Abstract
Background
The combination of major hepatectomy and pancreatoduodenectomy (PD), that is, a hepatopancreatoduodenectomy (HPD), is the only curative treatment for bile duct cancer with extensive horizontal tumor spread invading both the hepatic hilum and the intrapancreatic bile duct. However, this aggressive procedure remains controversial with regard to the balance between the survival benefit and high risk of mortality and morbidity, especially the risk for postoperative hepatic failure and postoperative pancreatic fistula. Here, we describe the efficacy of a novel modified technique of HPD with delayed division of the pancreatic parenchyma for hilar cholangiocarcinoma, and focus on the surgical technique and the short-term outcomes, with a representative case.
Technical Presentation
This new surgical technique involves dissection of the pancreatic parenchyma and relevant mesoduodenum at the final step after dissecting the required parts on the inferior side and superior side of the tumor, enabling excision of the resected specimen. This technique described herein can prevent saponification of the resected surface of the pancreas by dissecting the pancreatic parenchyma toward the latter half of the surgical procedure as much as possible. The results suggest that there may also be a relationship between this technique and the prevention of postoperative pancreatic fistula.
Conclusion
This new surgical technique of HPD may be able to prevent postoperative pancreatic fistula by performing intraoperative dissection of the pancreatic parenchyma as late as possible, which in turn, may improve the safety of HPD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatopancreatoduodenectomy (HPD) is the only curative treatment for bile duct cancer with extensive horizontal tumor spread invading both the hepatic hilum and the intrapancreatic bile duct. However, this aggressive procedure remains controversial because of the balance between the survival benefit and high risk of mortality and morbidity. In the recent review study, postoperative complications occurred in 78.9% patients, resulting in a perioperative mortality of 10.3%.1
Hepatic failure and pancreatic fistula were the most common and important postoperative complications of HPD. In terms of hepatic failure, preoperative portal vein embolism is aimed at improving safety and tolerance of major hepatectomy and increasing resectability by inducing homolateral atrophy and contralateral compensatory hypertrophy of the remnant liver. The most important strategy for preventing hepatic failure is the meticulous and precise evaluation of the remnant liver function preoperatively. In our institute, postoperative hepatic failure even after HPD can be prevented by using 99mTc-labeled galactosyl human serum albumin liver scintigraphy.2,3
Another life-threatening complication of HPD is pancreatic anastomotic leakage, which is associated with intraabdominal hemorrhage and abscesses. Many studies have reported that the incidence of pancreatic fistula in HPD is higher than that in PD. Various procedures in HPD, such as second-stage pancreatojejunostomy, inserting a tube into the main pancreatic duct, and wrapping an omental flap around the dissected gastroduodenal artery, have been reported to prevent pancreatic fistula. However, the definitive surgical procedure for preventing pancreatic fistula has been unclear, and the surgical technique is thought to require further modification in HPD.
The present study describes the efficacy of a novel modified technique of HPD with delayed division of the pancreatic parenchyma for hilar cholangiocarcinoma and focuses on the surgical technique with a representative case and short-term outcomes.
Surgical Technique
In the surgical procedure described herein, HPD is only described as PD with hepatectomy, without a description of the exact procedure. The primary procedure in many institutions begins with dissection from the caudal direction to the cranial direction. The exact steps are as follows: (1) resection of the small intestine and dissection of the mesoduodeum extending to the inferior margin of the pancreas, (2) dissection of the pancreatic parenchyma and severing of the superior margin of the mesoduodenum, (3) dissection of the hepatoduodenal ligament including excision of the gastroduodenal artery, (4) dissection of the portal vein on the resected side and the remnant bile duct, and (5) resection of the hepatic parenchyma and dissection of the hepatic vein. Since dissection of the remnant bile duct must be conducted between the tumor and remnant hepatic parenchyma in cases of hilar cholangiocarcinoma, it can be extremely technically difficult to execute the fourth step; therefore, this step is sometimes performed after bisection of the liver in the fifth step.
The aforementioned systematic procedure is the most favorable in terms of procedural safety. The reason being that while the surgeon performs the dissections, the tissues being bisected become detached, affording a clearer view for technically difficult procedures, such as dissection of the remnant bile duct. However, as resection of the pancreatic parenchyma occurs quite early in the procedure, leakage of the pancreatic juice from the pancreatic parenchyma is unavoidable even with insertion of a catheter into the main pancreatic duct. Thus, there is a markedly increased possibility of peripancreatic saponification, which would also potentially increase the risk of postoperative pancreatic fistula. To address this, we have proposed and performed the following new surgical technique.
