Abstract
The detection of left ventricular hypertrophy (LVH) is recommended for risk prediction, and changes in LV geometry may provide further prognostic information. Obesity is a major determinant of LVH, but the approach to LVH detection in obese hypertensives remains a challenge. In the present review, we discuss evidence leading to the recent acceptance of the use of LV mass indexed to height2.7 or height1.7 rather than body surface area, for LVH detection and its regression in obesity. We also review recent findings which indicate that obesity-induced LVH may be associated with concentric LV remodeling, and hence, that the presence of concentric LVH in obesity should not be assumed to indicate a cause of LVH other than obesity. We also discuss recent evidence for obesity and blood pressure producing additive and interactive effects on LV mass, and hence, that weight loss and blood pressure reduction are required to achieve appropriate regression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Left ventricular hypertrophy (LVH) and its regression predict cardiovascular events independent of conventional risk factors as well as coronary artery disease [1, 2]. Furthermore, as compared to a normal LV geometry, an increase in LV wall thickness or LV mass (LVM) exceeding that of increases in LV internal diameter or volume (concentric LV remodeling), is associated with a worse prognosis independent of LVM per se [3, 4]. The importance of LVH detection is acknowledged by recent guidelines [5]. The presence of LVH determines overall risk stratification and is an important therapeutic target in managing hypertension. Key factors which contribute to the development of LVH and alterations in LV geometry include obesity and hypertension. Given the current increasing prevalence of obesity worldwide [6], and recent changes in approaches to LVH detection and the clinical implications thereof, a review of the current state of knowledge in the field is timeous and of importance. An understanding of the role of LVH in obesity has major implications with respect to appropriate risk prediction and adequately guiding clinical interventions to prevent the development and regression of LVH.
Despite ongoing research since the late 1950s [7], unresolved controversies as to the combined role of obesity and hypertension as causes of LVH and concentric LV remodeling still remain. The purpose of this review is to highlight some recent advances with regard to the relative roles of obesity and hypertension in the development of alterations in LV morphology. In the present review, we discuss the impact of different types of indexation of LVM on the prevalence of LVH and risk prediction in obesity and hypertension. Second, we summarize current notions of obesity-induced alterations in LV geometry. Third, we review the present understanding of interactive effects of obesity and hypertension on LVH. In all sections, we consider the implications of these data for risk assessment and clinical interventions to prevent and/or reduce LVH and adverse LV remodeling.
Which Index of LVM is Preferable to Identify LVH in Obesity?
The prevalence of LVH in obesity varies widely. Indeed, prevalence rates ranging from 6.2 to 48.4 % have been reported (Table 1). Although, the severity and duration of obesity, as well as the presence (or absence) of comorbidities contribute to this wide range; the most important factor which determines whether LVH is considered to be present in obesity is the use of different indexes of LVM employed to normalize LVM to body size (Table 1). In this regard, LVM may be indexed to body surface area (BSA), where indexation to BSA is largely designed to eliminate the impact of body size, including the effects of obesity. In contrast, LVM indexation to allometric signals of height is employed to eliminate the impact of growth, but not obesity on LVM. Indexing LVM to allometric signals of height has now been acknowledged by guidelines [5].
The prevalence of LVH in normal weight hypertensives ranges from 5.6 % using LVM indexed to BSA to 11.7 % using LVM indexed to height2.7 [8] (Table 1). In obese hypertensives, however, the impact of differences in LVM indexation on the prevalence of LVH is far greater, ranging from 9.5 % using LVM indexed to BSA to 48.4 % using LVM indexed to height2.7 [8] (Table 1). In large community-based studies, the prevalence of LVH in overweight and obese individuals is markedly higher when LVM is indexed to various allometric signals of height (height2.7 or height1.7) as compared to when LVM is indexed to BSA [9••, 10, 11] (Table 1).
Although indexation to BSA is commonly used, it was criticized for ‘overadjustment’ and hence disregarding the effects of obesity on the LV [12]. The argument in favor of indexing LVM to BSA is that it is hypertensive-related LVH that is of interest when risk predicting. This argument assumes that obesity does not produce pathological LVH. However, assuming that obesity does indeed produce pathological LVH, in order to adjust for growth effects on the LV, indexations to various allometric signals of body height were introduced in order to accommodate the nonlinear association of body height with LV mass. Although LVM indexed to height2.7 may eliminate the differences in LVM due to body height [12], it has subsequently been suggested to overcorrect for body height. Indeed, residual negative correlations were identified between LVM indexed to height2.7 and height [9••].
