Abstract
Background
Endoscopic sleeve gastroplasty (ESG) is an option for patients with Class I and II obesity or patients who refuse to undergo a laparoscopic bariatric surgery. The aims of this study are as follows: (1) to demonstrate a short-term outcome after primary ESG and (2) to compare the effectiveness of weight loss between Class I and Class II obesity patients.
Methods
Patients undergoing ESG at four bariatric centers in Brazil between April 1, 2017 and December 31, 2018 were prospectively enrolled in the study (BMI 30.0–39.9 kg/m2). ESG was performed using Overstitch (Apollo Endosurgery, Austin, TX). Descriptive analysis, t test, Chi-square test, and Mann–Whitney test were used to present the results.
Results
A total of 233 patients underwent primary ESG. The mean age and BMI of the patients were 41.1 years and 34.7 kg/m2, respectively. Following ESG, the mean percentage of total weight loss (TWL) was 17.1% at 6 months and 19.7% at 12 months. Percentage of excess BMI loss (EBMIL) was 47.3% at 6 months and 54.8% at 12 months after ESG. The mean EBMIL was significantly greater among patients with Class I obesity than those with Class II obesity at 6 (51.1% vs. 43.7%) and 12 months (60.2% vs. 49.2%). One patient experienced bleeding during the procedure that was managed with sclerotherapy.
Conclusion
Short-term results suggest that ESG is a safe and effective option for patients with Class I and II obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The prevalence of obesity is increasing worldwide and poses a serious public health concern [1]. Obesity is associated with a higher risk of developing diabetes mellitus, hypertension, and various types of cancers [1]. For severe obesity [body mass index (BMI) ≥ 35 kg/m2], bariatric surgery is known to be effective for sustained significant weight loss [2]. Bariatric procedures, such as laparoscopic sleeve gastrectomy (LSG), are also effective for patients with Class I obesity (BMI less than 35 kg/m2). However, for patients with a lower BMI, many surgeons do not routinely perform bariatric surgery due to concerns about the risk–benefit ratio [3, 4]. In other words, the probability of surgical complications may outweigh the benefits of losing weight in patients with Class I and II obesity and without a comorbidity.
Therefore, in recent years, non-interventional therapies have attempted to induce weight loss in patients with Class I and Class II (BMI 35–40 kg/m2) obesity. Medications such as liraglutide and semagludite have shown 10–15% weight loss along with improvement in type 2 diabetes in this group of patients [5,6,7,8,9]. Novel endoscopic techniques, including intragastric balloon, endoscopic suturing, and aspiration therapy, also have been introduced for these patients [4, 10,11,12].
Among these, endoscopic sleeve gastroplasty (ESG) creates a restrictive sleeve by placing full-thickness triangular sutures from the pre-pyloric antrum to the gastroesophageal junction [13]. After its introduction in 2013, several other studies have reported technical feasibility, short-term effectiveness, and safety of ESG [13,14,15,16,17,18]. One study also presented physiologic changes (i.e. early satiety, delayed gastric emptying) after ESG that may be promising for sustained weight loss [19].
The primary aim of this study is to build on previous literature and demonstrate a short-term outcome after primary ESG in a large multicenter cohort. The secondary aim of this study is to compare the effectiveness of weight loss between Class I and Class II obesity patients.
Methods
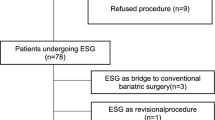
After institutional review board (IRB) approval and following the Health Insurance Portability and Accountability Act guidelines, the authors prospectively enrolled 308 patients undergoing ESG at four bariatric centers in Brazil between April 1, 2017 and December 31, 2018. Patients with prior gastric surgery, the use of anticoagulants, psychiatric disorders, and severe esophagitis were excluded from the study. Patients with a previous bariatric procedure were included in the study but excluded at the data analysis stage. Only patients with Class I and II obesity (BMI between 30.0 and 39.9 kg/m2) were included in the analyses. ESG was performed using Overstitch (Apollo Endosurgery, Austin, TX) by 8 surgeons in 4 bariatric centers as previously described [13].
Patients were followed up at our office clinic at 1, 3, 6, 9, 12 months postoperatively and every 6 months thereafter. Follow-up visits included weight measurement, and clinical history and examination.
