Abstract
Purpose
The treatment of acutely obstructed carcinoma of the left colon still represents a matter of controversy. The aim of the study was to evaluate the results of its management by emergency subtotal or total colectomy with immediate anastomosis without diversion.
Methods
An emergency subtotal/total colectomy was performed in 72 patients (mean age 74.9 years). Inclusion criteria were reasonable operative risk, resectable acutely obstructed carcinoma, massively distended colon of dubious viability, and likely to contain ischemic lesions, signs of impending cecal perforation, and masses suggesting synchronous colonic cancers.
Results
Postoperative mortality was 9.7% (7 patients). An 83-year-old woman died as a result of an anastomotic dehiscence; the six other deaths resulted of cardiopulmonary complications. Postoperative morbidity was 15% (11 patients) including two fistulas, which recovered without surgery. There were eight synchronous colon carcinomas. Six months after surgery, the mean daily stool frequency was two following subtotal colectomy and three after total colectomy.
Conclusion
Emergency subtotal colectomy achieves in one-stage relief of bowel obstruction and tumor resection by encompassing a massively distended and fecal-loaded colon with ischemic lesions and serous tears on the cecum. It ensures restoration of gut contiguity via a “safe” ileocolonic anastomosis and removes occasional lesions proximal to the index cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of acutely obstructed carcinoma of the left colon still represents a matter of controversy. Traditionally, left-sided acute bowel obstruction is treated by a staged procedure because immediate resection and anastomosis in a massive distended and unprepared colon carries a high complication rate [1–3]. The cumulative morbidity and mortality of staged procedures, however, are about as high, which has justified a more aggressive approach [1–3].
Increasingly, studies have been published advocating the advantages of primary resection with immediate anastomosis after decompression and cleansing of the obstructed colon [4–8]. The potential benefits include shorter hospital stay, reduced mortality and morbidity rates, and avoidance of a stoma. These advantages, however, have been claimed on the basis of selected patients.
The aims of this study were to review our results of emergency subtotal colectomy with immediate anastomosis without diversion for acute obstructed carcinoma of the left side of the colon and to report our experience.
Patients and methods
Between 1987 and 2003, 156 patients with acute left colonic obstruction presented to our surgical department. Sixty-two patients were treated by segmental resection following intraoperative colonic irrigation, 12 by Hartmann's procedure, and 10 by elective colostomy. An emergency subtotal colectomy or total colectomy with immediate anastomosis without diversion was performed in 72 patients selected from this series of occluded patients. There were 38 men and 34 women aged 29 to 98 (mean 74.9) years. A plain abdominal x-ray film revealed an average cecal diameter of 12.2 cm (range 10–18 cm), while pneumoperitoneum was reported in 2 cases. A gastrograffin (sodium meglumina amidotrizoate) enema examination performed in 45 patients showed complete obstruction in 34 cases, whereas this was incomplete in the remaining 11. A CT scan was performed in 25 patients and confirmed acute left colonic obstruction (descending colon, n=2; proximal sigmoid, n=8; distal sigmoid, n=13; rectosigmoid, n=2). Colonic carcinomas were associated with hepatic metastasis in 4 cases and with suspected synchronous colonic cancers in 4 cases.
Criteria to be met for patients with obstructed cancer of the left colon undergoing emergency subtotal colectomy included reasonable operative risk, resectable obstructing carcinoma, massively distended colon of dubious viability, and likely to contain ischemic lesions, signs of impending cecal perforation, masses suggesting synchronous colonic cancers at the CT scan, and a skilled surgical team.
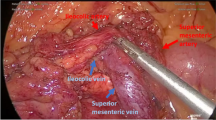
The colon, after mobilization, is resected from the terminal ileum distal to the tumor (minimum distance to the tumor was 5 cm). If a portion of the sigmoid colon was preserved for distal anastomosis, the origin of the inferior mesenteric artery would be preserved and the left colic artery would be ligated and divided at its origin. The inferior mesenteric vein was ligated and divided near the duodenum, thereby permitting a generous removal of mesenteric lymph node. Subtotal colectomy with ileosigmoid anastomosis was performed in 48 patients (66.5%), while 24 (33.5%) patients underwent a total colectomy with ileorectal anastomosis. There were 54 side-to-end anastomosis, 12 side-to-side, and 6 end-to-end. Forty-nine anastomoses were hand-sewn, whereas 23 were performed with stapling devices. Associated procedures included one splenectomy for splenic tears, two liver resections for hepatic metastases (one left lobectomy and one segmentectomy), three oophorectomies, and 10 cholecystectomies for associated gallbladder lithiasis. Decompression enterotomies were needed in 6 patients with competent ileocecal valve.
