Abstract
Background
Surgical treatment has proved to be effective for weight loss, improving the quality of life of obese individuals. However, metabolic and nutritional deficiencies may occur during the late postoperative period. The objective of the present study was to assess the metabolic and nutritional profile of grade III obese individuals for 12 months after Roux-en-Y gastric bypass (RYGBP).
Methods
Forty-eight patients with mean body mass index (BMI) of 51.9 ± 7.8 kg/m2 were submitted to RYGBP. Anthropometric, food intake, and biochemical data were obtained before and for 12 months after surgery.
Results
There was an average weight and body fat reduction of 35% and 46%, respectively. Calorie intake was reduced, ranging from 773 ± 206 to 1035 ± 345 kcal during the study. Protein intake remained below recommended values throughout follow-up, corresponding to 0.5 ± 0.3 g/kg/current body weight/day during the 12th month. Iron and fiber intake was significantly reduced, remaining below recommended levels throughout the study. Serum cholesterol, low-density lipoprotein cholesterol, and glycemia were reduced. Albumin deficiency was present in 15.6% of subjects at the beginning of the study vs 8.9% at the end, calcium deficiency was present in 3.4% vs 16.7%, and iron deficiency was present in 12.2% vs 14.6%.
Conclusions
RYGBP was effective for weight loss and for the reduction of obesity rates and risk factors for comorbidities. The diet of these patients, who frequently present inadequate intake of macronutrients and micronutrients, should receive special attention. Patient follow-up and assessment at short intervals are necessary for an early correction of nutritional deficiencies.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obesity is an increasingly prevalent chronic metabolic disease, which is acquiring epidemic proportions, representing one of the major public health nutritional problems of modern society [1]. Grade III obesity is related to a high incidence of degenerative diseases and to a high mortality rate. The disorders range from respiratory difficulties, dermatological problems, and disturbances of the locomotor apparatus to the induction of diseases such as dyslipidemia, cardiovascular diseases, diabetes mellitus, and certain types of cancer [2, 3].
The rapid increase in the prevalence of obesity and the failure of dietary and/or pharmacological treatments, especially on a long-term basis, among grade III obese patients (body mass index [BMI] ≥40 kg/m2), has led to an increasing demand for bariatric surgery. From 1990 to 2003, the number of procedures performed in the US increased from 16,000 to more than 100,000 per year [4]. Bariatric surgery is currently considered to be the most effective tool for the treatment and control of grade III obesity [5, 6].
Several surgical techniques have been proposed and tested since the 1950s using different physiological principles [7]. Capella Roux-en-Y gastric bypass (RYGBP), which combines restriction by means of a reduction of the gastric reservoir to 20 mL and secondary dysabsorption with bypass of the duodenum and proximal jejunum, is the technique most frequently used today [8].
Surgical treatment has proved to be effective for weight loss with a consequent improvement of the quality of life for persons with grade III obesity. In addition, the weight loss is associated with an improvement of morbidity, including respiratory disorders, systemic arterial hypertension, type 2 diabetes, hypercholesterolemia, and hypertriglyceridemia, among others [9]. However, metabolic and nutritional deficiencies consequent to inadequate food intake and dysabsorption may occur during the late postoperative period, although data about the repercussions of surgery on the nutritional status of these patients are scarce.
Thus, the objective of the present study was to assess the metabolic and nutritional profile of grade III obese patients for a period of 12 months after bariatric surgery.
Patients and Methods
The study was conducted on 48 patients, 41 women (85%) and seven men (15%) aged on average 41.9 ± 8.8 years. The mean preoperative weight was 139.7 ± 23.9 kg, mean height was 1.64 ± 7.3 m, and mean BMI was 51.9 ± 7.8 kg/m2. The patients had associated comorbidities and had been submitted to bariatric surgery 12 months before the present investigation. The technique used for all patients was RYGBP.
The patients were monitored by the multiprofessional team of the Service of Nutrology, Department of Internal Medicine and by the team of the Center of Bariatric Surgery, Division of Gastroenterology, Department of Surgery and Anatomy, Faculty of Medicine of Ribeirão Preto (HCFMRP-USP).
Nutritional Regimen
All patients were interviewed, attended, and counseled by a nutritionist before and after surgery. During the postoperative period, the patients were instructed to ingest a liquid diet for 1 month and then to switch to a diet of pureed/soft foods and progress to regular solid foods according to individual tolerance. After this period of adaptation, patients were advised to ingest a regular healthier diet. The patients were advised to follow a prescribed diet according to the postoperative feeding protocol. Food should be well-chewed and consumed very slowly, fluid should not be consumed for at least 30 min before and no sooner than 30 min after a meal. Food and beverages containing protein should be eaten before those containing only carbohydrate. Additionally, high-calorie foods (i.e., foods high in fat or sugar) should be avoided to promote optimal weight loss. The patients were instructed to begin vitamin and mineral supplementation during the first postoperative month. Compliance was checked during regular visits.
