Abstract
Background
We have done curative or palliative extended extrahepatic bile duct resection at the level of the hilar plate for selected patients with cholangiocarcinoma with hilar spreading, calling this procedure “hilar plate resection” (HPR), but the results of evaluating the clinical benefits of HPR for cholangiocarcinoma with hilar spreading have not been reported.
Patients and Methods
Fifty-two patients with cholangiocarcinoma underwent HPR: the curative procedure was performed in 28 patients (cHPR group) and the palliative in 24 patients (pHPR group). In the same period, 128 patients with cholangiocarcinoma underwent major hepatectomy with intrahepatic cholangiojejunostomy (Hx group). These groups were compared in terms of post-operative complications and survival.
Results
There were no significant differences in the rate of patients with post-operative complications and in post-operative hospital stay. The overall cumulative 5-year survival rates for each procedure (Hx group, cHPR group and pHPR group) were 40, 38 and 11 %, respectively. There was no significant difference between the Hx and cHPR groups in survival rates (p = 0.87).
Conclusion
In conclusion, HPR appears to be safe and feasible for selected patients with cholangiocarcinoma. However, the indications for HPR should be restricted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hilar cholangiocarcinoma or distal cholangiocarcinoma with hilar spreading continues to be among the most difficult cancers to manage in terms of staging and performing curative resection. In the treatment of hilar cholangiocarcinoma, several studies have advocated en bloc major hepatectomy to achieve negative histologic margins and improved survival.1 – 6
Since these extended surgical procedures have serious problems, including high morbidity, especially with post-operative liver failure, various parenchyma-preserving hepatectomy procedures with potential curability have been proposed, such as caudate lobectomy alone, caudate lobectomy combined with medial segmentectomy, anterior segmentectomy and central bisegmentectomy.2,4,5,7 – 11 However, these procedures were often dubbed “noble” operations, because their curability and low surgical risk were associated with heavy demands on the surgeon.
We know that there are some patients with distal cholangiocarcinoma with longitudinal spread remaining in the hilar portion (extrahepatic portion), without infiltration beyond the bile duct wall (distal cholangiocarcinoma with hilar spreading). These lesions should be treated thoroughly so as not to leave cancer at the proximal side of the bile duct. We also know that there are a few patients with Bismuth type I hilar cholangiocarcinoma without infiltration beyond the bile duct wall. These tumours are likely to have superficial spreading, which would be difficult to accurately diagnose preoperatively.12 It remains unknown whether, for patients with such a non-invasive tumour, extended hepatectomy would be appropriate. Some patients having hilar cholangiocarcinoma with non-invasive and limited spreading lesions could be treated with bile duct resection without hepatectomy.
Conventional hilar bile duct resection (CHBDR) at the level just above the bile duct confluence would likely result in cancer-positive margins due to superficial tumour in hilar malignancies.12,13 Therefore, we have done extended extrahepatic bile duct resection at the level of the hilar plate for selected patients, calling this procedure hilar plate resection (HPR).
The results of a retrospective study evaluating the clinical benefits in patients who underwent HPR for cholangiocarcinoma are reported.
Patients and Methods
Surgical Indications
As shown in our previous report, from 2000 to 2004, we choose various operative procedures according to evaluation of intraductal longitudinal spread by precise cholangiography. Preoperative diagnosis and operative strategy for hilar cholangiocarcinoma in this period were shown in previous our report in 2004.1
Since 2004, HPR has mainly been used for the following types of patients: (1) patients with distal cholangiocarcinoma with hilar spreading and (2) selected patients with hilar cholangiocarcinoma without infiltration beyond the bile duct, with longitudinal spread remaining in the area of resection of HPR and with the no obvious suspicions of spreading to caudate branch. These diagnoses were mainly made by precious cholangiography.1 Most patients with invasive tumour in the perihilar portion were diagnosed to be candidates for major hepatectomy.
