI decreased by 12 and 10 kg/m2 after LSG and LRYGB, respectively. LSG decreased LVM from 115 to 99 g and LVEDV from 170 to 123 mL, while increasing LVEF from 63 to 68%. LSG and LRYGB had similar effects on LVM, LVEF, and LVEDV.
The effects of LSG on LV remodeling were recently assessed in 53 morbidly obese patients by 3D echocardiography [27]. Mean age and BMI were 37 years and 49 kg/m2, respectively. Women comprised 62% of the patient population. LV measurements were obtained at baseline and 6 months after LSG. LVM decreased from 55 to 44 g/height2.7, while LVEF increased from 60 to 68%. LVEDV decreased from 146 to 122 mL. LVEDV and LVM at baseline and LVM after LSG were significantly greater in men than women.
In summary, few studies have evaluated the effects of LSG on LVM. Preliminary experience indicates that 3D echocardiography provide more detailed assessment of LV structure and function than 2D echocardiography. The improvement in LV performance after bariatric surgery in patients who were evaluated with 3D echocardiography supports the view that the obesity-related decrease in LV systolic performance is reversible.
LV Mass After Gastric Bypass and Adjustable Banding
In 2013, Cuspidi et al. and Grapsa et al. reviewed the quantitative data on LV structure and/or function after bariatric surgery [4, 13]. Cuspidi et al. selected 23 reports for systematic review and meta-analysis [13]. The surgical procedures were RYGB, AGB, or vertical banded gastroplasty (VBG) in 21 of the 23 reports. Absolute LVM was available in 13 reports, and LVM indexed to height2.7 in 8 reports. The decrease in absolute LVM averaged 33.6 g ranging from 13 to 63 g. While they conclude to an overall beneficial effect of bariatric surgery on LVM, Cuspidi et al. drew attention to the variable effects of bariatric surgery on LVM. They attributed the variability to the limited accuracy of 2D echocardiography for measurement of LVM, to differences in duration of obesity and follow up, as well as in pre-operative LVM and BMI, and in the various surgical procedures themselves [13]. Reviewing 11 studies that assessed the effect of bariatric surgery on LVM by 2D echocardiography, Grapsa et al. confirmed that LVM decreases after bariatric surgical procedures [4]. Nevertheless, these authors advocated for more precise measurement of LV structure and function than 2D echocardiography allows [4]. To put the bariatric surgery data in perspective, antihypertensive therapy for a mean duration of 67 months decreased LVM by 9 g/m2.7 in the 2173 patients of the Campania Salute Network (CSN) [65].
A decrease in LVM from 192 to 146 g over a period of 15 months after RYGB was recently reported in 37 young patients [63]. The decrease in LVM was significantly related to reductions in BMI (r = 0.53, p < 0.001) and VA (r = 0.47, p < 0.005), whereas improvement in insulin resistance (assessed by homeostasis computer modeling) was only related to the reduction in VAT [66]. The mechanisms that mediate LVM regression after bariatric surgery are being actively investigated [67]. Weight loss-induced hemodynamic alterations including reductions in cardiac work load, plasma volume, and BP contribute to lower LVM. Bariatric surgery may also lower LVM by modulating release of adipocyte hormones such as leptin, resistin, and adiponectin [60, 67]. The close correlation of LVM regression with change in BMI implies weight loss-induced hemodynamic alterations as predominant mechanisms of LVM regression [9]. On another hand, the continued decline of LVM without further decrease in BMI suggests that non-hemodynamic factors factors contribute to the decrease in LVM after bariatric surgery [10]. By providing accurate and relatively inexpensive measurements of LV structure and function, 3D echocardiography, in conjunction with serial determinations of BP and serum levels of adipocyte hormones, may allow to ascertain the relative contribution of hemodynamic factors and VAT hormones to LVM regression after bariatric surgery.
LV Mass by 2D and 3D Echocardiography
By convention, LVM is measured at the end of diastole. By 2D-guided M-mode echocardiography, LVM is derived from linear measurements of the LV as previously mentioned. By 2D echocardiography, LVM can also be derived from linear measurements of LV minor radius (b), the distance from the minor axis to the endocardium of the LV apex (a), the distance from the minor axis to the mitral plane (d), and LV wall thickness (t) according to the truncated ellipsoid formula LVM = 1.04 π{(b + t).[2/3 (a + t) + d—d 3/3(a + t)2 − b 2[2/3a + d − d 3/3a 2]} [68].