Nutritional Evaluation
The patients were evaluated anthropometrically and in terms of food ingestion before and 1, 3, 6, 8, and 12 months after surgery. Blood was collected for the determination of glycemia, triglycerides, total cholesterol, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) before and 3, 6, and 12 months after surgery.
Anthropometric evaluation consisted of measurement of weight and height and calculation of BMI by the formula: BMI = W/H 2 where W is the weight in kilograms and H is the height in meters. The patients were weighed on a Filizola® digital scale of the platform type with capacity of 300 kg and precision of 0.2 kg. Height was measured with a vertical rod with 0.5 cm graduation. Body composition was characterized by bioimpedanciometry using a Quantum BIA 101Q-RJL Systems® instrument.
Dietary intake was evaluated by the application of the 24-h food recall and calculated using the NUTWIN-UNIFESP® Nutrition Support software [10].
Biochemical evaluation consisted of blood determinations of glucose, total cholesterol, triglycerides, HDL-C, LDL-C, albumin, calcium, sodium, potassium, and iron.
Statistical Analysis
Data were analyzed statistically by the Friedman test. For the comparison between periods, the Dunn test for multiple comparisons was used. The level of significance was set at P ≤ 0.05 in all analyses. Data are reported as the mean±standard deviation.
Results
Anthropometry and Body Composition
Anthropometric and body composition data are presented in Table 1. Periodic evaluation showed that there was a gradual reduction of body weight and BMI with significant differences starting during the third postoperative month. By the 12th month, there was a 35% reduction of body weight and BMI compared to the preoperative values. A significant reduction of body fat occurred from the third month onward with a 46% reduction by the 12th month. No difference in lean mass was observed during the study.
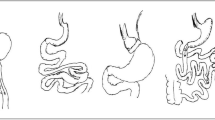
As illustrated in Fig. 1, an expressive improvement in obesity rates occurred at the end of the follow-up period, when 6.2% of the patients were eutrophic, 25% were overweight, 33.5% had grade I obesity, 25% had grade II obesity, and only 10.3% had grade III obesity.
Assessment of Food Intake
The food intake observed before admission and 12 months after surgery is presented in Table 2. On the basis of the nutrients evaluated, there was a significant reduction of calories, carbohydrate, protein, lipid, and cholesterol along the postoperative follow-up period compared to previous values. The percentage of macronutrients continued to be adequate at all time points assessed, although with a significant reduction of the amount ingested (in grams) starting on the first month after surgery. There was a significant reduction of iron and fiber intake starting on the first month with intake remaining below recommended levels throughout the study.
Biochemical Evaluation
Table 3 shows the biochemical evolution of glycemia, triglycerides, total cholesterol, LDL-C, and HDL-C. There was a significant reduction in serum cholesterol levels starting on the third month, of fasting glycemia starting on the sixth month, and an increase in HDL-C at the end of follow-up. The number of patients with elevated total cholesterol was reduced from 35% during the preoperative period to 25% at 12 months after surgery. The reduction of blood triglycerides was significant with the number of patients with hypertriglyceridemia being reduced from 40% during the preoperative period to 5% (one patient) at the end of follow-up. No difference in LDL-C levels was observed during the study, but the number patients with elevated levels was reduced from 88.9% at the beginning of the study to 33.4% at the end of the study period.
There was no difference in mean plasma albumin or potassium levels during the study. A reduction of sodium and serum iron levels were observed beginning on the third month after surgery, but the values remained within normal limits returning to initial values 12 months after surgery (Table 4).
Albumin deficiency was present in 15.6% of subjects at the beginning of the study vs 8.9% at the end, calcium deficiency was present in 3.4% vs 16.7%, and iron deficiency was present in 12.2% vs 14.6% (Table 5).
Discussion
In the present study, obese patients submitted to RYGBP and monitored by a multiprofessional team presented a significant weight reduction (35%) during the first postoperative year. This reduction was gradual, being more intense between the sixth and eighth month (8.1%), in agreement with a previous study [11]. The weight reduction was due to the loss of body fat, which decreased significantly starting on the first month with no change in lean mass along follow-up, again confirming the results of previous studies [12, 13].