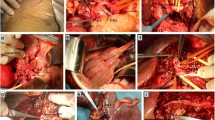
Generally, the new surgical technique involves dissection of the pancreatic parenchyma and relevant mesoduodenum as the final step, after dissecting the required parts on the inferior side and superior side of the tumor, enabling excision of the resected specimen. We describe this technique in detail in the following representative clinical case. A 72-year-old man required left hepatic lobectomy and pylorus-preserving PD with various modalities. The new step-by-step surgical technique was performed as follows: (1) resection of the small intestine and dissection of the mesoduodenum extending to the inferior margin of the pancreas; (2) isolation of Glisson’s pedicles in the liver remnant (Fig. 1a), by applying the hanging maneuver (Fig. 1b), taping only the pancreatic parenchyma that required dissection, and proceeding to dissection of the liver parenchyma (Fig. 1b); (3) isolation of all the blood vessels on the resected side of the portal vein and hepatic artery (Fig. 1c), dissection of the remnant bile duct (Fig. 1d), and then dissection of the portal vein (Fig. 1e) and hepatic artery (Fig. 1f) on the resected side; and (4) dissection of the pancreatic parenchyma (Fig. 1g), followed by dissection of the relevant mesoduodenum (Fig. 1h) and removal of the specimen. In this case, as the right hepatic artery was a total replacement of the superior mesenteric artery, the common hepatic artery was also dissected (Fig. 1f) while dissecting the left hepatic artery. Subsequently, we performed reconstructive procedures and were able to prevent peripancreatic saponification as much as possible. The operative time was 440 min, and blood loss was 450 g.
Picture and schema of the modified surgical approach. a Isolation of Glisson’s pedicles in the liver remnant, especially of the anterior and posterior Glissonian pedicles in this case. b Applying the hanging maneuver. c Isolation of all the blood vessels on the resected side of the portal vein and hepatic artery. d Dissection of the remnant bile duct. e Dissection of the portal vein on the resected side. f Dissection of the hepatic artery on the resected side, in which the common hepatic artery was also dissected, as the right hepatic artery was a total replacement of the superior mesenteric artery. g Dissection of the pancreatic parenchyma. h Dissection of the relevant mesoduodenum and removal of the specimen
This patient had no postoperative complications and an uneventful discharge from the hospital on postoperative day 28. We performed this procedure for two patients with hilar cholangiocarcinoma and these patients had no postoperative complications.
Discussion
As HPD has been reported to be associated with a high operative morbidity and mortality, the safety of HPD was our first priority. To minimize postoperative life-threatening complications, especially liver failure and postoperative pancreatic fistula, preoperative biliary drainage, preoperative portal vein embolization, and second-stage pancreatojejunostomy have been used. Recent studies from high-volume centers have reported improved operative outcomes with mortality rates below 5%.4,5 Certain techniques seem to make postoperative liver failure rare. However, pancreatic fistula remains a major postoperative complication. Second-stage pancreaticojejunostomy is a rather complicated and technically demanding procedure, although this strategy may reduce the degree of complications associated with pancreatic fistula.6 Based on the aforementioned background, it was thought necessary to modify a surgical technique to prevent pancreatic fistula after HPD.
At our institute, eight patients underwent the “traditional” surgical technique for biliary tract cancer between 2008 and 2018. Six patients developed complications over Clavien-Dindo grade III and four patients developed postoperative pancreatic fistula (POPF) grade B. There were no significant differences in the incidence of complications between the traditional and modified technique, and no factors associated with significant differences for all complications or POPF grade B because the number of cases was small.
This new surgical technique described herein can prevent saponification of the resected surface of the pancreas by dissecting the pancreatic parenchyma toward the latter half of the surgical procedure as much as possible. The results suggest that there may also be a relationship with the prevention of postoperative pancreatic fistula. The relationship between saponification and POPF is currently under investigation using basic experiments; however, no conclusion has been drawn. If saponification of the remnant pancreas declines, we may expect that the incidence of POPF will also decline. However, this depends on the degree of activation of the pancreatic juice, this is still unclear. Moreover, in terms of the condition of the pancreatic stump at the start of a pancreatic-jejunal anastomosis, the degree of saponification in this modified surgical technique might be attenuated due to appearance; however, quantifying this is still under consideration.