By 3D echocardiography, LVM is derived from the difference between LV epicardial and endocardial volumes. LV mass is equal to (LV epicardial − LV endocardial volume) × 1.05 g [68]. In contrast to M mode and 2D echocardiography, 3D echocardiography measures LVM without making any geometric assumptions [68]. 3D echocardiography is particularly suited for monitoring the LV remodeling process. 2D echocardiography with fixed geometric assumptions cannot account for changes in LV geometry with time, intervention, or both. Time-consuming data acquisition and data analysis initially thwarted the adoption of 3D echocardiography for evaluation of LV volumes [69]. The development of matrix array transducer and novel automated software has greatly facilitated full LV volume quantification by real-time 3D echocardiography [70]. Automated algorithm-derived LV volumes by 3D echocardiography have been validated against cardiac MRI [71]. 3D echocardiography slightly underestimates LV volume due to poor differentiation between the compacted myocardium and trabeculae, which is a greater issue in systole than in diastole [71]. However, quantifications of LVM by real-time 3D echocardiography and cardiac MRI are in high agreement [72].
Whether M-mode and 2D echocardiography provide accurate measurements of LVM has been previously questioned [34]. Poor echocardiographic windows in obese patients and geometric assumptions make it technically difficult to derive accurate LV volumes and mass by M-mode and 2D echocardiography. M-mode echocardiography overestimates LVM as the result of unintended oblique cuts, and 2D echocardiography underestimates LVM as the result of foreshortening of apical views [73,74,75]. M-mode echocardiography could have contributed to the high prevalence of eccentric LV remodeling in obesity due to overestimation of LV end diastolic dimension [76]. When assessed by MRI, the gold standard imaging technique, hyperglycemia/insulin resistance have consistent effects on cardiac function and structure [63] However, when assessed by 2D echocardiography, hyperglycemia/insulin resistance have markedly disparate effects that raise concerns about the accuracy of this imaging technique for assessment of cardiac function and structure [63].
Conclusion
In summary, M-mode and 2D echocardiography provide an incomplete and sometimes inaccurate assessment of LV remodeling in obesity. Further, assessment of LVM after bariatric surgery is hampered by changes in LV geometry that are not directly accounted for by M-mode and 2D echocardiography. In contrast, real-time 3D echocardiography appears particularly well suited for assessing LVM and function after bariatric surgery, as it does not rely on geometric assumptions to quantify LVM. Serial measurements of BP and LVM may help delineate the mechanisms that mediate LVM regression after bariatric surgery.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Woodiwiss AJ, Norton GR. Obesity and left ventricular hypertrophy: the hypertension connection. Curr Hypertens Rep. 2015;17(4):539. doi:10.1007/s11906-015-0539-z.
Aurigemma GP, de Simone G, Fitzgibbons TP. Cardiac remodeling in obesity. Circ Cardiovasc Imaging. 2013;6(1):142–52. doi:10.1161/CIRCIMAGING.111.964627.
• Alpert MA, Omran J, Bostick BP. Effects of obesity on cardiovascular hemodynamics, cardiac morphology, and ventricular function. Curr Obes Rep. 2016;5(4):424–34. doi:10.1007/s13679-016-0235-6. Historical perspectives on obesity and cardiac morphology and function.
Grapsa J, Tan TC, Paschou SA, Kalogeropoulos AS, Shimony A, Kaier T, et al. The effect of bariatric surgery on echocardiographic indices: a review of the literature. Eur J Clin Investig. 2013;43(11):1224–30. doi:10.1111/eci.12162.
Alpert MA, Omran J, Mehra A, Ardhanari S. Impact of obesity and weight loss on cardiac performance and morphology in adults. Prog Cardiovasc Dis. 2014;56(4):391–400. doi:10.1016/j.pcad.2013.09.003.
Peterson LR, Waggoner AD, Schechtman KB, Meyer T, Gropler RJ, Barzilai B, et al. Alterations in left ventricular structure and function in young healthy obese women: assessment by echocardiography and tissue Doppler imaging. J Am Coll Cardiol. 2004;43(8):1399–404. doi:10.1016/j.jacc.2003.10.062.