Despite a significant weight reduction, most patients were still obese at the end of the 12 months. However, it should be pointed out that the percentage of patients with a BMI ≥ 50 kg/m2 was 58% at the beginning of the study, being reduced to 2% at the end of the study. The mean BMI of the present patients was 51.9 ± 7.8 and 33.6 ± 5.9 kg/m2 at the beginning and at the end of the study, respectively, showing an important reduction, in agreement with data reported by Von Mach et al. [14]. According to the standard procedure of our institution, the patients were instructed to ingest a liquid diet for 1 month, followed by a diet of pasty consistency and progressing to a diet of general consistency according to individual tolerance. After this period of adaptation, the patients were instructed to ingest a balanced diet.
With their gastric capacity reduced to about 20 mL, the patients started to ingest a low-calorie diet corresponding to approximately 6.4 kcal/kg/current body weight/day during the first month after surgery and ranging from 773 ± 206 to 1,035 ± 345 kcal during the 12-month period. The diet continued to be hypocaloric throughout the study but, after the third month, with the modification of consistency, the proportions of macronutrients of a balanced diet were recommended. This pattern of caloric intake is similar to that reported by others [15, 16]. It is important to emphasize that, during the first year after bariatric surgery, this low-calorie food intake can promote severe nutritional deficiencies if not monitored.
The low protein intake along the 12 months should be emphasized. Protein intake ranged from 30.9 ± 12.3 g/day during the first month to 46.6 ± 20.0 g/day during the 12th month, corresponding to a mean intake of 0.5 ± 0.3 g/kg/current body weight/day, which is below recommended values. Moize et al. [15] observed a mean protein intake of 58 g/day 1 year after surgery. In agreement with our findings, previous studies have shown that, in most cases, the monitoring of protein intake should be intensified in order to reach a minimum of 60 g/day, the value established in various studies of patient follow-up after bariatric surgery [17]. One of the factors interfering with protein intake is intolerance of red meat ingestion, which may occur due to the lack of proper mastication and to reduced gastric secretion. It is a fact that patients consume more meat before than after surgery, but no study has reported details about this phenomenon of intolerance [15, 18, 19].
A choice of more nutritive foods should always be recommended since the amounts ingested daily are very small. During this phase, the patient should be able to select foods that will bring more comfort, satisfaction, and nutritional quality.
Dietary assessment before surgery demonstrated a low intake of fibers (vegetables, fruit, and legumes) and iron, which continued to be significantly low throughout the study. Few data are available in the literature regarding the intake of fibers, iron, and other micronutrients. Dias et al. [20], in a study of the diet of obese women after surgery, detected a low iron intake with a mean of 5.6 mg 12 months after surgery, a result confirmed by the present study. Other studies have pointed out that vitamin and mineral deficiency is greater and more significant in obese patients before surgery than previously thought [21, 22]. Morbidly obese patients are not well-nourished and may have clinical or subclinical nutritional deficiencies before bariatric surgery [23].
Capella surgery reduces food intake in terms of volume; therefore, patient collaboration is indispensable regarding compliance with medical and nutritional guidelines for adaptation to the new lifestyle. The need to select and chew well the foods implies the intake of the necessary foods and the availability of more time for each meal. The lack of proper mastication, observed in many patients, generates difficulties in the passage of certain foods such as meat or fiber through the containment band, often leading to a reduced intake of these nutrients and to a preference for carbohydrates and fluids.
Recent evidence has suggested a reduction of the risk of mortality after bariatric surgery. The consistent intentional weight loss results in a reduced risk for cancer, cardiovascular disease, and hormonal disorders [7, 24, 25]. Studies have shown normalization of blood glucose in 83% of patients [11] with a fivefold reduced incidence of diabetes after 8 years of patient follow-up [26]. In the present study, the reduction of fasting glucose levels was significant starting on the sixth month with only 4% of the patients continuing to have elevated glycemia at the end of follow-up.
A series of studies have demonstrated a significant improvement of lipid profile, including significantly decreased LDL levels, increased HDL levels, and reduced triglyceride levels [26, 27]. An improved lipid profile was observed in the present patients with a reduction of triglyceride, total cholesterol, and LDL levels and an increase of HDL.
Clinical or subclinical nutritional deficiencies may be present in some obese patients before surgery. These deficiencies may involve vitamins or minerals as the consequence of a hypercaloric diet which is simultaneously deficient in essential nutrients, possibly becoming more severe after surgery if no rapid replacement is provided [21, 22]. The deficient iron intake demonstrated in the present study explains the frequent treatment of anemia during the postoperative period [19]. In this study, mean serum iron levels remained within normal limits but the patients were regularly followed up, receiving iron supplementation whenever necessary.
Conclusion
Reducing surgery with RYGBP was effective in inducing weight loss and in reducing obesity rates and risk factors for comorbidities. However, special attention should be paid to the diet of these patients who frequently present macronutrient and micronutrient intake below recommended levels. Thus, the patients should be followed up and assessed at short time intervals for an early detection and correction of possible nutritional deficiencies.
