Abstract
Background
Bariatric surgery is currently the most effective treatment for morbid obesity. These procedures change the gastrointestinal system with the aim of reducing dietary intake. Improving diet quality is essential in maintaining nutritional health and achieving long-term benefits from the surgery. The aim of this systematic review was to examine the relationship between bariatric surgery and diet quality at least 1 year after surgery.
Methods
A systematic search of five databases was conducted. Studies were included that reported diet quality, eating pattern, or quality of eating in adult patients who had undergone laparoscopic-adjusted gastric banding (LAGB), Roux-en-Y gastric bypass (RYGB), and sleeve gastrectomy (SG) procedures. Data was extracted to determine the relationship between having had bariatric surgery and subsequent diet quality.
Results
A total of 34 study articles (described in 36 articles) met the inclusion criteria. The majority of studies were observational in nature and showed a reduction in energy intake following surgery, as well as inadequate intakes of micronutrients and protein, and an excessive intake of fats. There was evidence of nutrient imbalances, suboptimal compliance with multivitamin and mineral supplementation, and limited follow-up of patients.
Conclusion
The current evidence base suggests that despite being effective in reducing energy intake, bariatric surgery can result in unbalanced diets, inadequate micronutrient and protein intakes, and excessive intakes of fats. In combination with suboptimal adherence to multivitamin and mineral supplementation, this may contribute to nutritional deficiencies and weight regain. There is a need for high-quality nutrition studies, to identify optimal dietary compositions following bariatric surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery is currently the most effective treatment for the chronic condition of obesity. It results in a substantial weight loss, reduces the risk of comorbidities associated with excess weight, and improves quality of life [1]. Bariatric procedures change the anatomy and physiology of the gastrointestinal system and hence have an impact on diet quality, digestion, and absorption of food and nutritional status [2, 3]. Following surgery, the volume of food consumed and hence energy intake is significantly reduced [2]. However, diet quality can be compromised, particularly if gastrointestinal symptoms are experienced from ingesting certain foods. While the gastrointestinal system adapts over time and increased food intake has been reported [4, 5], malabsorption of nutrients may persist due to the anatomical changes. In general, the restrictions in diet quality and food intolerances are a problem in the first year following surgery. A balanced diet is expected to be tolerated by most patients, after this period of adjustment. Some foods may continue to present as challenges, even in the longer term. These food intolerances may contribute to avoidance of food groups and this in turn may impact diet quality [6, 7]. The extent of dietary change and associated nutritional consequences varies between procedures. The lap-adjusted gastric banding (LAGB) procedure appears to induce more gastrointestinal symptoms and hence food intolerances than sleeve gastrectomy (SG) and the Roux-en-Y gastric bypass (RYGB) procedure [6, 8]. This can affect the quality of the long-term diet consumed by patients.
Studies on dietary tolerance post bariatric surgery have been inconsistent, despite reports that the majority of patients tolerated most food groups [9]. A trend towards healthier food consumption and significantly better food tolerance over time has been shown in patients following SG [10]. Other studies have shown the opposite, with some patients continuing to experience problems with tolerance of basic (core) foods, due to adverse gastrointestinal symptoms, whereas others might choose to return to pre-operative suboptimal eating habits [11, 12]. Understanding what is happening in this clinical population is important, as adequate intake of protein, maintaining optimal nutritional status, and improving diet quality and lifestyle is essential in maintaining weight loss and improving long-term health [11].
Given that obesity is recognized as a chronic and relapsing condition, a long-term treatment plan for all contributing factors including diet and lifestyle is needed. The current bariatric guidelines focus on the dietary and nutritional recommendations in the first post-operative year, but there is very little evidence supporting the diet quality of patients in the long term [13]. Few studies have reported on the optimal long-term diet composition following bariatric surgery [14, 15] and there is a lack of high-quality evidence describing the optimal diet. In order to develop dietary guidelines for the long-term, an evaluation of the current evidence base is required. Hence, the aim of this systematic review was to examine the relationship between bariatric surgery and diet quality at least 1 year after surgery.
Method
Search Strategy
A systematic search of the databases Medline (EBSCO), PubMed, Scopus, Cochrane Central Registry of Controlled Trials, and CINAHL (EBSCO) (all years to October 2018) was conducted. The search terms used in Medline were as follows: ((MH “Bariatric Surgery+”) OR bariatric surgery OR Sleeve Gastrectomy OR Roux-en-Y Gastric Bypass OR gastric bypass) AND (“diet quality” OR “food groups” OR (MH”Diet+”) OR “nutrition”) (see Appendix for search tearm for Scopus).
The review protocol was pre-registered in PROSPERO in September 2018. The protocol can be accessed at: http://www.crd.york.ac.uk/PROSPERO/display_record.php?ID=CRD42018106564. This systematic review was reported according to The Preferred Reporting Items for Systematic Reviews and Meta- Analysis (PRISMA) statement [16].
Selection Criteria
Included studies were those conducted in human adults aged 18 years and older, who had undergone LAGB, gastric bypass and SG (Reviewer #2 Comment #2), and reported on diet quality: nutritional outcomes, macro- and micronutrient intake, and quality of eating beyond 1-year post-operative. This post-operative period was selected, as at this stage, the gastrointestinal system should have adjusted well enough for the patients to be able to tolerate a full consistency bariatric diet [17].
Initially, titles and abstracts were screened, with potentially eligible articles retrieved for full-text review. Article selection was conducted by the same researcher (NZ) and a second reviewer (EN) consulted in the case of ambiguity.