We have also used this operation as a palliative procedure for patients with insufficient future remnant hepatic reserve for major hepatectomy, with severe systemic comorbidities (e.g. cerebral infarctions, moderate to severe ischemic heart disease) or with decreased performance status. It was determined that these patients could undergo no residual tumour or microscopic residual tumour resection by HPR, even if the procedure was done with palliative intention. If the patient was found to have a macroscopic residual tumour resection with HPR, non-operative treatment was selected.
Operative indications for major hepatectomies or vascular combined resection were described in our previous report.2
Patients
From August 2000 to October 2010, 52 patients with cholangiocarcinoma (32 patients with hilar and 20 patients with distal cholangiocarcinoma with hilar spreading) underwent HPR at the Department of Surgery II, Hokkaido University Hospital.
In the same period, 128 patients underwent major hepatectomy with intrahepatic cholangiojejunostomy for cholangiocarcinoma (124 patients with hilar cholangiocarcinoma and 4 patients with distal cholangiocarcinoma with hilar spreading). A total of 180 patients were evaluated in this study (Table 1). Patients’ performance status (PS) was evaluated by the Eastern Cooperative Oncology Group score.14
Surgical Procedure of HPR
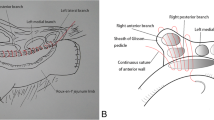
Nodal clearance around the pancreatic head and skeletonization of the portal vein and the hepatic artery were performed first. The portal vein and the hepatic artery were then separated from the surrounding tissue upward to the hilar plate, where the duct cannot be further separated from the vasculature. This was considered “the limit of ductal transection without hepatectomy”, which is at the right edge of the posterior portion of the right portal vein and the right edge of the umbilical portion of the left portal vein.15,16 Then, the gallbladder with the “cystic plate” was resected toward the hepatic hilum. Finally, the extrahepatic duct at the hilar plate was resected. The portions resected in HPR are shown in Fig. 1. The difference between HPR and CHBDR, which used to be performed by many surgeons, is the level of ductal resection. In a patient with HPR, the bile ducts at the level of the hilar plate were resected. On the other hand, in a patient with CHBDR, the hilar bile ducts were usually resected around the level of the confluence of bilateral hepatic ducts. The bile duct portions resected in CHBDR and HPR are shown in Fig. 1.
Schematic of hilar plate resection (HPR) and conventional hilar bile duct resection (CHBDR). In HPR, the extrahepatic ducts are resected to the limit of ductal transection without hepatectomy, which is at the right edge of the posterior portion of the right portal vein and the right edge of the umbilical portion of the left portal vein. In CHBDR, the extrahepatic bile ducts are resected at the level just above the bile duct confluence (BC). Thick lines indicate the level of the hilar bile ducts resected with HPR and CHBDR. UP umbilical portion, Bp bile duct of the posterior segment, B1r bile duct of right caudate lobe, B1l bile duct of left caudate lobe, B2 bile duct of segment 2, B3 bile duct of segment 3, B4 bile duct of segment 4, B5 bile duct of segment 5, B8 bile duct of segment 8
Depending on the anatomical characteristics, there were three to five or more divided duct stumps to be anastomosed. A Roux-en-Y cholangiojejunostomy was then performed. In this procedure, two orifices in the jejunum were created due to the distance between the ducts.17 Our surgical procedure for pancreaticoduodenectomy and hepatectomies for cholangiocarcinoma has been described previously.2,3,15,18
Pathological Diagnosis and Analysis
In this report, the clinical features and histological findings were described using the seventh edition of the American Joint Committee Cancer Classification.19 Tumour type in the present study was classified according to the fifth edition of the Japanese General Rules for Classification of Biliary Tract Carcinoma currently used in Japan.20
The pathological diagnosis protocol was based on prior studies.12 The bile duct of the specimen was opened longitudinally, pinned to a board and immediately fixed in 10 % formalin. The surgical margin was diagnosed by experienced pathologists. Descriptions of margin status in this report follow the second edition of the Japanese Classification of Biliary Tract Carcinoma: hepatic margin status (HM), distal (duodenal) cut-end margin (DM) and dissected periductal structure margin (EM).20 Patients with a cancer-free margin 5 mm or less in any direction were considered cancer-positive. Cases with a cancer-free margin of more than 5 mm in any direction from the biliary stump including the periductal margin were considered surgical margin-negative. Superior margin status was calculated by the macroscopic distance from the middle point of the confluence of the right and left hepatic bile ducts, as reported by Shimada et al..8 When there were multiple bile ducts on the right and left sides, the mean of the bile duct of each side was used.
