Abstract
Objectives
This systematic review and meta-analysis aimed to summarize the evidence on the associations of energy and macronutrient intakes (carbohydrates, fats, and proteins) with weight loss in adults after sleeve gastrectomy or gastric bypass and to determine whether these dietary characteristics of patients with suboptimal weight loss (SWL) or weight regain differ from those without these experiences.
Methods
PubMed, Scopus, and Web of Science were searched until December 2021. Twenty-three observational studies were included.
Results
Studies on the association of postoperative energy and macronutrients and weight loss used diverse approaches. Pooled results showed that patients with SWL consumed more energy than those with acceptable weight loss. Weight regainers consumed more energy and carbohydrates and less protein than non-regainers.
Conclusions
Higher energy consumption is related to SWL and weight regain after surgery. Associations between macronutrients and weight outcome following bariatric surgery warrant further investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery (BS) is currently the most effective option for achieving long-term weight loss and improving obesity-related diseases in individuals with morbid obesity [1, 2]. A meta-analysis showed a sustained weight reduction after BS for 10 years post-surgery, ranging from 45.8 to 80.9% excess weight loss (EWL) for various surgical methods [3]. However, nearly 20% of patients experienced suboptimal weight loss (SWL), defined as a percentage EWL of less than 50% in the first 12 months following BS [4]. Moreover, weight regain was seen in 5.7% of patients 2 years and 75.6% of patients 6 years after sleeve gastrectomy (SG) and in 50% of patients 2 years after Roux-en-Y gastric bypass (RYGB) [5, 6]. Therefore, the success of the surgery is not consistent among individuals, with some of them failing to achieve sufficient postoperative weight reduction (primary non-responders) or regaining most or all of the lost weight over time (secondary non-responders) [7]. These poor outcomes of BS lead to a recurrence of obesity-related comorbidities, worsen patients’ quality of life, and increase the BS revision rate and healthcare cost [8, 9].
Factors that predict responses to BS are typically separated into two categories: pre- and postoperative variables. Postoperative variables are considered more significant predictors of BS success than preoperative variables [7]. Dietary factors, including dietary intake and eating behavior after surgery, are proposed as one of the main postoperative risk factors for ineffective weight loss following BS [10, 11]. Identifying the dietary factors related to weight loss success following BS is essential for establishing dietary considerations to reduce the risk of SWL and weight regain. Therefore, in this systematic review and meta-analysis, we aimed to answer the following questions: (1) what is the current evidence on the associations between energy and macronutrients including carbohydrate, fat, and protein intakes and weight loss or regain the following BS in adults? (2) Are there any differences in energy and macronutrient intakes in those with SWL after BS compared to those with acceptable weight loss (AWL)? (3) Are there any differences in energy and macronutrient intakes in weight regainers (WRs) after BS compared to non-weight regainers (non-WRs)?
Method
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement was followed when conducting this systematic review and meta-analysis [12]. The protocol of this study was registered in the International Prospective Register for Systematic Reviews (PROSPERO) (registration number: CRD42022325140).
Information Sources and Search Strategy
We searched PubMed/Medline, Scopus, and Web of Science from inception to December 15, 2021. The following main keywords were used: gastric sleeve, sleeve gastrectomy, gastric bypass, weight, body mass index, BMI, body composition*, muscle mass, lean mass, carbohydrate*, protein* fat, fats, macronutrient*, food*, and eating. A full electronic search strategy for each database was provided in Supplementary Table 1. Reference lists of relevant publications were also manually searched for potentially relevant articles that were missed by the electronic search.
