Abstract
Introduction
Laparoscopic sleeve gastrectomy (LSG) can achieve excellent weight loss, yet sleeve dilatation with concomitant weight regain proves to be a relevant issue. Hence, additional restriction might improve results after LSG.
Methods
In a retrospective matched-pair analysis, 42 patients who underwent banded LSG (BLSG) using a MiniMizer® ring between January 2012 and October 2014 were analysed regarding weight loss, complications and comorbidity. Median follow-up was 3 years. Forty-two patients who had undergone conventional LSG were selected as matched pairs.
Results
Mean preoperative BMI was 54.93 ± 7.42 kg/m2 for BLSG and 53.46 ± 6.69 kg/m2 for LSG (Mann-Whitney P = 0.540). Total weight loss (%TWL) was significantly greater in the BLSG group 3 years after surgery (BLSG 38.22% ± 7.26; n = 26 vs. LSG 32.69 ± 9.47; n = 26; P = 0.0154). Ring placement had no relevant impact on new-onset reflux (Fisher’s exact test P = 1.0) but a tendency towards reflux improvement when reflux pre-existed (odds ratio 1.96). The major side effect of ring implantation was regurgitation with over 44% of patients presenting with regurgitation >1 per week (Fisher’s exact test P = 0.0019, odds ratio 18.07).
Conclusion
BLSG is a safe procedure showing similar comorbidity to conventional LSG. However, BLSG leads to a higher rate of postoperative regurgitation. Weight loss is significantly improved 3 years after surgery. Hence, additional ring implantation might be an option for increased restriction in LSG surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to its seemingly easy operative technique, low perioperative morbidity and feasibility even in the super super obese, the number of laparoscopic sleeve gastrectomy (LSG) performed worldwide is growing at an unprecedented rate [1]. LSG leads to good short and mid-term weight loss in many studies and is comparable to conventional Roux-en Y gastric bypass (RYGB) [2, 3]. In other words, LSG has become a widely accepted stand-alone bariatric procedure today. However, there is substantial evidence that many patients experience considerable weight regain beginning already 2 years after surgery [4]. Although long-term data on sleeve gastrectomy are limited, the procedure can be considered successful (defined as >50% EWL) in only 55% of patients 8–9 years after sleeve gastrectomy [5]. About one third of patients require redo surgery due to insufficient weight loss [6]. Being a primarily restrictive procedure, sleeve dilatation due to consistent, incremental increase of consumed meals is most likely the primary mechanism behind this phenomenon [7]. Hence, adding an element of non-compliant restriction might improve weight loss after LSG in the mid- and long term.
Aiming to both increase restriction and to maintain weight loss, many surgeons place a ring around the gastric pouch in gastric bypass surgery, essentially performing a banded gastric bypass (BRYGB) [8–10]. The ring proves to be highly effective in this type of bariatric surgery [10, 11]. With the same goal, our group began placing a non-adjustable gastric ring around the upper part of the sleeve in patients undergoing LSG. This operation was performed primarily in 2007 [12]. The study demonstrated that banded sleeve gastrectomy (BLSG) using a MiniMizer® ring is a safe procedure, yet weight loss was not influenced by the ring in the first 12 postoperative months [13]. However, experience with this method is sparse, and there is a paucity of follow-up data. We therefore performed a retrospective matched-pair analysis comparing patients after banded and conventional sleeve gastrectomy with the aim of presenting midterm results on weight loss and comorbidity with this new technique.