Hence, a further refinement of the allometric signal of height is LVM indexed to height1.7, which results in no residual negative correlation [9••].
The purpose of identifying LVH is risk prediction. Hence, clinically, the impact of the different indexes of LVM on the hazard ratios and population attributable risk for cardiovascular events is of importance. In this regard, allometric approaches, that increase the prevalence of LVH (height1.7 or height2.7) (Table 1) without decreasing LVH-associated relative risk, result in increases in the population attributable risk. Indeed, a 2- to 3-fold increase in the prevalence of LVH using LVM indexed to height2.7 (19.5 % for common threshold; 21.0 % for sex-specific thresholds) compared to LVM indexed to BSA (6.8 % for common threshold; 9.0 % for sex-specific thresholds) was noted, whereas hazard ratios (HR) for all cardiovascular events were only reduced by 20 % when employing height rather than BSA indexes (LVM indexed to height2.7: HR = 1.92; LVM indexed to BSA: HR = 2.39) [13]. Hence, comparing the population attributable risk of different methods of defining LVH, LVM indexed to height2.7 maximizes the population attributable risk for cardiovascular events (15.54 %) as compared to LVM indexed to BSA (8.87 %) [8, 13]. The age- and sex-adjusted population attributable risk for cardiovascular events was on average 1.8 fold greater when LVM was indexed to height2.7 in comparison to LVM indexed to BSA. Hence, for risk prediction and consequently risk reduction following appropriate interventions, LVH defined using height2.7 is preferable to that defined using LVM indexed to BSA. Indeed, the current European Society of Hypertension (ESH) and European Society of Cardiology (ESC) guidelines (2013) [5] recommend the use of LVM indexed to height2.7 or height1.7 in overweight or obese patients in preference to LVM indexed to BSA, in order to avoid the possible underdiagnosis of obesity-related pathological LVH.
Why was LVM indexed to height1.7 recommended as an alternative to LVM indexed to height2.7 in the 2013 ESH/ESC guidelines [5]? As indicated in the aforementioned discussion, LVM indexed to height2.7 produces a residual negative relationship between LVM indexed to height2.7 and height [9••]. Hence, it was suggested that the hazard ratios and population attributable risk due to LVM indexed to height2.7 incorporate a component of non-modifiable risk [9••], that is, the risk of cardiovascular events associated with short stature [14]. Chirinos et al. (2010) [9••] argue that it is risk based upon LVM alone which is of practical relevance from a clinical perspective. Notably, in the Multiethnic Study on Atherosclerosis (MESA), the hazard ratios for all-cause mortality were significant for LVM indexed to height1.7 (HR = 1.60, p = 0.02), whereas LVM indexed to height2.7 failed to predict all-cause mortality (HR = 1.42, p = 0.09) [9••]. Nevertheless, in the MESA, the hazard ratios for cardiovascular events were higher for LVM indexed to height2.7 (HR = 1.73, p = 0.001) than they were for LVM indexed to height1.7 (HR = 1.53, p = 0.01) [9••].
Direct comparisons of hazard ratios (and consequently calculated population attributable risks) from the studies of de Simone et al. (2005) [13] and Chirinos et al. (2010) [9••] are problematic due to differences in the characteristics of the populations. The hazard ratios provided by de Simone et al. (2005) [13] and de Simone (2013) [8] were obtained in a population in which 32 % were overweight and 56 % were obese; however, in the two studies (Asklepios and MESA) included in the Chirinos et al. (2010) [9••] analysis, the maximum body mass indexes (BMIs) were 29.2 and 31.0 kg/m2, respectively. Hence, the hazard ratios upon which Chirinos et al. (2010) recommended LVM indexed to height1.7 in preference to height2.7 were obtained from population samples where a very limited number of obese participants were included [9••]. In the Strong Heart Study in which 35 % of participants were overweight and 48 % were obese, the hazard ratios for cardiovascular events for LVM indexed to height1.7 were 1.76 (p = 0.003, for common threshold) and 1.53 (p = 0.03, for sex-specific thresholds) compared to 1.92 (p < 0.001, for common threshold) for LVM indexed to height2.7 [13, 15•]. Thus, in a population with a high prevalence of overweight and obesity, the population attributable risks due to LVM indexed to height1.7 (12.03 % using a common threshold and 9.58 % using sex-specific thresholds) [15•] are lower than those due to LVM indexed to height2.7 (15.54 % age and sex-adjusted using a common threshold) [13]. Hence, although it is clear that LVM indexed to BSA is not advisable when assessing cardiovascular risk associated with LVH in overweight or obese patients [5], whether indexation to height2.7 or height1.7 should be employed for use in clinical practice requires clarification. Further outcomes-based studies particularly in overweight and obese patients are required in order to resolve this issue.