Study Selection
After removing duplicate publications, two researchers (ZK and FRS) independently reviewed all records based on their titles and abstracts and retrieved the full texts of studies that met the inclusion criteria. The third researcher (NM) resolved discrepancies. The population, exposure, comparison, outcomes, and study design (PICOS) of this study are shown in Supplementary Table 2. Original studies that met the following inclusion criteria were included in the study: (1) participants were over 18 years old with a history of SG or gastric bypass (GB); (2) investigated the associations of postoperative intakes of energy and macronutrients (as grams/day (g/day) or percentage of energy intake with weight outcome (either weight loss or weight regain); and (3) had observational study design. Weight loss outcome in this study included various weight loss parameters as either the absolute changes in weight (kg) and body mass index (BMI) (kg/m2) from pre-surgery or their relative changes, including %EWL, percentage of total weight loss (%TWL), and percentage of excess BMI loss (%EBMIL).
The study exclusion criteria were: (1) abstracts, reviews, conference papers, editorials, and books; (2) studies on pediatrics, adolescents, or pregnant women; (3) non-human studies; (4) studies on micronutrients or food groups intakes after BS; (5) studies on eating behaviors or food preference after BS; (6) studies assessing only preoperative dietary intakes; (7) non-English articles; (8) studies that did not report the related information; and (9) study with dietary intervention.
Data Extraction
After obtaining the full text of the studies, an investigator (ZK) extracted data from eligible studies into Microsoft Excel spreadsheets, and a second investigator (NM) validated the data extraction. The following information was extracted: first author’s name, country, year of publication, sample size, type of surgery, postoperative time, dietary assessment tool, dietary exposures, % of women, the definition of weight loss parameters, SWL cut-off, the definition of weight regain, weight regain cut-off, number of those with SWL/AWL, number of WRs/non-WRs, and main statistical parameters reported for the association of dietary intakes with weight outcomes.
Quality Assessment
The Newcastle–Ottawa quality assessment scale (NOS) was used to assess the quality of the studies by an investigator (MG) [13]. The NOS score goes from 0 (highest risk of bias, lowest quality) to 9 (lowest risk of bias, highest quality), with a score of ≥ 7 being considered high quality.
Data Synthesis and Analysis
The results of the included studies were quantitatively summarized. The weighted mean difference (MD) and 95% confidence interval (CI) were calculated using the random-effects model to estimate differences in energy and macronutrient consumption in patients with SWL compared to those with AWL after BS. Differences in energy and macronutrients according to weight regain were also investigated, by estimation of MD (95% CI) in dietary intakes among WRs versus non-WRs using the random-effects model. Heterogeneity between studies was assessed using the I2 statistic and Cochran’s Q test; substantial heterogeneity was considered as I2 > 50% [14]. Egger’s regression test was used to investigate publication bias. p < 0.10 was used as the significant criteria for heterogeneity and publication bias. The statistical analysis was done with Stata, version 14.2 (Stata Corp, College Station, TX).
Results
Study Selection
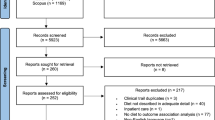
The process of study selection is shown in Fig. 1. The bibliographic searches in the three databases yielded 3683 unique articles. After excluding 3584 articles through screening of titles and abstracts, the full text of 99 articles was assessed for eligibility. Two articles were also found through manual reference checking of the retrieved articles [15, 16]. Ultimately, 23 studies were included in this systematic review and meta-analysis study [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37].
Study Characteristics
Thirteen studies were on weight loss [15,16,17,18,19,20,21,22,23,24, 29, 32, 36], eight on weight regain [25,26,27,28, 31, 33, 35, 37], and two on both outcomes [30, 34]. The characteristics of studies on weight loss after BS are reported in Table 1. These studies were published between 1983 and 2022. The mean age of participants ranged between 32.9 and 48.2 years, and they underwent GB in eleven [15, 17,18,19,20,21,22,23,24, 30, 36], SG in two [29, 34], and both in two studies [16, 32]. The sample size of the studies was between 25 and 355. Five studies had follow-up time from surgery < 12 months [15, 17, 19, 21, 29].
The characteristics of studies on weight regain after BS are reported in Table 2. The studies were published between 2012 and 2021. The mean age of the participants was 33.5–53.2 years; the type of surgery was GB in 6 [25, 27, 28, 30, 33, 35], SG in three [26, 31, 34], and both in one study [37]. The sample size of the studies ranged between 27 and 100, and the time since surgery for all studies was > 12 months.