Powell BD, Redfield MM, Bybee KA, Freeman WK, Rihal CS. Association of obesity with left ventricular remodeling and diastolic dysfunction in patients without coronary artery disease. Am J Cardiol. 2006;98(1):116–20. doi:10.1016/j.amjcard.2006.01.063.
Garza CA, Pellikka PA, Somers VK, Sarr MG, Collazo-Clavell ML, Korenfeld Y, et al. Structural and functional changes in left and right ventricles after major weight loss following bariatric surgery for morbid obesity. Am J Cardiol. 2010;105(4):550–6. doi:10.1016/j.amjcard.2009.09.057.
Owan T, Avelar E, Morley K, Jiji R, Hall N, Krezowski J, et al. Favorable changes in cardiac geometry and function following gastric bypass surgery: 2-year follow-up in the Utah obesity study. J Am Coll Cardiol. 2011;57(6):732–9. doi:10.1016/j.jacc.2010.10.017.
Algahim MF, Lux TR, Leichman JG, Boyer AF, Miller CC, Laing ST, et al. Progressive regression of left ventricular hypertrophy two years after bariatric surgery. Am J Med. 2010;123(6):549–55. doi:10.1016/j.amjmed.2009.11.020.
Brownell NK, Rodriguez-Flores M, Garcia-Garcia E, Ordoñez-Ortega S, Oseguera-Moguel J, Aguilar-Salinas CA, et al. Impact of body mass index >50 on cardiac structural and functional characteristics and surgical outcomes after bariatric surgery. Obes Surg. 2016;26(11):2772–8. doi:10.1007/s11695-016-2199-8.
Lee GK, Cha YM. Cardiovascular benefits of bariatric surgery. Trends Cardiovasc Med. 2016;26(3):280–9. doi:10.1016/j.tcm.2015.07.006.
Cuspidi C, Rescaldani M, Tadic M, Sala C, Grassi G. Effects of bariatric surgery on cardiac structure and function: a systematic review and meta-analysis. Am J Hypertens. 2014;27(2):146–56. doi:10.1093/ajh/hpt215.
Ashrafian H, le Roux CW, Darzi A, Athanasiou T. Effects of bariatric surgery on cardiovascular function. Circulation. 2008;118(20):2091–102. doi:10.1161/CIRCULATIONAHA.107.721027.
Gosse P. Left ventricular hypertrophy as a predictor of cardiovascular risk. J Hypertens Suppl. 2005;23(1):S27–33.
Jhaveri RR, Pond KK, Hauser TH, Kissinger KV, Goepfert L, Schneider B, et al. Cardiac remodeling after substantial weight loss: a prospective cardiac magnetic resonance study after bariatric surgery. Surg Obes Relat Dis. 2009;5(6):648–52. doi:10.1016/j.soard.2009.01.011.
Tsao CW, Gona PN, Salton CJ, Chuang ML, Levy D, Manning WJ, et al. Left ventricular structure and risk of cardiovascular events: a Framingham heart study cardiac magnetic resonance study. J Am Heart Assoc. 2015;4(9):e002188. doi:10.1161/JAHA.115.002188.
Nguyen NT, Nguyen B, Gebhart A, Hohmann S. Changes in the makeup of bariatric surgery: a national increase in use of laparoscopic sleeve gastrectomy. J Am Coll Surg. 2013;216(2):252–7. doi:10.1016/j.jamcollsurg.2012.10.003.
Reames BN, Finks JF, Bacal D, Carlin AM, Dimick JB. Changes in bariatric surgery procedure use in Michigan, 2006-2013. JAMA. 2014;312(9):959–61. doi:10.1001/jama.2014.7651.
Shi X, Karmali S, Sharma AM, Birch DW. A review of laparoscopic sleeve gastrectomy for morbid obesity. Obes Surg. 2010;20(8):1171–7. doi:10.1007/s11695-010-0145-8.
Kokkinos A, Alexiadou K, Liaskos C, Argyrakopoulou G, Balla I, Tentolouris N, et al. Improvement in cardiovascular indices after Roux-en-Y gastric bypass or sleeve gastrectomy for morbid obesity. Obes Surg. 2013;23(1):31–8. doi:10.1007/s11695-012-0743-8.
Graziani F, Leone AM, Cialdella P, Basile E, Pennestrì F, Della Bona R, et al. Effects of bariatric surgery on cardiac remodeling: clinical and pathophysiologic implications. Int J Cardiol. 2013;168(4):4277–9. doi:10.1016/j.ijcard.2013.04.202.