We assessed immediate postoperative results, analyzing mortality and morbidity rates and hospital stay. We also analyzed frequency of bowel movements during the first 6 months after subtotal or total colectomy.
Results
All index adenocarcinoma were respectable. Twenty-four neoplasms were localized on the midsigmoid, 30 on the proximal sigmoid, 5 on the rectum, while 13 were in the descending colon. All patients had a massively distended colon of dubious vitality. Serosal tears on the cecum, as a sign of impending perforation, were reported in 27 cases (37.5%), while perforation was found in those 2 patients with pneumoperitoneum, thought to have no fecal peritonitis.
Pathological examination of the specimens confirmed colonic carcinoma in the 72 patients (stage B: 30 cases, stage C: 29 cases, stage D: 13 cases) and revealed eight synchronous carcinoma (11%) localized on right colon (n=5), transverse colon (n=1), and descending colon (n=2). The mean number of examined lymph nodes was 20±7.7 (range 14–59). Ischemic lesions in distended colon were confirmed by histopathological analysis in all cases.
Postoperative mortality was 9.7% (7 patients). An 83-year-old woman died as a result of an anastomotic leak after a side-to-side stapled ileorectostomy on postoperative day 8. The six other deaths were attributed to pulmonary embolus (n=1), postoperative aspiration pneumonia (n=1), vascular cerebral disease (n=1), and cardiac failure (n=3). These seven deaths occurred in patients over 83 years (range 83–98 years). No mortality was attributed to an additional procedure. There was a morbidity of 15% (11 patients) including anastomotic fistula (n=2), candida albicans septicemia (n=1), arrhythmia (n=1), phlebitis (n=1), and wound infection (n=6). All these patients recovered without further surgery. The average hospital stay was 16 days (range 10–28 days). In the immediate postoperative period, 13 (20%) patients, 10 of whom had ileorectal anastomosis, complained of diarrhea, but recovered rapidly with antidiarrheal medication. In no case did fecal incontinence occur. All patients were interviewed about their stool frequency. No patient relied on the regular use of antidiarrheal drugs, and stool frequency was as shown in Table 1. No symptomatic anastomotic stricture was observed.
Discussion
Surgical treatment of acute left-sided colonic obstruction is a major procedure. The proximal colon is distended and filled with liquid faces, and its wall is often of dubious viability with signs of impending catcall perforation. Bowel contents are easily spilled through tears that are caused by distension or produced during mobilization. Primary anastomosis in left colonic obstruction bears the increased risk of breakdown because the unprepared colon is filled with large amounts of liquid fecal residue. Primary resection with immediate anastomosis is therefore associated with a high anastomotic leak rate and mortality [1, 3].
The surgical management of left-sided malignant large bowel obstruction has evolved considerably in the past few decades. The treatment consisted of a three-stage operation: formation of a colostomy followed later by resection with a further admission to hospital for closure of the colostomy; this approach was gradually superseded by a two-stage operation consisting of primary excision of the tumor with an end colostomy (Hartmann's procedure) and subsequent restoration of bowel continuity. Each stage has its own incidence of morbidity and mortality. In the study of Wigmore et al. [9], the overall postoperative morbidity rate of patients undergoing restoration of intestinal continuity was 29%, with 3.9% of anastomotic leak. Furthermore, restoration of intestinal continuity following Hartmann's procedure is about 70% in the literature. Wigmore et al. [9] reported 48% of no reversed patients. This rate increased when initial diagnosis was malignancy disease.
The safety of a primary colonic anastomosis can be increased by removing the feces during the surgical procedure. Saline solution is flushed through a tube in the cecum or ileum and drained together with colonic contents through a tube inserted proximal to the obstructing tumor (antegrade lavage) [10–13]. Another method is “surgical bowel preparation” in which distended proximal colon is removed (subtotal colectomy), and with it are all grass fecal residue [6, 12–16]. The distal colon never poses a problem, as it is well decompressed with minimal, if any, stool distal to the obstruction.
The results of these two surgical procedures with immediate resection and anastomosis have a lower reported morbidity and mortality than those of staged procedures [11–17]. The mortality and morbidity rates in the present study were similar to that reported in the recent literature: 2 to 13% and 12 to 40%, respectively [18–25] (Table 2).