Critical Appraisal/Quality Assessment
The main researcher (NZ) assessed the methodological quality of all the included papers using the American Dietetic Association evidence appraisal tool checklist [18]. A second reviewer with expertise in systematic reviews (EN) independently reviewed the included papers, and in case of any ambiguities, a third expert reviewer (LT) was consulted. Studies were also categorized according to Australia’s National Health and Medical Research Council (NHMRC) level of evidence guidelines: level I reflecting the highest level of evidence and level IV the lowest [19].
Data Extraction
Data was extracted by the principle investigator (NZ) and checked for accuracy by a second reviewer (EN). A standardized table was used to extract data and included details on study design, methodology, and study characteristics (patient demographics, surgical procedures, length post-operative of time, anthropometric measures, and dietary methodology). Dietary intake results were extracted for both the pre- and post-operative stage and these included energy intake, macro- and micronutrient intake, food intolerances, and adherence to multivitamin and mineral supplementation. Where additional details were required, authors were contacted to clarify details and provide further information. Due to the nature of studies and their variability in methodology, it was not considered appropriate to conduct a meta-analysis.
Results
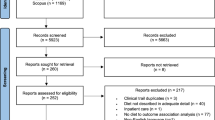
The initial search retrieved 3972 papers and 2184 papers were screened after removing 1789 duplicates. Full texts of 293 articles were reviewed, and subsequently 36 articles (describing 34 separate studies) met the inclusion criteria (Fig. 1).
Description of Studies
The studies were generally observational and classified as level IV evidence according to the NHMRC level of evidence criteria [19]. One prospective cohort study was part of a randomized controlled trial [20]. In one study [14], the participants were recruited from the Swedish Obese Subjects Study, which was a matched prospective trial (nonrandomized) that compared bariatric surgery with usual care for obese patients (Table 1). The studies were conducted across the world, including Asia, Australia, the Middle East, Europe, and North and South America. The sample size ranged from 17 to 1610 [14]. However, the majority of studies (n = 25) had a sample size of < 100. The majority of participants were female, with several papers reporting only on females [5, 17, 21,22,23,24,25]. The participants’ age ranged from 33 to 52 years.
The surgical intervention in the majority of studies (n = 20) was a standard RYGB, mostly performed laparoscopically. Few studies reported on banded RYGB [21,22,23], and in two studies, the RYGB was performed as an open procedure [11, 26]. There were only two articles (one study) presenting data following LAGB [3, 27] and four studies on SG [10, 20, 28, 29]. Two studies reported on both SG and RYGB [30,31,32] and others reported on a mixture of procedures [4, 6, 9, 14, 30,31,32,33,34]. Two studies also reported on historical techniques or procedures [4, 9].
The follow-up period of the studies as per our inclusion criteria was a minimum of 1-year post-operative and the majority of study follow-ups were < 3 years. Only three studies (n = 11) reported data on 5, 8, and 10 years post-operative [5, 14, 29]. Only a third of studies reported follow-up rates and these were found to decrease as time lengthened post surgery. The values were varied with follow-up at 1 year found to be in the range of 32–96%, at 18 months 15–38%, at 2 years 69.7–86%, at 3 years 10–64%, and at 5 years and beyond 3–59%.
Anthropometry
The pre-operative weight ranged from 115.8 ± 13.7 to 145.7 ± 40 kg, with BMI ranging from 30 ± 5.5 to 54.9 ± 8.9 kg/m2 (Table 1). Anthropometric changes were reported by almost all studies. Studies presenting data at 1-year post-operative showed a weight loss in the range of 26–32 kg and an excess weight loss (EWL) range of 58–77%. Those with data from 2–5 years post-operative showed 32–34% weight loss or 58% EWL. Only a small number of studies had over 5 years of data, with Kanerva et al. reporting a 14.9% weight loss in men and 16.9% weight loss in woman at 10 years post-operative [14].
Assessment of Dietary Intake
Dietary assessment methods utilized in the studies are summarized in Table 2. These methods were mostly retrospective in nature and included 24-h food recall, food frequency questionnaire, and other invalidated questionnaires. Studies generally used a self-administered questionnaire; however, assistance in person or via the phone in completing these was reported in 15 studies (44%) [3, 5, 7, 9, 11, 17, 24, 26, 27, 32, 35,36,37].
Energy Intake
A total of fourteen studies reported nutritional intake pre-operatively, with some only reporting energy intake, whereas others explored food groups or the macronutrient intake and diet composition. The range of pre-operative energy intake in these studies was 2005 to 3312 kcal/day (RYGB). One study reported pre-operative energy intake of SG patients to be 1658 kcal/day [30].
Energy intake following surgery was reported by twenty-five studies [2,3,4,5, 7, 11, 17, 20, 21, 24,25,26, 28,29,30,31,32, 35,36,37,38,39,40,41,42]. They collectively showed a substantial reduction in energy intake, up to a 50 to 68% reduction in some studies [28, 29], with a large range in values. The total reported energy intake less than 2 years pre-operatively ranged from 1006 kcal/day [28] to 2131 kcal/day [40]. These changes in all studies were reported to be statistically significant where compared to the pre-operative energy intake. Only one article reported energy intake following LAGB [3] with an estimated intake of 4894 ± 2360 kJ and a range of 1137 to 13,176 kJ (270–3137 kcal).
A total of eight studies [4, 5, 11, 28, 29, 31, 39, 40] reported energy intake beyond 1 year following surgery, showing an increase over time. Once again, a large range was observed with a caloric intake per day of 900 [28] to 2425 [40] at 2 years post-operative, 1386 at 3 years post-operative [4], 1221 to 1625 for up to 5 years post-operative [11, 29, 31], and 1680 kcal at 8 years following surgery [5]. Studies that compared the energy intake following RYGB vs. SG [30,31,32] did not find a statically significant difference between these surgical groups.