Iancu ME, Copăescu C, Şerban M, Ginghină C. Favorable changes in arterial elasticity, left ventricular mass, and diastolic function after significant weight loss following laparoscopic sleeve gastrectomy in obese individuals. Obes Surg. 2014;24(3):364–70. doi:10.1007/s11695-013-1097-6.
Leung M, Xie M, Durmush E, Leung DY, Wong VW. Weight loss with sleeve gastrectomy in obese type 2 diabetes mellitus: impact on cardiac function. Obes Surg. 2016;26(2):321–6. doi:10.1007/s11695-015-1748-x.
Cavarretta E, Casella G, Calì B, Dammaro C, Biondi-Zoccai G, Iossa A, et al. Cardiac remodeling in obese patients after laparoscopic sleeve gastrectomy. World J Surg. 2013;37(3):565–72. doi:10.1007/s00268-012-1874-8.
Kaier TE, Morgan D, Grapsa J, Demir OM, Paschou SA, Sundar S, et al. Ventricular remodelling post-bariatric surgery: is the type of surgery relevant? A prospective study with 3D speckle tracking. Eur Heart J Cardiovasc Imaging. 2014;15(11):1256–62. doi:10.1093/ehjci/jeu116.
Kemaloğlu Öz T, Ünal Dayı Ş, Seyit H, Öz A, Ösken A, Atasoy I, et al. The effects of weight loss after sleeve gastrectomy on left ventricular systolic function in men versus women. J Clin Ultrasound. 2016;44(8):492–9. doi:10.1002/jcu.22361.
Jaiswal A, Nguyen VQ, Carry BJ, le Jemtel TH. Pharmacologic and endovascular reversal of left ventricular remodeling. J Card Fail. 2016;22(10):829–39. doi:10.1016/j.cardfail.2016.03.017.
Greupner J, Zimmermann E, Grohmann A, Dübel HP, Althoff TF, Althoff T, et al. Head-to-head comparison of left ventricular function assessment with 64-row computed tomography, biplane left cineventriculography, and both 2- and 3-dimensional transthoracic echocardiography: comparison with magnetic resonance imaging as the reference standard. J Am Coll Cardiol. 2012;59(21):1897–907. doi:10.1016/j.jacc.2012.01.046.
Lee JH, Park JH. Role of echocardiography in clinical hypertension. Clin Hypertens. 2015;21:9. doi:10.1186/s40885-015-0015-8.
Chirinos JA, Segers P, De Buyzere ML, Kronmal RA, Raja MW, De Bacquer D, et al. Left ventricular mass: allometric scaling, normative values, effect of obesity, and prognostic performance. Hypertension. 2010;56(1):91–8. doi:10.1161/HYPERTENSIONAHA.110.150250.
• Ganau A, Devereux RB, Roman MJ, de Simone G, Pickering TG, Saba PS, et al. Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. J Am Coll Cardiol. 1992;19(7):1550–8. doi:10.1016/0735-1097(92)90617-V. Landmark characterization of the effects of hypertension on left ventricular mass and wall thickness and first description of left ventricular hypertrophy phenotypes. Concentric left ventricular remodeling and eccentric hypertrophy are more prevalent than concentric left ventricular hypertrophy in untreated hypertensive patients.
•• Khouri MG, Peshock RM, Ayers CR, de Lemos JA, Drazner MH. A 4-tiered classification of left ventricular hypertrophy based on left ventricular geometry: the Dallas heart study. Circ Cardiovasc Imaging. 2010;3(2):164–71. doi:10.1161/CIRCIMAGING.109.883652. Measurement of left ventricular volumes by cardian magnetic resonance imaging provided insight on left ventricular adaptation. The increase in left ventricular wall thickness is independent from the increase in left ventricular cavity.
Chinali M, Aurigemma GP. Refining patterns of left ventricular hypertrophy using cardiac MRI: "brother, can you spare a paradigm?". Circ Cardiovasc Imaging. 2010;3(2):129–31. doi:10.1161/CIRCIMAGING.110.944959.
de Simone G, Izzo R, Aurigemma GP, De Marco M, Rozza F, Trimarco V, et al. Cardiovascular risk in relation to a new classification of hypertensive left ventricular geometric abnormalities. J Hypertens. 2015;33(4):745–754; discussion 54. doi:10.1097/HJH.0000000000000477.