Assuming that allometric signals for height2.7 or height1.7 are best employed to index LVM in overweight and obese patients, what thresholds should be used? Most studies recommend sex-specific thresholds [8, 9••], as sex is an independent determinant of LVM, which is not totally accounted for by indexations of LVM [9••]. In this regard, de Simone et al. (2013) [8] recommend that the threshold values of 47 g/m2.7 in women and 50 g/m2.7 as suggested for the general population are also used in obese individuals. Chirinos et al. (2010) [9••] recommend threshold values of 60 g/m1.7 for white or black women and 80 or 81 g/m1.7 for white or black men, based upon 95 % values in reference samples. In addition, as significant ethnic differences in indexed LVM have been reported [9••, 16], ethnic specific thresholds have been recommended. Based upon prognostically validated data for cardiovascular and total mortality, threshold values of 55 and 68 g/m1.7 for Chinese women and men, respectively, and 71 and 81 g/m1.7 for Hispanic women and men, respectively, have been recommended [9••]. However, as previously indicated, a caveat to these proposed thresholds is that the prognostic validation of these thresholds for LVM indexed to height1.7 was performed in a population sample with a very low prevalence of obesity [9••].
In summary, in keeping with the important outcomes data provided by de Simone et al. (2005 and 2013) [8, 13], and Chirinos et al. (2010) [9••], showing a poor prognostic ability (cardiovascular events or all-cause mortality) of LVM indexed to BSA in comparison to either LVM indexed to height2.7 or height1.7, the ESH/ESC guidelines recommend the use of LVM indexed to height2.7 or height1.7 and the use of sex-specific thresholds in overweight or obese patients [5]. With respect to the American Heart Association guidelines, the Joint National Committee (JNC) 8 is silent on this issue, but the American Society of Echocardiography (ASE) committee has previously recommended LVM indexed to BSA [17], an approach which is clearly outdated when applied to obese individuals.
Impact of Obesity on LV Geometry: Concentric or Eccentric?
There are considerable inconsistencies in studies evaluating whether concentric or eccentric LVH predominate in obesity. In this regard, as compared to eccentric LVH, concentric LVH is well-recognized as carrying a higher risk for cardiovascular events and concentric LV geometry alone may predict outcomes [3, 4]. Based upon the current understanding of the hemodynamic alterations that accompany obesity in normotensive persons (increases in LV filling volume and hence stroke volume, together with decreases in total peripheral resistance), predictions were that obesity should associate with mainly eccentric LVH [7, 18] and hence may be a more benign form of LVH than for example hypertensive LVH. Indeed, earlier studies report the presence of eccentric LVH in obesity [19]. Hence, previously, the presence of concentric LVH was frequently seen as an indicator that the cause of LVH is through increases in blood pressure rather than obesity. However, as highlighted in recent reviews [7, 18], this is not the case. What is the present state of knowledge regarding the LV geometric changes in obesity associated LVH?
One of the factors that may explain the controversy of whether obesity determines concentric or eccentric LVH is the coexistence of elevations in blood pressure. In this regard, it has been suggested that uncomplicated obesity (that is obesity which is not accompanied by comorbidities such as hypertension, diabetes mellitus, and dyslipidemia) is associated with eccentric LVH, whereas obesity accompanied by hypertension (complicated obesity) is more likely to result in concentric LVH and concentric remodeling. Indeed, the hemodynamic alterations which accompany complicated obesity (decreases in filling volume and hence stroke volume together with increases in peripheral resistance) differ from those that occur in uncomplicated obesity and indeed would favor increases in LV concentric remodeling [7, 20].