These procedures relieve the obstruction, remove the tumor, and restore digestive continuity; as a result, total hospital stay is shorter, a temporary diverting stoma is not necessary, and the cost of medical care is less [12]. Although several reports have been published on small series of patients treated by subtotal colectomy or by segmental resection following intraoperative irrigation, the SCOTIA study [12] was the first prospective randomized trial comparing these two surgical treatments. In this study, no significant difference was observed in the two surgical procedures concerning hospital mortality and complication rate, but 4 months after operation, increased bowel frequency was significantly more common in the subtotal colectomy group.
In our experience, subtotal colectomy is commonly advocated as the preferred option, as on-table irrigation is rather messy and complicated, and operating time is prolonged. The risk of complication as a result of serosal tears or necrosis is eliminated; manipulation of the massively distended colon to insert the tubes causes an extra risk of rupture of the colonic wall, and disconnection of the tubes is also avoided [12]. One of the arguments for subtotal colectomy is that this procedure will remove synchronous proximal neoplasms and reduce the risk of subsequent metachronous tumor development compared with segmental resection [7, 21]. In our series, eight patients (11%) were found to have synchronous tumors. The possible advantage of subtotal colectomy in reducing the risk of metachronous tumors may be offset by postoperative coloscopic surveillance of patients who have had segmental colectomy. The rate of synchronous cancer is generally reported at 3 to 10% [18, 26–28]. Nowadays, computed tomographic colonography is an important diagnostic technique for preoperative evaluation of proximal colon in patients with distal occlusive carcinomas, as it gives good results and is well tolerated and less invasive [29]. In a recent study with decision analysis (Markov), unless surveillance results improve, subtotal colectomy still seems the preferred treatment for primary colorectal carcinoma in hereditary nonpolyposis colorectal cancer in view of the difference in life expectancy [30]. In the recent literature, there is no argument for the use of subtotal colectomy to avoid metachronous carcinomas, outside hereditary tumor syndromes.
After subtotal colectomy, it is common for the number of bowel movements to increase during the immediate postoperative period; however, this situation is temporary. In our series, the frequency of bowel movements fails or stabilizes spontaneously or with antidiarrheal medications (1–4 movements per days), disabling diarrhea being a rare occurrence [15, 20, 21]. Postoperative diarrhea appears more frequently when an ileorectal anastomosis is performed [6, 12, 15, 20].
In conclusion, emergency subtotal colectomy achieves in one-stage relief of bowel obstruction and tumor resection by encompassing a massively distended and fecal-loaded colon with ischemic lesions and serosals tears on the cecum, ensures restoration of gut continuity via a “safe” ileocolonic anastomosis, and removes occasional lesions proximal to the index cancer. Although advances in metal stents use might significantly influence the surgical approach to obstructed carcinoma of the colon, total or subtotal colectomy can be regarded as an acceptable operation in selected patients, provided that a skilled surgical team is available.
References
Clark J, Hall A, Mussa AR (1975) Treatment of obstructing cancer of the colon and rectum. Surg Gynecol Obstet 141:541–544
Carson SN, Poticha SM, Shields TW (1977) Carcinoma obstructing the left side of the colon. Arch Surg 122:523–526
Phillips RKS, Hittinger R, Fry JS, Fielding LP (1985) Malignant large bowel obstruction. Br J Surg 72:296–302
Deutsch AA, Zelikovski A, Sternberg A, Reiss R (1983) One-stage subtotal colectomy with anastomosis for obstructing carcinoma of the left colon. Dis Colon Rectum 26:227–230
Pollock AV, Palyforth MJ, Evans M (1987) Perioperative lavage of the obstructed left colon to allow safe primary anastomosis. Dis Colon Rectum 30:171–173
Stephenson BM, Shandall AA, Farouk R, Griffith G (1990) Malignant left-sided large bowel obstruction managed by subtotal/total colectomy. Br J Surg 77:1098–1102
Carty NJ, Corder AP, Johnson CD (1993) Colostomy is no longer appropriate in the management of uncomplicated large bowel obstruction: true or false? Ann R Coll Surg Engl 75:46–51