Bang CN, Gerdts E, Aurigemma GP, Boman K, de Simone G, Dahlof B, et al. Four-group classification of left ventricular hypertrophy based on ventricular concentricity and dilatation identifies a low-risk subset of eccentric hypertrophy in hypertensive patients. Circ Cardiovasc Imaging. 2014;7:422–9. doi:10.1161/CIRCIMAGING.113.001275.
Desai CS, Bartz TM, Gottdiener JS, Lloyd-Jones DM, Gardin JM. Usefulness of left ventricular mass and geometry for determining 10-year prediction of cardiovascular disease in adults aged >65 years (from the cardiovascular health study). Am J Cardiol. 2016;118(5):684–90. doi:10.1016/j.amjcard.2016.06.016.
Dorbala S, Crugnale S, Yang D, Di Carli MF. Effect of body mass index on left ventricular cavity size and ejection fraction. Am J Cardiol. 2006;97(5):725–9. doi:10.1016/j.amjcard.2005.09.122.
Reisin E, Jack AV. Obesity and hypertension: mechanisms, cardio-renal consequences, and therapeutic approaches. Med Clin North Am. 2009;93(3):733–51. doi:10.1016/j.mcna.2009.02.010.
• Turkbey EB, McClelland RL, Kronmal RA, Burke GL, Bild DE, Tracy RP, et al. The impact of obesity on the left ventricle: the multi-ethnic study of atherosclerosis (MESA). JACC Cardiovasc Imaging. 2010;3(3):266–74. doi:10.1016/j.jcmg.2009.10.012. Measurement of left ventricular size and function by cardiac magnetic resonance imaging definitively established that obesity is associated with concentric left ventricular remodeling.
Rider OJ, Lewandowski A, Nethononda R, Petersen SE, Francis JM, Pitcher A, et al. Gender-specific differences in left ventricular remodelling in obesity: insights from cardiovascular magnetic resonance imaging. Eur Heart J. 2013;34(4):292–9. doi:10.1093/eurheartj/ehs341.
Rider OJ, Francis JM, Ali MK, Petersen SE, Robinson M, Robson MD, et al. Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J Am Coll Cardiol. 2009;54(8):718–26. doi:10.1016/j.jacc.2009.02.086.
Litwin SE. Cardiac remodeling in obesity: time for a new paradigm. JACC Cardiovasc Imaging. 2010;3(3):275–7. doi:10.1016/j.jcmg.2009.12.004.
Bello NA, Cheng S, Claggett B, Shah AM, Ndumele CE, Roca GQ, et al. Association of Weight and Body Composition on Cardiac Structure and Function in the ARIC Study (Atherosclerosis Risk in Communities). Circ Heart Fail. 2016;9(8). doi:10.1161/CIRCHEARTFAILURE.115.002978.
Korre M, Porto LG, Farioli A, Yang J, Christiani DC, Christophi CA, et al. Effect of body mass index on left ventricular mass in career male firefighters. Am J Cardiol. 2016;118(11):1769–73. doi:10.1016/j.amjcard.2016.08.058.
Izzo R, Losi MA, Stabile E, Lönnebakken MT, Canciello G, Esposito G, et al. Development of left ventricular hypertrophy in treated hypertensive outpatients: the Campania salute network. Hypertension. 2017;69(1):136–42. doi:10.1161/HYPERTENSIONAHA.116.08158.
Markus MR, Werner N, Schipf S, Siewert-Markus U, Bahls M, Baumeister SE, et al. Changes in body weight and composition are associated with changes in left ventricular geometry and function in the general population: SHIP (study of health in Pomerania). Circ Cardiovasc Imaging. 2017;10(3):e005544. doi:10.1161/CIRCIMAGING.116.005544.
Murdolo G, Angeli F, Reboldi G, Di Giacomo L, Aita A, Bartolini C, et al. Left ventricular hypertrophy and obesity: only a matter of fat? High Blood Press Cardiovasc Prev. 2015;22(1):29–41. doi:10.1007/s40292-014-0068-x.
Hall JE, do Carmo JM, da Silva AA, Wang Z, Hall ME. Obesity-induced hypertension: interaction of neurohumoral and renal mechanisms. Circ Res. 2015;116(6):991–1006. doi:10.1161/CIRCRESAHA.116.305697.