Quality of Studies
The NOS score of the studies ranged from 3 to 9; four had a score ≥ 7 [21, 27, 35, 36]. Details of the NOS scoring are provided in Supplementary Tables 3–5.
Energy, Macronutrients, and Weight Loss
Ten studies examined associations between energy and macronutrient intakes and weight loss as continuous variables after BS [15,16,17,18,19, 21, 23, 32, 34, 36]. In the first study, postoperative changes in energy and all macronutrient intakes were significantly correlated with weight change during the first 6 months after the surgery in 25 GB patients. After 1 year, however, both protein and carbohydrate intake had increased, while fat intake had plateaued. Therefore, the authors concluded that a decrease in energy intake, predominantly from fat, may be related to weight reduction after 12 months of the surgery [17]. In the other study on energy and macronutrients over 1 year and weight reduction, energy intake was significantly related to weight loss in 50 RYGB women, whereas macronutrient composition revealed no association [15]. In a prospective study on 167 individuals undergoing RYGB, daily intake of protein per kg of body weight was positively related to BMI change and %EWL at 6 and 12 months after the surgery [21]. In contrast, a study on 53 patients with at least 6 months post-RYGB suggested carbohydrate intake as an important determinant of weight loss, accounting for 28.5% of the variance in average monthly excess weight loss (AMWL). In that study, a greater AMWL was linked with lower energy (r = − 0.373, p = 0.007), carbohydrate (g/day) (r = − 0.414, p = 0.003), and fat (g/day) (r = − 0.283, p = 0.044) intakes [19].
Among the studies with more than 12 months of follow-up, one study in 69 patients with a mean time since RYGB of 30 ± 8 months found that energy and fat intake (% of energy), along with other variables including age, excess weight, and weight before surgery, accounted for 47% of the %EWL [18]. In another study involving 86 patients undergoing SG, energy (r = − 0.54) and fat (r = − 0.35) were inversely correlated with %EWL at 7 years post-surgery [34]. In contrast, a cross-sectional study in 107 RYGB patients with a mean time since surgery of 3 ± 1.8 years demonstrated that only energy intake (not macronutrients) is associated with %EBMIL [23]. Consistent with the finding, a prospective study on 355 patients undergoing SG and RYGB demonstrated that energy intake, but not the proportion of individual macronutrients, independently predicted %EWL after 5 years [16]. Controlling for relevant confounders, another study showed that a greater decrease in energy intake is associated with a higher %TWL (β = − 0.004, p = 0.014) in 135 individuals undergoing SG and RYGB who were followed for more than 4 years [32]. Protein intake 1 year after RYGB was not related to %TWL at the mid-term (2–3 years) or long term (4–5 years) after the surgery in a retrospective study [36].
Two studies defined dietary intake as a categorical variable. One that evaluated the %EWL across three groups of patients with different energy intakes revealed that the mean %EWL of those with a greater energy intake did not differ significantly from those with a lower energy intake after 1–5 years post-RYGB [22]. Another one compared the mean of %TWL based on protein intake groups of < 60 and ≥ 60 g/day that found no significant differences in %TWL between the two groups at 6 and 12 months after SG [29].