Although the concept of uncomplicated versus complicated obesity is conceptually sound, obesity most commonly occurs together with comorbidities [18, 20] and infrequently occurs in isolation. Hence, in order to accurately identify the independent effects of obesity on LV geometry, it is important that adequate adjustments for confounders are made in analyses [7]. Indeed, increases in blood pressure are associated with concentricity and decreases in blood pressure due to antihypertensive therapy are accompanied by reductions in the prevalence on concentric LVH and concentric remodeling across BMI categories (36 to 4 % in normal weight; 33 to 4 % in overweight, 35 to 7 % in obese, 34 to 11 % in severely obese) [21]. However, many previous studies have failed to adequately adjust for blood pressure or the presence of hypertension [7]. In a study of participants not receiving treatment for hypertension, in which approximately 7 % of participants had concentric LVH, 16 % concentric LV remodeling, and 15 % eccentric LVH, our group was the first to show that obesity is associated with a predominance of concentric LVH and remodeling after adequate adjustments for blood pressure including ambulatory blood pressure [22]. In a larger cohort of participants not receiving treatment for hypertension (n = 606, 6.8 % with concentric LVH, 16.0 % with concentric LV remodeling, 14.0 % with eccentric LVH), and with a high prevalence of central (abdominal) obesity (36.0 %), we now confirm these data and show that after adjustments for potential confounders including systolic blood pressure, waist circumference is strongly related to concentric LVH (beta coefficient = 0.64 ± 0.21, p = 0.002). Nevertheless, in this larger sample size, we also show a modest relationship between waist circumference and eccentric LVH (beta coefficient = 0.32 ± 0.14, p = 0.025). Importantly, the association of obesity with a predominance of concentric LVH and remodeling is confirmed by data from a large magnetic resonance imaging (MRI) study showing that obesity is associated with increases in the LV mass to volume ratio, and that these relationships are attributed to increases in LVM and not decreases in LV volume, even after adjusting for blood pressure or the presence of hypertension [23••].
The impact of body fat distribution may in part account for conflicting data on the impact of obesity on changes in LV geometry. Even after adjustments for confounders including hypertension or blood pressure, magnetic resonance imaging-determined visceral adiposity (visceral fat or abdominal subcutaneous fat) is associated with an increased LV wall thickness and LV concentricity and is negatively associated with LV end-diastolic volume (p < 0.0001 for all), whereas lower body subcutaneous fat is negatively associated with LV wall thickness and LV concentricity and positively associated with LV end-diastolic volume (p < 0.0001 for all) [24••]. Moreover, in a separate study, intra-abdominal adipose tissue area was noted to be an independent determinant of LV relative wall thickness (p < 0.0001), whereas lean body mass determined LV end-diastolic diameter (p < 0.0001) [25]. In a larger cohort of randomly selected community participants (n = 796), with a high prevalence of central (abdominal) obesity (45.7 %), we now show that irrespective of whether hypertension is present or absent, that abdominal obesity is associated with an increase in LV wall thickness and end-diastolic dimensions, but that the wall thickness changes exceed the internal diameter changes. Hence, LV relative wall thickness is increased (Fig. 1, middle panels). Increases in the LV mass to volume ratio have also been associated with increases in waist circumference, waist-to-hip ratio, and fat mass, but not with BMI [23••], and LV mass to volume ratio is in fact negatively associated with lean body mass [23••]. Indeed, a 10-kg increase in lean body mass is associated with a 0.04-g/ml and a 0.07-g/ml decrease in LV mass to volume ratio in women and men, respectively. In comparison, a 10-kg increase in fat mass is associated with a 0.02-g/ml and a 0.06-g/ml increase in LV mass to volume ratio in women and men, respectively [23••].
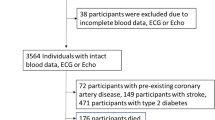
The impact of obesity (increased waist circumference, WC) and hypertension (HT) on left ventricular mass (LVM) indexed to height2.7 or height1.7, relative wall thickness, mean wall thickness, and left ventricular (LV) end-diastolic diameter. NT, normotensive; *p < 0.05, **p < 0.005, ***p < 0.0001 versus normal WC plus NT; † p < 0.05, †† p < 0.005, ††† p < 0.0001 versus increased WC plus NT; # p < 0.05, ## p < 0.0001 versus normal WC plus HT
In a meta-analysis of 22 echocardiographic studies in obese individuals, eccentric LVH prevailed over concentric LVH [26•]. However, ∼80 % of these studies included participants with complicated obesity, and yet, no adjustments for either the presence of hypertension or blood pressure were made [26•]. Despite eccentric LVH being the principle form of LVH in that study [26•], concentric LVH also occurred in a notable fraction (34 %) of obese individuals. Importantly, these data [26•] are in contrast to relations between obesity and MRI-determined LVM (which avoids the possibility of poor echocardiographic windows in obesity) where correlations between waist circumference and LV mass to volume ratio (a 3-dimensional measure of concentric geometry) are noted [23••] and where concentric rather than eccentric LVH is the predominant geometric pattern in obesity [18, 27].