Nadruz W. Myocardial remodeling in hypertension. J Hum Hypertens. 2015;29(1):1–6. doi:10.1038/jhh.2014.36.
Woodiwiss AJ, Libhaber CD, Majane OH, Libhaber E, Maseko M, Norton GR. Obesity promotes left ventricular concentric rather than eccentric geometric remodeling and hypertrophy independent of blood pressure. Am J Hypertens. 2008;21(10):1144–51. doi:10.1038/ajh.2008.252.
•• Neeland IJ, Gupta S, Ayers CR, Turer AT, Rame JE, Das SR, et al. Relation of regional fat distribution to left ventricular structure and function. Circ Cardiovasc Imaging. 2013;6(5):800–7. doi:10.1161/CIRCIMAGING.113.000532. As seminal investigation that linked visceral adipose tissue to concentric left ventricular remodeling and lower body subcutaneous fat tissue to eccentric left ventricular remodeling.
• de Simone G, Mancusi C, Izzo R, Losi MA, Aldo Ferrara L. Obesity and hypertensive heart disease: focus on body composition and sex differences. Diabetol Metab Syndr. 2016;8:79. doi:10.1186/s13098-016-0193-x. Control of blood pressure is needed is mandatory for prevention and regression of left ventricular hypertrophy. However, regression of left ventricular hypertrophy requires reduciton of visceral adipose tissue in obese hypertensive patients.
Gupta RK, Gupta R, Makar N, Chaudhary S, Bhatheja H, Pathak P. The association of left ventricular mass index with metabolic syndrome in comparison to hypertensive patients. J Cardiovasc Echogr. 2016;26(2):42–7. doi:10.4103/2211-4122.183748.
Abbasi SA, Hundley WG, Bluemke DA, Jerosch-Herold M, Blankstein R, Petersen SE, et al. Visceral adiposity and left ventricular remodeling: the multi-ethnic study of atherosclerosis. Nutr Metab Cardiovasc Dis. 2015;25(7):667–76. doi:10.1016/j.numecd.2015.03.016.
Yano Y, Vongpatanasin W, Ayers C, Turer A, Chandra A, Carnethon MR, et al. Regional fat distribution and blood pressure level and variability: the Dallas Heart Study. Hypertension. 2016;68(3):576–83. doi:10.1161/HYPERTENSIONAHA.116.07876.
Corradi D, Maestri R, Callegari S, Pastori P, Goldoni M, Luong TV, et al. The ventricular epicardial fat is related to myocardial mass in normal, ischemci and hypertrophic hearts. Cardiovasc Pathol. 2004;13(6):313–6. doi:10.1016/j.carpath.2004.08.005.
Iacobellis G, Ribaudo MC, Zappaterrena A, Iannucci CV, Leonetti F. Relation between epicardial adipose tissue and left ventricular mass. Am J Cardiol. 2004;94(8):1084–7. doi:10.1016/j.amjcard.2004.06.075.
Sacks HS, Fain JN. Human epicardial tissue: a review. Am Heart J. 2007;153(6):907–17. doi:10.1016/j.ahj.2007.03.019.
Lemieux I, Pascot A, Prud'homme D, Alméras N, Bogaty P, Nadeau A, et al. Elevated C-reactive protein: another component of the atherothrombotic profile of abdominal obesity. Arterioscler Thromb Vasc Biol. 2001;21(6):961–7. doi:10.1161/01.ATV.21.6.961.
Selvaraj S, Martinez EE, Aguilar FG, Kim KY, Peng J, Sha J, et al. Association of Central Adiposity With Adverse Cardiac Mechanics: Findings From the Hypertension Genetic Epidemiology Network Study. Circ Cardiovasc Imaging. 2016;9(6). doi:10.1161/CIRCIMAGING.115.004396.
Pou KM, Massaro JM, Hoffmann U, Vasan RS, Maurovich-Horvat P, Larson MG, et al. Visceral and subcutaneous adipose tissue volumes are cross-sectionally related to markers of inflammation and oxidative stress: the Framingham Heart Study. Circulation. 2007;116(11):1234–41. doi:10.1161/CIRCULATIONAHA.107.710509.
Velagaleti RS, Gona P, Chuang ML, Salton CJ, Fox CS, Blease SJ, et al. Relations of insulin resistance and glycemic abnormalities to cardiovascular magnetic resonance measures of cardiac structure and function: the Framingham Heart Study. Circ Cardiovasc Imaging. 2010;3(3):257–63. doi:10.1161/CIRCIMAGING.109.911438.