Statistical Analysis
Statistical calculations were performed using Stat Flex (Artech Co., Ltd., Osaka, Japan) and “Exact Test” produced by Prof. S. Aoki (http://aoki2.si.gunma-u.ac.jp/exact/exact.html). Chi-squared, Fisher’s exact and Mann-Whitney’s U tests were used as appropriate. Cumulative survival after surgery was calculated using the Kaplan-Meier method. The log-rank test was used to compare cumulative survival. A Cox proportional regression hazards model was used for multivariate analysis. Values of p < 0.05 were considered significant.
Results
Clinical Characteristics
Table 1 shows the patients’ characteristics. There were a few differences in clinical characteristics between patients who underwent HPR (HPR group) and those who underwent major hepatectomy (Hx group) (Table 1). The patients were older in the HPR group than in the Hx group (p < 0.01), there were more patients with hilar cholangiocarcinoma in the Hx group and there were more patients with lower performance status and respiratory complications in the HPR group.
HPR was performed with curative intention in 28 patients (cHPR group) and with palliative intention in 24 patients (pHPR group). In the cHPR group, there were 11 cases of hilar cholangiocarcinoma and 17 of distal cholangiocarcinoma with hilar spreading. In the pHPR group, there were 21 cases of hilar cholangiocarcinoma and 3 of distal cholangiocarcinoma with hilar spreading.
The reasons for performing pHPR were insufficient future remnant hepatic reserve for major hepatectomy (n = 17), low PS (n = 5) and bilateral superficial tumour spreading beyond the resection limit (n = 2).
Operative Results
Operative results of the HPR group and Hx group in the same period are shown in Table 2. There were no differences in length of operation time, morbidity and post-operative hospital stay. However, there were significant differences in operative blood loss (number of patients requiring blood transfusion) and number of bile ducts reconstructed (Table 2).
Pathological Results with HPR
The pathological results of the HPR group are shown in Table 3. The median length of the bile duct from the bile duct confluence was 17 (5–41) mm on the right side and 16 (10–41) mm on the left side. There were no significant differences between the cHPR group and the pHPR group in the lengths of the bile ducts in the hilar lesions.
The histological margins were positive in 33 patients. The pHPR group had more patients with a positive histological margin than the cHPR group (p < 0.01).
Survival
The overall cumulative survival rates of the hilar and distal cholangiocarcinoma patients (128 patients in the Hx group, 28 patients in the cHPR group and 24 patients in the pHPR group) were 58, 54 and 37 % at 3 years and 40, 38 and 11 at 5 years, respectively (Fig. 2). There was no significant difference between the Hx group and the cHPR group in survival rates (p = 0.87). The survival rate of the pHPR group was significantly lower than that of the Hx group (p = 0.03). The survival rate of the pHPR group was lower, but not significantly, than that of the cHPR group (p = 0.08).
Post-operative survival in resected patients with hilar and distal cholangiocarcinoma according to surgical procedure. There was no significant difference between the Hx and the cHPR in survival rates (p = 0.87). The survival rate of the pHPR group was significantly lower than that of the Hx group (p = 0.03). The survival rate of the pHPR group was lower, but not significantly, than that of the cHPR group (p = 0.08). Hx hepatectomy, cHPR group patients who underwent hilar plate resection with curative intention, pHPR group patients who underwent hilar plate resection with palliative intention
Next, to clarify the effect on survival of the surgical margin, the survival of the cHPR group was evaluated. The overall cumulative survival rates of patients who were surgical margin-free and patients with a surgical margin of less than 5 mm were 72 and 33 % at 3 years and 63 and 11 % at 5 years, respectively. There were significant differences between the two groups (p = 0.02).