In support of an association of obesity with a concentric rather than eccentric geometry, various bariatric surgery-induced weight loss studies have reported reductions in LV relative wall thickness after surgery [25, 28, 29••, 30, 31•] (Table 2). Indeed, after weight loss, LV relative wall thickness in the obese group may be no different from that of the lean group [25]. Moreover, a substantial decrease in the prevalence of concentric LVH and remodeling follow weight reduction, with more modest decreases in the prevalence of eccentric LVH [29••, 30] (Table 2). In a meta-analysis of bariatric surgery studies, a significant decrease in relative wall thickness (and hence, a less concentric LV geometry) together with reductions in LVM and LVM indexed to height2.7 occurred [31•] (Table 2). Nevertheless, after a 45.1 % reduction in excess BMI at 3 months after bariatric surgery, only the change in systolic blood pressure (p < 0.0001) determined changes in relative wall thickness [29••]. These data point to an important role of systolic blood pressure in the development of concentric LVH in obesity. Also, in support of an association of obesity with concentric rather than eccentric LVH, dietary weight loss interventions are associated with reductions in the prevalence of concentric LVH, whereas the prevalence of eccentric LVH is increased [32]. However, no adjustments were made for reductions in systolic blood pressure [32] (Table 2).
It is of interest to note that gender-specific differences in LV geometry in obesity may occur [33]. Although, concentric LVH is present in both obese men and women, concentric LVH predominates in obese men, whereas concentric and eccentric LVH occur in women. The relationship between BMI and LVM to volume ratio is steeper in men (a 0.13 increase in LVM to volume ratio per unit increase in BMI) compared to women (a 0.06 increase in LVM to volume ratio per unit increase in BMI) [33]. These gender differences in LV geometry may in part explain the greater cardiovascular mortality associated with obesity in men compared to women [34] and may also explain some of the contrasting findings of obesity-associated LV geometry in other studies.
In summary, contrary to the original studies suggesting that obesity-induced LVH was eccentric in nature [19], subsequent work has demonstrated that obesity-induced LVH is also associated with concentric LV remodeling and although still debated, concentric LVH may in fact predominate depending on which fat depot and gender one considers. However, the confounding effects of blood pressure are difficult to exclude. Therefore, before definitive conclusions can be reached on the impact of obesity on LV geometry, further intervention studies, which include adjustments for ambulatory blood pressure, are required. At this point, however, the presence of concentric LVH in obese individuals should not be seen as an indicator that the cause of LVH is through an effect other than obesity.
Additive or Interactive Effects of Obesity and Blood Pressure on LVH and LV Geometry?
Obesity and hypertension frequently coexist [18, 20], and in a large cross-sectional community-based study (n = 1185) in which 45.9 % of participants were hypertensive and 43.3 % were obese [11], 26.3 % were both obese and hypertensive. Hence, it is important to understand the possible additive and/or interactive effects of obesity and blood pressure on LVH. Additive effects would require managing each risk factor independently to achieve appropriate LVH regression. In contrast, interactive effects would suggest that if appropriate management of one risk factor is not possible, then lower targets for the other risk factor may nevertheless achieve LVH regression. Hence, for example, if blood pressure, rather than obesity, is the risk factor that is successfully managed (weight reduction often does not achieve therapeutic targets, and if it does, these targets are often not sustained), then lowering blood pressure to a greater extent in obese as compared to lean hypertensives may nevertheless achieve a similar reduction in LVM index.
It is well accepted that overweight and obesity are significant determinants of LVH independent of blood pressure (including ambulatory blood pressure) [35]. Furthermore, both systolic blood pressure and intra-abdominal adipose tissue area (visceral fat) are independent determinants of LV wall thickness [25]. Moreover, in a large study sample derived from a community with a high prevalence of obesity (43.6 %), central abdominal obesity (45.7 %), and hypertension (46.4 %), we show the independent effects of abdominal obesity and hypertension on LVM index and LV wall thickness (Fig. 1, upper and middle panels). The magnitude of the separate effects of obesity and hypertension on LVM has recently been highlighted. In this regard, in a 20-year follow-up study of 2426 participants, a 1-kg/m2 increase in BMI was reported to increase LVM by 2.5 g, and a 10-mmHg increase in mean arterial pressure increased LVM by 6.2 g [36•]. The odds ratio (OR) for developing abnormal LV geometry after 20 years was similar for a 10-mmHg increase in systolic blood pressure (OR = 1.22, p < 0.0001) as compared to a 1-kg/m2 increase in BMI (OR = 1.07, p < 0.0001) [35]. In addition, in severely obese subjects, the impact of systolic blood pressure (standardized beta-coefficient = 0.21, p = 0.001) on LVM indexed to height2.7 was similar to that of BMI (standardized beta-coefficient = 0.18, p = 0.002) [37]. Hence, the separate effects of obesity and blood pressure on LV mass and geometry, with the obvious additive action of both risk factors, are well-recognized. However, the possibility of interactive effects of obesity and hypertension on LVH and LV geometry is less well appreciated.