Energy, Macronutrients, and Suboptimal Weight Loss
In four studies, participants were divided based on the rate of weight loss, and then energy and macronutrient intakes were compared across the groups of participants [18, 20, 24, 30]. Participants in the four studies underwent RYGB. All of the studies defined SWL as 50% of EWL and looked at macronutrients as a percentage of energy, except for one, which used g/kg body weight to measure protein intake [20]. Patients were divided into two groups (< 50% and ≥ 50% of EWL) in three studies [18, 20, 30] and three groups (< 50%, 50–75%, and ≥ 75% of EWL) in one study [24]. In one study, although the energy intake of the SWL group was higher than that of the AWL group at 18–47 months post-surgery, the differences did not reach significance [18]. The other study found that women with SWL had higher energy intake at 8 years postoperative than those with AWL (1934 ± 501 vs. 1634 ± 526 kcal/day, p = 0.02), but energy intakes at 1 year postoperative did not differ significantly [20]. There were no significant differences in energy intake between the two groups of patients with SWL and AWL at > 1 year or 2–7 years post-surgery [24, 30]. None of the studies found significant differences in macronutrient contributions to energy intake across the groups of EWL. For the meta-analysis, we pooled the data of the two groups of 50–75% and > 75% EWL in the Novais et al. study [24] to generate a group for individuals with AWL consistent with the other studies. As it has been shown in Fig. 2, a meta-analysis of the 4 studies (96 SWL/227 AWL) indicated a significantly higher energy intake in SWL patients than in AWL patients (MD = 202.5 kcal/day, 95% CI = 77.3, 327.7; I2 = 0%, p heterogeneity = 0.691). The Egger test showed no evidence for small-study effects (p = 0.774). Meta-analyses of the studies revealed no significant differences in macronutrient composition as a percentage of energy between the two groups (Table 3).
Energy Intake and Weight Regain
Ten studies compared daily energy intakes between the WRs and non-WRs [25,26,27,28, 30, 31, 33,34,35, 37]; nine of them found that WRs consumed more energy [25,26,27,28, 30, 33,34,35, 37]. Two studies’ findings were statistically significant [25, 34], six were not [26,27,28, 30, 33, 35], and one did not provide a p value for the comparison [37]. Contrary to the other research, one found that WRs had a non-significant lower energy intake than non-WRs [31]. The forest plot for MD in energy intake between WRs and non-WRs is illustrated in Fig. 3. The meta-analysis of the 10 studies (238 WRs/323 non-WRs) showed a significantly higher intake of energy in WRs (MD = 192 kcal/day, 95%CI = 95.6, 288; I2 = 37.8%, p heterogeneity = 0.106). There was no publication bias by Egger’s test (p = 0.716). Subgroup analysis based on surgery type showed the difference was non-significant for SG, but there was high heterogeneity between the studies (Fig. 3) (I2 = 72.9%, p heterogeneity = 0.011).
Carbohydrate and Weight Regain
Nine studies compared daily carbohydrate intake between WRs and non-WRs [25,26,27,28, 30, 31, 33,34,35]. Four of them look at carbohydrates as a percentage of energy intake [25, 28, 30, 35], two as absolute intake (g/day) [33, 34], and three as both [26, 27, 31]. One of the seven studies examining carbohydrates as a percentage of energy found that WRs had a significantly higher carbohydrate intake than non-WRs (57.1% vs. 48.2%; p value < 0.001) [35], while the other studies showed no significant differences. Furthermore, in one of the five studies comparing carbohydrate consumption in g/day, WRs ingested more carbohydrates than non-WRs (222 ± 84.3 vs. 162 ± 67.5 g/d; p ≤ 0.05) [27]. Meta-analysis of seven studies indicated that the proportion of carbohydrates to energy intake did not significantly differ between WRs and non-WRs. However, the absolute intake of carbohydrates was 24.9 g/day (95%CI = 5.98, 43.8; I2 = 64.4%, p heterogeneity = 0.024) more in WRs vs. non-WRs according to the pooled analysis of five studies. Carbohydrate intake was also significantly greater in WRs undergoing SG, according to a subgroup meta-analysis by surgery type (Table 4).
Fat and Weight Regain
Of the nine studies that compared fat consumption in the two groups of WRs and non-WRs, four looked at fat as a percentage of energy [25, 28, 30, 35], two looked at fat in g/day [33, 34], and three looked at both [26, 27, 31]. The percent of energy from fat was not significantly different between WRs and non-WRs in four studies [25, 27, 28, 30], but in two studies, the percent was significantly lower in WRs [31, 35]. Considering absolute fat intake as g/day, Chou et al. study also found that WRs consumed less fat per day than non-WRs (40 ± 12.8 vs. 55 ± 27 g/day; p = 0.03) [31]. In contrast, studies by Alvarez et al. and Iossa et al. found that WRs consumed more fat [26, 34]. Two studies did not demonstrate any significant difference in the daily intake of fat as g/day [27, 33]. The pooled effect size of seven studies (179 WRs/225 non-WRs) for percent of energy from fat and five studies (81 WRs/120 WRs) for fat as g/day represented no significant differences between the groups. In addition, no significant differences in fat intake were found in the subgroup analysis (Table 4).