Procedure
Patients received intravenous prophylactic antibiotics, 5000 units of intravenous heparin, 4 mg of ondansetron, 10 mg of steroid, and 40 mg of omeprazole. Hyoscyamine 0.125 mg was also administered to prevent esophageal spasm.
All procedures were done under general anesthesia with the patient on left side down. An overtube was used to protect the patient. A single channel diagnostic scope (190 gastrointestinal videoscope, Olympus, Tokyo, Japan) was introduced, followed by a double channel scope (190 gastrointestinal videoscope, Olympus) with the Overstitch device attached.
All surgeons/endoscopists were proctored by a single proctor and performed the procedure using the same technique. Non-absorbable sutures were used to perform the tubulization of the stomach starting from the distal body at the angular incisure to the proximal body with gastric. Sutures were performed in U shape without reinforcement. Sutures were performed in the order of the anterior wall—great curvature—posterior wall—posterior wall—great curvature—anterior wall. The distance between one point and another was 2–3 cm (Fig. 1).
After the procedure, patients received 2 L of saline solution for hydration. Patients were continued with the anti-emetics, started on clear liquid, and kept in post-anesthesia care unit (PACU) for 2 h before discharge. The overall cost of the procedure was approximately $11,000.
Statistical analysis
All data for age and body mass index (BMI) are demonstrated as mean ± standard deviation unless otherwise noted. Descriptive analysis was used to demonstrate the overall weight loss outcome. Two-tailed Student’s t test for continuous variables and Chi-square test for categorical variables were used to demonstrate the comparison between Class I obesity and Class II obesity subsets of patients. Mann–Whitney test was used when continuous variables were not normally distributed. All statistical analyses were performed using SAS software version 9.4 (SAS Institute, Cary, NC).
Results
Overall outcome
A total of 233 patients underwent primary ESG and met the inclusion criteria. The mean age and BMI of the patients were 41.1 years and 34.7 kg/m2, respectively, and 73.0% (n = 170) were female (Table 1). In 9.5% of the patients, an abnormality was found in the upper endoscopy. Abnormal findings included esophagitis (n = 15), hiatal hernia (n = 6), and gastric polyp (n = 1).
Following ESG, the mean percentage of total weight loss (TWL) was 13.1%, 17.1%, 16.9%, and 19.7% at 3, 6, 9, and 12 months, respectively (Table 2, Fig. 2). Percentage of excess BMI loss (EBMIL) was 36.1% at 3 months, 47.3% at 6 months, 47.1% at 9 months, and 54.8% at 12 months after the ESG. Figure 3 shows non-parametric change trajectories of BMI in these patients.
Mild adverse events (i.e. abdominal pain, nausea, vomiting), which did not require further medical attention, were not systematically recorded. One patient experienced bleeding during the procedure that was managed with sclerotherapy.
Class I obesity vs. Class II obesity
Baseline characteristics were similar between patients with Class I obesity and those with Class II obesity (Table 1). However, patients with Class I obesity were more likely to be female (79.3% vs. 66.1%) and were less likely to have abnormality (5.8% vs. 13.4%) during preoperative upper endoscopy than patients with Class II obesity.
Following ESG, the mean TWL were similar between the two groups of patients (Table 3). However, the mean EBMIL was significantly greater among patients with Class I obesity than those with Class II obesity at 6 (51.1% vs. 43.7%) and 12 months (60.2% vs. 49.2%). Figure 4 shows non-parametric change trajectories of EBMIL between the two groups of patients.
Discussion
The gathered data suggest that ESG is safe and results in successful short-term weight loss and lowering of BMI among patients with BMI between 30.0 and 39.9 kg/m2. The risk of complications for this procedure was very low.