It is essential to perform liver resection and bile duct dissection earlier in the procedure, which makes the procedure slightly more complex. Other disadvantages include cases where there is rotation of the axis of the incision involving left lobectomy or 3-segmentectomy HPD that requires simultaneous removal of blood vessels, thereby increasing the difficulty of the procedure and potentially increasing blood loss caused by oozing from the dissected surfaces of the liver intraoperatively. We believe that it is possible to overcome these disadvantages by using methods such as approaching the hepatoduodenal ligament from the dorsal side after dissection of the pancreatic parenchyma or taking extra care with the incisions made during bisection of the liver.
Due to the recently proposed anatomy of the liver, the Glissonean pedicle can be entered only at the six gates.7 By applying this theory, it is possible to perform dissection of hepatic parenchyma at the beginning of the procedure in any hemihepatectomy, without particular impediment even in cases where reconstructive procedures for blood flow are required. In fact, a recent article reported that the liver parenchyma transection-first approach is the preferred technique for hemihepatectomy in hilar cholangiocarcinoma because it results in improved surgical outcomes compared with the conventional approach.8
It is important to perform the dissection of the liver parenchyma and bile duct in the early stages of surgical procedures in order to enable delayed dissection of pancreatic parenchyma as much as possible. The isolation of extrahepatic Glissonian pedicles and hanging taping will be a very helpful procedure for these techniques. The advantage of these procedures includes an oncological aspect of approaching from the furthest part from the cancer tumor. However, as a disadvantage, the surgical technique is more difficult and complicated than the traditional technique and it is necessary to ensure that there is no cancer invasion in the extrahepatic Glissonean isolation site during preoperative evaluation.
Conclusion
This new surgical technique in HPD may attenuate the saponification of the remnant pancreas and may prevent postoperative pancreatic fistula by performing dissection of the pancreatic parenchyma as late as possible intraoperatively, which in turn, may improve the safety of HPD.
References
Zhou Y, Zhang Z, Wu L, Li B. A systematic review of safety and efficacy of hepatopancreatoduodenectomy for biliary and gallbladder cancers. HPB (Oxford). 2016;18(1):1–6.
Chiba N, Shimazu M, Takano K, et al. Predicting hepatic failure with a new diagnostic technique by preoperative liver scintigraphy and computed tomography: a pilot study in 123 patients undergoing liver resection. Patient Saf Surg. 2017;11:29. https://doi.org/10.1186/s13037-017-0143-z.
Chiba N, Yokozuka K, Ochiai S, et al. The diagnostic value of 99m-Tc GSA scintigraphy for liver function and remnant liver volume in hepatic surgery: a retrospective observational cohort study in 27 patients. Patient Saf Surg. 2018;12:15. https://doi.org/10.1186/s13037-018-0161-5.
Ebata T, Yokoyama Y, Igami T, et al. Hepatopancreatoduodenectomy for cholangiocarcinoma: a single-center review of 85 consecutive patients. Ann Surg. 2012;256:297–305.
Sakamoto Y, Nara S, Kishi Y, et al. Is extended hemihepatectomy plus pancreaticoduodenectomy justified for advanced bile duct cancer and gallbladder cancer? Surgery. 2013;153:794–800.
Aoki T, Sakamoto Y, Kohno Y, et al. Hepatopancreaticoduodenectomy for biliary cancer. Strategies for near-zero operative mortality and acceptable long-term outcome. Ann Surg. 2018;267(2):332–337.
Sugioka A, Kato Y, Tanahashi Y. Systematic extrahepatic Glissonean pedicle isolation for anatomical liver resection based on Laennec’s capsule: proposal of a novel comprehensive surgical anatomy of the liver. JHBPS 2017;24:17–23.
Kawabata Y, Hayashi H, Yano S, et al. Liver parenchyma transection-first approach in hemihepatectomy with en bloc caudate lobectomy for hilar cholangiocarcinoma: A safe technique to secure favorable surgical outcomes. J Surg Oncol. 2017;115:963–970.
Author information
Authors and Affiliations
Contributions
Naokazu Chiba wrote the paper. Naokazu Chiba, Yuta Abe, and Shigeyuki Kawachi were involved with study conception and design. All authors were involved with acquisition, analysis, and interpretation of data.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest
Electronic Supplementary Material
(WMV 242835 kb)
Rights and permissions
About this article
Cite this article
Chiba, N., Abe, Y., Yokozuka, K. et al. Surgical Technique of Pancreatic Parenchyma Transection-Delayed Approach (PPTDA) in Hepatopancreatoduodenectomy for Hilar Cholangiocarcinoma. J Gastrointest Surg 23, 613–616 (2019). https://doi.org/10.1007/s11605-018-3923-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3923-6