Protein and Weight Regain
Daily protein intake in three studies was reported as a percentage of daily energy intake [25, 30, 35], in three studies reported as g/day [28, 34], and in three studies reported as both [26, 27, 31]. The seven studies could not show any significant difference in protein intake between the groups, either as a percent of energy from protein or g/day [25,26,27,28, 30, 33, 34]. Chou et al. found that WRs consume less protein than non-WRs (52.9 ± 17.5 vs. 77.5 ± 35.3 g/d; p = 0.01), but the difference was not significant when considered as percent energy from protein (20.3 ± 3 vs. 23.6 ± 5.3% of energy; p = 0.08) [31]. Moreover, WRs compared to non-WRs had a higher percentage of energy from the protein in the Damin et al. study (median (interquartile range), 15.2 (13.2–18.9) vs. 17.4 (14.5–22.2); p = 0.054) [35]. The pooled effect size of six studies (Table 4) demonstrated that the proportion of protein in daily energy intake was slightly lower in WRs than in non-WRs (MD = − 1.46%, 95% CI = − 2.52, − 0.41; I2 = 9%, p heterogeneity = 0.359), but there was no significant difference in protein intake as g (MD = − 3.59, 95%CI = − 11.2, 4.01; I2 = 35.3%, p heterogeneity = 0.172).
Discussion
Previous studies on the associations between postoperative intakes of energy and macronutrients with weight loss have employed three distinct approaches: considering both dietary intake and weight loss as continuous variables [15,16,17,18,19, 21, 23, 32, 34, 36]; comparing weight loss at different levels of dietary intake as a categorical variable [22, 29]; and comparing food intake at different levels of weight loss as a categorical variable [18, 20, 24, 30]. Studies using the first approach consistently showed that higher energy intake was associated with lower weight loss in both the short and long term after surgery. However, the results of the investigations into the relationship between macronutrients and weight loss were inconclusive. Some studies found no association between macronutrients and weight loss [15, 16, 23, 32], while others found that fat [17, 18, 34] or carbohydrates [19] were inversely associated with weight loss. In addition, one of the two studies on protein intake (g/day) and weight loss reported positive associations between protein intake and %EWL at 6 and 12 months post-RYGB [21], while the other found no significant associations between protein intake at 1 year postoperative and %TWL at mid-term and long term after RYGB [36]. We were unable to do meta-analyses since the studies were so diverse.
Studies employing the second approach demonstrated no significant differences in %EWL between the three groups of participants with varying energy intake 1–5 years after RYGB [22] or in %TWL between those with a protein intake of ≥ 60 g/day and those with a protein intake of < 60 g/day over 12 months after SG [29].
The results of the four investigations comparing the energy intake of patients with SWL and AWL using the third approach were likewise inconsistent [18, 20, 24, 30]. However, none of them could find significant differences in macronutrient intakes between SWL and AWL. According to the meta-analysis done in this study, SWL consumed 203 kcal/day (95% CI = 77, 328) more energy than AWL, although there were no differences in macronutrient consumption between the two groups.
The majority of prior research reported a greater energy intake in WRs than in non-WRs, but the difference was statistically significant only in two studies [25, 34]. Our meta-analysis indicated that WRs consume more energy (MD = 192 kcal/day; 95% CI = 95, 288) and carbohydrates (MD = 25 g/day; 95% CI = 5.98, 43.8) than non-WRs. We also found that the proportion of protein to energy in WRs is slightly lower than in non-WRs (MD = − 1.46, 95% CI = − 2.52, − 0.41).