This study showed that patients undergoing ESG achieved 19.7% of TWL and 54.8% of EBMIL at 12 months following the procedure. Graus Morales et al. [14] demonstrated that the mean TWL was 17.5% and the mean percentage of excess weight loss (EWL) was 75.4% at 12 months after ESG in their 144 patients. In the largest cohort of ESG studies so far, Alqahtani et al. [17] showed that the mean TWL was 15.0% at 12 months among their 1000 patients. Baseline mean BMIs of their patients (33.4 and 33.3 kg/m2, respectively) were slightly lower than that of our study population (34.7 kg/m2). In a retrospective study, Fayad et al. [20] showed that TWL was lower in the ESG group than in the LSG group at 6-month follow-up (17.1% vs. 23.6%, p < 0.01). As with previous studies, weight loss after ESG in our patients was smaller than the typical weight loss following laparoscopic bariatric procedures [17, 21]. However, ESG was associated with a significantly lower rate of morbidity compared to LSG and laparoscopic gastric banding [21]. In the 6-month retrospective study, Fayad et al. [20] also reported that ESG patients had significantly lower rates of adverse events than LSG patients (5.2% vs. 16.9%). One patient in the study by Graus Morales et al. [14] experienced bleeding at the insertion point of the helix. We also observed bleeding in only one patient (0.3%). Lopez-Nava et al. [13] reported complications in 2.0% of their patients, and Alqahtani et al. [17] reported a readmission rate of 2.4% after ESG. Our study supports these low complication rates by showing that none of our patients underwent a reoperation.
ESG is one of the options for patients who are not suitable for or unwilling to undergo a laparoscopic procedure. Pharmacotherapy (e.g. liraglutide and semagludite) also showed promising results (TWL 10–15%) without the risks of general anesthesia [5,6,7,8]. However, the risk of long-term medication use has not been well established; the cost can also be high (up to $1,000 a month out-of-pocket) for long-term use [7].
Other endoscopic options are also available [22, 23]. In a randomized controlled trial, patients undergoing aspiration therapy achieved 14.2%, 15.3%, 16.6%, and 18.7% TWL at 1, 2, 3, and 4 years, respectively, with minimal complication [24]. Nystrom et al. [25] also reported similar TWL of 18.2% at 1 year after aspiration therapy. The results of aspiration therapy are similar to our results after ESG. On the other hand, mean weight loss after an intragastric balloon procedure was poorer than that of an ESG [26, 27]. TWL after an intragastric balloon was approximately 9.7% at 6-month, and one balloon could only be placed for 6 months at an approximate cost of $8000 [28]. ESG is favorable than intragastric balloons in terms of cost and sustainability of weight loss [26, 27].
Graus Morales et al. [14] reported that the mean EWL among patients with BMI < 35 kg/m2 were significantly greater than that among patients with BMI between 35 and 40 kg/m2 at 12 months after ESG. Lopez-Nava et al. [13] showed that patients with BMI > 35 kg/m2 lost greater TWL than patients with BMI ≤ 35 kg/m2 at 6 and 24 months after ESG. As with the study by Graus Morales et al. [14], our study showed that the mean EBMIL among patients with Class I obesity was greater than those with Class II obesity at 6 and 12 months. However, unlike the study by Lopez-Nava et al. [13], our study did not show a significant difference in the mean TWL between the two groups. We should note that a higher variation was observed in EBMIL among patients with Class I obesity than those with Class II obesity. This suggests that although more patients with Class I obesity may achieve their goal weight, weight loss results could be less consistent in this group of patients.
ESG is generally considered safer than laparoscopic procedures; nevertheless, the outcomes of ESG could vary due to multifactorial reasons that ‘likely involve technical and patient-specific factors’ [29]. The experience and specialization of the executing endoscopists may also play a role. Furthermore, a laparoscopic procedure that is technically similar to ESG—laparoscopic gastric fundoplication—showed failure of weight loss that was associated with higher postoperative hunger sensation [30, 31]. Compared to LSG, laparoscopic gastric fundoplication was less effective in long-term weight loss [32].
This study is limited by short follow-up time. Although the study included a large number of prospectively followed patients, we lack information about 47% of patients at 1-year. A randomized study on ESG with a longer follow-up would provide more information on the sustainability of the weight loss. Furthermore, to better address the need for Class I and II obesity population, a more thorough evaluation of the metabolic impact of ESG is warranted.
Conclusions
Short-term results suggest that ESG is a safe and effective option for patients with Class I and II obesity.