Macronutrient and Food Group Intake
A total of eleven studies reported the percentage of energy intake from macronutrients pre-operatively (Table 2) [2, 4, 5, 14, 20, 28, 30, 31, 36, 40, 41], with generally an adequate protein, suboptimal carbohydrate, however excessive fat intake compared to dietary recommendations [43]. Only two studies looked at food groups pre-operatively and compared this to recommendations [30, 41]. The post-operative macronutrient intake is summarized in Table 2, with protein intake ranging from 95 ± 35.9 to 163.9 ± 123.8 g, carbohydrates from 224.7 ± 128.6 to 432.6 ± 51 g, and fat intake from 89 ± 7 to 177 ± 25.3 g. Fiber intake was only reported by three studies [2, 28, 41]. Percentage of macronutrient contribution to energy compared to dietary recommendations is summarized in Table 3. The comparison was made based on recommendations by Moize et al. and Kanerva et al. [14, 15] and based upon data which show that such diet composition was found to be most adequate in promoting weight loss and weight maintenance long term, following bariatric surgery.
Micronutrient Intake
The dietary intake of several micronutrients was shown to be inadequate compared to published recommendations (see Table 2 for recommendations used as references for individual studies) in several studies. These included vitamins D, E, C, folate, B12, B1, copper, zinc, calcium, and iron [2, 7, 17, 21, 23, 24, 27, 31, 41].
Food Intolerances and Changes in Preferences
Tolerance of food and satisfaction with diet quality was assessed and reported by 12 studies [6, 9, 10, 20, 22, 23, 26, 28, 33, 35,36,37]. Six studies (Kafri et al. 2011, Freeman et al. 2014, Coluzzi et al. 2016, Cano-Valderrama et al. 2017, Dagan et al. 2017) used a validated questionnaire to assess food tolerance following bariatric procedures. Coluzzi et al., Dragan et al., and Kari et al. showed an improvement in the eating questionnaire score over time, following SG, suggesting an improvement in food tolerance and hence quality of nutrition over time. Freeman et al. [6] assessed food tolerance and diet quality in a control group and following LAGB, SG, and RYGB. They found a superior food tolerance score in the control and the SG group followed by the RYGB compared to the LAGB (p < 0.001).
Gastrointestinal Symptoms and Other Side Effects
Gastrointestinal side effects were reported by several studies [6, 9, 20, 24, 28, 32, 37, 38] and these included vomiting, nausea, reflux, regurgitation, hiccups, flatulence, dumping syndrome (fast heartbeat and diarrhea after eating), altered bowel motion (diarrhea and constipation), and, to a lesser extent, weakness, dizziness, abdominal pain, and general malaise. These were inconsistent, for example, vomiting reported from as low as 5.2% of patients [20] to as high as 67% [37]. In general, beyond 1-year post-operative, these symptoms were present in < 30% of patients following SG and RYGB. Compared to other procedures, in a small study, patients following LAGB reported a significant higher incidence of vomiting and regurgitation compared to RYGB and SG [6].
Adherence to Supplementation
Only a small number of studies reported on adherence to vitamin and mineral supplementation [10,11,12, 20, 30, 36, 37]. In general, they showed a better adherence to the multivitamin supplement compared to other specific supplements such as calcium, iron, B12, and vitamin D [37]. Furthermore, the adherence to taking supplements decreased over time with 20–32% of patients reporting stopping or never taking their recommended supplements by 1 year post-operative [10, 36, 42].
Discussion
This systematic review is the first to report on the available evidence on diet quality beyond 1 year following the current main bariatric procedures (SG, RYGB, and LAGB). The results suggest that despite the benefits of the procedure, dietary intake after a year or more remained unbalanced, with an excessive intake of fats and an inadequate intake of protein. There was evidence of nutrient imbalances before and after surgery, inconsistent adherence to supplements, and poor long-term follow-up. To maintain the benefits of surgery and achieve optimal nutritional status, changes in eating habits and adherence to nutritional supplements as well as long-term nutritional assessment and counseling by a qualified dietitian are recommended.
The main surgical intervention in most studies was RYGB (n = 20), with less data available for LAGB [3, 27] and SG [10, 20, 28, 29]. A few studies reported on combinations of procedures [4, 6, 9, 14, 32, 34]. This highlights the long history and international preference for the RYGB as the surgical choice for obesity management. LAGB has been performed for over 20 years; however, very few studies have studied its nutritional implications and despite the international rise in popularity of the SG [44], long-term nutritional and dietary information following this procedure is limited. We did not identify any studies on one anastomosis gastric bypass (OAGB) in this review. Hence, there is limited information on nutritional consequences following SG and LAGB and a gap in the literature on nutritional impact following OAGB.
The review exposed evidence of a significant weight loss following all bariatric procedures. The maximum weight loss appeared in the first year, followed by a period of weight stabilization and then subsequent weight regains [5, 11, 14, 29, 42]. Over 60% of patients appeared able to achieve a weight loss in excess of 50%, which is considered a successful result [11, 20, 37]. In those experiencing weight regain however, poor diet quality, excessive intake of carbohydrates, sweets, fats, and alcohol, and inadequate follow-up appeared to be contributing factors [11, 25, 33, 38, 42]. RYGB and SG were found to produce similar weight loss and nutritional consequences [30,31,32], but this was better than for LAGB [6, 34]. The LAGB is a purely restrictive procedure with no changes to the gastrointestinal peptides and hence may have a lesser impact on hunger and satiety as RYGB and SG [45]. Furthermore to date, LAGB has not been shown to affect energy metabolism, and hence, patients may still be hungry and dissatisfied with the volume of food that is tolerated. It is challenging to find the right volume of fluid adjustment for each patient. In fact, the fluid volume level needed to achieve adequate restriction, and hence, weight loss may result in obstructive symptoms and hence poor diet quality. This leads to reduced protein and micronutrient intake as well as maladaptive eating habits and hence inadequate weight loss [3, 6, 27]. These factors may explain the reduction in the number of LAGB being performed [44].