In some studies, the postoperative time of participants included in a study was widely different [16, 19, 22,23,24,25, 30, 33] which may be a source of bias in their findings because the time since surgery is a predictor of weight loss after surgery [11, 16]. In addition, dietary intake may also change over time after surgery. If there was a temporal variation in both weight outcomes after surgery and energy and macronutrient intakes, future studies on the association of energy and macronutrient intakes with weight outcomes should be conducted in a more homogenous population.
A recent systematic review suggested 11 risk factors from five main categories for weight regain. Increased sweet consumption and portion size as well as eating behaviors were dietary risk factors for weight regain [11]. The systematic review also included 5 studies published until July 2019 on the association between energy and macronutrients and weight regain, but due to the mixed results of the studies, no conclusion was made. The systematic review only included studies with a predefined threshold of ≥ 10% for weight regain. Although the definition of WR has been different across the studies, we decided not to consider any exclusion criteria according to the definition for the following two main reasons. First, the standard definition and threshold for weight regain after BS have not been established yet. Second, findings of a prospective study showed that all the different weight regain measures after RYGB are associated with an increased risk of diabetes progression, declines in physical health-related quality of life, and satisfaction with surgery [38]. Indeed, the results of that study imply that any weight regained after BS may be clinically important and should not be neglected. Therefore, in our systematic review, two more studies published before July 2019 and 3 more studies that were published after the date were included compared to the earlier systematic review. Furthermore, we performed meta-analyses to make a clear conclusion on the association between energy and macronutrient intake after surgery and WR, which has not been done previously. To our knowledge, no systematic review has looked at how energy and macronutrient intakes are related to weight loss after BS.
A strength of the current study is that it covers both SWL and weight regain, the two distinct types of weight loss failure after BS [9]. Therefore, this study provides a comprehensive overview of the association between energy and macronutrient intakes and post-surgery weight outcomes after SG and GB. We also conducted meta-analyses to determine how much energy and macronutrients in individuals with SWL or WR consumed differently compared to individuals with AWL or non-WR.
When interpreting the findings of this study, its limitations should be kept in mind. First, only a few studies were included for the comparison of food intakes between SWL and AWL, and the surgery types were all GB. Second, the number of studies included to study weight regain was limited, and most of them were restricted by sample size and therefore the power to detect an association. Third, weight regain is defined as gaining weight following initial successful weight loss (EWL > 50%) [9]. However, WRs in some studies had a mean %EWL of less than 50% at the time of the study [27, 34]. Therefore, it is unclear if they achieved a satisfactory %EWL following surgery. Fourth, since the dietary assessment tools are self-reported, the possibility of under-reporting, particularly in those regaining weight, is high. An additional limitation was that, due to a paucity of data, we were unable to do subgroup meta-analyses based on the time after surgery and the weight regain definition. In addition, subgroup meta-analyses based on surgery types for weight regain revealed that the general directions of associations for SG and GB were comparable, but the significant findings in MD of energy, carbohydrate (g), and protein (% of energy) did not reach significance in SG for energy and percentage of protein and GB for absolute intake of carbohydrate. The lack of significance in one of the categories may be attributable to the limited number of studies, their small sample sizes, and the variability of the results among the studies.
In conclusion, GB patients with SWL consumed 203 kcal/day more energy than those with AWL, but the proportion of macronutrients to energy intake did not differ significantly between the two groups. In addition, WRs consumed an average of 192 kcal/day more energy and 25 g/day more carbohydrates than non-WRs, but the percentage of protein intake was 1.46% lower. Since there is no strong evidence supporting the association of dietary macronutrient compositions and weight outcomes after BS, it seems that energy intake, independent of macronutrient proportions, is crucial for weight reduction and prevention of weight rebound after GB or SG. Further studies with a larger sample size and a more homogenous population are needed to clarify the role of energy and macronutrients on weight outcomes after BS.
Data Availability
Data that support the findings of this study are available from the corresponding authors upon reasonable request.