References
Arroyo-Johnson C, Mincey KD (2016) Obesity epidemiology worldwide. Gastroenterol Clin North Am 45(4):571–579
Courcoulas AP, Christian NJ, Belle SH, Berk PD, Flum DR, Garcia L et al (2013) Weight change and health outcomes at 3 years after bariatric surgery among individuals with severe obesity. JAMA 310(22):2416–2425
Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N (2015) Bariatric surgery worldwide 2013. Obes Surg 25(10):1822–1832
Force ABET, Committee AT, Abu Dayyeh BK, Edmundowicz SA, Jonnalagadda S, Kumar N et al (2015) Endoscopic bariatric therapies. Gastrointest Endosc 81(5):1073–1086
Christensen RM, Juhl CR, Torekov SS (2019) Benefit-risk assessment of obesity drugs: focus on glucagon-like peptide-1 receptor agonists. Drug Saf 42(8):957–971
Iepsen EW, Torekov SS, Holst JJ (2015) Liraglutide for type 2 diabetes and obesity: a 2015 update. Expert Rev Cardiovasc Ther 13(7):753–767
Nuffer WA, Trujillo JM (2015) Liraglutide: a new option for the treatment of obesity. Pharmacotherapy 35(10):926–934
Fonseca VA, Capehorn MS, Garg SK, Jodar Gimeno E, Hansen OH, Holst AG et al (2019) Reductions in insulin resistance are mediated primarily via weight loss in subjects with type 2 diabetes on semaglutide. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2018-02685
Newsome P, Francque S, Harrison S, Ratziu V, Van Gaal L, Calanna S et al (2019) Effect of semaglutide on liver enzymes and markers of inflammation in subjects with type 2 diabetes and/or obesity. Aliment Pharmacol Ther 50(2):193–203
Movitz BR, Lutfi RE (2017) Endoscopic sleeve gastroplasty: are we burning bridges? Surg Obes Relat Dis. 13(12):2056–2058
Kumar N, Sullivan S, Thompson CC (2017) The role of endoscopic therapy in obesity management: intragastric balloons and aspiration therapy. Diabetes Metab Syndr Obes. 10:311–316
Khan Z, Khan MA, Hajifathalian K, Shah S, Abdul M, Saumoy M et al (2019) Efficacy of endoscopic interventions for the management of obesity: a meta-analysis to compare endoscopic sleeve gastroplasty, aspireassist, and primary obesity surgery endolumenal. Obes Surg 29(7):2287–2298
Lopez-Nava G, Sharaiha RZ, Vargas EJ, Bazerbachi F, Manoel GN, Bautista-Castano I et al (2017) Endoscopic sleeve gastroplasty for obesity: a multicenter study of 248 patients with 24 months follow-up. Obes Surg 27(10):2649–2655
Graus Morales J, Crespo Perez L, Marques A, Marin Arribas B, Bravo Arribas R, Ramo E et al (2018) Modified endoscopic gastroplasty for the treatment of obesity. Surg Endosc 32(9):3936–3942
Sharaiha RZ, Kumta NA, Saumoy M, Desai AP, Sarkisian AM, Benevenuto A et al (2017) Endoscopic sleeve gastroplasty significantly reduces body mass index and metabolic complications in obese patients. Clin Gastroenterol Hepatol 15(4):504–510
Sartoretto A, Sui Z, Hill C, Dunlap M, Rivera AR, Khashab MA et al (2018) Endoscopic sleeve gastroplasty (ESG) is a reproducible and effective endoscopic bariatric therapy suitable for widespread clinical adoption: a large, international multicenter study. Obes Surg. 28(7):1812–1821
Alqahtani A, Al-Darwish A, Mahmoud AE, Alqahtani YA, Elahmedi M (2019) Short-term outcomes of endoscopic sleeve gastroplasty in 1000 consecutive patients. Gastrointest Endosc 89(6):1132–1138
Gys B, Plaeke P, Lamme B, Lafullarde T, Komen N, Beunis A et al (2019) Endoscopic gastric plication for morbid obesity: a systematic review and meta-analysis of published data over time. Obes Surg 29(9):3021–3029
Abu Dayyeh BK, Acosta A, Camilleri M, Mundi MS, Rajan E, Topazian MD et al (2017) Endoscopic sleeve gastroplasty alters gastric physiology and induces loss of body weight in obese individuals. Clin Gastroenterol Hepatol 15(1):37–43