Bariatric procedures aim to reduce the volume of food consumed and consequently dietary energy. In patients presenting for bariatric surgery, pre-operative energy intake is reported to be excessive of energy requirements, albeit under-reported [30]. We found a large range in reported pre-operative energy intake which may reflect the variation in the dietary assessment tools in addition to the expected level of under-reporting [46]. The methodological problem may persist post-operatively, influencing reported outcomes. Our review was consistent with other studies in showing reductions in energy intake following RYGB and SG procedures, but with a gradual increase over the years [2, 20, 39]. Our data on LAGB was very limited, with only one article reported energy intake following this procedure [3]. The substantial variation reported here (4894 ± 2360 kJ; 1137 to 13,176 kJ (270–3137 kcal)) related to the nature of the LAGB and the need for an optimal adjustment of the band fluid levels. Over adjustment may adversely affect the adequacy of the diet leading to a lower energy intake than recommended for the general and post-bariatric population. Conversely, under adjustment may allow excessive intake in some patients contributing to suboptimal weight loss.
Our review found that patients presenting for bariatric surgery appeared to have adequate dietary protein intake, however were consuming a higher intake of fat compared to recommendations [43]. The details on types of fat were not provided [2, 4, 5, 14, 20, 28, 30, 31, 36, 40, 41], limiting further conclusions. Excessive energy intake from fats may be a contributing factor to the chronic condition of obesity and comorbidities such as coronary heart disease and hyperlipidemia. From a food perspective, two studies reported a low intake of dairy, fruit, vegetables, and whole grains compared to recommendations [30, 41]. Fiber intake was also below the recommendation of > 25 g/day for women and > 30 g/day for men [43], although fiber intake was only reported in three studies [2, 28, 41]. Regardless of the nutritional variable examined, there was consistent reporting of poor diet quality in patients with obesity and those presenting for weight loss surgery, which is consistent with other similar studies [47]. However, it should be noted that this pattern of dietary intake is very similar to that of the general population. National nutrition surveys report a suboptimal intake of fruit, vegetables, and high-fiber grains and an excessive intake of discretionary and processed foods. The western diet appears to continue to contribute the condition of obesity and related illnesses.
Overall, the results of this review suggest that the diet quality of post-bariatric surgical patients is unbalanced (Table 3). Only two studies were used as references to assess post-operative diet adequacy [14, 15]. The first developed a bariatric specific dietary and nutritional recommendations and presented these as a “bariatric food pyramid” in assisting patient education [15]. The second study proposed an optimal diet composition for better long-term weight loss [14]. Twelve studies reported an inadequate intake of protein and 13 studies reported an excessive intake of fats. The situation for carbohydrate intake was less consistent, reported as adequate in 14 studies and excessive in seven studies. Hence, it seems than an unbalanced dietary pattern may contribute to suboptimal weight loss, weight regains, and hence poor health outcomes in the long term [3, 12, 25, 38, 42].
Due to the expected restriction and reductive nature of bariatric procedures, it may be inappropriate for post-operative patients to be expected to meet the same recommendations for food volume as the general population. National dietary guidelines [43] are appropriate for a relatively healthy population and are not designed to meet the needs of the post-operative patient following significant weight loss. Bariatric patients suffer from the chronic and pro-inflammatory condition of obesity and its related comorbidities (diabetes, insulin resistance, fatty liver) [1]. They are also expected to experience a significant weight loss and change in metabolism after surgery and need specific dietary guidelines for the long term.
From a micronutrient perspective, intakes following bariatric surgery were assessed in several studies and compared to specific nutrient reference values of the relevant country. These results suggested inadequate dietary intakes of several micronutrients such as vitamins D, E, C, folate, B12, B1, copper, zinc, calcium, and iron [2, 7, 17, 21, 23, 24, 27, 31, 41]. The reasons for these findings were multifactorial and included a reduced volume of food intake [7], intolerance to certain food groups [6, 17, 27], and consuming an unbalanced diet by choice, with low intakes of associated sources of micronutrients [41]. This reinforces the need for adherence to vitamin and mineral supplementation ongoing nutritional assessment and counseling by a qualified dietitian as well as long-term follow-up as per bariatric guideline [13, 48, 49].
Food intolerances are common following bariatric surgery, however are inconsistently defined [6, 9, 10, 20, 22, 23, 26, 28, 33, 35,36,37]. Some of these intolerances observed could be beneficial as they may deter patients from choosing energy-dense food items through a negative feedback mechanism such as dumping syndrome, while others such as problems eating meat and dairy could be detrimental to the quality of the diet of the patient. Intolerances to breads and cereals, meat, and meat alternatives have been shown to be associated with reduced intake of these food groups [6]. In addition, other studies show a lower protein intake in those with protein intolerance [26]. The most reported food intolerances reported were red/tough meat, rice, bread, pasta, dairy, and fibrous vegetables and skin of fruit to a lesser extent. Some of these intolerances could persist up to 3 years following surgery but in general, it appears that food tolerance improves over time following RYGB and SG surgery [9]. This suggests an adaptation of the gastrointestinal system over time following these procedures [8].