References
Arterburn DE, Telem DA, Kushner RF, et al. Benefits and risks of bariatric surgery in adults: a review. JAMA. 2020;324:879–87.
Hua Y, Lou YX, Li C, et al. Clinical outcomes of bariatric surgery - updated evidence. Obes Res Clin Pract. 2022;16(1):1–9. https://doi.org/10.1016/j.orcp.2021.11.004.
O’Brien PE, Hindle A, Brennan L, et al. Long-term outcomes after bariatric surgery: a systematic review and meta-analysis of weight loss at 10 or more years for all bariatric procedures and a single-centre review of 20-year outcomes after adjustable gastric banding. Obes Surg. 2019;29:3–14.
Cadena-Obando D, Ramírez-Rentería C, Ferreira-Hermosillo A, et al. Are there really any predictive factors for a successful weight loss after bariatric surgery? BMC Endocr Disord. 2020;20:20.
Lauti M, Kularatna M, Hill AG, et al. Weight regain following sleeve gastrectomy-a systematic review. Obes Surg. 2016;26:1326–34.
Magro DO, Geloneze B, Delfini R, et al. Long-term weight regain after gastric bypass: a 5-year prospective study. Obes Surg. 2008;18:648–51.
Belligoli A, Bettini S, Segato G, et al. Predicting responses to bariatric and metabolic surgery. Curr Obes Rep. 2020;9:373–9.
Elshaer M, Hamaoui K, Rezai P, et al. Secondary bariatric procedures in a high-volume centre: prevalence, indications and outcomes. Obes Surg. 2019;29:2255–62.
El Ansari W, Elhag W. Weight regain and insufficient weight loss after bariatric surgery: definitions, prevalence, mechanisms, predictors, prevention and management strategies, and knowledge gaps—a scoping review. Obes Surg. 2021;31:1755–66.
Cornejo-Pareja I, Molina-Vega M, Gómez-Pérez AM, et al. Factors related to weight loss maintenance in the medium–long term after bariatric surgery: a review. J Clin Med. 2021;10:1739.
Athanasiadis DI, Martin A, Kapsampelis P, et al. Factors associated with weight regain post-bariatric surgery: a systematic review. Surg Endosc. 2021;35:4069–84.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6: e1000097.
Wells G, Shea B, O’connell D, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2010. Available at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 5 Jan 2023.
Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60.
Bobbioni-Harsch E, Huber O, Morel P, et al. Factors influencing energy intake and body weight loss after gastric bypass. Eur J Clin Nutr. 2002;56:551–6.
Moizé V, Andreu A, Flores L, et al. Long-term dietary intake and nutritional deficiencies following sleeve gastrectomy or Roux-En-Y gastric bypass in a mediterranean population. J Acad Nutr Diet. 2013;113:400–10.
Coughlin K, Bell RM, Bivins BA, et al. Preoperative and postoperative assessment of nutrient intakes in patients who have undergone gastric bypass surgery. Arch Surg. 1983;118:813–6.
Warde-Kamar J, Rogers M, Flancbaum L, et al. Calorie intake and meal patterns up to 4 years after Roux-en-Y gastric bypass surgery. Obes Surg. 2004;14:1070–9.
Faria SL, Faria OP, Lopes TC, et al. Relation between carbohydrate intake and weight loss after bariatric surgery. Obes Surg. 2009;19:708–16.
Kruseman M, Leimgruber A, Zumbach F, et al. Dietary, weight, and psychological changes among patients with obesity, 8 years after gastric bypass. J Am Diet Assoc. 2010;110:527–34.
Raftopoulos I, Bernstein B, O’Hara K, et al. Protein intake compliance of morbidly obese patients undergoing bariatric surgery and its effect on weight loss and biochemical parameters. Surg Obes Relat Dis. 2011;7:733–42.
Forbush S, Nof L, Echternach J, et al. Influence of activity levels and energy intake on percent excess weight loss after Roux-en-Y gastric bypass. Obes Surg. 2011;21:1731–8.