Discussion
With recent improvements in diagnostic and preoperative management, many surgeons have adopted an aggressive approach to hilar malignancies with satisfactory results.21 – 25 Our previous report showed that the survival of patients treated with right hepatectomy was significantly higher.1 This was most likely due to the fact that right hepatectomy enables en bloc resection of the hepatic ductal confluence and its surrounding structures, because the confluence lies on the right side of the hepatic hilum. Ikeyama et al. also showed that, even with a Bismuth type I or II tumour, hilar cholangiocarcinoma of the nodular and infiltrating types should be treated by right hepatectomy.13 These reports determined the operative strategy for hilar cholangiocarcinoma. Today, there is no doubt that major hepatectomy is the first-choice treatment for hilar cholangiocarcinoma.
However, several questions remained unsolved. One question was whether these extended procedures would be appropriate for patients with hilar or distal cholangiocarcinoma with hilar spreading. The second question was how to treat hilar cholangiocarcinoma patients with insufficient liver function or with lack of future remnant liver reserve for hepatectomy, as well as those with severe systemic complications. The present results are the key to resolving these questions.
HPR is a unique technique for complete extrahepatic bile duct resection. In this procedure, the extrahepatic bile ducts were resected at the level of the hilar plate. Therefore, we believe that HPR differs from hepatic parenchyma-preserving resections and CHBDR.
Shimada et al. were the first to report a similar procedure in 2002.8 They discussed five patients with hilar cholangiocarcinoma who underwent extended bile duct resection, and they concluded that their procedure was indicated for hilar cholangiocarcinoma in selected cases with a papillary or nodular appearance.
Aydin et al. also reported a similar procedure.26 They discussed 10 cases with hilar cholangiocarcinoma who underwent “high hilar resection”. There were several differences between Aydin’s procedure and our HPR. Their operation required parenchymal resection, including about 1–1.5 cm of the hilar part of segments 5 and 4b; they also partially resected segment 1. HPR was a complete hepatic parenchyma-preserving operation.
These previous studies had only small numbers of patients; therefore, the results of the present 52 cases of HPR for cholangiocarcinoma are the first to show the procedure’s safety. The present data show that there were no significant differences in morbidity and mortality compared with major hepatectomies, even though the present cases of HPR included more patients with severe systemic comorbidities or lower performance status. These results show that HPR for selected patients with extrahepatic cholangiocarcinoma appears to be an appropriate operation given its safety and survival.
The present data showed that the median bile duct lengths from bile duct confluence to hepatic stump resected in this procedure were 17 (5–41) mm on the right side and 16 (10–41) mm on the left side (Table 3). We believe that identification of both the limit of ductal resection and the length of the bile duct resected is extremely important for biliary surgery.15 Shimada et al. previously reported similar results.8 Masunari et al. analysed the length from the confluence of the hepatic duct to the “limit of the bile duct transected with hepatectomy”.16 They showed that the length from the confluence of the hepatic duct measured about 25 and 30 mm on the right and left sides, respectively. These results showed that the length of the resected hepatic duct that the surgeon could resect without hepatectomy was less than 20 mm.
The present data showed that selected patients in the cHPR group in whom a cancer-free margin of more than 5 mm in any direction (cancer-free) was obtained would have a satisfactory survival result (Fig. 3). This may explain the low survival rate in the pHPR group. The number of cancer-free patients was significantly higher in the pHPR group than in the cHPR group (Table 3).
Even though there were several clinical benefits of HPR, it is our view that the indications for HPR should be restricted. There were several problems with this procedure: anatomical difficulties requiring specialized technique and lengthy operation time; a relatively high cancer-positive rate even in the cHPR group, despite the fact that HPR was done for selected patients as described before; and a survival rate significantly worse in patients with a surgical margin of less than 5 mm than in surgical margin-free patients. Therefore, further investigations would be needed to determine suitable candidate for performing cHPR.