Another nutritional aspect is changes in taste and food preferences, which was found in studies following RYGB [50, 51] where there was a tendency to dislike sweet, fatty, and calorie-dense foods. However, whether taste changes are sustained long term has not been fully evaluated. For example, one study on SG patients [28] found after an initial reduced interest in sweets, this was only sustained by 25% at 12 months and 23% at 24 months (p = 0.001). An increased interest in sweet foods can contribute to the excessive intake of sweets, increased energy intake, and leading to an unbalanced diet and weight regain [11]. This highlights the importance of improving eating habits in the first year following surgery and not relying solely on the initial benefits of the operation.
Our review did not specifically search for side effects of bariatric surgical procedures but these were noted when studies reported post-operative side effects [6, 9, 20, 24, 28, 32, 37, 38]. The reductive and restrictive nature of bariatric procedures contributes to the expected gastrointestinal side effects such as vomiting, nausea, reflux, regurgitation, hiccups, and constipation. These symptoms may be more prevalent and last longer following LAGB due to the presence of the foreign body and the need for optimal adjustment of the band alongside changes in eating habits. This may affect the quality of diet and digestion more than other procedures [6, 8, 34]. The response to LAGB surgery varies, so regular multidisciplinary monitoring, optimal fluid level adjustment of the band, and long-term nutritional assessment are recommended in this population. To avoid complications and nutritional inadequacies, follow-up screening should include early detection of non-responders to this procedure, including those with significant gastrointestinal symptoms, dietary intolerances, and for which an optimal band adjustment volume cannot be found, and may involve revisional or reversal procedures.
Following RYGB and SG, the change in transient time and in particular the re-routing of ingested food through the gastrointestinal system in the RYGB may lead to dumping syndrome and altered bowel motion (diarrhea and constipation) [32]. For example, in one study comparing outcomes for SG and RYGB patients, the SG group reported experiencing more heartburn and vomiting (p < 0.001), regurgitation and nausea (p < 0.01), and constipation (p < 0.05) and the RYGB group reported experiencing more flatulence, dizziness (p < 0.001), diarrhea, and fast heartbeat after eating (p < 0.5) [32]. These symptoms were more pronounced following a long-limb RYGB [52]. Assessment, prevention, and management of these gastrointestinal symptoms are an important part of the post-operative care. These symptoms, if unmanaged, may not only impact the diet quality but also affect the quality of life of patients. Other reported symptoms such as hair loss, weakness, and general malaise may be due to suboptimal protein intake shown in this population [26]; however, these areas are not well evaluated by current literature.
Overall, due to the physiological adaptation of the gastrointestinal system as well as cognitive adaptation of patients, these symptoms can improve with time; however, some patients may have persisting symptoms that could affect diet quality long-term.
Finally, a major negative clinical outcome is micronutrient deficiency and related conditions. These have been reported before and after all bariatric procedures [4, 27, 53]. We found the most commonly reported pre-operative nutritional deficiencies to relate to vitamin D status, hyper-parathyroid conditions, and low hemoglobin levels. This was consistent with the findings of other studies [53, 54]. The literature attributes the pre-operative nutritional deficiencies in this population to poor eating habits, chronic dieting, and the inflammatory nature of chronic obesity [53]. Post-operatively, reduced oral intake, food intolerances, changes in taste, and dietary preferences as well as malabsorption related to some procedures contributed to nutritional deficiencies [48]. Nutrient digestion and absorption occurs in the stomach and small bowel and this is affected in both RYGB and SG. A portion of stomach and the proximal small bowel is bypassed in RYGB. Varying length of the bypassed small intestine as well as the patient’s individual response to surgery further affect absorption of nutrients especially vitamins and minerals, with macronutrient malabsorption being quite uncommon following the standard RYGB [52]. In SG, a portion of stomach is removed and hence reducing the gastric acid content, resulting in maldigestion and subsequently malabsorption of nutrients. Because of this, similar nutrient supplements are also recommended for the SG patients [49].
The studies that reported on adherence to vitamin and mineral supplementation showed a decrease in adherence to taking supplements over time [10, 36, 42]. This in combination with lower quality diet can potentially lead to significant nutritional deficiencies. Furthermore, as lost to follow-up increases with time from surgery, so does the potential detection and treatment of these deficiencies. As a result, weight regain and poor nutritional status may increase over time.
There are several limitations to this review. Firstly, the diet assessment methodologies used in the included studies were generally self-administered and retrospective and hence carry the limitation of recall bias and under-reporting. Secondly, in the absence of specific dietary guidelines for this population, best level evidence was used when interpreting the diet adequacy of the reported studies. Finally, we limited our search to published articles and those in English language only, and hence, potentially relevant articles may have been overlooked.
This review highlights the limitation of current studies reporting on dietary intake following bariatric surgery. The studies are generally from a single center, observational in nature, and have a weak to moderate quality with low-level study designs. Furthermore, the studies are relying on self-reported, retrospective dietary data collection and hence carry the risk of under-reporting, as reported by several authors [30]. These study limitations have been cited by other authors reviewing the literature in this field [47, 55], reinforcing the need for multicenter, larger, and more consistent study designs. The majority of participants were female, and hence, the findings cannot be extrapolated to all bariatric patients. This is consistent with the majority of studies in which patients seeking bariatric surgery are generally females. This may impact the data on dietary intake due to food preferences, some studies showing that females tended to eat less protein-rich foods and more carbohydrate-rich foods [12].