Material and Methods
A retrospective matched-pair analysis was performed with 42 patients who had received BLSG and 42 patients with conventional LSG. Patients were operated between November 2010 and October 2014 at the author’s institution. Patient follow-up included visits at the institution’s outpatient clinic after 1, 6 and 12 months in the first year after surgery and yearly visits thereafter. Data recording included body measurements, presence of medical comorbidities such as arterial hypertension and type 2 diabetes (T2DM), surgical complications, clinical assessment of reflux, vomiting and dysphagia as well as length of operation and total length of hospital stay (day of admission to day of discharge). Dysphagia was graded as suggested previously (grade 0: able to swallow all solid foods without difficulty; grade 1: able to swallow solid foods with some difficulty; grade 2: able to swallow soft or semi-solid foods only; grade 3: able to swallow liquefied foods and liquids only; grade 4: unable to swallow liquids/saliva) [14]. Overall outcome was assessed using the “Bariatric Analysis and Reporting Outcome System” (BAROS) [15]. All data were entered into a custom-designed database. Missing data were obtained via a telephone questionnaire. Written informed consent was obtained from all patients. For matched-pair analysis, patients were matched for age, gender, preoperative BMI and presence of T2DM.
All procedures performed were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study. The institutional ethics committee approved retrospective data evaluation of all patients (Ref. number: 321/13).
Operative Technique
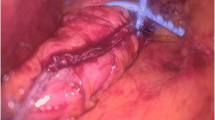
Laparoscopic banded and conventional sleeve gastrectomy was performed as published earlier [13]. Apart from the ring implantation, operative technique was identical in both groups. In brief, the operation is performed in a two-surgeon technique using five trocars with the patient in the lithotomic position and the operating table in a 30° reverse Trendelenburg tilt.
The dissection begins on the greater curvature 4–5 cm from the pylorus entering the bursa omentalis. The dissection is continued in a cephalic direction using a marSeal vessel-sealing device (KLS Martin GmbH, Freiburg, Germany) until the left crus of the diaphragm is visualized. Resection begins 4–5 cm from the pylorus along a 35-F calibration tube, using violet linear tri-staplers (GIA Roticulators, Covidien, Dublin, Ireland) up to the angle of His. A gastric sleeve less than 100 ml in volume remains.
For MiniMizer® ring implantation, a small insertion is made in the peritoneum of the lesser curvature 4–6 cm from the gastro-esophageal junction. The MiniMizer® ring is then pushed through the insertion between gastric wall and omentum minus and closed to leave a circumference of 6.5 cm. The introducer of the MiniMizer® ring is then removed, and the ring is fixed in position using a single Vicryl 3/0 suture. Starting in January 2014, the ring was closed at a circumference of 7.5 cm (n = 5).
Statistics
Statistical analysis was conducted using Prism 5 for Mac OS X (GraphPad Software, Inc.). The Mann-Whitney U test was used for group comparison; curves were analysed with two-way ANOVA. All patients were included in the statistical analyses. P < 0.05 was considered significant.
Results
Forty-two patients with a mean preoperative BMI of 54.93 ± 7.42 kg/m2 underwent BLSG. The mean preoperative BMI of patients in the matched-pair group with conventional LSG was 53.46 ± 6.69 kg/m2 (Table 1). The median follow-up was 3 years. Duration of surgery was 63.05 ± 29.96 min in the BLSG group (Table 2). Additional ring implantation did not prolong the duration of surgery with a mean operative time of 63.55 ± 24.3 min in the LSG group (Mann-Whitney P = 0.9; Table 1). Overall length of hospital stay was equal in both groups (BLSG 7.8 days vs. LSG 7.5 days, Mann-Whitney P = 0.188). Thirteen patients with BLSG and 12 patients in the LSG group had undergone previous abdominal surgery, but none in the upper gastrointestinal tract. A gastric balloon had been implanted as primary weight loss therapy in two patients from each group.
Weight Loss and Overall Outcome
Total weight loss was equal in both groups 1 and 2 years after surgery (BLSG vs. LSG 35.98% ± 9.05; n = 38 vs. 31.85 ± 10.26; n = 25; P = 0.1578 and 37.85% ± 7.76; n = 28 vs. 34.78 ± 11.25; n = 21; P = 0.2069 after 1 and 2 years, resp.). Overall, the BLSG group presented with a significantly improved weight loss over time (two-way ANOVA P = 0.0023, Fig. 1) resulting in a significantly greater %TWL 3 years after surgery (BLSG 38.22% ± 7.26; n = 26 vs. LSG 32.69 ± 9.47; n = 26; P = 0.0154). This was mainly due to a weight regain in the LSG group. Starting from an initial mean body weight of 157.8 kg, BLSG patients lost 10.61 kg more than patients with LSG.