References
World Health Organization. Preventing and managing the global epidemic of obesity. Report of the World Health Organization Consultation of Obesity. Geneva: World Health Organization; 1998.
Rashid MN, Fuentes F, Touchon RC, et al. Obesity and risk for cardiovascular diseases. Prev Cardiol 2003;6:42–7.
Buchwald H. Overview of bariatric surgery. J Am Coll Surg 2002;194:367–75.
Steinbrook R. Surgery for severe obesity. N Engl J Med 2004;350:1075–9.
Ferraro DR. Management of the bariatric surgery lifelong postoperative care. Clin Rev 2004;14:73–9.
Maggard MA, Sugarman LR, Suttorp M, et al. Meta-analysis: surgical treatment of obesity. Ann Intern Med 2005;142:547–59.
Bult MJ, Van Dalen T, Muller AF. Surgical treatment of obesity. Eur J Endocrinol 2008;158:135–45.
Fobi MAL, Lee H, Fleming AW. The surgical technique of the banded Roux-en-Y gastric bypass. J Obes Weight Regul 1989;8:99–102.
Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004;292:1724–37.
Anção MS, Cuppari L, Draibe AS, et al. Programa de Apoio à Nutrição-NutWin. Versão 1.5. São Paulo: Departamento de Informática em Saúde-SPDM-Unifesp/EPN, 2002. CD-ROM.
Pories WJ, Swanson MS, MacDonald KG, et al. Who would have thought it? An operation proves to be the most effective therapy for adult-onset diabetes mellitus. Ann Surg 1995;222:339–52.
Das SK, Roberts SB, Kehayas JJ, et al. Body composition assessment in extreme obesity and after massive weight loss induced by gastric bypass surgery. Am J Physiol Endocrinol Metab 2003;284:E1080–8.
Giusti V, Suter M, Heraief E, et al. Effects of laparoscopic gastric banding on body composition, metabolic profile and nutritional status of obese women: 12-months follow-up. Obes Surg 2004;14:239–45.
Von Mach MA, Stoeckli R, Bilz S, et al. Changes in bone mineral content after surgical treatment of morbid obesity. Metabolism 2004;53:918–21.
Moize V, Geliebter A, Gluck ME, et al. Obese patients have inadequate protein intake related to protein intolerance up to 1 year following Roux-en-Y gastric bypass. Obes Surg 2003;13:23–8.
Brolin RE, Leung M. Surgery of vitamin and mineral supplementation after gastric bypass and biliopancreatic diversion for mordid obesity. Obes Surg 1999;9:150–4.
MacLean LD, Rhode BM, Forse RA. Late results of vertical banded gastroplastry for morbid super obesity. Surgery 1990;107:20–7.
Avinoach E, Ovnat A, Charuzi I. Nutritional status 7 years after Roux-en-Y gastric bypass surgery. Surgery 1992;111:137–42.
Love AL, Billett HH. Obesity, bariatric surgery, and iron deficiency: true, true, true and related. Am J Hematol 2008;83:403–9.
Dias MCG, Ribeiro AG, Scabim VM, et al. Dietary intake of female bariatric patients after anti-obesity gastroplasty. Clinics 2006;61:93–8.
Kaidar-Person O, Person B, Szomstein S, et al. Nutritional deficiencies in morbidly obese patients: a new form of malnutrition? Part A: vitamins. Obes Surg 2008;18:870–6.
Kaidar-Person O, Person B, Szomstein S, et al. Nutritional deficiencies in morbidly obese patients: a new form of malnutrition? Part B: minerals. Obes Surg 2008;18:1028–34.
Tucker ON, Szomstein S, Rosenthal RJ. Nutritional consequences of weight-loss surgery. Med Clin N Am 2007;91:499–514.
Cristou NV, Sampalis JS, Liberman M, et al. Surgery decreases long-term mortality, morbidy, and health care use in morbidly obese patients. Ann Surg 2004;240:416–24.
Torgerson JS, Sjostrom L. The Swedish Obese Subjects (SOS) study rationale and results. Int J Obes Relat Metab Disord 2001;25:S2–4.
Sjomstrom CD, Peltonen M, Wedel H, et al. Differentiated long-term effects of intentional weight loss on diabetes and hypertension. Hypertension 2000;36:20–5.
Busetto L, Pisent C, Rinaldi D, et al. Variation in lipid levels in morbidly obese patient operated with LAP-BAND adjustable gastric banding system: effects of different levels of weight loss. Obes Surg 2000;10:569–77.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bavaresco, M., Paganini, S., Lima, T.P. et al. Nutritional Course of Patients Submitted to Bariatric Surgery. OBES SURG 20, 716–721 (2010). https://doi.org/10.1007/s11695-008-9721-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-008-9721-6