In cross-sectional studies, strong interactive effects, where obesity potentiates the effects of increased blood pressure on LVM, have been shown [38]. Moreover, in severely obese subjects, an interactive effect of BMI and hypertension on LVM was noted (p < 0.0001 for interaction), where the increase in LVM indexed to height2.7 was more pronounced in patients with hypertension compared to those without hypertension [37]. In a larger study sample, we confirm our previous data showing that in multivariate-adjusted models, obesity potentiates the effects of increased blood pressure on LVM [38] as well as shows the interactive effects of obesity and blood pressure on various indexes to height of LVM (Fig. 1, lower panels). In this regard, independent of confounders and the individual terms, blood pressure-waist circumference interactions were noted for LVM indexed to height2.7 (p < 0.02) and height1.7 (p < 0.05) (Fig. 1, lower panels). Importantly, as we had previously described [38], despite similar increases in blood pressure, independent of confounders, hypertension increased LVM index in those with abdominal obesity (increased waist circumference), but not in those with a normal waist circumference (Fig. 1, lower panels). Hence, relationships between blood pressure and LVMI are greater in obese as compared to lean individuals [38]. Are there longitudinal data to support an interactive effect of obesity and hypertension on LVM?
After 8 years, the risk of developing LVH in hypertensives is 8.5 (p < 0.0001) and 4.4 (p = 0.001) times greater in obese and overweight hypertensives, respectively, compared to normal weight hypertensives [35]. Further, BMI predicts a lack of decrease in LVM over a 4-year treatment period in hypertensives independent of percentage increase in blood pressure and class of antihypertensive medication [39•]. However, a lack of reduction in LVM was also independently associated with an increase in systolic blood pressure over time [39•]. Thus, in contrast to cross-sectional data which show a steeper slope of the relationship between blood pressure and LVM index in obesity [38], longitudinal data suggest that a greater reduction in blood pressure may be required to achieve a given decrease in LVM index in obesity. To date, there are no data to show whether complete LVH regression may be achieved in obese hypertensives just with antihypertensive medication titrated to achieve lower than normal blood pressure targets.
In summary, there is sufficient evidence to support a view that obesity and blood pressure may have both additive and interactive effects on LVM. Interactive effects between obesity and blood pressure suggest that to achieve complete LVH regression, current approaches to LVH regression should target both weight loss and blood pressure reduction. Nevertheless, if weight loss programs do not achieve target body weight, then blood pressure lowering may require lower targets than currently accepted to achieve adequate LVH regression. Further studies are required to address this question.
Conclusions
The past decade has seen considerable advances in our understanding of obesity-associated LVH. It is now accepted that in overweight and obese individuals, to identify LVH and its regression, LVM should be indexed to height to an allometric signal rather than to BSA. The issue of whether height2.7 or height1.7 should be employed nevertheless still requires resolution, but sex-specific thresholds for both have been provided. Second, there is sufficient evidence to indicate that in patients with obesity-associated LVH, obesity may be the cause of either concentric or eccentric LV remodeling. Hence, clinically, it is a spurious assumption that the presence of concentric LVH indicates a cause of LVH other than obesity. Third, there is sufficient evidence to support a view that obesity and blood pressure may have both additive and interactive effects, and that both weight loss programs and blood pressure reduction are required to achieve appropriate LVH regression. If weight loss programs do not achieve target body weight, then blood pressure lowering may require lower targets than currently accepted to achieve adequate LVH regression.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Vakili BA, Okin PM, Devereux RB. Prognostic implications of left ventricular hypertrophy. Am Heart J. 2001;141:334–41.
Verdecchia P, Angeli F, Borgioni C, et al. Changes in cardiovascular risk by reduction of left ventricular mass in hypertension: a meta-analysis. Am J Hypertens. 2003;16:895–9.
Gerdts E, Cramariuc D, de Simone G, et al. Impact of left ventricular geometry on prognosis in hypertensive patients with left ventricular hypertrophy (the LIFE study). Eur J Echocardiogr. 2008;9:809–15.
Krumholz HM, Larson M, Levy D. Prognosis of left ventricular geometric patterns in the Framingham Heart Study. J Am Coll Cardiol. 1995;25:879–84.
Mancia G, Fagard R, Narkiewicz K, et al. ESH/ESC guidelines for the management of arterial hypertension. Eur Heart J. 2013;34:2159–219.