As a standardized outcome measure after bariatric surgery, the BAROS score was significantly better in the BLSG 3 years after surgery (BLSG 7.08 ± 2.04; n = 26 vs. LSG 5.22 ± 2.06; n = 27; P < 0.0001, Fig. 2).
Morbidity, Mortality and Complications
Surgical complications were equal in both groups with one revision due to staple line bleeding in each group and one intraabdominal abscess in the LSG group (Fisher’s exact test P = 1.0). All revisions were conducted laparoscopically. There was no mortality in either group (Table 2).
Approximately, one half of all patients in both groups presented with pre-existing reflux (Table 3). Again, half of the patients with no preoperative reflux symptoms developed postoperative reflux (BLSG 45%, LSG 50%; Fisher’s exact test P = 1.0). When reflux was present at the time of sleeve gastrectomy, the majority of patients showed symptom improvement after surgery. Additional ring implantation slightly promoted reflux improvement (Table 3). Accordingly, postoperative PPI use increased significantly more in the LSG group (linear reg. P < 0.0001). However, patients with frequent regurgitation in the BLSG group likely also suffered from reflux (odds ratio 7.20, P = 0.081).
The majority of patients in both groups did not experience dysphagia 3 years postoperative (BLSG 72%, LSG 85%). Mild dysphagia (grades 1 and 2) was present in 28% of BLSG and 15% of LSG patients. Relative risk for dysphagia was 1.4 when a ring was placed (Fisher’s exact test P = 0.324). Relevant regurgitation, defined as regurgitation >1/week, was present in 44% of patients after BLSG, whereas only 4% of patients presented with similar symptoms after LSG. Ring implantation clearly had a significant impact on regurgitation 3 years after surgery (Fisher’s exact test P = 0.002).
In three patients, regurgitation was so severe that the ring had to be removed. Two patients underwent oral contrast studies before ring removal, showing an only mildly dilated pouch in one case and a huge pouch above the ring in the other case. Ring removal took place at a mean postoperative time of 14 months (range 13–16 months). The patient with a mildly dilated pouch underwent planned revision to a duodeno-ileostomy with sleeve gastrectomy (DIOS) operation 2 months after band removal. The patient with a grossly dilated pouch underwent conversion to RYGB with a latency of 23 months. The third patient had no further bariatric surgery. Apart from the patient with a planned revision after band removal, mean %EWL decreased considerably from 69.22% ± 12.52 at the time of ring explantation to 38.86% ± 7.86 in a mean time of 21.5 months (20 and 23).
Discussion
Banded laparoscopic sleeve gastrectomy is a novel procedure. Surgical experience is limited, and there is need for outcome reports. The authors’ group could show earlier that BLSG is a safe procedure yet has limited effect on weight loss in short-term follow-up [13].
In the current matched-pair analysis, surgical complications and length of hospital stay were within the range reported by others [16]. Analysing more than 10,000 sleeves from the German registry, Stroh et al. found a mean postoperative stay of 6.7 days after LSG in Germany [16]. This long hospital stay certainly also is a national preference.