Fayad L, Adam A, Schweitzer M, Cheskin LJ, Ajayi T, Dunlap M et al (2018) Endoscopic sleeve gastroplasty versus laparoscopic sleeve gastrectomy: a case-matched study. Gastrointest Endosc 89:782–788
Novikov AA, Afaneh C, Saumoy M, Parra V, Shukla A, Dakin GF et al (2018) Endoscopic sleeve gastroplasty, laparoscopic sleeve gastrectomy, and laparoscopic band for weight loss: how do they compare? J Gastrointest Surg 22(2):267–273
Glass J, Chaudhry A, Zeeshan MS, Ramzan Z (2019) New era: endoscopic treatment options in obesity-a paradigm shift. World J Gastroenterol 25(32):4567–4579
Perry ZH (2019) Commentary to “efficacy of endoscopic interventions for the management of obesity: a meta-analysis to compare endoscopic sleeve gastroplasty, aspireassist and primary obesity surgery endolumenal”. Obes Surg 29(7):2299–2300
Thompson CC, Abu Dayyeh BK, Kushnir V, Kushner RF, Jirapinyo P, Schorr AB et al (2019) Aspiration therapy for the treatment of obesity: 4-year results of a multicenter randomized controlled trial. Surg Obes Relat Dis 15(8):1348–1354
Nystrom M, Machytka E, Noren E, Testoni PA, Janssen I, Turro Homedes J et al (2018) Aspiration therapy as a tool to treat obesity: 1- to 4-year results in a 201-patient multi-center post-market european registry study. Obes Surg 28(7):1860–1868
Fayad L, Cheskin LJ, Adam A, Badurdeen DS, Hill C, Agnihotri A et al (2019) Endoscopic sleeve gastroplasty versus intragastric balloon insertion: efficacy, durability, and safety. Endoscopy 51(6):532–539
Haddad AE, Rammal MO, Soweid A, Shararra AI, Daniel F, Rahal MA et al (2019) Intragastric balloon treatment of obesity: long-term results and patient satisfaction. Turk J Gastroenterol 30(5):461–466
Tate CM, Geliebter A (2017) Intragastric balloon treatment for obesity: review of recent studies. Adv Ther 34(8):1859–1875
Storm AC, Abu Dayyeh BK (2019) Endoscopic sleeve gastroplasty for obesity: defining the risk and reward after more than 1600 procedures. Gastrointest Endosc 89(6):1139–1140
Gudaityte R, Adamonis K, Maleckas A (2018) Laparoscopic gastric greater curvature plication: intermediate results and factors associated with failure. Obes Surg 28(12):4087–4094
Alqahtani AR, Elahmedi M, Alqahtani YA, Al-Darwish A (2019) Laparoscopic sleeve gastrectomy after endoscopic sleeve gastroplasty: technical aspects and short-term outcomes. Obes Surg. https://doi.org/10.1007/s11695-019-04024-x
Barrichello S, Minata MK, Garcia Ruiz de Gordejuela A, Bernardo WM, de Souza TF, Galvao Neto M et al (2018) Laparoscopic greater curvature plication and laparoscopic sleeve gastrectomy treatments for obesity: systematic review and meta-analysis of short- and mid-term results. Obes Surg 28(10):3199–3212
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Dr. Neto is a proctor and consultant for Apollo Endosurgery. Dr. Teixeira is a consultant for Intuitive Surgical and Ethicon Endo-surgery. Dr. Jawad is a consultant for Ethicon Endo-surgery. Dr. Abu Dayyeh is a consultant for USGI and Olympus and the recipient of research support from Apollo Endosurgery. Drs. Moon, Quadros, Grecco, Filho, Souza, Mattar, Sousa, Morais, and Matz have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Neto, M.G., Moon, R.C., de Quadros, L.G. et al. Safety and short-term effectiveness of endoscopic sleeve gastroplasty using overstitch: preliminary report from a multicenter study. Surg Endosc 34, 4388–4394 (2020). https://doi.org/10.1007/s00464-019-07212-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-07212-z