With growing chronic condition of obesity and its surgical treatment options, this review highlights a need for high-quality nutrition studies in developing long-term dietary recommendations for this population. Our review suggests that bariatric surgery results in a significant reduction in energy intake, subsequent weight loss, and hence improvements in health outcomes. However, the diet composition of bariatric patients is suboptimal, the adherence to vitamin and mineral supplementation inconsistent, and the long-term follow-up poor. To maintain weight loss and optimal nutrition after surgery, change in eating habits, lifestyle change, and adherence and review of nutritional status by a qualified dietitian are recommended. Further longer term and more robust studies are needed to assist clinicians in providing nutritional care for patients following their weight loss treatment.
References
Sjöström L, Lindroos A-K, Peltonen M, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93.
Bavaresco M, Paganini S, Lima TP, et al. Nutritional course of patients submitted to bariatric surgery. Obes Surg. 2010;20(6):716–21. https://doi.org/10.1007/s11695-008-9721-6.
McGrice MA, Porter JA. What are gastric banding patients eating one year post-surgery? Obes Surg. 2012;22(12):1855–8. https://doi.org/10.1007/s11695-012-0741-x.
Brolin RE, Robertson LB, Kenler HA, et al. Weight loss and dietary intake after vertical banded gastroplasty and Roux-en-Y gastric bypass. Ann Surg. 1994;220(6):782–90.
Kruseman M, Leimgruber A, Zumbach F, et al. Dietary, weight, and psychological changes among patients with obesity, 8 years after gastric bypass. Journal of the American Dietetic Association. 2010;110(4):527–34. https://doi.org/10.1016/j.jada.2009.12.028. Language: English. Entry Date: 20100423. Revision Date: 20150819. Publication Type: Journal Article
Freeman RA, Overs SE, Zarshenas N, et al. Food tolerance and diet quality following adjustable gastric banding, sleeve gastrectomy and Roux-en-Y gastric bypass. Obes Res Clin Pract. 2014;8(2):e115–200. https://doi.org/10.1016/j.orcp.2013.02.002.
Gesquiere I, Foulon V, Augustijns P, et al. Micronutrient intake, from diet and supplements, and association with status markers in pre- and post-RYGB patients. Clinical Nutrition (Edinburgh, Scotland). 2017;36(4):1175–81. https://doi.org/10.1016/j.clnu.2016.08.009.
Suter M, Calmes JM, Paroz A, et al. A new questionnaire for quick assessment of food tolerance after bariatric surgery. Obes Surg. 2007;17:2–8.
Cano-Valderrama O, Sánchez-Pernaute A, Rubio-Herrera MA, et al. Long-term food tolerance after bariatric surgery: comparison of three different surgical techniques. Obes Surg. 2017;27(11):2868–72. https://doi.org/10.1007/s11695-017-2703-9.
Kafri N, Valfer R, Nativ O, et al. Health behavior, food tolerance, and satisfaction after laparoscopic sleeve gastrectomy. Surgery for obesity and related diseases : official journal of the American Society for Bariatric Surgery. 2011;7(1):82–8. https://doi.org/10.1016/j.soard.2010.09.016.
Freire RH, Borges MC, Alvarez-Leite JI, et al. Food quality, physical activity, and nutritional follow-up as determinant of weight regain after Roux-en-Y gastric bypass. Nutrition (Burbank, Los Angeles County, Calif). 2012;28(1):53–8. https://doi.org/10.1016/j.nut.2011.01.011.
Soares FL, Bissoni de Sousa L, Corradi-Perini C, et al. Food quality in the late postoperative period of bariatric surgery: an evaluation using the bariatric food pyramid. Obes Surg. 2014;24(9):1481–6. https://doi.org/10.1007/s11695-014-1198-x.
Aills L, Blankenship J, Buffington C, et al. Bariatric nutrition: suggestions for the surgical weight loss patient. Surg Obes Relat Dis. 2008;4(5):S73–S108.
Kanerva N, Larsson I, Peltonen M, et al. Changes in total energy intake and macronutrient composition after bariatric surgery predict long-term weight outcome: findings from the Swedish Obese Subjects (SOS) study. Am J Clin Nutr. 2017;106(1):136–45. https://doi.org/10.3945/ajcn.116.149112.
Moizé V, Pi-Sunyer X, Mochari H, et al. Nutritional pyramid for post-gastric bypass patients. Obes Surg. 2010;20:1133–41.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and metaanalyses: the PRISMA statement. BMJ (Clinical Research ed). 2009;339:b2535. https://doi.org/10.1136/bmj.b2535.
de Torres Rossi RG, Dos Santos MT, de Souza FI, et al. Nutrient intake of women 3 years after Roux-en-Y gastric bypass surgery. Obes Surg. 2012;22(10):1548–53. Epub 2012/06/13. https://doi.org/10.1007/s11695-012-0688-y.
ADA. American Dietetics Association. Evidence analysis manual: steps in ADA evidence analysis process. Chicago: Scientific Affairs and Research; 2010. p. 43–8.
NHMRC. National Health and Medical Research Council. Levels of evidence and grades for recommendations for developers of guidelines. Commonwealth of Australia.: Canberra; 2009.
Dagan S, Keidar A, Raziel A, et al. Do bariatric patients follow dietary and lifestyle recommendations during the first postoperative year? Obesity Surgery. 2017;27(9):2258–71. https://doi.org/10.1007/s11695-017-2633-6.
Novais PF, Rasera Jr I, Leite CV, et al. Food intake in women two years or more after bariatric surgery meets adequate intake requirements. Nutrition Research. 2012;32(5):335–41. https://doi.org/10.1016/j.nutres.2012.03.016.
Novais PF, Junior IR, Shiraga EC, et al. Food aversions in women during the 2 years after Roux-en-Y gastric bypass. Obes Surg. 2011;21(12):1921–7. https://doi.org/10.1007/s11695-010-0342-5.