Mean EWL after conventional LSG was as expected and comparable to others [16, 17]. Beginning 1 year after surgery, patients of the BLSG group showed gradually better weight loss than LSG patients. Three years after surgery, follow-up shows that BLSG patients largely maintain stable body weight, while LSG patients regained weight. This resulted in a significant discrepancy between the two groups at this time. Such a delayed difference in weight loss between banded and non-banded procedures is a phenomenon also seen after BRYGB [10]. The reason behind this observation is the fact that when the ring is closed at 6.5 cm, as in the majority of the current and Awad’s series, or at 7.5 cm, its diameter of 2.0 or 2.4 cm is still considerably larger than the diameter of a routine 35-Fr bougie (1.2-cm diameter). Therefore, sleeve (pouch) dilatation has to occur before the ring can exert its additional restriction. In turn, sleeve dilatation is linked to weight regain and most likely responsible for the weight regain seen after conventional LSG in the current series and following BRYGB 3 years after surgery [7, 18]. Consistently, Sarela et al. demonstrated weight regain after LSG with a concordant drop of EWL from 78% at 2 years to 60% at 8 or 9 years in their series. Overall, the bariatric procedure failed in almost half of the cohort with 45% of patients experiencing a weight loss less than 50% [5]. In contrast, weight stability in the BLSG group nicely demonstrates the effectiveness of the anticipated additional restriction in the current series.
Reflux remains an important issue before and after sleeve gastrectomy, yet the sleeve’s impact on reflux is not fully understood to date [19–21]. On the one hand, heavy reflux is considered to be a contraindication for LSG by some authors [22]. Furthermore, persistence and worsening of pre-existing reflux have been described as a relevant problem after LSG [19, 23]. On the other hand, there is substantial evidence that reflux symptoms may even be improved after sleeve gastrectomy as obesity is one main risk factor for this disease [20, 24]. Recently, LSG was even demonstrated to be highly protective of extra-oesophageal reflux disease in an animal model [25]. In our cohort, we saw an ambiguous development of reflux symptoms after LSG. There was a very large proportion with pre-existing reflux. In this sub-group, conventional LSG led to symptom improvement in over 70% of patients. In patients without preoperative reflux symptoms, conventional LSG led to new-onset reflux in about half of the cases. Overall, conventional LSG considerably increased PPI use, indicating a negative effect on reflux symptoms.
Our group earlier observed a higher rate of reflux improvement and a lower rate of new-onset reflux in after BLSG [13]. The current analysis supports these data in that BLSG patients were more likely to show symptom improvement than patients after LSG, when reflux pre-existed. Furthermore, the increase in PPI use postoperatively was significantly lower in the BLSG group. However, particularly, patients with frequent regurgitation in the BLSG group were likely to suffer from postoperative reflux. In other words, regurgitation could almost discriminate between patients with and without postoperative reflux. Proximal fundus dilatation is known to be a possible cause for heavy reflux after LSG and could explain the coexistence of regurgitation and reflux [26]. Potentially, ring placement aggravates reflux in this subgroup, as a fixed sleeve diameter 4–6 cm below the GE junction might promote proximal sleeve dilatation by acting as a functional stenosis. All in all, the ring probably has a minor impact on reflux symptoms as the main reason for reflux after LSG most likely is the creation of a vertical pouch impairing the angle of His combined with high intra-gastric pressure [27].
Regurgitation proved to be a relevant issue after BLSG. In a previous series including 25 patients after BLSG, the authors’ group reported a ring removal rate of 8% 13 months after surgery [13]. At that time, we speculated that both careful patient selection and creation of a short pouch when placing the ring were crucial to avoid ring-related regurgitation. Being a continuous process, utmost attention has since been paid to careful patient selection and to forming a short (4–6 cm) pouch. Now with a considerably longer follow-up period and more patients, only one additional ring had to be explanted, leaving the ring removal rate at 7.1% in the current series. Importantly, ring removal rate does not increase in a longer follow-up period. Stubbs et al. found the ring circumference to be the most relevant factor for ring removal rate after BRYGB, and an initial high removal rate essentially prompted them to increase the ring circumference from 5.5 to 6.5 cm [28]. Overall, 5% of rings had to be removed in that series [28]. A ring circumference of 6.5 cm was already used for the majority of patients in the current series. A recently published manuscript comparing ring circumferences of 6.2 and 7.5 cm in BRYGB patients demonstrated that the chance of chronic regurgitation was 4.5 times greater for the smaller ring size [29]. Hence, a further increase in ring circumference to 7.5 cm, as done in the last five patients of the current series, could possibly improve regurgitation after BLSG. However, number and follow-up are too short for statistical evaluation. Altogether, the increased rate of postoperative regurgitation had no impact on the overall outcome in the BLSG group. Indeed, the BAROS score was significantly better in this group 3 years after surgery.