Finucane MM, Stevens GA, Cowan MJ, et al. National, regional, and global trends in body-mass index since 1980: systematic analysis of health examination surveys and epidemiological studies with 960 country-years and 9.1 million participants. Lancet. 2011;377:557–67.
Alpert MA, Omran J, Mehra A, Ardhanari S. Impact of obesity and weight loss on cardiac performance and morphology in adults. Prog Cardiovasc Dis. 2014;56:391–400.
de Simone G, Izzo R, De Luca N, Gerdts E. Left ventricular geometry in obesity: is it what we expect? Nutr Metab Cardiovasc Dis. 2013;23:905–12.
Chirinos JA, Segers P, De Buyzere ML, et al. Left ventricular mass: allometric scaling, normative values, effect of obesity, and prognostic performance. Hypertension. 2010;56:91–8. This paper introduced the allometric exponent of 1.7 which eliminated the residual negative relationship between LVM indexed to height 2.7 and height. Sex- and ethnic-specific thresholds of LVM indexed to body surface area and height 1.7, as well as comparisons of the prognostic values of LVM indexed to body surface area, height 2.7 and height 1.7 are provided.
Sibiya MJ, Norton GR, Hodson B, et al. Gender-specific contribution of aortic augmentation index to variations in left ventricular mass index in a community sample of African ancestry. Hypertens Res. 2014;37:1021–7.
Booysen HL, Woodiwiss AJ, Sibiya MJ et al. Indexes of aortic pressure augmentation markedly underestimate the contribution of reflected waves toward variations in aortic pressure and left ventricular mass. Hypertension. 2015 (in press).
de Simone G, Daniels SR, Devereux RB, et al. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol. 1992;20:1251–60.
de Simone G, Kizer JR, Chinali M, et al. Normalization for body size and population—attributable risk of left ventricular hypertrophy. The Strong Heart Study. Am J Hypertens. 2005;18:191–6.
Paajanen TA, Oksala NK, Kuukasjarvi P, et al. Short stature is associated with coronary heart disease: a systematic review of the literature and a meta-analysis. Eur Heart J. 2012;31:1802–9.
de Simone G, Devereux RB. Method errors or unexplained biological information? Hypertension. 2010;56:e177–8. This letter compared the prognostic values of LVM indexed to body surface area, height 2.7 and height 1.7 and emphasized the importance of population attributable risk.
Poppe KK, Edgerton Bachmann M, Triggs CM, et al. Geographic variation in left ventricular mass and mass index: a systematic review. J Hum Hypertens. 2012;26:420–9.
Lang RM, Bierig M, Devereux R, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;8:1440–63.
Aurigemma GP, de Simone G, Fitzgibbons TP. Cardiac remodelling in obesity. Circ Cardiovasc Imaging. 2013;6:142–52.
Messerli FH, Sundgaard-Riise K, Reisin E, et al. Dimorphic cardiac adaptation to obesity and arterial hypertension. Ann Intern Med. 1983;99:757–61.
Bastien M, Poirier P, Lemieux I, Despres J-P. Overview of epidemiology and contribution of obesity to cardiovascular disease. Prog Cardiovasc Dis. 2014;56:369–81.
Gerdts E, de Simone G, Lund BP, et al. Impact of overweight and obesity on cardiac benefit of antihypertensive treatment. Nutr Metab Cardiovasc Dis. 2013;23:122–9.
Woodiwiss AJ, Libhaber CD, Majane OHI, et al. Obesity promotes left ventricular concentric rather than eccentric geometric remodeling and hypertrophy independent of blood pressure. Am J Hypertens. 2008;21:1144–52.
Turkbey EB, McClelland RL, Kronmal RA, et al. The impact of obesity on the left ventricle: the multi-ethnic study of atherosclerosis (MESA). JACC Cardiovasc Imaging. 2010;3:266–74. This large study (over 5000 participants) assessed the impact of obesity on left ventricular mass and geometry using cardiac magnetic resonance imaging (MRI), hence avoiding the possibility of poor echocardiographic windows in obesity.
Neeland IJ, Gupta S, Ayers CR, et al. Relation of regional fat distribution to left ventricular structure and function. Circ Cardiovasc Imaging. 2013;6:800–7. In this large study (2710 participants) dual energy x-ray absorptiometry and magnetic resonance imaging were used to assess fat distribution. Visceral adipose tissue (central obesity) was shown to be associated with concentric LV remodelling; whereas lower body subcutaneous fat was associated with eccentric LV remodelling.
Kardassis D, Bech-Hanssen O, Schonander M, et al. The influence of body composition, fat distribution, and sustained weight loss on left ventricular mass and geometry in obesity. Obesity. 2012;20:605–11.