Leiro LS, Melendez-Araújo MS. Diet micronutrient adequacy of women after 1 year of gastric bypass. Arquivos Brasileiros de Cirurgia Digestiva. 2014;27 Suppl 1:21–5.
Dias MC, Ribeiro AG, Scabim VM, et al. Dietary intake of female bariatric patients after anti-obesity gastroplasty. Clinics. 2006;61(2):93–8.
Benson-Davies S, Davies ML, Kattelmann K. Food preferences in patients after Roux-en Y gastric bypass surgery: a pilot study examining eating behaviors and weight maintenance. Topics in Clinical Nutrition. 2013;28(1):8–14. Language: English. Entry Date: 20130614. Revision Date: 20150818. Publication Type: Journal Article
Moize V, Geliebter A, Gluck ME, et al. Obese patients have inadequate protein intake related to protein intolerance up to 1 year following Roux-en-Y gastric bypass. Obes Surg. 2003;13(1):23–8.
McGrice MA, Porter JA. The micronutrient intake profile of a multicentre cohort of Australian LAGB patients. Obes Surg. 2014;24(3):400–4. https://doi.org/10.1007/s11695-013-1101-1.
Coluzzi I, Raparelli L, Guarnacci L, et al. Food intake and changes in eating behavior after laparoscopic sleeve gastrectomy. Obes Surg. 2016;26(9):2059–67. https://doi.org/10.1007/s11695-015-2043-6.
Chou JJ, Lee WJ, Almalki O, et al. Dietary intake and weight changes 5 years after laparoscopic sleeve gastrectomy. Obes Surg. 2017;27(12):3240–6. https://doi.org/10.1007/s11695-017-2765-8.
Verger EO, Aron-Wisnewsky J, Dao MC, et al. Micronutrient and protein deficiencies after gastric bypass and sleeve gastrectomy: a 1-year follow-up. Obes Surg. 2016;26(4):785–96. https://doi.org/10.1007/s11695-015-1803-7.
Moizé V, Andreu A, Flores L, et al. Long-term dietary intake and nutritional deficiencies following sleeve gastrectomy or Roux-en-Y gastric bypass in a Mediterranean population. Journal of the Academy of Nutrition & Dietetics. 2013;113(3):400–10. https://doi.org/10.1016/j.jand.2012.11.017. Language: English. Entry Date: 20130627. Revision Date: 20150711. Publication Type: Journal Article
El Labban S, Safadi B, Olabi A. The effect of Roux-en-Y gastric bypass and sleeve gastrectomy surgery on dietary intake, food preferences, and gastrointestinal symptoms in post-surgical morbidly obese Lebanese subjects: a cross-sectional pilot study. Obesity surgery. 2015;25(12 // (AUB) *American University of Beirut*):2393–9. https://doi.org/10.1007/s11695-015-1713-8.
Harbottle L. Audit of nutritional and dietary outcomes of bariatric surgery patients. Obesity Reviews: An Official Journal Of The International Association For The Study Of Obesity. 2011;12(3):198–204. https://doi.org/10.1111/j.1467-789X.2010.00737.x.
Ernst B, Thurnheer M, Wilms B, et al. Differential changes in dietary habits after gastric bypass versus gastric banding operations. Obesity Surgery. 2009;19(3):274–80.
Ortega J, Ortega-Evangelio G, Cassinello N, et al. What are obese patients able to eat after Roux-en-Y gastric bypass? Obesity facts. 2012;5(3):339–48. https://doi.org/10.1159/000339769.
Coughlin K, Bell RM, Bivins BA, et al. Preoperative and postoperative assessment of nutrient intakes in patients who have undergone gastric bypass surgery. Archives of Surgery (Chicago, Ill: 1960). 1983;118(7):813–6.
Warde-Kamar J, Rogers M, Flancbaum L, et al. Calorie intake and meal patterns up to 4 years after Roux-en-Y gastric bypass surgery. Obes Surg. 2004;14(8):1070–9. https://doi.org/10.1381/0960892041975668.
da Silva FB, Gomes DL, de Carvalho KM. Poor diet quality and postoperative time are independent risk factors for weight regain after Roux-en-Y gastric bypass. Nutrition (Burbank, Los Angeles County, Calif). 2016;32(11–12):1250–3. https://doi.org/10.1016/j.nut.2016.01.018.
Giusti V, Theytaz F, Di Vetta V, et al. Energy and macronutrient intake after gastric bypass for morbid obesity: a 3-y observational study focused on protein consumption. American Journal of Clinical Nutrition. 2016;103(1):18–24. https://doi.org/10.3945/ajcn.115.111732. Language: English. Entry Date: 20160115. Revision Date: 20160429. Publication Type: Article.
Laurenius A, Larsson I, Melanson KJ, et al. Decreased energy density and changes in food selection following Roux-en-Y gastric bypass. Eur J Clin Nutr. 2013;67(2):168–73. https://doi.org/10.1038/ejcn.2012.208.
Miller GD, Norris A, Fernandez A. Changes in nutrients and food groups intake following laparoscopic Roux-en-Y gastric bypass (RYGB). Obes Surg. 2014;24(11):1926–32. https://doi.org/10.1007/s11695-014-1259-1.
Reid RE, Oparina E, Plourde H, et al. Energy intake and food habits between weight maintainers and regainers, five years after Roux-en-Y gastric bypass. Canadian journal of dietetic practice and research. 2016;77(4):195–8. https://doi.org/10.3148/cjdpr-2016-013. Language: English. Entry Date: 20161121. Revision Date: 20161129. Publication Type: Article
NHMRC. Natonal Health and Medical Research Council. Departmnet of Health and Aging. Australian dietary guidelines: eat for health. 2013:https://www.eatforhealth.gov.au/sites/default/files/files/the_guidelines/n55_australian_dietary_guidelines.pdf.