When initially removing the three rings, it was uncertain whether removal would be uncomplicated or if patients would consecutively regain weight. Therefore, all three revisions were conducted as sole procedures. Even though experience is limited, based on the data presented, weight regain should be anticipated after ring removal, as a major restrictive component is taken away from the patient. Furthermore, the pouch above the ring has already dilated to some extent by the time the ring is removed. Surgical options for a revisionary bariatric procedure essentially do not differ from a conventional sleeve with insufficient weight loss [30]. If the proximal sleeve is dilated, conversion to an RYGB with pouch reshaping might be a suitable option, as this also tackles the often-present reflux in patients with dilated proximal sleeves [31, 32]. Possibly, a re-sleeve could be an option [32]. When the sleeve shape is largely intact and the main focus lies on weight loss, conversion to a BPD could be performed [33]. As the MiniMizer® ring causes very little scar formation and band removal can be considered simple, removal and bariatric revisions could be offered as a sole procedure.
The current analysis confirms the safety of the BLSG procedure. Surgical complication rate was low and equal to conventional LSG. There is increasing evidence that ring implantation might be favourable for reflux symptoms, a relevant comorbidity after LSG. However, improved weight loss comes at the cost of a higher rate of vomiting. To the best of our knowledge, the current analysis is the first to report improved weight loss in BLSG patients 3 years after surgery. Hence, BLSG might be an optional add-on treatment in patients who require extra restriction.
References
Angrisani L et al. Bariatric surgery worldwide 2013. Obes Surg. 2015;25(10):1822–32.
Colquitt JL et al. Surgery for weight loss in adults. Cochrane Database Syst Rev. 2014;8:CD003641.
Peterli R et al. Early results of the Swiss multicentre bypass or sleeve study (SM-BOSS): a prospective randomized trial comparing laparoscopic sleeve gastrectomy and roux-en-Y gastric bypass. Ann Surg. 2013;258(5):690–4. discussion 695
Liu SY et al. Long-term results on weight loss and diabetes remission after laparoscopic sleeve gastrectomy for a morbidly obese Chinese population. Obes Surg. 2015;25(10):1901–8.
Sarela AI et al. Long-term follow-up after laparoscopic sleeve gastrectomy: 8-9-year results. Surg Obes Relat Dis. 2012;8(6):679–84.
Felsenreich DM, et al. Weight loss, weight regain, and conversions to Roux-en-Y gastric bypass: 10-year results of laparoscopic sleeve gastrectomy. Surg Obes Relat Dis. 2016.
Alvarez V et al. Mechanisms of long-term weight regain in patients undergoing sleeve gastrectomy. Nutrition. 2016;32(3):303–8.
Lemmens L et al. Banded gastric bypass—four years follow up in a prospective multicenter analysis. BMC Surg. 2014;14:88.
Fobi MA. Placement of the GaBP ring system in the banded gastric bypass operation. Obes Surg. 2005;15(8):1196–201.
Awad W, Garay A, Martinez C. Ten years experience of banded gastric bypass: does it make a difference? Obes Surg. 2012;22(2):271–8.
Bhandari M et al. Comparison between banded and nonbanded Roux-en-Y gastric bypass with 2-year follow-up: a preliminary retrospective analysis. Obes Surg. 2016;26(1):213–8.
Karcz WK et al. Banded sleeve gastrectomy using the GaBP ring—surgical technique. Obes Facts. 2011;4(1):77–80.
Karcz WK et al. To band or not to band--early results of banded sleeve gastrectomy. Obes Surg. 2014;24(4):660–5.