It is still unknown whether this palliative procedure is indicated in hilar malignancies. The 5-year survival rate was significantly worse in the pHPR group than in the Hx group. Furthermore, this procedure had a relatively high morbidity as a palliative procedure. Nevertheless, some patients would derive clinical benefit such as a stent-free life, and a few patients showed long-term survival. A randomized trial would be almost impossible because of the very limited number of patients who present with this disease.
In conclusion, HPR appears to be safe and feasible for selected patients with cholangiocarcinoma. However, the indications for HPR should be restricted. Considering the clinical benefit and the associated problems, HPR appears to be indicated for tumours with or without superficial cancer spread limited to less than 10 mm above the bile duct confluence.
References
Kondo S, Hirano S, Ambo Y, Tanaka E, Okushiba S, Morikawa T, et al. Forty consecutive resections of hilar cholangiocarcinoma with no postoperative mortality and no positive ductal margins: results of a prospective study. Annals of surgery. 2004;240(1):95-101. Epub 2004/06/24.
Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K, et al. Outcome of surgical treatment of hilar cholangiocarcinoma: a special reference to postoperative morbidity and mortality. Journal of hepato-biliary-pancreatic surgery. 2009;17(4):455-62. Epub 2009/10/13.
Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K. No-touch resection of hilar malignancies with right hepatectomy and routine portal reconstruction. Journal of hepato-biliary-pancreatic surgery. 2009;16(4):502-7. Epub 2009/04/11.
Miyazaki M, Kimura F, Shimizu H, Yoshidome H, Otuka M, Kato A, et al. One hundred seven consecutive surgical resections for hilar cholangiocarcinoma of Bismuth types II, III, IV between 2001 and 2008. Journal of hepato-biliary-pancreatic sciences. 2010;17(4):470-5. Epub 2009/11/26.
Nagino M, Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, et al. Evolution of Surgical Treatment for Perihilar Cholangiocarcinoma: A Single-Center 34-Year Review of 574 Consecutive Resections. Annals of surgery. 2012. Epub 2012/10/13.
Seyama Y, Kubota K, Sano K, Noie T, Takayama T, Kosuge T, et al. Long-term outcome of extended hemihepatectomy for hilar bile duct cancer with no mortality and high survival rate. Annals of surgery. 2003;238(1):73-83. Epub 2003/07/02.
Kosuge T, Yamamoto J, Shimada K, Yamasaki S, Makuuchi M. Improved surgical results for hilar cholangiocarcinoma with procedures including major hepatic resection. Annals of surgery. 1999;230(5):663-71. Epub 1999/11/24.
Shimada H, Endo I, Fujii Y, Kunihiro O, Tanaka K, Misuta K, et al. Procedure of extended hilar bile duct resection and its application for hilar cholangiocarcinoma. Hepato-gastroenterology. 2002;49(44):300-5. Epub 2002/05/09.
Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Okaya T, et al. Parenchyma-preserving hepatectomy in the surgical treatment of hilar cholangiocarcinoma. Journal of the American College of Surgeons. 1999;189(6):575-83. Epub 1999/12/10.
Shimada H, Endo I, Sugita M, Masunari H, Fujii Y, Tanaka K, et al. Is parenchyma-preserving hepatectomy a noble option in the surgical treatment for high-risk patients with hilar bile duct cancer? Langenbeck’s archives of surgery / Deutsche Gesellschaft fur Chirurgie. 2003;388(1):33-41. Epub 2003/04/12.
Kawarada Y, Das BC, Naganuma T, Tabata M, Taoka H. Surgical treatment of hilar bile duct carcinoma: experience with 25 consecutive hepatectomies. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2002;6(4):617-24. Epub 2002/07/20.
Nakanishi Y, Zen Y, Kawakami H, Kubota K, Itoh T, Hirano S, et al. Extrahepatic bile duct carcinoma with extensive intraepithelial spread: a clinicopathological study of 21 cases. Modern pathology : an official journal of the United States and Canadian Academy of Pathology, Inc. 2008;21(7):807-16. Epub 2008/04/22.