Cuspidi C, Rescaldani M, Sala C, Grassi G. Left-ventricular hypertrophy and obesity: a systematic review and meta-analysis of echocardiographic studies. J Hypertens. 2014;32:16–25. This is a meta-analysis of echocardiographic studies showing that although obesity is largely associated with eccentric LV remodelling, a significant proportion of concentric LV remodelling was also observed. It is important to note that no adjustments for either the presence of hypertension or blood pressure were made in these studies.
Khouri MG, Peshock RM, Ayers CR, et al. A 4-tiered classification of left ventricular hypertrophy based on left ventricular geometry: the Dallas heart study. Circ Cardiovasc Imaging. 2010;3:129–31.
Owan T, Avelar E, Morley K, et al. Favorable changes in cardiac geometry and function following gastric bypass surgery: 2-year follow-up in the Utah obesity study. J Am Coll Cardiol. 2011;57:732–9.
Hsuan C-F, Huang C-K, Lin J-W, et al. The effect of surgical weight reduction on left ventricular structure and function in severe obesity. Obesity. 2010;18:1188–93. An intervention study assessing changes in LV mass and geometry 3 months after bariatric surgery, which showed that blood pressure reduction was the most important determinant of the regression of LV mass and relative wall thickness.
Luaces M, Cachofeiro V, Najar B+G-M-A, et al. Anatomical and functional alterations of the heart in morbid obesity. Changes after bariatric surgery. Rev Esp Cardiol. 2012;65:14–21.
Cuspidi C, Rescaldami M, Tadic M, et al. Effects of bariatric surgery on cardiac structure and function: a systematic review and meta-analysis. Am J Hypertens. 2014;27:146–56. A meta-analysis of 23 bariatric surgery studies showing that a significant decrease in relative wall thickness (and hence a less concentric LV geometry) occurred together with reductions in LVM and LVM indexed to height 2.7.
de las Fuentes L, Waggoner AD, Mohammed S, et al. Effect of moderate diet-induced weight loss and weight regain on cardiovascular structure and function. J Am Coll Cardiol. 2009;54:2376–86.
Rider OJ, Lewandowski A, Nethononda R, et al. Gender-specific differences in left ventricular remodelling in obesity: insights from cardiovascular magnetic resonance imaging. Eur Heart J. 2013;34:292–9.
de Gonzalez BA, Hartge P, Cerhan JR, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2011;363:2211–9.
Palatini P, Saladini F, Mos L, et al. Obesity is a strong determinant of hypertensive target organ damage in young-to-middle-age patients. Int J Obesity. 2013;37:224–9.
Gidding SS, Liu K, Colangelo LA, et al. Longitudinal determinants of left ventricular mass and geometry: the coronary risk development in young adults (CARDIA) study. Circ Cardiovasc Imaging. 2013;6:769–75. This is a large (2426 participants) longitudinal study which identified the determinants of increases in LV mass and relative wall thickness over 20 years.
Avelar E, Cloward TV, Walker JM, et al. Left ventricular hypertrophy in severe obesity: interactions among blood pressure, nocturnal hypoxemia, and body mass. Hypertension. 2007;49:34–9.
Norton GR, Majane OHI, Libhaber E, et al. The relationship between blood pressure and left ventricular mass index depends on an excess adiposity. J Hypertens. 2009;27:1873–83.
Simone G, Devereux RB, Izzo R, et al. Lack of reduction of left ventricular mass in treated hypertension: the strong heart study. J Am Heart Assoc. 2013;2:e000144. This is a longitudinal study which assessed the predictors of LVM regression.
Compliance with Ethics Guidelines
Conflict of Interest
Angela J. Woodiwiss and Gavin R. Norton declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
The authors data described in this article were part of studies conducted according to the principles outlined in the Helsinki declaration and approved by the Committee for Research on Human Subjects of the University of the Witwatersrand (approval numbers M02-04-72, renewed as M07-04-69 and M12-04-108). Participants gave informed consent. This article does not contain any studies with animal subjects performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Hypertension and Obesity
The authors are supported by the Medical Research Council of South Africa, the University Research Council of the University of the Witwatersrand, the National Research Foundation, the Circulatory Disorders Research Trust, and the Carnegie Corporation.
Rights and permissions
About this article
Cite this article
Woodiwiss, A.J., Norton, G.R. Obesity and Left Ventricular Hypertrophy: The Hypertension Connection. Curr Hypertens Rep 17, 28 (2015). https://doi.org/10.1007/s11906-015-0539-z
Published:
DOI: https://doi.org/10.1007/s11906-015-0539-z