Ortega J, Ortega-Evangelio G, Cassinello N, et al. What are obese patients able to eat after Roux-en-Y gastric bypass? Obes Facts. 2012;5:339–48.
Novais PF, Rasera I Jr, Leite CV, et al. Food intake in women two years or more after bariatric surgery meets adequate intake requirements. Nutr Res. 2012;32:335–41.
Freire RH, Borges MC, Alvarez-Leite JI, et al. Food quality, physical activity, and nutritional follow-up as determinant of weight regain after Roux-en-Y gastric bypass. Nutrition. 2012;28:53–8.
Alvarez V, Carrasco F, Cuevas A, et al. Mechanisms of long-term weight regain in patients undergoing sleeve gastrectomy. Nutrition. 2016;32:303–8.
Reid RER, Oparina E, Plourde H, et al. Energy intake and food habits between weight maintainers and regainers, five years after Roux-en-Y gastric bypass. Can J Diet Pract Res. 2016;77:195–8.
da Silva FB, Gomes DL, de Carvalho KM. Poor diet quality and postoperative time are independent risk factors for weight regain after Roux-en-Y gastric bypass. Nutrition. 2016;32:1250–3.
Sherf Dagan S, Tovim TB, Keidar A, et al. Inadequate protein intake after laparoscopic sleeve gastrectomy surgery is associated with a greater fat free mass loss. Surg Obes Relat Dis. 2017;13:101–9.
Amundsen T, Strommen M, Martins C. Suboptimal weight loss and weight regain after gastric bypass surgery-postoperative status of energy intake, eating behavior, physical activity, and psychometrics. Obes Surg. 2017;27:1316–23.
Chou JJ, Lee WJ, Almalki O, et al. Dietary intake and weight changes 5 years after laparoscopic sleeve gastrectomy. Obes Surg. 2017;27:3240–6.
Schoemacher LAHM, Boerboom AB, Thijsselink MMR, et al. The relationship between energy intake and weight loss in bariatric patients. Obes Surg. 2019;29:3874–81.
Vieira FT, Faria S, Dutra ES, et al. Perception of hunger/satiety and nutrient intake in women who regain weight in the postoperative period after bariatric surgery. Obes Surg. 2019;29:958–63.
Iossa A, Coluzzi I, Giannetta IB, et al. Weight loss and eating pattern 7 years after sleeve gastrectomy: experience of a bariatric center of excellence. Obes Surg. 2020;30:3747–52.
Damin D, Beato G, Crisp A, et al. Weight regain in association with macronutrient diet composition and quality of life in women at least 5 years after bariatric surgery. Rev Chil Nutr. 2021;48:698–706.
Holthuijsen DDB, Romeijn MM, Kolen AM, et al. Can routine clinical tests for protein intake and physical function predict successful weight loss? Bariatr Surg Pract Patient Care. 2022;17:85–91.
Jabbour J, Awada D, Naim N, et al. Impact of bariatric surgery on the healthy eating index, binge eating behavior and food craving in a middle eastern population: a Lebanese experience. Healthcare. 2021;9:1416.
King WC, Hinerman AS, Belle SH, et al. Comparison of the performance of common measures of weight regain after bariatric surgery for association with clinical outcomes. JAMA. 2018;320:1560–9.
Funding
This study was supported by Shahid Beheshti University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent to Participate
Informed consent does not apply.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key Points
• Post-bariatric surgery dietary macronutrient and weight loss studies are limited.
• Patients with suboptimal vs. acceptable weight loss consume 203 kcal/day more energy.
• Weight regainers consumed 192 kcal/day more energy than non-regainers.
• Weight regainers consumed 25 g more carbohydrates per day than non-regainers.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moslehi, N., Kamali, Z., Golzarand, M. et al. Association Between Energy and Macronutrient Intakes and Weight Change After Bariatric Surgery: a Systematic Review and Meta-analysis. OBES SURG 33, 938–949 (2023). https://doi.org/10.1007/s11695-022-06443-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06443-9