Ikeyama T, Nagino M, Oda K, Ebata T, Nishio H, Nimura Y. Surgical approach to bismuth Type I and II hilar cholangiocarcinomas: audit of 54 consecutive cases. Annals of surgery. 2007;246(6):1052-7. Epub 2007/11/29.
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. American journal of clinical oncology. 1982;5(6):649-55. Epub 1982/12/01.
Hirano S, Tanaka E, Shichinohe T, Suzuki O, Hazama K, Kitagami H, et al. Treatment strategy for hilar cholangiocarcinoma, with special reference to the limits of ductal resection in right-sided hepatectomies. Journal of hepato-biliary-pancreatic surgery. 2007;14(5):429-33. Epub 2007/10/03.
Masunari H, Shimada H, Endo I, Fujii Y, Tanaka K, Sekido H, et al. Surgical anatomy of hepatic hilum with special reference of the plate system and extrahepatic duct. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2008;12(6):1047-53. Epub 2007/10/17.
Hirano S, Tanaka E, Tsuchikawa T, Matsumoto J, Shichinohe T, Kato K. Techniques of biliary reconstruction following bile duct resection (with video). Journal of hepato-biliary-pancreatic sciences. 2012;19(3):203-9. Epub 2011/11/15.
Noji T, Miyamoto M, Kubota KC, Shinohara T, Ambo Y, Matsuno Y, et al. Evaluation of extra capsular lymph node involvement in patients with extra-hepatic bile duct cancer. World journal of surgical oncology. 2012;10:106. Epub 2012/06/12.
Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Annals of surgical oncology. 2010;17(6):1471-4. Epub 2010/02/25.
Surgery JSoB. Classification of Biliary Tract Carcinoma Second English Edition. 2nd edition ed: Kanehara Co.,LTD., Tokyo; 2001 2001/04/13.
Hirano S, Kondo S, Tanaka E, Shichinohe T, Tsuchikawa T, Kato K. Safety of combined resection of the middle hepatic artery in right hemihepatectomy for hilar biliary malignancy. Journal of hepato-biliary-pancreatic surgery. 2009;16(6):796-801. Epub 2009/04/24.
Nagino M. Perihilar cholangiocarcinoma: a surgeon’s viewpoint on current topics. Journal of gastroenterology. 2012;47(11):1165-76. Epub 2012/08/01.
Hidalgo E, Asthana S, Nishio H, Wyatt J, Toogood GJ, Prasad KR, et al. Surgery for hilar cholangiocarcinoma: the Leeds experience. Eur J Surg Oncol. 2008;34(7):787-94. Epub 2007/11/27.
Ebata T, Yokoyama Y, Igami T, Sugawara G, Takahashi Y, Nimura Y, et al. Hepatopancreatoduodenectomy for cholangiocarcinoma: a single-center review of 85 consecutive patients. Annals of surgery. 2012;256(2):297-305. Epub 2012/07/04.
Miyazaki M, Kimura F, Shimizu H, Yoshidome H, Otuka M, Kato A, et al. One hundred seven consecutive surgical resections for hilar cholangiocarcinoma of Bismuth types II, III, IV between 2001 and 2008. Journal of hepato-biliary-pancreatic surgery. 2009. Epub 2009/11/26.
Aydin U, Yedibela S, Yazici P, Aydinli B, Zeytunlu M, Kilic M, et al. A new technique of biliary reconstruction after "high hilar resection" of hilar cholangiocarcinoma with tumor extension to secondary and tertiary biliary radicals. Annals of surgical oncology. 2008;15(7):1871-9. Epub 2008/05/06.
Acknowledgments
The authors would like to dedicate this article to Dr. Satoshi Kondo who established HPR; he passed away on January 17, 2011.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Noji, T., Tsuchikawa, T., Okamura, K. et al. Surgical Outcome of Hilar Plate Resection: Extended Hilar Bile Duct Resection Without Hepatectomy. J Gastrointest Surg 18, 1131–1137 (2014). https://doi.org/10.1007/s11605-014-2490-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2490-8