Angarisani L, Santonicola A, Iovino P, et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25:1822–32.
Colquitt JL, Pickett K, Loveman E, et al. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8:1–244.
Goris A, Westerterp-Plantenga M, Westerterp KR. Undereating and underrecording of habitual food intake in obese men: selective underreporting of fat intake. Am J Clin Nutr. 2000;17:130–4.
Harbury CM, Verbruggen EE, Callister R, et al. What do individuals with morbid obesity report as a usual dietary intake? A narrative review of available evidence. Clin Nutr. 2016;13:15–22.
Mechanick JI, Youdim A, Jones DB, et al. Clinical practice guidelines for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient—2013 update: cosponsored by American Association of Clinical Endocrinologists, the Obesity Society, and American Society for Metabolic & Bariatric Surgery. Endocrine Practice. 2013;19(2):337–72. https://doi.org/10.4158/ep12437.Gl.
Parrott J, Frank L, Rabena R, et al. American Society for Metabolic and Bariatric Surgery integrated health nutritional guidelines for the surgical weight loss patient. Surgery for Obesity and Related Diseases. 2016;13:727–41.
le Roux CW, Bueter M, Theis N, et al. Gastric bypass reduces fat intake and preference. American Journal Of Physiology Regulatory, Integrative and Comparative Physiology. 2011;301(4):R1057–66. https://doi.org/10.1152/ajpregu.00139.2011.
Miras AD, Jackson RN, Jackson SN, et al. Gastric bypass surgery for obesity decreases the reward value of a sweet-fat stimulus as assessed in a progressive ratio task. American Journal of Clinical Nutrition. 2012;96(3):467–73. https://doi.org/10.3945/ajcn.112.036921.
Odstrcil EA, Martinez JG, Santa Ana CA, et al. The contribution of malabsorption to the reduction in net energy absorption after long-limb Roux-en-Y gastric bypass. American Journal of Clinical Nutrition. 2010;92(4):704–13. https://doi.org/10.3945/ajcn.2010.29870. Language: English. Entry Date: 20101119. Revision Date: 20151008. Publication Type: Journal Article.
Zarshenas N, Nacher M, Loi KW, et al. Investigating nutritional deficiencies in a group of patients 3 years post laparoscopic sleeve gastrectomy. Obes Surg. 2016;26(12):2936–43.
Toh SY, Zarshenas N, Jorgensen J. Prevalence of nutrient deficiencies in bariatric patients. Nutrition (Burbank, Los Angeles County, Calif). 2009;25(11–12):1150–6. https://doi.org/10.1016/j.nut.2009.03.012.
Dodsworth A, Warren-Forward H, Baines S. A systematic review of dietary intake after laparoscopic adjustable gastric banding. Journal Of Human Nutrition And Dietetics. 2011;24:327–41.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval and Informed Consent
Not applicable to the study design.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
The search terms used in Scopus were as follows:
((TITLE-ABS-KEY (“bariatric surgery”) OR TITLE-ABS-KEY (“sleeve gastrectomy”) OR TITLE-ABS-KEY (“gastric banding”) OR TITLE-ABS-KEY (“gastric bypass”) OR TITLE-ABS-KEY (“roux-en-y gastric bypass”))) AND ((TITLE-ABS-KEY (“meal pattern”) OR TITLE-ABS-KEY (“diet quality”) OR TITLE-ABS-KEY (diet*) OR TITLE-ABS-KEY (“food groups”) OR TITLE-ABS-KEY (nutri* ) ) ) AND (LIMIT TO (DOCTYPE, “ar”) OR LIMIT-TO (DOCTYPE, “re” ) ) AND (LIMIT-TO (SUBJAREA, “MEDI”) OR LIMIT-TO (SUBJAREA, “NURS”) OR LIMIT-TO (SUBJAREA, “NEUR”) OR LIMIT-TO (SUBJAREA, “PSYC”) OR LIMIT-TO (SUBJAREA, “HEAL”) OR LIMIT-TO (SUBJAREA, “SOCI” ) ) AND (LIMIT-TO (LANGUAGE, “English” ) ) AND (EXCLUDE (EXACTKEYWORD, “Animals”) OR EXCLUDE (EXACTKEYWORD, “Animal Experiment”) OR EXCLUDE (EXACTKEYWORD, “Animal”) OR EXCLUDE (EXACTKEYWORD, “Child”) OR EXCLUDE (EXACTKEYWORD, “Rat”) OR EXCLUDE (EXACTKEYWORD, “Animal Model” ) ) AND (EXCLUDE (EXACTKEYWORD, “Adolescent”) OR EXCLUDE (EXACTKEYWORD, “Nonhuman”) OR EXCLUDE (EXACTKEYWORD, “Sibutramine”) OR EXCLUDE (EXACTKEYWORD, “Unclassified Drug”) OR EXCLUDE (EXACTKEYWORD, “Pregnancy”) OR EXCLUDE (EXACTKEYWORD, “Adipose Tissue”) OR EXCLUDE (EXACTKEYWORD, “Antiobesity Agent” ) )
Rights and permissions
About this article
Cite this article
Zarshenas, N., Tapsell, L.C., Neale, E.P. et al. The Relationship Between Bariatric Surgery and Diet Quality: a Systematic Review. OBES SURG 30, 1768–1792 (2020). https://doi.org/10.1007/s11695-020-04392-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-020-04392-9