Devereux RB, Reichek N. Echocardiographic determination of left ventricular mass in man. Anatomic validation of the method. Circulation. 1977;55(4):613–8. doi:10.1161/01.CIR.55.4.613.
Lønnebakken MT, Izzo R, Mancusi C, Gerdts E, Losi MA, Canciello G et al. Left Ventricular Hypertrophy Regression During Antihypertensive Treatment in an Outpatient Clinic (the Campania Salute Network). J Am Heart Assoc. 2017;6(3). doi:10.1161/JAHA.116.004152.
Shin SH, Lee YJ, Heo YS, Park SD, Kwon SW, Woo SI, et al. Beneficial effects of bariatric surgery on cardiac structure and function in obesity. Obes Surg. 2017;27(3):620–5. doi:10.1007/s11695-016-2330-x.
Gottdiener JS, Kop WJ. Body and heart: effects of weight gain and loss on left ventricular size and function. Circ Cardiovasc Imaging. 2017;10(3):e006084. doi:10.1161/CIRCIMAGING.117.006084.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16(3):233–70. doi:10.1093/ehjci/jev014.
Rigolin VH. Automated cardiac volumetric analysis: one step closer to incorporating 3D TTE into routine daily workflow. JACC Cardiovasc Imaging. 2016;9(7):783–4. doi:10.1016/j.jcmg.2016.01.023.
Thavendiranathan P, Liu S, Verhaert D, Calleja A, Nitinunu A, Van Houten T, et al. Feasibility, accuracy, and reproducibility of real-time full-volume 3D transthoracic echocardiography to measure LV volumes and systolic function: a fully automated endocardial contouring algorithm in sinus rhythm and atrial fibrillation. JACC Cardiovasc Imaging. 2012;5(3):239–51. doi:10.1016/j.jcmg.2011.12.012.
Tsang W, Salgo IS, Medvedofsky D, Takeuchi M, Prater D, Weinert L, et al. Transthoracic 3D echocardiographic left heart chamber quantification using an automated adaptive analytics algorithm. JACC Cardiovasc Imaging. 2016;9(7):769–82. doi:10.1016/j.jcmg.2015.12.020.
Mor-Avi V, Sugeng L, Weinert L, MacEneaney P, Caiani EG, Koch R, et al. Fast measurement of left ventricular mass with real-time three-dimensional echocardiography: comparison with magnetic resonance imaging. Circulation. 2004;110(13):1814–8. doi:10.1161/01.CIR.0000142670.65971.5F.
Missouris CG, Forbat SM, Singer DR, Markandu ND, Underwood R, MacGregor GA. Echocardiography overestimates left ventricular mass: a comparative study with magnetic resonance imaging in patients with hypertension. J Hypertens. 1996;14(8):1005–10. doi:10.1097/00004872-199608000-00011.
Myerson SG, Montgomery HE, World MJ, Pennell DJ. Left ventricular mass: reliability of M-mode and 2-dimensional echocardiographic formulas. Hypertension. 2002;40(5):673–8. doi:10.1161/01.HYP.0000036401.99908.DB.
Kühl HP, Hanrath P, Franke A. M-mode echocardiography overestimates left ventricular mass in patients with normal left ventricular shape: a comparative study using three-dimensional echocardiography. Eur J Echocardiogr. 2003;4(4):312–9. doi:10.1016/S1525-2167(03)00035-0.
Pacileo G, Castaldi B, Di Salvo G, Limongelli G, Rea A, D'Andrea A, et al. Assessment of left-ventricular mass and remodeling in obese adolescents: M-mode, 2D or 3D echocardiography? J Cardiovasc Med (Hagerstown). 2013;14(2):144–9. doi:10.2459/JCM.0b013e3283515b80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no conflicts of interest relevant to this manuscript.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Hypertension and Obesity
Rights and permissions
About this article
Cite this article
Le Jemtel, T.H., Samson, R., Jaiswal, A. et al. Regression of Left Ventricular Mass After Bariatric Surgery. Curr Hypertens Rep 19, 68 (2017). https://doi.org/10.1007/s11906-017-0767-5
Published:
DOI: https://doi.org/10.1007/s11906-017-0767-5