Coia LR, Myerson RJ, Tepper JE. Late effects of radiation therapy on the gastrointestinal tract. Int J Radiat Oncol Biol Phys. 1995;31(5):1213–36.
Oria HE, Moorehead MK. Bariatric analysis and reporting outcome system (BAROS). Obes Surg. 1998;8(5):487–99.
Stroh C et al. Results of more than 11,800 sleeve gastrectomies: data analysis of the German bariatric surgery registry. Ann Surg. 2016;263(5):949–55.
Chopra A et al. Laparoscopic sleeve gastrectomy for obesity: can it be considered a definitive procedure? Surg Endosc. 2012;26(3):831–7.
Baumann T et al. Three-dimensional stomach analysis with computed tomography after laparoscopic sleeve gastrectomy: sleeve dilation and thoracic migration. Surg Endosc. 2011;25(7):2323–9.
DuPree CE et al. Laparoscopic sleeve gastrectomy in patients with preexisting gastroesophageal reflux disease: a national analysis. JAMA Surg. 2014;149(4):328–34.
Sucandy I et al. Gastroesophageal reflux symptoms after laparoscopic sleeve gastrectomy for morbid obesity. The importance of preoperative evaluation and selection. N Am J Med Sci. 2015;7(5):189–93.
Thereaux J et al. pH monitoring of gastro-oesophageal reflux before and after laparoscopic sleeve gastrectomy. Br J Surg. 2016;103(4):399–406.
Stenard F, Iannelli A. Laparoscopic sleeve gastrectomy and gastroesophageal reflux. World J Gastroenterol. 2015;21(36):10348–57.
Burgerhart JS et al. Effect of sleeve gastrectomy on gastroesophageal reflux. Obes Surg. 2014;24(9):1436–41.
Kindel TL, Oleynikov D. The improvement of gastroesophageal reflux disease and Barrett’s after bariatric surgery. Obes Surg. 2016;26(4):718–20.
Frenkel C, et al. The effect of sleeve gastrectomy on extraesophageal reflux disease. Surg Obes Relat Dis. 2015.
Silecchia G et al. Residual fundus or neofundus after laparoscopic sleeve gastrectomy: is fundectomy safe and effective as revision surgery? Surg Endosc. 2015;29(10):2899–903.
Kleidi E et al. The effect of laparoscopic sleeve gastrectomy on the antireflux mechanism: can it be minimized? Surg Endosc. 2013;27(12):4625–30.
Stubbs RS, O'Brien I, Jurikova L. What ring size should be used in association with vertical gastric bypass? Obes Surg. 2006;16(10):1298–303.
Arasaki CH et al. Incidence of regurgitation after the banded gastric bypass. Obes Surg. 2005;15(10):1408–17.
Iannelli A. et al. Laparoscopic conversion of sleeve gastrectomy to Roux-en-Y gastric bypass: indications and preliminary results. Surg Obes Relat Dis. 2016.
Quezada N et al. Laparoscopic sleeve gastrectomy conversion to Roux-en-Y gastric bypass: experience in 50 patients after 1 to 3 years of follow-up. Surg Obes Relat Dis. 2016;12(8):1611–5.
AlSabah S et al. Approach to poor weight loss after laparoscopic sleeve gastrectomy: re-sleeve vs. gastric bypass. Obes Surg. 2016;26(10):2302–7.
Homan J et al. Secondary surgery after sleeve gastrectomy: Roux-en-Y gastric bypass or biliopancreatic diversion with duodenal switch. Surg Obes Relat Dis. 2015;11(4):771–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study. The institutional ethics committee approved retrospective data evaluation of all patients (Ref. number: 321/13).
Conflict of Interest
The authors declare that they have no conflicts of interests.
Rights and permissions
About this article
Cite this article
Fink, J.M., Hoffmann, N., Kuesters, S. et al. Banding the Sleeve Improves Weight Loss in Midterm Follow-up. OBES SURG 27, 1098–1103 (2017). https://doi.org/10.1007/s11695-017-2610-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-017-2610-0