Deans GT, Krukowski ZH, Irwin ST (1994) Malignant obstruction of the left colon. Br J Surg 81:1270–1276
Wigmore SJ, Duthie GS, Young IE, Spalding EM, Rainey JB (1995) Restoration of intestinal continuity following Hartmann's procedure: the Lothian experience 1987–1992. Br J Surg 82:7–30
Dudley HAF, Radcliffe AG, McGeehan D (1980) Intra-operative irrigation of the colon to permit primary anastomosis. Br J Surg 67:80–81
Meijer S, Hoitsma HFW, Van Loenhout RM (1989) Intraoperative antegrade irrigation in complicated left-sided colonic cancer. J Surg Oncol 40:88–89
The SCOTIA Study Group (1995) Single-stage treatment for malignant left-sided colonic obstruction: a prospective randomised clinical trial comparing subtotal colectomy with segmental resection following intraoperative irrigation. Br J Surg 82:1622–1627
Torralba JA, Robles R, Parrilla P, Lujan JA, Liron R, Pinero A, Fernandez JA (1998) Subtotal colectomy versus intraoperative colonic irrigation in the management of obstructed left colon carcinoma. Dis Colon Rectum 41:18–22
Hughes ES (1970) Subtotal colectomy for carcinoma of the colon. J R Soc Med 63:41–42
Halevy A, Levi J, Orda R (1989) Emergency subtotal colectomy: a new trend for treatment of obstructing carcinoma of the left colon. Ann Surg 210:220–223
Arnaud JP, Bergamaschi R (1994) Emergency subtotal/total colectomy with anastomosis for acutely obstructed carcinoma of the left colon. Dis Colon Rectum 37:685–688
Murray JJ, Schoetz DJ Jr, Coller JA, Roberts PL, Veidenheimer MC (1991) Intraoperative colonic lavage and primary anastomosis in non elective colon resection. Dis Colon Rectum 34:527–531
Huang TJ, Wang JY, Lee LW, Chen FM, Chuan CH, Chan HM, Hou MF, Huang CJ, Huang YS, Hsieh JS (2002) Emergency one-stage surgery for obstructing left-sided colorectal carcinomas. Kaohsiung J Med Sci 18:323–328
Hsu TC (1998) One-stage resection and anastomosis for acute obstruction of the left colon. Dis Colon Rectum 41:28–32
Papa MZ, Karni T, Koller M, Klein E, Scott D, Bersuk D, Sareli M, Ben Ari G (1997) Avoiding diarrhea after subtotal colectomy with primary anastomosis in the treatment of colon cancer. J Am Coll Surg 184:269–272
Reemst PHM, Kuijpers HC, Wobbes T (1998) Management of left-sided colonic obstruction by subtotal colectomy and ileocolic anastomosis. Eur J Surg 164:537–540
Naraynsingh V, Rampaul R, Maharaj D, Kuruvilla T, Ramcharan K, Pouchet B (1999) Prospective study of primary anastomosis without colonic lavage for patients with an obstructed left colon. Br J Surg 86:1341–1343
Park UC, Chung SS, Kim KR, Seong MK, Yoon WH, Kim YJ et al (2004) Single-stage procedure with intraoperative colonoscopy and colonic irrigation in patients with obstructing left-sided colonic cancer. Int J Colorectal Dis 19:487–492
Hsu TC (2005) Comparison of one-stage resection and anastomosis of acute complete obstruction of left and right colon. Am J Surg 189:384–387
Lim JF, Tang CL, Seow-Choen F, Heah SM (2005) Prospective, randomized trial comparing intraoperative colonic irrigation with manual decompression only for obstructed left-sided colorectal cancer. Dis Colon Rectum 48:205–209
Passman MA, Pommier RF, Vetto JT (1996) Synchronous colon primaries have the same prognosis as solitary colon cancers. Dis Colon Rectum 39:329–334
Arenas RB, Fichera A, Mhoon D, Michelassi F (1997) Incidence and therapeutic implications of synchronous colonic pathology in colorectal adenocarcinoma. Surgery 122:706–710
Brief DK, Brener BJ, Goldenkranz R et al (1991) Defining the role of subtotal colectomy in the treatment of carcinoma of the colon. Ann Surg 213:248–252
Ridereau-Zins C, Leblay F, Aube C, Croquet V, Pessaux P, Pilleul F et al (2002) Etude de faisabilité et premiers résultats du coloscanner à l'eau. J Radiol 83:1460
De vos tot Nederveen Cappel WH, Buskens E, Van Duijvendijk P, Cats A, Menko FH, Griffioen G, Slors JF, Nagengast FM, Kleibeuker JH, Vasen HF (2003) Decision analysis in the surgical treatment of colorectal cancer due to a mismatch repair gene defect. Gut 52:1752–1755
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hennekinne-Mucci, S., Tuech, JJ., Bréhant, O. et al. Emergency subtotal/total colectomy in the management of obstructed left colon carcinoma. Int J Colorectal Dis 21, 538–541 (2006). https://doi.org/10.1007/s00384-005-0048-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-005-0048-7